Abstract
Purpose
The aim of this study was to investigate the incidence of bisphosphonate-related osteonecrosis of the jaw (BRONJ) after tooth extraction in patients with osteoporosis on oral bisphosphonates in Korea and to evaluate local factors affecting the development of BRONJ.
Materials and Methods
The clinical records of 320 patients who underwent dental extraction while receiving oral bisphosphonates were reviewed. All patients had a healing period of more than 6 months following the extractions. Each patient's clinical record was used to assess the incidence of BRONJ; if BRONJ occurred, a further radiographic investigation was carried out to obtain a more definitive diagnosis. Various local factors including age, gender, extraction site, drug type, duration of administration, and C-terminal telopeptide (CTx) level were retrieved from the patients' clinical records for evaluating their effect on the incidence of BRONJ.
Results
Among the 320 osteoporotic patients who underwent tooth extraction, 11 developed BRONJ, reflecting an incidence rate of 3.44%. Out of the local factors that may affect the incidence of BRONJ, gender, drug type, and CTx level showed no statistically significant effects, while statistically significant associations were found for age, extraction site, and duration of administration. The incidence of BRONJ increased with age, was greater in the mandible than the maxilla, and was associated with a duration of administration of more than 3 years.
Conclusion
Tooth extraction in patients on oral bisphosphonates requires careful consideration of their age, the extraction site, and the duration of administration, and close postoperative follow-up should be carried out to facilitate effective early management.
Keywords: Bisphosphonate-Associated Osteonecrosis of the Jaw, Osteoporosis, Tooth Extraction, Risk Factors
Introduction
Osteoporosis is a systemic skeletal condition that causes reduction of the bone mass. The incidence of osteoporosis increases with age, and its greatest risk is bone fracture, which results in a decreased quality of life.1,2 Bisphosphonates are widely used treatment agents for osteoporosis due to their suppression of osteoclast activity, which slows down the bone remodeling process and increases the bone mineral density.1,3,4,5,6,7,8,9,10
Bisphosphonates are known to suppress bone resorption that occurs during the normal healing process, thereby delaying bone healing. Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is the main side effect of bisphosphonate; it was first reported in 2003 by Marx11 and can be defined as follows:12,13 1) exposed bone in the maxillofacial region that is present for 8 weeks or more, 2) current or previous bisphosphonate use, and 3) no history of radiation therapy to the jaws. The exact etiopathology of BRONJ is not well known, but several factors that affect its development have been reported. Dental surgery is one of these factors, and tooth extraction is known to be a high-risk procedure because of the production of a bony socket.
In the Korean population that takes bisphosphonates for osteoporosis, the incidence of BRONJ after tooth extraction has been rarely reported. Therefore, whether tooth extraction is a causative factor of BRONJ in patients with osteoporosis is uncertain. In this study, we aimed to investigate the incidence of BRONJ after tooth extraction in patients with osteoporosis exposed to oral bisphosphonates and to evaluate the local factors that affect the development of BRONJ.
Materials and Methods
In all, 320 patients were selected as the subjects for this study; these patients were on oral bisphosphonates treatment for osteoporosis and underwent tooth extraction at Yonsei University Dental Hospital. This study was approved by the Institutional Review Board (IRB) of Yonsei University Dental Hospital (Approval number: 13-0114 (2-2013-0062)). Written or verbal informed consent was not obtained from any participants because the IRB waived the need for individual informed consent, as this study had a non-interventional retrospective design and all data were analyzed anonymously. The reasons for tooth extraction included periodontitis, residual root, advanced dental caries, and tooth fracture. In all, 651 teeth were selected, which included 94 maxillary anterior teeth, 84 maxillary premolars, 187 maxillary molars, 74 mandibular anterior teeth, 67 mandibular premolars and 145 mandibular molars.
