Abstract
Background
Health-related quality of life (HRQOL) is increasingly measured as an outcome for clinical and health services research. However, relatively little is known about how non-health factors affect HRQOL. Personality is a potentially important factor, yet evidence regarding the effects of personality on HRQOL measures is unclear.
Methods
This systematic review examined the relationships among aspects of personality and HRQOL. Eligible studies were identified from Medline and PsycINFO. The review included 76 English-language studies with HRQOL as a primary outcome and that assessed personality from the psychological perspective. Individuals with various health states, including ill (e.g., cancer, cardiovascular disorders), aging, and healthy, were included in this review study.
Results
Some personality characteristics were consistently related to psychosocial aspects more often than physical aspects of HRQOL. Personality characteristics, especially neuroticism, mastery, optimism, and sense of coherence were most likely to be associated with psychosocial HRQOL. Personality explained varying proportions of variance in different domains of HRQOL. The range of variance explained in psychosocial HRQOL was 0 to 45% and the range of explained variance in physical HRQOL was 0 to 39%.
Conclusions
Personality characteristics are related to HRQOL. Systematic collection and analysis of personality data alongside HRQOL measures may be helpful in medical research, clinical practice, and health policy evaluation.
Introduction
Health-related quality of life (HRQOL) is increasingly used to evaluate treatment effectiveness be affected by psychological characteristics. Previous studies have begun to explore the relationships between personality characteristics and HRQOL [1–3]. Evidence indicates that adult personality tends to remain stable over long periods of time [4]. There is a general consensus that personality is a trait (a stable tendency to react a certain way) rather than a state (a reaction to an immediate situation). This distinction is of particular interest for research and evaluation, because personality influences an individual’s thoughts, feelings, and behaviors [5, 6].
Two personality measurement frameworks are commonly used to guide personality research: Eynsenck’s Three-Factor Model, which comprises neuroticism, extraversion, and psychoticism [7]; and the Five-Factor Model, which comprises neuroticism, extraversion, agreeableness, conscientiousness, and openness to experience [8]. These models capture the personality traits that the authors believe to be essential and orthogonal. A limitation of both models is that they emphasize superordinate traits rather than subordinate traits (or facets) that might be of interest to researchers [9]. Another approach to delineating personality is to focus on individual traits that may be incorporated into one of the superordinate factors of the models but also have their own specific focus. Individual traits typically considered in medical research include optimism (expecting good things will be plentiful in the future and bad things will be scarce), aggression (attempting to harm another person), hopefulness (tendency to construct and respond to the perceived future positively), negative affectivity (disposition to subjective distress), and sense of coherence (confidence that one’s internal and external environment are predictable and that there is a high probability things will work out).
Two different approaches have been used by investigators to study the relationships between personality and HRQOL. One approach examines the direct effect of specific personality traits on HRQOL [1, 4, 9]. Other approach emphasizes the functional aspects of personality, for example examining how personality influences health through perceptions, cognition, values, goals adjustment, motivations, biological factors, and behaviors [10, 11].
A greater understanding of the relationships between personality and health could enhance research on the effectiveness of health care interventions and treatments, by increasing the amount of variance in patient outcomes that can be explained. It could also help physicians identify barriers to treatment adherence and subsequently improve their patients’ health outcomes. For example, optimistic people adhere better to treatment regimens, use adaptive coping to reduce physiological consequences of stress, and report fewer stressful events, fewer somatic symptoms, and better functional status than pessimistic patients [12–14]. However, to our knowledge, there has not been a comprehensive review of the influence of personality on HRQOL.
We conducted a systematic review of literature on the relationships among personality characteristics and dimensions of HRQOL. We aimed to identify the magnitude of personality characteristics associated with different domains of HRQOL, investigate the potential mechanisms through which personality affects HRQOL, and examine the amount of variance in HRQOL that is explained by specific personality characteristics.
Methods
Literature search strategy
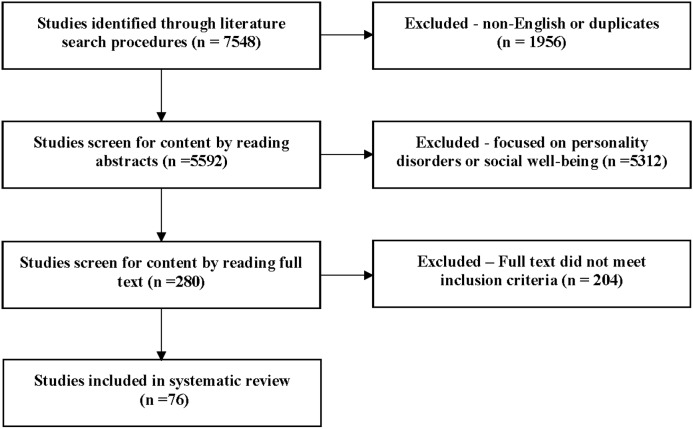
We used PubMed and PsycINFO to identify relevant studies using the medical subject heading (MeSH) keywords “quality of life” and “personality” (Fig 1). To identify additional studies, we applied 26 of the most widely used HRQOL measures [15] as key words. References cited in the identified articles were examined to obtain additional studies for further consideration. We restricted the search to English-language articles published between January 1, 1985, and December 31, 2009.
Fig 1. Flowchart of studies selected to be included in the systematic review.
Inclusion and exclusion criteria for study selection
Different terms related to personality traits have appeared in the literature. The inclusion of specific personality traits to this study is based on the two most commonly used frameworks (Eynsenck’s Three-Factor Model [7] and the Five-Factor Model [8]) and the consensus among our team members after reviewing the literature on the association of personality trait and HRQOL. The definitions for more specific personality characteristics and related measures are listed in S1 Appendix. We included studies that used standard psychological measures of personality that possess acceptable measurement properties (i.e., reliability and content and construct validity) [16]. We excluded studies that treated personality measures as diagnostic criteria for psychopathology [15], and those that focused on social or subjective well-being [17, 18] since this construct is distinct from HRQOL. Additionally, we excluded studies that explored the relationships between personality and HRQOL solely for the purpose of validating HRQOL measures. For validation studies, developers might further revise HRQOL measures; therefore, the psychometric properties of HRQOL measures are not always optimal. Finally, we excluded studies that reported personality characteristics and HRQOL, but did not examine the relationships between the two variables.
Two investigators (ICH, AWW) independently reviewed the abstract of each study to confirm the eligibility. If an abstract was selected as eligible, the same authors independently reviewed the respective articles to confirm that they met the inclusion criteria. Discrepancies were adjudicated by consensus, or failing this, by other investigators (PK, MAA).
Data extraction and analysis
We designed a data extraction form to extract information from each study on the specific aims, population, settings, design, methods, domains of personality, domains of HRQOL, and major findings. The study design was categorized as cross-sectional (CS) versus longitudinal cohort (CO). We categorized HRQOL domains into overall/global QOL, psychological functioning/well-being, role functioning, social functioning, vitality, physical functioning, bodily pain, general health perceptions, somatic symptoms, and other functioning. We further classified these domains as either physical aspects or psychosocial aspects of HRQOL [19].
We analyzed and reported the findings based on the relationships between personality characteristics and HRQOL. Specifically, we examined the magnitude of bivariate association between individual personality characteristics and HRQOL variables using correlation coefficients (r) and effect sizes (Cohen’s d), and examined the variance in HRQOL explained by personality characteristics (R2). We also examined separately the statistical significance of the relationships conducted by t-test, analysis of variance (ANOVA), linear regression analysis, logistic regression analysis, path analysis, or structural equation modeling, and reported the percentage of analyses that demonstrated a significant relationship between personality and HRQOL domains. We defined the percentage of significant results as the number of analyses with statistically significant findings (p-value <0.05) divided by the number of analyses identified from the studies under our review.
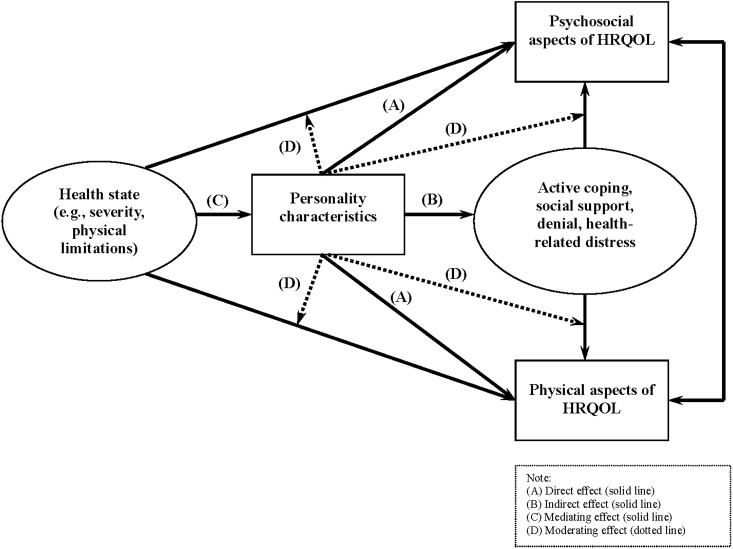
We hypothesized that personality characteristics would be more strongly associated with psychosocial aspects than physical aspects. A schematic of the potential mechanisms through which personality influences HRQOL is shown in Fig 2, in which the specific mechanisms were classified as direct (Route A), indirect (Route B), mediating (Route C), and moderating effects (Route D). We generated this personality-HRQOL conceptual framework up front to guide our analyses.
Fig 2. Pathways of personality to psychosocial aspects and physical aspects of HRQOL.
Indirect effects were defined as the influence of personality characteristics on HRQOL through the effects of other variables, such as social support or coping style. Path analysis or structural equation modeling was generally used to identify the presences of indirect effects [20].
Mediating effects occur when an independent variable, such as disease severity, affects HRQOL by acting through the influence of the effect of a personality characteristic. Ideally, this effect can be tested using datasets containing changes in independent variables, personality traits, and HRQOL. In this review study, we categorized an effect as mediating if 1) there was a significant association between personality and the independent variable, 2) there was a significant association between personality and HRQOL, and 3) the association between the independent variable and HRQOL diminished subsequently after adjusting for the effect of personality variables. In contrast, moderating effects were defined as the relationships between HRQOL and personality characteristics that differ depending upon a third variable, such as a stressful event. An interaction term of personality with the third variable is usually tested to identify the moderating effects. If no moderating effects exist, then we can regard personality variables as independent predictors of HRQOL [21].
We investigated whether personality characteristics were more likely to affect HRQOL reported by patients themselves or that reported by proxies (e.g., family members, physicians or observers). We hypothesized that personality would be more strongly associated with self-ratings of HRQOL than with proxy-ratings for the patients, and personality characteristics would associate with the discrepancy in HRQOL rated by patients themselves and their proxies.
Finally, we investigated the importance of personality characteristics on HRQOL relative to other factors (e.g. sociodemographic or biomedical) by examining the standardized coefficients of regression analysis or structural equation models, and the amount of variance explained in the reviewed studies.
Results
Characteristics of the selected studies
We initially identified 7,548 studies through literature search procedures, of which 1,956 were excluded because they were non-English or duplicates. Of the 5,592 remaining studies, we excluded an additional 5,312 studies after reviewing the abstracts either because they did not investigate the association between personality characteristics and HRQOL, they focused on personality disorders or social well-being rather than HRQOL, or they were designed to validate HRQOL measures. Of the 280 remaining studies, we excluded 204 after reviewing the full-text articles based on the review inclusion criteria (Fig 2). Table 1 shows the characteristics of 76 studies under our review in a chronological order from newest to oldest; these studies included a total of 336 individual statistical analyses investigating the relationships between personality characteristics and HRQOL.
