Abstract
AIM
To investigate suicidality and attention-deficit/hyperactivity disorder (ADHD), this paper aims to systematically review the literature as an extension of previous reviews.
METHODS
We searched five databases (Ovid MEDLINE, Psychinfo, PubMed, Scopus, Web of Science) with two categories of search terms: (1) suicide; suicidal; suicide behavior; suicide attempt; suicidal thought; and (2) ADHD.
RESULTS
The search resulted 26 articles. There is a positive association between ADHD and suicidality in both sexes and in all age groups. Comorbid disorders mediate between suicidality and ADHD.
CONCLUSION
Recognizing ADHD, comorbid conditions and suicidality is important in prevention.
Keywords: Attention-deficit/hyperactivity disorder, Suicide, Systematic review
Core tip: This review of the last four years strengthens previous findings that there is a positive association between attention-deficit/hyperactivity disorder (ADHD) and suicidality in both sexes and in all age groups. Suicidality should screen in patients with ADHD. Comorbid disorders mediate between suicidality and ADHD. Recognizing ADHD and comorbid conditions can be important in suicide prevention as well.
INTRODUCTION
Suicide prevention is a public health issue all over the world[1]. Recently, several studies have focused on attention-deficit hyperactivity disorder (ADHD) as a possible psychiatric disorder that may serve as a suicide risk factor as well[2-5]. One of the theoretical backgrounds of it is the construct of impulsivity, which is a well-know personality trait. Impulsivity is a core symptom of ADHD[6,7], moreover it is known, that it correlates to suicidal behavior[8]. Another theoretical background behind the possible association between ADHD and suicide is, that two-thirds of ADHD cases have at least one comorbid psychiatric diagnosis, which most often is conduct disorder, substance use or major depressive episode[9-11]. These comorbid disorders are well-known risk factors of suicide[12-15]. As ADHD is one of the most prevalent (2%-12%) psychiatric disorders among children and adolescents and in 40%-60% of the cases, it continues into adulthood[16,17], all additional knowledge on the possible association between ADHD and suicidality has high clinical importance and can add to suicide prevention.
The growing body of publications on ADHD and suicidality has already resulted in five review or summary papers on this topic. First, James et al[18] searched two electronic databases (MEDLINE, Psychlit) for the period from 1966 to 2003. In their review, they included psychological autopsy studies of teenage and young adult suicides and long-term follow-up studies of ADHD children. They found a positive association between ADHD and completed suicides in males, concluding that ADHD could increase the risk for suicide through comorbid conditions such as conduct disorder and depression. Second, Impey et al[19] performed a search for the period up to January 2011 using three main databases (MEDLINE, EMBASE and PSYCHINFO). They concluded from their review that most suicidal study groups showed a higher rate of ADHD than the controls: At least double the rate for suicidal ideation and around 1.5-2.0 times for suicide attempts and completion. The authors emphasized that comorbidity had a large influence, especially in the cases of delinquency and substance misuse. Third, Furczyk et al[20] published a selective review on the most important currently known associations between ADHD and suicidality. They concluded, similar to the previous reviews[18,19], that there is substantial evidence supporting an association between ADHD and increased suicide risk, and that it is at least partially mediated by comorbidities. They highlight the importance of raising the awareness of health professionals of the risk of suicide in ADHD patients, but further research on the long-term outcomes of the treatment of ADHD patients with a risk of suicide is needed. The selective review paper of Nigg[21] had a wider focus: He overviewed the current knowledge on the health-related impairments of ADHD, including smoking, drug abuse, accidental injury, sleep, obesity, hypertension and diabetes, as well as suicidal behavior. On the topic of ADHD and suicide, the author concluded that ADHD is associated with an elevated risk of suicide attempts (particularly in girls) and completed suicide (particularly in boys), and this risk is mediated by comorbid disorders, which may vary with gender: They include conduct and emotional problems in males and depression in females. Finally, we have to mention Renaud et al[22] summary paper: Based on some selected important research in the field, the authors concluded that there is not a direct link between ADHD and suicide, however, ADHD’s constructs of impulsivity and aggression are related to the development of conduct and oppositional defiant disorders, which can lead to deviancy and drug abuse; all of these comorbid conditions increase the risk of suicide.
Knowing of the growing interest in this topic over the last couple of years, we found it useful to conduct an up-to-date systematic review, which can provide important extensions. The search of James et al[18] was conducted more than one decade ago, and even Impey et al[19] completed their search in January, 2011. The most recently published reviews were not systematic[20-22]. Additionally, all of the reviews have mainly been limited to males[18,19]. Moreover knowing more about the methodology of the studies can lead to a better understanding of the prevalence data. Considering all of this, the current systematic review aims to present an overview on suicidality and ADHD as an extension of the previous ones, not only in the time period of the search, but also by focusing on the following topics: (1) Is ADHD more common in people who are suicidal? (2) Is suicide more prevalent in people with ADHD? and (3) Which other identifiable risk factors can be associated with suicide in ADHD?
Additionally, to be able to compare the included studies, we investigated what kinds of assessments are used for measuring ADHD, suicidality and comorbid conditions.
MATERIALS AND METHODS
Selection of publications
A systematic literature search was conducted in the following five computerized literature databases on January 27, 2015: Ovid MEDLINE, Psychinfo, PubMed, Scopus, Web of Science from 2011 to 2015. Search terms from two categories were used: (1) suicide; suicidal; suicide behavior; suicide attempt; suicidal thought; and (2) ADHD; attention deficit hyperactivity disorder. Search terms within both categories were separated by the Boolean operator OR, and the categories were separated by the operator AND. Using prespecified inclusion and exclusion criteria, we screened the titles and/or abstracts. The relevant full texts of papers that passed the first search were read, and the ones that met the inclusion criteria were collected. The reference lists of the retrieved papers were screened, and papers that possibly met the inclusion criteria were retrieved and studied. The inclusion criteria were: Peer-reviewed journals; publications written in English or Hungarian. The exclusion criterion was the lack of any empirical data. It was not in the focus of our study to examine suicidal behavior, as a safety concern about ADHD drug treatment. We excluded those studies, which aim was to examine pharmacological treatment (e.g., atomoxetine) induced suicide in patients with ADHD, e.g., Capuano et al[23], who present a series of cases of Italian children who experienced suicidal ideation during ADHD pharmacological therapy with atomoxetine.
RESULTS
Included studies
The search strategy resulted in a total of 278 articles (excluding duplicates), of which 26 were included in the systematic review after the screening process (Figure 1, Tables 1-3).
Figure 1.
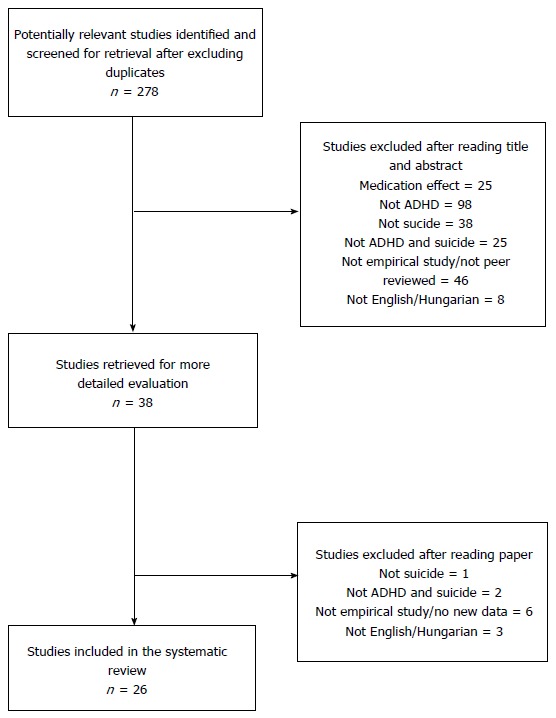
QUORUM flow chart detailing results of literature search. ADHD: Attention-deficit/hyperactivity disorder.
Table 1.
