Abstract
The current work describes the implementation of the American Association of Physicists in Medicine (AAPM)'s Task Group 119 report on a volumetric phantom (Delta4, Scandidos, Uppsala, Sweden) following the stated dose goals, to evaluate the step-and-shoot intensity modulated radiation therapy (IMRT) system. Delta4 consists of diode detectors, lying on two crossed planes, measuring the delivered dose, and providing two-dimensional dosimetric information. Seven plans of different goals and complexity were performed, with individual structure sets. TG199 structure sets and plans were transferred and implemented on the Delta4 phantom taking into account its cylindrical geometry. All plans were delivered with a 6 MV linear accelerator equipped with multileaf collimator of 1 cm thickness. Plan results for each test met the recommended dose goals. The evaluation was performed in terms of dose deviation, distance to agreement, and gamma index passing rate. In all test cases, the gamma index passing rate was measured >90%. Delta4 phantom has proven to be fast, applicable, and reliable for the step-and-shoot IMRT commissioning following TG119's recommended tests. Although AAPM's TG119 report is referring to the implementation of test plans that do not correspond to patient plans, it could be used as an evaluation tool of various IMRT systems, considering the local treatment planning system and the delivery system.
Keywords: Commissioning, intensity modulated radiation therapy, quality assurance, volumetric phantom
Introduction
There are many articles and reports referring to the commissioning and the verification process of intensity-modulated radiation therapy (IMRT) system consisting of a linear accelerator (linac) equipped with a multileaf collimator (MLC) and a treatment planning system (TPS) with an inverse planning option. The American Association of Physicists in Medicine (AAPM) 2003 Guidance Document[1] refers to the planning and delivery techniques that are used to enhance the prospects for more accurate and trustworthy results in IMRT commissioning. The document states that the verification measurements are initially implemented on a phantom plan, where the beam segments and the position of the MLCs have to be checked. In clinical routine and for patient-specific quality assurance (QA), a patient plan is transferred on a phantom computed tomography study, recalculating the specific dose distribution on the phantom geometry to be delivered in the phantom. The resulting dose distribution is measured using either ionization chambers, films, or other detectors. The resulting measurement is then compared to the predicted dose to the phantom[1] and the objective is to coincide the planned dose distributions with the measured one.
In 2009, AAPM Task Group (TG) 119[2,3] focused on the problem of quantifying the overall performance of an IMRT system. The report recommends a set of test cases, to assess the accuracy of planning and delivery process of IMRT treatments. It basically refers that those tests should be performed at a primary level in every institution to be able to proceed on IMRT treatments. TG119 recommends verification measurements with ionization chamber for one-dimensional (1D) point measurements and film for two-dimensional (2D) measurements, all performed on a solid water phantom. It is essential to study many different cases and run multiple measurements during the commissioning process to be as accurate as possible and make comparisons between IMRT delivery systems. Performing treatment plans of different type and complexity may arise unidentified inaccuracies of the local treatment and delivery system procedure and hence lead institutions to improve the IMRT process.
Although AAPM TG119 suggests 1D and 2D measurements, it has not been applied so far in literature with a volumetric phantom. The aim of this study is the implementation of AAPM's TG119 Report on a volumetric dosimetric phantom to evaluate step-and-shoot IMRT procedure at our department.
Materials and Methods
All measurements were carried out at Aretaieion University Hospital in a 6 MV photon beam linac Siemens Oncor Impression. It is equipped with an MLC of 82 leaves in the X-axis and a nominal width of 1 cm at the isocenter. The Y-axis jaws could move independently creating the desirable field length. The treatment planning was done on the local TPS Oncentra V4.3 (Nucletron, Elekta). The dose distribution for all the test cases was calculated using a collapsed cone convolution algorithm both for optimization process and for final dose calculation. The calculation grid used during the planning process was 0.15 cm.