Table 1. Characteristics of reviewed studies of personality characteristics and HRQOL.
| Author [Reference #] | Country | Disease-specific population | Sample Size | SD | Personality trait | Personality measure | HRQL domain | HRQL measure |
|---|---|---|---|---|---|---|---|---|
| Badura-Brzoza et al [22] | Poland | Total hip replacement | 102 | CO | State and trait anxiety, sense of coherence, neuroticism, and extraversion | STAI, SOC, and EPI | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-36 |
| Bartoces et al [23] | USA | Cervical cancer | 145 | CS | Self esteem | RSE | Generic (PCS, and MCS) | SF-36 |
| Dubayova et al [24] | Slovakia | Parkinson's disease |
153 | CS | Type D personality and negative affectivity | DS-14 | Condition-specific (overall QOL, mobility, activities of daily living, emotional well-being, stigma, social support, cognition, communication, and bodily discomfort) | PDQ-39 |
| Dubayova et al [25] | Slovakia | Parkinson's disease | 153 | CS | Neuroticism and extraversion | EPQ-R | Condition-specific (mobility, activities of daily living, emotional well-being, stigma, social support, cognition, communication, and bodily discomfort) | PDQ-39 |
| Kall et al [26] | Sweden | Whiplash associated disorders | 40 | CO | Self-efficacy | SES | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-12 |
| Kobayashi et al [27] | Japan | Cervical cancer | 60 | CS | Self-esteem | RSE | Condition-specific (physical, social/family, emotional, and functional) | FACT-G |
| Kvarme et al [28] | Norway | School children | 279 | CS | Self-efficacy | GSE | Generic (physical well-being, emotional well-being, self-esteem, and friends) | KINDL |
| Siassi et al [29] | Germany | Post major colorectal surgery | 79 | CO | Neuroticism, extraversion, agreeableness, and sense of coherence | NEO-FFI and SOC | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) Condition-specific (overall QOL) | SF-36 and GLQI-39 |
| Tsaousides et al [30] | USA | Adults under 65 with traumatic brain injury | 425 | CS | Self-efficacy | IND/BBQ | Overall QoL | LLATBI |
| Visser-Meily et al [31] | Netherlands | Post aneurysmal subarachnoid hemorrhage | 141 | CS | Neuroticism | EPQ | Condition-specific (emotional functioning) | SSQOL |
| Warrian et al [32] | USA | Glaucoma | 147 | CS | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | NEO-PI-R | Condition-specific (overall QOL, general vision, mental health, social functioning, role limitation, and ocular pain) | VFQ |
| Aarstad et al [33] | Norway | Head and neck squamous cell carcinoma | 55 | CO | Neuroticism, extraversion, and lie | EPI | Condition-specific (global QOL, functioning scale, cancer symptom scale, and head and neck cancer symptom scale) | EORTC QLQ-H&N35 and EORTC-QLQ-C30 |
| Boye et al [34] | Norway | Ulcerative colitis and Crohn's disease | 110 | CS | Aggression, alexithymia, neuroticism, and lie | BPA, EPQ, and TAS | Condition-specific (overall QOL, emotional functioning, social functioning, systemic symptoms, and bowel functioning) | IBDQ |
| Boye et al [35] | Norway | Ulcerative colitis and Crohn's disease | 109 | CS | Aggression, alexithymia, neuroticism, and lie | BPA, EPQ, and TAS | Generic (BP, PF, RP, RE, MH, SF, VT, and GH) | SF-36 |
| De Bolle et al [36] | Belgium | Children with cancer | 54 | CS | Neuroticism, extraversion, imagination, benevolence, and conscientiousness | HiPIC | Generic (overall QOL, PF, EF, SF, and SC) | PedsQL 4.0 |
| Jerant et al [37] | USA | Chronic conditions | 245 | CS | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | NEO-FFI | Generic (overall QOL, mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) | EQ-5D |
| Aquarius et al [38] | Netherlands | Peripheral arterial disease | 150 | CS | Type D personality | DS-14 | Generic (overall QOL, physical health, and level of independence) | WHOQOL-100 |
| Aquarius et al [39] | Netherlands | Peripheral arterial disease | 203 | CO | Type D personality | DS-14 | Generic (BP, PF, RP, RE, MH, SF, VT, and GH) | RAND-36 |
| Chapman et al [40] | USA | Elderly | 442 | CS | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | NEO-FFI and SOC | Generic (SF, RE, RP, and PF) | SF-36 |
| Cohen et al [41] | Israel | Adolescents with heart disease | 173 | CS | Self esteem | RSE | Condition-specific (limitations) | TAAQOL-CHD |
| Karlsson et al [42] | Sweden | Coronary artery disease | 224 | CO | Type D personality, sense of coherence, and negative affectivity | DS-24 and SOC | Generic (overall QOL) | Cantril Ladder of Life |
| Middleton et al [43] | Australia | Spinal cord injuries | 106 | CS | Self-efficacy | Moorong and SES | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-36 |
| Moreno-Jimenez et al [44] |
Spain | Crohn's disease and ulcerative colitis | 120 | CS | Neuroticism | EPI-N and RSE | Condition-specific (overall QOL, emotional function, social function, systemic symptoms, and bowel function) | IBDQ |
| Pedersen et al [45] | Netherlands | Post implantation of cardiverter-defibrillator | 154 | CO | Type D personality | DS-14 | Generic (BP, PF, RP, RE, MH, SF, VT, and GH) | SF-36 |
| van der Steeg et al [46] | Netherlands | Breast disease | 202 | CO | Neuroticism, extraversion, openness, and state-trait anxiety | NEO-PI-R and STAI | Generic (overall QOL, physical health, psychological health, and social relationships) | WHOQOL-100 |
| Arnold et al [47] | Netherlands | Chronic obstructive pulmonary disease | 39 | CO | Self-efficacy | Sullivan and SES | Generic (PF, MH, SF, and overall) | SF-36 and Cantril Ladder or Life |
| Friedman et al [48] | USA | Breast cancer | 81 | CS | Optimism | LOT | Condition-specific (physical well-being, emotional well-being, and functional well-being) | FACIT-G |
| Hantash et al [49] | Palestine | Teeth implant | 50 | CO | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | NEO-FFI | Condition-specific (overall QOL, appearance, pain, oral comfort, general performance, and eating ability) | DIDL |
| Ong et al [50] | Canada | Atrial fibrillation | 93 | CS | Optimism |
LOT | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-36 |
| Pedersen et al [51] | Netherlands | Heart transplantation | 188 | CS | Type D personality | DS-14 | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-36 |
| Aquarius et al [52] | Netherlands | Peripheral arterial disease | 300 | CS | Type D personality | DS-14 | Generic (overall QOL,physical health, and level of independence) | WHOQOL-100 |
| van den Berg et al [53] | Netherlands | Paroxysmal atrial fibrillation | 73 | CS | Neuroticism | EPQ-R | Generic (BP, PF, RP, RE, MH, SF, VT, and GH) | SF-36 |
| Vollrath et al [54] | Norway | Pediatric patients with unintentional injuries | 107 | CO | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | HiPIC | Generic (overall QOL, physical complaints, motor functioning, autonomy, cognitive functioning, social functioning, positive emotions, and negative emotions) | TACQOL |
| Zhang et al [55] | China | Liver transplant candidates | 55 | CS | Neuroticism, extraversion, psychoticism, and lie | EPQ | Generic (physical, material, social, and psychological well-being) | GQOLI-74 |
| De Clercq et al [56] | Belgium | Pediatric cancer survivors | 67 | CS | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | HiPIC | Generic (overall QOL, physical functioning, emotional functioning, social functioning, and school functioning) | PedsQL 4.0 |
| Sears et al [57] | USA | Implantable cardioverter defibrillator | 88 | CO | Optimism | LOT | Generic (MH, SF, and GH) | SF-36 |
| Wittkowski et al [58] | UK | Atopic dermatitis | 125 | CS | Self esteem | RSES | Condition-specific (work, leisure, relationships, daily activities and treatment) | DLQI |
| Aarstad et al [59] | Norway | Head and neck squamous cell carcinoma | 96 | CS | Neuroticism, extraversion, and lie | EPI | Condition-specific (global QOL, functioning scale, cancer symptom scale, and head and neck cancer symptom scale) | EORTC QLQ-H&N35 and EORTC-QLQ-C30 |
| Duberstein et al [60] | USA | Aging primary care patients | 265 | CS | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | NEO-FFI | Generic (PF, GH) | SF-36 |
| Han et al [61] | Korea | Chronic conditions | 1748 | CS | Self-efficacy and self-esteem | RSE and SES | Generic (physical, psychological, and socio-economic) | Ro's |
| Penedo et al [62] |
USA | HIV/AIDS | 116 | CS | Neuroticism, extraversion, openness, agreeableness, and conscientiousness | NEO-PI-R | Condition-specific (overall function, life satisfaction, medical worries, financial worries, medication worries, HIV master, disclosure worries, provider trust, and sexual functioning) | HAT-QOL |
| Cormier et al [63] | France | Prostate cancer screening | 334 | CS | Trait-anxiety | STAI | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-36 |
| Goodwin et al [64] | USA | General population | 3606 | CS | Neuroticism, extraversion, conscientiousness, openness, and agreeableness | MIDI | Generic (overall subjective health perception) | Newly-developed health perception scale |
| Rose et al [65] | Germany | Diabetes | 625 | CS | Optimism | SWOP | Generic (overall QOL) | WHOQOL-BREF |
| Wasylkiw et al [66] | Canada | Psychology students | 350 | CS | Neuroticism, extraversion, conscientiousness, openness, and agreeableness | NEO-PI | Generic (PF, RP, RE, MH, SF, VT, and GH) | SF-36 |
| Cederfjall et al [67] | Sweden | HIV | 189 | CS | Sense of coherence | SOC | Generic (overall QOL) and condition-specific (HIV symptoms) | HI and self-developed HIV symptom Scale |
| Kressin et al [68] | USA | General population | 691 | CS | Negative affectivity | EPI-Q | Condition-specific (oral HRQOL, psychosocial functioning, physical functioning, and pain) | OHQOL, OHIP, and GOHAI |
| Tanum et al [69] | Norway | Functional gastrointestinal disorder | 111 | CS | Neuroticism, extraversion, conscientiousness, openness, and agreeableness, and hostility | EPQ and NEO-PI | Generic (pain) | McGill Pain Questionnaire |
| Achat et al [70] | USA | General population | 659 | CO | Optimism | LOT | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-36 |
| Allison et al [71] | France | Head and neck cancer | 101 | CO | Optimism | LOT | Condition-specific (overall QOL, functioning scale, and symptom scale) | EORTC-QLQ-C30 |
| Burgess et al [72] | UK | HIV seropositive | 279 | CS | Neuroticism, extraversion, and psychoticism | EPQ-R | Condition-specific (role functioning, physical functioning, health distress, and mental health) | MOS-HIV |
| Canizares et al [73] | Spain | Epilepsy | 33 | CO | Neuroticism | EPQ-A | Condition-specific (cognitive functioning) | QOLIE-31 |
| Denollet et al [74] | Holland | Coronary heart disease | 319 | CO | Type D personality | DS-16 | Generic (perceived health symptoms and disability) | HCS and GMS |
| Fritz [75] | USA | Heart attack or check pain | 65 | CO | Agency, communion, and unmitigated communion | PAQ and HUCS | Generic (MCS and PCS) | SF-36 |
| Kempen et al [76] | Holland | Congestive heart failure and acute myocardial infarction | 213 | CS | Neuroticism | EPQ-R | Generic (functional disability | GARS |
| Kressin et al [77] | USA | General population | 1629 | CS | Negative affectivity | EPI-Q | Generic (BP, PF, RP, RE, MH, SF, VT, GH, PCS, and MCS) | SF-36 |
| Nesbitt et al [78] | USA | Elderly | 137 | CS | Sense of coherence | SOC | Generic (Overall QOL) | Ferrans and Power Quality of Life Index-General Version |
| Spiro III et al [18] | USA | General population | 1257 | CS | Extraversion | EPI-Q | Generic (PF, RP, BP, GH, VT, SF, RE, MH) and condition-specific (cognitive functioning) | SF-36 and MHI |
| Scott et al [79] | USA | Orthognathic surgery | 117 | CO | Neuroticism | EPI-Q | Generic (psychosocial scale) and condition-specific (general oral health, effect on work and social activities, oral esthetics, pain/sensitivity, and oral functioning) | SIP and OHSQ |
| Yamaoka et al [80] | Japan | Stomach cancer | 828 | CS | Neuroticism, extraversion, and psychoticism | EPQ | Generic (positive and negative HRQOL) | HRQOL-20 (Japanese version) |
| Zhu et al [81] | China | Epilepsy | 201 | CS | Neuroticism, extraversion, and psychoticism | EPQ | Generic (general physical health) | General well-being Schedule |
| Carr et al [82] | Australia | Earthquake victims | 845 | CO | Neuroticism, and extraversion | EPI | Generic (psychological distress) | GHQ-12 |
| Hollifield et al [83] | USA | Panic attack | 123 | CS | Neuroticism | NEO-FFI | Generic (PF, MH, and GH) | SF-36 |
| Kempen et al [84] | Holland | Elderly | 5279 | CS | Neuroticism | EPQ-R | Generic (PF, RF, SF, HP, BP, and MH) | SF-20 |
| Wettergren et al [85] | Sweden | Malignant blood disorders | 20 | CO | Sense of coherence | SOC | Condition-specific (overall QOL, functioning scale, and symptom scale) | EORTC-QLQ-C30 |
| Chen et al [86] | UK | Suspicion of breast cancer | 121 | CO | Neuroticism and extraversion | EPI | Generic (psychological distress) | GHQ-12 |
| Joukamaa et al [87] | Finland | Elderly | 190 | CO | Alexithymia | TAS-26 | Generic (psychological distress) | GHQ-32 |
| Kempen et al [88] | Holland | Elderly | 624 | CO | Neuroticism, extraversion | EPQ | Generic (motor, hearing, and vision functioning) | OECD indicator, HHDI-D, and a self-developed scale for vision. |
| Kempen et al [89] | Holland | Elderly | 753 | CO | Neuroticism, extraversion, and mastery | EPQ | Generic (functioning activity) | GARS-ADL subscale |
| Hidding et al [90] | Holland | Ankylosing spondylitis | 67 | CO | Neuroticism | DPI | Generic (global health) | SIP, HAQ-S, Functional Index for Ankylosing spondylitis, and self-developed hospital visual analogue scale |
| Carver et al [91] | USA | Breast cancer | 70 | CO | Optimism | LOT | Generic (subjective well-being, sex quality, and pain) | Profile of Mood States, Life Satisfaction Scale, Quality of Sex Life, and self-developed pain scale |
| Hidding et al [92] | Holland | Ankylosing spondylitis | 144 | CS | Neuroticism | DPI | Generic (overall QOL) and Condition-specific (activities of daily living, physical functioning, and psychosocial functioning) | SIP, HAQ-S, and SAF |
| Jorm et al [93] | Australia | Elderly | 711 | CS | Neuroticism and extraversion | EPQ-R | Generic (Overall QOL, physical functioning, vision, hearing, pain, activity of daily living, and symptom) | Self-developed scales |
| Hooker et al [94] | USA | Caregivers of Alzheimer disease or dementia | 51 | CS | Neuroticism and optimism | NEO-FFI and LOT | Generic (mental and physical HRQOL) | Bradbun Affect Balance, HPQ- Current Health Subscale, self-developed health index, and MAI |
| Wilson et al [95] | UK | Globus sensation | 46 | CS | Neuroticism, extraversion, and lie | EPI | Generic (psychological distress) | GHQ-60 |
| Scheier et al [96] | USA | Psychology students | 141 | CO | Optimism | LOT | Generic (physical symptoms) | Physical Symptom Checklist- 39 |
SD: Study Design.
