Abstract
The aim of the study was to evaluate the role of the longus colli muscles in cervical vertigo.
We retrospectively analyzed 116 adult patients who underwent anterior cervical discectomy and fusion (ACDF) during 2014 in our department. Patients were assigned to the vertigo group or the nonvertigo group. Demographic data were recorded. Inner distance and cross-sectional area (CSA) of longus colli were measured using coronal magnetic resonance imaging (MRI).
The vertigo group (n = 44) and the nonvertigo group (n = 72) were similar in demographic data. Mean preoperative Japanese Orthopaedic Association (JOA) score was higher in the vertigo group than in the nonvertigo group (P = 0.037), but no difference postoperatively. Mean JOA scores increased significantly postoperatively in both groups (P = 0.002 and P = 0.001). The mean vertigo score decreased significantly from pre- to postoperatively in the vertigo group (P = 0.023). The mean preoperative Cobb angle was significantly smaller in the vertigo group than in the nonvertigo group (P <0.001), but no significant difference postoperatively. After ACDF, the mean Cobb angle increased significantly in the vertigo group (P <0.001). The instability rates of C3/4 and C4/5 were significantly higher in the vertigo group (P <0.001 and P <0.001). The inner distance of longus colli was significantly shorter (P = 0.032 and P = 0.026) and CSA significantly smaller (P = 0.041 and P = 0.035), at C3/4 and C4/5 in the vertigo group than in the nonvertigo group. Mean Miyazaki scores were significantly higher in the vertigo group at C3/4 and C4/5 (P = 0.044 and P = 0.037). Moreover, a shorter inner distance and smaller CSA were related to a higher Miyazaki score.
Inner distance and cross-sectional area (CSA) of longus colli are associated closely with cervical vertigo. Shorter inner distance and smaller CSA of the longus colli muscles might be risk factors for cervical vertigo. ACDF provided a good resolution of cervical vertigo.
Keywords: ACDF, cervical vertigo, disc degeneration, longus colli, MRI
1. Introduction
Vertigo is 1 of the 20 most common causes of medical consultation in adult patients; in 80% cases, the symptoms are so severe that medical intervention is required.[1] One form of vertigo, cervical vertigo, is caused by neck disorders and is the most controversial.[2] Several hypotheses about cervical vertigo have been put forward,[3,4] but no study has investigated the relationship between the longus colli muscle and cervical vertigo. Previous studies have focused mainly on how the deep cervical flexor (DCF) muscles affect chronic neck pain.[5,6]
The longus colli are deep prevertebral muscles consisting of 3 parts. They originate on the anterior aspects of the vertebral bodies from C5 to T3, the anterior tubercle of the transverse processes of C3 to C5, and the sides of the T1 to T3 vertebral bodies bilaterally.[7,8] One study reported that longus colli muscles diverge laterally and have a close relationship with the sympathetic trunk.[9] We have observed clinically that the distance between the inner edges of the longus colli appear related to the type of cervical spondylosis, that is, the shorter the distance, the more likely that the patient will develop cervical vertigo. However, there is a lack of evidence of this relationship in the literature. Therefore, the aims of this study were (1) to determine whether the longus colli muscles are associated with cervical vertigo, (2) to determine the relationship between the longus colli and cervical stability, and (3) to determine whether anterior cervical discectomy and fusion (ACDF) can lead to a good prognosis for cervical vertigo.
2. Materials and methods
2.1. Ethics statements
Given the retrospective nature of the study, written consent was not obtained. However, we got the oral consent from all participants in the study by telephone contact, and patient records were anonymized and deidentified prior to analysis. Then, related data were extracted from hospital's electronic and written medical records. The study was reviewed and obtained the approval from Institutional Review Board of East Hospital, Tongji University.
