Abstract
Purpose:
We aim to perform a meta-analysis on prevalence of all kinds of operation-related complications following surgery treating cervical compressive myelopathy (CCM) and to provide reference for surgeons making surgical plan.
Methods:
An extensive search of literature was performed in PubMed/MEDLINE, Embase, the Cochrane library, CNKI, and WANFANG databases on incidence of operation-related complications from January 2007 to November 2016. Data was calculated and data analysis was conducted with STATA 12.0 and Revman 5.3.
Results:
A total of 107 studies included 1705 of 8612 patients (20.1%, 95% CI 17.3%–22.8%) on overall complications. The incidence of C5 plasy, cerebrospinal fluid (CSF), infection, axial pain, dysphagia, hoarseness, fusion failure, graft subsidence, graft dislodgment, and epidural hematoma is 5.3% (95% CI 4.3%–6.2%), 1.9% (95% CI 1.3%–2.4%), 2.8% (95% CI 1.7%–4.0%), 15.6% (95% CI 11.7%–19.5%), 16.8% (95% CI 13.6%–19.9%), 4.0% (95% CI 2.3%–5.7%), 2.6% (95% CI 0.2%–4.9%), 3.7% (95% CI 2.0%–5.5%), 3.4% (95% CI 2.0%–4.8%), 1.1% (95% CI 0.7%–1.5%), respectively. Patients with ossification of posterior longitudinal ligament (OPLL) (6.3%) had a higher prevalence of C5 plasy than those with cervical spondylotic myelopathy (CSM) (4.1%), and a similar trend in CSF (12.2% vs 0.9%). Individuals after laminectomy and fusion (LF) had highest rate of C5 plasy (15.2%), while those who underwent anterior cervical discectomy and fusion (ACDF) had the lowest prevalence (2.0%). Compared with patients after other surgical options, individuals after anterior cervical corpectomy and fusion (ACCF) have the highest rate of CSF (4.2%), infection (14.2%), and epidural hematoma (3.1%). Patients after ACDF (4.8%) had a higher prevalence of hoarseness than those with ACCF (3.0%), and a similar trend for dysphagia between anterior corpectomy combined with discectomy (ACCDF) and ACCF (16.8% vs 9.9%).
Conclusions:
Based on our meta-analysis, patients with OPLL have a higher incidence of C5 palsy and CSF. Patients after LF have a higher incidence of C5 palsy, ACCDF have a higher incidence of dysphagia, ACCF have a higher incidence of CSF and infection and ACDF have a higher incidence of hoarseness. These figures may be useful in the estimation of the probability of complications following cervical surgery.
Keywords: cervical, complications, incidence, meta-analysis
1. Introduction
Cervical compressive myelopathy (CCM), caused by cervical spondylotic myelopathy (CSM) or ossification of posterior longitudinal ligament (OPLL), is a common cervical degenerative disease with increasing elder population, seriously impacting quality of life and even leading to disability.[1–3] The aim of surgery is to decompress spinal cord and preserve the stability of the spinal column.[3–7] However, the selection of optimal surgical treatment for CCM remains controversial.[4,5,8–11] Surgeries, widely used in clinic mainly involved anterior and posterior approaches, including anterior cervical discectomy and fusion (ACDF), anterior cervical corpectomy and fusion (ACCF), anterior corpectomy combined with discectomy (ACCDF), laminoplasty (LP), and laminectomy with fusion (LF).[10–16] Each approach has its own advantages and disadvantages. Anterior approaches are propitious to solve pathogenic structures from anterior, but it has a high risk of complications, like dysphagia, hoarseness, or artery injury, as reported by previous studies.[3–5,7,9] Posterior approaches could adequately decompress spinal cord, but it was reported that posterior approaches were more likely to cause C5 plasy and cervical kyphosis.
Even though, many studies reported on surgical selection for CCM. But there is no meta-analysis on prevalence of complications following cervical surgery treating for CCM. The purpose of our study is to explore incidence of operation-related complications after cervical surgery and we hope that it is helpful in the estimation of the probability of complications following cervical surgery.
2. Materials and methods
2.1. Ethics statement
There is no need to seek informed consent from patients, since this is a meta-analysis based on the published data, without any potential harm to the patients; this is approved by Ethics Committee of The Third Hospital of HeBei Medical University.
2.2. Search strategy
An extensive search of literature was performed in PubMed/MEDLINE, Embase, the Cochrane library, CNKI, and WANFANG databases. The following key words were used for search: “complications,” “cervical,” “C5 plasy,” “CSF,” “infection,” “axial pain,” “dysphagia,” “hoarseness,” “fusion failure,” “graft subsidence,” “graft dislodgment,” “epidural hematoma,” “anterior cervical discectomy and fusion,” “anterior cervical corpectomy and fusion,” “corpectomy combined with discectomy,” “laminoplasty,” “laminectomy and fusion,” “cervical spondylotic myelopathy,” and “ossification of posterior longitudinal ligament” from January 2007 to November 2016, with various combinations of the operators “AND” and “OR.” Language was restricted to Chinese and English.
2.3. Inclusion criteria
Studies were included if they met the following criteria: randomized or nonrandomized controlled study; age greater than or equal to 18 years old; studies on complications after cervical surgery.
2.4. Exclusion criteria
Studies were excluded if they met the following criteria: had repeated data; did not report outcomes of interest; in vitro human cadaveric biomechanical studies; earlier trial, reviews, and case-reports; sample size >1000 or <30; CCM caused by trauma or tumour; have a history of cervical surgery.
2.5. Selection of studies
Two reviewers independently reviewed all subjects, abstracts, and the full text of articles. Then the eligible trials were selected according to the inclusion criteria. When consensus could not be reached, a third reviewer was consulted to resolve the disagreement.
2.6. Data extraction and management
Two reviewers extracted data independently. The data extracted including the following categories: study ID, study design, study location, number of total patients and patients with complications, diagnose, complications category, incidence of complications after anterior or posterior approaches including ACDF, ACCF, ACCDF, LP, and LF.
2.7. Statistical analysis
Data analysis was performed with STATA 12.0 (Stata Corporation, College Station, TX). Both were reported with 95% confidence intervals (CI), and a P value of 0.05 was used as the level of statistical significance. Assessment for statistical heterogeneity was calculated using the I2 tests, which described the proportion of the total variation in meta-analysis assessments from 0% to 100%. The random effects model was used for the analysis when an obvious heterogeneity was observed among the included studies (I2 >50%). The fixed-effects model was used when there was no significant heterogeneity between the included studies (I2 ≤50%).[17,18] Flow diagram was performed with Revman 5.3
2.8. Test for risk of publication bias
We performed a visual inspection of the funnel plot for publication bias. The funnel plot should be asymmetric when there is publication bias and symmetric in the case of no publication bias. We performed Egger and Begg tests to measure the funnel plot asymmetry by using a significance level of P<0.05. The trim and fill computation was used to estimate the effect of publication bias.
3. RESULTS
3.1. Search results
We had searched 631 English studies in MEDLINE, EMBASE, 93 Chinese studies in WANFANG and CNKI. Of these, 103 English articles and 30 Chinese articles after duplicates removed, 368 English articles and 36 Chinese articles were excluded due to unrelated studies. Seventy-three English articles and 7 Chinese articles were excluded due to eligibility criteria. As a result, a total of 107 studies were identified for this meta-analysis. The literature search procedure is shown in Fig. 1.
Figure 1.
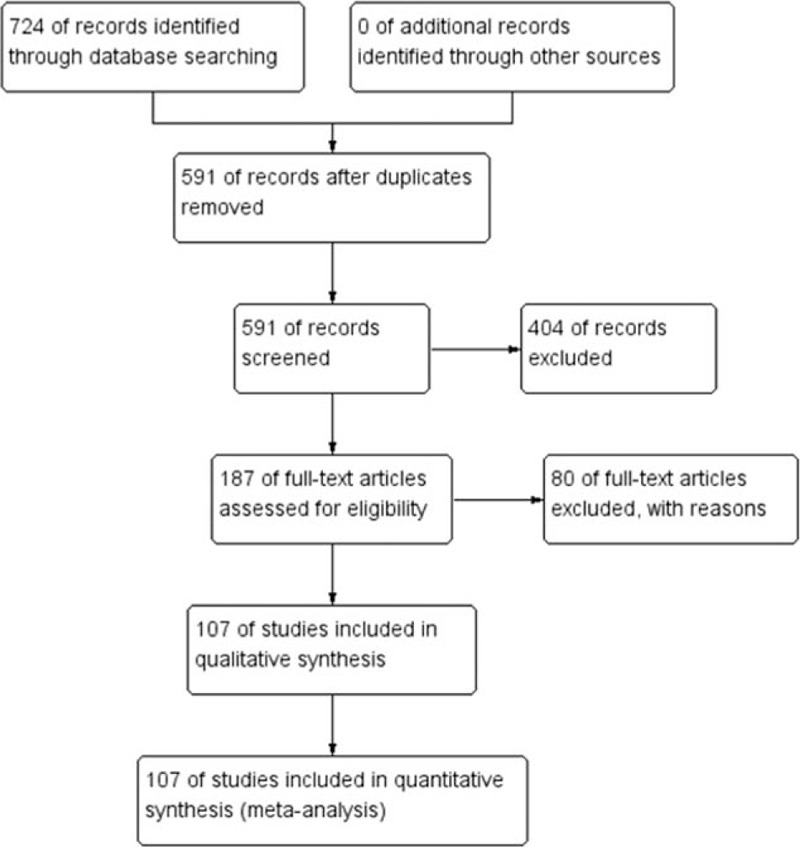
Flow diagram of study selection.
3.2. Baseline characteristics and quality assessment
A total of 8612 patients from 75 studies on total complications, 6349 patients from 57 studies on C5 plasy, 5007 patients from 36 studies on CSF, 591 patients from 6 studies on graft subsidence, 1102 patients from 10 studies on graft dislodgment, 2234 patients from 19 studies on hoarseness, 3489 patients from 25 studies on infection, 5841 patients from 38 studies on dysphagia, 689 patients from 5 studies on fusion failure, 2185 patients from 14 studies on epidural hematoma, 2650 patients from 23 studies on axial pain were included in our study. Table 1 shows the baseline characteristics of included articles.
Table 1.
Characteristics of included studies.
