Abstract
We performed an observational analysis of a prospective cohort of immunocompetent hospitalized adults with community-acquired pneumonia (CAP) to determine the epidemiology, clinical features, and outcomes of pneumonia in patients with diabetes mellitus (DM). We also analyzed the risk factors for mortality and the impact of statins and other cardiovascular drugs on outcomes. Of 2407 CAP episodes, 516 (21.4%) occurred in patients with DM; 483 (97%) had type 2 diabetes, 197 (40%) were on insulin treatment, and 119 (23.9%) had end-organ damage related to DM. Patients with DM had different clinical features compared to the other patients. They were less likely to have acute onset, cough, purulent sputum, and pleural chest pain. No differences in etiology were found between study groups. Patients with DM had more inhospital acute metabolic complications, although the case-fatality rate was similar between the groups. Independent risk factors for mortality in patients with DM were advanced age, bacteremia, septic shock, and gram-negative pneumonia. Patients with end-organ damage related to DM had more inhospital cardiac events and a higher early case-fatality rate than did the overall population. The use of statins and other cardiovascular drugs was not associated with better CAP outcomes in patients with DM. In conclusion, CAP in patients with DM presents different clinical features compared to the features of patients without DM.
INTRODUCTION
Diabetes mellitus (DM) is one of the most common chronic diseases worldwide and is associated with high morbidity and mortality.2 This metabolic disorder causes damage in multiple organs. Moreover, several aspects of immunity are altered in patients with diabetes. The normal role of polymorphonuclear leukocytes, leukocyte adherence, chemotaxis, and the processes of phagocytosis may all be compromised.7,16,27 Antioxidant systems involved in bactericidal activity can also be impaired.31 However, the impact that these disturbances have on the development and outcomes of infectious diseases has been poorly studied.
Community-acquired pneumonia (CAP) is one of the most frequent infections requiring hospitalization in developed countries.29 However, information regarding the clinical features, etiology, and outcomes of CAP in patients with DM is scarce. In a 2011 report,9 patients with DM compared with patients without DM had a higher risk of death from pneumonia and other infectious diseases. However, it is not known whether factors related to mortality in patients with both DM and CAP differ from those in CAP patients without DM. The use of statins and other cardiovascular drugs has been suggested as a promising option for improving the prognosis of CAP.37 Since DM poses a high cardiovascular risk even in the absence of known coronary artery diseases, the American Diabetes Association states that statin treatment is frequently indicated in this population.2 Prospective studies testing the effect of statins on outcomes in patients with DM and CAP are, however, lacking. Interestingly, a recent study34 documented that statin treatment may reduce the incidence of pneumonia. Among 17,802 patients, incident pneumonia was reported as an adverse event in 214 (1.1%) participants in the rosuvastatin group and 257 (1.3%) in the placebo group.
We conducted the current study to determine the epidemiology, clinical features, and outcomes of CAP in patients with DM. A further aim was to assess the risk factors for mortality in patients with DM and CAP and to evaluate the impact of the severity of DM and the use of statins and other cardiovascular drugs on outcomes.
PATIENTS AND METHODS
Setting, Patients, and Study Design
This observational study was conducted at an 800-bed university hospital for adults in Barcelona, Spain. All nonseverely immunosuppressed adult patients admitted with pneumonia through the hospital’s emergency department between January 2002 and July 31, 2010, were prospectively recruited and followed. Patients with CAP were identified at the emergency department by the attending physicians and/or the study investigators. Clinical and laboratory data on all patients were prospectively recorded using a computer-assisted protocol. Patients with neutropenia, solid organ transplantation, chemotherapy, acquired immunodeficiency syndrome, or current corticosteroid therapy (≥20 mg prednisone/d or equivalent) at admission were excluded. The study was approved by the ethics committee of our institution.
Clinical Assessment and Antibiotic Therapy
Patients were seen daily during their hospital stay by 1 or more of the investigators, who recorded clinical data in a computer-assisted protocol. Data were collected on demographic characteristics, comorbidities (for example, chronic pulmonary disease, chronic cardiac disease, chronic renal disease, chronic liver disease, dementia, and cancer), causative organisms, antibiotic susceptibilities, biochemical analysis, empirical antibiotic therapy, and outcomes. Baseline glycemia was obtained from the central laboratory database. The Pneumonia Severity Index (PSI) was used to stratify patients into risk classes.13
Antibiotic therapy was initiated in the emergency department in accordance with hospital guidelines, which recommend the administration of a β-lactam (ceftriaxone sodium or amoxicillin/clavulanate potassium) with or without levofloxacin. Combination therapy was recommended for patients with clinical suspicion of a Legionella species or an atypical pathogen, as well as in the absence of a demonstrative finding on sputum Gram stain results. Levofloxacin monotherapy was recommended for patients with a positive urine antigen test for Legionella pneumophila serogroup 1, as described elsewhere.5 Combined amoxicillin/clavulanate was recommended for patients with clinical suspicion of aspiration pneumonia to provide adequate antianaerobic coverage.
Definitions
Pneumonia was defined as the presence of an infiltrate on a chest radiograph plus an acute illness associated with 1 or more of the following signs and symptoms: new cough with or without sputum production, pleuritic chest pain, dyspnea, fever or hypothermia, altered breath sounds on auscultation, or leukocytosis. Aspiration pneumonia was diagnosed on a clinical and radiologic basis in patients who had risk factors such as compromised consciousness, altered gag reflex, dysphagia, severe periodontal disease, putrid sputum, and radiographic evidence of involvement of a dependent pulmonary segment or necrotizing pneumonia.
A diagnosis of DM was made when the fasting plasma glucose concentration was ≥7.0 mmol/L (126 mg/dL) on 2 or more separate occasions, or when a random plasma glucose ≥11.1 mmol/L (200 mg/dL) was found in a patient with classic symptoms of hyperglycemia.1 Alternatively, the diagnosis was based on a previous clinical and/or biochemical diagnosis of DM and/or treatment with oral antidiabetic agents or insulin. DM-related end-organ disease was defined as the presence of microvascular complications (retinopathy, nephropathy, and somatic neuropathy) or macrovascular complications (peripheral vascular disease, coronary artery disease, and stroke). The use of statins and cardiovascular drugs (angiotensin-converting-enzyme inhibitor, acetylsalicylic acid, and beta-blockers) was documented by medical records and patients’ self-reported prescription and drug compliance.
Vaccination status was assessed from interviews with patients or their relatives, as well as from reviews of hospital and personal health records (vaccination card). Patients were considered to be pneumococcal-vaccinated if 23-valent polysaccharide pneumococcal vaccine had been administered in the 5 years before admission, and influenza-vaccinated if seasonal influenza vaccine had been administered during the year before admission. The diagnosis of septic shock was based on a systolic blood pressure of less than 90 mm Hg and peripheral hypoperfusion with the need for vasopressors. A comorbid condition was defined by the presence of 1 or more disorders in addition to diabetes. Initial inappropriate therapy was defined as the absence of antimicrobial agents directed at a specific type of organism or administration of an antibiotic to which the organism was resistant, according to susceptibility test criteria for lower respiratory tract pathogens.