Gamma index: A quantitative tool for dose distribution comparison
The idea of dose deviation (DD) was introduced by Van Dyk et al.[4] It referred to the comparison between two dose distributions at low dose gradient areas. Mistreatments that may occur during setup and alignment of a detector system showed a great influence on the results of the comparison. To confront those drawbacks, Van Dyk introduced another quantitative tool, described by the distance to agreement (DTA) for low dose at low gradient areas. It was applied then by Harms et al.,[5] as a software tool, introducing the idea of the closest distance between two dose distributions, which lie at the same dose level. To achieve more precise and accurate results, Low[6] combined the two parameters, DD and DTA, into one factor, the gamma index. This factor is satisfied when both variables DD and DTA pass specific criteria. Many groups have attempted to develop methods for the improvement of the calculation of gamma index, with Stock et al.[7] in 2005, to introduce 2D gamma analysis and gamma histograms for complex dose distributions.
Hence, within the gamma index, DTA, and DD were summarized to one evaluation tool for the verification of a treatment plan. Gamma criteria of 3 mm DTA and 3% DD were used for the evaluation of IMRT treatment plans. The criteria's threshold, as Low stated, could be modified depending on the clinical needs that are examined.[6] Moreover, it is possible to set an acceptable benchmark passing rate, below which, the gamma index is unacceptable and above that, passes the criteria. In this work, a passing rate of 90% and above for the gamma index (3% DD/3 mm DTA) was considered as acceptable.[8]
Delta4 phantom
All test cases, investigated in this work, were planned and delivered on Delta4 Phantom (Scandidos, Uppsala, Sweden). Delta4 is a cylindrical, polymethylmethacrylate phantom, consisting of two orthogonal detector planes in a crossed array. It consists of 1069 p-type silicon diodes that can measure point doses and can be used for QA of patient-specific treatment delivery. The detector planes spatial resolution is 5 mm at the central area of 6 cm × 6 cm and 10 mm at the outer area in each plane. The cylindrical phantom has diameter and length of 22 cm and 40 cm, respectively.[9]
For the verification of a patient treatment plan, it was applied on a Delta4 phantom and the dose distribution inside the phantom was recalculated in the TPS. The comparison between the calculated and the measured radiotherapy (RT) dose was translated to DTA, DD, and gamma index. The evaluated gamma passing rate is only given for the measured points in the two detector planes, therefore the analysis is limited to the measurement points.[9] Diodes that received a dose less than a certain percentage of the maximum absorbed dose was ignored in the analysis. These ignored readings typically were located in the low gradient regions where the diode response is less reliable.[10] In this work, dose values below 10% of the dose maximum were excluded from the final result. It has to be emphasized that there is not a direct calculation of the delivered dose for every point within the phantom. However, according to the manufacturer, a 3D calculation of the delivered dose is available, even if the planned control points are missing. This interpolation method theoretically uses depth dose distributions for different field sizes, calculated with the TPS for the Delta4 phantom and processed by its software. The 3D dose determination for a single beam in the cylindrical Delta4 phantom requires the planned dose to be known in the complete cylindrical volume, while the measured dose to be known in the two orthogonal detector planes.
The planned dose for each beam is renormalized using the ratio between the planned and the measured dose at the intersection point of the beam with the detector plane. Finally, the dose is calculated for all the radiation fields.[11] The above process has been carried out during the calibration of the phantom, which is recommended by the manufacturer to be performed once a year including the wing uniformity response, directional dependence, and absolute dose calibration.
Reference treatment planning data, such as DICOM RT objects, beam arrangement, and structures from the original plan were transferred to the Delta4 system. The software has a variety of tools for displaying the differences between the measured and the calculated dose. The gamma analysis was performed based on the formulae by Low et al.[12] The histograms of DD, DTA, gamma index,[6] and the passing rates were calculated by the Delta4's software (Scandidos, Uppsala, Sweden). For the statistical calculation, all detectors from both the detector boards were used.