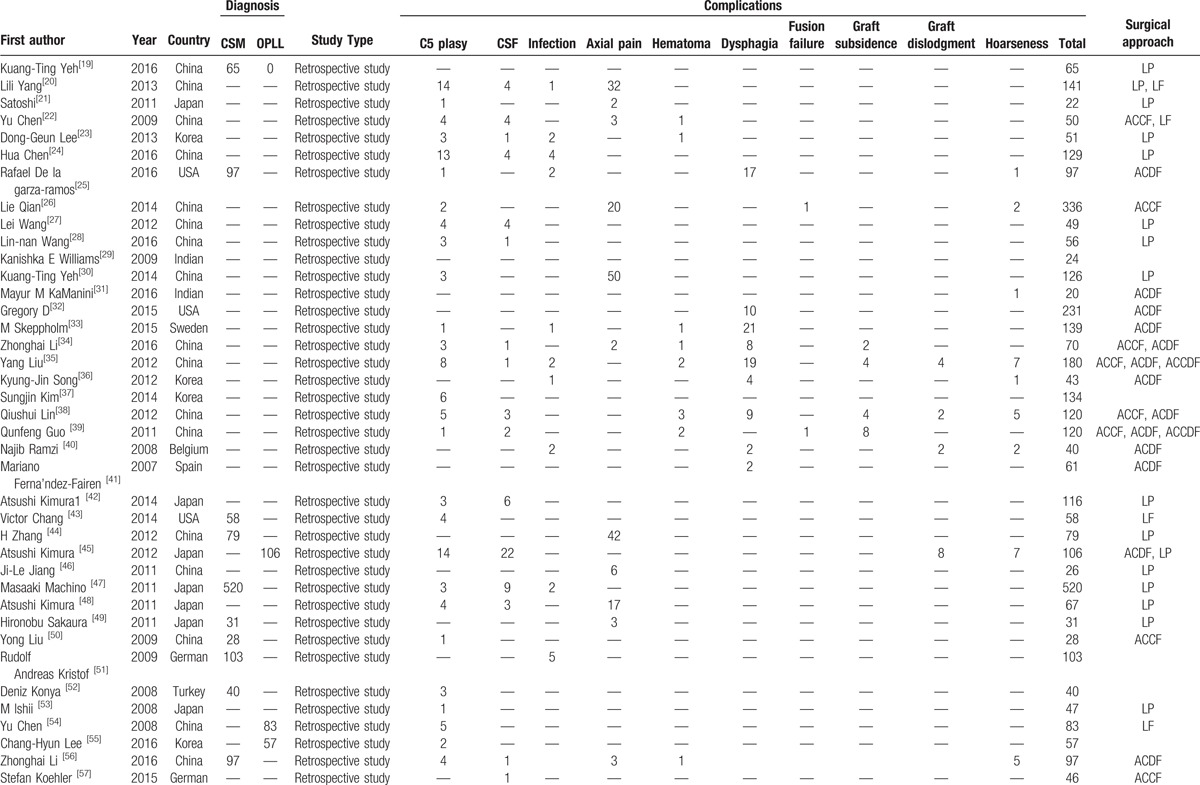
Table 1 (Continued).
Characteristics of included studies.
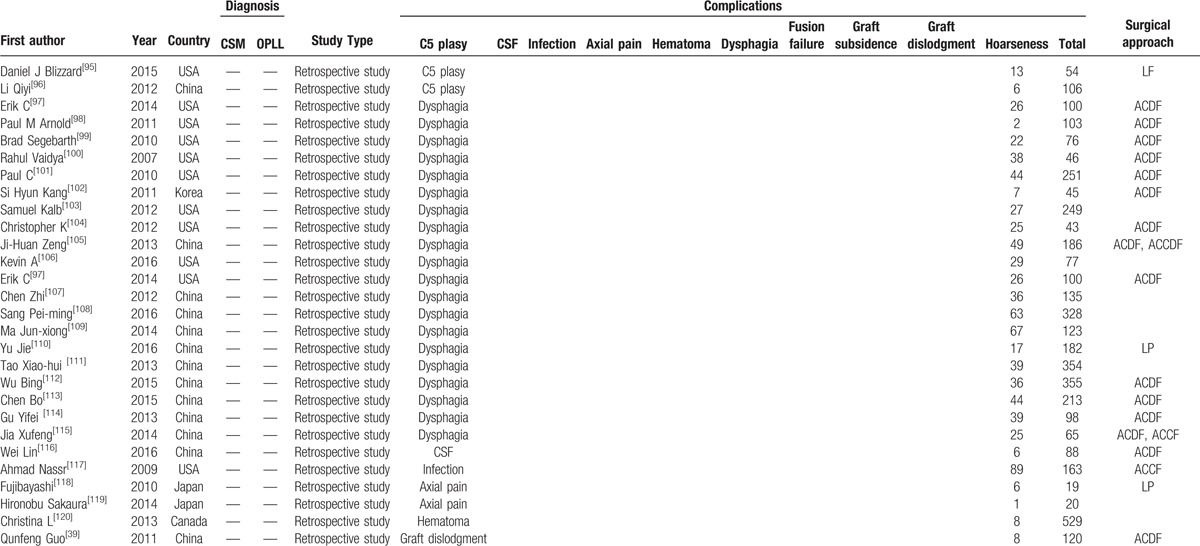
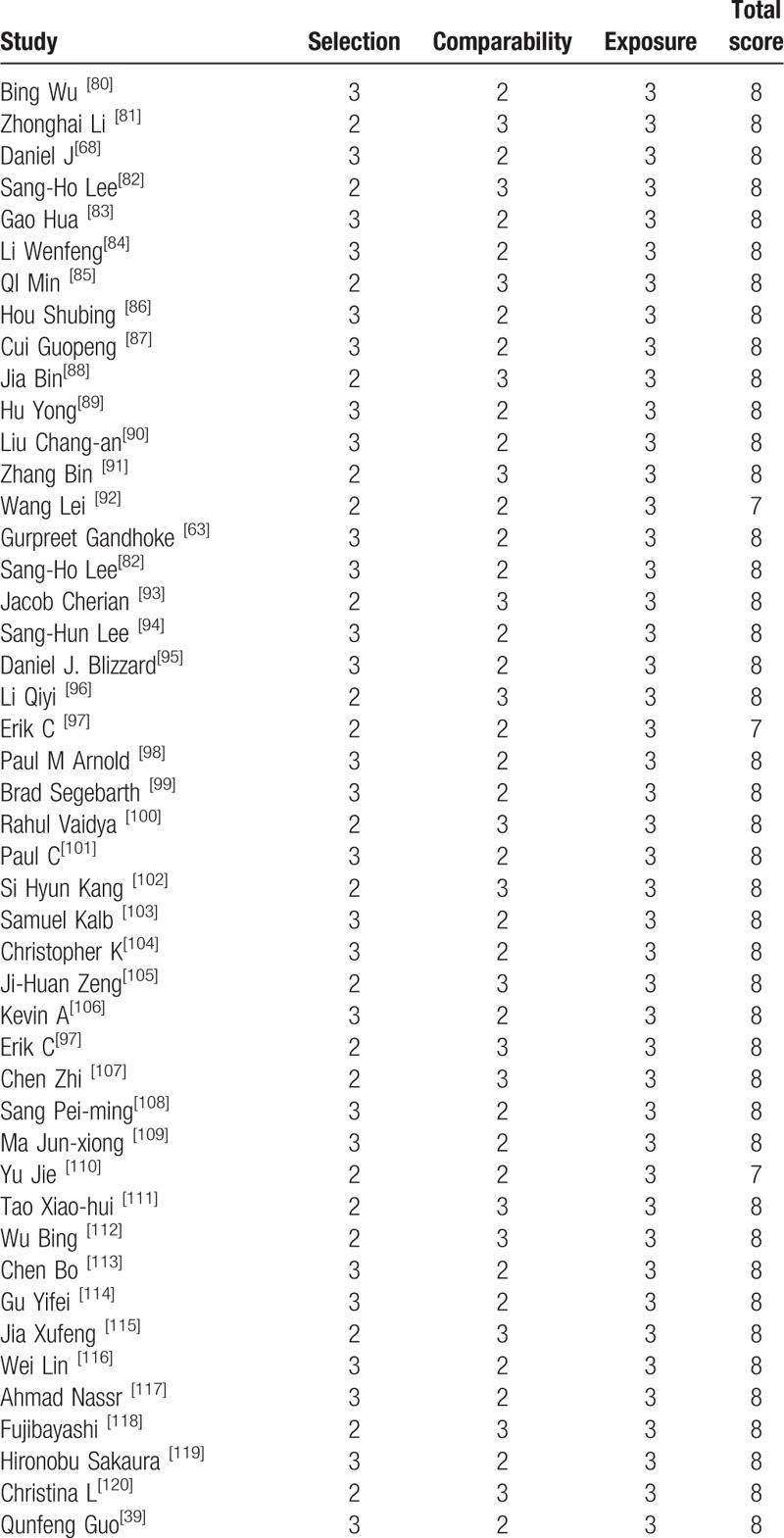
All included studies were retrospective studies, Newcastle Ottawa Quality Assessment Scale (NOQAS) was applied to estimate the quality of each study. We used NOQAS, the maximum of 9 points, to assess quality of selection for nonrandomized case controlled studies and cohort studies in terms of comparability, exposure, and outcomes. Among these studies, 95 studies scored 8 points and 3 studies scored 12 points. Therefore, each study has relatively high quality (Table 2 ).
Table 1 (Continued).
Characteristics of included studies.