2.2. Study population
We retrospectively identified 146 adult patients who underwent ACDF in our department during 2014. Patients diagnosed with cervical injury, tumor, infection, or hematoma, or who had previous cervical spine surgery were excluded. Cervical vertigo was diagnosed as follows: (1) obvious sympathetic symptoms such as vertigo, headache, tinnitus and palpitation, and so on; (2) careful diagnosis of cervical spondylosis with disc degeneration or definite spinal cord compression on MRI or cervical instability on x-ray; and (3) patients who suffered from neurological diseases, cardiovascular diseases, Ménière's disease, menopausal syndrome and neurosis, and so on, are excluded after consulting the otolaryngology and neurology departments. All the included patients were not alleviated of their symptoms after 3 months’ strict conservative therapy including cervical immobilization, traction, physiotherapy, and medication. All together, 116 patients were included in this study. Forty-six patients were set in the vertigo group and 72 patients with cervical radiculopathy, myelopathy, or radiculomyelopathy were in the nonvertigo group. Sex, age, body mass index (BMI), and presence of hypertension or diabetic mellitus (DM) were recorded.
2.3. X-ray assessment
Preoperative and postoperative sagittal cervical Cobb angles were measured and recorded in degrees. The global cervical Cobb angle was measured by first drawing 2 lines, 1 parallel to the inferior endplate of the C2 vertebra, and the other parallel to the superior endplate of the C7 vertebra [10] (Figs. 1B and 2B).
Figure 1.
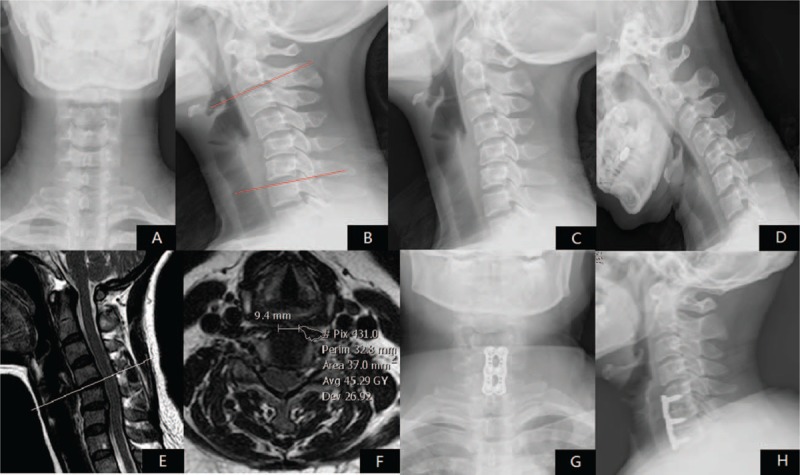
A 56-year-old female, complaint of walking clumsy and vertigo for 2 and half years, underwent ACDF after distinguishing from BPPV, vascular vertigo, neurological diseases, and so on, and failure of 3 months’ conservative treatment. Severity of vertigo was reduced from 4 to 1 after surgery and JOA score increased from 9 to 15 half year after surgery. Preoperative x-ray: (A) A-P view; (B) neutral lateral view; (C) extension lateral view; (D) flexion lateral view. Preoperative MRI: (E) sagittal MRI indicated disc degeneration and herniation of C4/5 and C5/6; (F) coronary MRI at C4/5 indicated CSA was 37.0 mm2 and inner distance of longus colli was 9.4 mm. 1 year's postoperative x-ray: (G) A-P view; (H) lateral view. ACDF = anterior cervical discectomy and fusion, BPPV = Benign Paroxysmal Positional Vertigo, CSA = cross-sectional area, JOA = Japanese Orthopaedic Association, MRI = magnetic resonance imaging.
Figure 2.