CO: cohort study.
CS: cross-sectional study.
Personality Measures.
BPA: Buss-Perry Aggression Questionnaire.
DPI: Dutch Personality Inventory.
DS-14: Type D Scale 14.
DS-16: Type D Scale 16.
DS-24: Type D Scale 24.
EPI: Eysenck Personality Inventory.
EPI-Q: Short form of Eysenck Personality Inventory Emotional Stability Scale.
EPQ: Eysenck Personality Questionnaire.
EPQ-A: Eysenck Personality Questionnaire – Spanish Adult version.
EPQ-R: Eysenck Personality Questionnaire Revised.
GSE: Generalized Self-Efficacy Scale.
HiPIC: Hierarchical Personality Inventory for Children.
HUCS: Helgeson’s Unmitigated Communion Scale.
IND/BBQ: Independence (IND) subscale of the Bigelow Quality of Life Questionnaire (BBQ).
LOT: The Life Orientation Test.
MIDI: Midlife Development Inventory Personality Scales.
NEO-PI: The Neuroticism, Extraversion and Openness Personality Inventory.
NEO-PI-R: The Neuroticism, Extraversion and Openness Personality Inventory Revised.
NEO-FFI: The Neuroticism, Extraversion and Openness Five-Factor Inventory- short version.
PAQ: Personal Attributes Questionnaire.
RSE: Rosenberg Self Esteem scale.
SES: Self-Efficacy Scale.
SOC: Antonovsky’s Sense of Coherence Questionnaire.
STAI: State and Trait Anxiety Inventory.
SWOP: The Assessment of Beliefs in Self-Efficacy and Optimism.
TAS: Toronto Alexithymia Scale.
HRQOL Measures
DIDL: Dental Impact on Daily Living.
EORTC-QLQ-C30: European Research and Treatment of Cancer Quality of Life Core Questionnaire.
EORTC-QLQ-H&N35: European Research and Treatment of Cancer Quality of Life Questionnaire module for patients with head and neck cancer.
EQ-5D: EuroQol-5 Dimension questionnaire.
FACIT-G: The Functional Assessment of Chronic Illness Therapy-General.
GARS: Groningen Activity Restriction Scale.
GHQ-12/GHQ-32/GHQ-60: General Health Questionnaire 12-/ 32-/60-item versions.
GOHAI: Geriatric Oral Health Assessment Instrument.
GLQI-39: Gastrointestinal Quality of Life Index.
GMS: Global Mood Scale.
GQOLI-74: General Quality of Life Inventory.
HAQ-S: Health Assessment Questionnaire for the Spondyloarthropathies
HAT-QOL: The HIV/AIDS-Targeted Quality of Life Instrument.
HCS: The Health Complaints Scale.
HHDI-D: Hearing Handicap and Disability Inventory – Disability Subscale.
HI: Health Index.
HPQ: Health Perceptions Questionnaire.
HRQOL-20: Health Related Quality of Life questionnaire.
IBDQ: Inflammatory Bowel Disease Questionnaire
KINDL: A generic instrument for assessing HRQOL in children and adolescents.
LLATBI: The Living Life After Traumatic Brain Injury.
MAI: Multilevel Assessment Instrument.
MHI: Mental Health Index.
MOS-HIV: Medical Outcomes Study-HIV Health Survey.
OHIP: Oral Health Impact Profile.
OHQOL: Oral Health Related Quality of Life.
OHSQ: Oral Health Status Questionnaire.
PedsQL 4.0: Pediatric Quality of Life Inventory version 4.0.
PDQ-39: Parkinson’s Disease Questionnaire.
QOLIE-31: Quality of Life in Epilepsy Inventory.
RAND-36: RAND 36-Item Health Survey.
SAF: Self-Assessed Function questionnaire.
SF-20/SF-36: The Short Form 20-Item/36-Item Health Survey.
SIP: Sickness Impact Scale.
SSQOL: Stroke-Specific Quality of Life.
TACQOL: TNO-AZL Children’s Quality of Life questionnaire.
VFQ: National Eye Institute's Visual Function Questionnaire.
WHOQOL-100: World Health Organization Quality of Life Assessment.
HRQOL Domains of the SF-36/ RAND-36/SF-20.
PF: Physical functioning.
RP: Role limitation due to physical problems.
BP: Bodily pain.
GH: General health perceptions.
VT: Vitality
SF: Social functioning.
RE: Role limitation due to emotional problems.
MH: Mental health.
Among personality measures, 45 studies (59%) assessed neuroticism (including negative affectivity) using either the Eysenck Personality Inventory/Questionnaire (EPI/EPQ), the NEO-Personality Inventory (NEO-PI), the NEO Five-Factor Inventory (NEO-FFI), the Dutch Personality Inventory (DPI), HiPIC, MIDI, DS-14, or DS-24; 29 (38%) assessed extraversion, and 9 assessed optimism (12%) (Table 1). Other personality characteristics that were included by >5 studies were openness to experience, agreeableness, conscientiousness, self-esteem, self-efficacy, and Type D personality. S1 Appendix summarizes the definitions of personality dimensions, the corresponding traits, and tools to assess personality traits.
Regarding HRQOL measures, 23 studies (30%) used generic and condition-specific measures derived from the Medical Outcomes Studies (MOS), including the SF-36/SF-20 (21 studies), the RAND-36 (one study), and the MOS-HIV (one study). Of other generic measures, 4 studies (5%) used the General Health Questionnaire, 3 (4%) used the Sickness Impact Profile (SIP), and 4 (5%) used the World Health Organization Quality of Life Assessment Instrument (WHOQOL). Of other condition-specific measures, 4 studies (5%) used the European Research and Treatment of Cancer Quality of Life Questionnaire (EORTC-QLQ) (Table 1).
Relationships between personality characteristics and HRQOL
All of the studies found the relationships between specific personality characteristics and HRQOL to be in the same direction. For example, greater extraversion, agreeableness, openness, conscientiousness, optimism, self-esteem, self-efficacy, and sense of coherence were all related to better HRQOL, while greater neuroticism, negative affectivity, and type D personality were related to poorer HRQOL (Table 2).
Table 2. Relationships between personality dimension, single personality trait, and HRQOL.
| Personality dimensions | Overall or global QOL | General health perception | Psychological functioning | Physical functioning | Role functioning | Social functioning | Other specific functioning | Vitality | Bodily pain | Somatic symptom |
|---|---|---|---|---|---|---|---|---|---|---|
| Agreeableness |
● [56]‡ ○ [32]‡, [36]‡, [37]‡ |
● [64]‡ ○ [64]‡ , [60]‡ |
○ [32]‡, [36]‡ |
○ [36]‡, [40]‡ [60]‡ |
○ [32]‡, [40]‡ |
● [36]‡, ○ [32]‡, [40]‡ |
○ [32]‡, [36]‡ |
● [49]‡ ○ [32]‡ |
||
| Conscientiousness |
● [32]‡, ○ [36]‡, [37]‡, [56]‡ |
● [64]‡ ○ [60]‡ |
○ [32]‡, [36]‡ |
○ [36]‡, [40]‡ [60]‡ |
● [40]‡
○ [32]‡ |
○ [32]‡, [36]‡, [40]‡ |
● [32]‡ ○ [36]‡ |
○ [32]‡ | ||
| Extraversion |
● [32]‡, [81]‡
○ [25]‡, [36]‡, [37]‡, [56]‡ |
● [64]‡
○ [60]‡ |
○ [22]‡, [25]‡, [36]‡, [64]‡, [72]‡, [18]‡, [82]‡, [86]‡ |
● [18]‡, ○ [22]‡, [25]‡, [36]‡, [40]‡, [72]‡ [60]‡ |
○ [32]‡, [40]‡ |
● [32]‡
○ [25]‡, [36]‡, [40]‡ |
● [25]‡, [88]‡, ○ [25]‡, [32]‡, [36]‡, [88]‡ |
○ [25]‡, [32]‡ | ||
| Neuroticism |
● [25]‡, [33]†‡, [34]‡, [37]‡, [56]‡, [79]‡, [81]‡, [92]‡ ○ [32]‡, [36]‡, [90]‡ |
● [53]‡, [64]‡, [83]‡, [84]‡ [60]‡ ○ [35]‡, [36]‡ |
● [22]‡, [25]‡, [31]‡, [32]‡, [34]‡, [35]‡, [44]‡, [53]‡, [63]‡, [18]‡, [82]‡, [83]‡, [84]‡, [86]‡, [25]‡, [33]‡ ○ [22]‡, [36]‡ |
● [22]‡, [18]‡, [94]‡ ○ [22]‡, [25]‡, [35]‡, [36]‡, [40]‡, [53]‡, [72]‡, [76]‡, [83]‡, [84]‡ [60]‡ |
● [40]‡ ○ [32]‡, [35]‡, [53]‡, [84]‡ |
● [25]‡, [40]‡, [44]‡, [53]‡, [84]‡ ○ [32]‡, [34]‡, [35]‡, [36]‡ |
● [25]‡, [33] †‡, [44]‡, [59]†, [73]‡, [79]‡, [88]‡
○ [25]‡, [32]‡, [34]‡, [36]‡, [88]‡ |
● [35]‡ ○ [53]‡ |
● [25]‡, [33]†‡, [84]‡ ○ [32]‡, [53]‡, [69]‡ |
● [33]†‡, [44]‡, [59]† ○ [34]‡ |
| Openness to experience |
● [56]‡ ○ [32]‡, [36]‡, [37]‡ |
● [64]‡
○ [60]‡ |
○ [32]‡, [36]‡, |
● [60]‡ ○ [36]‡, [40]‡ |
○ [32]‡, [40]‡ |
● [40]‡ ○ [32]‡, [36]‡ |
● [36]‡ ○ [32]‡ |
○ [32]‡ | ||
| Psychoticism | ● [81]‡ | |||||||||
| %, significant results | 46% | 50% | 50% | 17% | 15% | 36% | 29% | 50% | 33% | 75% |
| Single Personality Trait | ||||||||||
| Agency | ● [75]‡ | ○ [75]‡ | ||||||||
| Aggression | ○ [34]‡ | ○ [34]‡, [35]‡ | ● [35]‡ | ○ [34] ‡ | ○ [34]‡ | ● [69]‡ | ○ [34]‡, | |||
| Alexithymia | ○ [34] ‡ | ○ [34]‡, [35]‡, [87]‡ | ● [35]‡ | ● [35]‡ |
● [35]‡ ○ [34]‡ |
○ [34]‡ | ○ [35]‡ | ● [87]‡ | ||
| Communion | ○ [75]‡ | ○ [75]‡ | ||||||||
| Dispositional optimism | ● [65]‡, [71]‡ |
● [70]‡ ○ [57]† |
● [48]‡, [50]‡, [57]†, [70]‡, [71]‡ ○ [94]‡ |
○ [50]‡, [70]‡, [71]‡, [94]‡ |
● [94]‡ ○ [70]‡ |
● [48]‡, [57]†, ○ [70]‡, [71]‡ |
● [48]‡
○ [71]‡ |
● [70]‡ | ● [70]‡, [71]‡ | ● [71]‡ |
| Hopefulness | ● [82]‡ | |||||||||
| Lie | ● [34]‡ | ○ [22]‡, [34]‡ |
● [35]‡ ○ [22] |
○ [35]‡ | ●[34]‡ | ○ [34]‡ | ○ [35]‡ | ○ [34]‡ | ||
| Negative affectivity | ● [68]‡ | ● [77]‡ | ● [68]‡, [77]‡ |
● [68]‡
○ [77]‡ |
● [77]‡ | ● [68]‡, [77]‡ | ● [68]‡ | ● [77]‡ | ● [68]‡, [77]‡ | |
| Self-efficacy | ● [26]‡, [28]‡ | ● [43]† | ● [43]†, [44]‡, [28]‡ |
● [43]†, [28]‡ |
● [43]† |
● [43]†, [28]‡ ○ [44]‡ |
● [44]‡ | ● [43]† | ● [43]† | |
| Self-esteem |
● [27]†, [41]‡, ○ [58]‡ |
●[23]‡, [27]† | ○ [23]‡, [27]† | ● [27]† | ||||||
| Sense of Coherence | ● [67]‡, [78]‡ | ● [42]† |
● [22]‡
○ [22]‡ |
● [22]‡
○ [22]‡ |
● [67]‡, | |||||
| Trait-anxiety | ● [46]‡ | ● [63]‡ |
● [22]‡, [46]‡, [63]‡ ○ [36]‡ |
● [22]‡, [46]‡
○ [22]‡, [63]‡ |
○ [63]‡ | ● [46]‡, [63]‡ | ● [63]‡ | ○ [63]‡ | ||
| Type-D | ● [24]‡, [38]^, [45]†, [52]^, [74]^ |
● [39]†, [42]† ○ [51]^ |
● [24]‡, [39]†, [51]^, [74]‡ |
● [38]^, [51]^, [52]^
○ [24]‡, [39]† |
● [39]†, [51]^ | ● [24]‡, [39]†, [51]^ | ● [24]‡, [38]^, [52]^ | ● [39]†, [51]^ |
● [39]†, ○ [24]‡, [51]^ |
|
| Unmitigated communion | ○ [75]‡ | ○ [75]‡ | ||||||||
| %, significant results | 84% | 78% | 65% | 39% | 70% | 74% | 60% | 86% | 64% | 60% |
● Statistically significant.
