Abstract
Knee osteoarthritis (KOA) is a common disease in middle-aged and elderly people. Pain is the chief complaint of symptomatic KOA and a leading cause of chronic disability, which is most often found in medial knees. The aim of this study is to evaluate the efficacy of pain relief and functional improvement in KOA patients treated with ultrasound-guided adductor canal block (ACB).
This is a 3-month retrospective case-controlled comparative study. Two hundred patients with anteromedial knee pain owing to KOA that was unresponsive to 3-month long conservative treatments. Ninety-two patients received ACB with 9 mL of 1% of lidocaine and 1 mL of 10 mg triamcinolone acetonide (ACB group), and 108 continued conservative treatments (control group). The main outcome measure was visual analog scale (VAS) of the average knee pain level for the past one week. Secondary outcomes were the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the timed up and go test, numbers of analgesic ingestion per day, and opioid consumption per day.
During the 3-month follow-up, 86 patients in ACB group and 92 in control group were analyzed. There was no significant difference, with the exception of the duration of symptoms, between the 2 groups in age, sex, body mass index, and Kellgren-Lawrence grade. Repeated-measures analysis of variance and post hoc tests showed improvement of VAS (at month 1), WOMAC (at month 1), and opioid consumption per day (at month 1 and 2) in ACB group. No adverse events were reported.
To our knowledge, this is the first study to assess the efficacy of ACB for patients with KOA. ACB is an effective and safe treatment and can be an option for patients who are either unresponsive or unable to take analgesics.
Keywords: arthritis, knee joint, knee pain, nerve block, osteoarthritis
1. Introduction
Knee osteoarthritis (KOA) is a common disease in middle-aged and elderly people. Pain is the chief complaint of symptomatic KOA and a leading cause of chronic disability [1] which is most often found in medial knees.[2,3] Management of patients with knee pain requires a combination of pharmacological and nonpharmacological treatments, including surgical interventions when necessary.[4]Pharmacological treatments would often be the first option, and if pain still continues, rehabilitation including exercises and physical therapies may be added as part of nonpharmacological interventions, on top of pharmacological treatments.[5]
The saphenous nerve is the pure sensory branch of the femoral nerve. It runs laterally to the femoral artery, and then enters the adductor canal (Hunter canal, or sartorius canal) where it crosses in front of the femoral artery. The saphenous nerve provides an extensive cutaneous innervation over the anteromedial side of the knee, lower leg, and foot.[6] Saphenous nerve block, used in the leg during the surgical anesthesia,[7] can help increase the success rate of saphenous nerve block in the adductor canal (adductor canal block, ACB) when performed with an ultrasound-guided approach.[8] Recent studies have reported the efficacy of ACB in the management of analgesia following total knee arthroplasty [9–12] and post-meniscectomy.[13] In addition, the administration of ACB may be accomplished also as a single-shot injection after total knee arthroplasty.[12,14] However, no study has yet reported the efficacy of ACB for KOA. The aim of this study is to evaluate the efficacy of ultrasound-guided ACB as a therapeutic option for refractory anteromedial knee pain owing to KOA.
2. Methods
2.1. Study design and subjects
This is a retrospective case-controlled comparative study. After the approval of the institutional review board, medical records of 292 patients who were diagnosed with KOA with anteromedial pain between January 2010 and April 2015 were reviewed. They were outpatients at the rehabilitation and orthopedic clinics of the university hospital. All patients underwent a standardized history-taking, physical examination, blood test, and knee x-rays. Inclusion criteria were patients diagnosed as having symptomatic bilateral KOA according to the criteria of the American College of Rheumatology;[15] grade of Kellgren–Lawrence grading scale (a scoring tool used to assess the severity of knee osteoarthritis on a plain radiograph)[16] 2 to 4 of KOA; age 50 years and above; reporting at least 6-month duration of symptoms; having matching symptom (anteromedial knee pain) and simple x-ray findings with KOA; and with direct tenderness on anteromedial aspect of the knee owing to KOA. Exclusion criteria were the presence of other obvious knee pathology, such as fracture, or rheumatic diseases; referred pain from the lower back suggestive of lumbar radiculopathy; previous surgery to the knee; knee synovitis; and abnormal sensory perception suggestive of injury or entrapment of saphenous nerve.