Complications were defined as any untoward circumstances occurring during hospitalization, with the exception of side effects from medication. Inhospital cardiac events included acute coronary syndromes, arrhythmias, and decompensated heart failure. Inhospital metabolic complications included hyperglycemia, altered sodium or potassium values, alkalosis, and acidosis. Diabetic ketoacidosis was defined as glycemia greater than 13.8 mmol/L (>250 mg/dL), arterial pH <7.30, a serum bicarbonate concentration <15 mmol/L, presence of urine ketone and anion gap >12 mEq/L.24 Time to clinical stability was defined as described elsewhere.20 The early case-fatality rate was defined as death due to any cause <48 hours after hospitalization, whereas the overall case-fatality rate was death due to any cause <30 days after hospitalization.
Microbiologic Studies
Pathogens in blood, normally sterile fluids, sputum, and other samples were investigated using standard microbiologic procedures. The Streptococcus pneumoniae antigen in urine was detected using a rapid immunochromatographic assay (NOW Assay; Binax Inc., Portland, ME). Isolation of Legionella was attempted in sputum and other respiratory samples using selective media (BCYE-α). L. pneumophila serogroup 1 antigen in urine was detected by either an immunochromatographic method (NOW Legionella Urinary Antigen Test; Binax Inc.) or an enzyme-linked immunosorbent assay (ELISA-Bartels, Bartels, Trinity Biotech, Wicklow, Ireland). Standard serologic methods were used to determine antibodies against the following pathogens: Mycoplasma pneumoniae (indirect agglutination), Chlamydophila psittaci (immunofluorescence [IF]), Chlamydophila pneumoniae (micro-IF), Coxiella burnetii (IF), L. pneumophila (serogroups 1-6) (enzyme immunoassay [EIA]), respiratory syncytial virus (EIA), parainfluenza 3 virus (EIA), and influenza A virus (EIA) (on admission and 3–4 weeks thereafter). The etiology was considered if 1 of the following criteria was met: a fourfold increase in IgG titers for C. pneumoniae (IgG >1:512), C. psittaci (IgG >64), L. pneumophila >1:128, C. burnetii >1:80, and respiratory viruses; or a single increased IgM titer for C. pneumoniae >1:32, C. burnetii >1:80, and M. pneumoniae (any titer).
The antibiotic sensitivity of all isolates was determined at the laboratory of the microbiology service, Bellvitge University Hospital, by microdilution method, in accordance with criteria of the Clinical and Laboratory Standards Institute.
Statistical Analysis
Categorical variables were described using counts and percentages from available data. Continuous variables were expressed as the mean and standard deviation, or median and interquartile range for non-normally distributed data (Kolmogorov-Smirnov test). In the first analysis we compared patients with and without DM. Significant differences between groups were detected by means of the chi-square test or Fisher exact test for categorical variables, and by the Student t test or Mann-Whitney test for continuous variables, as appropriate.
A second analysis was then performed to compare patients with DM who died with those who survived. This was a multivariate analysis to determine independent risk factors for mortality in patients with DM. Significant variables detected in the univariate analysis and that were considered clinically important variables were entered into the multivariate analysis. The relative risks were expressed as odds ratios and 95% confidence intervals.
Three subanalyses were performed. First, we compared the outcomes of DM patients according to whether or not they received statins, and then repeated this analysis for other cardiovascular drugs. To determine the impact of the severity of DM on CAP, we analyzed the clinical features, etiology, and outcomes of patients who received insulin therapy with those of nondiabetic patients, and then performed the same analysis to compare patients with DM and end-organ damage with nondiabetic patients.
The results were analyzed using SPSS version 15.0 (SPSS Inc., Chicago, IL). A p value of < 0.05 was considered statistically significant. All reported p values are 2-tailed.
RESULTS
Patient Characteristics
We documented 2407 CAP episodes, of which 516 (21.4%) corresponded to diabetic patients. Of the latter, 483 (97%) had type 2 DM, and of these 197 (40%) were on insulin treatment. The median time from DM diagnosis to CAP was 5 years (interquartile range, 3–13). A total of 119 (23.9%) patients had end-organ damage, mainly retinopathy (43%) and vasculopathy (23%).
Table 1 shows the demographic, clinical, and laboratory findings of patients with and without DM. Patients with DM were older and were more likely to present other chronic comorbid conditions, especially chronic pulmonary diseases, chronic heart diseases, cerebrovascular disease, and chronic renal disease. They had more often received statins and were more likely to have been vaccinated against pneumococcus and influenza. By contrast, they were less likely to receive prior antibiotic therapy and to be current smokers and heavy alcohol drinkers. Patients with DM were more often classified into high-risk PSI classes.
TABLE 1.
