Abstract
Due to the current lack of standard definitions for rapidly progressive osteoarthritis of the hip (RPOH) in the literature, this observational study aimed to describe new diagnostic criteria and a grading system for the disease.
From a consecutive series of patients undergoing total hip replacement, 2 groups were selected: 1 with RPOH and 1 with primary hip osteoarthritis (POH), and their clinical, paraclinical, and demographic data were compared. The newly proposed clinico-radiological diagnostic criteria are based on characteristics of pain, joint mobility, and radiological assessment. The radiological grading system's inter- and intraobserver reliability was assessed through serial evaluations by 2 blinded reviewers.
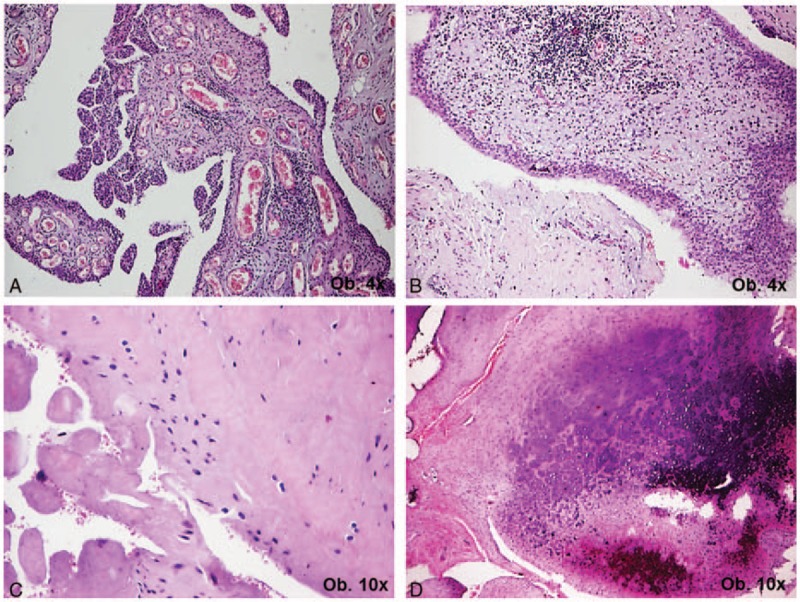
From the total 863 cases, 82 cases (9.5%) of RPOH were identified and compared with 107 cases of POH. Mean age and disease bilaterality were similar, with a predominance of female patients in the RPOH group (P = 0.03). There were significant differences between the 2 groups in disease onset and aggravation, and intraoperative blood loss. The grading system showed significant inter- and intraobserver agreement (weighted kappa 0.93, and 0.89).
Our study presents distinctive, easily recognizable clinico-radiological characteristics of RPOH and confirmed the inter- and intraobserver reliability of the newly proposed grading system.
Keywords: clinical, diagnostic criteria, primary hip osteoarthritis, radiological, rapidly progressive hip osteoarthritis
1. Introduction
Rapidly progressive osteoarthritis of the hip (RPOH), also known as rapidly destructive arthritis/osteoarthritis/hip disease is considered a rare syndrome that can lead to joint destruction in as little as 6 months to 3 years. First reported by Postel and Kerboull in 1970,[1] the disease was defined by Lequesne as chondrolysis >2 mm in 1 year, or 50% joint-space narrowing in 1 year,[2] associated with no evidence of other forms of rapidly destructive arthropathy, such as osteonecrosis or Charcot neuroarthropathy.
The etiology of the disease is still unclear, and only a few case series and case reports have been published in the literature. The hypothesized pathologic mechanisms involved include drug toxicity, cytokine-mediated immunological mechanisms, autoimmune reactions, or subchondral insufficiency fractures.[1,3–8] Although the histological degenerative changes are usually similar to those occurring in primary osteoarthritis of the hip (POH),[9] the rapid evolution, rate and severity of joint destruction, as well as some radiographic features clearly differentiate RPOH from primary osteoarthritis (OA).