Two hundred ninety-two patients were diagnosed to have KOA and underwent conservative treatment for at least 3 months before the ACB (Fig. 1). We prescribed analgesics including acetaminophen, nonsteroidal anti-inflammatory drugs, tricyclic antidepressant, selective serotonin and norepinephrine reuptake inhibitor, tramadol, and opioids. Acetaminophen was prescribed for first-line use, with nonsteroidal anti-inflammatory drugs and opioids as second and third lines of treatment according to the guidelines.[5,17] When pain mitigated, the reverse order was applied to reduce the dosage. Patients had institutional flexibility and strengthening exercise of quadriceps with physical therapists 1 or 2 times a week for 4 to 8 weeks, and were educated to carry out the same exercise at home. Patients who could not accommodate regular exercise at the hospital were given educational leaflets and instruction by physical therapists at each outpatient follow-up. When a patient entered the inflammatory phase of osteoarthritis such as increased fluid in the joint, ultrasonography-guided intra-articular corticosteroid injection with triamcinolone acetonide 20 mg was administered.
Figure 1.
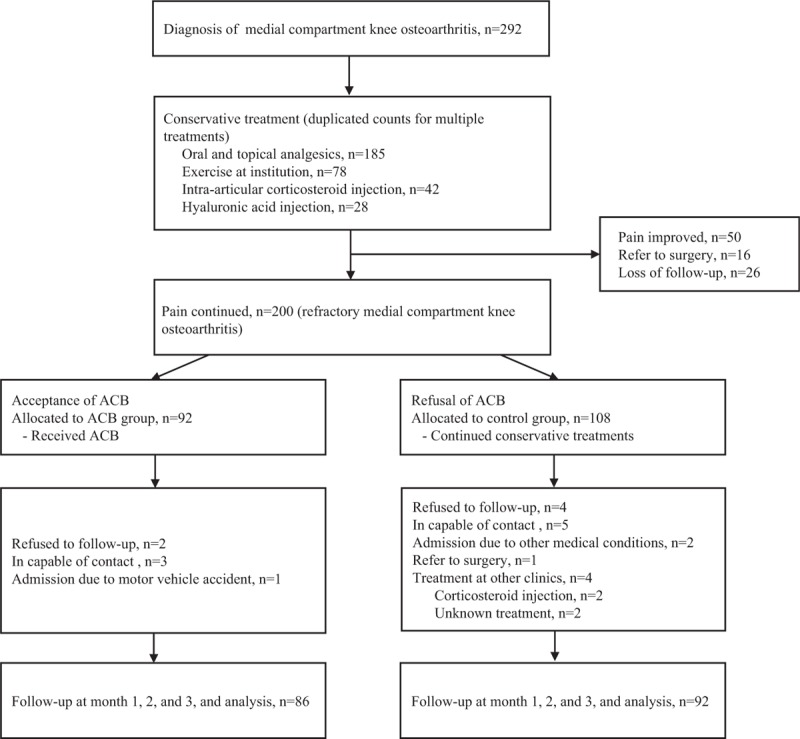
Flow diagram indicating progress of subjects through the study.ACB = adductor canal block.
If despite the conservative treatment, a patient continued to complain about knee pains with score ≥4 on a visual analog scale (VAS) of the average knee pain level for the past 1 week, we recommended ACB explaining also its indication and complications. Patients were free to choose either the ACB or other treatment options. Patients were given a choice to unilateral or bilateral injection depending on the level of pain. Among 200 patients with refractory KOA, 92 opted for ACB (ACB group) and 108 for conservative treatments (control group) including analgesics and exercise.
2.2. ACB
The patients in the ACB group received an ultrasound-guided single-shot ACB, based on earlier studies.[18,19] ACB was performed at mid-thigh (midpoint between the knee and the inguinal crease) by the lead author with ultrasound equipment (Logiq P6, GE Healthcare, Buckinghamshire, UK) using a 10 to 13 Hz high-frequency linear ultrasound transducer which was placed transverse to the longitudinal axis of the leg. Underneath the sartorius muscle, the saphenous nerve was identified in a short axis view as it descends lateral to the femoral artery in the adductor canal. The lead author injected 9 mL of 1% of lidocaine and 1 mL of 10 mg triamcinolone acetonide with a 23-gauge 6-cm long needle.
