Abstract
Little is known about the epidemiology of contact dermatitis (CD) in the Chinese clothing industry. This study aimed to investigate the prevalence and some risk factors of contact dermatitis among clothing manufacturing employees in Beijing.
This cross-sectional study was conducted by interview using self-administered questionnaires and skin examination between May and August in 2016. Five-hundred twenty-nine employees who had worked at sewing, ironing, and as managers at 12 clothing manufacturing factories were studied.
The overall 1-year prevalence of CD among the clothing employees was 28.5% (151/529 employees), with significantly higher prevalence among ironing workers (50%) and sewers (31.7%) compared with managers (12.7%; P < 0.001, n = 529). A significant association was noticed between the 1-year prevalence of CD and types of occupation (sewers and ironing workers versus managers, respectively), exposure to garment materials (leather and feather), dry skin, allergic rhinitis, age, and smoking.
Among employees in Chinese clothing industry, sewers and ironing workers had a higher 1-year prevalence of CD than managers. It is noteworthy that exposure to leather and feather materials and the types of manual work are associated with CD, as well as dry skin and allergic rhinitis.
Keywords: clothing manufacturing employees, contact dermatitis, occupational contact dermatitis, prevalence, risk factor
1. Introduction
Occupational contact dermatitis (OCD) has been observed to have a high risk of occurrence among blue-collar workers at workplace.[1,2] However, although the number of cases and costs of OCD are increasing,[3] there are few occupational population-based epidemiological studies.
Contact dermatitis (CD) is an important health issue in occupations that involve mostly manual work, and is generally associated with prolonged or frequent contact with allergens or irritants.[4] Furthermore, exposure to certain metal working tools and contact with dermatitis-causing chemicals such as dyes and finish agents are known to be risk factors for CD.[4,5] Employees with the highest risk of development CD are those working in the healthcare, hairdressing, car repair, leather manufacture, and shoe manufacturing industries.[6–9] Nevertheless, studies on textile and garment dermatitis have only been undertaken among registered patients,[5,10,11] literature related to OCD of employees in the Chinese clothing industry is very limited.
During the garment manufacturing process, there is the potential for occupational exposure to substances, such as leather, polyester fiber, feathers, finishing agents, adhesives, and metal working tools (irons and scissors), which may result in employees developing CD.[12,13] Moreover employees also may suffer from skin complaints caused by hot and humid conditions at the workplace,[4,6] this is likely to affect ironing workers in particular.
The clothing manufacturing industry is well-developed in China and many of the population are engaged in this occupation. Daxing District is the center of clothing distribution and collection in China. Our hospital is located near clothing factories in the Daxing District, and we noted that the clothing employees accounted for about 15% of outpatients with dermatitis in 2014, and around 19% of them at our clinic in 2015, possibly because of occupational exposure. Recurrence has also been found in some patients after conventional treatments. Repeated recurrence and a refractory disease course severely affect the quality of life of the employees. Therefore, there is an indispensable need to examine the prevalence and related risk factors of CD among clothing employees.
We conducted a cross-sectional survey of self-reported symptoms by filling in questionnaires and used skin examination to investigate the prevalence of CD and to determine some of its risk factors among employees of clothing factories in Daxing District, a suburb of Beijing.
2. Methods
2.1. Study population and design
The strengthening the reporting of observational studies in epidemiology (STROBE) checklist was followed with respect to the study design as much as possible.[14] Five hundred sixty employees were recruited from 12 factories in Daxing District, which is a distribution center for the clothing industry of China. The inclusion criteria were: factory size was between 30 and 50 employees; factory was located in Daxing District in Beijing; employees had worked in the garment factories for at least 1 year. Finally, 529 employees were eligible for inclusion in the study. Figure 1 presented a flowchart of the study population.
Figure 1.
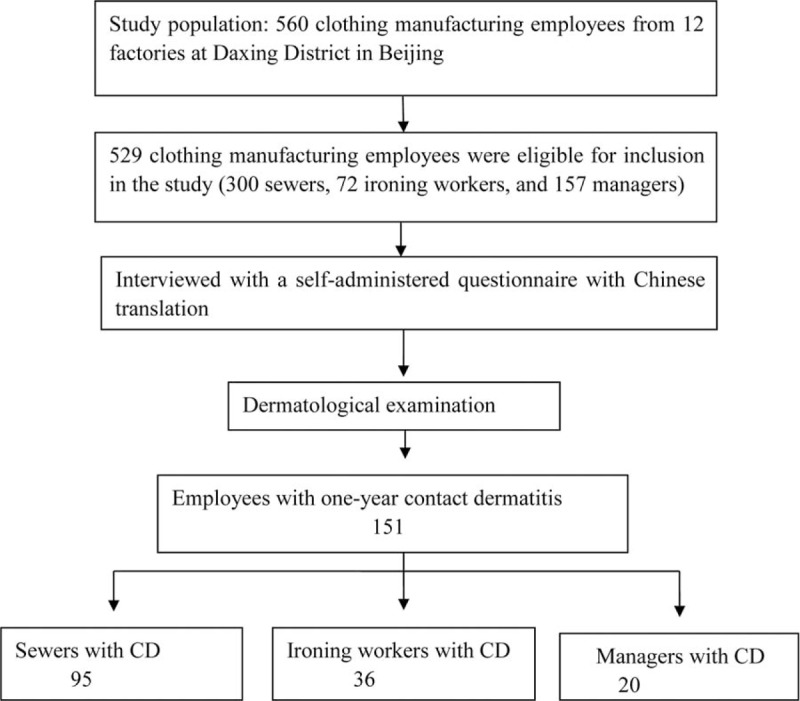
Flowchart of the study population: 560 clothing manufacturing employees. CD = contact dermatitis.