The most obvious concern regarding RPOH is the possible poor outcome of patients if treatment is delayed. Temporizing surgical management in these cases might lead to considerable difficulties in total hip replacement (THR) due to the potentially severe loss of bone stock that can occur in as little as a few months after diagnosis. Considering that currently there are no standard definitions used in the literature for RPOH, and that diagnostic criteria described by Lequesne involve following the patient in evolution for 12 months, we considered it necessary to establish a new, more practical set of clinico-radiological criteria for diagnosing and grading the disease. This study was aimed to describe these new criteria and grading system in a series of patients undergoing THR, and to offer some additional data about the epidemiological features of RPOH, as well as to raise awareness of this particular pathology.
2. Patients and methods
Our analysis was based on the assessment of a consecutive series of patients treated by THR by the senior author in our institution between January 2006 and December 2015. The protocol of this STROBE-compliant retrospective observational study was approved by the hospital's local Ethics Committee (2846/15.02.2016). Data were retrieved from patient records, and from this larger series of patients, a group was identified that had a history of rapid destruction of the hip joint—from these cases, patients with a clear diagnosis of (or clinical or laboratory results that could imply) infectious, metabolic, endocrine, or neurologic disorders were excluded in order to select only cases of RPOH. Based on this latter patient group's history, clinical and radiological features, the newly proposed clinic-radiological diagnosis criteria for RPOH were formulated (Table 1). They were developed in order to identify cases of RPOH by corroborating patient history and clinical data with a single time point radiological observation of the hip joint.
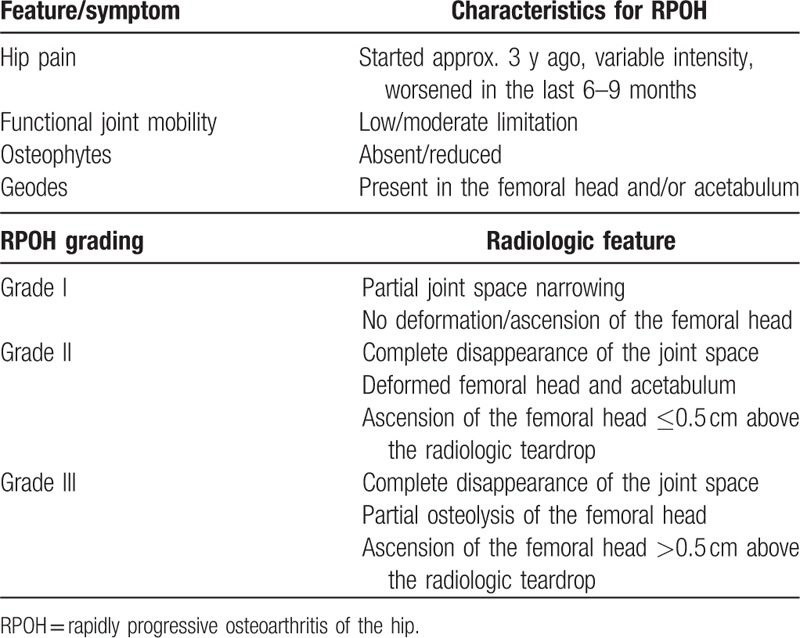
Table 1.
The newly proposed clinic-radiologic diagnostic criteria and radiologic grading system for rapidly progressive osteoarthritis of the hip.
In a next step, the established group of patients with a diagnosis of RPOH was compared to a consecutive series of patients that underwent THR for POH between January 2014 and December 2015 (selected from the previous larger series). The comparison was based on clinical and demographic data, as well as intraoperative data (appearance of bone and soft tissues, blood loss, etc.), and immediate postoperative complications. Where available, the results of the histopathologic assessment of tissue samples obtained intraoperatively (femoral head, synovial tissue fragments) were also recorded for both RPOH and POH.
Besides the new diagnostic criteria for RPOH, Table 1 also contains the proposed radiologic grading system. The inter- and intraobserver reliability of the radiological grading system was assessed based on the results of serial evaluations performed by 2 blinded reviewers on AP and axial radiographs of the hip/pelvis.
Statistical Package for Social Sciences (SPSS, version 20, Chicago, IL) was used for the statistical analysis; data were considered normal or quantitative variables. Frequencies were used for normal variables, while quantitative variables were tested for normal distribution using the Kolmogorov–Smirnov test, and characterized by median and percentages (25–75%) with interquartile range (IQR), or mean and range when appropriate. The Mann–Whitney test was used for comparing variables, while inter- and intraobserver differences in RPOH grading were determined using the Bland–Altman method. Statistical significance was set at P < 0.05.