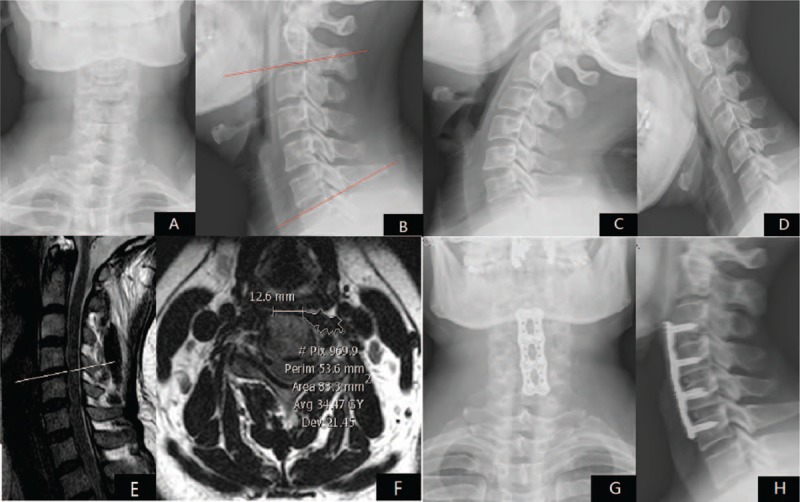
A 58-year-old female, complaint of walking clumsy and radiation pain for both upper extremities for more than 2 years, JOA score was 6 pre-surgery, underwent ACDF after distinguishing from neurological diseases, and so on, and the failure of 3 months’ conservative treatment. Half year after surgery, the JOA score significantly increased from 6 to 15. Preoperative x-ray: (A) A-P view; (B) neutral lateral view; (C) extension lateral view; (D) flexion lateral view. Preoperative MRI: (E) Sagittal MRI indicated disc degeneration and herniation of C4/5 and C5/6; (F) Coronary MRI at C4/5 indicated CSA was 83.3 mm2 and inner distance of longus colli was 12.6 mm. 1 year's postoperative x-ray: (G) A-P view; (H) lateral view. ACDF = anterior cervical discectomy and fusion, CSA = cross-sectional area, JOA = Japanese Orthopaedic Association, MRI = magnetic resonance imaging.
Cervical instability was diagnosed using White's criteria: (a) more than 3.5 mm of horizontal displacement of 1 vertebra in relation to an adjacent vertebra measured on lateral roentgenograms (resting or flexion-extension), and (b) a difference of >11 degrees of rotation compared with that of either adjacent vertebra measured on a resting lateral or flexion-extension roentgenogram.[11] Preoperative resting anteroposterior and lateral radiographs are shown in Figs. 1A and B and 2A and B. Preoperative lateral flexion-extension radiographs are shown in Figs. 1C and D and 2C and D.
2.4. MRI protocol and data analysis
Prior to the study, we obtained cervical magnetic resonance imaging (MRI) for each subject. The MRI scans were obtained using a 3.0-tesla unit and phased-array spine coil with sagittal T1-weighted turbo spin echo, sagittal T2-weighted turbo spin echo, and axial T2-weighted turbo spin echo imaging protocol for the entire cervical spine. The subjects were placed in a comfortable and relaxed supine position with their hips flexed to 45 degrees and their legs supported by foam wedges. The head was positioned in a neutral position with the longus colli muscles relaxed. The distances between inner edges of the longus colli muscles were measured at each level from C2/3 to C6/7 (Figs. 1F and 2F). The cross-sectional areas (CSAs) were measured bilaterally at each disc level, and a mean value was calculated for each level (Figs. 1F and 2F). The severity of cervical disc degeneration was graded according to the 5-level system of Miyazaki et al,[12] with a higher grade indicating more severe degeneration. All data were collected by 1 experienced surgeon who was blinded to patients’ identities to diminish the measurement error.
2.5. Japanese orthopedic association scores and severity of cervical vertigo
Neurological function was assessed using the 17-item Japanese Orthopedic Association (JOA) score,[13] with higher scores representing better neurological function. Severity of cervical vertigo was assessed according to the standard of the American Academy of Otolaryngology-Head and Neck Surgery Committee on Hearing and Equilibrium.[14]
2.6. Surgical procedure
All patients underwent standard ACDF by the same surgeon. Using the method described by Smith and Robinson [15] and Cloward,[16] a right anterolateral approach to the anterior cervical disc via a 3-cm transverse skin incision was used. During the operation, a Caspar screw distracter was used to distract the involved disc space. A small Kerrison punch and curettes were used to remove anterior and posterior hypertrophic osteophytes, which were later used as bone graft material, and to perform cervical discectomy. The upper and lower endplates were prepared by removing the cartilage. Following this, with slight distraction of the disc space with the Caspar screw distracter, trialing was performed and a polyetheretherketone (PEEK) cage of appropriate size was selected. The inner cavity of the PEEK cage was then packed with the local bone chips obtained from removal of the anterior hypertrophic osteophytes. Anterior cervical plates were used in all patients. Surgical levels were decided by definite MRI finding of disc degeneration, spinal cord compression, or cervical instability on x-ray. Postoperative images are shown in Figs. 1G and H and 2G and H.
