Abstract
Background:
To compare medical students’ skills for vaginal operative delivery by vacuum extraction (VE) after hands-on training versus video demonstration.
Methods:
We randomized medical students to an expert demonstration (group 1) or a hands-on (group 2) training using a standardized VE algorithm on a pelvic training model. Students were tested with a 40-item Objective Structured Assessment of Technical Skills (OSATS) scoring system after training and 4 days later. OSATS scores were the primary outcome. Performance time, self-assessment, confidence, and global rating scale were secondary outcomes. We assessed the constructive validity of OSATS in this VE model comparing metric scores of experts and students.
Results:
In all, 137 students were randomized. OSATS scores were higher in group 2 (n = 63) compared with group 1 (n = 74) (32.89 ± 6.39 vs 27.51 ± 10.27, respectively; P < 0.0001). Global rating scale (1.49 ± 0.76 vs 2.33 ± 0.94, respectively; P < 0.0001), confidence (2.22 ± 0.75 vs 3.26 ± 0.94, respectively; P = 0.04), self-assessment (2.03 ± 0.62 vs 2.51 ± 0.77, respectively; P < 0.0001), and performance time (38.81 ± 11.58 seconds vs 47.23 ± 17.35 seconds, respectively; P = 0.001) also favored group 2. After 4 days, this effect persisted with OSATS scores still being significantly higher in group 2 (30.00 ± 6.50 vs 25.59 ± 6.09, respectively; P = 0.001). The assessed OSATS scores showed constructive validity. In a multiple linear regression analysis, group assignment independently influenced OSATS scores, whereas sex, handedness, sports activities, and type of curriculum were not independently associated with OSATS scores.
Conclusions:
Hands-on training is superior to video demonstration for teaching VE on a pelvic model.
Keywords: delivery, operative vaginal delivery, OSATS, randomized controlled trial, technical skills, training, vacuum extraction
1. Introduction
Vaginal operative delivery occurs in 15% of all deliveries.[1] Forceps and vacuum extractors are commonly used for vaginal operative delivery based on randomized trials demonstrating the feasibility, safety, and comparable efficacy of these methods.[2] However, the use of those instruments can provoke serious complications such as fourth-degree tears, fetal facial injury, or fetal asphyxia.[3–6]
Whatever the specific technique used in a given obstetric hospital, teaching obstetric residents the technique of vacuum extraction (VE) is challenging. Traditionally, residents gain experience with VE performance using a learning-by-doing approach under expert guidance. However, many vaginal operative deliveries are performed under stressful conditions due to maternal or fetal distress. This interferes with the efficiency of the teaching and learning process, since it is well-known that teaching and also learning performance is hampered by stress.[7] Also, it is ethically questionable to teach residents obstetric techniques with women as study objects, especially in the early stages of surgical training.[8]
Low and high-fidelity training models and simulators have therefore been tested as potentially effective tools to enhance technical performance of medical staff.[8–11] Based on these data, standardized trainings on pelvic models may be potentially useful to prepare residents before they start to perform VEs on women. No data have been published regarding the validity of various training methods of VE (PUBMED search; 03-february-2016; search terms: vacuum extraction, training, model, randomized, pelvic trainer, vaginal operative delivery).
Since surgical and manual obstetric techniques such as hysteroscopy, resolution of a shoulder dystocia, and vaginal delivery for breech presentation can be effectively trained with dummy models,[12–16] it is reasonable to assume that dummy trainings for VE may also be effective. Previously, our group has demonstrated that Objective Structured Assessment of Technical Skills (OSATS) in combination with pelvic dummy training can effectively improve the skills of obstetric trainees.[12,14] Specifically, we have shown in a randomized trial of 172 medical students that OSATS scores, performance time (PT), global effectiveness, and confidence (CON) for vaginal delivery for breech presentation were significantly higher after hands-on dummy training compared with demonstration alone.[14] In another randomized trial, we randomized 203 probands to a 30-minute hands-on and a 30-minute demonstration training session, teaching a standardized shoulder dystocia management scheme on a pelvic training model. In this study, hands-on dummy training helped to achieve a significant improvement of shoulder dystocia management. OSATS scores, and also PT, global effectiveness, self-assessment (SA), and CON were significantly higher after hands-on dummy training.[12]
The present study adds to and builds on these previous OSATS studies in a number of ways. For example, in the present study, we have added participant characteristics such as handedness and sports activities to the multivariate analysis. Also, the OSATS procedure has been improved compared with the previous studies using a number of metric scores. Also, we used a standardized teaching video in the control group to avoid intra and interteacher variabilities observed in previous experiments. Lastly, we tested for constructive validity using a comparison of metric scores between experts and nonexperts.