3. Results
Specific radiographic examples of anteroposterior (AP) and axial views of hips with grades I–III of RPOH based on our newly proposed criteria and found in the studied series of patients are presented in Figs. 1 to 3, with Fig. 3 showing a case of bilateral disease and the method for evaluating femoral head ascension.
Figure 1.
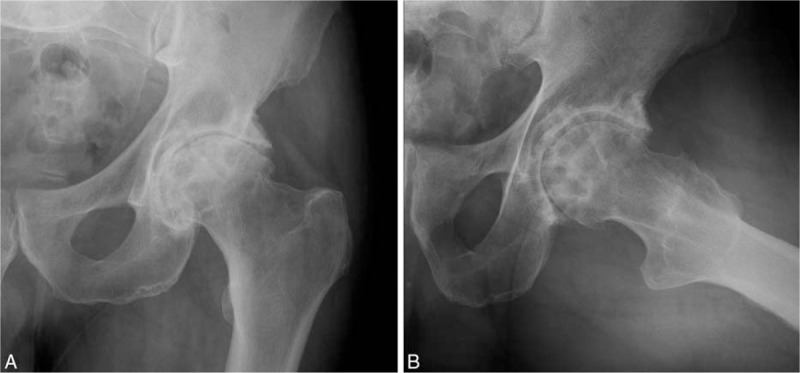
Grade I RPOH in a 69 years old male patient: AP (A) and axial (B) views of the left hip show partial joint space narrowing and clearly visible geodes in both the acetabulum and femoral head, creating and inhomogeneous aspect. The femoral head is not deformed or ascended.
Figure 3.
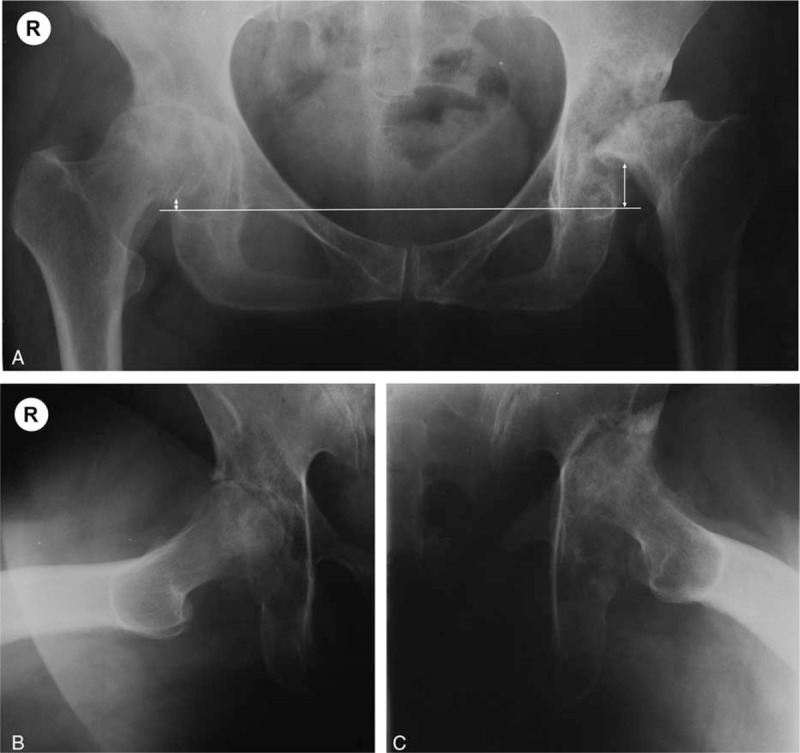
Bilateral RPOH in a 64 years old female patient—AP view of the pelvis (A), and axial views of the right (B) and left (C) hip. Femoral head ascension was determined on the AP view of the pelvis: the horizontal line connects the radiologic teardrops, while the vertical lines connect the horizontal to the inferior junction of the femoral head and neck. The right hip presents grade II RPOH, while the left hip is grade III: complete disappearance of the joint line, multiple geodes and deforming of the acetabulum and femoral head, major femoral head osteolysis and ascension >0.5 cm above the level of the radiological teardrop.