2.3. Outcome measurements
VAS for knee pain intensity, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the timed up and go test, and numbers of analgesic ingestion per day, and opioid consumption per day were compared for pre-, and 1, 2, and 3 months post-injection. All outcome measurements were evaluated by the lead author. The primary outcome measure was VAS of the average knee pain level for the past 1 week. Patients answered the question “With respect to the worst pain you have experienced in your life, what was the average level of your knee pain in the past one week?? by placing a mark somewhere along the 10-cm horizontal line between 2 end-points (left: “No pain" and right: “the worst imaginable pain." WOMAC is a self-reporting questionnaire for patients with KOA, which consists of 24 items that are divided into 3 subscales: pain (5 items), stiffness (2 items), and physical function (17 items).[20] The timed up and go test is a reliable test with adequate minimal detectable change for clinical use in individuals with KOA.[21,22] Numbers of analgesic ingestion per day were measured based on the average number of analgesics patients have taken per day during the past 1 week. Opioid consumption per day is the past 1 week's average value of opioids consumed by patients per day, which has been converted to the morphine equivalent dose.
2.4. Statistical analysis
After a normality test, we compared 2 groups in terms of age, sex, duration of symptoms, Kellgren-Lawrence grade, and body mass index by performing independent t- or χ2 analysis. The effect of injection during 3 months was evaluated with repeated-measures analysis of variance. If the repeated-measures analysis of variance for group-by-time interaction was significant, post hoc tests (Bonferroni) of between-group comparison were conducted. The P value was adjusted using the Bonferroni method. Significance was accepted for P values of <0.05. All these analyses were performed using SPSS statistical software, version 22 (IBM, Armonk, NY).
3. Results
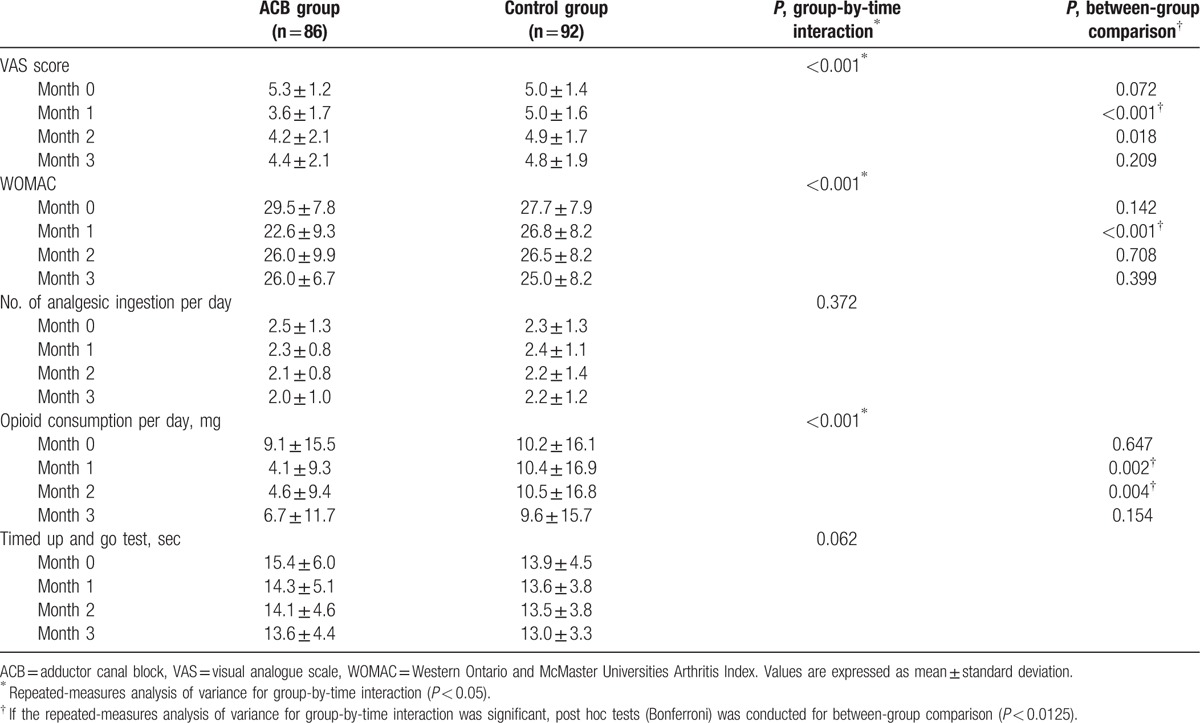
Out of a total of 200 refractory KOA patients, 92 received ACB and 108 current conservative treatments (Fig. 1). Of them, respectively 86 and 92 patients were included in the final analysis. Among the ACB group, 70 patients (81.4%) received bilateral and 16 (18.6%) unilateral ACB injection. Table 1 lists the baseline characteristics of the study subjects. There were no statistical differences between the 2 groups in terms of age, sex, body mass index, and Kellgren-Lawrence grade, except for the duration of symptoms which lasted longer in the ACB group (8.1 ± 4.4 vs. 6.8 ± 4.1 years). Table 2 shows the changes of outcome measurements of ACB and control groups. Repeated-measures analysis of variance showed significant effect of time in all outcome measurements (P < 0.001). This means that compared to pretreatment, all outcome measures improved significantly in both groups with time. Group-by-time interactions were significant for VAS, WOMAC, and opioid consumption per day between groups (P < 0.001). Post hoc tests for between-group comparisons revealed that there are significant differences in VAS and WOMAC at month 1, and opioid consumption per day at month 1 and 2. There were no adverse events reported such as bleeding, infection, cellulitis, or weakness.