2.7. Statistical analysis
Data are presented as mean ± standard deviation. Age, BMI, JOA score, vertigo score, Cobb angle, CSA, inner distance, and Miyazaki score were compared using unpaired t tests. Sex and incidences of hypertension, DM, and instability were compared using the chi-square test. Differences with a P value < 0.05 or 0.01 were considered statistically significant. Pearson correlation analysis was adopted to identify the relationship between inner distance or CSA of longus colli and severity of disc degeneration. All statistical analyses were performed using the IBM SPSS Statistics software (SPSS) for Windows, Version 19.0 (IBM Corp., Armonk, NY).
3. Results
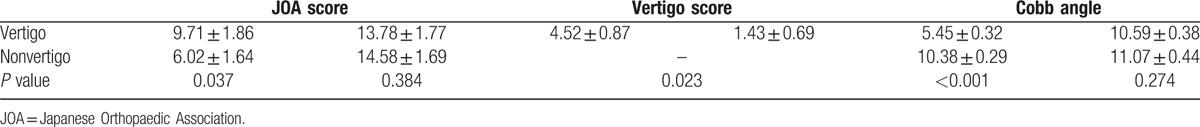
The vertigo group (n = 44; 18 males; mean age 53.81 ± 9.55 years) and the nonvertigo group (n = 72; 30 males; mean age 58.29 ± 9.86 years) show no intergroup differences in sex, age, BMI, and presence of hypertension and diabetes mellitus (Table 1). Table 2 presents pre- and postoperative results of JOA scores, vertigo scores, and Cobb angles. The mean preoperative JOA score was higher in the vertigo group than in the nonvertigo group (P = 0.037), but no difference in the mean JOA score was seen between groups postoperatively. Mean JOA scores increased significantly postoperatively in both the vertigo and nonvertigo group (P = 0.002 and P = 0.001, respectively). The mean vertigo score decreased significantly from pre- to postoperatively in the vertigo group (P = 0.023). The mean preoperative Cobb angle was significantly smaller in the vertigo group than in the nonvertigo group (P <0.001), but there was no significant difference between groups postoperatively. After ACDF, the mean Cobb angle increased significantly in the vertigo group compared with preoperatively (P <0.001) (Table 2).
Table 1.
Demographic data of the 2 groups.
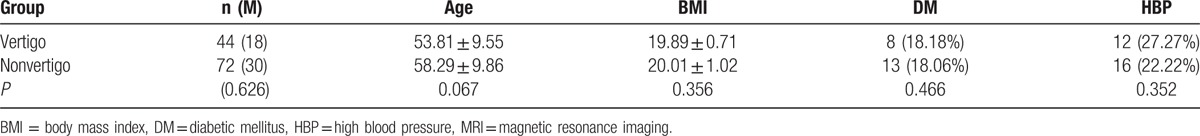
Table 2.
Surgical results of the 2 groups.
The rates of instability of C3/4 and C4 /5 were significantly higher in the vertigo group (P <0.001 and P <0.001, respectively), but no significant intergroup differences were seen in instability of C2/3, C5 /6, and C6/7. The inner distance of longus colli was significantly shorter (P = 0.032 and P = 0.026, respectively), and CSA significantly smaller (P = 0.041 and P = 0.035, respectively), at C3/4 and C4/5 in the vertigo group than in the nonvertigo group, but the differences were not significant at C2/3, C5/6, and C6/7. Mean Miyazaki scores were significantly higher in the vertigo group at C3/4 and C4/5 (P = 0.044 and P = 0.037, respectively), but the differences were not significant at C2/3, C5/6, and C6/7 (Table 3). Moreover, a shorter inner distance was related to a higher Miyazaki score (r = –0.38, P = 0.026 of C3/4; r = –0.41, P = 0.019 of C4/5) and a smaller CSA of longus colli did as well (r = –0.26, P = 0.017 of C3/4; r = –0.33, P = 0.012 of C4/5).
Table 3.
Comparison of radiography characteristics between the 2 groups in different disc levels.

