Abstract
Rationale:
Ethylenediaminetetraacetic acid-dependent pseudothrombocytopenia (EDTA-PTCP) is a rare phenomenon characterized by spuriously low platelet counts when EDTA reacts with harvested blood. However, to the best of our knowledge, only two cases involving EDTA-PTCP in postoperative patients with sepsis have been reported. Here, we describe a case of EDTA-PTCP that appeared transiently in a postoperative patient with sepsis.
Patient Concerns:
A 68-year-old female patient underwent laparoscopic tension-free hernioplasty for incisional hernia. Postoperatively, the patient developed very low platelet counts. The number of platelets in this patient had not improved following treatment with fresh-frozen plasma and platelet transfusions.
Diagnoses:
The diagnosis of EDTA-PTCP was confirmed from the discovery of platelet aggregation in peripheral blood smears.
Interventions:
We used sodium citrate-anticoagulated blood samples for platelet counting.
Outcomes:
The patient's platelet counts returned to normal with the use of sodium citrate-anticoagulated blood samples. Furthermore, the phenomenon of EDTA-PTCP disappeared when the patient was cured.
Lessons:
The phenomenon of low platelet counts in postoperative patients with sepsis should be considered as possible EDTA-PTCP. In addition, peripheral blood smears and the use of sodium citrate anticoagulant are effective and valuable methods that can help identify EDTA-PTCP.
Keywords: EDTA, postoperative, pseudothrombocytopenia, sepsis, transient appearance
1. Introduction
Ethylenediaminetetraacetic acid-dependent pseudothrombocytopenia (EDTA-PTCP) is characterized by spuriously low platelet counts, as measured by automated analyzers.[1] This phenomenon occurs as in vitro platelet clumps caused by antiplatelet autoantibodies in EDTA-anticoagulated blood.[2] EDTA-PTCP has an incidence of ∼0.1% to 0.21% in both healthy subjects and hospitalized patients.[3–6] Furthermore, it is very easy for clinicians to overlook the signs of EDTA-PTCP, resulting in excessive examination and unnecessary platelet transfusions. More importantly, transient EDTA-PTCP has been reported in only a few cases.[7–9] In this report, we outline a case of EDTA-PTCP that appeared transiently in a postoperative patient with sepsis.
2. Case report
A 68-year-old woman underwent laparoscopic tension-free hernioplasty for incisional hernia. She had a history of repair of sigmoid perforation. The platelet count was found to be 224.1 × 109/L before operation. The surgical procedures performed were done without reports of excessive bleeding or hemorrhagic complications and the surgery was a success. However, on the 4th postoperative day (POD), a routine blood cell count showed a low platelet count with a value of 70.8 × 109/L. Test tubes containing EDTA were used to collect the blood and erythrocyte counts were obtained on an automated analyzer (COULTER LH750 Hematology Analyzer, Beckman Coulter, Inc., Harbor Blvd Fullerton, US).
As disease progressed, the patient suddenly developed shortness of breath, chest tightness, dizziness, abdominal distension, and nausea. Laboratory investigation revealed a low platelet count (36.9 × 109/L) and a low white blood cell count (3.32 × 109/L). In addition, culture from a purulent secretion revealed the growth of Escherichia coli, as well as a level of 54.51 pg/mL in serum endotoxin, indicating sepsis. Furthermore, an abdominal computed tomography scan showed extensive gas-fluid levels in the intestinal tract and intestinal wall swelling, consistent with acute intestinal obstruction. The patient underwent exploratory laparotomy, which confirmed intra-abdominal infections. Results of other arterial blood gas analyses were abnormal (PaO2, 51 mmHg; PaCO2, 45 mm Hg), indicating respiratory failure. As a result, the patient was transferred to the intensive care unit on the 6th POD.
On the ward, the patient was treated with fresh-frozen plasma and platelet transfusions, teicoplanin, ornidazole, imipenem, and cilastatin sodium. However, the patient failed to respond to continuous platelet transfusions. Up until the 10th POD, cell counts were measured by collecting the patient's blood containing anticoagulant EDTA or sodium citrate. The number of platelets with EDTA was 7.20 × 109/L, whereas with sodium citrate was 136.00 × 109/L (Fig. 1). Moreover, platelet clumps were identified by the microscopic examination of blood smears (Fig. 2), indicating pseudothrombocytopenia. With the resolution of infection, the phenomenon of EDTA-PTCP disappeared.
