Abstract
Background and Objective:
Hysterectomy is one of the most common surgical procedures women will undergo in their lifetime. Several factors affect surgical outcomes. It has been suggested that high-volume surgeons favorably affect outcomes and hospital cost. The objective is to determine the impact of individual surgeon volume on total hospital costs for hysterectomy.
Methods:
This is a retrospective cohort of women undergoing hysterectomy for benign indications from 2011 to 2013 at 10 hospitals within the University of Pittsburgh Medical Center System. Cases that included concomitant procedures were excluded. Costs by surgeon volume were analyzed by tertile group and with linear regression.
Results:
We studied 5,961 hysterectomies performed by 257 surgeons: 41.5% laparoscopic, 27.9% abdominal, 18.3% vaginal, and 12.3% robotic. Surgeons performed 1–542 cases (median = 4, IQR = 1–24). Surgeons were separated into equal tertiles by case volume: low (1–2 cases; median total cost, $4,349.02; 95% confidence interval [CI] [$3,903.54–$4,845.34]), medium (3–15 cases; median total cost, $2,807.90; 95% CI [$2,693.71–$2,926.93]) and high (>15 cases, median total cost $2,935.12, 95% CI [$2,916.31–$2,981.91]). ANOVA analysis showed a significant decrease (P < .001) in cost from low-to-medium– and low-to-high–volume surgeons. Linear regression showed a significant linear relationship (P < .001), with a $1.15 cost reduction per case with each additional hysterectomy. Thus, if a surgeon performed 100 cases, costs were $115 less per case (100 × $1.15), for a total savings of $11,500.00 (100 × $115).
Conclusion:
Overall, in our models, costs decreased as surgeon volume increased. Low-volume surgeons had significantly higher costs than both medium- and high-volume surgeons.
Keywords: Cost analysis, Gynecology, Hysterectomy, Minimally invasive surgery
INTRODUCTION
Hysterectomy is one of the most common surgical procedures in women, with >600,000 performed in 2003.1 Several factors can impact perioperative outcomes. Recent studies have focused on the impact of high-volume surgeons on patient outcomes. In the literature, high-volume surgeons are defined in many ways, the most common being separation into tertiles or choosing an arbitrary cutoff in number of cases performed. Typically, the cutoff is 10–30 hysterectomies annually.2–5 Numerous retrospective cohort studies of large national and state databases found that high-volume gynecologic surgeons improve multiple patient outcomes including decreased blood loss, operative time, intraoperative and postoperative complications, ICU admissions, transfusions, hospital readmissions, and length of hospital admissions.2–4,6–8 These benefits have led healthcare systems to start funneling cases to high-volume surgeons in an attempt to reproduce these benefits within their own systems.
In addition, there is emerging evidence that high-volume surgeons have significantly lower per-case costs when compared with those of low-volume surgeons. Two studies separated surgeons into tertiles to compare costs. High-volume surgeons performing 55 vaginal hysterectomies, and 14 laparoscopic hysterectomies per year found a cost savings of $443 and $867, respectively.2,3 The cost estimations were based on median costs per surgeon, which were not always accrued hospital costs, but more often hospital charges, charge cost ratios, or insurance reimbursement amounts. Also, there was no attempt to create a model to determine per case cost savings for any surgeon based on volume. In this study our primary intent was to determine the impact of individual surgeon volume on total hospital costs when hysterectomy is performed for benign conditions and to determine where these cost differences occur when total costs are divided into subcategories.
MATERIALS AND METHODS
After Institutional Review Board approval, costs were collected from all hysterectomies performed at the University of Pittsburgh Medical Center, including 10 hospitals during the fiscal years, 2011 through 2013. Hysterectomies were excluded if the indication for surgery was malignancy or if concomitant procedures other than salpingo-oophorectomy were performed, to avoid artificially inflating costs. The University of Pittsburgh Medical Center's internal accounting department provided a deidentified database of costs per procedure, reported as total and subcategory costs. Costs were actual hospital costs accrued during the patients' hospital admission and were not calculated from hospital charges or insurance reimbursement. Initially, there were 17 subcategories for cost. We excluded subcategories with a median cost of $0. Nine subcategories were available for analysis: anesthesia, laboratory, medical/surgical floor, respiratory therapy, postanesthesia care unit, operating room equipment, blood bank, operating room time, and pharmacy.