4. Discussion
Colledge et al[17] suggested that cervical spondylosis is the second most frequent cause of vertigo in the elderly. However, because of the lack of a specific diagnostic test, cervical vertigo is a controversial entity.[4] According to our experience, a strict diagnose of cervical vertigo should be based on patients’ episode of sympathetic cervical spondylosis with other vertigo-inducing causes excluded. Several hypotheses regarding the etiology of cervical vertigo, such as neurovascular, somatosensory input, vascular and cervical instability, have been put forward.[4] In the present study, we used MRI to investigate the relationship between the longus colli muscles and cervical vertigo.
In recent years, researchers have focused on identifying and quantifying deficits in the DCF muscles in patients with neck pain.[18–21] Deficits in strength and endurance of the DCF muscles have been demonstrated in patients with chronic neck pain,[20] and some authors have observed that the CSA of the longus colli was smaller in patients with ossification of the posterior longitudinal ligament than in healthy control subjects.[18]
In the present study, shorter inner distance and smaller CSA of the longus colli at C3/4 and C4/5 were observed in the vertigo group. The rates of instability of C3/4 and C4 /5 were significantly higher, and the cervical spine significantly straighter, in the vertigo group than in the nonvertigo group preoperatively. Low activation of the DCF muscles has been shown to be associated with smaller muscle size, and a smaller muscle CSA is considered synonymous with atrophy and impairment; therefore, the size of the DCF muscles can be a good indicator of the significant stabilizing function of these muscles.[20–22] For this reason, we suspected that a shorter inner distance and smaller CSA would represent weaker longus colli muscles, which could lead to cervical spine instability and cause vertigo symptoms. Furthermore, in our study, we observed that a shorter inner distance and smaller CSA of longus colli were related to more severe disc degeneration, which also indicates that the weaker DCF is related to cervical dysfunction.
According to Falla et al[23] many proprioceptors are distributed over the longus colli and longus capitis muscles. Because these proprioceptors provide postural information as quickly as possible with early contraction during movements of the head or upper limbs, they facilitate suitable movements depending on the stability and posture of the neck region. However, atrophy of the longus colli muscles in patients with chronic neck pain can restrict neck stabilization during head or upper limb movements, resulting in unnatural and nonfunctional mobility of the neck, thus leading to cervical instability and cervical vertigo.
Researchers have also reported on the proximity of the longus colli muscles to the sympathetic trunk and the close relationship between these structures.[24,25] The sympathetic trunk would receive more stimulation from an unstable cervical spine, which could cause the sensation of vertigo; an unstable cervical spine would also cause friction on the cervical discs, which would exacerbate disc degeneration process. Future studies that attempt to analyze muscle the strength and the relationship between the sympathetic trunk and longus colli muscles are warranted.
In terms of treatment of cervical vertigo, all patients in the present study had a good prognosis from cervical vertigo after ACDF, and the mean Cobb angles increased significantly in the vertigo group. This could have resulted from postoperative stability of the cervical spine. Indeed, some studies have suggested that, because vertigo symptoms probably originate from irritation of the sympathetic trunk, nerve blockade and surgical denervation are 2 effective treatments.[26–28] It has also been suggested that routine ACDF with resection of the posterior longitudinal ligament could provide relief of sympathetic symptoms [29,30].
A number of interventions have focused on strengthening and re-training the longus colli muscles to improve function.[31] One neck-stabilization exercise attempts to flatten the curvature of the cervical spine without head movement by having patients lie in a supine position and perform chin nodding directed into the occiput, which selectively contracts the longus colli and longus capitis muscles.[32] Moon et al[31] also reported that co-contraction of the masticatory muscles during neck stabilization exercise can help to increase the thickness of the longus colli muscle. Falla et al[19] confirmed that reduced performance of the craniocervical flexion test was associated with dysfunction of the DCF muscles and suggested that this was a valid test for patients with neck pain. Gong[33] reported that massage of the longus colli muscles can be performed on inpatients who cannot perform neck-stabilizing exercises, or before performing other neck-stabilizing exercises. Physical therapy may therefore be a good choice for patients with longus colli muscle dysfunction.