Factories with between 30 and 50 employees account for the vast majority of clothing manufacturing factories included the survey. In these factories, the employee turnover rate is extremely high. In addition, the employees with CD in the clinic mainly came from factories with 30 to 50 employees.
The employees were categorized into 3 groups: the sewers group, the ironing workers group (both groups had regular and direct exposure to work materials at the workplace), and the managers group who had regular and indirect exposure to work materials, and were mainly in charge of supervision at the workplace. Figure 2 showed working scenes and workers at workplace.
Figure 2.
Working scenes and workers at clothing manufacturing workplace.
We recruited the factories using a quota sampling method on the basis of regional division; Daxing District was divided into 5 areas, and 3 factories were selected from each area on the basis of convenience sampling. In all, there were 15 factories contacted, and 3 factory owners refused to participate in the investigation.
The sample size of the study was calculated on the basis of an estimate from a previous general population survey in Beijing.[15]
2.2. Questionnaire
A self-administered questionnaire based on the validated Nordic Occupational Skin Questionnaire 2002 (NOSQ-2002) was used.[16] A modified version of NOSQ that collects data on the prevalence of OSD as a questionnaire based on self-reported diagnoses seemed to be a good tool.[17,21] The interview was conducted face-to-face at the workplace. The employees had their skin examined and were asked to fill in the questionnaire. The questionnaire consisted of 3 parts. The first part recorded demographic and individual characteristics, including age, sex, skin type, their personal perceived relationship between their current occupation and skin complaints, personal habits, housing conditions, sleeping quality, bathing frequency, among others. The second part recorded any case history and current skin problems during the past year, locations and course of lesions, and family and personal history of atopy including atopic dermatitis, dry skin, asthma, allergic conjunctivitis, and allergic rhinitis. The third part recorded occupation-related conditions, including the type of occupation, exposure to substances while working, garment materials (leather, feathers, polyester fibers), and metal work tools (irons and scissors), whether protective masks were used, working duration (years), and average working hours per day, among others.
2.3. Skin examination
On the basis of the interview, CD was diagnosed by the dermatologist depending on the following well-recognized indicators, by a dermatologist that had received training on professional skin examination.
Skin examination was conducted for signs of CD such as erythema, papules, vesicles, scales, and fissure, including their sites and subjective symptoms. OCD was confirmed depending on evidence to support the diagnosis of OCD, and if the cases met the following well-recognized criteria:[18] occupational contact with an agent known to cause similar skin changes in other individuals; the occurrence of similar dermatitis in fellow workers within the same occupation; a time relationship between exposure and dermatitis; types and sites of lesions consistent with occupational exposure; and similarity to other post-exposure episodes of dermatitis followed by an improvement and resolution after removal.
2.4. Ethical issues
This study was approved by the Ethics Committee of the Friendship Hospital, Capital Medical University (No. 2016-P2–029–02) and verbal consents were obtained.
2.5. Statistical analysis
Statistical analyses were performed with SPSS version 20.0 (SPSS, Chicago, IL). The P values of 2-sided analysis were regarded as statistically significant if the level was P < 0.05, and 95% confidence intervals (CIs) were used.
Descriptive statistics were used for baseline data of all respondents. Categorical variables are presented as numbers and relative frequencies of respondents. Continuous variables were summarized by the median and range, including minimum and maximum.
χ2 Tests and Kruskal-Wallis tests were used for comparison of demographic and work characteristics and prevalence of CD between different types of work. Binary logistic regression (stepwise method) was used to screen risk factors for CD. Only risk factors with P < 0.05 in the univariate analyses were included in the multiple logistic regression.
3. Results
3.1. Population characteristics
In this study, 529 employees were available for inclusion (response rate of 94%, based on 12 factories). The demographic characteristics of the 529 respondents are given in Table 1. Of all respondents, 43.7% were female. The overall median age was 33 years (range 16–57 years).
Table 1.
Demographic and work characteristics of the 529 respondents.