Characteristics of Pneumonia by Study Group
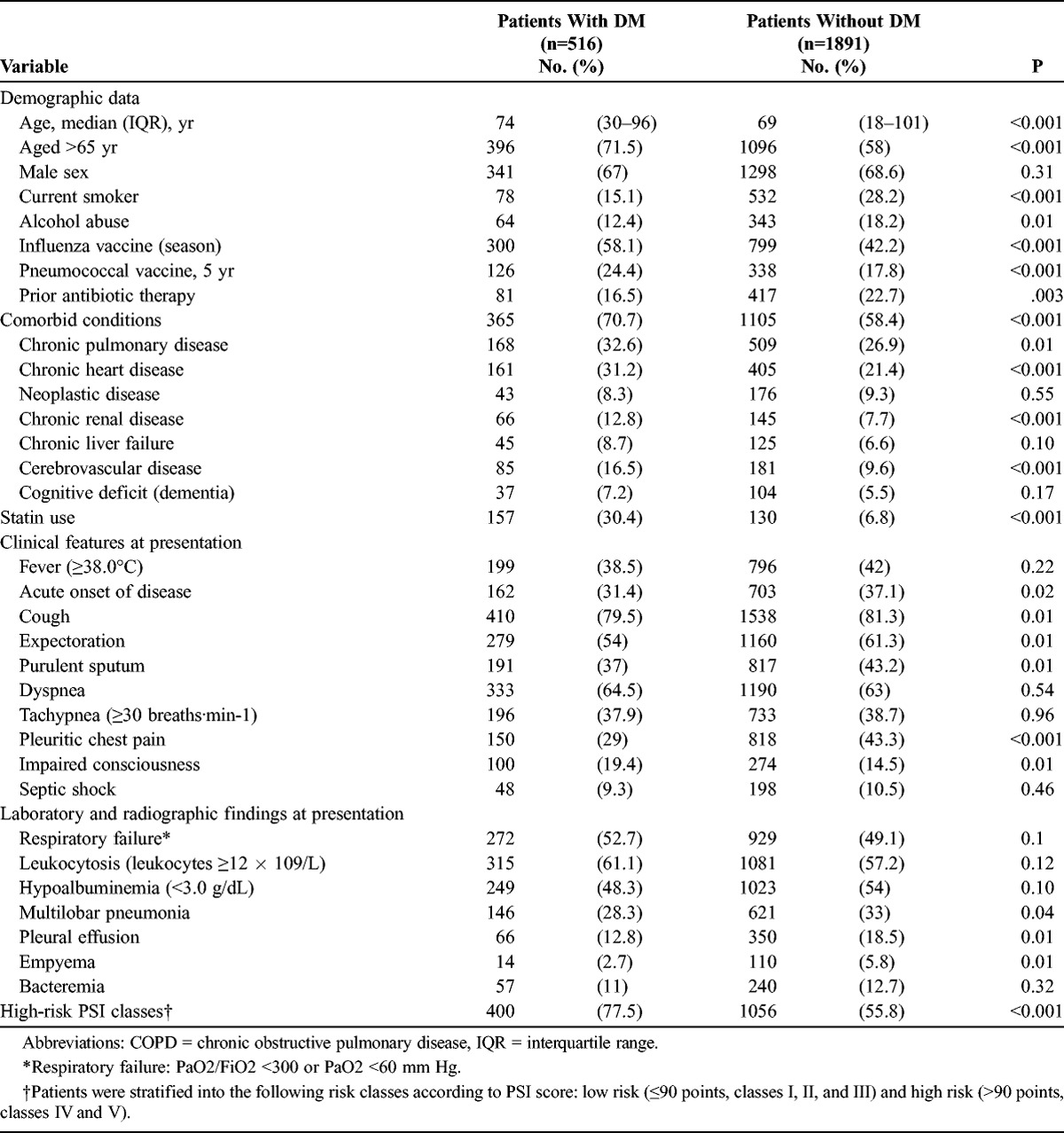
Regarding clinical features, patients with DM more commonly presented with impaired consciousness at admission than patients without DM. Conversely, acute onset of disease, cough, purulent sputum, and pleuritic chest pain were less frequent among patients with DM. Multilobar infiltrates, pleural effusion, and empyema were also less common in patients with DM.
Causative Organisms
The distribution of causative organisms in both groups is detailed in Table 2. There were no significant differences between the study groups as regards pathogens. S. pneumoniae was the most frequent causative organism in patients with DM, followed by aspiration pneumonia, L. pneumophila, and nontypeable Haemophilus influenzae. In patients without DM, the most common causative organism was again S. pneumoniae, followed by aspiration pneumonia, H. influenzae, and L. pneumophila. Serologic tests were performed in 670 patients (26.4% vs. 28.3%; p = 0.40). The frequency of atypical agents was similar in the 2 study groups. In patients with DM, the identified causative pathogens using serologic methods were M. pneumoniae and C. pneumoniae (6 cases each).
TABLE 2.
Etiology of Pneumonia by Study Group
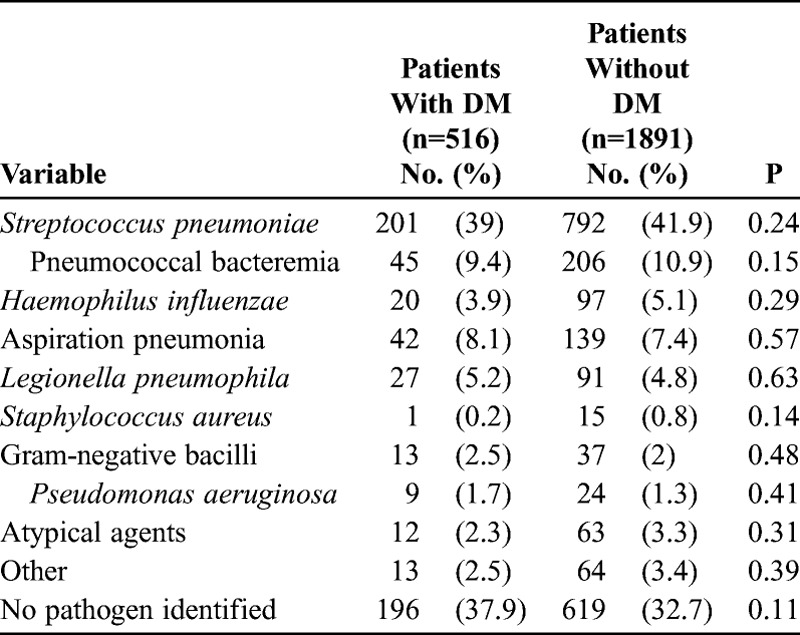
The rates of pneumococcal bacteremia were similar in the 2 groups. Other causative pathogens identified in blood cultures in patients with DM were Pseudomonas aeruginosa (3 cases), Escherichia coli (2 cases), H. influenzae (2 cases), and Staphylococcus aureus, Streptococcus pyogenes, and Klebsiella pneumoniae (1 case each).
Clinical Outcomes
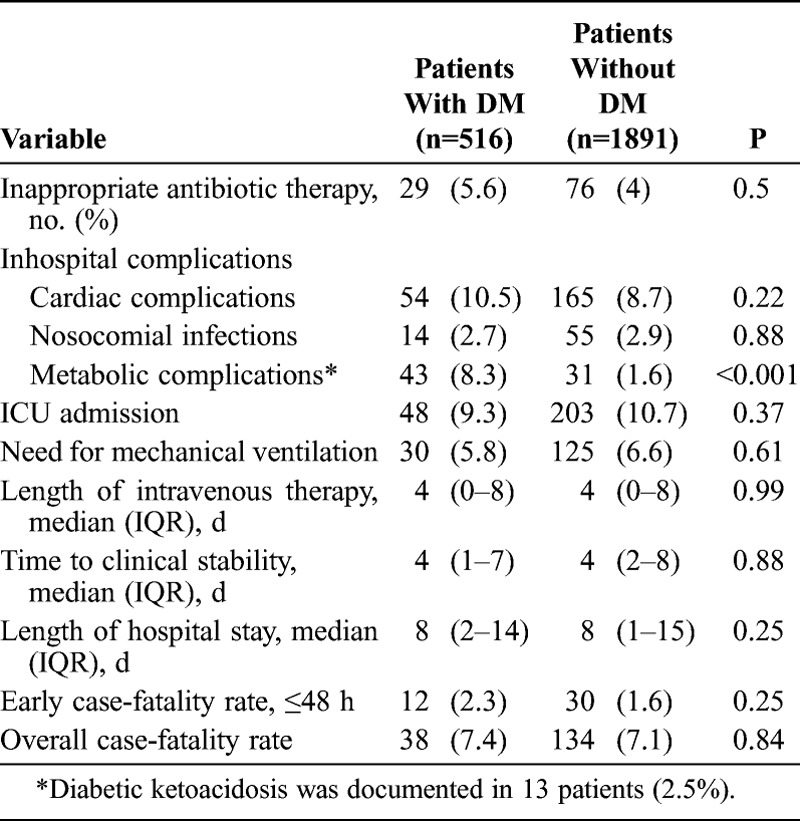
The susceptibility test for pathogen isolates indicated that most patients had received adequate initial empirical antibiotic therapy (Table 3). Significantly, patients with DM were more likely to have metabolic disorders during hospitalization, especially hyperglycemia (5.8%). Diabetic ketoacidosis was documented in 13 patients (2.5%). There were no differences between the groups in terms of intensive care unit (ICU) admission rates, need for mechanical ventilation, time to clinical stability, or length of hospital stay. Early case-fatality rates and overall case-fatality rates were also similar.