Figure 2.
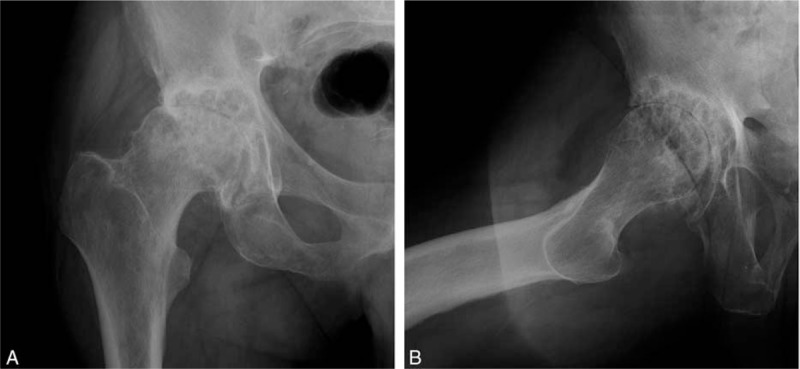
Grade II RPOH in a 78 years old male patient: AP (A) and axial (B) views of the right hip show complete disappearance of the joint space, associated with femoral head deformation, but minimal ascension. Many geodes are present in the acetabulum and femoral head, but there is no evident osteolysis of the latter.
A total of 863 cases (754 patients) were included in the epidemiological assessment, with 82 cases (9.5%) identified as RPOH based on the above mentioned criteria—their distribution is shown in Table 2.
Table 2.
Diagnosis distribution of cases undergoing total hip replacement by the senior author between January 2006 and December 2015.
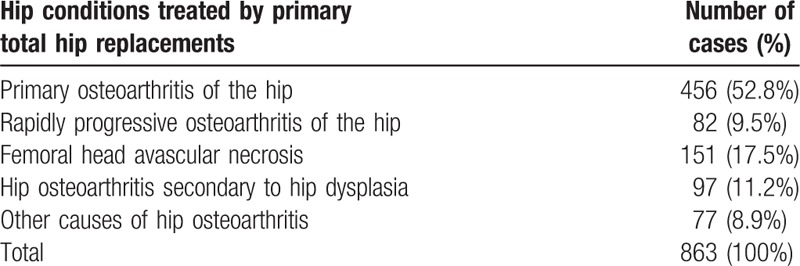
The 67 patients with RPOH (15 bilateral cases, with a total of 82 hips) were compared to a consecutive series of 93 patients with POH (14 bilateral cases, with a total of 107 hips). Mean age was similar in the 2 groups, while sex distribution showed a predominance of female patients in the RPOH group (P = 0.03). Although there were also differences in disease bilaterality, these did not reach statistical significance (P = 0.68, Table 3).
Table 3.
Demographic data in the 2 compared series of patients (primary vs rapidly progressive osteoarthritis of the hip).
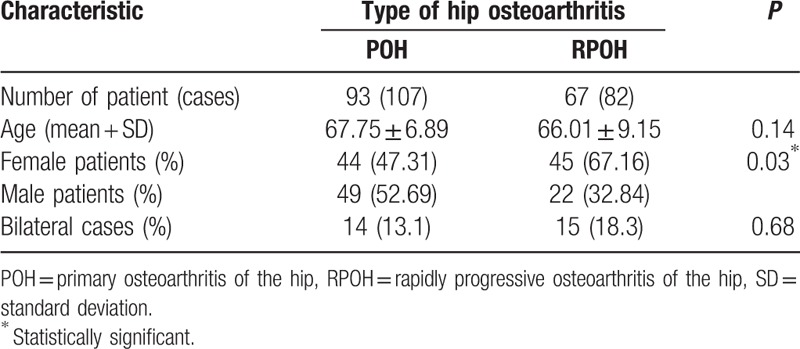
The principal symptom in all patients was hip pain, with onset of a median of 3 years (IQR 7) before THR in patients with RPOH, compared to the median of 5 years (IQR 19) in POH; thus there was a highly significant difference in disease onset (P = 0.0001, Mann–Whitney test, Fig. 4A). The same was true for disease aggravation, that showed a median of 6 months (IQR 46) in RPOH cases, compared to 12 months (IQR 60) for cases of POH (P = 0.002, Mann–Whitney test, Fig. 4B). Most cases of RPOH had maintained functional join mobility, while patients with POH complained of a reduction of hip range of motion. Radiological data showed acetabular and femoral head geodes in all cases of RPOH, regardless of disease grade, and a relative absence of osteophytes, while cases of POH displayed the characteristic osteophyte formation, osteosclerosis and almost no geodes. Patients presenting with grades III of RPOH reported a higher level of pain—based on Visual Analog Scale (VAS) assessment—but maintained joint mobility.