Figure 1.
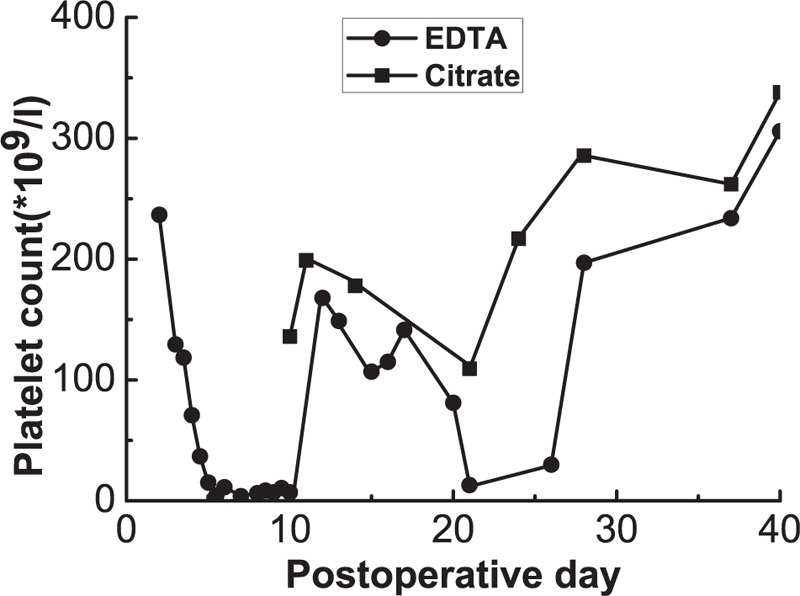
Changes in platelet counts in EDTA (circles) and citrate (squares) anticoagulated blood. On the 10th postoperative day, blood drawn into an EDTA tube showed aggregation compared with blood drawn into a citrate tube. EDTA = ethylenediaminetetraacetic acid.
Figure 2.

An example picture (Wright Stain, 100×) of platelet aggregation (black arrow) in blood smear of an EDTA-anticoagulated sample and no platelet aggregation (black arrow) in blood smear of a citrate-anticoagulated sample.
3. Discussion
EDTA-dependent pseudothrombocytopenia (EDTA-PTCP) is an in vitro phenomenon of false low platelet counts because of antiplatelet autoantibodies resulting in platelet aggregation in EDTA-anticoagulated blood by automated analyzers.[1,2] According to previous studies, EDTA can dissociate the Ca2+-dependent platelet membrane glycoprotein (GP) IIb/IIIa heterodimer by its chelating calcium.[10–13] Meanwhile, these antiplatelet autoantibodies, mainly in the form of immunoglobulin (Ig) M, IgG, or IgA subsets,[14,15] recognize the exposure of the epitopes on GPIIb/IIIa leading to platelet clumps. In addition, agglutination appears to occur more readily at cold temperature rather than at 37°C.[16]
The precise cause of EDTA-PTCP is still unknown. The phenomenon of EDTA-induced platelet aggregation was first reported by Gowland et al[17] in 1969. Until now, this phenomenon has been observed in patients with autoimmune diseases, neoplastic diseases, liver diseases, cardiovascular diseases, and viral infections.[1,18–21] It has been suggested that EDTA-PTCP may be an acquired phenomenon.[22] Our case, a remarkable diagnosis of EDTA-PTCP with the development of postoperative infection, is consistent with this view. In contrast, other researchers have shown that EDTA-PTCP had little to do with any particular pathology or use of specific drugs and was present in healthy subjects and also patients with various diseases.[15] They suggest that EDTA-PTCP is related to natural autoantibodies with antiplatelet activity, devoid of pathological significance. In addition, Van der Lelie et al[23] found that platelet autoantibodies were strictly or partially EDTA-dependent in patients with septicemia. They proposed that these antibodies are mainly directed against cryptantigens, which are exposed in vivo only on platelets damaged by septicemia and in vitro in the presence of EDTA. With regards to this case, one possible explanation for the appearance of EDTA-PTCP may be because of the damage of bacterial toxins or inflammatory factors to platelets, leading to the exposure of cryptic antigens. Another possible reason may be that the same antigenic determinant, in both bacterial antigens and exposed cryptic antigens on platelets, caused antigenic cross-reaction. Unfortunately, because of the limitations of our study, we could not provide any supporting evidence for this hypothesis. We were also unable to demonstrate that the mechanisms underlying EDTA-PTCP disappeared with the resolution of infection. However, to the best of our knowledge, such cases of EDTA-PTCP have been described only sporadically in the literature.[7,8]