Tooth extractions were performed using routine protocols as follows: All patients received prophylactic antibiotics 1 hour prior to the extractions, which were carried out under local anesthesia. The extraction sockets were sutured. Antibiotic, anti-inflammatory, and analgesic drugs were prescribed for 3 days. The minimum follow-up period following the extraction was 6 months. A definitive diagnosis of BRONJ was made using the patients' clinical records, including the presence of clinical symptoms and radiographic findings. At the time of extraction, various local factors, data regarding which were gathered from the clinical records, were recorded as follows: 1) gender: male or female; 2) age: below 65 years or over 65 years; 3) extraction site: maxilla or mandible (anterior, premolar, or molar); 4) drug type: alendronate, ibandronate, or risedronate; 5) duration of administration: less than 3 years or more than 3 years; and 6) C-terminal telopeptide (CTx) level (pg/mL): below 150 or over 150.
A statistical analysis was carried out to determine the difference in the rate of incidence according to each factor by using the chi-square test in SPSS version 20.0 (IBM Corp., Armonk, NY, USA).
Results
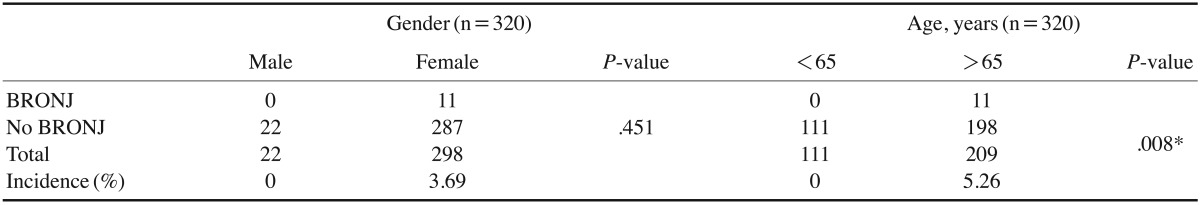
Incidence according to gender and age
In all, 11 of the 320 patients with osteoporosis developed BRONJ, with an incidence rate of 3.44%. The incidence of BRONJ according to gender and age is as presented in Table 1. The number of male patients with osteoporosis was only 22, which was considerably less than that of female patients; therefore, comparisons according to gender may not be absolutely reliable. However, no statistically significant difference was observed according to gender with respect to the incidence rate. No male patients with osteoporosis developed BRONJ, and all patients who developed BRONJ were female. A statistically significant difference was found in the rate of incidence with respect to the age group, as all 11 patients who developed BRONJ were over 65 years old.
Table 1. Prevalence of bisphosphonate-related osteonecrosis of the jaw according to the gender and age.
*Statistically significant difference at P<.05, BRONJ: bisphosphonate-related osteonecrosis of the jaw
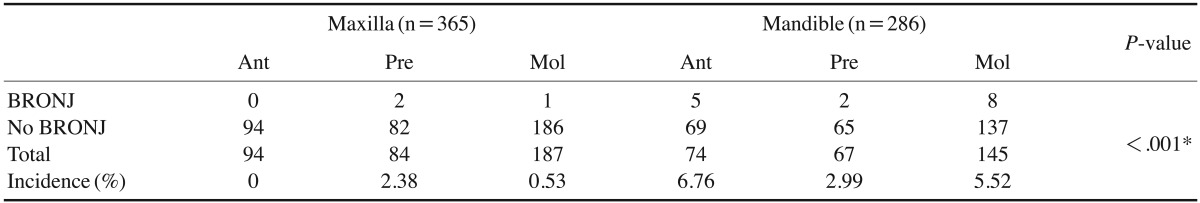
Incidence according to extraction site
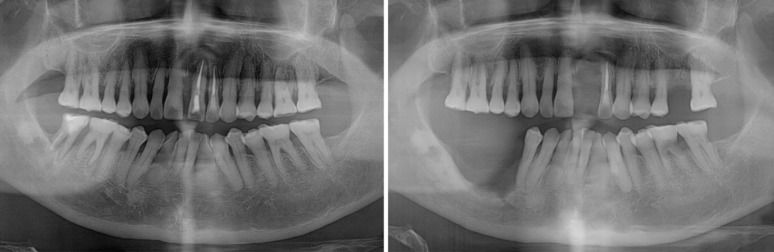
The incidence of BRONJ according to the extraction site is presented in Table 2. In all, 651 teeth were extracted. Three of the 365 maxillary teeth (0.82%) and 15 of the 286 mandibular teeth (5.24%) developed BRONJ. Therefore, mandibular teeth showed a greater rate of incidence of BRONJ than the maxillary teeth; this difference was statistically significant. Representative cases of BRONJ are shown in Figures 1, 2, 3.