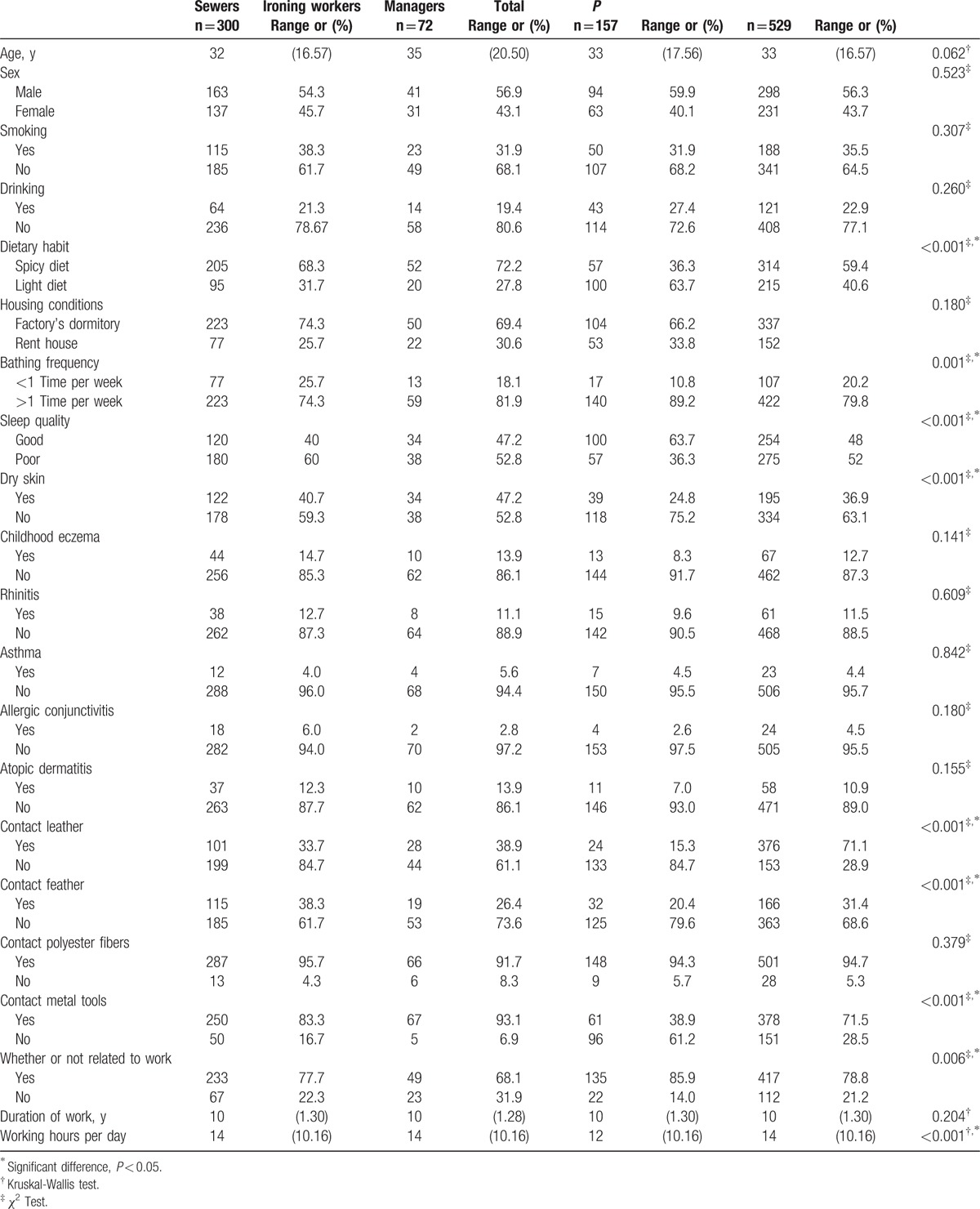
3.2. Work characteristics
The work characteristics of the 529 respondents are also presented in Table 1. Of the respondents, 56.7% (300 of 529) were sewers, 13.6% (72 of 529) were ironing workers, and 29.7% (157 of 529) were managers.
The median duration of working in the clothing industry was 10 years (range 1–30 years). The median working hours per day was 14 hours (range 10–16 hours). It was found that 20.2% of workers bathed <1 times per week, and 71.3% of workers noted that they resided at a factory dormitory. Only 4.5% of them reported that they used protective masks while working.
3.3. Prevalence of CD and its characteristics and consequences
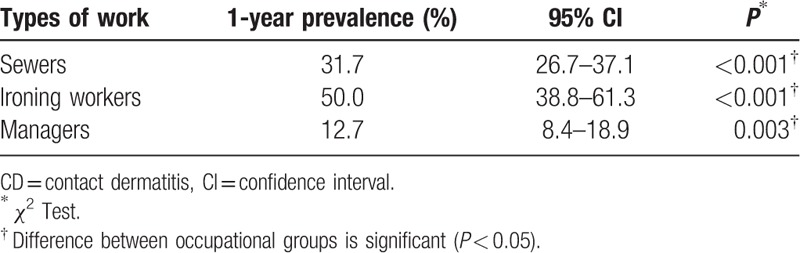
In total, 28.5% of 529 employees had experienced CD in the past year. Figure 3 illustrates the distribution of overall respondents and respondents with CD by work types. According to their type of work, the highest 1-year prevalence of CD was noted in ironing workers (50.0%, 95% CI: 38.8–61.3), followed by sewers (31.7%, 95% CI: 26.7–37.1), and the lowest 1-year prevalence (12.7%, 95% CI: 8.4–18.9) in managers in Table 2.
Figure 3.