TABLE 3.
Antibiotic Therapy and Pneumonia Outcome by Study Group
Risk Factors for Case-Fatality Rates Among Patients With DM
We compared the demographic and clinical features of DM patients who died with those of DM patients who survived (Table 4). Patients who died were older and more often had chronic heart disease, chronic renal disease, dementia, multilobar pneumonia, bacteremia, and septic shock at hospital admission than patients who survived. They were also more likely to be classified into high-risk PSI classes, and more frequently required ICU admission and mechanical ventilation. Pneumonia due to gram-negative bacilli and aspiration pneumonia were significantly more common in DM patients who died compared with those who survived.
TABLE 4.
Factors Associated With Mortality in Patients With DM and Pneumonia: Univariate Analysis
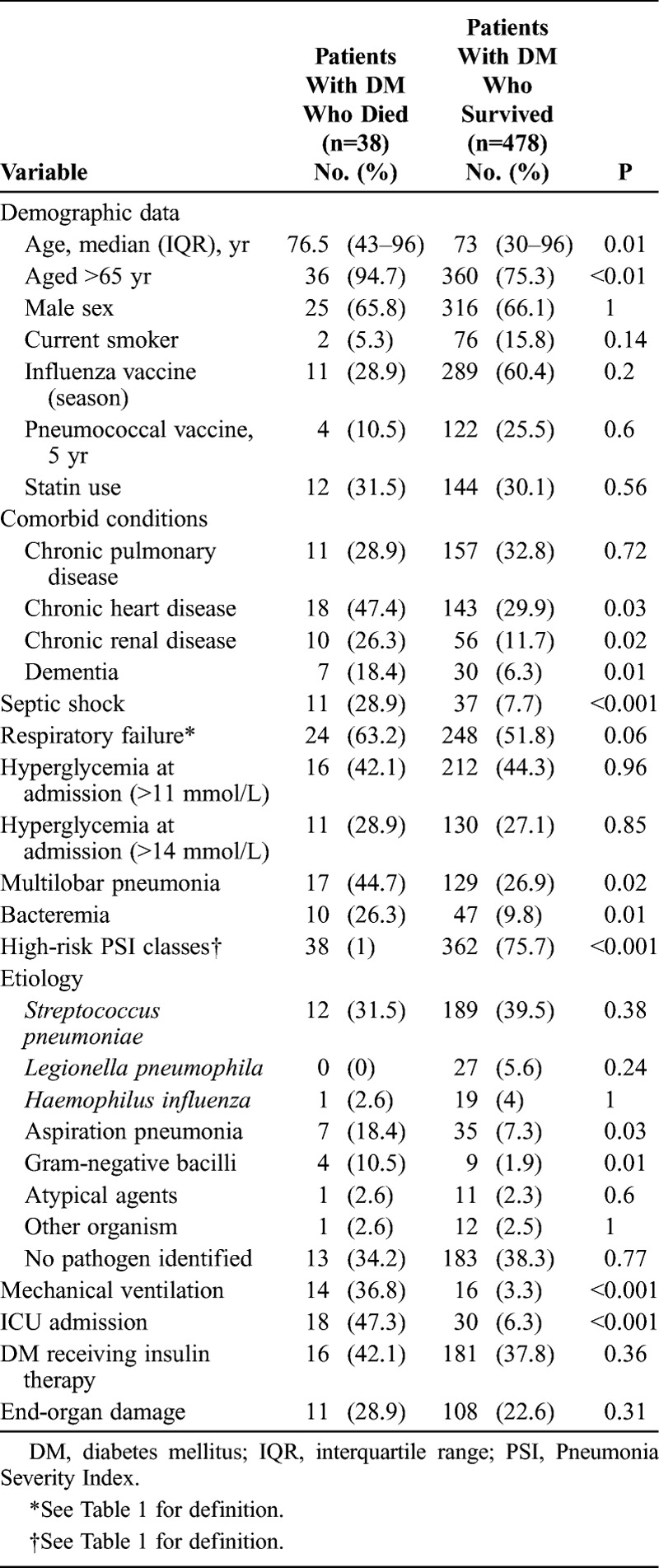
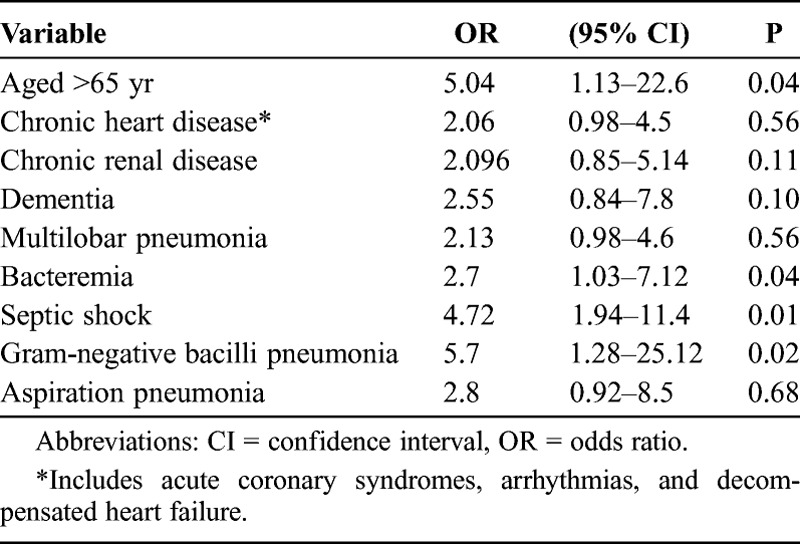
The results of the multivariate logistic regression analysis for factors potentially associated with overall case-fatality rates in patients with DM are summarized in Table 5. After adjustment, advanced age, bacteremia, septic shock at admission, and gram-negative pneumonia were found to be independent risk factors for case-fatality rates.
TABLE 5.