We created tertiles to assess surgeon volume and cost by dividing the surgeons into 3 equal groups based on the number of hysterectomies performed during the 3-year period to compare our data to previous publications. Hysterectomy costs were not normally distributed in this dataset. To compare groups by using parametric statistics with ANOVA, we performed a natural log transformation. This approach is common with cost data, as there is a minimum, but no maximum, cost. The use of transformations permits the increased power of the parametric tests, as compared to nonparametric statistics.
In addition, our goal was to determine the relationship between costs as surgeon volume increased using linear regression. Linear curve were generated by applying the “best fit” for the equation Y = (A * X) + B where Y is cost and B is the y-intercept which, is the baseline costs when surgeon volume is 0. The slope of the line is A, which equals the additional costs per case. Negative values for A signify that costs per case are lower with each additional hysterectomy performed. X represents each additional hysterectomy performed.
RESULTS
During fiscal years 2011 through 2013, 257 surgeons performed 5,961 hysterectomies: 41.5% laparoscopic, 27.9% abdominal, 18.3% vaginal, and 12.3% robotic. Surgeons performed 1–542 cases during the 3-year interval (median = 4; IQR = 1–24). Median total hysterectomy costs were $2,838.18 (IQR $2,178.74–$3,963.10). Costs were lowest with the vaginal route (median = $1,984.98; IQR $1,603.42–$2,639.04) and highest with robotics (median = $4,331.43; IQR $3,624.84–$5,216.67; P < .001). Other hysterectomy routes in the database included laparoscopic (median = $2,606.26; IQR $2,197.23–$3,313.82) and open laparotomy ($3,349.07; IQR $2,544.27–$4,685.99). There was a significant difference in cost comparing all 4 routes by using ANOVA, followed by post hoc comparisons with Dunnett T3 (all P < .001).
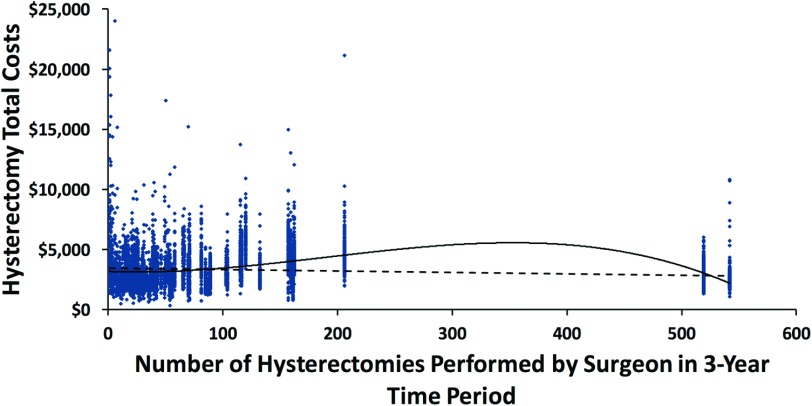
When surgeons were divided into equal tertiles, the lowest tertile performed 1–2 hysterectomies and the highest tertile performed >15 (Table 1). ANOVA post hoc analysis, with Dunnett T3 because of inhomogeneous variance, showed that costs were significantly higher in the lowest tertile compared to the middle and highest tertiles (P < .001). We did not see a difference in cost between the middle and highest tertiles (P = .125). The 95% confidence interval (CI) for mean costs was also widest in the lowest tertile and most narrow in the highest tertile by volume. This finding indicates that lower volume surgeons also have a higher variability in their total costs, which is visibly evident in Figure 1.
Table 1.