Table 1.
Baseline characteristics of patients.
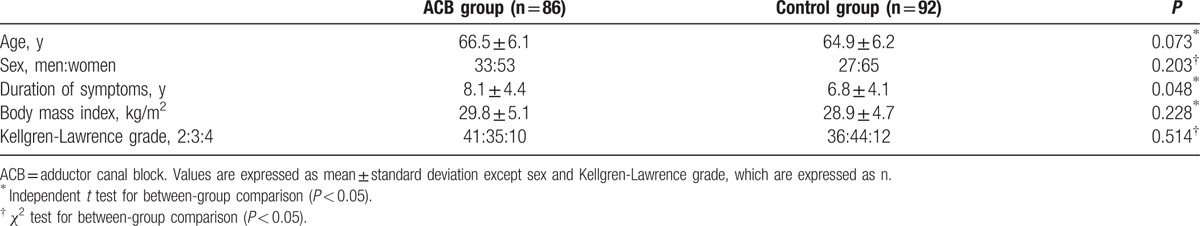
Table 2.
Changes of outcome measurements.
4. Discussion
ACB has often been used to control pain after the anesthesia and operation of the lower leg[7,9–12,14] and has been reported to be effective on knee pains caused by saphenous nerve neuropathy and postmeniscectomy pain.[13,23] To our best knowledge, this is the first study to evaluate the efficacy of ACB in KOA. In this 3-month follow-up study, ACB was used to treat patients who had anteromedial knee pain owing to KOA but failed 3-month-long conservative treatments. The ACB group showed improvement in VAS (at month 1), WOMAC (at month 1), and opioid consumption per day (at month 1 and 2), compared to the control group. KOA is very common and the medial compartment is affected most frequently than other areas.[2,3] ACB is easily performed at the outpatient clinic and can reduce pain up to at least 1 month for patients with KOA who continue to show no response to analgesics.
Adductor canal is an aponeurotic tunnel in the middle third of the thigh composed medially of the adductor longus, laterally of the vast us medialis, and interiorly of the sartorius and the subsartorial fascia. ACB blocks the largest sensory contributions from the femoral nerve to the knee, the saphenous nerve.[10,24] In addition to the saphenous nerve, the adductor canal contains the nerve to the vastus medialis, the medial femoral cutaneous nerve, the medial retinacular nerve, and the articular branches from the posterior division of obturator nerve which enters the distal part of the canal. Except for the nerve to the vastus medialis, these branches have a sole sensory function, and most of them play a major role in the sensory innervation of the knee region. Many trials have recently hypothesized that administration of local anesthetic into the ACB could be a useful option for postoperative analgesia after total knee arthroplasty.[9–12] Since KOA is a disease of the entire knee joint, the cause of knee pain can origin not only from degenerative changes of cartilages and bones, such as cartilage wearing, sclerosis of subchondral bone, and osteophytes, but also from tears and subluxation of menisci, sprain of ligaments, tendinitis, bursitis, and synovitis.[1,25–27] As part of its mechanism, ACB is thought to interrupt the pain signal, which originates from various lesions of KOA.