Included relevant articles examining attention-deficit/hyperactivity disorder and suicidality from January 2011 to January 2015: Attention-deficit/hyperactivity disorder in suicidal patients
| ADHD in suicidal patients | |||||||
| Ref. | Country | Study design | Sample | Population at onset | Population’s age at onset | Measures for ADHD, comorbid conditions and suicidality | Main findings |
| Ben-Yehuda et al[24] | Israel | Cross-sectional | Clinical sample | The survey involved all minors (age < 18) (n = 266) who were referred to a psychiatric emergency department due to a suicide attempt or suicidal ideation during a 3-yr period (2005-2007) | Children: Age range: ≤ 12 yr Adolescents: Age range: > 12 yr | The diagnosis was made by the examiner in the emergency department: diagnoses were coded using the ICD-10 | The distribution of psychiatric diagnoses differed significantly in the two age groups ADHD was significantly more prevalent among suicidal children, while mood disorders were more prevalent among suicidal adolescents The second most prevalent diagnosis among suicidal children was ADHD (25.6%) (following adjustment disorder/38.5%/and followed by conduct disorders/23.1%) In adolescents ADHD was not among the most common diagnoses: it was found in only 5.7% in the adolescent group |
| Evren et al[25] | Turkey | Cross-sectional | Community sample | A representative sample of 10th grade students: n = 4938 (male ratio: 52.7%) | Mean age: 15.58 yr (SD = 2.85) | PSTA | Those with a lifetime suicidal thoughts had a higher mean ADHD symptom score than those without. Suicidal thoughts predicted the symptoms of ADHD |
| Soole et al[26] | Australia | Cross-sectional | Community sample | 469 deaths by external causes were recorded in the Queensland CDR for children and adolescents aged 10-17 between 2004 and 2012 | Between 2004 and 2012, 149 suicides were recorded: 34 of children aged 10-14 yr and 115 of adolescents aged 15-17 yr | Causes of death were categorized using the ICD-10 | Mental and behavioral disorders were observed in 50% of children and 57.3% of adolescents who died by suicide. Disorders usually diagnosed in infancy, childhood, and adolescence, such as ADHD, were significantly more frequent in children than in adolescents. Mood disorders, such as depression, were significantly more common in adolescents compared with children |
CDR: Child Death Register; ADHD: Attention-deficit/hyperactivity disorder; PSTA: Psychological screening test for adolescents.
Table 3.
Included relevant articles examining attention-deficit/hyperactivity disorder and suicidality from January 2011 to January 2015: Suicidality in patients with psychiatric disorders who have attention-deficit/hyperactivity disorder comorbidity
| Suicidality in patients with psychiatric disorders who have ADHD comorbidity | |||||||
| Ref. | Country | Study design | Sample | Population at onset | Population’s age at onset | Measures for ADHD, comorbid conditions and suicidality | Main findings |
| Bácskai et al[41] | Hungary | Cross-sectional | Clinical sample | 198 patients with drug dependence (male ratio: 76%) Drug dependent patients without ADHD: n = 154 Drug dependent patients with ADHD: n = 44 | Age range: 18-40 yr Mean age of the whole sample: 27 yr (SD = 6.31) | ASRS, EuroADAD, BDI | Drug dependent patients with ADHD showed a significantly higher proportion of suicidal ideation, suicidal attempts and self-injuries associated with suicidal attempts than drug dependent patients without ADHD |
| Berkol et al[42] | Turkey | Cross-sectional | Clinical sample | Patients with BD type I and II Adult BP with ADHD: n = 23 Adult BP without ADHD: n = 32 | BP adults with ADHD: Mean age: 35.1 yr (SD = 10.7) BP adults without ADHD: Mean age: 41.3 yr (SD = 13.0) | ADHD scale Mood disorder modul of SCID-I-CV | In the BP with ADHD group, the rate of suicide attempts (47.8%) was significantly higher than in the BP without ADHD group (21.9%) |
| Donev et al[43] | Germany | Cross-sectional | Clinical sample | Patients with schizophrenia according to ICD-10 criteria: n = 27 (14 male) Patients with schizophrenia and no ADHD: n = 15 Patients with schizophrenia and ADHD: n = 12 | Age range: 18-44 yr Mean age: 25.7 yr (SD = 7.6) | ADHD-HKS Questionnaire | Among patients with both schizophrenia and ADHD there were significantly higher number of suicide attempts than among those with schizophrenia without ADHD |
| Huntley et al[31] | United Kingdom | Cross-sectional | Clinical sample | Participants from two in-patient alcohol and drug detoxification units: n = 226 (male ratio: 76.5%) Patient with alcohol/drug intoxication + ADHD: n = 11 Patient with alcohol/drug intoxication without ADHD: n = 183 | Mean age: 39.0 yr (SD = 10.3) | DSM-IV 18-item self-report ADHD screening questionnaires for both current and childhood behavior Impairment questions from the Barkley scales DIVA | Patients with both substance use disorders and ADHD had significantly higher rates of prior suicide attempts than patients with substance use disorder without ADHD |
| Patros et al[44] | United States | Cross-sectional | Community sample | College students: n = 1056 (male ratio: 38.5%) | Age range: 18 yr of age or older; 96.4% aged 18-24 yr | CSS, HDSQ | Higher hyperactive/attention symptoms were associated with increase in suicidal thoughts, suicide attempts, and need for medical attention after suicide attempts, among participants with depressed mood |
| Penney et al[45] | Canada | Cross-sectional | Clinical sample | Clients who presented for treatment at an addictions facility: n = 5990 (male ratio: 63.1%) Clients who reported being hospitalized for attempting suicide in the past year: n = 76 All other clients: n = 5914 | Age range: 11-86 yr Mean age: 32.60 yr (SD = 14.55) | Clients reported whether or not they had been diagnosed by a mental health professional in the last 12 mo and in heir lifetime | Compared to all other clients, clients who attempted suicide in the past year were significantly more likely to have ADHD (9.2% vs 2.5%) |
| Sáez-Francàs et al[46] | Spain | Cross-sectional | Clinical sample | Adult CFS patients: n = 158 CFS patients with adult ADHD: n = 33 (male ratio: 3.0%) CFS patients without adult ADHD (male ratio: 6.4%) | CFS + ADHD: Mean age: 47.55 yr (SD = 7.99) CFS: Mean age: 48.60 yr (SD = 8.88) | CAADID Suicide risk was studied with the Plutchick Risk of Suicide Scale (Plutchik et al, 1989), a 15-item self-report scale with dichotomous responses. Values above the cut-off point of 6 indicate a risk of suicide | CFS patients with adult ADHD had a higher risk of suicide than CFS patients without ADHD |
CFS: Chronic fatigue syndrome; ADHD: Attention-deficit/hyperactivity disorder; ASRS: Adult Self-Report Scale; EuroADAD: European Version of the Adolescent Assessment Dialogue; BDI: Beck Depression Inventory; SCID-I-CV: Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version; DIVA: Diagnostic Interview for ADHD in Adults; CSS: Current Symptoms Scale–Self-Report Form; HDSQ: Hopelessness Depression Symptom Questionnaire-Suicidality Subscale; CAADID: Conners’Adult ADHD Diagnostic Interview for DSM-IV.
The 26 papers were written in 16 countries on four continents. Of the 26 studies, only two had a longitudinal design. Detailed information on the origin, design, sample and instruments of the studies can be found in Tables 1-3.
Is ADHD more common in people who are suicidal?
Table 1 summarizes the three studies on ADHD in suicidal patients[24-26].
Is suicide more prevalent in people with ADHD?
Table 2 includes the 14 studies, which examines suicidality in patients with ADHD[27-40].
Table 2.