In the present study, we tested the hypothesis that hands-on training of VE in a pelvic training model is more effective than expert video training with effectiveness defined as high OSATS scores. To test this hypothesis, we designed a randomized controlled trial measuring OSATS scores of students working through a defined VE management algorithm after a 30-minute hands-on training compared with a 30-minutes expert demonstration using a training video (https://youtu.be/XpZOHSq2-qA). To test for immediate and also delayed training effects, we tested students immediately after training (day 1) and retested them after 4 days (day 5).
2. Methods
This randomized, single-blinded, single-center trial was carried out between May 2015 and October 2015 at the Department of Obstetrics and Gynecology, Ruhr University Bochum, Bochum, Germany. The study participants were medical students who did an Obstetrics rotationship. This randomized study was approved by the local Ethics Committee (approval number: 4999–14; Date of approval: 23.10.2014). The trial was registered with ClinicalTrials.gov (NCT02468427). Informed consent was obtained from all study participants. Figure 1 shows a CONSORT diagram of the students flow through the study. There were no specific inclusion or exclusion criteria other than informed consent and language barrier. For group assignment, we used a computer-generated randomization list, with a 1:1 allocation ratio without blocking. After randomization, students were allocated to different rooms, where the hands-on training and the video training session took place. The assessor (A.K.), who tested the students afterwards, was not present at the allocation, during the hands-on training, and during the video training session. Thus, the assessor was unaware of the participants’ group assignment. Students allocated to group 1 underwent a 30-minute video training session, watching an instruction video demonstrating all 40 items of VE as listed in Table 1. The video was produced by our Department and is in use for resident training purposes. In this 30-minute training video, 1 of the authors (C.T.) acts as an expert instructor, demonstrating all 40 steps of performing a VE according to the OSATS checklist used in this study (Table 1). For the training video, we used the same pelvic training model also used in the study (Phantom; Schultes Medacta, Germany). Students allocated to group 2 underwent a 30-minute hands-on training session with the students performing all 40 items of VE as listed in Table 1 at least once under expert instruction. The key maneuvers were as follows: vaginal digital examination, correct diagnosis of fetal lie, placement of the cup, episiotomy, correct traction, and delivery of the fetal head. Also, additional items such as establishing the indication for VE, information of a senior obstetrician and anesthesiologist, or addition of oxytocin and emptying of the bladder were part of the OSATS (Table 1). The pelvic model and the model of the baby used in this study allowed the correct determination of the fetal position. We used a soft cup, single use vacuum extractor (KIWI OmniCup Single Use VAC 6000 M; Clinical Innovations LLC, South Murray), licensed in the EU, for obstetric use.
Figure 1.
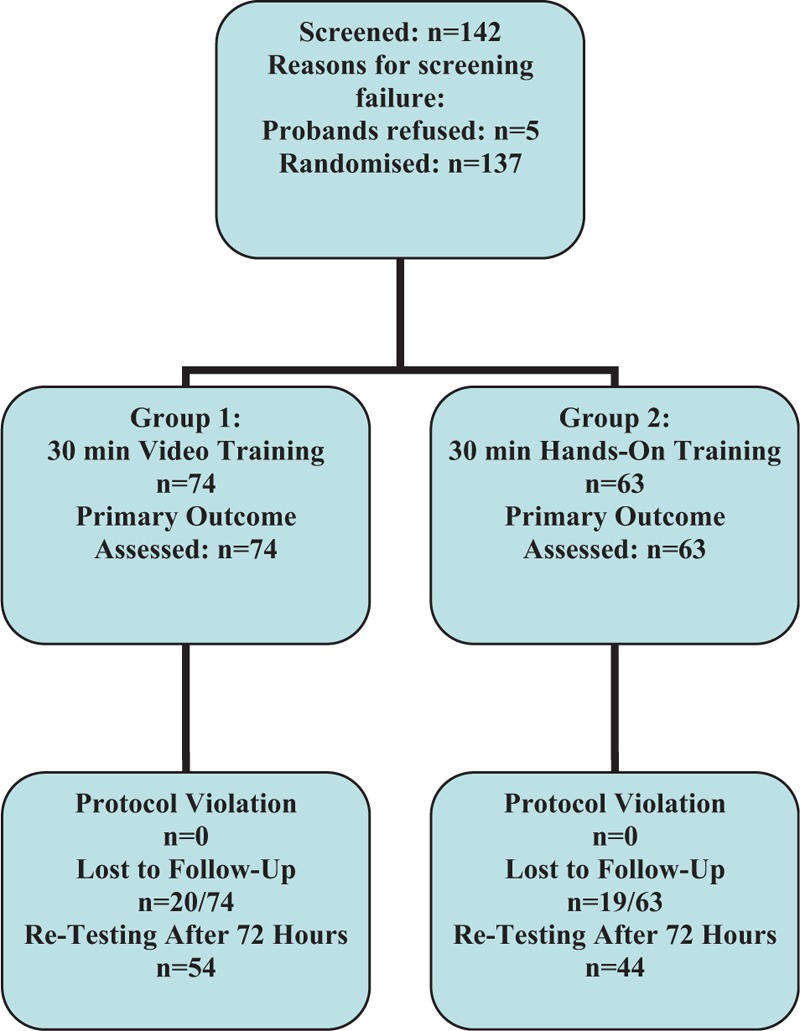
Consort diagram of the students flow through the study.