The saphenous nerve departs from the adductor canal in the distal thigh, piercing the fascia between the sartorius and gracilis muscles to become subcutaneous.[30] From this point, the saphenous nerve is first divided distally into 2 branches, sartorial and infrapatellar,[28,29] and then again into multiple small subcutaneous branches. This makes it hard to identify the nerve in more distal locations. In a cadaveric study, the authors found that the saphenous nerve divides into 2 branches from outside the adductor canal at a mean of 2.7 cm proximal to the base of the patella. They reported the block at this location to be successful.[8] In the present study, we blocked the saphenous nerve in the middle of the adductor canal. Ultrasonography was used to identify the entry point of the needle, on average 10 cm proximal to the knee crease. This is an ideal location to block the nerve while using the femoral artery as a landmark. It is also proximal enough to ensure the blocking of both main branches, sartorial and infrapatellar.[18]
Although no difference was found between the 2 groups in terms of the number of analgesic (opioids included) ingestion per day, the ACB group was found to have consumed less opioids per day in month 1 and 2. The difference came from the fact that we had reduced the opioids first among other prescribed analgesics when pain resided and educated the patients to switch to acetaminophen or nonsteroidal anti-inflammatory drugs according to the treatment guidelines.[5,17] Therefore, it was possible for opioid consumption to go down but not the total number of analgesic intake. Although claiming the long-term effect of a single round of ACB in lowering the opioid dosage may be farfetched, there is a clear advantage of ACB in reducing the usage of opioid at least during the first 2 months. Taking into account the common adverse events of opioids that can occur in elderly patients (cognitive impairment, delirium related falls and fractures, depression, cardiovascular events, and pneumonia),[31,32] it may be possible to consider a combined therapy of ACB over additional opioid intake for patients who complain transient acute pain.
We used 10 mL of anesthetic for ACB in this study. The volume of anesthetic that is going to be used needs to be considered as one of the factors impacting the analgesia and side effects of ACB. Although not enough of the anesthetic may result in an insufficient analgesic effect, too much can lead to an undesirable anesthesia or weakness owing to the blocking of the femoral or sciatic nerves, as the adductor canal is connected proximally to the femoral triangle and extended to the adductor hiatus to distally connect with the popliteal fossa.[33,34] Previous trials that administered ACB after a knee surgery have used 10 to 30 mL.[10,13,35] ACBs that used volume of 20 mL have reported sufficient pain relief while at the same time finding little or no weakness owing to femoral nerve blockades.[35–37] However, recent studies have reported that even a volume of <20 mL may affect the femoral or sciatic nerve or branches. In one cadaveric study, 15 mL of injectate that was administered into the adductor canal spread proximally to the femoral triangle and distally to the adductor hiatus.[34] And the results of a study that evaluated the electromyographic activity of vastus medialis and lateralis and muscle weakness of quadriceps femoirs by administering 10, 20, and 30 mL of 1% lidocaines to 20 volunteers showed a strong association between volume and vastus medialis effects. A volume of 30 mL resulted in an affection in all subjects, a volume of 20 mL resulted in an affection in 84% of the subjects, whereas a volume of 10 mL only resulted in an affection in 35% of the subjects.[38] We asked patients whether they had any weakness of quadriceps before ACB and upon follow-up; however, none of the patient reported any weakness. Still, as no quadricep muscle power or electromyographic activity was used for the measurement, we were not able to identify whether the volume used had impacted femoral or scitic nerves. As there is no consensus on how different volumes affect analgesic effect and quadriceps weakness, patients should be monitored for motor strength to reduce the risk of fall.
The greatest limitation of this study lies in the fact that it is a retrospective study and that the group allocation was not randomized. Patients chose to take the therapy according to their own will, and no randomization process was involved. Nonetheless, it has relatively low drop-out rate (11.0% in total), a large sample size (N = 178), enough follow-up period (3 months) to monitor the effect of ACB, and consistent baseline characteristics (age, sex, body mass index, and Kellgren-Lawrence grade) across both groups compared. It also includes at least 3 rounds of follow-ups (at month 1, 2, and 3) after ACB to monitor whether other treatments have been received, which was a part of the effort to reduce bias as much as possible. Second, the aim of this study was to evaluate the changes in the long-term evaluation (1, 2, and 3 months) of pain and function of ACB; therefore, the outcome measurement immediately after ACB was not measured. However, the fact that sensory evaluation was not performed to confirm the success of sensory blockade can be a limitation. Third, not only are there many factors impacting pain including psychological and environmental factors, drugs, stress, and concomitant diseases, but also great changes that take place between these factors with time. In an effort to take these into consideration, we tried to identify mid-term changes in pain rather than immediate changes claimed on the day of the follow-up visit. VAS of the average knee pain level for the past 1 week was therefore used as our tool. However, this tool may have a greater recall bias than the ordinary VAS.