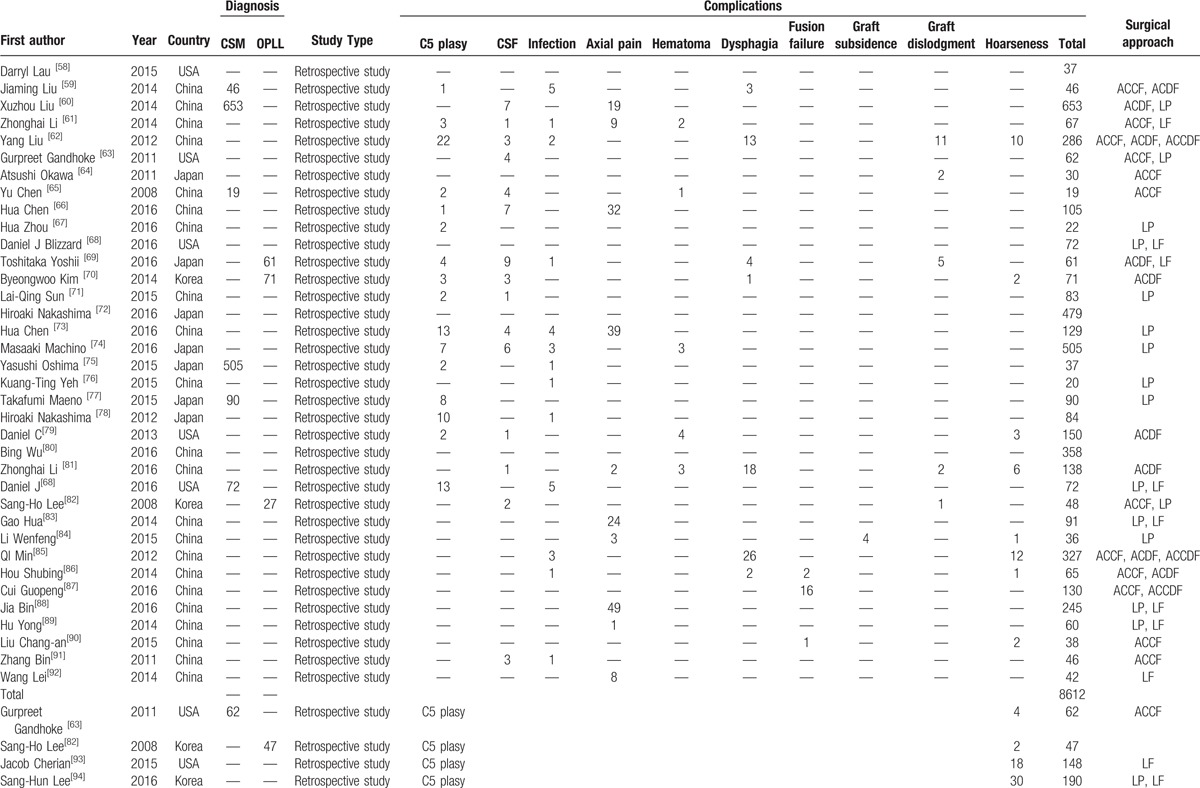
Table 2.
The quality assessment according to the Newcastle Ottawa Quality Assessment Scale (NOQAS) of each study.
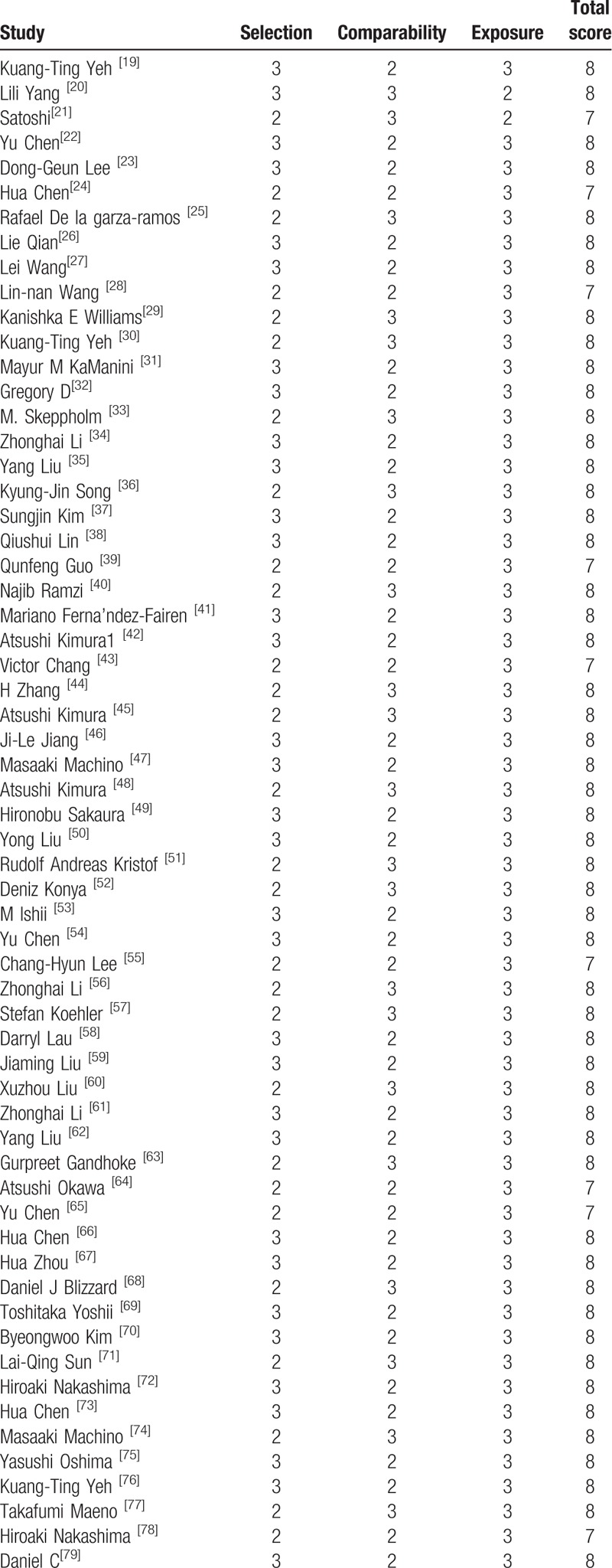
Table 2 (Continued).
The quality assessment according to the Newcastle Ottawa Quality Assessment Scale (NOQAS) of each study.
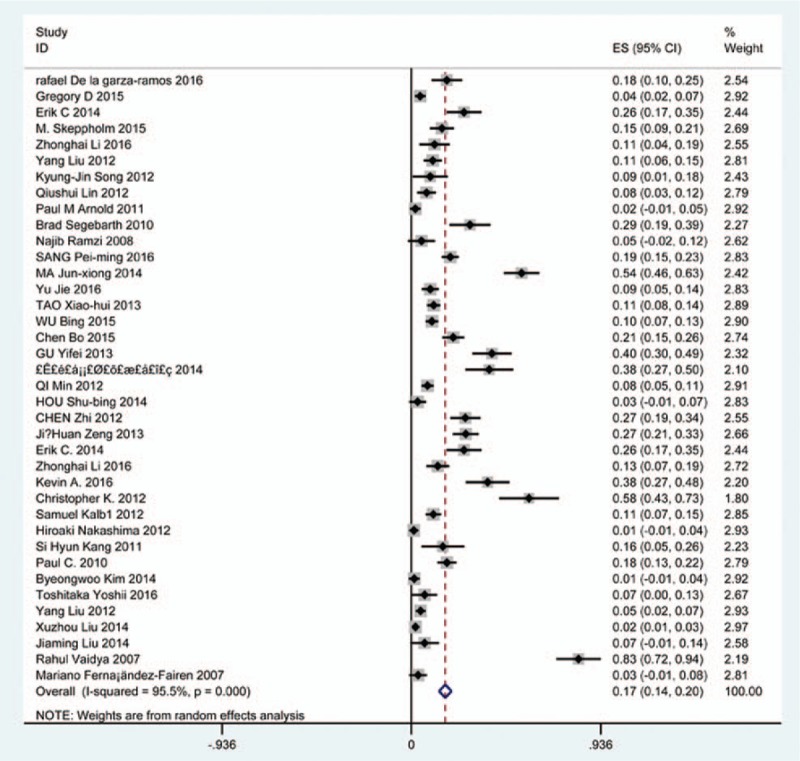
3.3. Prevalence of overall complications
Seventy-five studies[19–92] containing 1705 patients with overall complications of 8612 patients after cervical surgery were included. Figure 2 shows that the incidence was 20.1% (95% CI 17.3%–22.8%), with substantial heterogeneity of incidence observed. The incidence varied between 2.6% and 58.1%.
Figure 2.