Included relevant articles examining attention-deficit/hyperactivity disorder and suicidality from January 2011 to January 2015: Suicidality in patiens with attention-deficit/hyperactivity disorder
| Suicidality in patiens with ADHD | |||||||
| Ref. | Country | Study design | Sample | Population at onset | Population’s age at onset | Measures for ADHD, comorbid conditions and suicidality | Main findings |
| Agosti et al[27] | United States | Cross-sectional | Clinical sample | Current ADHD: 365 adults: With Suicide attempts: n = 59 No suicide attempts: n = 306 | Age range: 18-66 yr | CIDI, ACDS, DIS-IV | Sixteen percentage of participants with current ADHD diagnosis had previous suicide attempt. While ADHD increased the risk of previous suicide attempt only 1.5 fold, having one or more comorbid disorders increased the risk of previous suicide attempt 4 to 12 fold |
| Balazs et al[28] | Hungary | Cross-sectional | Clinical sample | ADHD and subthreshold ADHD children: n = 220 ADHD and subthreshold ADHD adolescents: n = 198 | Children: Age range: 3-11 yr Mean age: 7.67 yr (SD = 2.03) Adolescents: Age range: 12-17 yr Mean age: 14.31 yr (SD = 1.67) | MINI-KID | The relationship between ADHD and suicidality was fully mediated by comorbid psychiatric disorders. In children, symptoms of anxiety disorders mediated this relationship, while in the adolescent group, symptoms of major depressive episode, dysthymia, and substance abuse/dependence were found to be significant mediators |
| Barbaresi et al[29] | United States | Cross-sectional | Community sample | Adults with childhood ADHD: n = 232 Non-ADHD controls: n = 335 | ADHD group: Mean age: 27 yr Non-ADHD group: Mean age: 28.6 yr | MINI | The rate of death from suicide was significantly higher among adults with childhood ADHD compared to non-ADHD adults |
| Cheng et al[30] | Taiwan | Cross-sectional | Community sample | 5405 University students: n = 5405 (male ratio: 64.8%) ADHD symptoms were elevated in 8.6% of the sample: (male ratio: 75.1%) | University students | ASRS, BSRS-5 | Individuals with higher levels of ADHD symptoms were more likely to have higher suicidal ideation |
| Huntley et al[31] | United Kingdom | Cross-sectional | Clinical Sample | Participants from two in-patient alcohol and drug detoxification units: n = 226 (male ratio: 76.5%) Patient with alcohol/drug intoxication + ADHD: n = 11 Patient with alcohol/drug intoxication without ADHD: n = 183 | Mean age: 39.0 yr (SD = 10.3) | DSM-IV 18-item self-report ADHD screening questionnaires for both current and childhood behavior Impairment questions from the Barkley scales DIVA | Patients with both substance use disorders and ADHD had significantly higher rates of prior suicide attempts than patients with substance use disorder without ADHD |
| Hurtig et al[32] | Finland | Longitudinal: 16 yr. First follow up: at ages 7, 8, second follow up at ages 15, 16 | Community sample | ADHD adolescents: n = 104 Non-ADHD adolescents: n = 169 | Adolescents from the same birth cohort | At 8 yr of age: Rutter B2 During the 15-16 yr follow up: SWAN, K-SADS-PL | Adolescents with ADHD had more suicide ideation, acts than adolescents without ADHD. The effect of ADHD on suicidal ideation remained strong after controlling for other variables |
| Kavakci et al[33] | Turkey | Cross-sectional | Community sample | 980 university students (male ratio: 55.9%) ADHD: n = 48 Non-ADHD: n = 932 | Age range: 17-44 yr Mean age: 21.4 yr (SD = 2.3 yr) | ASRS SCID I, SCID II, Adult ADHD Module of MINI Plus | Adolescents with ADHD reported significantly more lifetime suicide attempts than those without ADHD |
| Keresztény et al[34] | Hungary | Cross-sectional | Clinical sample | Children: n = 168 (male ratio: 87.5%) Adolescents: n = 43 (male ratio: 62.8%) | Children: Age range: 3-12 yr Mean age: 8.23 yr (SD = 2.22) Adolescents: Mean age: 14.65 yr (SD = 1.6 yr) boys: 27 (62.8%) | MINI-KID | The most common comorbid diagnoses with ADHD were oppositional defiant disorder, conduct disorder and suicide behavior in both age-groups. The rate of suicide behavior was 17% among children and 58% among adolescents |
| Ljung et al[35] | Sweden | Cross-sectional | Patient and prescribed drug registers and population-based registers | ADHD: n = 51707 (male ratio: 69.8%) Control: n = 258535 | Age range: 3-40 yr | Discharge diagnosis of ADHD | Participants with ADHD had an increased risks of both attempted and completed suicide compared with control participants. This result was the same even after adjusting for comorbid psychiatric conditions. While the highest familial risk was reported among first-degree relatives, lower risk was observed among more genetically distant relatives. The results suggests that shared genetic factors are important for this association |
| Mayes et al[36] | United States | Cross-sectional | Community and clinical sample | 1706 children and adolescents with psychiatric disorders and typical development: ADHD-C: n = 566 (male ratio: 74.6%) ADHD-I: n = 235 (male ratio: 57.4%) Other psychiatric disorders (autism, depression/ anxiety, eating disorder, intellectual disability): n = 719 (male ratio: 67.2%) Typical: n = 186 (male ratio: 43.5%) | Age range: 6-18 yr | All participants had a clinical diagnosis of ADHD made by a licensed PhD psychologist. The clinical diagnosis was based on a comprehensive psychological evaluation including diagnostic inter- views with the parent and child, parent and teacher rating scales, review of educational and medical records, extensive psychological testing PBS | All psychiatric groups had far more suicide behavior than typically developed children. ADHD-C: 20.7% had suicide ideation, 6.0% attempt ADHD-I: 7.3% had suicide ideation, 2.6% attempt |
| Mayes et al[37] | United States | Cross-sectional | Clinical sample | Children and adolescents with ADHD: n = 925 (male ratio: 68.5%) ADHD-C: n = 666 ADHD-I: n = 259 | Age range: 3-16 yr Mean age: 8.8 yr (SD = 2.6) | All participants had a clinical diagnosis of ADHD made by a licensed PhD psychologist. The clinical diagnosis was based on a comprehensive psychological evaluation including diagnostic inter- views with the parent and child, parent and teacher rating scales, review of educational and medical records, extensive psychological testing PBS - suicide ideation and attempt items | For the total sample with ADHD, 15.8% had suicide ideation (sometimes or more) and 5.5% had attempts Ideation and attempts were more than twice as prevalent among participants with ADHD-C than among participants with ADHD-I ADHD-C: 19% had suicide ideation, 7% attempt ADHD-I: 7% had suicide ideation, 3% attempt Those, who had ADHD alone: 6% had suicide ideation and 2% had suicide attempt. Those, who had ADHD + co-occurring sadness and ODD, 46% had ideation and 21% had attempts |
| Park et al[38] | South Korea | Cross-sectional | Community sample | A total of 6081 subjects: Non-ADHD symptom group: n = 6012 ADHD symptom group: n = 69 | Age range: 18-59 yr | K-CIDI Adult ADHD Self-Report Scale | Adult ADHD symptoms are significantly associated with lifetime suicidality. However, the association disappeared after adjusting for other comorbid psychiatric disorders |
| Swanson et al[39] | United States | Longitudinal: 10 yr: First 5 yr follow up and second 10 yr follow-up | Community and clinical sample | ADHD girls: n = 140 Non-ADHD girls: n = 88 | Age range: 6-12 yr at ascertainment Mean age at 5 yr follow-up: 14.2 yr Mean age at 10 yr follow-up: 19.6 yr (range 17-24 yr) | At ascertainment: DISC-IV First follow up: SNAP-IV, Second follow up: SIQ, Barkley Suicide Questionnair, DISC-IV-YA | Women with a childhood diagnosis of ADHD-C, compared with those with ADHD-I and control group, were at higher risk for suicide attempts. Furthermore, women with a persistent ADHD diagnosis were at higher risk than women with a transient diagnosis and the control group |
| Van Eck et al[40] | United States | Cross-sectional | Community sample | Undergraduate psychology students: n = 627 (male ratio: 40%) | Mean age: 20.23 yr (SD = 1.40) | CSS BSI | ADHD indirectly increased suicidal ideation through depression. The moderator factors in the indirect effect of ADHD on suicidal ideation were emotion regulation deficits of accepting negative emotions, emotional awareness, and goal-oriented behavior |
ADHD: Attention-deficit/hyperactivity disorder; CIDI: Composite International Diagnostic Interview; ACDS: Adult ADHD Clinical Diagnostic Scale; DIS-IV: The Diagnostic Interview Schedule for DSM-IV; MINI-KID: Mini-International Neuropsychiatric Interview for children and adolescents; PBS: Pediatric Behavior Scale; MINI: Mini-International Neuropsychiatric Interview; ASRS: Adult Self-Report Scale; BSRS-5: Brief Symptoms Rating Scale; DIVA: Diagnostic Interview for ADHD in Adults; SWAN: Strengths and Weaknesses of ADHD symptoms and Normal Behaviors; SCID-I: Structured Clinical Interview for DSM-IV Axis I Disorders; ODD: Oppositional defiant disorder; K-CIDI: Korean version of Composite International Diagnostic Interview; SNAP-IV: Swanson, Nolan, and Pelham Rating Scale; SIQ: Self-Injury Questionnaire; DISC-IV-YA: Diagnostic Interview Schedule for Children 4th ed., Young Adult version; ADHD-C: ADHD combined type; ADHD-I: ADHD inattentive type, ADHD-HKS Questionnaire.