In conclusion, this study looked into the possibility of ACB as an alternative treatment for anteromedial knee pain owing to KOA. Although a palliative treatment, and not one that stops the progression of the disease or changes its natural course, ACB can be an option for patients with refractory KOA who cannot take or are not responsive to analgesics. However, to prove the efficacy of ACB, further studies on prospective randomized controlled trials would be needed to overcome the limitations mentioned in the discussions.
Acknowledgment
The authors thank Aeree Park, MA, for English translation of Korean manuscript.
Footnotes
Abbreviations: ACB = adductor canal block, KOA = knee osteoarthritis, VAS = visual analogue scale, WOMAC = the Western Ontario and McMaster Universities Osteoarthritis Index.
The authors report no conflicts of interest.
References
- [1].Torres L, Dunlop DD, Peterfy C, et al. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage 2006;14:1033–40. [DOI] [PubMed] [Google Scholar]
- [2].Dearborn JT, Eakin CL, Skinner HB. Medial compartment arthrosis of the knee. Am J Orthop (Belle Mead NJ) 1996;25:18–26. [PubMed] [Google Scholar]
- [3].Ledingham J, Regan M, Jones A, et al. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Ann Rheum Dis 1993;52:520–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64:465–74. [DOI] [PubMed] [Google Scholar]
- [5].Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008;16:137–62. [DOI] [PubMed] [Google Scholar]
- [6].Hadzic A. Textbook of Regional Anesthesia and Acute Pain Management. 2007;New York: McGraw-Hill, Medical Pub Division, 43–77. [Google Scholar]
- [7].van der Wal M, Lang SA, Yip RW. Transsartorial approach for saphenous nerve block. Can J Anaesth 1993;40:542–6. [DOI] [PubMed] [Google Scholar]
- [8].Horn JL, Pitsch T, Salinas F, et al. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med 2009;34:486–9. [DOI] [PubMed] [Google Scholar]
- [9].Jenstrup MT, Jaeger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand 2012;56:357–64. [DOI] [PubMed] [Google Scholar]
- [10].Lund J, Jenstrup MT, Jaeger P, et al. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand 2011;55:14–9. [DOI] [PubMed] [Google Scholar]
- [11].Jaeger P, Koscielniak-Nielsen ZJ, Schroder HM, et al. Adductor canal block for postoperative pain treatment after revision knee arthroplasty: a blinded, randomized, placebo-controlled study. PLoS One 2014;9:e111951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ludwigson JL, Tillmans SD, Galgon RE, et al. A Comparison of single shot adductor canal block versus femoral nerve catheter for total knee arthroplasty. J Arthroplasty 2015;30:68–71. [DOI] [PubMed] [Google Scholar]
- [13].Akkaya T, Ersan O, Ozkan D, et al. Saphenous nerve block is an effective regional technique for post-menisectomy pain. Knee Surg Sports Traumatol Arthrosc 2008;16:855–8. [DOI] [PubMed] [Google Scholar]
- [14].Shah NA, Jain NP, Panchal KA. Adductor canal blockade following total knee arthroplasty-continuous or single shot technique? Role in postoperative analgesia, ambulation ability and early functional recovery: a randomized controlled trial. J Arthroplasty 2015;30:1476–81. [DOI] [PubMed] [Google Scholar]
- [15].Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 1986;29:1039–49. [DOI] [PubMed] [Google Scholar]
- [16].Emrani PS, Katz JN, Kessler CL, et al. Joint space narrowing and Kellgren-Lawrence progression in knee osteoarthritis: an analytic literature synthesis. Osteoarthritis Cartilage 2008;16:873–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Richmond J, Hunter D, Irrgang J, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of osteoarthritis (OA) of the knee. J Bone Joint Surg Am 2010;92:990–3. [DOI] [PubMed] [Google Scholar]
- [18].Manickam B, Perlas A, Duggan E, et al. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med 2009;34:578–80. [DOI] [PubMed] [Google Scholar]