Figure 4.
Statistical comparison of the 2 patient groups in terms of disease onset (A), disease aggravation (B), intraoperative blood loss (C), and postoperative blood loss (D) (Mann–Whitney test).
There was a statistically significant difference between the 2 groups in terms of intraoperative blood loss determined by gravimetric methods (P = 0.003, Mann–Whitney test, Fig. 4C), but in terms of postoperative blood loss, the difference was not significant (P = 0.64, Mann–Whitney test, Fig. 4D). There were also no differences in immediate postoperative complications.
Intraoperative findings were similar in all cases of RPOH: the weight bearing surface was flattened in most cases, and articular cartilage was eroded or had completely disappeared from the weight bearing surfaces of the femoral head, with evident destruction of the subchondral bone. There was some eburnation of both the femoral head and acetabulum, with multiple geodes observed in both locations. The geodes were found to be filled with fibrous tissue and needed to be removed with a curette from the acetabulum in order to prepare the bone for endoprosthesis implantation. Synovial tissue was more abundant in RPOH compared to POH cases, and appeared to be more vascularized, and more prone to profuse bleeding.
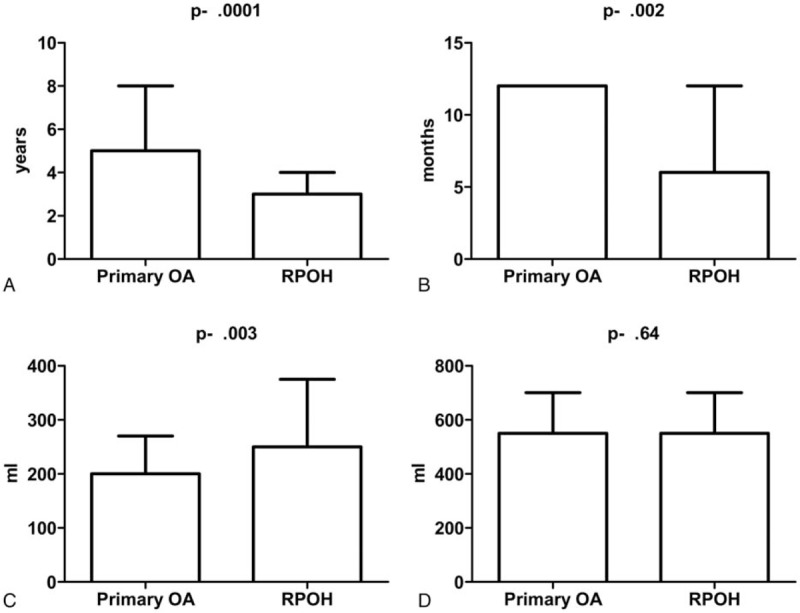
Histologic assessment was only available in 24 cases of RPOH, and showed chronic perivascular inflammation, marked synovial hyperplasia in most cases and severe degenerative changes, including fibrosis, hyalinization, and chondromatosis (Fig. 5). In 7 of the 24 cases there were areas of segmental necrosis of the subchondral bone, but no histological signs of femoral head osteonecrosis were noted. None of the analyzed specimens showed evidence of acute inflammation that could suggest sepsis.
Figure 5.
Histological features of rapidly progressive hip osteoarthritis: synovial cells hyperplasia (A and B) with perivascular monocytic inflammatory infiltrate (B) and large areas of hyalinization (C) and chondromatosis (D).