Which other identifiable risk factors can be associated with suicide in ADHD?
Gender differences in suicidality and ADHD: Examining the gender distribution of ADHD cases among suicidal patients, only one study provided relevant data[24]: 8.6% of suicidal male adolescents had ADHD, and 4.7% of suicidal female adolescents had ADHD.
Focusing on the gender differences in suicidal cases among ADHD patients, in the above-described 12 papers, which examined the prevalence of suicidality among patients with ADHD, three studies focused on gender differences[27,35,37], and one study enrolled only girls[39].
Regarding suicidal ideation, Mayes et al[37] found no differences between boys and girls with ADHD with suicidal ideation (18% and 11%, respectively). All three studies examined the gender of those who attempted suicide among ADHD patients, and two did not find differences[28,37]. Agosti et al[27] found that 52.9% of patients with ADHD who had previous suicide attempts were male, while the rate of males was 58.3% in patients with ADHD without previous suicide attempts. Mayes et al[37] found no differences between boys and girls with ADHD and suicidal ideation (7% and 3%, respectively). Ljung et al[35] found that the risk of suicide attempts among ADHD patients differed significantly by gender (χ2 = 1271.0; P < 0.001): The adjusted estimate was 2.93 (95%CI: 2.60-3.29) for males and 5.41 (95%CI: 4.60-6.36) for females. Only one study examined gender differences in ADHD patients who completed suicide[35] and found no gender differences.
Suicidality in patients with psychiatric disorders who have ADHD comorbidity: Table 3 summarizes the seven studies among the 26, which investigated ADHD, as a comorbid condition of other psychiatric disorders, and its association with suicidality[30,41-46].
Suicidality in ADHD patients who have psychiatric comorbidity: From the 26 papers of this review, the 10 studies, which investigated comorbidity in ADHD patients with suicidality are presented in Table 4[27,28,35-39,47,48].
Table 4.
Included relevant articles examining attention-deficit/hyperactivity disorder and suicidality from January 2011 to January 2015: Suicidality in attention-deficit/hyperactivity disorder patients who have psychiatric comorbidity
| Suicidality in ADHD patients who have psychiatric comorbidity | |||||||
| Ref. | Country | Study design | Sample | Population at onset | Population’s age at onset | Measures for ADHD, comorbid conditions and suicidality | Main findings |
| Agosti et al[27] | United States | Cross-sectional | Clinical sample | Current ADHD: 365 adults: With Suicide attempts: n = 59 No suicide attempts: n = 306 | Age range: 18-66 yr | CIDI, ACDS, DIS-IV | Sixteen percentage of participants with current ADHD diagnosis had previous suicide attempt. While ADHD increased the risk of previous suicide attempt only 1.5 fold, having one or more comorbid disorders increased the risk of previous suicide attempt 4 to 12 fold |
| Balazs et al[28] | Hungary | Cross-sectional | Clinical sample | ADHD and subthreshold ADHD children: n = 220 ADHD and subthreshold ADHD adolescents: n = 198 | Children: Age range: 3-11 yr Mean age: 7.67 yr (SD = 2.03) Adolescents: Age range: 12-17 yr Mean age: 14.31 yr (SD = 1.67) | MINI-KID | The relationship between ADHD and suicidality was fully mediated by comorbid psychiatric disorders. In children, symptoms of anxiety disorders mediated this relationship, while in the adolescent group, symptoms of major depressive episode, dysthymia, and substance abuse/dependence were found to be significant mediators |
| Daviss et al[47] | Lebanon | Cross-sectional | Clinical sample | Youth with ADHD: n = 101 (male ratio: 63.4%) Lifetime SBs n = 28 (male ratio: 42.9%) No lifetime SBs: n = 73 (male ratio: 71.2%) | Age range in the whole sample: 11-18 yr Lifetime SBs: Mean age: 14.6 yr (SD = 2.1) No lifetime SBs: Mean age: 13.5 yr (SD = 1.8) | K-SADS-PL ADHD Rating Scale | In this ADHD sample, after controlling for the age, female sex, and comorbid disorders, lifetime SB remained significantly associated with parent-child conflict, and impairment in nonacademic domains of function and breadth of exposure to victimization events Past and current ADHD symptoms and signs were not associated with lifetime SB |
| Ljung et al[35] | Sweden | Cross-sectional | Patient and prescribed drug registers and population-based registers | ADHD: n = 51707 (male ratio: 69.8%) Control: n = 258535 | Age range: 3-40 yr | Discharge diagnosis of ADHD | Participants with ADHD had an increased risks of both attempted and completed suicide compared with control participants. This result was the same even after adjusting for comorbid psychiatric conditions. While the highest familial risk was reported among first-degree relatives, lower risk was observed among more genetically distant relatives. The results suggests that shared genetic factors are important for this association |
| Mayes et al[36] | United States | Cross-sectional | Community and clinical sample | 1706 children and adolescents with psychiatric disorders and typical development: ADHD-C: n = 566 (male ratio: 74.6%) ADHD-I: n = 235 (male ratio: 57.4%) Other psychiatric disorders (autism, depression/ anxiety, eating disorder, intellectual disability): n = 719 (male ratio: 67.2%) Typical: n = 186 (male ratio: 43.5%) | Age range: 6-18 yr | All participants had a clinical diagnosis of ADHD made by a licensed PhD psychologist. The clinical diagnosis was based on a comprehensive psychological evaluation including diagnostic inter- views with the parent and child, parent and teacher rating scales, review of educational and medical records, extensive psychological testing PBS | All psychiatric groups had far more suicide behavior than typically developed children. ADHD-C: 20.7% had suicide ideation, 6.0% attempt ADHD-I: 7.3% had suicide ideation, 2.6% attempt |
| Mayes et al[37] | United States | Cross-sectional | Clinical sample | Children and adolescents with ADHD: n = 925 (male ratio: 68.5%) ADHD-C: n = 666 ADHD-I: n = 259 | Age range: 3-16 yr Mean age: 8.8 yr (SD = 2.6) | All participants had a clinical diagnosis of ADHD made by a licensed PhD psychologist. The clinical diagnosis was based on a comprehensive psychological evaluation including diagnostic inter- views with the parent and child, parent and teacher rating scales, review of educational and medical records, extensive psychological testing PBS - suicide ideation and attempt items | For the total sample with ADHD, 15.8% had suicide ideation (sometimes or more) and 5.5% had attempts. Ideation and attempts were more than twice as prevalent among participants with ADHD-C than among participants with ADHD-I. ADHD-C: 19% had suicide ideation, 7% attempt ADHD-I: 7% had suicide ideation, 3% attempt Those, who had ADHD alone: 6% had suicide ideation and 2% had suicide attempt |
| Park et al[38] | South Korea | Cross-sectional | Community sample | A total of 6081 subjects: Non-ADHD symptom group: n = 6012 ADHD symptom group: n = 69 | Age range: 18-59 yr | K-CIDI Adult ADHD Self-Report Scale | Those, who had ADHD + co-occurring sadness and ODD, 46% had ideation and 21% had attempts Adult ADHD symptoms are significantly associated with lifetime suicidality. However, the association disappeared after adjusting for other comorbid psychiatric disorders |
| Swanson et al[39] | United States | Longitudinal: 10 yr: First 5 yr follow up and second 10 yr follow-up | Community and clinical sample | ADHD girls: n = 140 Non-ADHD girls: n = 88 | Age range: 6-12 yr at ascertainment Mean age at 5 yr follow-up: 14.2 yr Mean age at 10 yr follow-up: 19.6 yr (range 17-24 yr) | At ascertainment: DISC-IV First follow up: SNAP-IV, Second follow up: SIQ, Barkley Suicide Questionnaire, DISC-IV-YA | Women with a childhood diagnosis of ADHD-C, compared with those with ADHD-I and control group, were at higher risk for suicide attempts. Furthermore, women with a persistent ADHD diagnosis were at higher risk than women with a transient diagnosis and the control group |
| Taylor et al[48] | New Zealand | Cross-sectional | Community sample | 66 adults (43 men, 23 women ADHD: n = 35 (male ratio: 65.7%) Non-ADHD: n = 31 (male ratio: 64.5%) | Age range: 18-65 yr Mean age: 31.9 yr (SD = 1.6) | CAARS DSHI SCID-I (suicidality) CAADID | There was a significant associations between ADHD symptom severity and self-reported suicidal ideation and suicide attempts. These associations between suicidal behaviours and ADHD symptom severity were significantly and differentially mediated by psychosocial variables such as comorbidities (mood, anxiety, drug, and alcohol abuse disorders) and emotion-focussed coping style |
SB: Suicidal behavior; ADHD: Attention-deficit/hyperactivity disorder; CIDI: Composite International Diagnostic Interview; ACDS: Adult ADHD Clinical Diagnostic Scale; DIS-IV: The Diagnostic Interview Schedule for DSM-IV; MINI-KID: Mini-International Neuropsychiatric Interview for children and adolescents; K-SADS-PL: Schedule for Affective Disorder and Schizophrenia for School-Age Children- Present and Lifetime Version; K-CIDI: Korean version of Composite International Diagnostic Interview; DISC-IV-YA: Diagnostic Interview Schedule for Children 4th ed., Young Adult version; SNAP-IV: Swanson, Nolan, and Pelham Rating Scale; SIQ: Self-Injury Questionnaire; CAADID: Conners’Adult ADHD Diagnostic Interview for DSM-IV; CAARS: Conners’ Adult ADHD Rating Scale; DSHI: Deliberate Self-Harm Inventory; ADHD-C: ADHD combined type; ADHD-I: ADHD inattentive type, ADHD-HKS Questionnaire.