Table 2. Prevalence of bisphosphonate-related osteonecrosis of the jaw according to the extraction sites.
*Statistically significant difference at P<.05, BRONJ: bisphosphonate-related osteonecrosis of the jaw, Ant: anterior teeth, Pre: premolars, Mol: molars
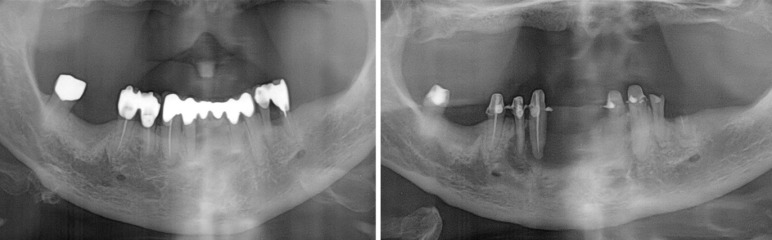
Fig. 1. Panoramic radiographs of a bisphosphonate-related osteonecrosis of the jaw (BRONJ) patient. Three months prior to the extraction of the right mandibular incisor (left) and 1 year after the extraction (right).
Fig. 2. Panoramic radiographic view of a bisphosphonate-related osteonecrosis of the jaw (BRONJ) patient prior to the extraction of the root remnant of the right mandibular first molar (upper left) and panoramic view (upper right); computed tomographic scan (lower) taken 1 year after the extraction.
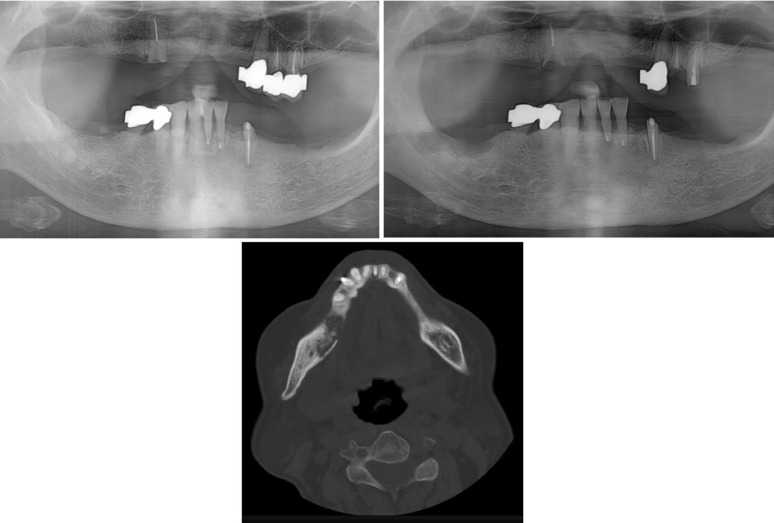
Fig. 3. Panoramic radiographic images of a bisphosphonate-related osteonecrosis of the jaw (BRONJ) patient prior to the extraction of the right mandibular first and second molars (left), and 6 months after the extraction (right).