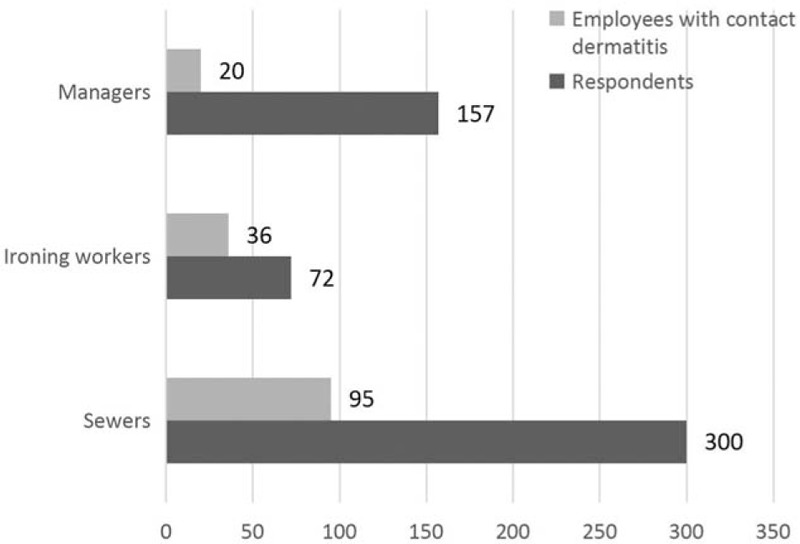
Distribution of total respondents and employees with contact dermatitis by types of work.
Table 2.
One-year prevalence (95% confidence interval) of CD among clothing manufacturing employees by types of work.
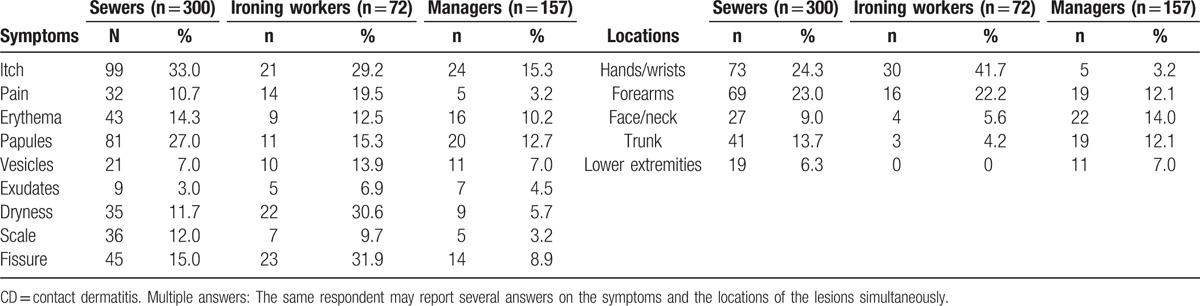
The skin symptoms and the locations of the lesions in respondents with CD in the last year are shown in Table 3 according to their type of work. Overall, itch (27.2%), pain (9.6%), fissures (15.5%), erythema (12.9%), and scales (9.1%) were the most frequent skin complaints. The hands/wrists (20.4%), the forearms (19.7%), and the neck/face (10.0%) were the most often affected sites on the body.
Table 3.
Skin symptoms and localizations of the lesions of respondents with CD in the last year (multiple answers).
The frequencies of CD were observed to be 36.9% in clothing employees with dry skin, 12.7% of them with a history of childhood eczema, 11.5% in those with allergic rhinitis, and 10.9% in those with atopic dermatitis. Furthermore, 19.8% of the employees stated that they developed a rash when they had contact with leather materials and metal work tools. Although, 78.8% of them reported that their symptoms had worsened because of their occupation and regarded them as work-related diseases. Only 11.7% of them responded that they affected their life very much and 15.9% had decided to consult a dermatologist.
3.4. Factors affecting CD
According to univariate analysis, factors that indicated an association with 1-year prevalence of CD among the respondents are shown in Table 4. There was no significant difference in CD prevalence between different sexes of the participants (P = 0.71), whereas there was a significant difference in CD prevalence with age (P < 0.01).
Table 4.
Association between 1-year prevalence of CD and related factors among the respondents.