Mean Hysterectomy Costs By Tertile
| Tertile | Hysterectomies per Surgeon | Mean Costs | 95% CI |
|---|---|---|---|
| 1* | 1–2 | $4,349.02 | $3,903.54–$4,845.34 |
| 2*,† | 3–15 | $2,807.90 | $2,693.71–$2,926.93 |
| 3*,† | > 15 | $2,935.12 | $2,916.31–$2,981.91 |
Tertiles were composed of an equal number of surgeons. Mean costs are reported with 95% CI. Costs for low-volume surgeons (the first tertile) were significantly higher than those for the medium- and high-volume surgeons (P < .001). The second tertile or medium-volume surgeons' cost was not significantly different than that of the high-volume surgeons (P = .125).
Post hoc testing with ANOVA showed P < .001 for tertile 1 vs 2 and 1 vs 3.
Post hoc testing with ANOVA showed P = .125 for tertile 2 vs 3.
Figure 1.
hysterectomy total costs by individual surgeon volume. Each dot represents a single case. The dashed line represents the best-fit linear regression line from the following equation: cost = –1.15(cases performed) + 3,440.47. A significant relationship was found, as surgeon volume increased cost per hysterectomy decreased (P <.001).
We performed a linear regression to determine whether there was a linear relationship between surgeon volume and total costs where we found a significant negative linear relationship (P < .001). As the number of cases increased, the cost per hysterectomy decreased, as represented by the following equation:
The equation shows a $1.15 savings per case, with increased savings as the total number of cases a surgeon performs increases. For example, if a surgeon performs 100 cases in 3 years, each case will cost $115 less than the baseline costs of $3,440.47. There is a total savings of $115 × 100 = $11,500 resulting in a 3.34% cost reduction. Thus, the more cases a surgeon performs, the more savings per case they will generate.
After dividing costs into subcategories, linear regression was performed on 9 categories. Congruent with the analysis of total costs, costs decreased as surgeon volume increased for the following categories: anesthesia, laboratory, medical/surgical floor, and respiratory therapy costs. Conversely, costs increased as surgeon volume increased for postanesthesia care unit and operating room equipment. There was no significant linear relationship for blood bank, operating room time, or pharmacy costs (Table 2).
Table 2.
Cubic Equations by Route of Hysterectomy
| Route | Cubic Cost Equation | Cost by Surgeon Volume | R2 | P |
|---|---|---|---|---|
| All routes combined | Cost = −0.00014 * X3 + 0.079 * X2 − 3.849 * X + 3176.273 | Cost ↑ 0–27, ↓ 27–350, ↑ >350 cases | .089 | <.001 |
| All routes combined, high-volume surgeons excluded* | Cost = −0.001 * X3 + 0.414 * X2 − 33.270 * X + 3702.453 | Cost ↓ 0–49, ↑ 49–227, ↓ >227 cases | .081 | <.001 |
| Laparoscopic cases only, high-volume surgeons excluded* | Cost = −0.009 * X3 + 1.302 * X2 − 44.393 * X + 3433.759 | Cost ↓ 0–22, ↑ 22–74, ↓ >74 cases | .029 | <.001 |
| All routes combined, low-volume surgeons excluded† | Cost = 0.0000792 * X3 + 0.032 * X2 + 4.706 * X + 2802.493 | Cost ↑ 0–60, ↓ >60 cases | .115 | <.001 |
Curve estimation was performed for all hysterectomies combined and by route. X represents the number of cases performed for an individual surgeon. The vaginal hysterectomy route did not have a significant curvilinear relationship between costs and surgeon volume. The laparoscopic, abdominal, and robotic cases each had 2 inflection points that varied as case volume increased. Independently, the laparoscopic cases had the highest R2 value.
There were 2 extremely high-volume surgeons present as outliers in the data. We excluded them and repeated the analyses for all routes combined and then for laparoscopic alone. Results were drastically different when we removed the extremely high-volume surgeons from the laparoscopic analysis. Hysterectomy costs decreased when surgeons performed >74 cases over 3 years, whereas before removing these surgeons, >111 cases were needed to decrease costs, indicating their direct impact on the curve. †Last, we excluded extremely low-volume surgeons and repeated the analysis for all routes combined and likewise found a significant impact on cost. Surgeons who performed >60 hysterectomies in 3 years had decreased costs. That model had the highest R2 value of all the models created, indicating less variability in cost within the data.