Factors Associated With Mortality in Patients With DM and Pneumonia: Multivariate Analysis
Impact of Statins and Other Cardiovascular Drugs on CAP Outcomes
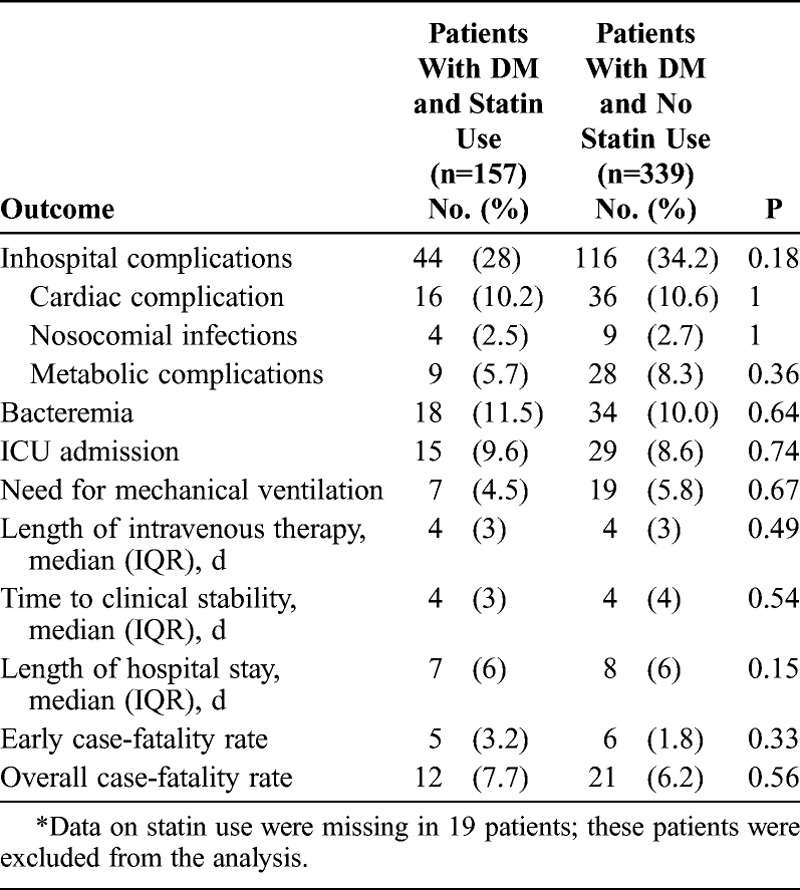
We compared the outcomes of DM patients according to whether or not they received statins (Table 6). No differences were found between these groups. The same analysis was then repeated in the subset of patients receiving insulin therapy and in relation to end-organ damage, and again revealed no differences between the groups. Likewise, the use of other cardiovascular drugs (angiotensin-converting-enzyme inhibitor, acetylsalicylic acid, and beta-blockers) was not associated with better outcomes in patients with CAP and DM.
TABLE 6.
Outcomes of Patients With DM and Pneumonia by Statin Use∗
Patients With DM Who Received Insulin Therapy
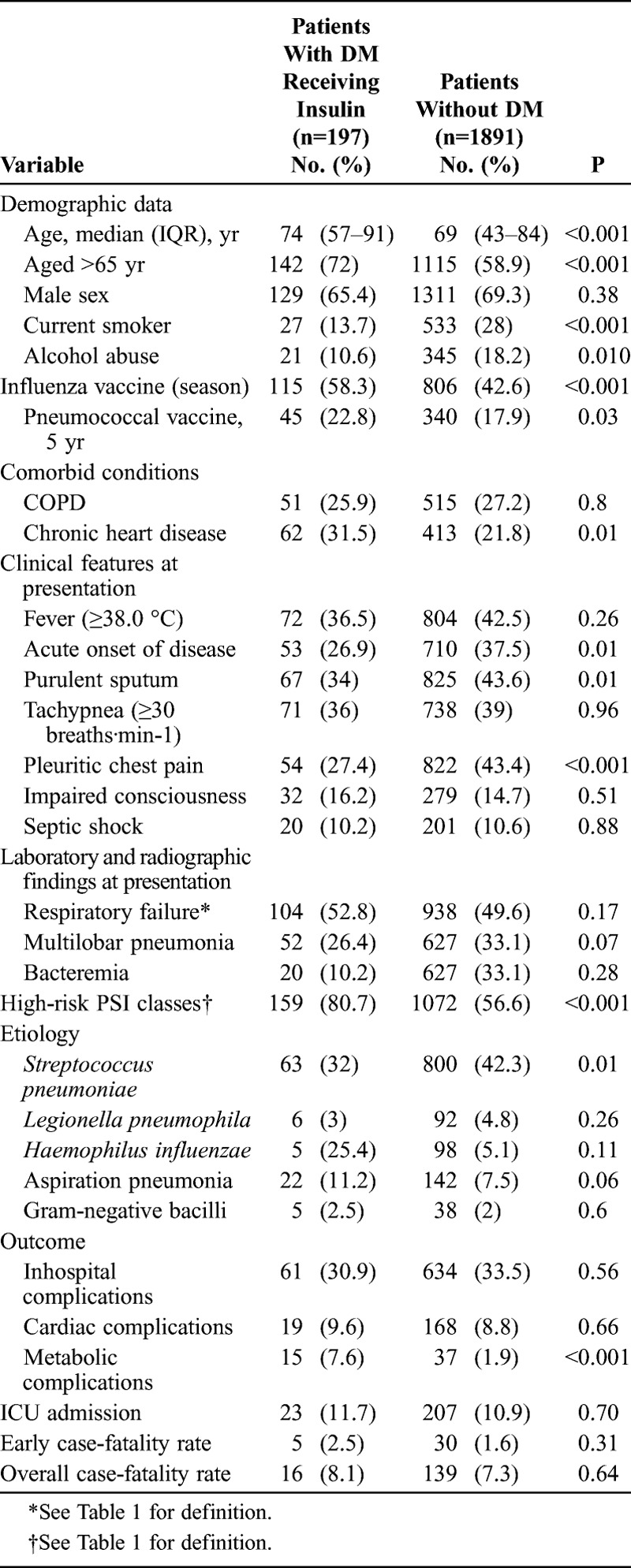
In a further analysis, 197 DM patients who were receiving insulin therapy were compared with patients without DM (Table 7). DM patients on insulin therapy were more often older and they were more likely to have received influenza and pneumococcal vaccination than patients without DM. Chronic heart disease was also more common among these patients, and they were more frequently classified into higher-risk PSI groups at admission. Conversely, patients with DM who were receiving insulin therapy were less likely to present acute onset of disease, purulent sputum, and pleuritic chest pain than patients without DM. Although S. pneumoniae was the most common etiology in both groups, the rate of CAP caused by S. pneumoniae was lower among patients with DM who received insulin therapy. Regarding outcomes, these patients more often presented metabolic complications than did the remaining patients, but there was no significant difference between the groups in terms of the early and overall case-fatality rates.
TABLE 7.