The recognition of EDTA-PTCP by laboratory staff and physicians plays an important role in clinical diagnosis and treatment. When patients with significantly low platelet counts do not match clinical expectations, the following methods in routine hematological laboratory testing are effective at identifying EDTA-PTCP. Firstly, anticoagulated blood with amikacin can be used or test tubes containing alternative anticoagulants, such as sodium citrate and magnesium sulfate, can be used.[24–26] Secondly, examination of the peripheral blood smears, widely regarded as the gold standard for the detection of EDTA-PTCP, should be applied. Finally, more sophisticated techniques include the use of flow cytometric analysis or the observation of typical patterns of a platelet and white blood cell histograms using hematology analyzers.[27,28] Lastly, any case of newly-occurring low platelet count should always be considered a possible cause of EDTA-PTCP, particularly in patients with postoperative complications.
Acknowledgments
The authors would like to thank the patient featured in this case report. The patient's consent was obtained by and approved by the ethics committee of the First Affiliated Hospital of Guangxi Medical University.
Footnotes
Abbreviations: EDTA-PTCP = ethylenediaminetetraacetic acid-dependent pseudothrombocytopenia, POD = postoperative day.
XS and ZL contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Shreiner DP, Bell WR. Pseudothrombocytopenia: manifestation of a new type of platelet agglutinin. Blood 1973;42:541–9. [PubMed] [Google Scholar]
- [2].Pegels JG, Bruynes EC, Engelfriet CP, et al. Pseudothrombocytopenia: an immunologic study on platelet antibodies dependent on ethylene diamine tetra-acetate. Blood 1982;59:157–61. [PubMed] [Google Scholar]
- [3].Payne BA, Pierre RV. Pseudothrombocytopenia: a laboratory artifact with potentially serious consequences. Mayo Clinic Proc 1984;59:123–5. [DOI] [PubMed] [Google Scholar]
- [4].Garcia Suarez J, Merino JL, Rodriguez M, et al. Pseudothrombocytopenia: incidence, causes and methods of detection. Sangre 1991;36:197–200. [PubMed] [Google Scholar]
- [5].Garcia Suarez J, Calero MA, Ricard MP, et al. EDTA-dependent pseudothrombocytopenia in ambulatory patients: clinical characteristics and role of new automated cell-counting in its detection. Am J Haematol 1992;39:146–8. [DOI] [PubMed] [Google Scholar]
- [6].Bartels PC, Schoorl M, Lombarts AJ. Screening for EDTA-dependent deviations in platelet counts and abnormalities in platelet distribution histograms in pseudothrombocytopenia. Scand J Clin Lab Invest 1997;57:629–36. [DOI] [PubMed] [Google Scholar]
- [7].Mori M, Kudo H, Yoshitake S, et al. Transient EDTA-dependent pseudothrombocytopenia in a patient with sepsis. Intensive Care Med 2000;26:218–20. [DOI] [PubMed] [Google Scholar]
- [8].Wenzel F, Lasshofer R, Rox J, et al. Transient appearance of postoperative EDTA-dependent pseudothrombocytopenia in a patient after gastrectomy. Platelets 2011;22:74–6. [DOI] [PubMed] [Google Scholar]
- [9].Ohno N, Kobayashi M, Hayakawa S, et al. Transient pseudothrombocytopenia in a neonate: transmission of a maternal EDTA-dependent anticoagulant. Platelets 2012;23:399–400. [DOI] [PubMed] [Google Scholar]
- [10].Fitzgerald LA, Phillips DR. Calcium regulation of the platelet membrane glycoprotein IIb–IIIa complex. J Biol Chem 1985;260:11366–74. [PubMed] [Google Scholar]
- [11].Rivas GA, Gonzalez-Rodriguez J. Calcium binding to human platelet integrin GPIIb/IIIa and to its constituent glycoproteins. Effects of lipids and temperature. Biochem J 1991;276(pt 1):35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Golanski J, Pietrucha T, Baj Z, et al. A novel approach to inhibit the anticoagulant-induced spontaneous activation of blood platelets—effect of magnesium on platelet release reaction in whole blood. Thromb Res 1997;85:127–32. [DOI] [PubMed] [Google Scholar]