Our study had some shortcomings in addition to its small sample size. First, we investigated only the longus colli, but stability of the cervical spine is maintained by a number of cervical muscles. Second, we did not use electromyography to confirm our suspici on that with a larger CSA and longer inner distance was associated with greater muscle strength. Third, the mechanism of cervical vertigo and disc degeneration with respect to the longus colli muscles was not thoroughly investigated and should be studied in the future.
5. Conclusion
MRI evaluation of 116 patients who underwent standard ACDF revealed that patients with shorter inner distance and smaller CSA of the longus colli muscles might have a greater tendency to develop cervical instability, and they were more likely to suffer from cervical vertigo and disc degeneration. ACDF was a suitable choice for patients with cervical vertigo.
Footnotes
Abbreviations: ACDF = anterior cervical discectomy and fusion, BMI = body mass index, CSA = cross-sectional area, DCF = deep cervical flexor, DM = diabetic mellitus, JOA = Japanese Orthopaedic Association, MRI = magnetic resonance imaging, PEEK = polyetheretherketone.
X-ML and F-MP contributed equally to this study.
Disclosure of interest: No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Authorship: WDS and WSJ designed the study. LZ and BZY collected the data. LXM, PFM, YZY performed the statistics and drafted and revised the manuscript. WSJ, ZWD, WDS revised the manuscript. All authors read and approved the final manuscript.
Funding: Funded by the National Natural Science Foundation of China (81201418, 81572181), Key Discipline Construction Project of Pudong Health Bureau of Shanghai (PWZx2014–02), and China Scholarship Council (CSC NO. 201606260106).
The authors have no conflicts of interest to disclose.
References
- [1].Schappert SM. National Ambulatory Medical Care Survey: 1989 summary. Vital Health Stat 13 1992;110:1–80. [PubMed] [Google Scholar]
- [2].Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Manual Ther 2005;10:4–13. [DOI] [PubMed] [Google Scholar]
- [3].Hain TC. Cervicogenic causes of vertigo. Curr Opin Neurol 2015;28:69–73. [DOI] [PubMed] [Google Scholar]
- [4].Yacovino DA, Hain TC. Clinical characteristics of cervicogenic-related dizziness and vertigo. Semin Neurol 2013;33:244–55. [DOI] [PubMed] [Google Scholar]
- [5].Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J 2006;15:834–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hoy DG, Protani M, De R, et al. The epidemiology of neck pain. Best Pract Res Clin Rheumatol 2010;24:783–92. [DOI] [PubMed] [Google Scholar]
- [7].Vasavada AN, Li S, Delp SL. Influence of muscle morphometry and moment arms on the moment-generating capacity of human neck muscles. Spine 1998;23:412–22. [DOI] [PubMed] [Google Scholar]
- [8].Kamibayashi LK, Richmond FJ. Morphometry of human neck muscles. Spine 1998;23:1314–23. [DOI] [PubMed] [Google Scholar]
- [9].Ebraheim NA, Lu J, Yang H, et al. Vulnerability of the sympathetic trunk during the anterior approach to the lower cervical spine. Spine 2000;25:1603–6. [DOI] [PubMed] [Google Scholar]
- [10].Lau D, Chou D, Mummaneni PV. Two-level corpectomy versus three-level discectomy for cervical spondylotic myelopathy: a comparison of perioperative, radiographic, and clinical outcomes. J Neurosurg Spine 2015;23:280–9. [DOI] [PubMed] [Google Scholar]
- [11].White AA, 3rd, Johnson RM, Panjabi MM, et al. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Relat Res 1975;109:85–96. [DOI] [PubMed] [Google Scholar]
- [12].Miyazaki M, Hong SW, Yoon SH, et al. Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech 2008;21:288–92. [DOI] [PubMed] [Google Scholar]
- [13].Seng KY, Lee Peter VS, Lam PM. Neck muscle strength across the sagittal and coronal planes: an isometric study. Clin Biomech (Bristol, Avon) 2002;17:545–7. [DOI] [PubMed] [Google Scholar]