- [19].Krombach J, Gray AT. Sonography for saphenous nerve block near the adductor canal. Reg Anesth Pain Med 2007;32:369–70. [DOI] [PubMed] [Google Scholar]
- [20].Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–40. [PubMed] [Google Scholar]
- [21].Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142–8. [DOI] [PubMed] [Google Scholar]
- [22].Alghadir A, Anwer S, Brismee JM. The reliability and minimal detectable change of Timed Up and Go test in individuals with grade 1-3 knee osteoarthritis. BMC Musculoskelet Disord 2015;16:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Taheri A, Hatami M, Dashti M, et al. Effect of ultrasound-guided subsartorial approach for saphenous nerve block in cases with saphenous nerve entrapment in adductor canal for controlling chronic knee pain. Middle East J Anaesthesiol 2015;23:25–8. [PubMed] [Google Scholar]
- [24].Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res 1994;221–6. [PubMed] [Google Scholar]
- [25].Hill CL, Hunter DJ, Niu J, et al. Synovitis detected on magnetic resonance imaging and its relation to pain and cartilage loss in knee osteoarthritis. Ann Rheum Dis 2007;66:1599–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Naredo E, Cabero F, Palop MJ, et al. Ultrasonographic findings in knee osteoarthritis: a comparative study with clinical and radiographic assessment. Osteoarthritis Cartilage 2005;13:568–74. [DOI] [PubMed] [Google Scholar]
- [27].Yoon HS, Kim SE, Suh YR, et al. Correlation between ultrasonographic findings and the response to corticosteroid injection in pes anserinus tendinobursitis syndrome in knee osteoarthritis patients. J Korean Med Sci 2005;20:109–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lundblad M, Kapral S, Marhofer P, et al. Ultrasound-guided infrapatellar nerve block in human volunteers: description of a novel technique. Br J Anaesth 2006;97:710–4. [DOI] [PubMed] [Google Scholar]
- [29].Hunter LY, Louis DS, Ricciardi JR, et al. The saphenous nerve: its course and importance in medial arthrotomy. Am J Sports Med 1979;7:227–30. [DOI] [PubMed] [Google Scholar]
- [30].Mansour NY. Sub-sartorial saphenous nerve block with the aid of nerve stimulator. Reg Anesth 1993;18:266–8. [PubMed] [Google Scholar]
- [31].O’Neil CK, Hanlon JT, Marcum ZA. Adverse effects of analgesics commonly used by older adults with osteoarthritis: focus on non-opioid and opioid analgesics. Am J Geriatr Pharmacother 2012;10:331–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Scherrer JF, Salas J, Copeland LA, et al. Increased risk of depression recurrence after initiation of prescription opioids in noncancer pain patients. J Pain 2016;17:473–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Gautier PE, Hadzic A, Lecoq JP, et al. Distribution of Injectate and Sensory-Motor Blockade After Adductor Canal Block. Anesth Analg 2016;122:279–82. [DOI] [PubMed] [Google Scholar]
- [34].Andersen HL, Andersen SL, Tranum-Jensen J. The spread of injectate during saphenous nerve block at the adductor canal: a cadaver study. Acta Anaesthesiol Scand 2015;59:238–45. [DOI] [PubMed] [Google Scholar]
- [35].Abdallah FW, Whelan DB, Chan VW, et al. Adductor canal block provides noninferior analgesia and superior quadriceps strength compared with femoral nerve block in anterior cruciate ligament reconstruction. Anesthesiology 2016;124:1053–64. [DOI] [PubMed] [Google Scholar]
- [36].Jaeger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med 2013;38:526–32. [DOI] [PubMed] [Google Scholar]
- [37].Perlas A, Kirkham KR, Billing R, et al. The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med 2013;38:334–9. [DOI] [PubMed] [Google Scholar]
- [38].Grevstad U, Jaeger P, Sorensen JK, et al. The effect of local anesthetic volume within the adductor canal on quadriceps femoris function evaluated by electromyography: a randomized, observer- and subject-blinded, placebo-controlled study in volunteers. Anesth Analg 2016;123:493–500. [DOI] [PubMed] [Google Scholar]