Both inter- and intraobserver assessments of the newly proposed grading system showed significant agreement (weighted kappa 0.93, and 0.89, respectively, Bland–Altman test, Fig. 6A and B).
Figure 6.
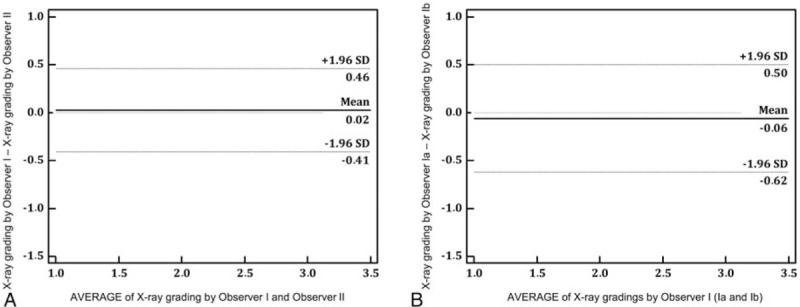
Interobserver (A) and intraobserver (B) assessments of the proposed grading system (weighted kappa 0.93, and 0.89, respectively, Bland–Altman test).
4. Discussion
Although described as early as the 1970, RPOH remains a disease with relatively few mentions in the literature, and it has been considered either as variant, severe form or inflammatory phase of OA, a subset of OA, or an entirely distinct type of hip disease. The confusion surrounding this pathologic entity is also demonstrated by the many names and terms used for describing it, as well as the fact that its etiology is still unclear. Most authors reported individual cases or small case series, with some trying to raise awareness of the profound socio-economic implications of this disease, and make it a better understood and more frequently thought of differential diagnosis in the clinical setting.[10–17] In an effort to subscribe to this process and endeavor, our study aimed to design and propose a series of easily usable clinico-radiological diagnostic criteria and a grading system for practitioners to identify RPOH. These are based on history, clinical aspects, and a single time point radiographic assessment of the hip, without the need for a lengthy observation of the patient, and thus hopefully expediting treatment.
The diagnostic criteria were based on the most frequently reported symptoms and on simple radiologic features that can easily be identified on plain radiographs of either the hip or the pelvis. As opposed to Lequesne's definition that implies observing chondrolysis and joint space narrowing during a period of 12 months, our criteria offer quickly identifiable characteristics (especially the presence of geodes) that can differentiate RPOH from other hip disorders and alert the practitioner about a possible severe bone loss in the disease's evolution. As patient might present at either stage of the disease, determining the grade of RPOH can aid in the proper management of these cases, which usually need a rapid, prioritized intervention.
We consider the presence of geodes in the acetabulum/femoral head a hallmark of RPOH, identifiable in grades I through III—these were also described by Boutry et al[18] on magnetic resonance imaging (MRI) assessments. As the disease progresses, so does the joint space narrowing, which starts of as partial in grade I, and evolves to a complete disappearance of the joint space in grades II and III. The femoral head and acetabulum are deformed in grade II, while partial osteolysis—characteristic of grade III—will lead to the ascension of the femoral head. These findings imply a gradual deterioration of the hip joint, as opposed to the classification system suggested by Pivec et al[19] which differentiates 2 types of RPOH: type I with only joint space narrowing, and type II with severe joint degeneration and acetabular and femoral head destruction. The bilateral cases, with a good sample in Fig. 3—offering a representative example of different grades in a bilateral disease—also supports our idea of gradual hip destruction in RPOH.
The relative absence of osteophytes has also been described by other authors, who consider the disease an atrophic rather than hypertrophic form of OA.[13,19–21] This might also explain the clinical finding of almost normal joint mobility that characterizes these cases.
Most authors reported a rather reduced prevalence of RPOH, but we found it to be 9.5% in a cohort of 863 cases of THR performed by the senior author during a period of 10 years. Also, the majority of studies suggest an average age of onset that is greater compared to POH, as well as a predominance of female patients with unilateral disease.[19] In contrast, although a difference in sex distribution and disease bilaterality was identified in our cases, only the sex distribution differences reached statistical significance, and the mean age was similar in patients with RPOH and POH, with no significant difference (P = 0.19). Interestingly we even found a few cases in patients as young as 35 years, and around 1/3 of the patients were male. Also most bilateral cases (11 of the 15) were found in females, some in their 40s and 50s.