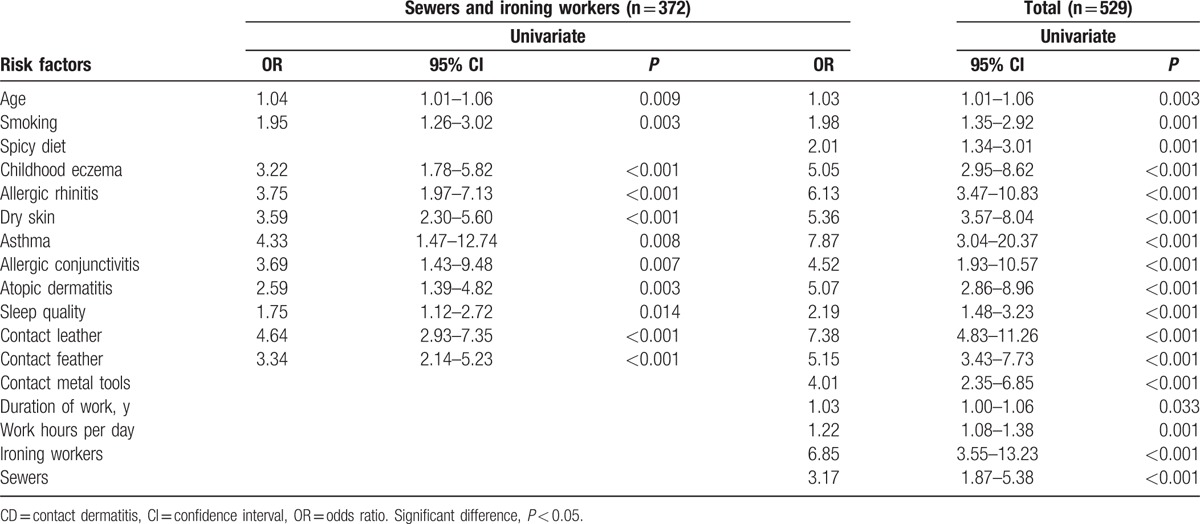
On analysis of the risk factors that affected CD, it also was revealed that having a history of atopic diseases, including a history of allergic rhinitis, childhood eczema, atopic dermatitis, asthma, allergic conjunctivitis, as well as dry skin were the factors with significant difference (P < 0.001, respectively). Although no statistically significant differences were found in housing conditions, bathing frequency, and drinking, spicy food, smoking, and sleeping quality did show a statistically significant difference (spicy food: odds ratio [OR] 2.01, 95% CI:1.34–3.01, P < 0.001; smoking: OR 1.98, 95% CI: 1.35–2.92, P < 0.001; sleeping quality: OR 2.19, 95% CI: 1.48–3.23, P < 0.001, respectively).
The following variables related to work characteristics: working as sewers and ironing workers, having a rash caused by garment materials and metal work tools were indicated to be statistically significant; in addition, working duration and average working hours per day were also statistically significant (Table 4).
3.5. Relationship between the risk factors and CD
Having CD was determined to be a dependent variable of the binary logistic regression. In Table 5, significant risk factors for CD of 1-year prevalence are summarized. Those who had worked as sewers and ironing workers were more likely to experience CD than managers (sewers: OR 2.4, 95% CI: 1.21–4.59; ironing workers: OR 7.6, 95% CI: 3.38–17.24, respectively), and work types were the most substantial forecaster.
Table 5.
Association between 1-year prevalence of CD and risk factors among the respondents.
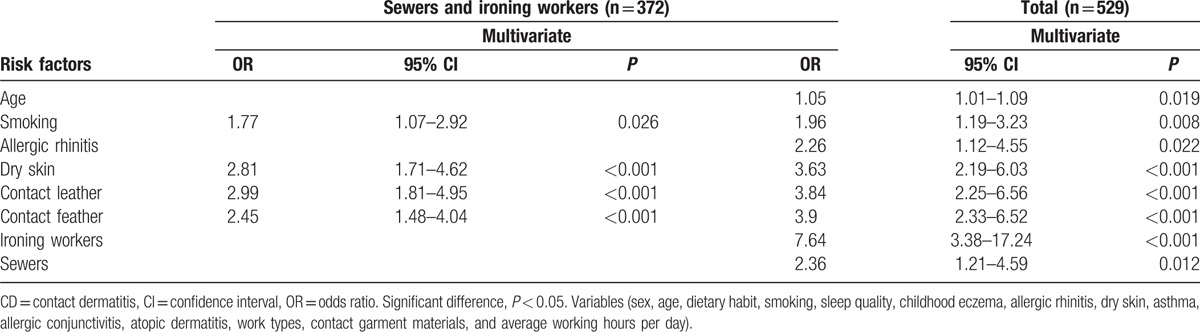
Moreover, employees with exposure to leather and feather materials were more likely to have CD than those in contact with polyester fiber and metal work tools, (leather: OR 3.8, 95% CI: 2.25–6.56; feather: OR 3.9, 95% CI: 2.33–6.52, respectively), and these were the strongest predictors (Table 5).
Other statistically significant risk factors were relevant to allergic rhinitis and dry skin. Those having allergic rhinitis and dry skin were more likely to experience CD than those without it (allergic rhinitis: OR 2.3, 95% CI: 1.12–4.55; dry skin: OR 3.6, 95% CI 2.19–6.03, respectively). In addition, having CD was relevant to the aged individuals and smoking (age: OR 1.1, 95% CI: 1.01–1.09; smoking: OR 1.9, 95% CI: 1.19–3.23).
4. Discussion
There are few available data on the prevalence of CD in the clothing processing industry in China. We expected the problem of OCD to be rather neglected among clothing employees. Our survey showed that clothing employees in Beijing have a higher 1-year prevalence of CD, and risk factors were identified relating to exogenous work-related exposure as well as endogenous susceptibility. To the best of our knowledge, this is the first epidemiological study targeted at the Chinese clothing population, and our results are expected to provide evidence for establishing preventative policies and regulations by management.