Assessments for measuring ADHD, suicidality and comorbid conditions
Assessments for measuring ADHD: Table 5[49-55] summarizes assessments for measuring ADHD.
Table 5.
Assessments for measuring attention-deficit/hyperactivity disorder
| Ref. | Scale | Abbriviation |
| [49] | Adult ADHD Clinic Diagnostic Scale | ACDS |
| [50] | Adult Self-Report Scale | ASRS |
| [51] | Adult ADHD DSM-IV-Based Diagnostic Screening and Rating Scale, ADHD-C: ADHD combined type, ADHD-I: ADHD inattentive type, ADHD-HKS Questionnaire | ADHD scale |
| [52] | Conners’ Adult ADHD Diagnostic Interview for DSM-IV | CAADID |
| [53] | Conners’ Adult ADHD Rating Scale | CAARS |
| [54] | Diagnostic Interview for ADHD in Adults | DIVA |
| [55] | Strengths and Weaknesses of ADHD symptoms and Normal Behaviors | SWAN |
ADHD: Attention-deficit/hyperactivity disorder; DSM-IV: Diagnostic and statistical manual of mental disorders fourth edition; ADHD-HKS: Attention deficit hyperactivity disorder - hyperkinetic syndrome.
Assessments for measuring suicidality and comorbid conditions: Table 6[56-80] summarizes assessments for measuring suicidality and comorbid conditions.
Table 6.
Assessments for measuring suicidality and comorbid conditions
| Ref. | Scale | Abbriviation |
| [56] | Beck Depression Inventory | BDI |
| [57] | Brief Symptoms Inventory | BSI |
| [58] | Brief Symptoms Rating Scale | BSRS-5 |
| [59] | Composite International Diagnostic Interview | CIDI |
| [60,61] | Current Symptoms Scale-Self-Report Form | CSS |
| [62] | Deliberate Self-Harm Inventory | DSHI |
| [63] | Diagnostic Interview Schedule for DSM-IV | DIS-IV |
| [64] | Diagnostic Interview Schedule for Children | DISC-IV |
| [65] | Diagnostic Interview Schedule for Children 4th ed., Young Adult version | DISC-IV-YA |
| [66,67] | European Version of the Adolescent Assessment Dialogue | EuroADAD |
| [68] | Hopelessness Depression Symptom Questionnaire-Suicidality Subscale | HDSQ |
| [69] | Korean version of Composite International Diagnostic Interview | K-CIDI |
| [70] | Schedule for Affective Disorder and Schizophrenia for School-Age Children- Present and Lifetime Version | K-SADS-PL |
| [71] | Psychological Screening Test for Adolescents | PSTA |
| [72] | Rutter's Behaviour Scale for Children (Teacher’s Scale) | Rutter B2 |
| [73] | Mini International Neuropsychiatric Interview | MINI |
| [73,74] | Mini International Neuropsychiatric Interview Kid | MINI Kid |
| [75] | Pediatric Behavior Scale | PBS |
| [76,77] | Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version | SCID-I-CV |
| [78] | Structured Clinical Interview for DSM-III-R Personality Disorders | SCID-II |
| [79] | Self-Injury Questionnaire | SIQ |
| [80] | Swanson, Nolan, and Pelham Rating Scale 4th ed. | SNAP-IV |
DISCUSSION
This review of the last four years strengthens the recent finding that ADHD is related to high suicidality in all age groups and in both girls and boys.
Although our current systematic review was conducted only for the last four years, we still found 26 papers that presented data on ADHD and suicidality. Moreover, we know that several systematic review papers and overviews had been done previously. Impey et al[19], who performed a systematic search on the same topic, covering all studies up to January 2011, the starting point of our search period, found 25 papers. All of them support the view that research on the association of ADHD and suicidality is a subject of high and growing interest, and clinicians and researchers need to have access to up-to-date knowledge in this field.
The studies of this review are culturally diverse, as they come from four continents. This shows that this topic has relevance all over the world and that the conclusions can be used in wider aspects.
Regarding the age groups investigated on the topic of ADHD and suicidality, the studies have been balanced over the last four years: Exactly half of them investigated children/adolescents, and half of them examined adults. This reflects the growing interest in ADHD in adulthood among both healthcare professionals and researchers[81]. Considering the previous studies on this topic - which were included in the review of Impey et al[19] - a majority of them involved the 12-18 age group, although there were a few studies in older and younger age groups as well. Additionally, in their review, Impey et al[19] concluded that, based on the studies included in their review paper, age differences were not clearly definable. In this way, the current review extends our knowledge with further information on all age groups with ADHD and suicidality, including children under 12 and adults, and makes it possible to compare different age groups.
Systematically searching the literature of the last four years, we found only two studies that reported the prevalence data of ADHD among patients with suicidality[24,45]; however, there were a total of six studies addressing that study question in the review of Impey et al[19]. There were five in the review of James et al[18], but four of them were included in the review of Impey et al[19] as well. In both studies in the current review, the diagnoses of ADHD and suicidality were based on a clinician’s opinion. A very important and new result shown in our review is that one-quarter of the suicidal children under 12 years old had ADHD. The prevalence rate of ADHD among suicidal adolescents was lower (5.7%) than in children, and it was lower than in previous studies[19]. One possible explanation could be that these studies did not use either diagnostic interviews or screening tools for the diagnoses of ADHD and suicidality. All of them show that there is still limited data on the prevalence of ADHD among patients with suicidality; however, all of the studies performed found a high prevalence of ADHD in this population, especially among young children. Further studies are needed, but based on the current knowledge, we suggest a routine screening for ADHD patients with suicidal thoughts and attempts, with a special focus on young children.
Almost half of the papers reported prevalence data on suicidality in ADHD patients. The results strengthen the findings of previous studies[18-21] that there is a positive association between ADHD and suicidality, including completed suicides, attempts, as well as ideation. We would like to highlight that, in adolescence, based on the studies of the last four years, more than half of the patients with ADHD had suicidal thoughts, and this prevalence rate is even higher than what has been described previously[19]. It is important to note that even in adulthood, one third of ADHD patients had suicidal ideation. Based on these results, we suggest the introduction of routine screening questions on suicidal thoughts in outpatient/inpatient ADHD clinics, both for those specializing in adults and those specializing in children/adolescents. This improvement in clinical practice can be an important step towards suicide prevention.
The rate of previous suicide attempts was the highest (16%) in the adult ADHD age group; however, adolescents need attention in this respect as well, as almost one-tenth of ADHD patients in this age group had a previous suicide attempt. As one of the strongest predictors of a completed suicide is a previous suicide attempt, close follow-up of these ADHD patients could be of core importance in suicide prevention.