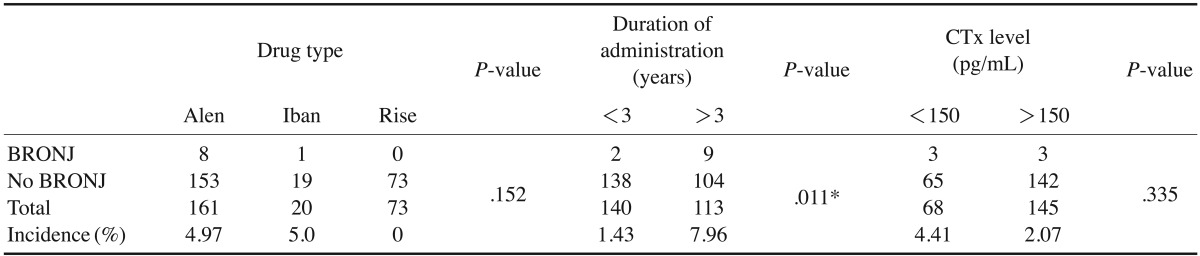
Incidence according to drug type, duration of administration, and CTx level
The incidence rate of BRONJ according to the drug type, duration of administration, and CTx level is presented in Table 3. Patients on ibandronate showed the highest incidence rate (5.0%); however, no statistically significant difference was found according to the drug type. With respect to the duration of administration, the incidence rate was higher (7.96%) in patients who were administered the drugs for more than 3 years, which was significantly higher than was observed in those with a drug administration period of less than 3 years. The incidence rate was slightly higher in patients with a CTx level of less than 150 pg/mL, but this finding was not statistically significant.
Table 3. Prevalence of bisphosphonate-related osteonecrosis of the jaw according to drug type, duration of administration, and CTx level.
*Statistically significant difference at P<.05, BRONJ: bisphosphonate-related osteonecrosis of the jaw, CTx: C-terminal telopeptide, Alen: alendronate, Iban: iIbandronate, Rise: risedronate
Discussion
The key pharmacological mechanism of bisphosphonates as a treatment agent for osteoporosis is known to be the suppression of osteoclast activity and the subsequent prevention of bone resorption. Consequently, the bone turnover rate is reduced in patients who take bisphosphonates, which slows down wound healing in extraction sockets and increases susceptibility to complications.1 In a previous study, the overall disease rate of BRONJ in patients on bisphosphonates was estimated to be around 0.03%-0.1%,14 and the rate of incidence was reported to increase following surgical procedures such as tooth extraction.1,15,16,17 Osteoporosis is a disease of the elderly, for whom tooth extraction is one of the most common treatment modalities. However, insufficient statistical data have been reported on the rate of incidence of BRONJ after extraction in this age group. In this study, the incidence rate of BRONJ following tooth extraction was investigated in patients on oral bisphosphonates, and local factors potentially affecting the incidence rate were evaluated.
In the current study, the incidence rate of BRONJ in patients on oral bisphosphonates who underwent tooth extraction was 3.44%, which is higher than that reported in previous studies. This was because the previous research presumably involved a wider pool of patients than the current study, which was limited to patients who underwent tooth extraction. In the study of Taylor et al.18 in which methods similar to those used in the current study were utilized, 5 (2.5%) out of 202 patients developed BRONJ, showing comparable results. A retrospective study by Sedghizadeh et al.19 of 66 patients who were taking alendronate and had undergone extraction reported a higher incidence (6%) of BRONJ development than was found in our study. Hansen et al.20 reported that among the osteoporosis patients on oral bisphosphonate, the incidence rate of BRONJ following dental treatment was 2.27%, which is higher than the general consensus.
Although the male subjects of this study were considerably fewer in number than the female subjects, there was no statistically significant difference with respect to the incidence of BRONJ. Taylor et al.18 demonstrated that male patients were significantly more likely to develop BRONJ after tooth extraction than females, but this difference in outcome might have been caused by the intravenous administration of bisphosphonates in 6 of the 7 BRONJ patients suffering from malignant tumors.
The incidence rate of BRONJ showed a statistically significant difference between groups above and below the age of 65 years. The groups were divided at 65 years, as was done in a previous study by Taylor et al.,18 in which there was no statistically significant difference according to age; however, the inclusion of patients with malignancies makes a direct comparison with the current study inappropriate. As all 11 patients with BRONJ in this study were over the age of 65 years, age can be considered a significant factor affecting the incidence of BRONJ.
The location of the extracted tooth was shown to be a significant determinant of the occurrence of BRONJ, as BRONJ occurred more frequently in the mandible than the maxilla. However, no variation within the dental arch was detected. Similarly, in previous research, Pazianas et al.1 reported that in 16 out of 22 patients, BRONJ occurred in the maxilla; in the rest of the cases, it occurred in the mandible. Further, O'Ryan and Lo14 reported that BRONJ occurrence in the mandible was twice as common as in the maxilla.