Table 1.
Objective Structured Assessment of Technical Skills (OSATS) checklist using 40 items to test proficiency in performing a vacuum extraction (VE) on a pelvic training model.
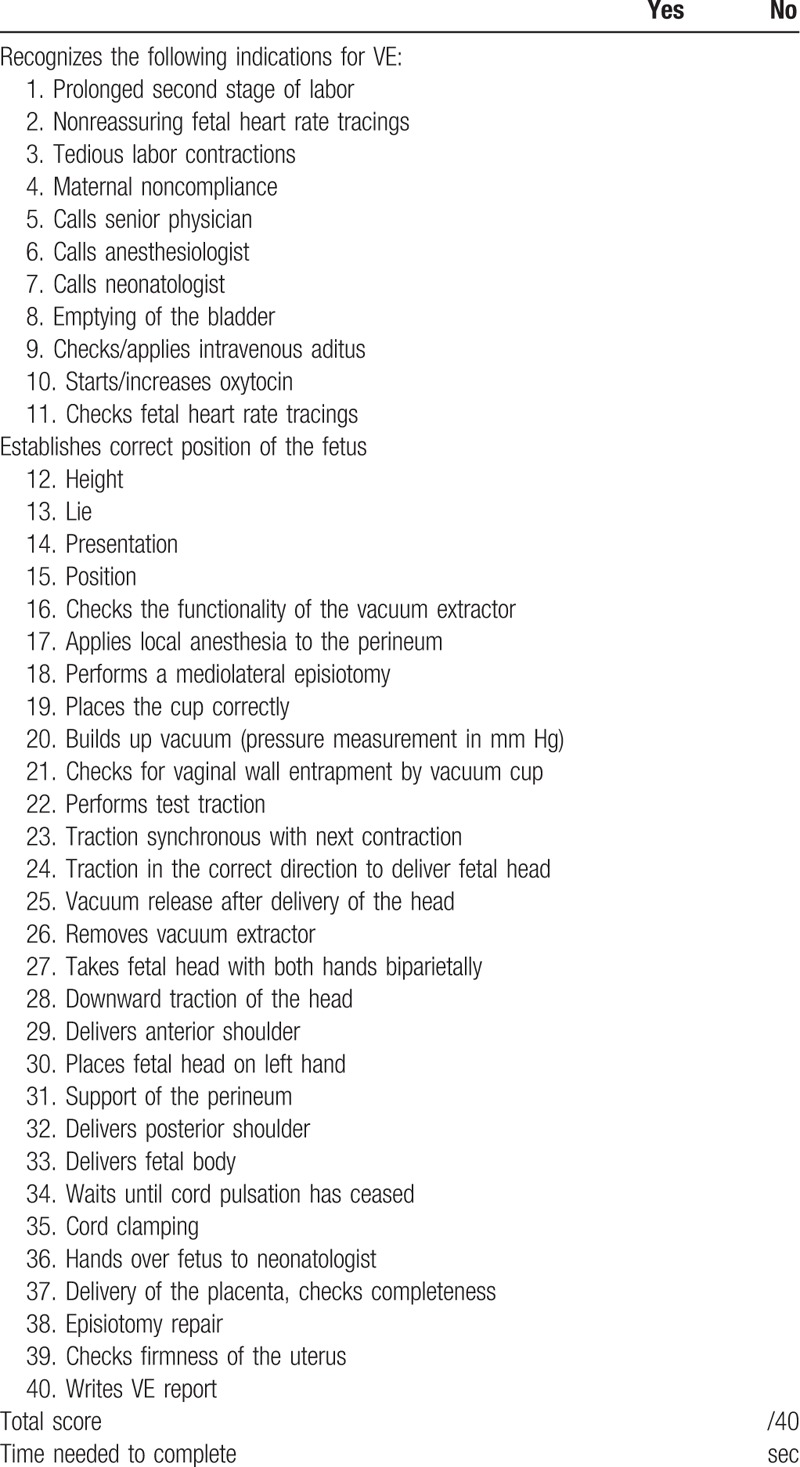
Students did not take photographs or cell phone videos during the study procedures and they were not allowed to take written notes. After the training session, study participants were tested by an assessor (A.K.). Testing was repeated 4 days later. The assessor was unaware of the group assignment of the study participants. Testing of the study participants was performed using the OSATS technique. Specifically, the assessor calculated an OSATS score by adding points given for each of the 40 items on a task-specific check list (Table 1), with 1 point for correctly performing each item and 0 point for not performing or not correctly performing the item. Thus, a higher score indicates greater proficiency. The secondary outcomes SA, CON, and global rating scale (GRS) were graded using a 5-scale Likert scale, with lower values denominating better performance.