○ Not statistically significant.
† t-test/ ANOVA.
‡ Multivariate regression analysis.
^ Multivariate (odds ratio) analysis.
The level of significance of the relationships between personality and HRQOL varied depending upon the type of personality characteristics and domains of HRQOL measured (Table 2). A total of 75% of the statistical analyses showed significant associations between personality characteristics and vitality, 54% with social functioning, and 58% with psychological functioning. Only 28% of analyses showed significant associations with physical functioning (Table 2). A total of 60% of analyses showed significant associations with general health perception, and 57% with overall quality of life (Table 2).
The magnitude of correlation coefficients (in absolute value) between personality and specific domains of HRQOL ranged from 0.04 to 0.74; the magnitude of effect sizes (in absolute value) between personality and the specific domain of HRQOL ranged from 0 to 4.2 (Table 3). Studies consistently showed that personality characteristics were more likely to be associated with psychosocial aspects (e.g. psychological functioning, vitality, and social functioning) than physical aspects of HRQOL (e.g. physical functioning, role limitation due to physical problems, or bodily pain) (Table 3). For the MOS questionnaires, the correlation coefficients (in absolute value) of personality characteristics with mental component scores (MCS) were larger than with physical component scores (PCS); 0.29–0.64 versus 0.28–0.34.
Table 3. The strength of relationships between personality characteristics and HRQOL.
| Personality characteristics | Correlation coefficient¶ | Effect size§ | ||
|---|---|---|---|---|
| Agency [75] | • PCS | • 0.28 | ||
| Aggression [34, 35] | • Psychological functioning • Role limitation- emotional • Social functioning • Overall QOL |
• 0.26-0.43 (0.33) • 0.38 • 0.24 • 0.24-0.31 |
||
| Agreeableness [29, 40, 49, 54, 60, 66] | • General health perceptions • Role limitation- physical • Role limitation- emotional • Social functioning • PCS • MCS • Overall QOL • Oral functioning |
• 0.10 • 0.13 • 0.22 • 0.18 • 0.32-0.34 • 0.37 • 0.18-0.22 • 0.35 |
||
| Alexithymia [34, 35] | • Physical functioning • Role limitation- physical • Psychological functioning • Role limitation- emotional • Vitality • Social functioning |
• 0.33 • 0.29 • 0.26-0.49 • 0.25 • 0.25 • 0.30 |
||
| Conscientiousness [32, 40, 54, 60, 62, 66] | • Physical functioning • Role limitation- physical • Psychological functioning • Role limitation- emotional • General health perceptions • Social functioning • Overall QOL • Cognitive functioning • HIV functioning • Sexual functioning • Visual functioning |
• 0.18 • 0.19-0.28 • 0.27 • 0.22-0.29 • 0.16-0.24 • 0.21-0.26 • 0.24-0.25 • 0.28 • 0.20 • 0.22 • 0.19 |
• Role limitation- physical | • 0.12 |
| Extraversion [18, 29, 40, 55, 59, 60, 62, 66, 80, 81, 82, 88, 93] | • Physical functioning • Role limitation- physical • Psychological functioning • Role limitation- emotional • General health perceptions • Bodily pain • Vitality • Social functioning • MCS • Overall QOL • Cognitive functioning • HIV functioning • Sexual functioning • Visual functioning • Hearing functioning |
• 0.12-0.39 (0.26) • 0.16-0.25 • 0.18-0.26 (0.20) • 0.10-0.26 • 0.17-0.21 • 0.08-0.15 (0.15) • 0.25 • 0.08-0.29 (0.28) • 0.32-0.50 (0.46) • 0.10-0.47 (0.27) • 0.19 • 0.30 • 0.31 • 0.10 • 0.12 |
||
| Mastery [89] | • Performance-based measure | • 0.20 | ||
| Negative affectivity [77] | • Physical functioning • Psychological functioning |
• 0.17 • 0.67 |
• Role limitation- physical • Psychological functioning • Role limitation- emotional • General health perceptions • Bodily pain • Vitality • Social functioning • MCS |
• 0.14-0.20 • 0.25-0.50 (0.44) • 0.16-0.30 (0.27) • 0.12-0.14 • 0.06-0.21 • 0.15-0.18 • 0.16-0.17 • 0.22-0.43 (0.37) |
| Neuroticism 25, 29, 31-35, 37, 40, 44, 49, 54, 55, 59, 60, 62, 66, 73, 80-84, 86, 88, 92-95] | • Physical functioning • Role limitation- physical • Psychological functioning • Role limitation- emotional • General health perceptions • Bodily pain • Vitality • Social functioning • MCS • Overall QOL • Role functioning • Cognitive functioning • Oral functioning • HIV functioning • Hearing functioning • Visual functioning • Sexual functioning |
• 0.12-0.39 (0.28) • 0.10-0.33 (0.24) • 0.21-0.67 (0.53) • 0.12-0.47 (0.28) • 0.17-0.54 (0.32) • 0.23-0.46 (0.31) • 0.20-0.48 (0.37) • 0.14-0.44 (0.29) • 0.44-0.58 (0.48) • 0.04-0.71 (0.33) • 0.13-0.40 (0.21) • 0.23-0.55 (0.45) • 0.40-0.54 • 0.39 • 0.10-0.24 • 0.23-0.27 • 0.27 |
• Physical functioning • Psychological functioning • Role limitation- emotional • General health perceptions • Social functioning • Overall QOL |
• 0 • 1.4 • 0.34 • 0.6 • 0.22 • 0.16 |
| Psychoticism [55, 81] | • Psychological functioning • Overall QOL |
• 0.40 • 0.40 |
||
| Self-efficacy [26, 28, 30, 43, 61] | • Overall QOL • Physical functioning • Social functioning • Psychological functioning • Bodily pain • Role functioning • Vitality • General Health • Somatic Symptom • PCS/MCS |
• 0.39-0.40 • 0.54 • 0.64 • 0.41 • 0.38 • 0.41-0.43 • 0.60 • 0.64 • 0.40 • 0.64-0.68 |
• Physical functioning • Psychological functioning • Social functioning |
• 0.21 • 0.26 • 0.30 |
| Self-esteem [23, 41, 58, 61] | • Overall QOL | • 0.35-0.47 (0.38) | • MCS | • 0.11 |
| Sense of coherence [29, 78, 85] | • Physical functioning • Role functioning • Social functioning • MCS • Overall QOL |
• 0.40-0.68 • 0.46 • 0.62-0.64 • 0.56-0.64 (0.61) • 0.42-0.74 (0.58) |
||
| Openness [40, 54, 60] | • Physical functioning • Role limitation- emotional • Social functioning • Cognitive functioning |
• 0.11-0.13 • 0.17 • 0.20 • 0.33 |
• Social functioning | • 0.16 |
| Optimism [48, 50, 70, 91, 94, 96] | • Physical functioning • Psychological functioning • Social functioning • PCS • MCS |
• 0.22-0.54 (0.31) • 0.37- 0.55 (0.37) • 0.40 • 0.30 • 0.38-0.50 (0.45) |
• Physical functioning • Role limitation- physical • Psychological functioning • Role limitation- emotional • General health perceptions • Bodily pain • Vitality • Social functioning • PCS • MCS |
• 0.01-1.60 • 0.01-1.70 • 0.03-2.40 • 0.03-2.20 • 1.80-4.21 • 1.72-2.00 • 2.40-2.61 • 0.01-1.90 • 1.60 • 2.50 |
| Lie [55] | • Psychological functioning | • 0.32 | ||
| Unmitigated communion [75] | • MCS | • 0.29 | ||
¶ Correlation coefficient reported for statistically significant results; absolute value reported; median reported in parentheses (where available).
§ Effect size = unit change in HRQOL scores for 1 standard deviation unit change in personality variable; absolute value reported; median reported in parentheses (where available)
Examination of specific personality characteristics suggested that neuroticism, negative affectivity, and sense of coherence were more likely than other characteristics to correlate with psychosocial aspects of HRQOL. Neuroticism and sense of coherence were moderately correlated with MCS, with absolute correlation coefficients of 0.44–0.58 and 0.56–0.64, respectively. There was a strong correlation between sense of coherence and social functioning and between negative affectivity and psychological functioning, with absolute correlation coefficients 0.62–0.64 and 0.67, respectively. In contrast, the correlation coefficients of agreeableness, extraversion, and optimism with MCS were 0.37, 0.32–0.50, and 0.38–0.50, respectively.
Self-ratings vs. proxy-ratings of HRQOL
Personality characteristics were more likely to be associated with self-ratings of HRQOL than proxy-ratings of HRQOL [88, 89, 93]. For example, Kempen et al. showed that the significant association between the patient’s self-rating of dressing/getting around the house and mastery was maintained after adjusting for the proxy-rating of motor and hearing functioning [89]. Personality characteristics were also associated with a discrepancy between self- and proxy-ratings of HRQOL [88, 89]. For example, patients with lower mastery and extraversion were also likely to report lower scores in self-rating of dressing, getting around the house, and standing, compared to proxy-ratings [89].
Impact on the change of HRQOL
This review study includes 27 studies that collected data across multiple time points. However, only three studies investigated if personality at baseline can predict the change in HRQOL over time, and the remaining 24 studies measured HRQOL at a follow-up time point alone. These three studies found that personality can influence the change of HRQOL. Aquarius et al. found that among patients with peripheral arterial disease, type-D personality was related to more impaired HRQOL over time than those with non-type-D personality [39]. Allison et al. found that cancer patients who were optimistic were more likely to improve their global and role HRQOL than their pessimistic counterparts [71]. Interestingly, Hidding et al. reported that after group physical therapy, ankylosing spondylitis patients with low self-esteem tended to improve more in global HRQOL than those with high self-esteem [90].
Significant associations of other factors with HRQOL
Personality characteristics were stronger determinants of HRQOL than sociodemographic factors such as age [67], social integration [78] and income [78] as well as clinical factors such as comorbidity [78], CD4+ counts and HIV disease stage [67, 72] and seizure outcome after epilepsy surgery [73].
Specific effects of personality characteristics on HRQOL
Personality characteristics had indirect, mediating, and moderating effects on different aspects of HRQOL (Table 4). Eight studies [33, 50, 65, 72, 75, 78, 79, 94] provided evidence that personality characteristics were indirectly associated with HRQOL, that is, personality characteristics affected HRQOL through another variable, such as coping style [33, 72], social support [72], stress [94], and doctor-patient relationships [65]. One study found that the effects of physical disability on HRQOL were mediated by sense of coherence [78]. Three studies [71, 82, 84] examining moderating effects of personality on HRQOL demonstrated that personality could modify the effects (or strength of the effect) of other variables on HRQOL. Neuroticism modified the effect of an earthquake stressor on psychological distress [82] and the effects of chronic conditions on physical and social functioning [84]. Optimism modified the effect of duration of disease on overall QOL and role functioning [71].