When we examined, which identifiable risk factors can be associated with suicide in ADHD, first we focused on gender. There are still a limited number of studies examining gender differences within this topic. The only study[24] that reported data on the gender distribution of suicidal patients with ADHD is in agreement with the conclusion of previous reviews[18,19] that ADHD is present more often among suicidal men than suicidal women. However, when we examined the prevalence of suicidality (e.g., ideation, attempts and completed suicides) in ADHD patients, two out of three of the studies did not find a difference between men and women[27,37], and one study reported an adjusted estimate for the risk of suicide attempts in females that was almost twice as high[35]. In his selected review paper, Nigg[21] reported that girls had an elevated risk of a suicide attempt as well; however, the author stated that boys have a higher risk of completed suicide among ADHD patients. It is important to note that there are very few studies that have focused on female patients with ADHD[82]. One of them was conducted during the search period of this review[39], while in the previous review on this topic, there were several studies in which only men were enrolled, as well as those in which both females and men were included[19]. Based on the currently available results, both females and males with ADHD need a special focus to recognize their possible suicide risk; however, further studies are needed to gain a better understanding of the gender differences in all age groups.
Second, when we examined identifiable risk factors, which can be associated with suicide in ADHD, we focused on comorbidities. One of the most exciting questions, which also has been raised in all of the previous review and summary papers[18-21], is whether there is a direct association between ADHD and suicidality or if ADHD increases the risk of suicide through comorbid conditions. In the current review, we examined two aspects of this question. First, we reviewed all of the papers within the examined period that measured the prevalence of ADHD in suicidal patients with other psychiatric disorders, such as mood disorders, schizophrenia, alcohol/drug intoxication and chronic fatigue syndrome. The results of all seven studies on this topic showed that the prevalence of suicidality is higher when psychiatric disorders are comorbid with ADHD than in their absence. These findings suggest that the presence of ADHD, as a comorbid condition, conveys an increased risk of suicide for patients with other psychiatric disorders. Second, we investigated the role of comorbidity in ADHD patients with suicidality. The majority of the studies (7/9) found that comorbid disorders mediate between suicidality and ADHD[27,36,38-41,49], which is in line with the conclusion of previous review papers[18-21]. It highlights the importance of raising clinicians’ awareness of the need to screen and treat comorbidity in ADHD, which may reduce suicidality as well.
These findings are limited in that only studies published in English and in Hungarian were included. Three potentially relevant studies were excluded because they were neither in English nor in Hungarian. The vast majority of the studies included in this review have a cross-sectional design, which limits the possible conclusions. Additionally, most of the studies that were conducted before this review paper have a cross-sectional design as well[19]. This should draw the attention of the researchers that, in the future, more studies are needed with a longitudinal design. Additionally, similar to the previous review of Impey et al[19], the measurement methods for both ADHD and suicidality in the studies included in the current review are very different, i.e., diagnostic interviews, rating questionnaires and clinician-made diagnoses - which means that a comparison of the numerical results is not possible.
In conclusion, our systematic highlights that the early recognition and treatment of ADHD - either as a comorbid condition or as a main diagnosis- and the co-occurring psychiatric disorders, can play an important role in the secondary prevention of suicide. Additionally, it could be useful to incorporate routine measurements of suicidality in the daily practice of ADHD clinics.
ACKNOWLEDGMENTS
This work was supported by OTKA K108336 grant. Judit Balázs was supported by the János Bolyai Research Scholarship of the Hungarian Academy of Sciences.
COMMENTS
Background
Recently, several studies have focused on attention-deficit/hyperactivity disorder (ADHD) as a possible psychiatric disorder that may serve as a suicide risk factor as well. This paper presents a systematic review of suicidality and ADHD as an extension of previous reviews for the search period and with study questions.
Research frontiers
Suicide prevention is a public health issue all over the world. As ADHD is one of the most prevalent psychiatric disorders among children and adolescents and in 40%-60% of the cases, it continues into adulthood. All additional knowledge on the possible association between ADHD and suicidality has high clinical importance and can add to suicide prevention.
Innovations and breakthroughs
Although this systematic review was conducted only for the last four years, the authors still found 26 papers that presented data on ADHD and suicidality.
Applications
This systematic review strengthens the finding that ADHD is related to high suicidality in all age groups and in both girls and boys. It highlights that the early recognition and treatment of ADHD - either as a comorbid condition or as a main diagnosis - and the co-occurring psychiatric disorders, can play an important role in the secondary prevention of suicide.
Terminology
Attention-deficit/hyperactivity disorder: ADHD is a neurodevelopmental disorder with ongoing pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development; Suicidality: It includes suicidal thought, suicidal plan, suicidal attempt and completed suicide; Systematic review: A systematic review is a type of literature review which aims to provide a thorough, complete, exhaustive summary of current literature relevant to a research question.
Peer-review
The authors have reviewed the evidence for an association between ADHD and suicide. This is a descriptive review that does not include meta-analysis.
Footnotes
Conflict-of-interest statement: Author Judit Balazs has received a speaker honorarium from E. Lilly Company and she is a member of the Advisory Board committee of E. Lilly Company. Author Agnes Kereszteny declares that she has no conflict of interest.
Data sharing statement: The current manuscript does not describe a study, it is a systematic review.
Manuscript source: Invited manuscript
Specialty type: Psychiatry
Country of origin: Hungary
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
Peer-review started: November 2, 2016
First decision: November 30, 2016
Article in press: January 18, 2017
P- Reviewer: Gazdag G, Poulton A, Pivac N S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.World Health Organization. Figures and Facts About suicide ([accessed 2015 Nov 27]) Available from: http: //www.who.int/mediacentre/news/releases/2014/suicide-prevention-report/en/
- 2.Biederman J, Ball SW, Monuteaux MC, Mick E, Spencer TJ, McCreary M, Cote M, Faraone SV. New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. J Am Acad Child Adolesc Psychiatry. 2008;47:426–434. doi: 10.1097/CHI.0b013e31816429d3. [DOI] [PubMed] [Google Scholar]
- 3.Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2010;67:1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galéra C, Bouvard MP, Encrenaz G, Messiah A, Fombonne E. Hyperactivity-inattention symptoms in childhood and suicidal behaviors in adolescence: the Youth Gazel Cohort. Acta Psychiatr Scand. 2008;118:480–489. doi: 10.1111/j.1600-0447.2008.01262.x. [DOI] [PubMed] [Google Scholar]