Characteristics of Pneumonia in Patients With DM Who Received Insulin Therapy Compared With Patients Without DM
Patients With End-Organ Damage Related to DM
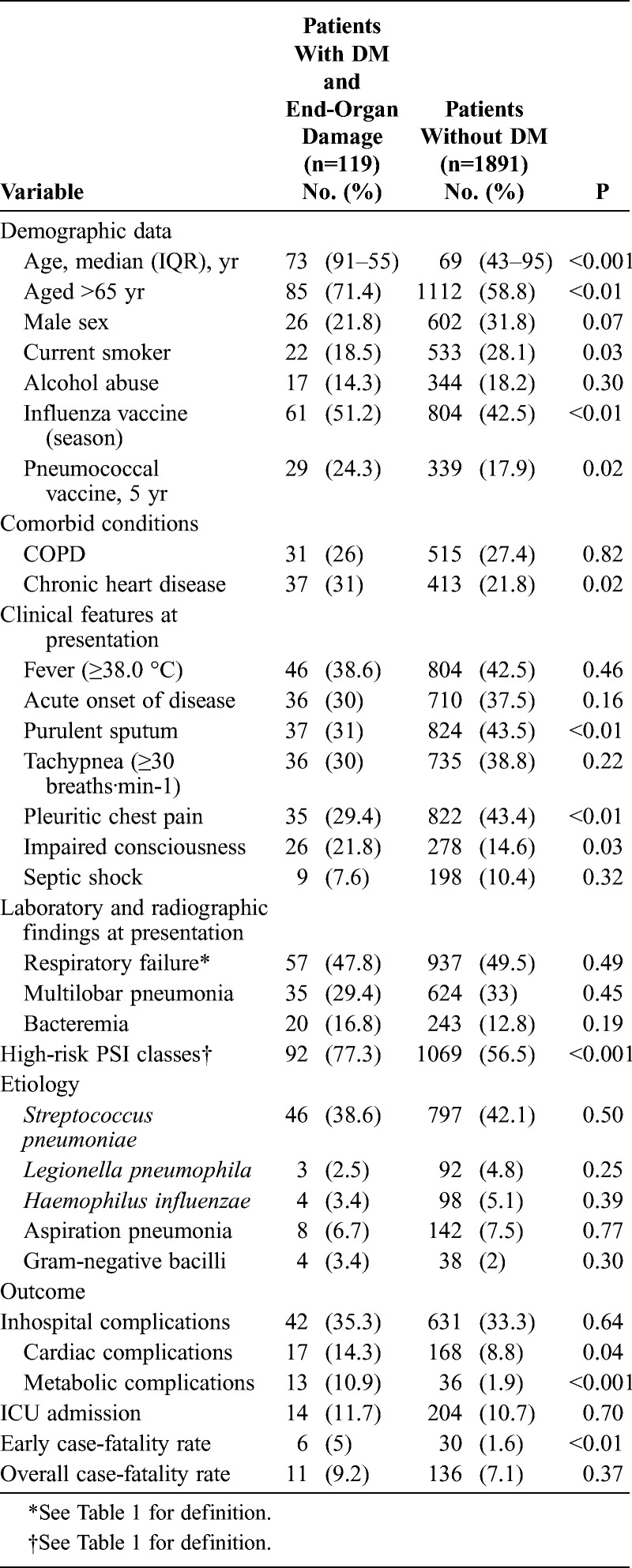
The 119 patients with end-organ damage related to DM were then compared with nondiabetic patients (Table 8). Patients with end-organ damage related to DM were older, more likely to have received influenza and pneumococcal vaccination, and more often had chronic heart disease than patients without DM. They were also more frequently classified into higher-risk PSI groups. Regarding clinical features, purulent sputum and chest pain were less common among patients with end-organ damage related to DM, but conversely they were more likely to present impaired consciousness at admission than patients without DM. No differences in etiology were documented between the groups. Patients with end-organ damage related to DM had poor outcomes, specifically, more cardiac and metabolic complications and a higher early case-fatality rate.
TABLE 8.
Characteristics of Pneumonia in Patients With DM and End-Organ Damage Compared With Patients Without DM
DISCUSSION
The current prospective study of a large cohort of patients offers a detailed evaluation of epidemiology, etiology, clinical features, and pneumonia outcomes in patients with DM. The main findings were that 1) patients with DM had different clinical features and more severe pneumonia at admission compared to nondiabetic patients; 2) S. pneumoniae was the most frequent causative organism of pneumonia in both groups; 3) patients with DM were more likely to have acute metabolic disorders during hospitalization than were nondiabetic patients; 4) no significant differences in case-fatality rates were found between the groups; 5) independent risk factors for mortality in patients with DM were advanced age, bacteremia, septic shock at admission, and gram-negative pneumonia; 6) the use of statins or other cardiovascular drugs was not associated with better outcomes in patients with DM and CAP; 7) the subgroup of patients with end-organ damage related to DM had more acute inhospital cardiac and metabolic complications and a higher early case-fatality rate than did patients without DM.
Patients with DM are at high risk of hospitalization due to CAP.25 Moreover, the rate of DM among hospitalized patients with pneumonia is high, ranging between 16% and 35%.4,11 In the present study, DM was present in 21.4% of patients admitted with CAP. Interestingly, we found that patients with DM did not exhibit some of the expected clinical features during the pneumonia episode. Previous studies dealing with diabetes and pneumonia have not reported information on the clinical presentation of CAP. However, physicians should be aware that the classical clinical triad of bacterial pneumonia with cough, purulent sputum, and pleuritic chest pain is less common in patients with DM than in other patients. This lower rate of cough and expectoration could be related to the disturbances in pulmonary host defense that are associated with DM, leading to decreased pulmonary inflammatory function.7,16,27 The low rate of pleuritic chest pain is probably associated with the less common occurrence of pleural effusion. However, it is important to note that pleuritic pain is the most characteristic clinical consequence of the presence of inflammatory fluid in the pleural space, even in the absence of pleural effusion on the chest radiograph.10 In this context, the finding that patients with DM were less likely to report pleuritic pain than other patients may also reflect a poor inflammatory response in these patients.
Some studies have shown that patients with DM have a higher risk of infection by S. pneumoniae23 and pneumococcal bacteremia, although others have not replicated this finding.11,26,28 In the current study, S. pneumoniae was the most frequent causative organism of pneumonia in both groups. It should be noted that patients with DM were more likely to have previously received pneumococcal vaccination. Our findings show that patients with DM are not at risk of pneumonia caused by multidrug-resistant microorganisms, so empirical antibiotic treatment for CAP in this population should be based on CAP guidelines.29
Our patients with DM had more inhospital complications than patients without DM. Notably, patients with end-organ damage related to DM presented more cardiac complications during hospitalization than did nondiabetic patients. Previous studies have found that cardiovascular events are present in a significant number of patients with CAP.32–36 However, information regarding which patients have a higher risk of cardiac complications is scarce, although Perry et al35 did relate DM to the diagnosis of heart failure in the context of pneumonia. Clinicians should take into account that the subset of patients with end-organ damage related to DM is at high risk of complications during their hospitalization for pneumonia. The optimal strategies to minimize the morbidity and mortality associated with cardiovascular events during pneumonia care should therefore be delineated.