Table 4. Specific effect of personality characteristics on HRQOL.
| Personality characteristics | Indirect effect | Mediating effect | Moderating effect | Reference |
|---|---|---|---|---|
| Neuroticism | On QOL scores through coping efforts | [33] | ||
| Optimism | On mental QOL and psychological distress through symptom preoccupation | [50] | ||
| Optimism | On overall QOL through doctor-patient relationships | [65] | ||
| Optimism | Optimism modifies time effect (duration of disease) on role functioning and overall QOL | [71] | ||
| Neuroticism | On psychological HRQOL through coping style and social support | [72] | ||
| Unmitigated communion, communion, and agency | Unmitigated communion: on psychological HRQOL through instrumental constrains and failure to adhere an exercise regimen | [75] | ||
| Sense of coherence | On HRQOL though illness appraisal | Mediates the effect of physical health limitation on HRQOL | [78] | |
| Neuroticism | On oral HRQOL through psychological distress and psychological functioning affect | [79] | ||
| Neuroticism | Neuroticism modifies the effect of earthquake stressor on psychological distress | [82] | ||
| Neuroticism | Neuroticism modifies the effect of chronic condition on health perception, physical functioning, and social functioning; | [84] | ||
| Neuroticism and extraversion | Neuroticism and extraversion modifies the effect of aging on general health perceptions | [60] | ||
| Neuroticism and optimism | Neuroticism: on mental HRQOL through perceived stress. Optimism: on mental and psychical HRQOL through perceived stress | [94] |
Additional variance in HRQOL explained by personality characteristics
Personality characteristics explained varying proportions of variance in HRQOL, depending on the specific personality types and domains of HRQOL measured (Table 5). As expected, personality characteristics explained greater variance in psychosocial aspects of HRQOL than physical aspects. Variance explained in psychosocial HRQOL was often >10%, with a range between 0 and 45%. In contrast, the variance in physical HRQOL explained was a range between 0 and 39%. For overall QOL, the variance explained by personality ranged between 1 and 40%. Comparing the variance explained by single personality characteristics, Hooker et al. found that neuroticism explained 39% of the variance in psychological HRQOL, but only 17–29% in physical HRQOL [94].
Table 5. Additional variance in HRQOL explained by personality characteristics.
| Personality characteristics | Variance explained in HRQOL % by personality characteristics | Reference |
|---|---|---|
| Negative affectivity | 9-13% (overall QOL) | [24] |
| Negative affectivity | 0.1-4% (pain), 1-12% (physical functioning), 1-12% (overall QOL), 10% (social functioning), 4-8% (psychological functioning), 3-18% (psychosocial functioning) | [68] |
| Negative affectivity | 0% (physical function), 0-2% (vitality), 0-2% (social functioning), 0-1% (pain), 0-1% (general health perception), 1-3% (role physical functioning), 2-5% (role emotional functioning), 3-14% (mental functioning) | [77] |
| Neuroticism | 10% (overall QOL) | [33] |
| Neuroticism | 7% (overall QOL) | [54] |
| Neuroticism | 17-25% (overall QOL), 30% (emotional functioning) | [59] |
| Neuroticism | Neuroticism: 25% (overall QOL) | [92] |
| Neuroticism and extraversion | Neuroticism: 1% (overall QOL); extraversion: 11% (overall QOL) | [36] |
| Neuroticism and optimism | Neuroticism: 39% (mental HRQOL), 17-29% (physical HRQOL); optimism: 34% (mental HRQOL), 10-19% (physical HRQOL) | [94] |
| Neuroticism and lie | Neuroticism: 36% (overall QOL), 23% (emotional functioning); lie: 15% (overall QOL) | [34] |
| Neuroticism, extraversion, conscientiousness, openness, and agreeableness | Combined personality traits: 12% (child self-rated social functioning), 36% (child self-rated school functioning), 36% (parent rated emotional functioning), 26% (parent-rated social functioning), 14% (parent rated school functioning), and 18% (parent-rated overall QOL) | [35] |
| Neuroticism, extraversion, conscientiousness, openness, and agreeableness | 38% (child self-rated overall QOL), 16% (parent-rated overall QOL) | [56] |
| Neuroticism, extraversion, conscientiousness, openness, and agreeableness | Combined personality traits: 0% (physical functioning); 6% (role physical functioning); 12% (social functioning); 12% (role emotional functioning); 14% (general health perception); 28% (vitality); 45% (mental health) |
[66] |
| Neuroticism, extraversion, conscientiousness, openness, and agreeableness | 3% (physical functioning), 4% (general health perceptions) | [60] |
| Sense of coherence | 28% (overall QOL) | [78] |
| Mastery | 6.5% (Performance-based measure) | [89] |
| Optimism | 21% (MCS), 41% (psychological distress) | [50] |
| Self-efficacy | 40% (overall QOL) | [26] |
| Self-efficacy | 16% (overall QOL) | [30] |
| Self-esteem | 5% (overall QOL) | [61] |
| Trait anxiety | 24-39% (physical functioning), 18% (psychological functioning) | [46] |
Discussion
We conducted a systematic review of 76 studies that examined the relationship of personality characteristics to HRQOL. Personality appears to have consistent relationships with HRQOL that are moderate in magnitude and often outweigh the effects of demographic, social, and even clinical factors. However, personality is more often related to psychosocial aspects of HRQOL than to physical aspects. The magnitude of correlation coefficients between personality characteristics and specific domains of HRQOL ranged from 0.04 to 0.74 (median = 0.30) and the effect sizes ranged from 0 to 4.2 (median = 0.18). Variance explained in psychosocial HRQOL was between 0 and 45% (median = 11%), whereas the variance in physical HRQOL was between 0 and 39% (median = 2%). In particular, neuroticism, negative affectivity, and sense of coherence generally show moderate correlations with psychosocial HRQOL. Neuroticism was most likely to be related to psychological functioning; for example, 39% of the variance in psychological HRQOL versus 17–29% in physical HRQOL was explained by neuroticism [94]. Few studies have examined the impact of personality traits on the longitudinal change of HRQOL. It is evident that individuals with type-D [39] and pessimism [71] personality, respectively, possess higher risk of consistently impaired HRQOL over time than those with non-type-D and optimism personality.
As expected, personality characteristics were more strongly related to patients’ self-rating of their own HRQOL than were proxy-ratings made on their behalf. Interestingly, personality characteristics also predicted the discrepancy between self- and proxy-ratings of functioning. For example, patients with higher neuroticism and lower extraversion and mastery were likely to self-report more impaired hearing, motor, and ADL functioning than their proxies reported for them [88, 89, 97]. This suggests that personality may bias the proxy ratings of patients’ health status.
Although explorations of the mechanisms between personality and health are increasing, existing theories and models focus on the outcomes of health state/illness [16], subjective well-being (SWB) [98], and death [99–101] rather than HRQOL. Fig 2 illustrates the possible links between personality characteristics and HRQOL based on the rubric of trait-related theories explaining the direct effects of personality on HRQOL and the rubric of cognitive behavior-related theories explaining the indirect effects.
Trait theory emphasizes the effect of common genetic biological factors [102, 103]. There is evidence that genetic factors explain 30%-60% of the variance in personality traits [104] and 40% of the variance in HRQOL. Trait theory explains individual differences from two perspectives (emotional reactivity and cognitive processing of information), which helps explain how personality is related to HRQOL [105]. The emotional reactivity hypothesis [106] suggests that the differences in an individual’s well-being may be due to differences in emotional reactivity, which are governed by personality traits. For example, extraverts may react more strongly to pleasant emotional stimuli than introverts, and may be more likely to experience pleasant affect when exposed to a positive event. The cognitive processing of information hypothesis [107] suggests that individuals are more likely to perceive trait-congruent information than incongruent information. For example, extraverts were quicker to relate events to their motives when they were in a positive mood, whereas introverts were quicker when in a negative mood [107]. Therefore, personality characteristics influence both what information is processed and how it is interpreted. The proposed direct links between personality characteristics and HRQOL (route A in Fig 2) reflect the results of the majority of the studies under our review (also see specific studies listed in Tables 2 and 3). This direct links incorporate both schools of thought to suggest that personality influences emotional reactivity and the cognitive schema through which individuals perceive, interpret, and encode their internal somatic experience and HRQOL.
Trait-related theories, unfortunately, cannot explain the mechanisms by which personality influence HRQOL [108]. Cognitive behavior theory (or the Transactional model) emphasizes that personality affects the illness appraisal and influences individuals’ coping process [16]. Although this theory was initially applied to SWB rather than HRQOL, illness appraisal behavior is a significant process influencing HRQOL, and the conclusions can be extended to HRQOL. This theory focuses on two aspects of individual differences (congruence and goal adjustment). The congruence hypothesis proposes that individuals may experience high HRQOL when they engage in behaviors (e.g., coping) that are concordant with their personality traits [105]. The goal adjustment hypothesis argues that individuals have a global tendency to experience HRQOL in a way determined by their personality [105]. Individuals with a personality characterized of being able to disengage from unattainable goals and reengage elsewhere are able to support active coping and avoid failure experiences, consequently maintaining a higher HRQOL [9]. Based on cognitive behavior-related theories, the linkages (route B in Fig 2) suggest that the effects of personality characteristics on HRQOL might be mediated by social support, coping skill, health behaviors (e.g. smoking, drug abuse), or psycho-physiological mechanisms [70, 79, 94, 109, 110].
It is also possible that personality mediates the effect of other variables (e.g. severity and physical limitations) on HRQOL (route C in Fig 2). Although personality traits have a considerable hereditary component and are less modifiable than HRQOL [111], some evidence suggests individuals who experience traumatic events (e.g., crime and hurricane [112]) or deteriorating health states (e.g., stroke, respiratory disease [113, 114] or cancer [115]) may trigger the change of personality to some extent. Recent studies even suggest that individuals who experience traumatic events may encounter positive personality change (or post-traumatic growth) [116, 117]. Although we found that mediating roles are evident for sense of coherence [78], this finding was derived from cross-sectional design. Nevertheless, Fig 2 provides a framework for testing mediating roles of personality on HRQOL, and adjudication of meaningful mediating effects can be further supported by datasets containing changes in health, personality, and HRQOL.
When studying the association of personality and HRQOL outcomes, caution should be taken with respect to several methodological and practical issues. First, a perennial problem in personality research is that the personality measures labeled the same name may capture different dimensions and the measures labeled different names may capture the same dimension. Several of the traits that we deem single can be explained by the Five-Factor Model. For example, type D is little more than high neuroticism and low extraversion; and aggressiveness is high neuroticism, low agreeableness, and low conscientiousness. To distinguish between single traits and personality dimensions, it is important to conduct additional analyses, for example calculating Pearson’s correlation to list a micro-trait (e.g., optimism) under a macro-dimension (e.g., neuroticism) if the magnitude exceeds a threshold (e.g., coefficient ≥0.4). Unfortunately, the majority of the papers we reviewed did not provide the intercorrelations that are needed to separate putative single traits from personality dimensions. Therefore, the approach we have taken may potentially inflate or deflate the magnitude of our findings.
Second, the relationships between personality characteristics and HRQOL can be partly attributed to the overlap in operationalization of the constructs and scale items. For example, extraversion is characterized by positive affect, and neuroticism is characterized by negative affect. This makes the relationship between neuroticism and reduced HRQOL somewhat tautological [103]. This argument may also help to explain why personality characteristics are more strongly associated with psychosocial aspects of HRQOL and share more variance in the construct than physical aspects of HRQOL. Kressin et al suggested the adjustment for symptoms of depression or anxiety as a strategy when investigating relationships between personality and HRQOL [77]. This approach helps partition out the common effect of disturbances in mood or other symptoms of affective disorder [60, 77].
Third, the extent to which dimensions of personality and HRQOL are congruent will influence the observed associations. Wasylkiw et al. suggested that the associations between personality and HRQOL may be more interpretable if specific aspects of personality dimensions (e.g. impulsiveness, angry hostility, self-consciousness) were matched with specific aspects of HRQOL [66]. Our systematic review sheds light on which personality traits are related in important ways to specific aspects of HRQOL.
Fourth, the practical application of existing standard personality measures is limited by their length. Most personality measures included in our review were lengthy; for example, 57 items in the EPI [79], and 88 items in the EPQ [81]. These measures are useful for psychological research, but may be cumbersome for clinical research and application. One possible solution is to select one or several important dimensions to assess. Another solution is to use short form measures that retain complex dimensions of personality characteristics, with acceptable psychometric properties. Some sample measures include the Midlife Development Inventory (MIDI) Personality Scale (25 items) [64], the Health-relevant Personality Inventory (HP5i) (20 items) [118], and the Ten-Item Personality Inventory (TIPI) [119].
Fifth, personality characteristics might contribute to the phenomena of response shift in HRQOL. Response shift is initially defined as the change of people’s internal standard or expectation in describing HRQOL concepts or interpreting HRQOL items after the occurrence of interventions or major events such as cancer [120, 121]. Rapkin and Schwartz introduced the concept of appraisal into the response shift framework and divided response shift into direct and moderated components [122, 123]. Direct response shift means the changes in appraisal affect HRQOL rating directly, as a result of personality characteristics relating to set-point maintenance after a change of health state. Moderated response shift means the changes in appraisal affect HRQOL ratings by attenuating the impact of health state changes. However, the effects of personality characteristics on response shift in HRQOL have not been fully investigated. One study found that cancer patients with pessimistic traits may report less improvement in HRQOL than patients with optimistic traits over time despite similar change in underlying health status [124]. Another study using advanced psychometric methods found that cancer patients were susceptible to response shift in general health assessment related to optimism [125].