In this study, the 1-year prevalence of CD among the clothing manufacturing population in China was 28.5%, which was very high, compared with the studies performed previously. We performed a χ2 test of the 1-year prevalence by different work types, and significant differences were found regarding the 1-year prevalence between sewers (31.7%), ironing workers (50.0%), and managers (12.7%) who were not more likely to experience CD. From as early as 1985, Mathur et al[19] performed a survey on the prevalence of CD among tie dye industry workers in India (16.6%, 49/250), and reported textile dyes and their finishing chemicals caused CD, then Singhi et al (2005)[20] conducted a study concerned with the prevalence of CD among workers engaged in the tie dye, and textile industries in and around Jodhpur (Western Rajasthan) (7.69%, 100/1300). In 2011, Kurpiewska et al[21] carried out a survey of work-related skin diseases in Poland, and showed that about 24% (17/69) of textile factory workers reported skin manifestations during their time of employment, which they thought could be work-related. But in recent years, only limited number of subjects and several epidemic events have been reported relating to clothing workers.[5,10,11] Regarding the status of the present research, few studies are available that have analyzed the prevalence of CD among clothing population in China. Furthermore, the prevalence of self-reported skin symptoms in our study tends to be an underestimate of the true prevalence.
Most work-related dermatitis (>95%) are subtypes of CD, and 80% of CD cases affect the skin of the hands.[2] These results show that the 1-year prevalence of CD (28.5%) was slightly higher than the 1-year prevalence for hand eczema (21%) of 2274 health care workers performed by Diepgen et al in 2012.[8] The prevalence of dermatitis for other occupations have also previously been reported such as health care workers, hairdressers, car mechanics, shoe manufacturing workers, tanner, and vehicle equipment workers.[6–9,25] As there are few studies among clothing employees, it is not easy to specify the CD prevalence for the clothing industry. Also, because the relevant literature is mostly only concerned with dermatitis caused by textile dyes, and the studies are not up-to-date, these results are often not worthy of comparison.[12,13] Moreover, in many cross-sectional studies on occupational diseases, the consequences may be influenced by a healthy worker survivor effect.[22]
Dryness, redness, scaling, and itching were the main skin symptoms of OCD; 80% of cases affected the skin of the hands and forearms in Joanna Kurpiewska's survey.[21] Our study found that the most frequently affected sites of the body were the hands/wrists and forearms in sewers and ironing workers, especially the hands/wrists among ironing workers, whereas the most frequent affected sites of body were the face/neck in managers, which may be induced by airborne allergens such as feathers in down garments and volatile organic compounds in leather, but this has not been reported in previous studies and needs further investigation. Itch, erythema, and fissures were reported the most frequent skin complaints. These results are very similar to those obtained in previous relevant studies.[11,21,23] Our finding related to face/neck dermatitis is that managers tend to be more frequently affected at the workplace.
In China, CD is rarely recognized as an occupational disease at the workplace. When responding to the question “Whether or not related to work,” the manager group had a higher frequency of answering “yes” (135/157). That could be caused by a stronger expectation of self-health among managers, whereas the workers have generally accepted a low sense of self-health. In the present study, 95.5% employees were not using protective masks, and 78.8% of the employees had considered their skin complaints to be related to their occupation. Nonetheless, only 14.9% employees regarded their symptoms as being severe enough to consult a dermatologist, and 11.7% of the employees reported that their symptoms had affected their life very much. These suggest that it is of considerable significance to promote occupational health protection awareness in this special occupational group. Even though in Poland, only in a few cases did dyers mention that they used skin protection measures.[21]
It was demonstrated that contact with leather and feather materials were exogenous risk factors and strong predictors of CD in the multivariate analysis. The employees were exposed to leather materials containing dyes and resin agents, and exposed to feather materials while tailoring down garments. A study in tannery workers showed contact with leather was the most important risk of developing OCD, and OCD was suspected in 77 (16%) of the 472 workers.[24] Another study, among three tannery workers conducted by Febriana et al, showed that CD was caused by benzidine derived leather materials.[7,25] Many other studies have shown the association between CD and leather among shoe manufacturing workers owing to the numerous chemicals used in the preparation of leather.[7,24,25] Among the known sensitizers, potassium dichromate, N, N-diphenylguanidine, benzidine, and sodium metabisulfite are associated with OCD.[7,24–26] In general, contact with leather is already considered to be a risk factor for CD, which is very similar to our results; furthermore, we also found clothing employees were exposed to feathers, and this may have been a potential allergen inducing CD, something that has not previously been much reported. Moreover, the relevant literature is very limited, as long ago as 1967 it was reported that avicultural workers experienced allergic disorders,[27] then in 2002, animal products, for example feathers, are also shown to be susceptible to triggering an allergic reaction.[28]
It was indicated that another exogenous risk factor for CD was the type of work, which was strongly associated with presence of CD in the multivariate analysis. Disease risk prediction among sewers and ironing workers was 2 to 7 times more likely to experience CD than among managers, especially, there was a stronger association with ironing workers. A speculative reason for this could be that sewers and ironing workers endure greater exposure to work materials than managers. It was found that ironing workers are repeatedly exposed to hot and humid conditions, which cause and aggravate dermatitis.[29]
In the present study, allergic rhinitis and dry skin were crucial risk factors for the 1-year prevalence of CD; although a history of atopic dermatitis, allergic conjunctivitis, asthma, and childhood eczema were not statistically significant in the multivariate analysis, they were strongly significant in the univariate analysis. This finding seems be contradicted in the different statistical analyses. In contrast to the present results, previous studies showed a significant difference in atopic dermatitis, allergic conjunctivitis, asthma, and childhood eczema.[30] Another study reported that atopic history played a role in the development of dermatitis in work setting.[31] Consistent with the present results, another study reported an insignificant correlation between hand eczema and asthma or childhood eczema in car mechanics.[32] In terms of an atopic background and whether or not this is a risk factor for CD, the conclusions in previous studies are controversial. A possible explanation for these differences is that the present study is based on only a few observations, so no statistical significance was found in multivariate logistic regression. Nevertheless, this study still showed that allergic rhinitis and dry skin were predictors of CD.