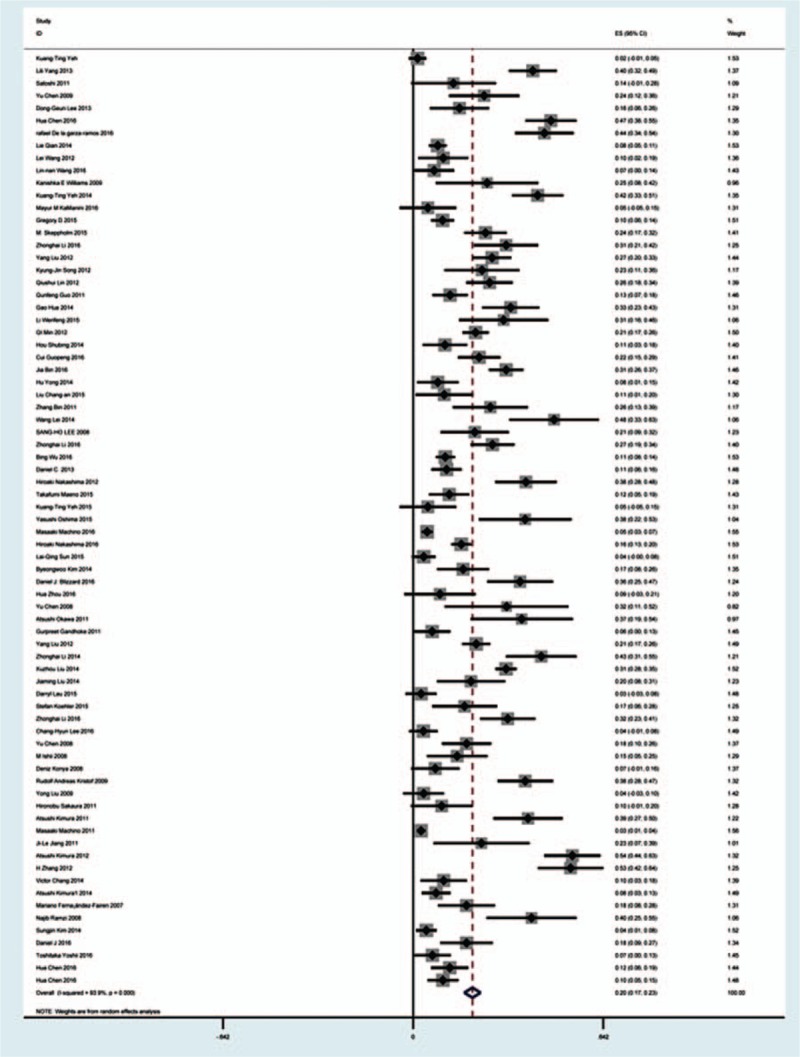
Forest plot showing incidence of overall complications after cervical surgery. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
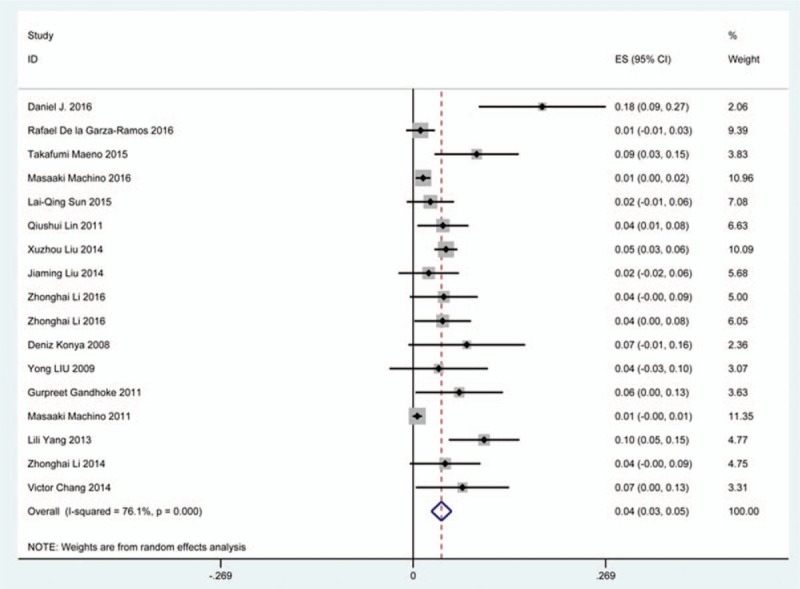
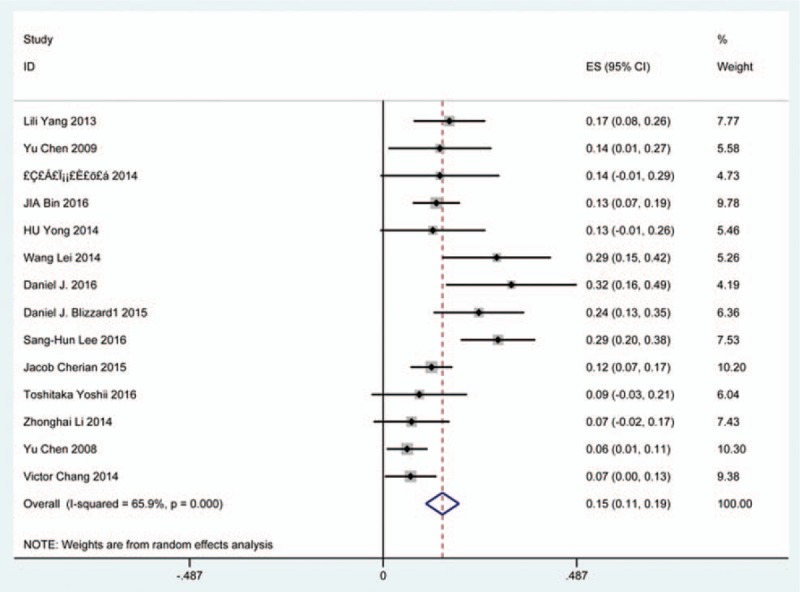
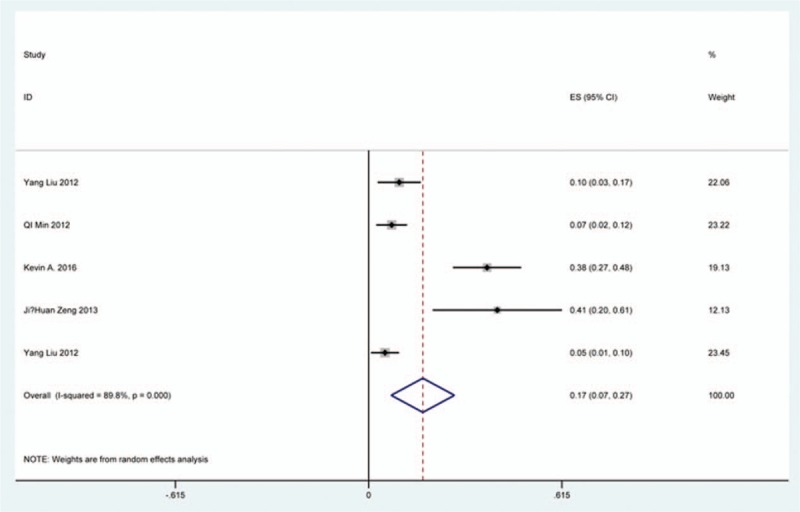
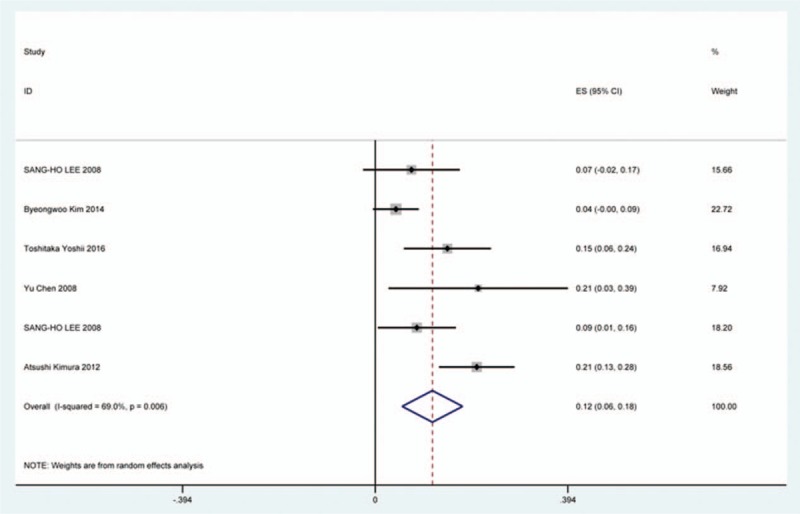
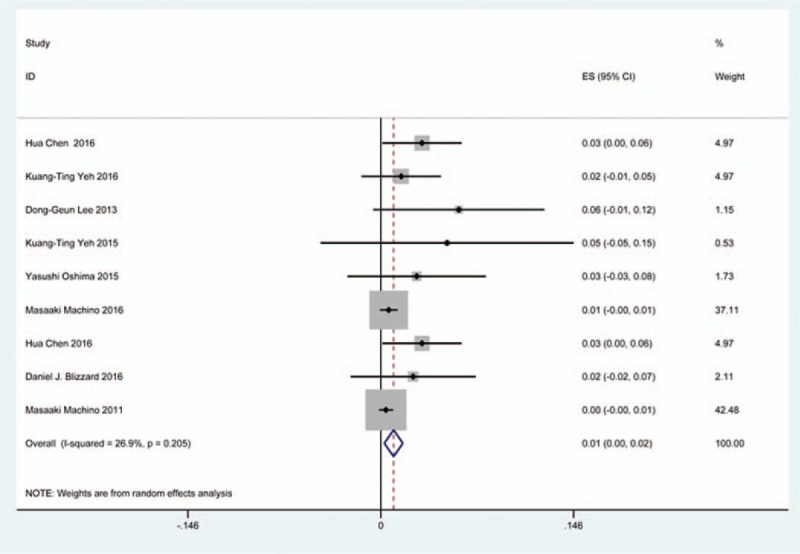
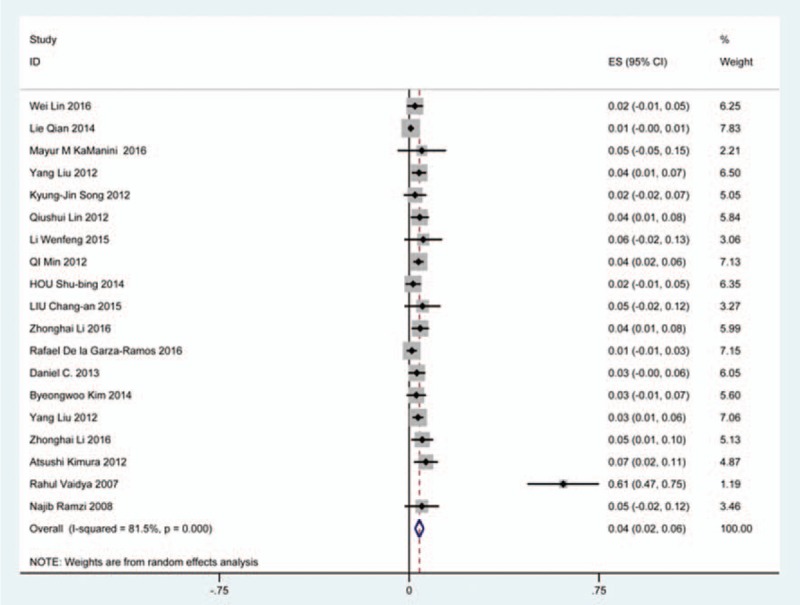
3.4. C5 plasy
Fifty-seven studies[20–28,30,33–35,37–39,42–43,45,47–48,50,52–56,59,61–71,73–75,77–79,82–85,88,89,91–96] containing 355 patients with C5 plasy of 6349 patients after cervical surgery were included. Figure 3 shows that the incidence was 5.3% (95% CI 4.3%–6.2%), with substantial heterogeneity of incidence observed. The incidence varied between 0.6% and 28.6%. Compared with patients with CSM (4.1%, 95% CI 2.9%–5.2%), patients with OPLL (6.3%, 95% CI 2.4%–5.2%) has a higher incidence (Figs. 4, 5). In terms of surgical methods, patients who underwent LP had the highest rate (15.2%, 95% CI 10.9%–19.1%), while those who received ACDF had the lowest rate (2.0%, 95% CI 0.8%–2.4%) (Fig 6, Fig 7, Fig 8, Fig 9, Fig 10).
Figure 3.