As expected, there was a highly significant difference in both disease onset and disease aggravation between RPOH and POH. However, in spite of the more abundant and better vascularized synovial tissue found in RPOH cases, intra and postoperative blood loss was similar in the 2 groups, and there were no differences in recorded intraoperative and immediately postoperative complications. This is in contrast with the results of Charrois et al[22] who found significantly more blood loss during THR for RPOH compared to POH, but the differences might be based on the use of distinct methods of measurement.
Unfortunately the small number of cases with histological assessment of intraoperative specimens did not allow us to draw conclusions about the histologic characteristics of RPOH. As much as 29.17% of the available histologic evaluations showed areas of necrosis in the subchondral bone, however it is not clear whether these are part of the primary cause of RPOH or simply a consequence of degenerative changes. In all cases the articular cartilage had disappeared, and in most cases the synovial membrane showed inflammation and hyperplasia. The observed severe degenerative changes were similar to those described in the literature.[9,13,15] Specific characteristics of RPOH also identified in our cases were the relative lack of new bone formation (and osteophytes implicitly) and the absence of a demarcation between healthy and necrotic tissue, differentiating the disease from both POH and avascular necrosis of the femoral head.
The main limitation of our study is its retrospective design, which implies possible selection bias. Also, given that there are no clear definitions of the disease, validation of the new criteria and grading system was not possible, due to lack of comparable standards in the literature. Furthermore, the alternative of keeping the patient under observation for a few months in order to determine the grade of chondrolysis/12 months does not seem to be an ethical option, especially in the cases encountered by us on a regular basis, with very few patients presenting with early stages of OA. We consider that the newly described simple diagnostic criteria and grading system may be a necessary further step in familiarizing clinicians with this special pathologic entity, and hopefully prove useful in the proper management of resources and patients in need of THR. The best feature of our diagnostic and grading criteria is their simplicity, making them easily usable in the clinical setting in order to make correct management decisions.
Based on our results we support the concept of RPOH being an entirely distinct form of hip OA. Our study presents distinctive, easily recognizable clinico-radiological characteristics of RPOH and confirmed the inter- and intraobserver reliability of the newly proposed grading system. Because of the ease of use of the diagnostic criteria and grading system, our hope is that more orthopedic surgeons will be helped in correctly identifying the disease and making quick and efficient management choices when faced with patients suffering from RPOH.
Acknowledgments
We would like to thank Lecturer Dr. Septimiu Voidăzan, MD, PhD, from the Department of Epidemiology and Preventive Medicine of the University of Medicine and Pharmacy Tîrgu Mureş, for his help with statistical analysis. This study was funded by an internal research grant from S.C. Biosintex S.R.L., through the University of Medicine and Pharmacy of Tîrgu Mureş (contract no. 8645/2015).
Footnotes
Abbreviations: AP = anteroposterior, IQR = interquartile range, MRI = magnetic resonance imaging, OA = osteoarthritis, POH = primary osteoarthritis of the hip, ROM = range of motion, RPOH = rapidly progressive osteoarthritis of the hip, THR = total hip replacement, VAS = Visual Analog Scale.
Funding: This study was funded by an internal research grant from S.C. Biosintex S.R.L., through the University of Medicine and Pharmacy of Tîrgu Mureş (contract no. 8645/2015).
Role of the funding source: The study sponsors had no involvement in the study design, collection, analysis and interpretation of data, or in the writing of the manuscript and decision to submit the manuscript for publication.
Ethics approval of research on humans or animals: The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. As the study had a retrospective design, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
The authors have no conflicts of interest to disclose.