Before the evaluation of an IMRT plan, two more measurements were done by delivering 100 cGy with a 10 cm × 10 cm field at gantry angles of 0° and 90°, in order to check the phantom for positional corrections and linac output constancy.[13] These setup corrections were then applied to the rest of the measurements performed with the same phantom position.
American Association of Physicists in Medicine Task Group-119 report
TG119 report suggests seven test cases for the evaluation of the IMRT procedure. Each case included a target and peripheral normal structure shapes in a DICOM format, which were imported in the TPS. Thereafter, the DICOM RT structures were fused and registered on the dosimetric phantom. Each test also included specific dose goals [Tables 1–5] and beam arrangement to be applied. The seven tests were of varying type and complexity, and hence different optimization criteria had to be used. Each case required certain specific measurements to be performed for testing the accuracy of both delivery and planning systems, through comparison of the results with the published values in the report.
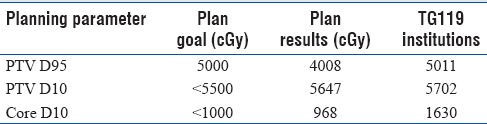
Table 1.
Treatment planning statistics for multitarget
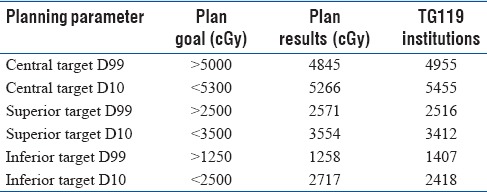
Table 5.
Treatment planning statistics for C-shape (harder)
Preliminary/forward planning test cases
Test P1: Anterior-posterior: Posterior-anterior and Test P2: Bands
Test P1 is a simple, parallel-opposed setup of the phantom using anterior-posterior: Posterior-anterior (AP: PA), 10 cm × 10 cm fields to a dose of 200 cGy to the isocenter.
Test P2 (Bands test) is also a simple, parallel-opposed setup using a series of adjacent AP: PA fields, to create a set of five bands, 3 cm wide and a total field length of 15 cm. This was achieved by opening the jaws at Y-axis up to 15 cm at field length, while the MLC's, which lie in X-axis, were moving asymmetrically producing gradually a field width of 15 cm of 3 cm per time). The proposed dose escalation to be achieved was 40–200cGy, in five 40cGy steps.
Inverse planning test cases
Test I1: Multitarget
Multitarget consists of three cylindrical targets, which are stacked along the axis of rotation of the gantry. Each has a diameter of 4 cm and length of 4 cm. The objective of the test is to deliver different doses to each target, with the central target receiving the largest dose per fraction, and the superior and targets receiving 50% and 25% of the prescribed dose respectively. Dose goals are specified as D99, referring to the dose of 99% of the volume and D10, referring to the dose of 10% of the volume respectively, for each and every target [Table 1].
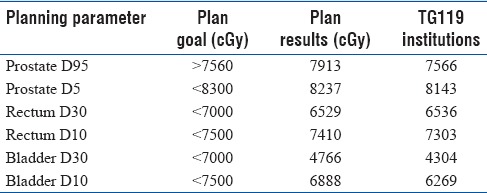
Test I2: Mock prostate
At the mock prostate test case, the planning target volume (PTV) is expanded 0.6 cm around the clinical target volume of the prostate with a posterior concavity. The bladder and the rectum are also included in the structure set and need to be protected. Dose goals for prostate PTV, are specified as D95 and D5, referring to the dose of 95% and 5%, respectively. In addition, rectum and bladder have to be protected, and dose has to be kept under specific limits. D30 and D10, which are referring to the dose of 30% and to the dose of 10% of the volume, respectively, have to be characterized [Table 2].
Table 2.