In contrast to previous studies,11,26 we found that patients with DM had similar early and overall case-fatality rates to those of nondiabetic patients. However, the early case-fatality rate was higher among patients with end-organ damage related to DM. These patients frequently have certain characteristics that have previously been related to poor outcomes, such as advanced age, high rates of impaired consciousness at admission, or chronic kidney disease.14,19 The independent risk factors for mortality in our patients with DM and pneumonia are similar to those reported in previous studies involving patients with CAP. Indeed, advanced age, bacteremia, septic shock at admission, and gram-negative pneumonia have all been related to poor prognosis in previous investigations.12,14,17 Interestingly, a 2011 study documented that antibiotic administration later than 8 hours after triage in the emergency department was associated with increased inhospital mortality among patients with DM and CAP.3 Similarly, hyperglycemia at admission predicted increased pneumonia-related mortality in another study.25 Another study38 documented that the mechanism of higher risk of death within the first year after CAP in patients with DM is not due to an altered immune response, at least as measured by a broad panel of circulating and cell surface markers, but may be due to worsening of preexisting cardiovascular and kidney disease.
The use of pneumococcal vaccine may help to prevent bacteremic pneumococcal pneumonia,18,22 and thus it could conceivably be useful to lower the fatality rate in CAP. In this regard, some studies have found that pneumococcal polysaccharide vaccine is effective in preventing hospitalizations for pneumonia8 and reduces the rates of ICU admission and inhospital mortality in immunosuppressed and nonimmunosuppressed patients with CAP or invasive pneumococcal disease.15,21–33 However, there is little evidence of vaccine protection for pneumonia.30
Finally, we found no evidence to suggest that statins improve the outcomes of patients with DM and pneumonia. It has previously been suggested that statins may improve the prognosis of CAP because of the immunomodulatory, antioxidative, and anticoagulant effects of these drugs. However, some studies have related the benefits of statins to a “healthy user effect.” To explore this issue, some authors6 have studied the effect of prior use of several classes of cardiovascular drugs on outcomes in CAP. In the current study, there was no association between the use of any cardiovascular drug and better outcomes.
In conclusion, CAP in patients with DM has distinct clinical characteristics compared to those found in nondiabetic patients. We found no significant differences between the DM and non-DM groups as regards the causative pathogen of pneumonia or bacteremia rates. Acute metabolic complications were more frequent in patients with DM, and patients with end-organ damage related to DM were more likely to have cardiac events during their hospitalization for CAP. Overall, patients with DM had similar early and overall case-fatality rates to those of nondiabetic patients. Independent factors for mortality in patients with DM were advanced age, bacteremia, septic shock at admission, and gram-negative pneumonia. The subset of patients with end-organ damage constitutes the most fragile population, and had higher early mortality than the overall population. Efforts should be made to improve the management of CAP among patients with end-organ damage related to DM.
Footnotes
Abbreviations: CAP = community-acquired pneumonia, DM = diabetes mellitus, EIA = enzyme immunoassay, ICU = intensive care unit, IF = immunofluorescence, PSI = Pneumonia Severity Index
Financial support: This study was supported by the Ministerio de Ciencia e Innovación, Instituto de Salud Carlos III and co-financed by the European Regional Development Fund “A way to achieve Europe” ERDF, Spanish Network for Research in Infectious Diseases (REIPI RD06/0008). Dr. Garcia-Vidal is the recipient of a Juan de la Cierva research grant from the Instituto de Salud Carlos III, Madrid, Spain. Dr Viasus is the recipient of a research grant from the Institut d’Investigació Biomèdica de Bellvitge (IDIBELL).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012; 35 (Suppl 1): S64–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2012; 35 (Suppl 1): S11–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bader MS, Abouchehade KA, Yi Y, Haroon B, Bishop LD, Hawboldt J. Antibiotic administration longer than eight hours after triage and mortality of community-acquired pneumonia in patients with diabetes mellitus. Eur J Clin Microbiol Infect Dis. 2011; 30: 881–886. [DOI] [PubMed] [Google Scholar]
- 4.Benfield T, Jensen JS, Nordestgaard G. Influence of diabetes and hyperglycaemia on infectious disease hospitalization and outcomes. Diabetologia. 2007; 50: 549–554. [DOI] [PubMed] [Google Scholar]
- 5.Carratala J, Garcia-Vidal C. Update on Legionella. Curr Opin Infect Dis. 2010; 23: 152–157. [DOI] [PubMed] [Google Scholar]
- 6.Chalmers JD, Singanayagam A, Murray MP, Hill AT. Prior statin use is associated with improved outcomes in community-acquired pneumonia. Am J Med. 2008; 121: 1002–1007. [DOI] [PubMed] [Google Scholar]
- 7.Delamaire M, Maugendre D, Moreno M, Le goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997; 14: 29–34. [DOI] [PubMed] [Google Scholar]
- 8.Dominguez A, Izquierdo C, Salleras L, Ruiz L, Sousa D, Bayas JM, Nebot M, Varona W, Celorrio JM, Carratala J; for the Working Group for the Study of Prevention of CAP in the Elderly. Effectiveness of the pneumococcal polysaccharide vaccine in preventing pneumonia in the elderly. Eur Respir J. 2010; 36: 608–614. [DOI] [PubMed] [Google Scholar]
- 9.Emerging Risk Factors Collaboration, Seshasai SR, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, Whincup PH, Mukamal KJ, Gillum RF, Holme I, Njølstad I, Fletcher A, Nilsson P, Lewington S, Collins R, Gudnason V, Thompson SG, Sattar N, Selvin E, Hu FB, Danesh J. Diabetes mellitus, fasting glucose, and risk of cause-specific death N Engl J Med. 2011; 364: 1281. [Google Scholar]
- 10.Falguera M, Carratala J, Bielsa S, Garcia-Vidal C, Ruiz-Gonzalez A, Chica I, Gudiol F, Porcel JM. Predictive factors, microbiology and outcome of patients with parapneumonic effusion. Eur Respir J. 2011; 38: 1173–1179. [DOI] [PubMed] [Google Scholar]