We tested the construct validity of the OSATS setting used in this study by comparing predefined metric scores between 6 experts and the 137 medical students recruited for this study. The metric scores were: number of cup detachments, pressure applied by the vacuum extractor (measured in mm Hg using the pressure scale attached to the KIWI OmniCup vacuum extractor), PT, and OSATS scores. PT was defined as the time between the starting point (start of item 1 of the OSATS checklist) and the stop time (completion of item 40 of the OSATS checklist). The 6 experts were consultants and residents with at least 4 years of practical obstetrical experience. We defined construct validity as given, when all metric scores were different between the 2 groups favoring the experts.
We chose to randomize medical students, because they had no previous obstetrics training or practical obstetric experience. In contrast to residents with various degrees of expertise and personal experience, this fact makes students ideal study participants in the sense that they make training effects easily visible.
Categorical variables were analyzed by chi-square test, and continuous variables were compared using the Mann–Whitney U test, with a significance level of 0.05. We performed a multiple linear regression model to test whether the training effect, as measured by OSATS scores, was independent of potential confounders such as the students’ sex (male vs female) or handedness. In addition, we included regular sports activities as a potential confounder, based on the assumption that engagement in regular sports may select a population with expert manual and coordination skills. Values are given as medians or means. A power calculation demonstrated that, with a sample size of 137, the study has a power of >80% to detect an absolute 20% difference in OSATS scores at a significance level of 0.05 using a Mann–Whitney U test. An OSATS score difference of 20%, that is, a median score difference of 4, range 0 to 8, was estimated to be achievable by hands-on training and to be clinically relevant based on previous OSATS training trials.[12,13,17] We used the statistical software SPSS 11.0 for Windows (SPSS 11.0, SPSS Inc., Chicago, IL) for statistical analysis.
3. Results
We randomized 137 students. Table 2 shows the characteristics of the study population. Table 3 shows the primary and secondary outcomes broken down by group assignment. Specifically, we found that the OSATS scores (the primary outcome) were significantly higher in group 2 (n = 63) compared with group 1 (n = 74) (32.89 ± 6.39 vs 27.51 ± 10.27, respectively; P < 0.0001). Figure 2 shows a box plot of OSATS scores in both groups. The secondary outcomes GRS (1.49 ± 0.76 vs 2.33 ± 0.94, respectively; P < 0.0001), CON (2.22 ± 0.75 vs 3.26 ± 0.94, respectively; P = 0.04), SA (2.03 ± 0.62 vs 2.51 ± 0.77, respectively; P < 0.0001), and PT (38.81 ± 11.58 vs 47.23 ± 17.35 seconds, respectively; P = 0.001) were also significantly different favoring group 2.
Table 2.
Group-specific characteristics of study participants in groups 1 and 2.