Treatment planning statistics for mock prostate
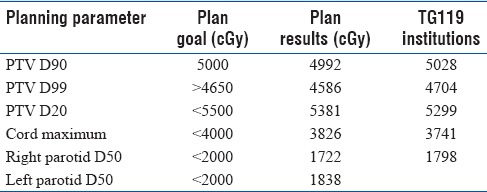
Test I3: Mock head/neck
The PTV head/neck test case includes all anterior volume from the base of the skull to the upper neck, including the posterior neck nodes. The parotid glands and the spinal cord are also outlined and have to be protected. For the PTV, dose goals are specified as D99, D90, and D20 describing the respective dose percentages of the target. For the parotids, D50 was used, referring to the dose received by 50% of the volume, whereas the maximum dose for the cord has to be kept under 4000 cGy [Table 3].
Table 3.
Treatment planning statistics for mock head/neck
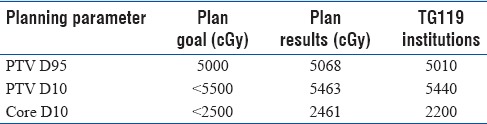
Test I4 and I5: C-shape
The last two IMRT plans refer to a C-shaped target that surrounds a central avoidance structure. The center core is a cylinder 1 cm in radius and is located in the inner arc of the PTV. Two versions of this test case, with different numerical goals but with the same beam arrangements, were examined. In the first and easier one, the central core must be kept under 50% of the target dose, while in the second and harder test case the central core has to be kept below 20% of the target dose. For both cases, PTV dose goals are specified as D95, aka the dose to 95% of the volume and D10, aka the dose to 10% of the volume. For the core, D10 needs to meet individual criteria, which are stricter for the harder case [Tables 4 and 5].
Table 4.
Treatment planning statistics for mock C-shape (easier)
Results
The proposed dose goals from TG119 and plan results from the local TPS are shown in Tables 1–5, individually for all the tests performed at our department. Mean values achieved by the institutions referred to the TG119 report are also shown in Tables 1–5, respectively. Results refer to the doses in cGy of the different PTV's and to the organs at risk that have to be protected according to TG119.
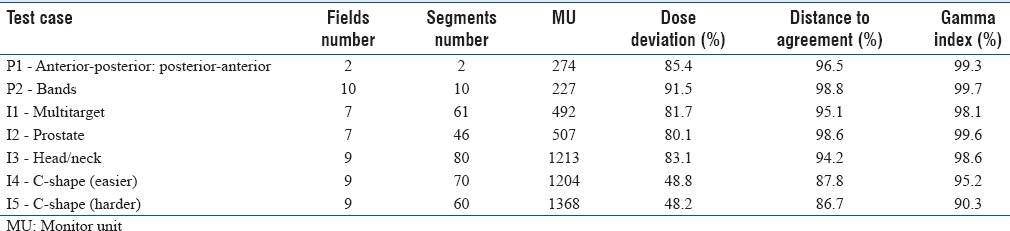
Planning parameters, including number of fields, segments and monitor units (MU's), and the gamma analysis results of each test case, including DD, DTA, and gamma index passing rates, are also presented in Table 6.
Table 6.
Results of dose deviation, distance to agreement, and gamma index for all the test cases
Test P1: Anterior-posterior: Posterior-anterior and P2: Bands
The percentage of gamma passing rate of the test P1 is 99.3%, and for the test, P2 is 99.7%. For the simple irradiation of parallel-opposed fields, AP: PA and bands test, the results of gamma index were high. Those tests could also be performed as a primary accuracy check of a delivery system for everyday practice.
Tests I1: Multitarget
The gamma passing rate for the multitarget was calculated at 98.1%. Test case I1 represents a concomitant target IMRT, asking from the planner to achieve gradually different doses to the three targets. The DD pass percentage was 81.7% and the DTA pass percentage was 95.1%.