There were some outliers in our dataset: 2 surgeons who performed 519 and 542 cases, respectively. No other surgeons performed over 206 cases. These surgeons' mean costs were $2,571.97 (95% CI $2,522.73–$2,621.22). We also had 120 surgeons (46.7% of all surgeons) who performed ≤3 hysterectomies in 3 years, or ≤1 per year. These surgeons' mean costs were $4,698.56 (95% CI $4,164.76–$5,232.37).
DISCUSSION
In summary, we came to 2 major conclusions from our analysis. First, when we analyzed volume by tertile, low-volume surgeons had significantly higher costs, which is consistent with previous studies.2,3 Second, we found a significant linear relationship between surgeon volume and hysterectomy costs. The cost savings on linear regression was $1.15 per case performed. Although this modest savings is much lower than previously reported in the literature, it becomes multiplicatively more significant when total case number per surgeon increases, yielding greater total cost savings.3
In the literature, cost analysis for hysterectomies has traditionally been performed on data from large national databases where the costs are reported from the hospital as a combination of charges or insurance reimbursements, but rarely from actual costs. In addition these “costs” are from multiple hospitals throughout the country and can vary according to region, hospital size, and health care system. In this study, we had the ability to use data from a diverse group of gynecologic surgeons all under the umbrella of a single health care system. Obtaining accrued hospital costs directly from accounting provided us with a unique opportunity to perform a cost analysis on individual surgeons and the cost for each case they performed. The large number of data points allowed us to make a more accurate cost model by using linear regression than previously reported models that used mean or median costs per surgeon by tertile.
We found relatively higher variability in costs with low-volume surgeons, but overall, there was high cost variability in the entire dataset (for the linear regression, R2 = 0.016). R2 values determine how much the variability in the data can be explained by the model's equation. If every data point falls exactly on the line predicted by the model, R2 = 1.0. However, the cost per hysterectomy in our data was extremely variable, keeping R2 values low. We hypothesized that the high variability in costs was due to factors other than surgeon volume which were not included in our analysis such as surgical complexity, uterine weight, previous surgical procedures, resident and fellow education, and referral patterns. These factors, had they been included in the statistical model, would likely increase the R2 value. Unfortunately, our database lacked this information, and so it could not be included.
In this study, surgeons had a wide case volume distribution with 46.7% performing ≤3 hysterectomies in 3 years. When we divided surgeons into tertiles the high-volume surgeons had performed >15 hysterectomies in 3 years, or 5 per year. This number is somewhat lower than the typical range used in the literature, of 8–30 hysterectomies annually.2–5 However, it is reflective of our large university based health care system.
There are multiple studies demonstrating improved patient outcomes including decreased hospital admission length and operative complications when high-volume surgeons perform hysterectomies.2–4,6–8 Hospital credentialing boards may soon use patient outcome and cost analysis data, including findings like ours, to determine minimum annual case numbers to maintain hysterectomy privileges.9 Low-volume surgeons may need to refer their hysterectomy cases to more high-volume surgeons. Our hospital system has already started this practice pattern, as is evident by the 2 extremely high-volume surgeons in our dataset.
Strengths of this study include the data collected and the type of cost analysis performed. Our dataset contains individual accrued hospital costs stratified by each surgeon's volume for over 200 surgeons in a single health care system. This type of information is rarely available. We then were able to use the data to perform multiple cost analyses using analysis by tertiles and linear regression. Linear regression was challenging because of the variability in cost but using individual data points versus median costs provides us with a more detailed cost model. Our findings likely correspond to the variability in costs seen at other large health care systems. Last, as more people become insured and have access to medical care through the Affordable Health Care Act, hospitals and health care systems must responsibly allocate resources. Eliminating extremely low-volume surgeons and referring hysterectomies to high-volume surgeons may be a necessary step.