Finally, this study is restricted to publications prior to December 31st, 2009. We have surveyed publications since 2009 and found that the current review covered a comprehensive list of personality and HRQOL measures and that the observed trends would not altered by adding these additional publication. Therefore, we believe that updating the literature would not change our conclusions significantly. Additionally, findings derived from this review study relied on a crude pooled estimate instead of a meta-analysis because only few studies were available for synthesizing the association with each of the specific personality traits and specific HRQOL domains in each meta-analysis (Table 2). However, the snapshot reported in this review provides a foundation for implementing future meta-analyses of the association of a specific personality trait with a specific HRQOL domain when a sufficient number of studies are available.
Understanding individual patients’ personality characteristics may help clinicians manage patients’ behaviors toward successful treatment adherence and health outcomes. Although a person’s personality characteristics are difficult to alter [126–129], it is possible to ameliorate or buffer the effect of personality on HRQOL by providing individualized treatment, counseling, or enhancing patients’ coping skill based on their unique personality characteristics. There are increasing interests in directing interventions at the processes through which personality is expressed in behavior and HRQOL. For example, strategies for illness appraisal and coping can be targeted, based on personality characteristics, with the goal of improving HRQOL [130]. Understanding the relationships of personality characteristics to HRQOL may be able to improve patient self-management. It is also possible self-knowledge by patients of their own personality characteristics and the predictable relationship of these characteristics to their well-being may influence their proclivity to adopt specific, targeted interventions.
An important next step for research is to apply pathway approaches [130] to explain the mechanism by which personality characteristics lead to important outcomes (e.g., behaviors, longevity, HRQOL, well-being) over the life course [131]. If personality characteristics confound the relationships between variables of interest (such as treatment regimens) and HRQOL outcomes, personality variables should be collected and accounted for in study design or statistical models. All of this suggests that it may be useful for clinicians and researchers to collect and identify individuals’ personality characteristics to better understand and interpret subsequent HRQOL.
The clinical and research significance of the relationships between personality and HRQOL suggest further implications for policy and practice. We believe that personality should be measured more routinely in clinical practice, as well as for clinical and health care research. There is the opportunity to introduce personality measures into the electronic health record as a form of patient-generated data, using patient portals and other electronic collection methods. Doing so would make information on personality characteristics available for multiple applications, and to generate new evidence for the usefulness of these data [132].
Conclusions
In conclusion, personality characteristics at the levels of domain or individual trait, respectively, are associated with HRQOL at overall, physical, psychological, social, and other domains, respectively. However, the magnitudes for the corresponding associations are different. Specifically, we found that personality is more often related to psychosocial aspects of HRQOL than to physical aspects, and personality traits such as neuroticism and negative affectivity are strongly associated with mental aspects of HRQOL. Personality characteristics had indirect, mediating, and moderating effects on different aspects of HRQOL. Interpreting these relationships is complicated by overlap in how the concepts of personality and HRQOL are operationalized. Future research is needed to distinguish among the various constructs and measures of personality and HRQOL. The thoughtful and systematic collection of personality data could be useful for both research and clinical practice.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
Authors would like to thank Dr. Geetha Jayaram, a psychiatrist from Johns Hopkins University Hospital, who worked with the research team as a consultant to help identify appropriate personality measures to be included in this review study.
Data Availability
This is a review study and data are available from PubMed from the sources discussed within the paper.
Funding Statement
This work was supported in part by the National Institutes of Health K23 HD057146. The funder provided support in the form of salary for the first author ICH. Additionally, Outcomes Research, Evidera provided support in the form of salary for the author DAR. These funders did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of authors are articulated in the ‘author contributions’ section. No additional external funding was received for this study.
References
- 1.Wilson I. B., & Cleary P. D. (1995). Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. Journal of the American Medical Association, 273(1), 59–65. [PubMed] [Google Scholar]
- 2.Muldoon M. F., Barger S. D., Flory J. D., & Manuck S. B. (1998). What are quality of life measurements measuring? BMJ, 316(7130), 542–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barsky A. J., Cleary P. D., & Klerman G. L. (1992). Determinants of perceived health status of medical outpatients. Social Science & Medicine, 34(10), 1147–1154. [DOI] [PubMed] [Google Scholar]
- 4.Watten R. G., Vassend O., Syversen J. L., & Myhrer T. (1995). Personality and quality of life. Social Indicators Research, 35(3), 289–302. [Google Scholar]
- 5.Derlega V. J., Winstead B. A., & Jones W. H. (2005). Personality: Contemporary theory and research. Belmont, CA: Cengage Learning/Wadsworth. [Google Scholar]
- 6.Matthews G., & Deary I. J. (1998). Personality traits. Cambridge, UK: Cambridge University Press. [Google Scholar]
- 7.Eysenck H. J. (1967). The biological basis of personality. Springfield, IL: Transaction Publishers. [Google Scholar]
- 8.Costa P. T., & McRae R. R. (1985). The NEO Personality Inventory Manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- 9.Wrosch C., & Scheier M. F. (2003). Personality and quality of life: The importance of optimism and goal adjustment. Quality of Life Research, 12(Suppl 1), 59–72. [DOI] [PubMed] [Google Scholar]
- 10.Mischel W., & Shoda Y. (1995). A cognitive-affective system theory of personality: reconceptualizing situations, dispositions, dynamics, and invariance in personality structure. Psychological Review, 102(2), 246–268. [DOI] [PubMed] [Google Scholar]
- 11.Smith T. W., & Spiro A. Iii (2002). Personality, health, and aging: Prolegomenon for the next generation. Journal of Research in Personality, 36(4), 363–394. [Google Scholar]
- 12.Scheier M. F., Matthews K. A., Owens J. F., Schulz R., Bridges M. W., Magovern G. J., & Carver C. S. (1999). Optimism and rehospitalization after coronary artery bypass graft surgery. Archives of Internal Medicine, 159(8), 829–835. [DOI] [PubMed] [Google Scholar]
- 13.Maruta T., Colligan R. C., Malinchoc M., & Offord K. P. Optimists vs pessimists: survival rate among medical patients over a 30-year period (2nd ed., Vol. 75, pp. 140–143). Presented at the Mayo Clinic Proceedings, Elsevier. [DOI] [PubMed] [Google Scholar]
- 14.Chang E. C. (2001). Optimism & pessimism: Implications for theory, research, and practice. Washington, D.C.: American Psychological Association. [Google Scholar]
- 15.Garratt A., Schmidt L., Mackintosh A., & Fitzpatrick R. (2002). Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ (Clinical research ed.), 324(7351), 1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larsen R. J., & Buss D. M. (2009). Personality psychology: domains of knowledge about human nature (Vol. 4). New York: McGraw-Hill Higher Education. [Google Scholar]
- 17.Diener E., Suh E. M., Lucas R. E., & Smith H. L. (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125(2), 276–303. [Google Scholar]
- 18.Spiro A. Iii, & Bosse R. (2000). Relations between health-related quality of life and well-being: The gerontologist's new clothes? International Journal of Aging and Human Development, 51(4), 297–318. [DOI] [PubMed] [Google Scholar]
- 19.Ware J. E., & Kosinski M. (2001). SF-36 physical & mental health summary scales: a manual for users of version 1 (Vol. 2). Lincoln, RI: QualityMetric. [Google Scholar]
- 20.Maruyama G. M. (1997). Basics of structural equation modeling. Thousand Oaks, CA: Sage Publications, Incorporated. [Google Scholar]
- 21.Baron R. M., & Kenny D. A. (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- 22.Badura-Brzoza K., Zajac P., Brzoza Z., Kasperska-Zajac A., Matysiakiewicz J., Piegza M., et al. (2009). Psychological and psychiatric factors related to health-related quality of life after total hip replacement - preliminary report. European Psychiatry, 24(2), 119–124. 10.1016/j.eurpsy.2008.06.009 [DOI] [PubMed] [Google Scholar]
- 23.Bartoces M. G., Severson R. K., Rusin B. A., Schwartz K. L., Ruterbusch J. J., & Neale A. V. (2009). Quality of Life and Self-Esteem of Long-Term Survivors of Invasive and Noninvasive Cervical Cancer. Journal of Women's Health, 18(5), 655–661. 10.1089/jwh.2008.0959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dubayova T., Nagyova I., Havlikova E., Rosenberger J., Gdovinova Z., Middel B., et al. (2009). The association of type D personality with quality of life in patients with Parkinson's disease. Aging and Mental Health, 13(6), 905–912. 10.1080/13607860903046529 [DOI] [PubMed] [Google Scholar]
- 25.Dubayova T., Nagyova I., Havlikova E., Rosenberger J., Gdovinova Z., Middel B., et al. (2009). Neuroticism and extraversion in association with quality of life in patients with Parkinson’s disease. Quality of Life Research, 18(1), 33–42. 10.1007/s11136-008-9410-x [DOI] [PubMed] [Google Scholar]
- 26.Kall L. B. (2009). Psychological determinants of quality of life in patients with whiplash associated disorders-a prospective study. Disability and Rehabilitation, 31(3), 227–236. 10.1080/09638280801912030 [DOI] [PubMed] [Google Scholar]
- 27.Kobayashi M., Ohno T., Noguchi W., Matsuda A., Matsushima E., Kato S., & Tsujii H. (2009). Psychological distress and quality of life in cervical cancer survivors after radiotherapy: do treatment modalities, disease stage, and self-esteem influence outcomes? International Journal of Gynecological Cancer, 19(7), 1264–1268. 10.1111/IGC.0b013e3181a3e124 [DOI] [PubMed] [Google Scholar]
- 28.Kvarme L., Haraldstad K., Helseth S., Sorum R., & Natvig G.(2009). Associations between general self-efficacy and health-related quality of life among 12-13-year-old school children: a cross-sectional survey. Health and Quality of Life Outcomes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siassi M., Weiss M., Hohenberger W., Lösel F., & Matzel K. (2009). Personality rather than clinical variables determines quality of life after major colorectal surgery. Diseases of the Colon & Rectum, 52(4), 662–668. [DOI] [PubMed] [Google Scholar]
- 30.Tsaousides T., Warshowsky A., Ashman T. A., Cantor J. B., Spielman L., & Gordon W. A. (2009). The relationship between employment-related self-efficacy and quality of life following traumatic brain injury. Rehabilitation Psychology, 54(3), 299–305. 10.1037/a0016807 [DOI] [PubMed] [Google Scholar]
- 31.Visser-Meily J. M. A., Rhebergen M. L., Rinkel G. J. E., van Zandvoort M. J., & Post M. W. M. (2009). Long-Term Health-Related Quality of Life After Aneurysmal Subarachnoid Hemorrhage Relationship With Psychological Symptoms and Personality Characteristics. Stroke, 40(4), 1526–1529. 10.1161/STROKEAHA.108.531277 [DOI] [PubMed] [Google Scholar]
- 32.Warrian K. J., Spaeth G. L., Lankaranian D., Lopes J. F., & Steinmann W. C. (2009). The effect of personality on measures of quality of life related to vision in glaucoma patients. British Journal of Ophthalmology, 93(3), 310–315. 10.1136/bjo.2008.139592 [DOI] [PubMed] [Google Scholar]
- 33.Aarstad A. K. H., Aarstad H. J., & Olofsson J. (2008). Personality and choice of coping predict quality of life in head and neck cancer patients during follow-up. Acta Oncologica, 47(5), 879–890. 10.1080/02841860701798858 [DOI] [PubMed] [Google Scholar]