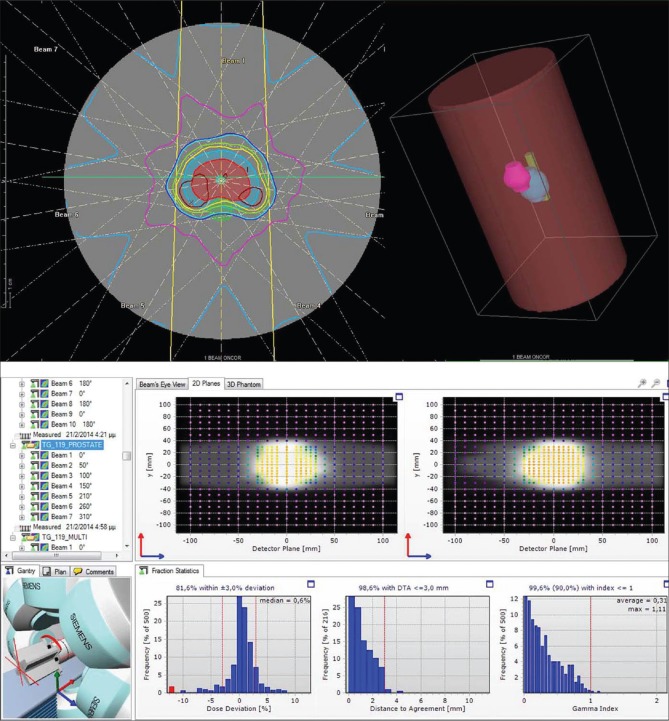
Test I2: Mock prostate
The gamma passing rate for test I2 was 99.6%, while the pass percentages of DD and DTA were 80.1% and 98.6% respectively. Dose distribution at axial projection and on the Delta4 planes and the gamma index results are also provided [Figure 1].
Figure 1.
Dose distribution, dose deviation, distance to agreement, and gamma index of test case I2: Prostate.
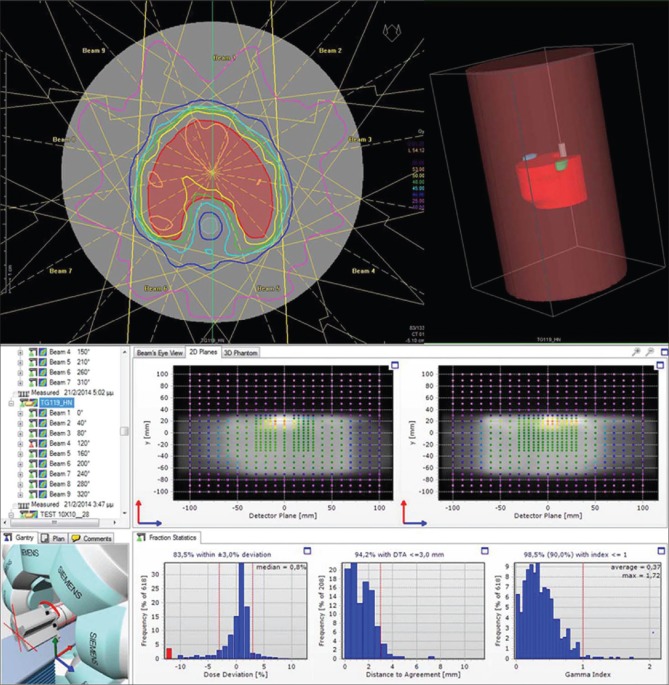
Test I3: Mock head/neck
The gamma passing rate for the I3 test case was 98.6%, while the pass percentages of DD and DTA were 83.1% and 94.2% respectively. The mock structures of the spinal cord and the parotid glands showed a decline in dose, while target receives at least 95% of the prescribed dose [Figure 2].
Figure 2.
Dose distribution, dose deviation, distance to agreement, and gamma index of test case I3: Head/neck.