References
- [1].Postel M, Kerboull M. Total prosthetic replacement in rapidly destructive arthrosis of the hip joint. Clin Orthop Relat Res 1970;72:138–44. [PubMed] [Google Scholar]
- [2].Lequesne M. [Rapid destructive coxarthritis]. Rhumatologie 1970;22:51–63. [PubMed] [Google Scholar]
- [3].Kellgren JH. Osteoarthrosis in patients and populations. Br Med J 1961;2:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bock GW, Garcia A, Weisman MH, et al. Rapidly destructive hip disease: clinical and imaging abnormalities. Radiology 1993;186:461–6. [DOI] [PubMed] [Google Scholar]
- [5].Komiya S, Inoue A, Sasaguri Y, et al. Rapidly destructive arthropathy of the hip. Studies on bone resorptive factors in joint fluid with a theory of pathogenesis. Clin Orthop Relat Res 1992;273–82. [PubMed] [Google Scholar]
- [6].Tamai M, Sagawa K, Kawabata R, et al. Production of IL-6 by T cells from the femoral head of patients with rapidly destructive coxopathy (RDC). Clin Exp Immunol 1996;103:506–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Yamamoto T, Bullough PG. The role of subchondral insufficiency fracture in rapid destruction of the hip joint: a preliminary report. Arthritis Rheum 2000;43:2423–7. [DOI] [PubMed] [Google Scholar]
- [8].Berger CE, Kroner A, Stiegler H, et al. Elevated levels of serum type I collagen C-telopeptide in patients with rapidly destructive osteoarthritis of the hip. Int Orthop 2005;29:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Rosenberg ZS, Shankman S, Steiner GC, et al. Rapid destructive osteoarthritis: clinical, radiographic, and pathologic features. Radiology 1992;182:213–6. [DOI] [PubMed] [Google Scholar]
- [10].Nguyen C, Rannou F, Revel M. Total loss of femoral head and acetabulum in rapidly destructive hip disease. J Rheumatol 2008;35:2445–6. [DOI] [PubMed] [Google Scholar]
- [11].Trevisan C, Sportelli G, Guerrasio S, et al. Rapidly destructive bilateral hip disease: a case report and review of the literature. J Orthop Traumatol 2002;2:165–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Flik K, Vargas JH., III Rapidly destructive hip disease: a case report and review of the literature. Am J Orthop (Belle Mead NJ) 2000;29:549–52. [PubMed] [Google Scholar]
- [13].Batra S, Batra M, McMurtrie A, et al. Rapidly destructive osteoarthritis of the hip joint: a case series. J Orthop Surg Res 2008;3:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Fukui K, Kaneuji A, Fukushima M, et al. Early MRI and intraoperative findings in rapidly destructive osteoarthritis of the hip: a case report. Int J Surg Case Rep 2015;8C:13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Shu J, Ross I, Wehrli B, et al. Rapidly destructive inflammatory arthritis of the hip. Case Rep Rheumatol 2014;2014:160252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Marley WD, Ruiz A. Rapidly progressive osteoarthritis presenting as acute limb shortening. BMJ Case Rep 2013;2013:bcr2013009086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kuo A, Ezzet KA, Patil S, et al. Total hip arthroplasty in rapidly destructive osteoarthritis of the hip: a case series. HSS J 2009;5:117–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Boutry N, Paul C, Leroy X, et al. Rapidly destructive osteoarthritis of the hip: MR imaging findings. AJR Am J Roentgenol 2002;179:657–63. [DOI] [PubMed] [Google Scholar]
- [19].Pivec R, Johnson AJ, Harwin SF, et al. Differentiation, diagnosis, and treatment of osteoarthritis, osteonecrosis, and rapidly progressive osteoarthritis. Orthopedics 2013;36:118–25. [DOI] [PubMed] [Google Scholar]
- [20].Altman RD, Bloch DA, Dougados M, et al. Measurement of structural progression in osteoarthritis of the hip: the Barcelona consensus group. Osteoarthritis Cartilage 2004;12:515–24. [DOI] [PubMed] [Google Scholar]
- [21].Conrozier T, Ferrand F, Poole AR, et al. Differences in biomarkers of type II collagen in atrophic and hypertrophic osteoarthritis of the hip: implications for the differing pathobiologies. Osteoarthritis Cartilage 2007;15:462–7. [DOI] [PubMed] [Google Scholar]
- [22].Charrois O, Kahwaji A, Vastel L, et al. Blood loss in total hip arthroplasty for rapidly destructive coxarthrosis. Int Orthop 2001;25:22–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