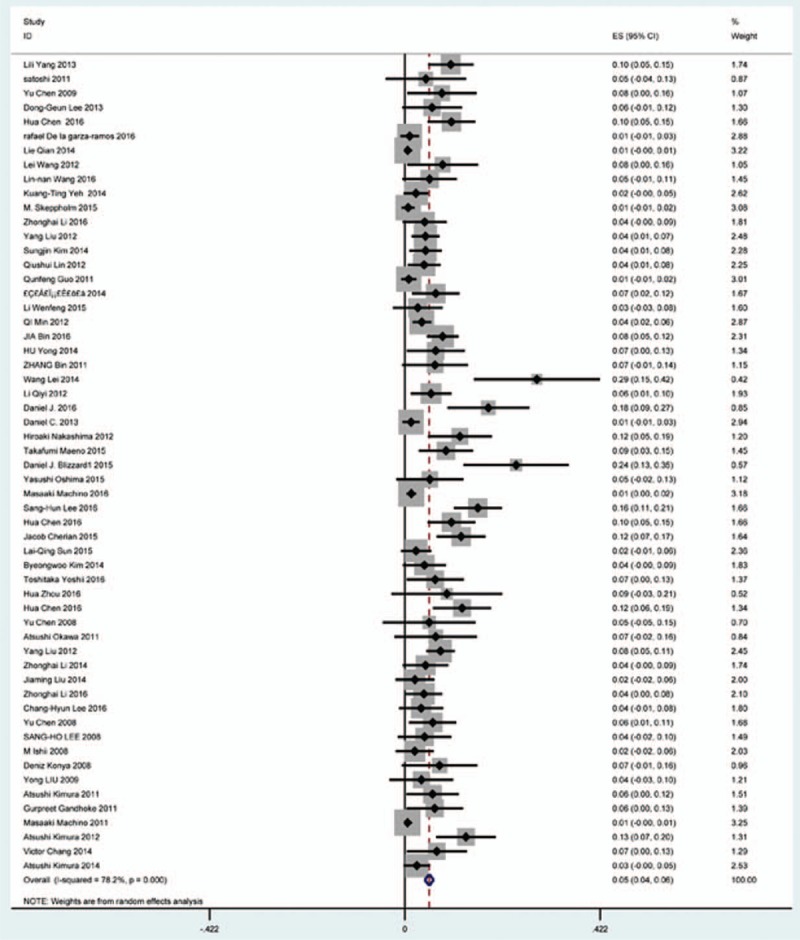
Forest plot showing incidence of C5. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 4.
Forest plot showing incidence of C5 for patients with CSM. CI = confidence interval, CSM = cervical spondylotic myelopathy, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 6.
Forest plot showing incidence of C5 after ACCF. ACCF = anterior cervical corpectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 7.
Forest plot showing incidence of C5 after ACDF. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 8.
Forest plot showing incidence of C5 after ACCDF. ACCDF = anterior corpectomy combined with discectomy, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 9.
Forest plot showing incidence of C5 after LP. CI = confidence interval, df = degrees of freedom, LP = laminoplasty, M–H = Mantel–Haenszel.
Figure 10.
Forest plot showing incidence of C5 after LF. CI = confidence interval, df = degrees of freedom, LF = laminectomy and fusion, M–H = Mantel–Haenszel.
Figure 5.
Forest plot showing incidence of C5 for patients with OPLL. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel, OPLL = ossification of posterior longitudinal ligamen.
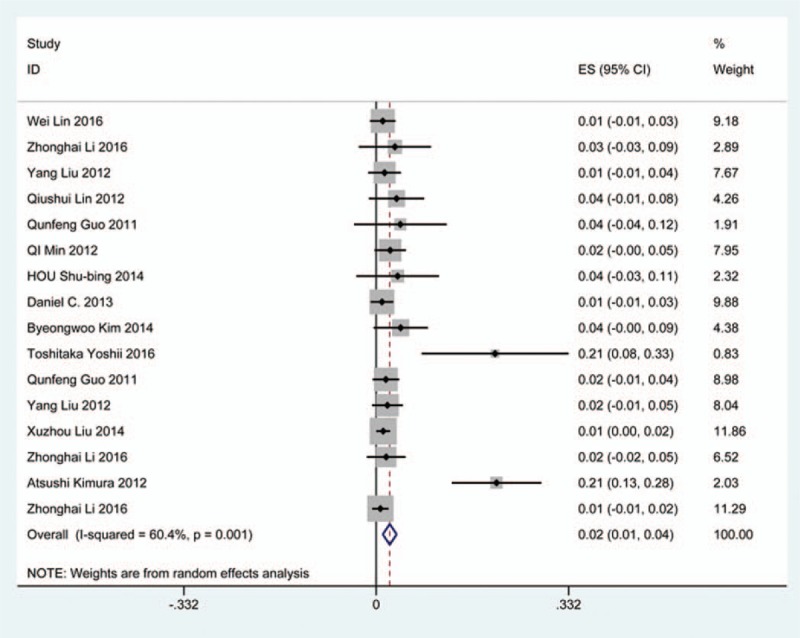
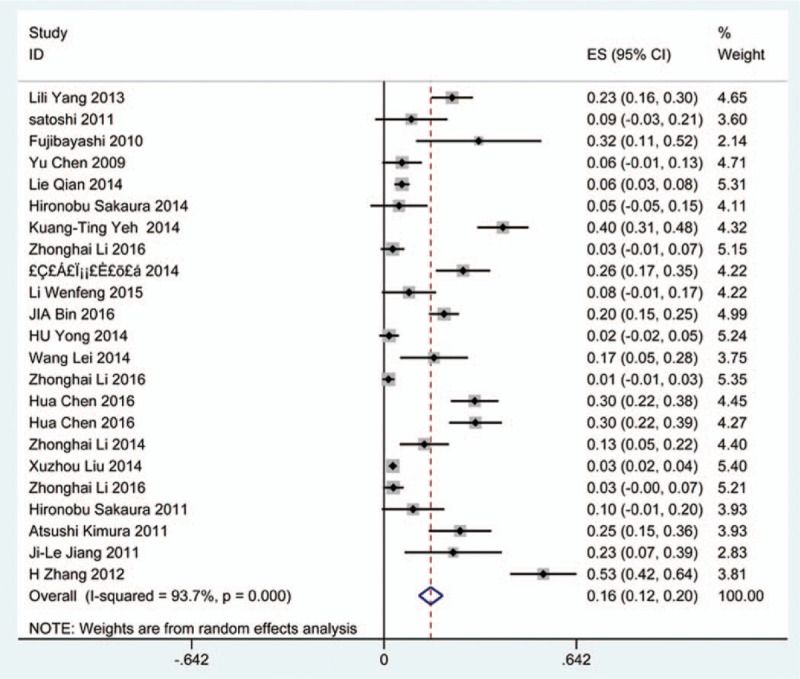
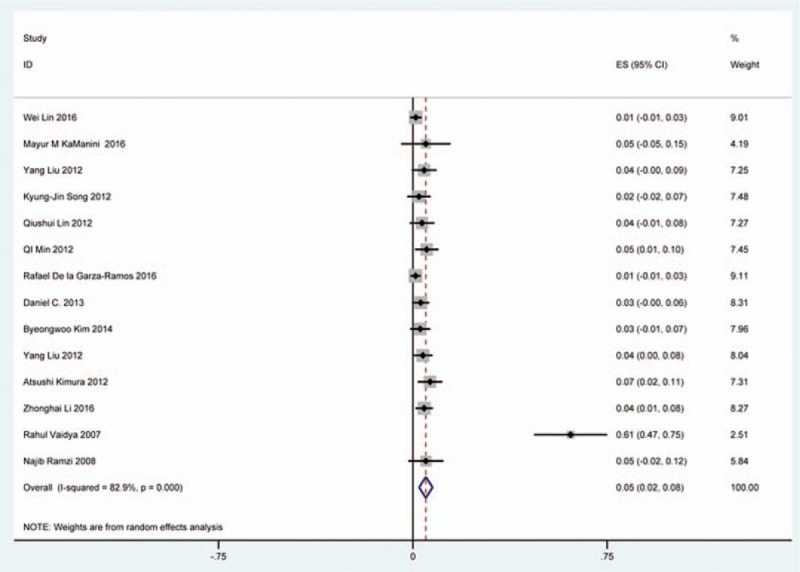
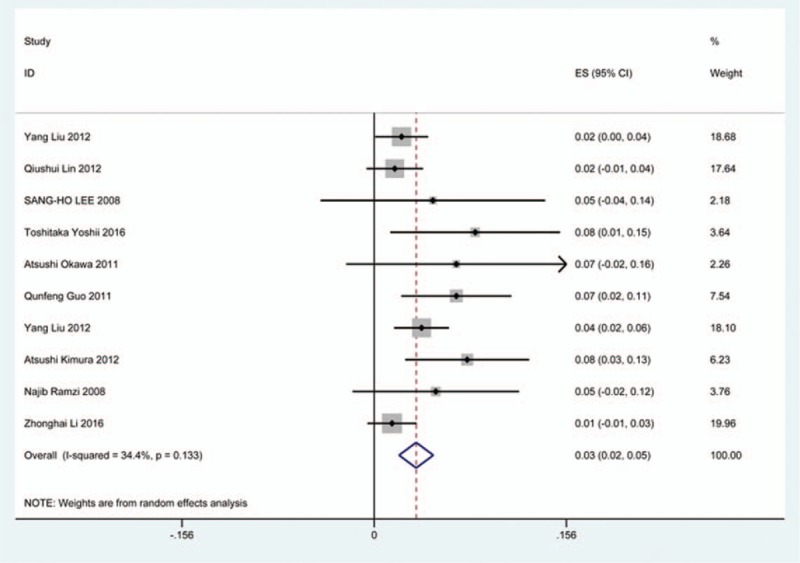
3.5. Dysphagia
Thirty-eight studies[25,32–36,38,40–41,59–60,62,69–70,78,81,85,86,97–115] containing 835 patients with dysphagia of 5841 patients after cervical surgery were included. Figure 11 shows that the incidence was 16.8% (95% CI 13.6%–19.9%), with substantial heterogeneity of incidence observed. The incidence varied between 1.4% and 58.1%. Incidence for patients who underwent ACCDF and ACDF was 16.8% (95% CI 6.9%–27.2%) and 16.2% (95% CI 11.7%–19.8%), which is higher than those who received ACCF 9.9% (95% CI 4.8%–15.9%) (Fig 12, Fig 13, Fig 14).
Figure 11.
Forest plot showing incidence of dysphagia. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 12.
Forest plot showing incidence of dysphagia after ACCDF. ACCDF = anterior corpectomy combined with discectomy, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 13.