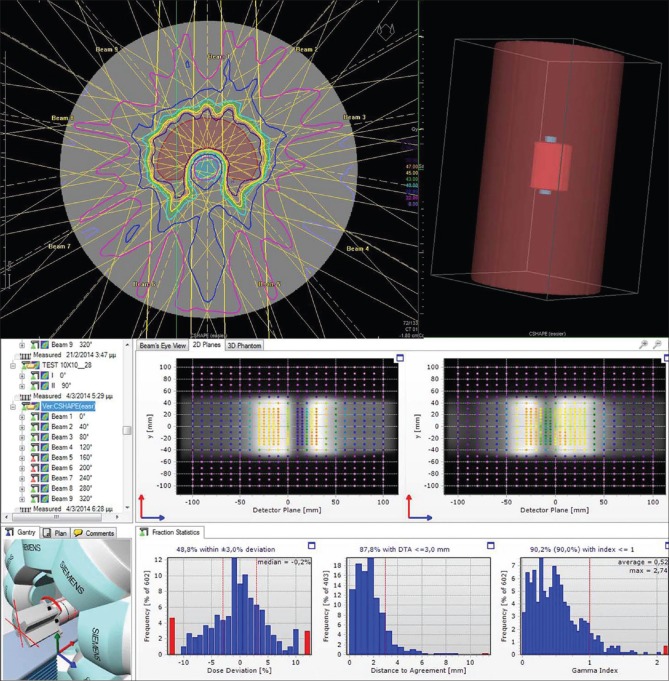
Tests I4 and I5: C-shape
For each case of the C-shape test, different objectives and constraints had to be achieved. For the easier case, the pass percentage of gamma index was 95.2%, while that for DD and DTA were 48.8%, and 87.8% respectively and are presented below [Figure 3]. For the harder case, the gamma index pass percentage was 90.3%. For the DD and DTA, the pass percentages were 48.2% and 86.7% respectively.
Figure 3.
Dose distribution, dose deviation, distance to agreement, and gamma index of test case I2: C-shape (easier).
Discussion
For each TG119 test case, there were specific dose goals that had to be fulfilled by the IMRT system, including the TPS, the optimization algorithm, and the linac's MLC system. In Tables 1–5, the plan results of our IMRT system are presented. As it can be seen most of our plan results met the TG119 recommended dose goals.
The multitarget test case was satisfied for most of the planning goals, except the D99 for the central target with a difference of 3.1% lower dose coverage than the required constraint and the D10 for the superior target with a difference of 1.5% higher value than the TG119's constraint. These differences are low and could be considered as acceptable, while the rest parameters satisfied the TG119 needs. Considering the results of the institutions with the dose goals of TG119, there was a difficulty in achieveing the goals of D99 and D10 of the central target by 0.9% lower and 2.9% higher than the asked values, respectively.
Regarding mock prostate test case, all the specified goals were met. Like the other institutions, the doses to critical organs were kept much lower than the proposed doses. Furthermore, the dose coverage at the PTV both for the D95 and the D5 did satisfy the stated goals.
For the head/neck test case there was a 1.4% deficiency in reaching the goal for D99 of the PTV and also a deficiency of 0.2% in achieving the goal of PTV D90, while PTV D20 stayed below 2.2% the required dose. On the other hand, the published results in the report satisfied all the goals both for the PTV and for organ-at-risks (OARs). However, due to the fact that the deviations of the dose that we measured are lower than 3% of the proposed dose, they could be considered as acceptable.
In the easy case of C-shape, the objectives referring to PTV were satisfied with the core to be kept under the proposed dose. TG119 results for the easy case of C-shape were also acceptable for the D95 and D10 of the PTV, and also the core kept under the asked limits. However, in the harder case of C-Shape, there was a disability to keep PTV D10 lower than the goal, and there was a deficiency in meeting the benchmark value of D95 for PTV. Nevertheless, the cord dose was kept lower than 1000 cGy. Unlike other institutions, we chose to preserve the core and underdose the PTV in order to stay below the core constraint. The report's results, on the contrary, satisfied the dose coverage of PTV95 by remaining 0.2% above the proposed goal, but at the same time, PTV D10 exceeded the proposed value by 3.7% and also D10 for the core exceeded by 63% of the required constraint.