- [13].Chae H, Kim M, Lim J, et al. Novel method to dissociate platelet clumps in EDTA-dependent pseudothrombocytopenia based on the pathophysiological mechanism. Clin Chem Lab Med 2012;50:1387–91. [DOI] [PubMed] [Google Scholar]
- [14].Imai H, Nakamoto Y, Miki K, et al. Pseudothrombocytopenia and IgA-related platelet agglutinin in a patient with IgA nephritis. Nephron 1983;34:154–8. [DOI] [PubMed] [Google Scholar]
- [15].Bizzaro N. EDTA-dependent pseudothrombocytopenia: a clinical and epidemiological study of 112 cases, with 10-year follow-up. Am J Haematol 1995;50:103–9. [DOI] [PubMed] [Google Scholar]
- [16].Isobe T, Fujita T, Kinoshita S, et al. Pseudothrombocytopenia with cold-type platelet agglutinins. Jpn J Med 1983;22:9–13. [DOI] [PubMed] [Google Scholar]
- [17].Gowland E, Kay HE, Spillman JC, et al. Agglutination of platelets by a serum factor in the presence of EDTA. J Clin Pathol 1969;22:460–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sahin C, Kirli I, Sozen H, et al. EDTA-induced pseudothrombocytopenia in association with bladder cancer. BMJ Case Rep 2014;2014:bcr2014205130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tomonari A, Hirai K, Aoki H, et al. Pure red cell aplasia and pseudothrombocytopenia associated with hepatitis A. Jpn J Clin Haematol 1991;32:147–51. [PubMed] [Google Scholar]
- [20].Saburi Y, Aragaki M, Matsui S, et al. An adult patient with EDTA-dependent pseudothrombocytopenia due to rubella virus infection. Kansenshogaku Zasshi 1993;67:594–7. [DOI] [PubMed] [Google Scholar]
- [21].Sawazaki A, Nakamura N, Jyokaji H, et al. Guillain-Barre syndrome and ethylene diamine tetraacetic acid-dependent pseudothrombocytopenia associated with mumps. Int Med (Tokyo, Japan) 1996;35:996–9. [DOI] [PubMed] [Google Scholar]
- [22].Berkman N, Michaeli Y, Or R, et al. EDTA-dependent pseudothrombocytopenia: a clinical study of 18 patients and a review of the literature. Am J Haematol 1991;36:195–201. [DOI] [PubMed] [Google Scholar]
- [23].van der Lelie J, van der Plas-Van Dalen CM, von dem Borne AE. Platelet autoantibodies in septicaemia. Brit J Haematol 1984;58:755–60. [DOI] [PubMed] [Google Scholar]
- [24].Schuff-Werner P, Steiner M, Fenger S, et al. Effective estimation of correct platelet counts in pseudothrombocytopenia using an alternative anticoagulant based on magnesium salt. Brit J Haematol 2013;162:684–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lombarts AJ, Zijlstra JJ, Peters RH, et al. Accurate platelet counting in an insidious case of pseudothrombocytopenia. Clin Chem Lab Med 1999;37:1063–6. [DOI] [PubMed] [Google Scholar]
- [26].Zhou X, Wu X, Deng W, et al. Amikacin can be added to blood to reduce the fall in platelet count. Am J Clin Pathol 2011;136:646–52. [DOI] [PubMed] [Google Scholar]
- [27].Nishioka T, Yokota M, Tsuda I, et al. Flow cytometric analysis of platelet activation under calcium ion-chelating conditions. Clin Lab Haematol 2002;24:115–9. [DOI] [PubMed] [Google Scholar]
- [28].Nagler M, Keller P, Siegrist D, et al. A case of EDTA-dependent pseudothrombocytopenia: simple recognition of an underdiagnosed and misleading phenomenon. BMC Clin Pathol 2014;14:19. [DOI] [PMC free article] [PubMed] [Google Scholar]