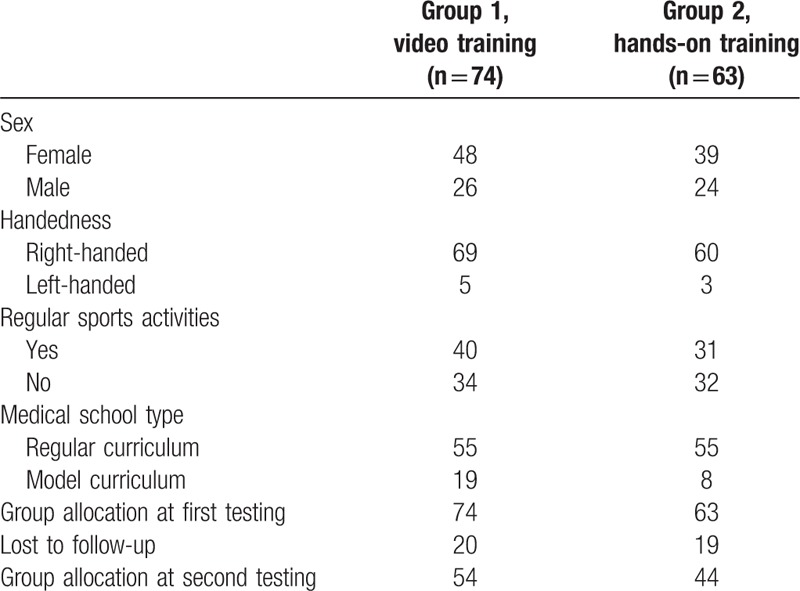
Table 3.
Primary and secondary outcome parameters after video training (group 1) and hands-on training (group 2).
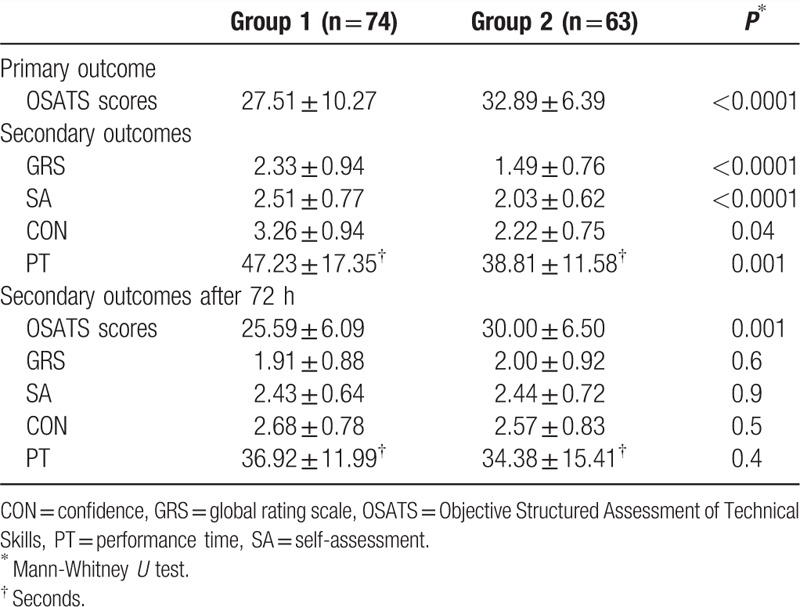
Figure 2.
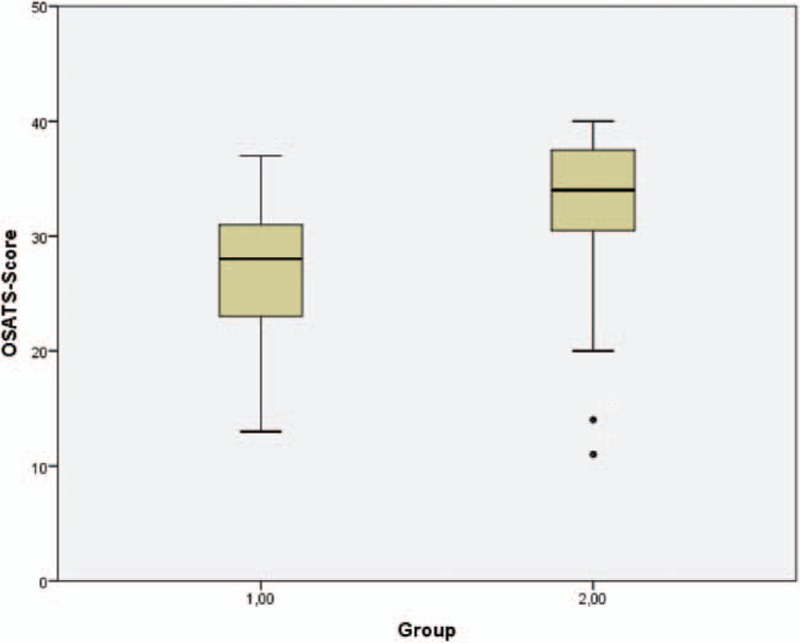
Box plots with Objective Structured Assessment of Technical Skills (OSATS) scores in group 1 (demonstration) and group 2 (hands-on training), with the boxes representing 50% of cases and the whiskers representing 1.5× the interquartile range. Circles represent outliers.