Another basic purpose of the implementation of the tests was to check if the measured dose from the diodes of the phantom agreed with the planned dose from the TPS. The comparison included measuring the percentages of DD, DTA, and from those two the percentage of gamma index. It is essential, these three parameters to be combined for more accurate results. Acceptance criteria of 3% DD, 3 mm DTA, and 90% threshold of the passing rate for the gamma index were used. As presented in Table 4, in all test cases, the gamma index passing rate was measured >90%. Furthermore, in each test case DTA was measured closer to the gamma index value than the DD value, respectively. However, in the C-shape test cases, even though the gamma index has been satisfied, DD or/and DTA have been measured relatively low. The above has been stated by Low et al.,[14] to prove that it is not obligatory for the acceptance of gamma index percentage to conclude to also acceptable percentages of DD and DTA. In particular, it is mentioned that DTA tool is more intense and variable at steep dose gradient regions, where as the spatial discrepancy of dose distributions is rather low. In clinical practice, a treatment plan, in order to be accepted, must be verified by comparing the measured dose with the planned dose. Different practice has to be followed for different cases, referring to the criteria that a plan needs to satisfy depending on tumor/critical organs and taking into account the uncertainties of spatial resolution. Nevertheless, Low et al.[14] studied and have proved that these two vectors tend to conclude to similar results. As an illustration, all above measurements have shown this tendency of DTA to the gamma index pass percentage. The DD pass percentage on the other hand, shows a general decline to most of the test cases, despite gamma index's acceptable percentage. The DD pass percentage was the lowest for the harder case of C-shape test at 50%. The complexity of the planning goals for the individual plans was varied according to the objectives and the constraints given in TG119. The measured DD, DTA, and gamma index histograms of the forward plans resulted in high pass percentages. The two forward plans can be used as an initial cross-check of the planning and the delivery system, before the IMRT procedure. The IMRT plans resulted in acceptable pass percentages of the gamma index and did meet the criteria asked from the report. In addition, from IMRT results it was revealed an increase in the planned MU's with the complexity of the plans and respectively a decrease in the gamma passing rate.
Summing up, Delta4 provides a thorough data analysis and a relatively faster way to take measurements without necessitating further QA systems. Measurements take place on the two planes of the phantom, where a 3D dose distribution of the dose could be computed by the software of the phantom through an interpolation method. A major advantage using a volumetric phantom for the implementation of TG119 is that one measurement is enough to calculate absolute doses at different points corresponding to points in PTVs and OARs. The measurement procedure with the volumetric phantom gives much more information than point dose measurement with an ionization chamber. The Delta4 phantom can be set-up easily, and positional errors could be diminished to the minimum. It is important that the initial calibration and the commissioning process of Delta4 has to be accomplished with rigorous and careful measurements to ensure patient specific QA tests are accurate.[8] Last but not least, it should be noted that TG119 report refers to commissioning process of an IMRT system at a primary level. Consequently, it cannot be used directly on the clinical practice, because it refers to methods that should be followed in order to test the IMRT planning and delivery system before perform IMRT plans on actual patients. In addition, the report's test cases refer to specific mock structures but in real patient cases there might be multiple OARs, and also the size of PTVs/OARs may differ. The requirements to fulfill according to TG119 report were of high intricacy both for the planning and for the delivery system. Comparing our results with those of other institutions, it was concluded that even if they are similar in most of the test cases, (except the test case of harder C-shape), they cannot be compared directly. This is basically because institutions referred in this report used different delivery and planning systems. Results reported in TG119 report refer to mean values of doses that were achieved by all institutions collectively and not individually.