- [14].Committee on Hearing and Equilibrium. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere's disease. American Academy of Otolaryngology-Head and Neck Foundation, Inc. Otolaryngol Head Neck Surg 1995;113:181–5. [DOI] [PubMed] [Google Scholar]
- [15].Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607–24. [PubMed] [Google Scholar]
- [16].Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg 1958;15:602–17. [DOI] [PubMed] [Google Scholar]
- [17].Colledge NR, Barr-Hamilton RM, Lewis SJ, et al. Evaluation of investigations to diagnose the cause of dizziness in elderly people: a community based controlled study. BMJ 1996;313:788–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Jeong SY, Eun JP, Oh YM. Magnetic resonance imaging analysis of deep cervical flexors in patients with ossification of the posterior longitudinal ligament and clinical implication. Am J Phys Med Rehabil 2015;94:967–74. [DOI] [PubMed] [Google Scholar]
- [19].Falla DL, Jull GA, Hodges PW. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine 2004;29:2108–14. [DOI] [PubMed] [Google Scholar]
- [20].Javanshir K, Mohseni-Bandpei MA, Rezasoltani A, et al. Ultrasonography of longus colli muscle: a reliability study on healthy subjects and patients with chronic neck pain. J Bodywork Mov Ther 2011;15:50–6. [DOI] [PubMed] [Google Scholar]
- [21].Javanshir K, Rezasoltani A, Mohseni-Bandpei MA, et al. Ultrasound assessment of bilateral longus colli muscles in subjects with chronic bilateral neck pain. Am J Phys Med Rehabil 2011;90:293–301. [DOI] [PubMed] [Google Scholar]
- [22].Cagnie B, D’Hooge R, Achten E, et al. A magnetic resonance imaging investigation into the function of the deep cervical flexors during the performance of craniocervical flexion. J Manipulative Physiol Ther 2010;33:286–91. [DOI] [PubMed] [Google Scholar]
- [23].Falla D, Jull G, Hodges PW. Feedforward activity of the cervical flexor muscles during voluntary arm movements is delayed in chronic neck pain. Exp Brain Res 2004;157:43–8. [DOI] [PubMed] [Google Scholar]
- [24].Saylam CY, Ozgiray E, Orhan M, et al. Neuroanatomy of cervical sympathetic trunk: a cadaveric study. Clin Anat 2009;22:324–30. [DOI] [PubMed] [Google Scholar]
- [25].Ibrahim M, Parmar H, Yang L. Horner syndrome associated with contusion of the longus colli muscle simulating a tumor. J Neuroophthalmol 2010;30:70–2. [DOI] [PubMed] [Google Scholar]
- [26].Yoo HS, Nahm FS, Lee PB, et al. Early thoracic sympathetic block improves the treatment effect for upper extremity neuropathic pain. Anesth Analg 2011;113:605–9. [DOI] [PubMed] [Google Scholar]
- [27].Rocha Rde O, Teixeira MJ, Yeng LT, et al. Thoracic sympathetic block for the treatment of complex regional pain syndrome type I: a double-blind randomized controlled study. Pain 2014;155:2274–81. [DOI] [PubMed] [Google Scholar]
- [28].Yu Z, Liu Z, Dang G. Effect of cervical instability in sympathetic cervical spondylosis. Zhonghua Wai Ke Za Zhi [Chinese journal of surgery] 2002;40:881–5. [PubMed] [Google Scholar]
- [29].Li J, Gu T, Yang H, et al. Sympathetic nerve innervation in cervical posterior longitudinal ligament as a potential causative factor in cervical spondylosis with sympathetic symptoms and preliminary evidence. Med hypotheses 2014;82:631–5. [DOI] [PubMed] [Google Scholar]
- [30].Hong L, Kawaguchi Y. Anterior cervical discectomy and fusion to treat cervical spondylosis with sympathetic symptoms. J Spinal Disord Tech 2011;24:11–4. [DOI] [PubMed] [Google Scholar]
- [31].Moon HJ, Goo BO, Cho SH. The effect of cocontraction of the masticatory muscles during neck stabilization exercises on thickness of the neck flexors. J Phys Ther Sci 2015;27:659–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Jull G, Barrett C, Magee R, et al. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia 1999;19:179–85. [DOI] [PubMed] [Google Scholar]
- [33].Gong W. Impact of longus colli muscle massage on the strength and endurance of the deep neck flexor muscle of adults. J Phys Ther Sci 2013;25:591–3. [DOI] [PMC free article] [PubMed] [Google Scholar]