- 5.Manor I, Gutnik I, Ben-Dor DH, Apter A, Sever J, Tyano S, Weizman A, Zalsman G. Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents - a pilot study. Eur Psychiatry. 2010;25:146–150. doi: 10.1016/j.eurpsy.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC, London, England: American Psychiatric Association; 2013. [Google Scholar]
- 7.World Health Organization. ICD-10, the international classification of diseases. Classification of mental and behavioural disorders. Diagnostic criteria for research. Geneva, Switzerland: World Health Organization; 1993. [Google Scholar]
- 8.Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatr Scand. 2006;113:180–206. doi: 10.1111/j.1600-0447.2005.00702.x. [DOI] [PubMed] [Google Scholar]
- 9.Balázs J, Gádoros J. Comorbidity in child psychiatry: is the comorbidity of pediatric mania and ADHD really that high? Psychiatr Hung. 2005;20:293–298. [PubMed] [Google Scholar]
- 10.Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry. 1991;148:564–577. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- 11.A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 12.Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. 2003;160:1093–1099. doi: 10.1176/appi.ajp.160.6.1093. [DOI] [PubMed] [Google Scholar]
- 13.Brent DA, Perper JA, Goldstein CE, Kolko DJ, Allan MJ, Allman CJ, Zelenak JP. Risk factors for adolescent suicide. A comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry. 1988;45:581–588. doi: 10.1001/archpsyc.1988.01800300079011. [DOI] [PubMed] [Google Scholar]
- 14.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 15.Lowe GA, Gibson RC. Depression in adolescence: new developments. West Indian Med J. 2005;54:387–391. doi: 10.1590/s0043-31442005000600009. [DOI] [PubMed] [Google Scholar]
- 16.Brown RT, Freeman WS, Perrin JM, Stein MT, Amler RW, Feldman HM, Pierce K, Wolraich ML. Prevalence and assessment of attention-deficit/hyperactivity disorder in primary care settings. Pediatrics. 2001;107:E43. doi: 10.1542/peds.107.3.e43. [DOI] [PubMed] [Google Scholar]
- 17.Scahill L, Schwab-Stone M. Epidemiology of ADHD in school-age children. Child Adolesc Psychiatr Clin N Am. 2000;9:541–555, vii. [PubMed] [Google Scholar]
- 18.James A, Lai FH, Dahl C. Attention deficit hyperactivity disorder and suicide: a review of possible associations. Acta Psychiatr Scand. 2004;110:408–415. doi: 10.1111/j.1600-0447.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- 19.Impey M, Heun R. Completed suicide, ideation and attempt in attention deficit hyperactivity disorder. Acta Psychiatr Scand. 2012;125:93–102. doi: 10.1111/j.1600-0447.2011.01798.x. [DOI] [PubMed] [Google Scholar]
- 20.Furczyk K, Thome J. Adult ADHD and suicide. Atten Defic Hyperact Disord. 2014;6:153–158. doi: 10.1007/s12402-014-0150-1. [DOI] [PubMed] [Google Scholar]
- 21.Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev. 2013;33:215–228. doi: 10.1016/j.cpr.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Renaud J, MacNeil S, Rinaldis S. Current psychiatric morbidity and aggression/impulsivity in child and adolescent suicide and ADHD. Directions in Psychiatry. 2012;32:137–1345. [Google Scholar]
- 23.Capuano A, Scavone C, Rafaniello C, Arcieri R, Rossi F, Panei P. Atomoxetine in the treatment of attention deficit hyperactivity disorder and suicidal ideation. Expert Opin Drug Saf. 2014;13 Suppl 1:S69–S78. doi: 10.1517/14740338.2014.941804. [DOI] [PubMed] [Google Scholar]
- 24.Ben-Yehuda A, Aviram S, Govezensky J, Nitzan U, Levkovitz Y, Bloch Y. Suicidal behavior in minors-diagnostic differences between children and adolescents. J Dev Behav Pediatr. 2012;33:542–547. doi: 10.1097/01.DBP.0000415830.85996.e6. [DOI] [PubMed] [Google Scholar]
- 25.Evren C, Dalbudak E, Evren B, Can Y, Umut G. The severity of attention deficit hyperactivity symptoms and its relationship with lifetime substance use and psychological variables among 10th grade students in Istanbul. Compr Psychiatry. 2014;55:1665–1670. doi: 10.1016/j.comppsych.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Soole R, Kõlves K, De Leo D. Factors related to childhood suicides: analysis of the Queensland Child Death Register. Crisis. 2014;35:292–300. doi: 10.1027/0227-5910/a000267. [DOI] [PubMed] [Google Scholar]
- 27.Agosti V, Chen Y, Levin FR. Does Attention Deficit Hyperactivity Disorder increase the risk of suicide attempts? J Affect Disord. 2011;133:595–599. doi: 10.1016/j.jad.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balazs J, Miklósi M, Keresztény A, Dallos G, Gádoros J. Attention-deficit hyperactivity disorder and suicidality in a treatment naïve sample of children and adolescents. J Affect Disord. 2014;152-154:282–287. doi: 10.1016/j.jad.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 29.Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131:637–644. doi: 10.1542/peds.2012-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng SH, Lee CT, Chi MH, Sun ZJ, Chen PS, Chang YF, Yeh CB, Yang YK, Yang YC. Factors Related to Self-Reported Attention Deficit Among Incoming University Students. J Atten Disord. 2016;20:754–762. doi: 10.1177/1087054714550335. [DOI] [PubMed] [Google Scholar]
- 31.Huntley Z, Maltezos S, Williams C, Morinan A, Hammon A, Ball D, Marshall EJ, Keaney F, Young S, Bolton P, et al. Rates of undiagnosed attention deficit hyperactivity disorder in London drug and alcohol detoxification units. BMC Psychiatry. 2012;12:223. doi: 10.1186/1471-244X-12-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hurtig T, Taanila A, Moilanen I, Nordström T, Ebeling H. Suicidal and self-harm behaviour associated with adolescent attention deficit hyperactivity disorder-a study in the Northern Finland Birth Cohort 1986. Nord J Psychiatry. 2012;66:320–328. doi: 10.3109/08039488.2011.644806. [DOI] [PubMed] [Google Scholar]
- 33.Kavakci O, Kugu N, Semiz M, Meydan F, Karsikaya S, Dogan O. (). Prevalence of attention-deficit/hyperactivity disorder and co-morbid disorders among students of Cumhuriyet University. Eur J Psychiat. 2012;26:107–117. [Google Scholar]
- 34.Keresztény A, Dallos G, Miklósi M, Róka A, Gádoros J, Balázs J. Comparing the comorbidity of attention-deficit/hyperactivity disorder in childhood and adolescence. Psychiatr Hung. 2012;27:165–173. [PubMed] [Google Scholar]
- 35.Ljung T, Chen Q, Lichtenstein P, Larsson H. Common etiological factors of attention-deficit/hyperactivity disorder and suicidal behavior: a population-based study in Sweden. JAMA Psychiatry. 2014;71:958–964. doi: 10.1001/jamapsychiatry.2014.363. [DOI] [PubMed] [Google Scholar]
- 36.Mayes SD, Baweja R, Calhoun SL, Syed E, Mahr F, Siddiqui F. Suicide ideation and attempts and bullying in children and adolescents: psychiatric and general population samples. Crisis. 2014;35:301–309. doi: 10.1027/0227-5910/a000264. [DOI] [PubMed] [Google Scholar]
- 37.Mayes SD, Calhoun SL, Baweja R, Feldman L, Syed E, Gorman AA, Montaner J, Annapareddy J, Gupta N, Bello A, et al. Suicide Ideation and Attempts are Associated with Co-occurring Oppositional Defiant Disorder and Sadness in Children and Adolescents with ADHD. J Psychopathol Behav. 2015;37:274–282. [Google Scholar]
- 38.Park S, Cho MJ, Chang SM, Jeon HJ, Cho SJ, Kim BS, Bae JN, Wang HR, Ahn JH, Hong JP. Prevalence, correlates, and comorbidities of adult ADHD symptoms in Korea: results of the Korean epidemiologic catchment area study. Psychiatry Res. 2011;186:378–383. doi: 10.1016/j.psychres.2010.07.047. [DOI] [PubMed] [Google Scholar]
- 39.Swanson EN, Owens EB, Hinshaw SP. Pathways to self-harmful behaviors in young women with and without ADHD: a longitudinal examination of mediating factors. J Child Psychol Psychiatry. 2014;55:505–515. doi: 10.1111/jcpp.12193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Eck K, Ballard E, Hart S, Newcomer A, Musci R, Flory K. ADHD and Suicidal Ideation: The Roles of Emotion Regulation and Depressive Symptoms Among College Students. J Atten Disord. 2015;19:703–714. doi: 10.1177/1087054713518238. [DOI] [PubMed] [Google Scholar]