Group 2 had a significantly higher proportion of participants achieving 90%, 80%, and 70% of the maximum OSATS scores (3/74, 17/74, and 37/74 vs 27/63, 46/63, and 52/63; all comparisons P < 0.0001).
To test for a delayed training effect, we retested students after 4 days. Fifty-four students in group 1 and 44 students in group 2 took part in retesting. There was no significant difference in the lost to follow-up rate between groups 1 and 2 (20/74 vs 19/63; P = 0.4). After 4 days, OSATS scores were still significantly higher in group 2 (30.00 ± 6.50 vs 25.59 ± 6.09, respectively; P = 0.001). After 4 days, the secondary outcome parameters GRS, SA, CON, and PT were not significantly different between groups 2 and 1 (2.00 ± 0.92 vs 1.91 ± 0.88, respectively; P = 0.6 for GRS; 2.44 ± 0.72 vs 2.43 ± 0.64, respectively; P = 0.9 for SA; 2.57 ± 0.83 vs 2.68 ± 0.78, respectively; P = 0.5 for CON; 34.38 ± 15.41 vs 36.92 ± 11.99 seconds, respectively; P = 0.4 for PT).
Students differed regarding their sex (female; n = 87 vs male; n = 50), handedness (right-handed; n = 129 vs left-handed; n = 8), regular sports activities (defined as at least 3 times/wk; yes; n = 71 vs no; n = 66), and regarding the type of Medical School curriculum (regular curriculum; n = 110 vs an experimental “model” curriculum; n = 27). Assessing these potential confounders, we found that males and females achieved equally high OSATS scores (31.12 ± 12.04 vs 29.37 ± 6.87, respectively; P = 0.2). Right-handers and left-handers also performed equally (29.89 ± 9.23 vs 31.75 ± 4.30, respectively; P = 0.5), as did those who did or did not engage in regular sports activities (30.37 ± 10.61 vs 29.61 ± 7.15, respectively; P = 0.6). Lastly, students of the regular curriculum and students of the model curriculum also performed equally (30.26 ± 9.42 vs 28.96 ± 7.59, respectively; P = 0.5). In a multiple linear regression analysis, group assignment (odds ratio [OR] 7.72, 95% confidence interval [CI] 3.49–17.06, P < 0.0001) independently influenced OSATS scores, whereas sex, handedness, sports activities, and type of curriculum were not independently associated with OSATS scores. Therefore, group assignment was an independent predictor of OSATS scores.
The assessed OSATS scores showed constructive validity. Specifically, the metric scores were different between the experts (n = 6) and the nonexperts (n = 137), all favoring the expert group (number of cup detachments [0 vs 2, respectively], pressure applied by the vacuum extractor [0.78 ± 0.04 vs 0.76 ± 0.07 mm Hg, respectively], PT [33.83 ± 10.57 vs 43.68 ± 15.09 seconds, respectively], and OSATS scores [37.83 ± 0.75 vs 30.50 ± 10.79, respectively]).
4. Discussion
In the present study, we found that structured hands-on training on a pelvic dummy is more effective than a teaching video regarding OSATS scores for technical achievement, and also CON and procedural speed when performing a delivery by VE. In a multivariate linear regression model, group assignment was an independent predictor of OSATS scores. Based on these results, hands-on training helps to achieve a significant improvement of VE management skills compared with expert video demonstration, with the effect persisting for at least 5 days. Based on these results, we conclude that hands-on training is superior to expert video demonstration and should be recommended for teaching residents how to perform VE on a pelvic model.
Surgical simulators and pelvic training models have been described as useful tools for residents and advanced physicians for the training of surgical skills.[8–10,18,19] However, no data are available regarding the effectiveness of dummy trainings for VE delivery (PUBMED search; 03-february-2016; search terms: vaginal breech, training, model, randomized, pelvic trainer, vaginal breech management). The present study is the first controlled trial establishing the superiority of hands-on training over expert video demonstration in a frontal teaching setting. The results of our trial are in line with previous studies on shoulder dystocia or vaginal breech delivery trainings.[12,14] Specifically, hands-on training of shoulder dystocia management using a pelvic training model improved technical performance in a previously published randomized trial.[12] In this trial, students achieved significantly higher performance scores, had higher CON, and were quicker to complete the necessary steps after hands-on training compared with expert demonstration. The data of our actual trial show similar results demonstrating that hands-on training improves technical skills, in this case, performing a VE in a pelvic training model. Another randomized trial also demonstrated the superiority of hands-on training over expert demonstration regarding the management of a vaginal breech delivery.[14] Thus, our data and the data of others support the use of training models and simulators in clinical practice in general and for the training of obstetric interventions in particular. In addition, the present study also looked at additional participant characteristics such as handedness and sports activities, and included a number of metric scores to test for constructive validity.