With respect to the drug type, ibandronate showed the highest incidence rate of BRONJ, although its small sample size may have caused discrepancies in the result. This result is in concurrence with a previous report that suggested that there was no statistically significant difference in the incidence rate of BRONJ among different drug types.1 However, further research is needed for a more accurate statistical analysis in a larger sample size.
In the current study, the incidence rate of BRONJ was compared and evaluated after 3 years of drug administration, a period determined by a study by Saia et al.,3 in which an increased risk of BRONJ was reported in subjects who received oral nitrogen-containing bisphosphonates for more than 3 years. An incidence rate of 7.96% was reported in patients with more than 3 years of drug administration, whereas an incidence of 1.43% was reported in patients with less than 3 years of administration, which was a statistically significant difference. Pazianas et al.1 reported that the period of administration had no relationship with the incidence of BRONJ, with 3 out of 9 BRONJ patients having less than 3 years and the other 6 patients having more than 3 years of drug administration. However, direct comparisons with the results of the current study cannot be drawn, as the subjects were selected from patients already affected by BRONJ. According to the results of the current study, the length of the drug administration period had a greater significance in predicting the probability of BRONJ occurrence than the drug type.
The CTx level as an indirect numerical indicator of osteoclast activity has been suggested to be mandatory for consideration prior to tooth extractions, with a cut-off point of 150 pg/mL.21 Lazarovici et al.15 claimed that the CTx level cannot be a definitive predictor of BRONJ incidence but may play an important role in the preoperative risk assessment. In this study, the incidence rate of BRONJ was higher in the group with a CTx level of less than 150 pg/mL, but not to a statistically significant extent; this result is comparable to that of previous studies.
Various local factors may affect the incidence rate of BRONJ; among those, age, site of extraction, and the drug administration period can be considered to be important factors. Therefore, among the patients on oral bisphosphonates for the treatment of osteoporosis, greater care needs to be taken for those who are older than 65 years and for those with a period of administration longer than 3 years. In addition, close follow-up is necessary in the case of BRONJ incidence so that appropriate treatment can be delivered in the early phase of the condition.
Footnotes
This material is based on work supported by the Ministry of Trade, Industry & Energy (MOTIE, Korea) under the Advanced Technology Center Program, No. 10062362: The development of dental and medical prosthetics modeling, rapid fabrication and integrated trading system based and converged on CBCT image, using Cloud networking.
References
- 1.Pazianas M, Miller P, Blumentals WA, Bernal M, Kothawala P. A review of the literature on osteonecrosis of the jaw in patients with osteoporosis treated with oral bisphosphonates: prevalence, risk factors, and clinical characteristics. Clin Ther. 2007;29:1548–1558. doi: 10.1016/j.clinthera.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Tosteson AN, Gabriel SE, Grove MR, Moncur MM, Kneeland TS, Melton LJ., 3rd Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int. 2001;12:1042–1049. doi: 10.1007/s001980170015. [DOI] [PubMed] [Google Scholar]
- 3.Saia G, Blandamura S, Bettini G, Tronchet A, Totola A, Bedogni G, et al. Occurrence of bisphosphonate-related osteonecrosis of the jaw after surgical tooth extraction. J Oral Maxillofac Surg. 2010;68:797–804. doi: 10.1016/j.joms.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 4.Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention TriaI. JAMA. 1998;280:2077–2082. doi: 10.1001/jama.280.24.2077. [DOI] [PubMed] [Google Scholar]