Older age was a potential risk factor in clothing employees. Indeed, previous studies showed that ageing was associated with the appearance of allergic diseases.[33] Ventura et al[34] also noted that the dry skin and the senescence of mucous membranes could be linked to allergic rhinitis. Therefore, ageing also may be associated with dry skin and allergic rhinitis, and they influence each other and facilitate the occurrence of dermatitis together. In other words, the present results often contain inconsistencies compared with previous studies; therefore, it is necessary to undertake further study with an expanded sample size to improve the management of the work-related CD.
4.1. Limitations and strengths
The limitations of the present study are that the inclusion was not based on random sampling but convenience sampling, which may cause a selection bias. In addition, more detailed analysis cannot be conducted because with more variables there is a worse statistical power on the premise of the same sample size. Because of the cross-sectional nature of the survey, a history of 1-year skin symptoms is prone to recall bias. Moreover, the representativeness of the study is limited to some extent because the targeted population is from small and medium-sized clothing factories in the Daxing District.
Notwithstanding its limitations, first of all the survey was conducted to a targeted occupational population among the Chinese clothing population, whereas previous studies were based on the patient populations in clinics and registration of occupational people with OCD. Although the present study did not use random sampling, quota sampling was used on the basis of regional division, and convenience sampling was adopted at each area. In addition, the present study has a high response rate of 94%, and this study does reveal the real-life condition among Chinese clothing employees for the first time. Furthermore, the study included comparison with different work types.
5. Conclusions
We observed that the garment population in Daxing district in Beijing has a high-risk of work-related CD, based on self-reported symptoms. The present results have indicated poor work conditions and a lack of knowledge about skin protection.
Acknowledgments
The authors thank all employees who have participated in this study in twelve factories located Daxing District in Beijing.
Footnotes
Abbreviations: CD = contact dermatitis, NOSQ = Nordic Occupational Skin Questionnaire, OCD = occupational contact dermatitis, STROBE = strengthening the reporting of observational studies in epidemiology.
The authors declare no conflicts of interest.
References
- [1].Diepgen TL. Occupational skin diseases. J Dtsch Dermatol Ges 2012;10:297–313. quiz 314-295. [DOI] [PubMed] [Google Scholar]
- [2].Diepgen TL, Coenraads PJ. The epidemiology of occupational contact dermatitis. Int Arch Occup Environ Health 1999;72:496–506. [DOI] [PubMed] [Google Scholar]
- [3].Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol 2014;134:1527–34. [DOI] [PubMed] [Google Scholar]
- [4].Schwensen JF, Menne T, Veien NK, et al. Occupational contact dermatitis in blue-collar workers: results from a multicentre study from the Danish Contact Dermatitis Group (2003–2012). Contact Dermatitis 2014;71:348–55. [DOI] [PubMed] [Google Scholar]
- [5].Wigger-Alberti W, Elsner P. Occupational contact dermatitis in the textile industry. Curr Probl Dermatol 2003;31:114–22. [DOI] [PubMed] [Google Scholar]
- [6].Aktas E, Esin MN. Skin disease symptoms and related risk factors among young workers in high-risk jobs. Contact Dermatitis 2016;75:96–105. [DOI] [PubMed] [Google Scholar]
- [7].Febriana SA, Soebono H, Coenraads PJ. Occupational skin hazards and prevalence of occupational skin diseases in shoe manufacturing workers in indonesia. Int Arch Occup Environ Health 2014;87:185–94. [DOI] [PubMed] [Google Scholar]
- [8].Ibler KS, Jemec GB, Flyvholm MA, et al. Hand eczema: prevalence and risk factors of hand eczema in a population of 2274 healthcare workers. Contact Dermatitis 2012;67:200–7. [DOI] [PubMed] [Google Scholar]
- [9].Kieć-Świerczyńska M, Swierczyńska-Machura D, Chomiczewska-Skóra D, et al. Occupational allergic and irritant contact dermatitis in workers exposed to polyurethane foam. Int J Occup Med Environ Health 2014;27:196–205. [DOI] [PubMed] [Google Scholar]
- [10].Slodownik D, Williams J, Tate B, et al. Textile allergy–the Melbourne experience. Contact Dermatitis 2011;65:38–42. [DOI] [PubMed] [Google Scholar]