In the expert demonstration group, we used a training video instead of a live expert demonstrator. This approach was chosen to standardize the frontal teaching experience and to avoid variations in the quality of the expert demonstration based on intraindividual variations in daily performance or interindividual variations due to changing experts. Moreover, the training video is in practical use at our Department and has consistently demonstrated its practical usefulness. On the contrary, we cannot rule out that live experts may have achieved better results.
Hands-on simulator training programs are time-consuming. Therefore, it is important to document their effectiveness in prospective randomized trials. Based on the results of our trial, we support the implementation of hands-on simulator training schemes into medical staff training programs.
Regular trainings for the management of obstetric complications such as breech presentation, shoulder dystocia, and vaginal operative delivery are recommended at least on a yearly basis for both novices and experts to acquire and maintain manual skills.[11,15,16,20] However, the exact means of training are unknown. Therefore, our study may help to design specific training plans by using the checklist described in our study and OSATS-scoring to judge the trainees’ performance. Our data indicate that technical proficiency in the management of VE can be objectively measured by OSATS. We found that OSATS had constructive validity differentiating between the performances of experts and novices.
Our study has limitations. First, we cannot report period. Therefore, we cannot exclude that the training effect may disappear over time. However, the beneficial effect of hands-on training was still visible after 4 days in our study, suggesting the presence of a delayed training effect after hands-on training. Based on the lack of longer follow-up data in our study, we cannot rule out that additional trainings may be necessary to achieve durable results in the long term.
Loss to follow-up was considerable in both groups between days 1 and 5 of the study. We have not used systematic measures of evaluation to find out the reasons for nonadherence. Therefore, we cannot comment on the reasons why study students decided not to participate in the testing on day 5. On the contrary, the number of students lost to follow-up did not differ significantly between the 2 study groups. Therefore, a bias of the day 5 study results due to group-specific self-selection of study participants is unlikely.
The internal validity of our study is high, because all participants were medical students without prior experience, thus forming a homogenous population. On the contrary, the performance of medical students may be representative of young residents, but may not necessarily translate to older Obstetrics and Gynecology residents and other staff.
In our study, we assessed training performance, which may not be consistent with the performance in a real clinical situation. Our study suggests, but does not prove, that better VE performance on a model will also result in better performance in women. This assumption is supported by literature demonstrating improved real-life performance of shoulder dystocia management, and also laparoscopic surgery after simulator training.[15,21] Lastly, not all OSATS items used in our study may be the standard of care of VE in other institutions.
In summary, the data collected in this prospective, randomized study provide level I evidence that hands-on training helps to achieve a significant improvement of VE performance over expert demonstration in a pelvic training model. These data support the incorporation of hands-on training and OSATS for teaching and training of VE into educational curriculums.
5. Conclusions
Hands-on training is superior to video demonstration for teaching VE on a pelvic model.
Acknowledgment
We acknowledge support by the DFG Open Access Publication Funds of the Ruhr-Universität Bochum.
Footnotes
Abbreviations: CON = confidence, GRS = global rating scale, OSATS = Objective Structured Assessment of Technical Skills, PT = performance time, SA = self-assessment, VE = vacuum extraction.
Author contributions: Z.H. made substantial contributions to the conception and design of the study, to the analysis and interpretation of data, and to writing the article, and gave final approval of the version to be published. A.K. contributed to the design of the study, collected and analyzed data, and revised and gave final approval of the data to be published. G.R. contributed to the design of the study, collected and analyzed data, and revised and gave final approval of the data to be published. C.C. contributed to the design of the study, collected and analyzed data, and revised and gave final approval of the data to be published. E.T.-B. analyzed and interpreted the data, drafted the article and revised it critically for important intellectual content, and gave final approval of the version to be published. C.T. made substantial contributions to the conception and design of the study, to the analysis and interpretation of the data, and approved the version to be published.
The authors declare no conflict of interest.