- 11.Falguera M, Pifarre R, Martin A, Sheikh A, Moreno A. Etiology and outcome of community-acquired pneumonia in patients with diabetes mellitus. Chest. 2005; 128: 3233–3239. [DOI] [PubMed] [Google Scholar]
- 12.Fernandez-Sabe N, Carratala J, Roson B, Dorca J, Verdaguer R, Manresa F, Gudiol F. Community-acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes. Medicine (Baltimore). 2003; 82: 159–169. [DOI] [PubMed] [Google Scholar]
- 13.Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997; 336: 243–250. [DOI] [PubMed] [Google Scholar]
- 14.Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, Kapoor WN. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996; 275: 134–141. [PubMed] [Google Scholar]
- 15.Fisman DN, Abrutyn E, Spaude KA, Kim A, Kirchner C, Daley J. Prior pneumococcal vaccination is associated with reduced death, complications, and length of stay among hospitalized adults with community-acquired pneumonia. Clin Infect Dis. 2006; 42: 1093–1101. [DOI] [PubMed] [Google Scholar]
- 16.Gallacher SJ, Thomson G, Fraser WD, Fisher BM, Gemmell CG, MacCuish AC. Neutrophil bactericidal function in diabetes mellitus: evidence for association with blood glucose control. Diabet Med. 1995; 12: 916–920. [DOI] [PubMed] [Google Scholar]
- 17.Garcia-Vidal C, Ardanuy C, Tubau F, Viasus D, Dorca J, Linares J, Gudiol F, Carratala J. Pneumococcal pneumonia presenting with septic shock: host- and pathogen-related factors and outcomes. Thorax. 2010; 65: 77–81. [DOI] [PubMed] [Google Scholar]
- 18.Garcia-Vidal C, Carratala J, Fernandez-Sabe N, Dorca J, Verdaguer R, Manresa F, Gudiol F. Aetiology of, and risk factors for, recurrent community-acquired pneumonia. Clin Microbiol Infect. 2009; 15: 1033–1038. [DOI] [PubMed] [Google Scholar]
- 19.Garcia-Vidal C, Fernandez-Sabe N, Carratala J, Diaz V, Verdaguer R, Dorca J, Manresa F, Gudiol F. Early mortality in patients with community-acquired pneumonia: causes and risk factors. Eur Respir J. 2008; 32: 733–739. [DOI] [PubMed] [Google Scholar]
- 20.Halm EA, Fine MJ, Marrie TJ, Coley CM, Kapoor WN, Obrosky DS, Singer DE. Time to clinical stability in patients hospitalized with community-acquired pneumonia. Implications for practice guidelines. JAMA. 1998; 279: 1452–1457. [DOI] [PubMed] [Google Scholar]
- 21.Imaz A, Falco V, Penaranda M, Jordano Q, Martinez X, Nadal C, Curran A, Planes AM, Dalmau D, Ribera E, Riera M, Ruiz de Gopegui E, Pahissa A. Impact of prior pneumococcal vaccination on clinical outcomes in HIV-infected adult patients hospitalized with invasive pneumococcal disease. HIV Med. 2009; 10: 356–363. [DOI] [PubMed] [Google Scholar]
- 22.Johnstone J, Marrie TJ, Eurich DT, Majumdar SR. Effect of pneumococcal vaccination in hospitalized adults with community-acquired pneumonia. Arch Intern Med. 2007; 167: 1938–1943. [DOI] [PubMed] [Google Scholar]
- 23.Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999; 341: 1906–1912. [DOI] [PubMed] [Google Scholar]
- 24.Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crisis in adult patients with diabetes: a consensus statement from the American Diabetes Association. Diabetes Care. 2006; 29: 2739–2748. [DOI] [PubMed] [Google Scholar]
- 25.Kornum J, Thomsen R, Riis A, Lervang HH, Schonheyder HC, Sorensen HT. Diabetes, glycemic control, and risk of hospitalization with pneumonia. Diabetes Care. 2008; 8: 1541–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kornum JB, Thomsen RW, Riis A, Lervang HH, Schonheyder HC, Sorensen HT. Type 2 Diabetes and pneumonia outcomes. Diabetes Care. 2007; 30: 2251–2257. [DOI] [PubMed] [Google Scholar]
- 27.Koziel H, Koziel M. Pulmonary complications of diabetes mellitus. Infect Dis Clin North Am. 1995; 9: 65–95. [PubMed] [Google Scholar]
- 28.Lipsky BA, Boyko EJ, Inui TS, Koepsell TD. Risk factors for acquiring pneumococcal infections. Arch Intern Med. 1986; 146: 2179–2185. [PubMed] [Google Scholar]
- 29.Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Jr, Musher DM, Niederman MS, Torres A, Whitney CG. Infectious Disease Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007; 44 (Suppl 2): S27–S72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moberley SA, Holden J, Tatham DP, Andrews RM. Vaccines for preventing pneumococcal infection in adults. Cochrane Database Syst Rev. 2008; (1): CD000422. [DOI] [PubMed] [Google Scholar]
- 31.Muchova J, Liptakova A, Orszaghova Z, Garaiova I, Tison P, Carsky J, Durackova Z. Antioxidant systems in polymorphonuclear leucocytes of type 2 diabetes mellitus. Diabet Med. 1999; 16: 74–78. [DOI] [PubMed] [Google Scholar]
- 32.Musher D, Rueda A, Kaka A, Mapara S. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis. 2007; 45: 158–165. [DOI] [PubMed] [Google Scholar]
- 33.Mykietiuk A, Carratala J, Dominguez A, Manzur A, Fernandez-Sabe N, Dorca J, Tubau F, Manresa F, Gudiol F. Effect of prior pneumococcal vaccination on clinical outcome of hospitalized adults with community-acquired pneumococcal pneumonia. Eur J Clin Microbiol Infect Dis. 2006; 25: 457–462. [DOI] [PubMed] [Google Scholar]
- 34.Novack V, Macfadyen J, Malhotra A, Almog Y, Glynn RJ, Ridker PM. The effect of rosuvastatin on incident pneumonia: results from the JUPITER trial. CMAJ. 2012; 184: E367–E372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perry T, Pugh M, Waterer G, Nakashima B, Orihuela C, Copeland L, Restrepo M, Anzueto A, Mortensen E. Incidence of cardiovascular events after hospital admission for pneumonia. Am J Med. 2011; 124: 244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramirez J, Aliberti S, Mirsaeidi M, Peyrani P, Filardo G, Amir A, Moffett B, Gordon J, Blasi F, Bordon J. Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clin Infect Dis. 2008; 15: 182–187. [DOI] [PubMed] [Google Scholar]
- 37.Viasus D, Garcia-Vidal C, Gudiol F, Carratala J. Statins for community-acquired pneumonia: current state of the science. Eur J Clin Microbiol Infect Dis. 2010; 29: 143–152. [DOI] [PubMed] [Google Scholar]
- 38.Yende S, van der Poll T, Lee M, Huang DT, Newman AB, Kong L, Kellum JA, Harris TB, Bauer D, Satterfield S, Angus DC; GenIMS and Health ABC study. The influence of pre-existing diabetes mellitus on the host immune response and outcome of pneumonia: analysis of two multicentre cohort studies. Thorax. 2010; 65: 870–877. [DOI] [PMC free article] [PubMed] [Google Scholar]