Conclusion
Delta4 phantom has proven to be fast and reliable for the step-and-shoot IMRT commissioning following TG119's recommended tests. AAPM TG119 test cases have been applied successfully on the Delta4 volumetric phantom, providing accurate results at a primary level and before any clinical use. It has to be noted that the test cases refer to theoretical objectives and constraints but not to practical guidelines on performing IMRT plans on actual patients. Nevertheless, the TG119 report could be used as an evaluation tool of different IMRT systems between institutions, in order to compare results for different combinations of planning and delivery techniques.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Galvin JM, Low D, Palta JR, Rosen I, Sharpe MB, Xia P, et al. AAPM REPORT: Guidance Document on Delivery, Treatment Planning, and Clinical Implementation of IMRT: Report of the IMRT Subcommitte of the AAPM Radiation Therapy Committee. 2003 doi: 10.1118/1.1591194. [DOI] [PubMed] [Google Scholar]
- 2.Ezzell GA, Burmeister JW, Dogan N, LoSasso TJ, Mechalakos JG, Mihailidis D, et al. IMRT commissioning: Multiple institution planning and dosimetry comparisons, a report from AAPM Task Group 119. Med Phys. 2009;36:5359–73. doi: 10.1118/1.3238104. [DOI] [PubMed] [Google Scholar]
- 3.TG-119 IMRT Commissioning Tests Instruction for Planning, Measurement, and Analysis Version 10/21/2009, Digital File Support. www,aapm.org/pubs/tg119/default.asp .
- 4.Van Dyk J, Barnett RB, Cygler JE, Shragge PC. Commissioning and quality assurance of treatment planning computers. Int J Radiat Oncol Biol Phys. 1993;26:261–73. doi: 10.1016/0360-3016(93)90206-b. [DOI] [PubMed] [Google Scholar]
- 5.Harms WB, Sr, Low DA, Wong JW, Purdy JA. A software tool for the quantitative evaluation of 3D dose calculation algorithms. Med Phys. 1998;25:1830–6. doi: 10.1118/1.598363. [DOI] [PubMed] [Google Scholar]
- 6.Low DA. Gamma dose distribution evaluation tool. J Phys Conf Ser. 2010;250:12071. [Google Scholar]
- 7.Stock M, Kroupa B, Georg D. Interpretation and evaluation of the gamma index and the gamma index angle for the verification of IMRT hybrid plans. Phys Med Biol. 2005;50:399–411. doi: 10.1088/0031-9155/50/3/001. [DOI] [PubMed] [Google Scholar]
- 8.Low DA, Moran JM, Dempsey JF, Dong L, Oldham M. Dosimetry tools and techniques for IMRT. Med Phys. 2011;38:1313–38. doi: 10.1118/1.3514120. [DOI] [PubMed] [Google Scholar]
- 9.Scandidos, Delta4PT user manual. Uppsala, Sweden: Scandidos; [Google Scholar]
- 10.Nilsson J, Karlsosn Hauer A, Bäck A. IMRT patient-specific QA Using the Delta4 Dosimetry System and Evaluation Based on ICRU 83 Recommendations”. Paper Presented at: 7th International Confernsce on 3D RAdiation Dosimetry. 2013 [Google Scholar]
- 11.Calvo O, Gutiérrez A, Stathakis S, Mavridis P, Moral S, Esquivel C, Shi C, Papanikolaou N. Validation of the Delta4 dosimetry phantom against ionometic measurements. Med Phys. 2009;36:2610. [Google Scholar]
- 12.Low DA, Harms WB, Mutic S, Purdy JA. A technique for the quantitative evaluation of dose distributions. Med Phys. 1998;25:656–61. doi: 10.1118/1.598248. [DOI] [PubMed] [Google Scholar]
- 13.Antypas C, Floros I, Rouchota M, Armpilia C, Lyra M. MLC positional accuracy evaluation through the picket fence test on EBT2 films and a 3D volumetric phantom. J Appl Clin Med Phys. 2015;16:5185. doi: 10.1120/jacmp.v16i2.5185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Low DA, Morele D, Chow P, Dou TH, Ju T. Does the dose distribution comparison technique default to the distance to agreement test in clinical dose distributions? Med Phys. 2013;40:071722. doi: 10.1118/1.4811141. [DOI] [PubMed] [Google Scholar]