- 41.Bácskai E, Czobor P, Gerevich J. Trait aggression, depression and suicidal behavior in drug dependent patients with and without ADHD symptoms. Psychiatry Res. 2012;200:719–723. doi: 10.1016/j.psychres.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 42.Berkol TD, Yargic I, Ozyildirim I, Yazici O. Comorbidity of Adult Attention Deficit and Hyperactivity Disorder in Bipolar Patients: Prevalence, Sociodemographic and Clinical Correlates. Archives of Neuropsychiatry. 2014;33:542–547. doi: 10.4274/npa.y6376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Donev R, Gantert D, Alawam K, Edworthy A, Hässler F, Meyer-Lindenberg A, Dressing H, Thome J. Comorbidity of schizophrenia and adult attention-deficit hyperactivity disorder. World J Biol Psychiatry. 2011;12 Suppl 1:52–56. doi: 10.3109/15622975.2011.599212. [DOI] [PubMed] [Google Scholar]
- 44.Patros CH, Hudec KL, Alderson RM, Kasper LJ, Davidson C, Wingate LR. Symptoms of attention-deficit/hyperactivity disorder (ADHD) moderate suicidal behaviors in college students with depressed mood. J Clin Psychol. 2013;69:980–993. doi: 10.1002/jclp.21994. [DOI] [PubMed] [Google Scholar]
- 45.Penney A, Mazmanian D, Jamieson J, Black N. Factors associated with recent suicide attempts in clients presenting for addiction treatment. Int J Ment Health Addict. 2012;10:132–140. [Google Scholar]
- 46.Sáez-Francàs N, Alegre J, Calvo N, Antonio Ramos-Quiroga J, Ruiz E, Hernández-Vara J, Casas M. Attention-deficit hyperactivity disorder in chronic fatigue syndrome patients. Psychiatry Res. 2012;200:748–753. doi: 10.1016/j.psychres.2012.04.041. [DOI] [PubMed] [Google Scholar]
- 47.Daviss WB, Diler RS. Suicidal behaviors in adolescents with ADHD: associations with depressive and other comorbidity, parent-child conflict, trauma exposure, and impairment. J Atten Disord. 2014;18:680–690. doi: 10.1177/1087054712451127. [DOI] [PubMed] [Google Scholar]
- 48.Taylor MR, Boden JM, Rucklidge JJ. The relationship between ADHD symptomatology and self-harm, suicidal ideation, and suicidal behaviours in adults: a pilot study. Atten Defic Hyperact Disord. 2014;6:303–312. doi: 10.1007/s12402-014-0139-9. [DOI] [PubMed] [Google Scholar]
- 49.Adler L, Spence T. The Adult ADHD Clinical Diagnostic Scale (ACDS), version 1.2. Washington DC: New York University School of Medicine; 2004. [Google Scholar]
- 50.Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- 51.Bullinger M, Brütt AL, Erhart M, Ravens-Sieberer U. Psychometric properties of the KINDL-R questionnaire: results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17 Suppl 1:125–132. doi: 10.1007/s00787-008-1014-z. [DOI] [PubMed] [Google Scholar]
- 52.Epstein JN, Johnson DE, Conners CK. Conners’ adult ADHD diagnostic interview for DSM-IV. North Tonawanda: Multi-Health Systems; 2001. [Google Scholar]
- 53.Conners CK, Erhart D, Sparrow E. Conners’ Adult ADHD Rating Scales, technical manual. New York, NY: Multi-Health Systems; 1999. [Google Scholar]
- 54.Kooij JJS. Adult ADHD: Diagnostic assessment and treatment. 3rd ed. Berlin: Springer; 2012. [Google Scholar]
- 55.Swanson J, Schuck S, Mann M, Carlson C, Hartman C, Sergeant J, Beck R. Over-identification of extreme behavior in the evaluation and diagnosis of ADHD/HKD, 2001 ([accessed 2009 Nov]) Available from: http: //www.adhd.net.
- 56.Beck AT, Beamesderfer A. Assessment of depression: The depression inventory. In P. Pichot & R. Olivier-Martin (Eds.), Modern problems of pharmacopsychiatry: Psychological measurements in psychopharmacology. Basel, Switzerland: S. Karger; 1974. pp. 151–169. [Google Scholar]
- 57.Derogatis LR, Coons HL. Self-report measures of stress. In Breznitz S, Goldberger L (Eds.). Handbook of stress: Theoretical and clinical aspects. 2nd ed. New York, NY: Free Press; 1993. pp. 200–233. [Google Scholar]
- 58.Lee MB, Lee YJ, Yen LL, Lin MH, Lue BH. Reliability and validity of using a Brief Psychiatric Symptom Rating Scale in clinical practice. J Formos Med Assoc. 1990;89:1081–1087. [PubMed] [Google Scholar]
- 59.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry. 1993;50:565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- 61.Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. New York, NY: Guilford Press; 2008. [Google Scholar]
- 62.Gratz KL. Measurement of deliberate self-harm: preliminary data on the deliberate self-harm inventory. J Psychopathol Behav. 2001;23:253–263. [Google Scholar]
- 63.Robins L, Helzer J. Diagnostic Interview Schedule (DIS), Version II-A. St. Louis: Washington University School of Medicine; 1985. [Google Scholar]
- 64.Shaffer D, Fisher P, Piacentini J, Schwab-Stone M, Wicks J. Diagnostic Interview Schedule for Children. New York, NY: Columbia University; 1993. [Google Scholar]
- 65.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 66.Czobor P, Bácskai E, Oberg D, Haack MJ, Gerevich J. The European Adolescent Assessment Dialogue (EuroADAD): a psychometric evaluation. Eur Addict Res. 2011;17:302–315. doi: 10.1159/000329989. [DOI] [PubMed] [Google Scholar]
- 67.Gerevich J, Bácskai E, Kó J, Rózsa S. Reliability and validity of the Hungarian version of the European Addiction Severity Index. Psychopathology. 2005;38:301–309. doi: 10.1159/000088918. [DOI] [PubMed] [Google Scholar]
- 68.Metalsky GI, Joiner Jr TE. The Hopelessness Depression Symptom Questionnaire. Cognitive Therapy and Research. 1997;21:359–384. [Google Scholar]
- 69.Cho MJ, Hahm BJ, Suh DW, Hong JP, Bae JN, Kim JK, Lee DW, Cho SJ. Development of a Korean version of the Composite International Diagnostic Interview (K-CIDI) Korean Neuropsychiatr Assoc. 2002;41:123–137. [Google Scholar]
- 70.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 71.Ogel K, Karadayi G, Senyuva G, Kanoglu H. The reliability and validity study of psychological screening test for adolescents. Düşünen Adam Journal of Psychiatry and Neurological Sciences. 2012;25:8–16. [Google Scholar]
- 72.Rutter M. A children’s behaviour questionnaire for completion by teachers: preliminary findings. J Child Psychol Psychiatry. 1967;8:1–11. doi: 10.1111/j.1469-7610.1967.tb02175.x. [DOI] [PubMed] [Google Scholar]
- 73.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–33; quiz 34-57. [PubMed] [Google Scholar]
- 74.Balazs J, Bíró A, Dálnoki D, Lefkovics E, Tamás Zs, Nagy P, Gádoros JA, Gyermek MINI. kérdőív magyar nyelvű változatának ismertetése. [Development of the Hungarian version of the M.I.N.I. Kid] Psychiatria Hungarica. 2004;19:358–364. [Google Scholar]
- 75.Lindgren SD, Koeppl GK. Assessing child be- havior problems in a medical setting: Development of the Pediatric Behavior Scale. In Prinz RJ (Ed.), Advances in behavioral assessment of children and families. Greenwich, CT: JAI; 1987. pp. 57–90. [Google Scholar]
- 76.First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV Axis I disorders, research version, non- patient edition (SCID-I/NP) New York: New York State Psychiatric Insti- tute, Biometrics Research; 2002. [Google Scholar]
- 77.Ozkurkcugil A, Aydemir O, Yıldız M. Adaptation and Reliability Study of Turkish Structured clinical interview for DSM-IV Axis I Disorders. Ilacve Tedavi Dergisi. 1999;12:233–236. [Google Scholar]
- 78.Sorias S, Saygili R, Elbi H. Structured Clinical Interview for DSM- III-R Personality Disorders (SCID II) Turkish Version: Ege University Press; 1990. [Google Scholar]
- 79.Claes L, Vandereycken W, Vertommen H. Self-injurious behaviors in eating-disordered patients. Eat Behav. 2001;2:263–272. doi: 10.1016/s1471-0153(01)00033-2. [DOI] [PubMed] [Google Scholar]
- 80.Swanson JM. School-based assessments and interventions for ADD students. Irvine, CA: K. C. Publishing; 1992. [Google Scholar]
- 81.Ramos-Quiroga JA, Montoya A, Kutzelnigg A, Deberdt W, Sobanski E. Attention deficit hyperactivity disorder in the European adult population: prevalence, disease awareness, and treatment guidelines. Curr Med Res Opin. 2013;29:1093–1104. doi: 10.1185/03007995.2013.812961. [DOI] [PubMed] [Google Scholar]
- 82.Cho SC, Kim JW, Choi HJ, Kim BN, Shin MS, Lee JH, Kim EH. Associations between symptoms of attention deficit hyperactivity disorder, depression, and suicide in Korean female adolescents. Depress Anxiety. 2008;25:E142–E146. doi: 10.1002/da.20399. [DOI] [PubMed] [Google Scholar]