- [11].Lisi P, Stingeni L, Cristaudo A, et al. Clinical and epidemiological features of textile contact dermatitis: an Italian multicentre study. Contact Dermatitis 2014;70:344–50. [DOI] [PubMed] [Google Scholar]
- [12].Coman G, Blattner CM, Blickenstaff NR, et al. Textile allergic contact dermatitis: current status. Rev Environ Health 2014;29:163–8. [DOI] [PubMed] [Google Scholar]
- [13].An DG. Textile dye dermatitis. J Am Acad Dermatol 1995;32:321–3. [DOI] [PubMed] [Google Scholar]
- [14].Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495–9. [DOI] [PubMed] [Google Scholar]
- [15].Yan-ming You, Lin-feng Li. The prevalence of skin diseases in a community of Bingjing and analysis of risk factor. Chinese J Dermatovenereol 2011;25:459–61. [Google Scholar]
- [16].Susitaival P, Flyvholm MA, Meding B, et al. Nordic Occupational Skin Questionnaire (NOSQ-2002): a new tool for surveying occupational skin diseases and exposure. Contact Dermatitis 2003;49:70–6. [DOI] [PubMed] [Google Scholar]
- [17].The China Central Institute for Disease Control, Jianing Survey on contact dermatitis of metal machinery manufacturing industry [D]. 2010. [Google Scholar]
- [18].Nicholson PJ. Evidence-based guidelines: occupational contact dermatitis and urticaria. Occup Med (Lond) 2010;60:502–4. [DOI] [PubMed] [Google Scholar]
- [19].Mathur NK, Mathur A, Banerjee K. Contact dermatitis in tie and dye industry workers. Contact Dermatitis 1985;12:38–41. [DOI] [PubMed] [Google Scholar]
- [20].Singhi MK, Menghani PR, Gupta LK, et al. Occupational contact dermatitis among the traditional ’tie and dye’ cottage industry in Western Rajasthan. Indian J Dermatol Venereol Leprol 2005;71:329–32. [DOI] [PubMed] [Google Scholar]
- [21].Kurpiewska J, Liwkowicz J, Benczek K, et al. A survey of work-related skin diseases in different occupations in Poland. Int J Occup Saf Ergon 2011;17:207–14. [DOI] [PubMed] [Google Scholar]
- [22].Siebert U, Rothenbacher D, Daniel U, et al. Demonstration of the healthy worker survivor effect in a cohort of workers in the construction industry. Occup Environ Med 2001;58:774–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Giusti F, Mantovani L, Martella A, et al. Hand dermatitis as an unsuspected presentation of textile dye contact sensitivity. Contact Dermatitis 2002;47:91–5. [DOI] [PubMed] [Google Scholar]
- [24].Caroe C, Andersen KE, Thyssen JP, et al. Fluctuations in the prevalence of chromate allergy in Denmark and exposure to chrome-tanned leather. Contact Dermatitis 2010;63:340–6. [DOI] [PubMed] [Google Scholar]
- [25].Febriana SA, Jungbauer F, Soebono H, et al. Occupational contact allergy caused by benzidine in three tannery workers. Contact Dermatitis 2012;66:345–6. [DOI] [PubMed] [Google Scholar]
- [26].Thyssen JP, Strandesen M, Poulsen PB, et al. Chromium in leather footwear-risk assessment of chromium allergy and dermatitis. Contact Dermatitis 2012;66:279–85. [DOI] [PubMed] [Google Scholar]
- [27].Gheorghiu T, Popescu IG, Paun R, et al. [Contribution to the study of irritative-allergic disorders observed in workers of an avicultural combine]. Stud Cercet Med Interna 1967;8:249–54. [PubMed] [Google Scholar]
- [28].Krakowiak A, Palczynski C, Walusiak J, et al. Allergy to animal fur and feathers among zoo workers. Int Arch Occup Environ Health 2002;75suppl:S113–6. [DOI] [PubMed] [Google Scholar]
- [29].Behroozy A, Keegel TG. Wet-work exposure: a main risk factor for occupational hand dermatitis. Saf Health Work 2014;5:175–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Minamoto K, Watanabe T, Diepgen TL. Self-reported hand eczema among dental workers in Japan: a cross-sectional study. Contact Dermatitis 2016;75:230–9. [DOI] [PubMed] [Google Scholar]
- [31].Garcon-Michel N, Paul M, Lodde B, et al. [Overview of five years of occupational dermatology: The role of atopy]. Ann Dermatol Venereol 2010;137:681–7. [DOI] [PubMed] [Google Scholar]
- [32].Attwa E, el-Laithy N. Contact dermatitis in car repair workers. J Eur Acad Dermatol Venereol 2009;23:138–45. [DOI] [PubMed] [Google Scholar]
- [33].Seyfarth F, Schliemann S, Antonov D, et al. Dry skin, barrier function, and irritant contact dermatitis in the elderly. Clin Dermatol 2011;29:31–6. [DOI] [PubMed] [Google Scholar]
- [34].Ventura MT, Scichilone N, Gelardi M, et al. Management of allergic disease in the elderly: key considerations, recommendations and emerging therapies. Expert Rev Clin Immunol 2015;11:1219–28. [DOI] [PubMed] [Google Scholar]