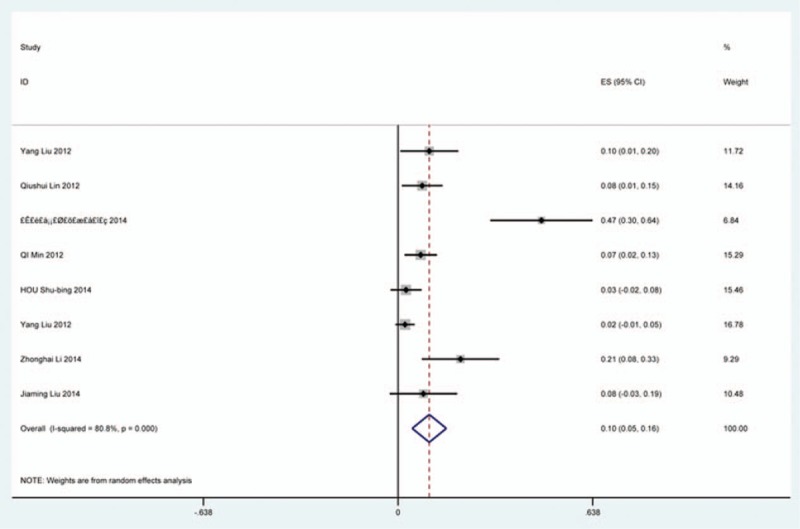
Forest plot showing incidence of dysphagia after ACCF. ACCF = anterior cervical corpectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 14.
Forest plot showing incidence of dysphagia after ACDF. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
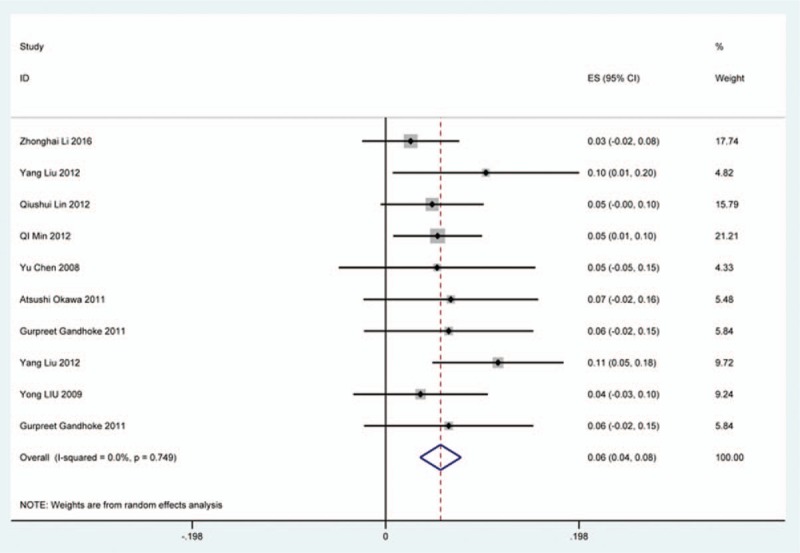
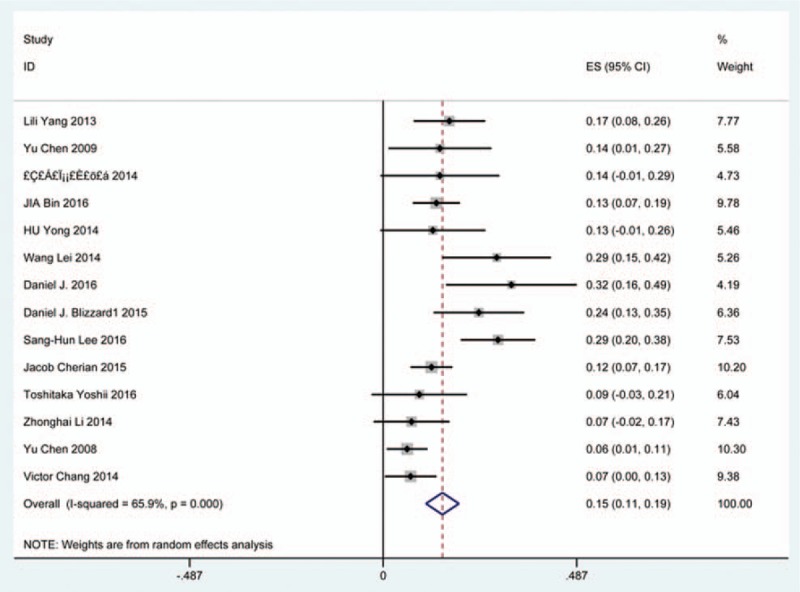
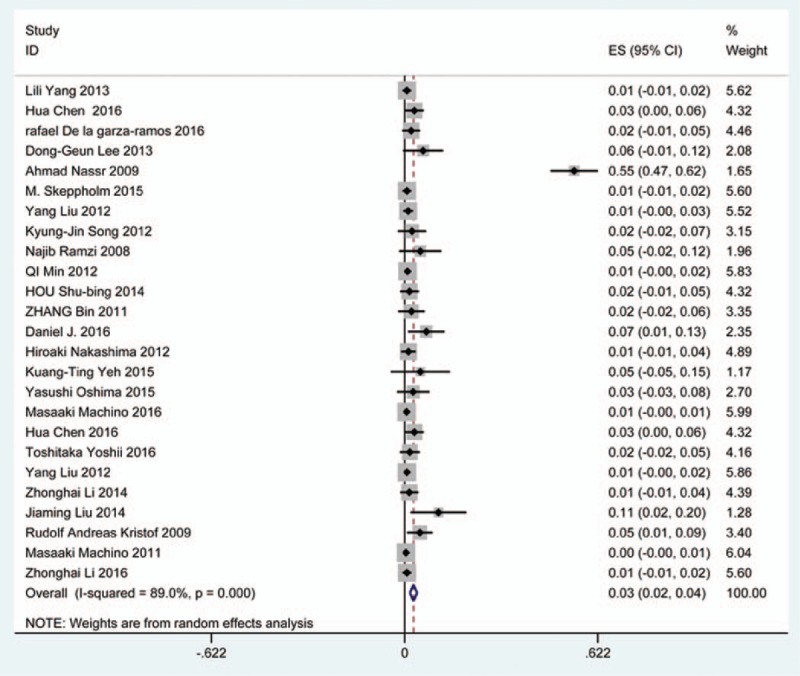
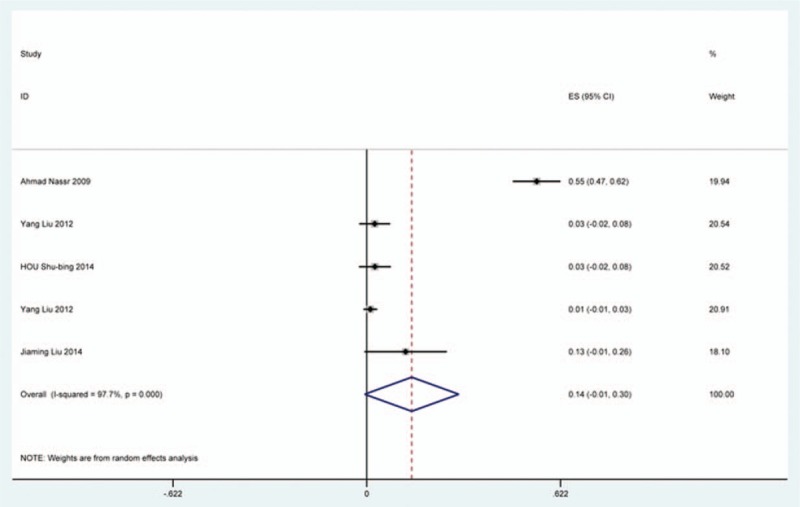
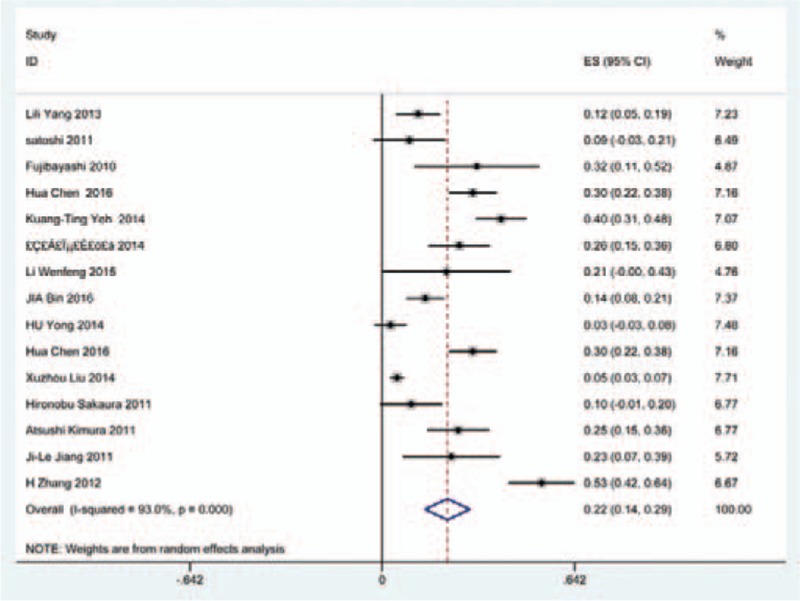
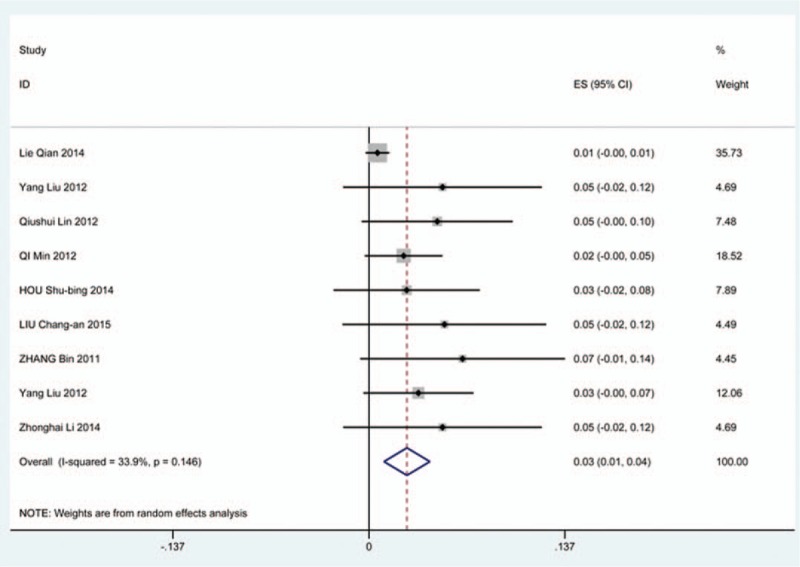
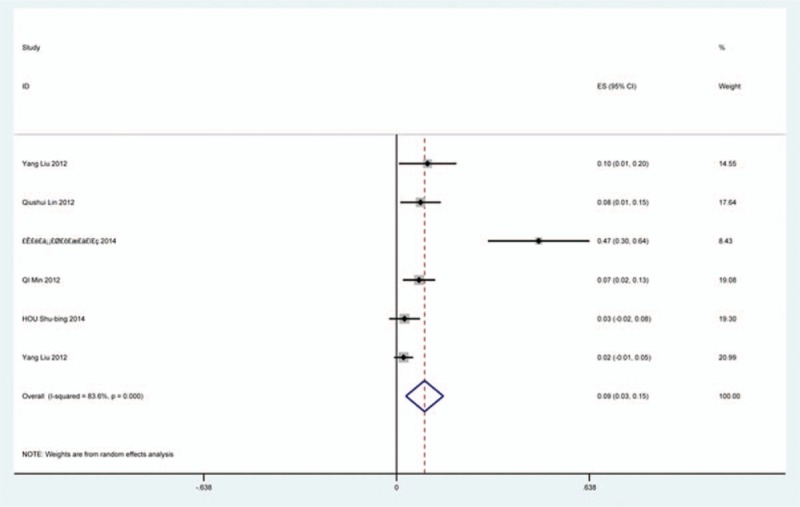
3.6. Cerebrospinal fluid
Thirty-six studies[20,22–24,27,28,34,35,38,39,42,45,47,48,56,57,60–62,65,66,69–71,73,74,79,81,82,84–86,88,90,91,116] containing 129 patients with CSF of 5007 patients after cervical surgery were included. Figure 15 shows that the incidence was 1.9% (95% CI 1.3%–2.4%), with substantial heterogeneity of incidence observed. The incidence varied between 0.4% and 21.1%. Compared with patients with CSM (0.9%, 95% CI 0.6%–1.7%), patients with OPLL (12.2%, 95% CI 6.2%–17.8%) have a higher incidence (Figs. 16, 17). As for surgical methods, patients who underwent ACCF had the highest rate (4.2%, 95% CI 0.3%–8.2%), while those who received ACDF had the lowest rate (1.9%, 95% CI 0.9%–4.0%) (Figs. 18–20 Fig 18, Fig 19, Fig 20).