- 5.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, et al. Fracture Intervention Trial Research Group. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet. 1996;348:1535–1541. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 6.Delmas PD, Recker RR, Chesnut CH, 3rd, Skag A, Stakkestad JA, Emkey R, et al. Daily and intermittent oral ibandronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int. 2004;15:792–798. doi: 10.1007/s00198-004-1602-9. [DOI] [PubMed] [Google Scholar]
- 7.Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, et al. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. JAMA. 1999;282:1344–1352. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 8.Delmas PD, Adami S, Strugala C, Stakkestad JA, Reginster JY, Felsenberg D, et al. Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum. 2006;54:1838–1846. doi: 10.1002/art.21918. [DOI] [PubMed] [Google Scholar]
- 9.Roelofs AJ, Thompson K, Gordon S, Rogers MJ. Molecular mechanisms of action of bisphosphonates: current status. Clin Cancer Res. 2006;12:6222s–6230s. doi: 10.1158/1078-0432.CCR-06-0843. [DOI] [PubMed] [Google Scholar]
- 10.Stepensky D, Kleinberg L, Hoffman A. Bone as an effect compartment: models for uptake and release of drugs. Clin Pharmacokinet. 2003;42:863–881. doi: 10.2165/00003088-200342100-00001. [DOI] [PubMed] [Google Scholar]
- 11.Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61:1115–1117. doi: 10.1016/s0278-2391(03)00720-1. [DOI] [PubMed] [Google Scholar]
- 12.Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaw - 2009 update. Aust Endod J. 2009;35:119–130. doi: 10.1111/j.1747-4477.2009.00213.x. [DOI] [PubMed] [Google Scholar]
- 13.Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, et al. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2007;22:1479–1491. doi: 10.1359/jbmr.0707onj. [DOI] [PubMed] [Google Scholar]
- 14.O'Ryan FS, Lo JC. Bisphosphonate-related osteonecrosis of the jaw in patients with oral bisphosphonate exposure: clinical course and outcomes. J Oral Maxillofac Surg. 2012;70:1844–1853. doi: 10.1016/j.joms.2011.08.033. [DOI] [PubMed] [Google Scholar]
- 15.Lazarovici TS, Mesilaty-Gross S, Vered I, Pariente C, Kanety H, Givol N, et al. Serologic bone markers for predicting development of osteonecrosis of the jaw in patients receiving bisphosphonates. J Oral Maxillofac Surg. 2010;68:2241–2247. doi: 10.1016/j.joms.2010.05.043. [DOI] [PubMed] [Google Scholar]
- 16.Mavrokokki T, Cheng A, Stein B, Goss A. Nature and frequency of bisphosphonate-associated osteonecrosis of the jaws in Australia. J Oral Maxillofac Surg. 2007;65:415–423. doi: 10.1016/j.joms.2006.10.061. [DOI] [PubMed] [Google Scholar]
- 17.Lazarovici TS, Yahalom R, Taicher S, Schwartz-Arad D, Peleg O, Yarom N. Bisphosphonate-related osteonecrosis of the jaw associated with dental implants. J Oral Maxillofac Surg. 2010;68:790–796. doi: 10.1016/j.joms.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 18.Taylor T, Bryant C, Popat S. A study of 225 patients on bisphosphonates presenting to the bisphosphonate clinic at King's College Hospital. Br Dent J. 2013;214:E18. doi: 10.1038/sj.bdj.2013.327. [DOI] [PubMed] [Google Scholar]
- 19.Sedghizadeh PP, Stanley K, Caligiuri M, Hofkes S, Lowry B, Shuler CF. Oral bisphosphonate use and the prevalence of osteonecrosis of the jaw: an institutional inquiry. J Am Dent Assoc. 2009;140:61–66. doi: 10.14219/jada.archive.2009.0019. [DOI] [PubMed] [Google Scholar]
- 20.Hansen PJ, Knitschke M, Draenert FG, Irle S, Neff A. Incidence of bisphosphonate-related osteonecrosis of the jaws (BRONJ) in patients taking bisphosphonates for osteoporosis treatment - a grossly underestimated risk? Clin Oral Investig. 2013;17:1829–1837. doi: 10.1007/s00784-012-0873-3. [DOI] [PubMed] [Google Scholar]
- 21.Marx RE, Cillo JE, Jr, Ulloa JJ. Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg. 2007;65:2397–2410. doi: 10.1016/j.joms.2007.08.003. [DOI] [PubMed] [Google Scholar]