- 34.Boye B., Jahnsen J., Mokleby K., Leganger S., Jantschek G., Jantschek I., et al. (2008). The INSPIRE study: Are different personality traits related to disease- specific quality of life (IBDQ) in distressed patients with ulcerative colitis and Crohn's disease? Inflammatory Bowel Diseases, 14(5), 680–686. 10.1002/ibd.20367 [DOI] [PubMed] [Google Scholar]
- 35.Boye B., Lundin K. E. A., Leganger S., Mokleby K., Jantschek G., Jantschek I., et al. (2008). The INSPIRE study: Do personality traits predict general quality of life (Short form-36) in distressed patients with ulcerative colitis and Crohn's disease? Scandinavian Journal of Gastroenterology, 43(12), 1505–1513. 10.1080/00365520802321196 [DOI] [PubMed] [Google Scholar]
- 36.De Bolle M., De Clercq B., De Fruyt F., & Benoit Y. (2008). Self-and parental perspectives on quality of life in children with cancer. Journal of Psychosocial Oncology, 26(2), 35–47. [DOI] [PubMed] [Google Scholar]
- 37.Jerant A., Chapman B. P., & Franks P. (2008). Personality and EQ-5D scores among individuals with chronic conditions. Quality of Life Research, 17(9), 1195–1204. 10.1007/s11136-008-9401-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aquarius A. E., Denollet J., Hamming J. F., Van Berge Henegouwen D. P., & De Vries J. (2007). Type-D personality and ankle brachial index as predictors of impaired quality of life and depressive symptoms in peripheral arterial disease. Archives of Surgery, 142(7), 662–667. 10.1001/archsurg.142.7.662 [DOI] [PubMed] [Google Scholar]
- 39.Aquarius A. E., Denollet J., de Vries J., & Hamming J. F. (2007). Poor health-related quality of life in patients with peripheral arterial disease: Type D personality and severity of peripheral arterial disease as independent predictors. Journal of Vascular Surgery, 46(3), 507–512. 10.1016/j.jvs.2007.04.039 [DOI] [PubMed] [Google Scholar]
- 40.Chapman B., Duberstein P., & Lyness J. M. (2007). Personality traits, education, and health-related quality of life among older adult primary care patients. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62(6), 343–352. [DOI] [PubMed] [Google Scholar]
- 41.Cohen M., Mansoor D., Langut H., & Lorber A. (2007). Quality of Life, Depressed Mood, and Self-Esteem in Adolescents With Heart Disease. Psychosomatic Medicine, 69(4), 313–318. 10.1097/PSY.0b013e318051542c [DOI] [PubMed] [Google Scholar]
- 42.Karlsson M. R., Edström-Plüss C., Held C., Henriksson P., Billing E., & Wallén N. H. (2007). Effects of expanded cardiac rehabilitation on psychosocial status in coronary artery disease with focus on type D characteristics. Journal of Behavioral Medicine, 30(3), 253–261. 10.1007/s10865-007-9096-5 [DOI] [PubMed] [Google Scholar]
- 43.Middleton J., Tran Y., & Craig A. (2007). Relationship Between Quality of Life and Self-Efficacy in Persons With Spinal Cord Injuries. Archives of Physical Medicine and Rehabilitation, 88(12), 1643–1648. 10.1016/j.apmr.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 44.Moreno-Jiménez B., López Blanco B., Rodríguez-Muñoz A., & Garrosa Hernández E. (2007). The influence of personality factors on health-related quality of life of patients with inflammatory bowel disease. Journal of Psychosomatic research, 62(1), 39–46. 10.1016/j.jpsychores.2006.07.026 [DOI] [PubMed] [Google Scholar]
- 45.Pedersen S. S., Theuns D. A. M. J., Muskens-Heemskerk A., Erdman R. A. M., & Jordaens L. (2007). Type-D personality but not implantable cardioverter-defibrillator indication is associated with impaired health-related quality of life 3 months post-implantation. Europace, 9(8), 675–680. 10.1093/europace/eum041 [DOI] [PubMed] [Google Scholar]
- 46.van der Steeg A. F. W., De Vries J., van der Ent F. W. C., & Roukema J. A. (2007). Personality predicts quality of life six months after the diagnosis and treatment of breast disease. Annals of Surgical Oncology, 14(2), 678–685. 10.1245/s10434-006-9175-9 [DOI] [PubMed] [Google Scholar]
- 47.Arnold R., Ranchor A. V., Koëter G. H., de Jongste M. J. L., Wempe J. B., Hacken, ten N. H. T., et al. (2006). Changes in personal control as a predictor of quality of life after pulmonary rehabilitation. Patient Education and Counseling, 61(1), 99–108. 10.1016/j.pec.2005.02.015 [DOI] [PubMed] [Google Scholar]
- 48.Friedman L. C., Kalidas M., Elledge R., Chang J., Romero C., Husain I., et al. (2006). Optimism, social support and psychosocial functioning among women with breast cancer. Psycho‐Oncology, 15(7), 595–603. 10.1002/pon.992 [DOI] [PubMed] [Google Scholar]
- 49.Abu Hantash R. O., Al-Omiri M. K., & Al-Wahadni A. M. (2006). Psychological impact on implant patients' oral health-related quality of life. Clinical Oral Implants research, 17(2), 116–123. 10.1111/j.1600-0501.2005.01219.x [DOI] [PubMed] [Google Scholar]
- 50.Ong L., Cribbie R., Harris L., Dorian P., Newman D., Mangat I., et al. (2006). Psychological correlates of quality of life in atrial fibrillation. Quality of Life Research, 15(8), 1323–1333. 10.1007/s11136-006-0029-5 [DOI] [PubMed] [Google Scholar]
- 51.Pedersen S. S., Holkamp P. G., Caliskan K., van Domburg R. T., Erdman R. A., & Balk A. H. (2006). Type D personality is associated with impaired health-related quality of life 7 years following heart transplantation. Journal of Psychosomatic Research, 61(6), 791–795. 10.1016/j.jpsychores.2006.06.008 [DOI] [PubMed] [Google Scholar]
- 52.Aquarius A. E., Denollet J., Hamming J. F., & De Vries J. (2005). Role of disease status and type D personality in outcomes in patients with peripheral arterial disease. The American Journal of Cardiology, 96(7), 996–1001. 10.1016/j.amjcard.2005.05.059 [DOI] [PubMed] [Google Scholar]
- 53.van den Berg M. P., Ranchor A. V., van Sonderen F. L., van Gelder I. C., & van Veldhuisen D. J. (2005). Paroxysmal atrial fibrillation, quality of life and neuroticism. The Netherlands Journal of Medicine, 63(5), 170–174. [PubMed] [Google Scholar]
- 54.Vollrath M., & Landolt M. A. (2005). Personality predicts quality of life in pediatric patients with unintentional injuries: a 1-year follow-up study. Journal of Pediatric Psychology, 30(6), 481–491. 10.1093/jpepsy/jsi073 [DOI] [PubMed] [Google Scholar]
- 55.Zhang S. J., Huang L. H., Wen Y. L., Hu Z. H., Jin J., Shen L. H., & Cai L. X. (2005). Impact of personality and coping mechanisms on health related quality of life in liver transplantation recipients. Hepatobiliary & Pancreatic Diseases International, 4(3), 356–359. [PubMed] [Google Scholar]
- 56.De Clercq B., De Fruyt F., Koot H. M., & Benoit Y. (2004). Quality of life in children surviving cancer: A personality and multi-informant perspective. Journal of Pediatric Psychology, 29(8), 579–590. 10.1093/jpepsy/jsh060 [DOI] [PubMed] [Google Scholar]
- 57.Sears S. F., Serber E. R., Lewis T. S., Walker R. L., Conners N., Lee J. T., et al. (2004). Do positive health expectations and optimism relate to quality-of-life outcomes for the patient with an implantable cardioverter defibrillator? Journal of Cardiopulmonary Rehabilitation and Prevention, 24(5), 324–331. [DOI] [PubMed] [Google Scholar]
- 58.Wittkowski A., Richards H. L., Griffiths C. E. M., & Main C. J. (2004). The impact of psychological and clinical factors on quality of life in individuals with atopic dermatitis. Journal of Psychosomatic Research, 57(2), 195–200. 10.1016/S0022-3999(03)00572-5 [DOI] [PubMed] [Google Scholar]
- 59.Aarstad H. J., Aarstad A. K. H., Birkhaug E. J., Bru E., & Olofsson J. (2003). The personality and quality of life in HNSCC patients following treatment. European Journal of Cancer, 39(13), 1852–1860. [DOI] [PubMed] [Google Scholar]
- 60.Duberstein P. R., Sörensen S., Lyness J. M., King D. A., Conwell Y., Seidlitz L., & Caine E. D. (2003). Personality is associated with perceived health and functional status in older primary care patients. Psychology and Aging, 18(1), 25–37. [DOI] [PubMed] [Google Scholar]
- 61.Han K., Lee P., Lee S., & Park E. (2003). Factors Influencing Quality of Life in People with Chronic Illness in Korea. Journal of Nursing Scholarship, 35(2), 139–144. [DOI] [PubMed] [Google Scholar]
- 62.Penedo F. J., Gonzalez J. S., Dahn J. R., Antoni M., Malow R., Costa P., & Schneiderman N. (2003). Personality, quality of life and HAART adherence among men and women living with HIV/AIDS. Journal of Psychosomatic Research, 54(3), 271–278. [DOI] [PubMed] [Google Scholar]
- 63.Cormier L., Guillemin F., Valéri A., Fournier G., Cussenot O., Mangin P., & Litwin M. S. (2002). Impact of prostate cancer screening on health-related quality of life in at-risk families. Urology, 59(6), 901–906. [DOI] [PubMed] [Google Scholar]
- 64.Goodwin R., & Engstrom G. (2002). Personality and the perception of health in the general population. Psychological Medicine, 32(2), 325–332. [DOI] [PubMed] [Google Scholar]
- 65.Rose M., Fliege H., Hildebrandt M., Schirop T., & Klapp B. F. (2002). The network of psychological variables in patients with diabetes and their importance for quality of life and metabolic control. Diabetes Care, 25(1), 35–42. [DOI] [PubMed] [Google Scholar]
- 66.Wasylkiw L., & Fekken G. C. (2002). Personality and self-reported health: matching predictors and criteria. Personality and Individual Differences, 33(4), 607–620. [Google Scholar]
- 67.Cederfjäll C., Langius-Eklöf A., Lidman K., & Wredling R. (2001). Gender differences in perceived health-related quality of life among patients with HIV infection. AIDS Patient Care and STDs, 15(1), 31–39. 10.1089/108729101460083 [DOI] [PubMed] [Google Scholar]
- 68.Kressin N. R., Reisine S., Spiro A. 3., & Jones J. A. (2001). Is negative affectivity associated with oral quality of life? Community Dentistry and Oral Epidemiology, 29(6), 412–423. [DOI] [PubMed] [Google Scholar]
- 69.Tanum L., & Malt U. F. (2001). Personality and physical symptoms in nonpsychiatric patients with functional gastrointestinal disorder. Journal of Psychosomatic Research, 50(3), 139–146. [DOI] [PubMed] [Google Scholar]
- 70.Achat H., Kawachi I., Spiro A., DeMolles D. A., & Sparrow D. (2000). Optimism and depression as predictors of physical and mental health functioning: the Normative Aging Study. Annals of Behavioral Medicine, 22(2), 127–130. [DOI] [PubMed] [Google Scholar]
- 71.Allison P. J., Guichard C., & Gilain L. (2000). A prospective investigation of dispositional optimism as a predictor of health-related quality of life in head and neck cancer patients. Quality of Life Research, 9(8), 951–960. [DOI] [PubMed] [Google Scholar]
- 72.Burgess A. P., Carretero M., Elkington A., Pasqual-Marsettin E., Lobaccaro C., & Catalan J. (2000). The role of personality, coping style and social support in health-related quality of life in HIV infection. Quality of Life Research, 9(4), 423–437. [DOI] [PubMed] [Google Scholar]
- 73.Canizares S., Torres X., Boget T., Rumia J., Elices E., & Arroyo S. (2000). Does neuroticism influence cognitive self-assessment after epilepsy surgery? Epilepsia, 41(10), 1303–1309. [DOI] [PubMed] [Google Scholar]
- 74.Denollet J., Vaes J., & Brutsaert D. L. (2000). Inadequate response to treatment in coronary heart disease: adverse effects of type D personality and younger age on 5-year prognosis and quality of life. Circulation, 102(6), 630–635. [DOI] [PubMed] [Google Scholar]
- 75.Fritz H. L. (2000). Gender-linked personality traits predict mental health and functional status following a first coronary event. Health Psychology, 19(5), 420–428. [DOI] [PubMed] [Google Scholar]
- 76.Kempen G. I. J. M., Sanderman R., Miedema I., Meyboom-de Jong B., & Ormel J. (2000). Functional decline after congestive heart failure and acute myocardial infarction and the impact of psychological attributes. A prospective study. Quality of Life Research, 9(4), 439–450. [DOI] [PubMed] [Google Scholar]
- 77.Kressin N. R., Spiro A. Iii, & Skinner K. M. (2000). Negative affectivity and health-related quality of life. Medical Care, 38(8), 858–867. [DOI] [PubMed] [Google Scholar]
- 78.Nesbitt B. J., & Heidrich S. M. (2000). Sense of coherence and illness appraisal in older women's quality of life. Research in Nursing & Health, 23(1), 25–34. [DOI] [PubMed] [Google Scholar]
- 79.Scott A. A., Hatch J. P., Rugh J. D., Rivera S. M., Hoffman T. J., Dolce C., & Bays R. A. (1999). Psychosocial predictors of high-risk patients undergoing orthognathic surgery. The International Journal of Adult Orthodontics and Orthognathic Surgery, 14(2), 113–124. [PubMed] [Google Scholar]