A major limitation of our study was the inability to account for surgical complexity that can significantly drive costs. However, high-volume surgeons, often subspecialists, are likely referred more difficult cases, and we found they had lower costs. Similarly, we did not look at surgical or fellowship training as a confounding factor. Finally, we only looked at surgeons' case volume as it related to hysterectomy. We did not account for volume of other major gynecologic surgical procedures such as excision of endometriosis or removal of pelvic masses, which likely also contribute to a surgeon's ability and ultimately affect their hysterectomy costs.
CONCLUSIONS
Ultimately, we were able to demonstrate that surgeon volume impacts costs. Low-volume surgeons have significantly higher costs. Costs decreased in a linear fashion as volume increased with a per-case savings for each additional hysterectomy performed. There was still high variability in costs from factors not accounted for in the models, implying that the relationship between costs and surgical volume is highly complex making it difficult to predict costs. Nevertheless, our analysis showed decreased costs as volume increased. Our data support that surgeon volume clearly drives costs.
Contributor Information
Jonathan P. Shepherd, Department of Obstetrics and Gynecology, St Francis Hospital and Medical Center, Hartford, Connecticut, USA..
Charelle M. Carter-Brooks, Department of Obstetrics, Gynecology and Reproductive Sciences of the University of Pittsburgh, Magee Women's Hospital, Pittsburgh, Pennsylvania, USA..
Kelly L. Kantartzis, Department of Obstetrics, Gynecology and Reproductive Sciences of the University of Pittsburgh, Magee Women's Hospital, Pittsburgh, Pennsylvania, USA..
Ted Lee, Department of Obstetrics, Gynecology and Reproductive Sciences of the University of Pittsburgh, Magee Women's Hospital, Pittsburgh, Pennsylvania, USA..
Michael J. Bonidie, Department of Obstetrics, Gynecology and Reproductive Sciences of the University of Pittsburgh, Magee Women's Hospital, Pittsburgh, Pennsylvania, USA..
References:
- 1. Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110:1091–1095. [DOI] [PubMed] [Google Scholar]
- 2. Wallenstein MR, Ananth CV, Kim JH, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119:709–716. [DOI] [PubMed] [Google Scholar]
- 3. Rogo-Gupta LJ, Lewin SN, Kim JH, et al. The effect of surgeon volume on outcomes and resource use for vaginal hysterectomy. Obstet Gynecol. 116:1341–1347. [DOI] [PubMed] [Google Scholar]
- 4. Tunitsky E, Citil A, Ayaz R, Esin S, Knee A, Harmanli O. Does surgical volume influence short-term outcomes of laparoscopic hysterectomy? Am J Obstet Gynecol. 2010;203:24.e1–e6. [DOI] [PubMed] [Google Scholar]
- 5. Bristow RE, Zahurak ML, Diaz-Montes TP, Giuntoli RL, Armstrong DK. Impact of surgeon and hospital ovarian cancer surgical case volume on in-hospital mortality and related short-term outcomes. Gynecol Oncol. 2009;115:334–338. [DOI] [PubMed] [Google Scholar]
- 6. Vree FE, Cohen SL, Chavan N, Einarsson JI. The impact of surgeon volume on perioperative outcomes in hysterectomy. JSLS, 2014;18:174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wright JD, Lewin SN, Deutsch I, Burke WM, Sun X, Herzog TJ. Effect of surgical volume on morbidity and mortality of abdominal hysterectomy for endometrial cancer. Obstet Gynecol. 2011;117:1051–1059. [DOI] [PubMed] [Google Scholar]
- 8. Wright JD, Hershman DL, Burke WM, et al. Influence of surgical volume on outcome for laparoscopic hysterectomy for endometrial cancer. Ann Surg Oncol. 2012;19:948–958. [DOI] [PubMed] [Google Scholar]
- 9. Doll KM, Milad MP, Gossett DR. Surgeon volume and outcomes in benign hysterectomy. J Minim Invasive Gynecol. 2013;20:554–561. [DOI] [PubMed] [Google Scholar]