Figure 15.
Forest plot showing incidence of CSF. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 16.
Forest plot showing incidence of CSF for patients with OPLL. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel, OPLL = ossification of posterior longitudinal ligamen.
Figure 18.
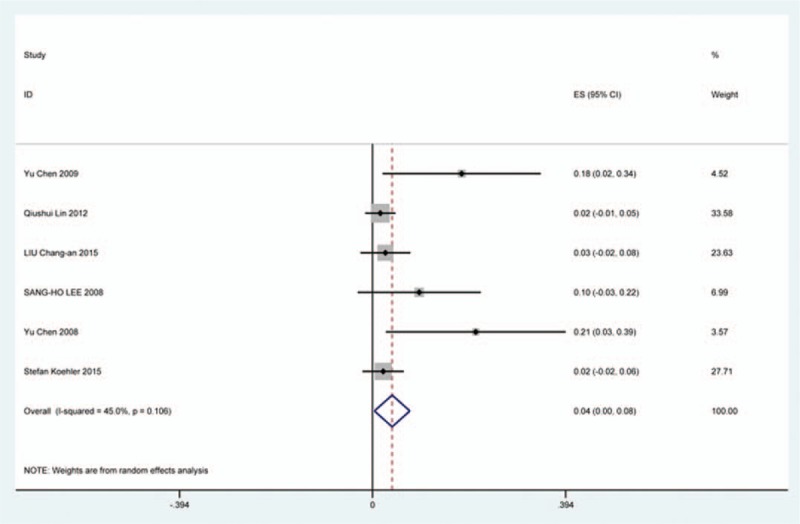
Forest plot showing incidence of CSF after ACCF. ACCF = anterior cervical corpectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 20.
Forest plot showing incidence of CSF after LP. CI = confidence interval, df = degrees of freedom, LP = laminoplasty, M–H = Mantel–Haenszel.
Figure 17.
Forest plot showing incidence of CSF for patients with CSM. CI = confidence interval, CSM = cervical spondylotic myelopathy, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 19.
Forest plot showing incidence of CSF after ACDF. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
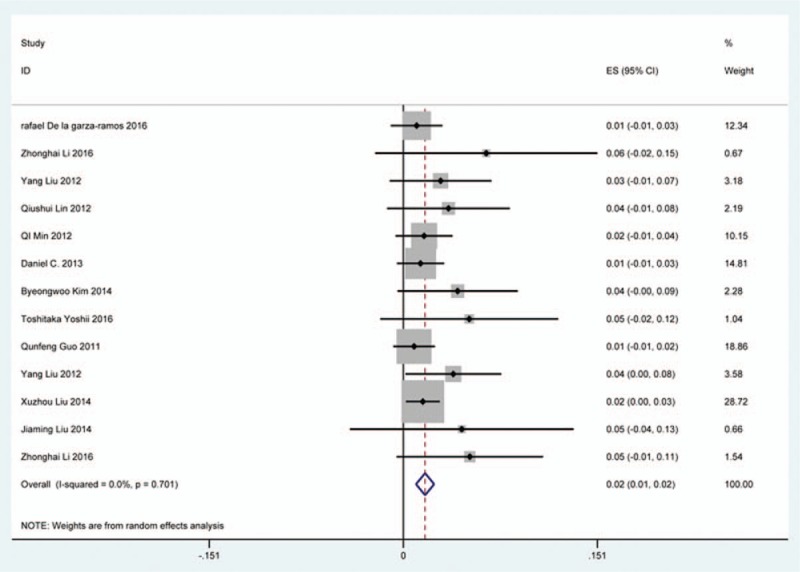
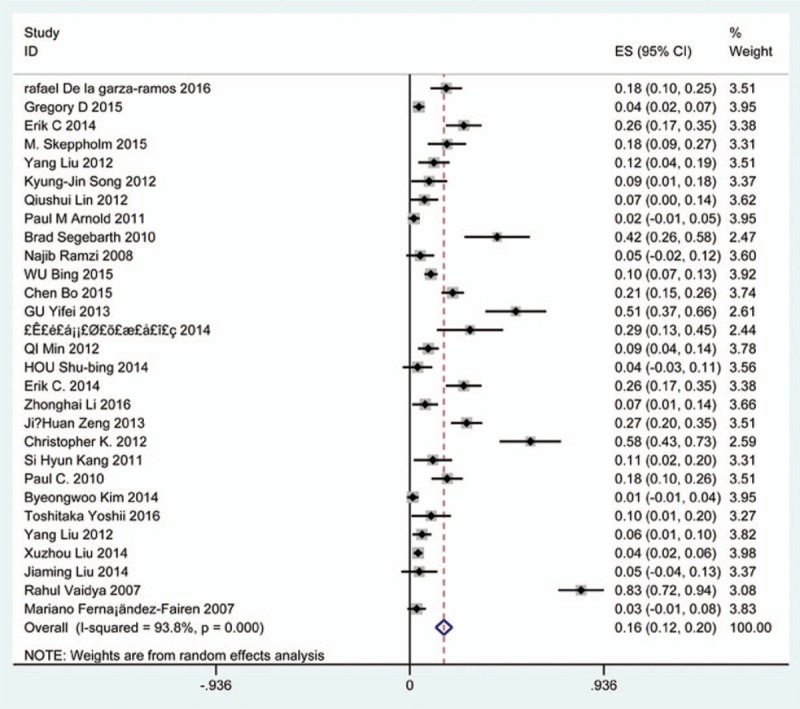
3.7. Infection
Twenty-five studies[20,23–25,33,35,36,40,47,51,59,61,62,68,69,73–76,78,85,86,91,117,118] containing 142 patients with infection of 3489 patients after cervical surgery were included. Figure 21 shows that the incidence was 2.8% (95% CI 1.7%–4.0%), with substantial heterogeneity of incidence observed. The incidence varied between 0.4% and 54.6%. Incidence for the patients who underwent ACCF was 14.2% (95% CI −1.1%–30.3%), which higher than those who received ACDF (0.9%, 95% CI 0.2%–2.8%) and LP (2.1%, 95% CI 0.9%–3.2%) (Fig 22, Fig 23, Fig 24).
Figure 21.
Forest plot showing incidence of infection. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 22.
Funnel plot showing incidence of infection after ACCF. ACCF = anterior cervical corpectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 23.
Forest plot showing incidence of Infection after ACDF. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 24.
Forest plot showing incidence of infection after LP. CI = confidence interval, df = degrees of freedom, LP = laminoplasty, M–H = Mantel–Haenszel.