- 80.Yamaoka K., Shigehisa T., Ogoshi K., Haruyama K., Watanabe M., Hayashi F., & Hayashi C. (1998). Health-related quality of life varies with personality types: a comparison among cancer patients, non-cancer patients and healthy individuals in a Japanese population. Quality of Life Research, 7(6), 535–544. [DOI] [PubMed] [Google Scholar]
- 81.Zhu D. T., Jin L. J., Xie G. J., & Xiao B. (1998). Quality of life and personality in adults with epilepsy. Epilepsia, 39(11), 1208–1212. [DOI] [PubMed] [Google Scholar]
- 82.Carr V. J., Lewin T. J., Kenardy J. A., Webster R. A., Hazell P. L., Carter G. L., & Williamson M. (1997). Psychosocial sequelae of the 1989 Newcastle earthquake: III. Role of vulnerability factors in post-disaster morbidity. Psychological Medicine, 27(1), 179–190. [DOI] [PubMed] [Google Scholar]
- 83.Hollifield M., Katon W., Skipper B., Chapman T., Ballenger J. C., Mannuzza S., & Fyer A. J. (1997). Panic disorder and quality of life: variables predictive of functional impairment. American Journal of Psychiatry, 154(6), 766–772. 10.1176/ajp.154.6.766 [DOI] [PubMed] [Google Scholar]
- 84.Kempen G. I. J. M., Jelicic M., & Ormel J. (1997). Personality, chronic medical morbidity, and health-related quality of life among older persons. Health Psychology, 16(6), 539–546. [DOI] [PubMed] [Google Scholar]
- 85.Wettergren L., Langius A., Björkholm M., & Björvell H. (1997). Physical and psychosocial functioning in patients undergoing autologous bone marrow transplantation-a prospective study. Bone Marrow Transplantation, 20(6), 497–502. 10.1038/sj.bmt.1700921 [DOI] [PubMed] [Google Scholar]
- 86.Chen C. C., David A., Thompson K., Smith C., Lea S., & Fahy T. (1996). Coping strategies and psychiatric morbidity in women attending breast assessment clinics. Journal of Psychosomatic Research, 40(3), 265–270. [DOI] [PubMed] [Google Scholar]
- 87.Joukamaa M., Saarijärvi S., Muuriaisniemi M. L., & Salokangas R. K. R. (1996). Alexithymia in a normal elderly population. Comprehensive Psychiatry, 37(2), 144–147. [DOI] [PubMed] [Google Scholar]
- 88.Kempen G., Van Heuvelen M. J. G., Van den Brink R. H. S., Kooijman A. C., Klein M., Houx P. J., & Ormel J. (1996). Factors affecting contrasting results between self-reported and performance-based levels of physical limitations. Age and Ageing, 25(6), 458–464. [DOI] [PubMed] [Google Scholar]
- 89.Kempen G. I. J. M., Steverink N., Ormel J., & Deeg D. J. H. (1996). The assessment of ADL among frail elderly in an interview survey: self-report versus performance-based tests and determinants of discrepancies. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 51(5), 254–260. [DOI] [PubMed] [Google Scholar]
- 90.Hidding A., & Linden S. (1995). Factors related to change in global health after group physical therapy in ankylosing spondylitis. Clinical Rheumatology, 14(3), 347–351. [DOI] [PubMed] [Google Scholar]
- 91.Carver C. S., Pozo Kaderman C., Harris S. D., Noriega V., Scheier M. F., Robinson D. S., et al. (1994). Optimism versus pessimism predicts the quality of women's adjustment to early stage breast cancer. Cancer, 73(4), 1213–1220. [DOI] [PubMed] [Google Scholar]
- 92.Hidding A., De Witte L., & Van der Linden S. (1994). Determinants of self-reported health status in ankylosing spondylitis. Journal of Rheumatology, 21(2), 275–278. [PubMed] [Google Scholar]
- 93.Jorm A. F., Christensen H., Henderson S., Korten A. E., Mackinnon A. J., & Scott R. (1993). Neuroticism and self-reported health in an elderly community sample. Personality and Individual Differences, 15(5), 515–521. [Google Scholar]
- 94.Hooker K., Monahan D., Shifren K., & Hutchinson C. (1992). Mental and physical health of spouse caregivers: The role of personality. Psychology and Aging, 7(3), 367–375. [DOI] [PubMed] [Google Scholar]
- 95.Wilson J. A., Deary I. J., & Maran A. G. (1988). Is globus hystericus? The British Journal of Psychiatry, 153(3), 335–339. [DOI] [PubMed] [Google Scholar]
- 96.Scheier M. F., & Carver C. S. (1985). Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychology, 4(3), 219–247. [DOI] [PubMed] [Google Scholar]
- 97.Skinner T. C., Hampson S. E., & Fife-Schaw C. (2002). Personality, personal model beliefs, and self-care in adolescents and young adults with Type 1 diabetes. Health Psychology, 21(1), 61–70. [PubMed] [Google Scholar]
- 98.Kahneman D., Diener E., & Schwarz N. (2003). Personality and subjective well-being In Well-being: The foundations of hedonic psychology (pp. 213–229). Russell Sage Foundation Publications. [Google Scholar]
- 99.Ploubidis G. B., & Grundy E. (2009). Personality and all cause mortality: Evidence for indirect links. Personality and Individual Differences, 47(3), 203–208. [Google Scholar]
- 100.Denollet J. (1998). Personality and coronary heart disease: the type-D scale-16 (DS16). Annals of Behavioral Medicine, 20(3), 209–215. [DOI] [PubMed] [Google Scholar]
- 101.Martin L. R., Friedman H. S., & Schwartz J. E. (2007). Personality and mortality risk across the life span: the importance of conscientiousness as a biopsychosocial attribute. Health Psychology, 26(4), 428–436. 10.1037/0278-6133.26.4.428 [DOI] [PubMed] [Google Scholar]
- 102.DeNeve K. M. (1999). Happy as an extraverted clam? The role of personality for subjective well-being. Current Directions in Psychological Science, 8(5), 141–144. [Google Scholar]
- 103.Diener E. (1996). Traits can be powerful, but are not enough: Lessons from subjective well-being. Journal of Research in Personality, 30(3), 389–399. [Google Scholar]
- 104.Bouchard T. J. (1994). Genes, environment, and personality. Science, 24(5166), 1700–1701. [DOI] [PubMed] [Google Scholar]
- 105.Diener E., Oishi S., & Lucas R. E. (2003). Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annual Review of Psychology, 54(1), 403–425. [DOI] [PubMed] [Google Scholar]
- 106.Larsen R. J., & Ketelaar T. (1991). Personality and susceptibility to positive and negative emotional states. Journal of Personality and Social Psychology, 61(1), 132–140. [DOI] [PubMed] [Google Scholar]
- 107.Tamir M., Robinson M. D., & Clore G. L. (2002). The epistemic benefits of trait-consistent mood states: an analysis of extraversion and mood. Journal of Personality and Social Psychology, 83(3), 663–677. [DOI] [PubMed] [Google Scholar]
- 108.Emmons R. A. (1995). Levels and domains in personality: an introduction. Journal of Personality, 63(3), 341–364. [DOI] [PubMed] [Google Scholar]
- 109.Lara M. E., Leader J., & Klein D. N. (1997). The association between social support and course of depression: Is it confounded with personality? Journal of Abnormal Psychology, 106(3), 478–482. [DOI] [PubMed] [Google Scholar]
- 110.Bailis D. S., Segall A., Mahon M. J., Chipperfield J. G., & Dunn E. M. (2001). Perceived control in relation to socioeconomic and behavioral resources for health. Social Science & Medicine, 52(11), 1661–1676. [DOI] [PubMed] [Google Scholar]
- 111.Caspi A., Roberts B. W., & Shiner R. L. (2005). Personality development: stability and change. Annual Review of Psychology, 56, 453–484. 10.1146/annurev.psych.55.090902.141913 [DOI] [PubMed] [Google Scholar]
- 112.Lockenhoff C. E., Terracciano A., Patriciu N. S., Eaton W. W., & Costa P. T. J. (2009). Self-reported extremely adverse life events and longitudinal changes in five-factor model personality traits in an urban sample. Journal of Traumatic Stress, 22(1), 53–59. 10.1002/jts.20385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Stone J., Townend E., Kwan J., Haga K., Dennis M. S., & Sharpe M. (2004). Personality change after stroke: some preliminary observations. Journal of Neurology, Neurosurgery, and Psychiatry, 75(12), 1708–1713. 10.1136/jnnp.2004.037887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jokela M., Hakulinen C., Singh-Manoux A., & Kivimäki M. (2014). Personality change associated with chronic diseases: pooled analysis of four prospective cohort studies. Psychological Medicine, In Press. [DOI] [PubMed] [Google Scholar]
- 115.Porcelli P., Tulipani C., Di Micco C., Spedicato M. R., & Maiello E. (2011). Temporal stability of alexithymia in cancer patients following a psychological intervention. Journal of Clinical Psychology, 67(12), 1177–1187. 10.1002/jclp.20839 [DOI] [PubMed] [Google Scholar]
- 116.Jim H. S., & Jacobsen P. B. (2008). Posttraumatic stress and posttraumatic growth in cancer survivorship: a review. Cancer Journal (Sudbury, Mass.), 14(6), 414–419. [DOI] [PubMed] [Google Scholar]
- 117.Sumalla E. C., Ochoa C., & Blanco I. (2009). Posttraumatic growth in cancer: reality or illusion? Clinical Psychology Review, 29(1), 24–33. 10.1016/j.cpr.2008.09.006 [DOI] [PubMed] [Google Scholar]
- 118.Gustavsson J. P., Jönsson E. G., Linder J., & Weinryb R. M. (2003). The HP5 inventory: definition and assessment of five health-relevant personality traits from a five-factor model perspective. Personality and Individual Differences, 35(1), 69–89. [Google Scholar]
- 119.Gosling S. D., Rentfrow P. J., & Swann W. B. (2003). A very brief measure of the Big-Five personality domains. Journal of Research in Personality, 37(6), 504–528. [Google Scholar]
- 120.Carver C. S., & Scheier M. F. (2000). Scaling back goals and recalibration of the affect system are processes in normal adaptive self-regulation: understanding “response shift” phenomena. Social Science & Medicine, 50(12), 1715–1722. [DOI] [PubMed] [Google Scholar]
- 121.Sprangers M. A. G., & Schwartz C. E. (1999). Integrating response shift into health-related quality of life research: a theoretical model. Social Science & Medicine, 48(11), 1507–1515. [DOI] [PubMed] [Google Scholar]
- 122.Rapkin B. D., & Schwartz C. E. (2004). Toward a theoretical model of quality-of-life appraisal: Implications of findings from studies of response shift. Health and Quality of Life Outcomes, 2, 14 10.1186/1477-7525-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schwartz C. E., & Sprangers M. A. (2009). Reflections on genes and sustainable change: toward a trait and state conceptualization of response shift. Journal of Clinical Epidemiology, 62(11), 1118–1123. 10.1016/j.jclinepi.2009.02.008 [DOI] [PubMed] [Google Scholar]
- 124.Beeken R. J., Eiser C., & Dalley C. (2011). Health-related quality of life in haematopoietic stem cell transplant survivors: a qualitative study on the role of psychosocial variables and response shifts. Quality of Life Research, 20(2), 153–160. 10.1007/s11136-010-9737-y [DOI] [PubMed] [Google Scholar]
- 125.King-Kallimanis B. L., Oort F. J., Visser M. R. M., & Sprangers M. A. G. (2009). Structural equation modeling of health-related quality-of-life data illustrates the measurement and conceptual perspectives on response shift. Journal of Clinical Epidemiology, 62(11), 1157–1164. 10.1016/j.jclinepi.2009.04.004 [DOI] [PubMed] [Google Scholar]
- 126.Eysenck H. J., & Eysenck M. W. (1985). Personality and individual differences: A natural science approach. New York: Plenum Press. [Google Scholar]
- 127.McCrae R. R., & Costa P. T. (1990). Personality in Adulthood (Vol. Reprint). New York: Guilford Press. [Google Scholar]
- 128.McCrae R. R., Costa P. T. Jr, Ostendorf F., Angleitner A., Hřebíčková M., Avia M. D., et al. (2000). Nature over nurture: temperament, personality, and life span development. Journal of Personality and Social Psychology, 78(1), 173–186. [DOI] [PubMed] [Google Scholar]
- 129.Torrey W. C., Mueser K. T., McHugo G. H., & Drake R. E. (2000). Self-esteem as an outcome measure in studies of vocational rehabilitation for adults with severe mental illness. Psychiatric Services, 51(2), 229–233. 10.1176/appi.ps.51.2.229 [DOI] [PubMed] [Google Scholar]
- 130.Hampson S. E. (2012). Personality processes: mechanisms by which personality traits “get outside the skin.” Annual Review of Psychology, 63, 315–339. 10.1146/annurev-psych-120710-100419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Roberts B. W., Kuncel N. R., Shiner R., Caspi A., & Goldberg L. R. (2007). The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science, 2(4), 313–345. 10.1111/j.1745-6916.2007.00047.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wu A. W., Kharrazi H., Boulware L. E., & Snyder C. F. (2013). Measure once, cut twice—adding patient-reported outcome measures to the electronic health record for comparative effectiveness research. Journal of Clinical Epidemiology, 66(8 Suppl), S12–20. 10.1016/j.jclinepi.2013.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
This is a review study and data are available from PubMed from the sources discussed within the paper.