References
- [1].Popowski T, Porcher R, Fort J, et al. Influence of ultrasound determination of fetal head position on mode of delivery: a pragmatic randomized trial. Ultrasound Obstet Gynecol 2015;46:520–5. [DOI] [PubMed] [Google Scholar]
- [2].Williams MC, Knuppel RA, O’Brien WF, et al. A randomized comparison of assisted vaginal delivery by obstetric forceps and polyethylene vacuum cup. Obstet Gynecol 1991;78:789–94. [PubMed] [Google Scholar]
- [3].O’Mahony F, Hofmeyr GJ, Menon V. Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev 2010;CD005455. [DOI] [PubMed] [Google Scholar]
- [4].Ismail NA, Saharan WS, Zaleha MA, et al. Kiwi Omnicup versus Malmstrom metal cup in vacuum assisted delivery: a randomized comparative trial. J Obstet Gynaecol Res 2008;34:350–3. [DOI] [PubMed] [Google Scholar]
- [5].Kuit JA, Eppinga HG, Wallenburg HC, et al. A randomized comparison of vacuum extraction delivery with a rigid and a pliable cup. Obstet Gynecol 1993;82:280–4. [PubMed] [Google Scholar]
- [6].Groom KM, Jones BA, Miller N, et al. A prospective randomised controlled trial of the Kiwi Omnicup versus conventional ventouse cups for vacuum-assisted vaginal delivery. BJOG 2006;113:183–9. [DOI] [PubMed] [Google Scholar]
- [7].Roberts MJ, Gale TC, McGrath JS, et al. Rising to the challenge: acute stress appraisals and selection centre performance in applicants to postgraduate specialty training in anaesthesia. Adv Health Sci Educ Theory Pract 2016;21:323–39. [DOI] [PubMed] [Google Scholar]
- [8].Nagendran M, Gurusamy KS, Aggarwal R, et al. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2013;8:CD006575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Agha RA, Fowler AJ. The role and validity of surgical simulation. Int Surg 2015;100:350–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Goff BA, VanBlaricom A, Mandel L, et al. Comparison of objective, structured assessment of technical skills with a virtual reality hysteroscopy trainer and standard latex hysteroscopy model. J Reprod Med 2007;52:407–12. [PubMed] [Google Scholar]
- [11].ACOG Committee on Obstetric Practice. ACOG Committee Opinion No. 340. Mode of term singleton breech delivery. Obstet Gynecol 2006;108:235–7. [DOI] [PubMed] [Google Scholar]
- [12].Buerkle B, Pueth J, Hefler LA, et al. Objective structured assessment of technical skills evaluation of theoretical compared with hands-on training of shoulder dystocia management: a randomized controlled trial. Obstet Gynecol 2012;120:809–14. [DOI] [PubMed] [Google Scholar]
- [13].Alici F, Buerkle B, Tempfer CB. Objective Structured Assessment of Technical Skills (OSATS) evaluation of hysteroscopy training: a prospective study. Eur J Obstet Gynecol Reprod Biol 2014;178:1–5. [DOI] [PubMed] [Google Scholar]
- [14].Buerkle B, Rueter K, Hefler LA, et al. Objective Structured Assessment of Technical Skills (OSATS) evaluation of theoretical versus hands-on training of vaginal breech delivery management: a randomized trial. Eur J Obstet Gynecol Reprod Biol 2013;171:252–6. [DOI] [PubMed] [Google Scholar]
- [15].Draycott TJ, Crofts JF, Ash JP, et al. Improving neonatal outcome through practical shoulder dystocia training. Obstet Gynecol 2008;112:14–20. [DOI] [PubMed] [Google Scholar]
- [16].Lavin JP, Jr, Eaton J, Hopkins M. Teaching vaginal breech delivery and external cephalic version. A survey of faculty attitudes. J Reprod Med 2000;45:808–12. [PubMed] [Google Scholar]
- [17].Hefler L, Grimm C, Kueronya V, et al. A novel training model for the loop electrosurgical excision procedure. Am J Obstet Gynecol 2012;206:e1–4. [DOI] [PubMed] [Google Scholar]
- [18].Egi H, Tokunaga M, Hattori M, et al. Evaluating the correlation between the HUESAD and OSATS scores: concurrent validity study. Minim Invas Ther Allied Technol 2013;22:144–9. [DOI] [PubMed] [Google Scholar]
- [19].Steehler MK, Chu EE, Na H, et al. Teaching and assessing endoscopic sinus surgery skills on a validated low-cost task trainer. Laryngoscope 2013;123:841–4. [DOI] [PubMed] [Google Scholar]
- [20].Dhingra S, Raffi F. Obstetric trainees’ experience in VBD and ECV in the UK. J Obstet Gynaecol 2010;30:10–2. [DOI] [PubMed] [Google Scholar]
- [21].Larsen CR, Soerensen JL, Grantcharov TP, et al. Effect of virtual reality training on laparoscopic surgery: randomised controlled trial. BMJ 2009;338:b1802. [DOI] [PMC free article] [PubMed] [Google Scholar]