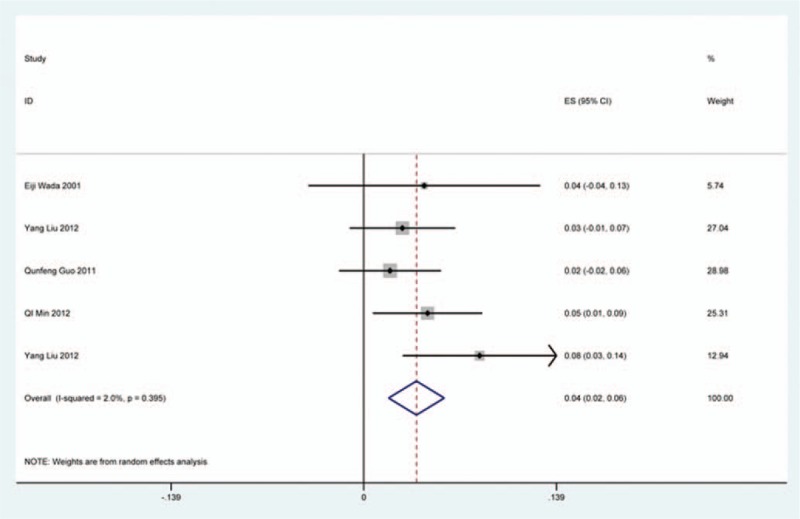
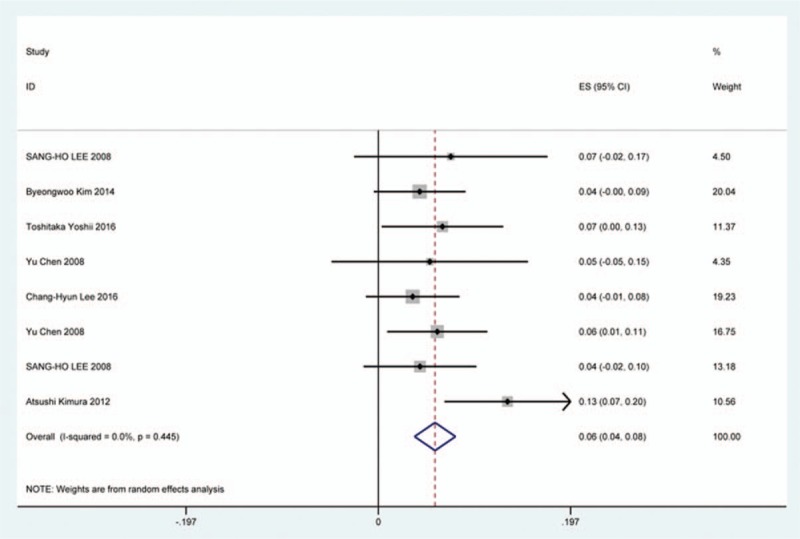
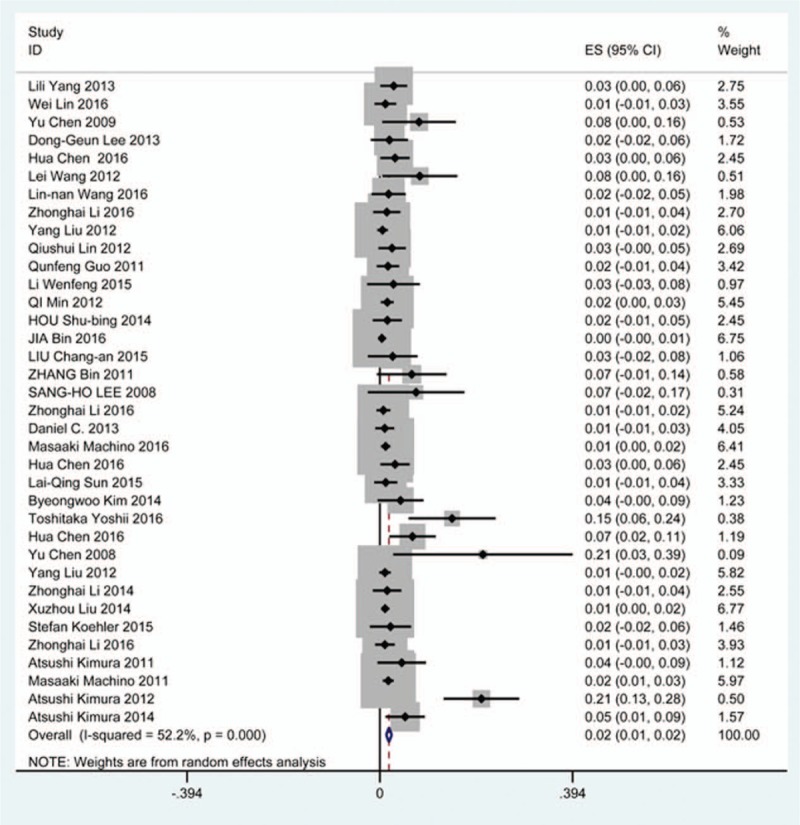
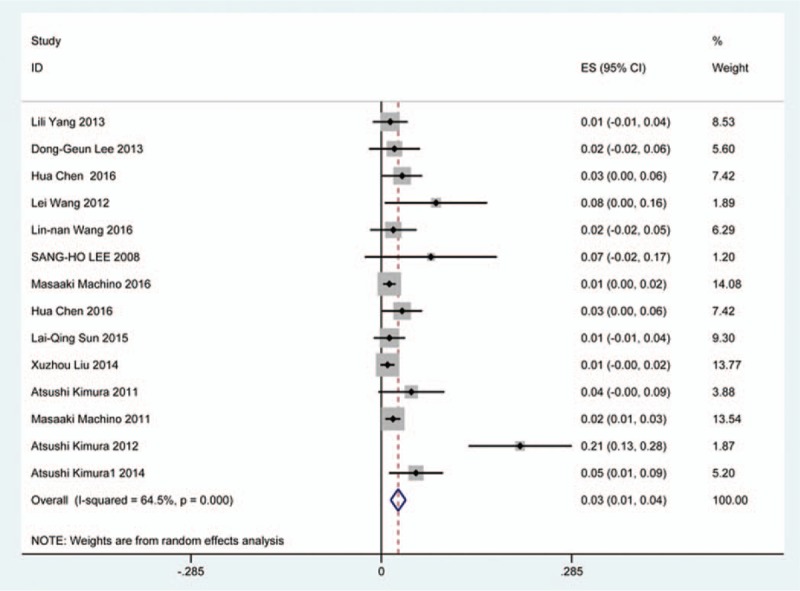
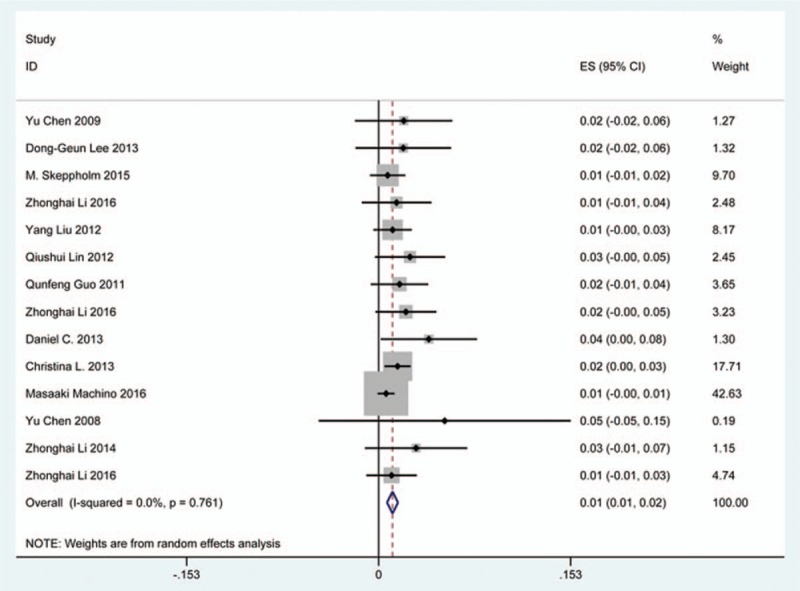
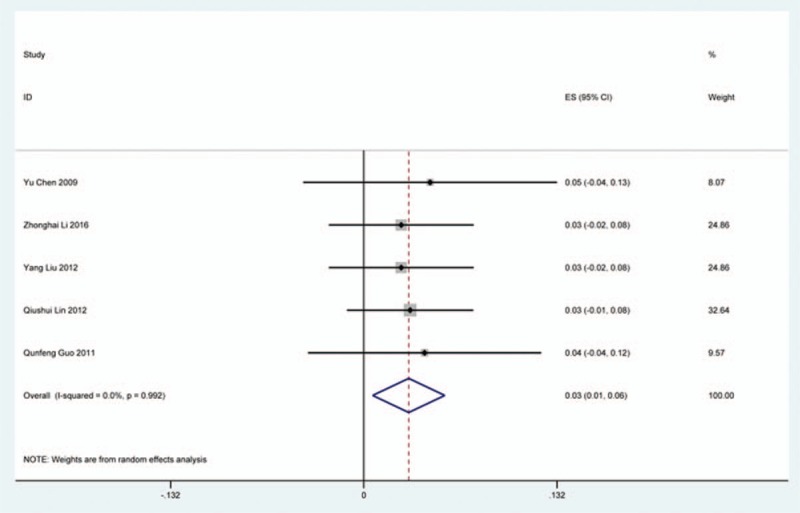
3.8. Axial pain
Twenty-three studies[20–22,26,30,34,44,46,48,49,56,60,61,66,73,81,83,84,88,89,92,118,119] containing 372 patients with axial pain of 2650 patients after cervical surgery were included for meta-analysis. Figure 25 shows that the incidence was 15.6% (95% CI 11.7%–19.5%), without substantial heterogeneity of incidence observed. The incidence varied between 1.7% and 53.2%. Incidence of axial pain for those following LP and LF was 22.2% (95% CI 14.1%–29.3%) and 23.2% (95% CI 15.8%–31.3%) (Figs. 26, 27).
Figure 25.
Forest plot showing incidence of axial pain. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 26.
Forest plot showing incidence of axial pain after LP. CI = confidence interval, df = degrees of freedom, LP = laminoplasty, M–H = Mantel–Haenszel.
Figure 27.
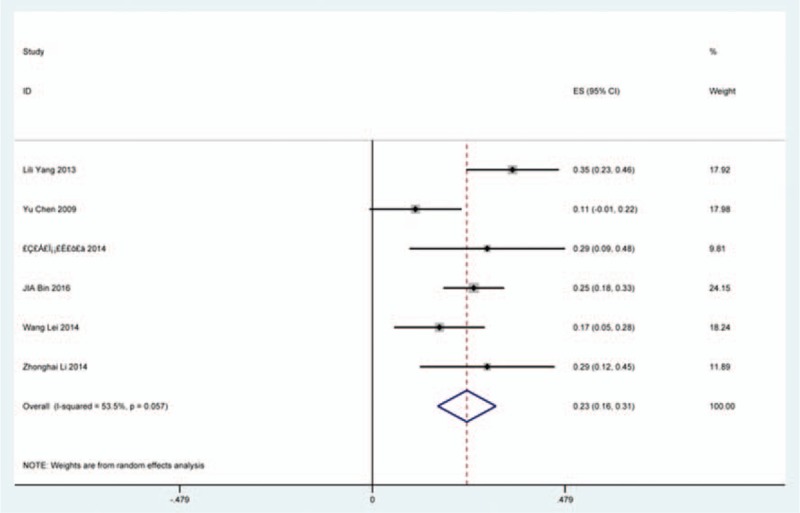
Forest plot showing incidence of axial pain after LF. df = degrees of freedom, I = confidence interval, LF = laminectomy and fusion, M–H = Mantel–Haenszel.
3.9. Hoarseness
Nineteen studies[25,26,31,35,36,38,40,45,56,62,70,79,81,84–86,90,100,116] containing 99 patients with hoarseness of 2234 patients after cervical surgery were included. Figure 28 shows that the incidence of hoarseness was 4.0% (95% CI 2.3%–5.7%), with substantial heterogeneity of incidence observed. The incidence varied between 0.6% and 60.9%. Patients after ACDF (4.8%, 95% CI 1.9%–7.8%) had a slight higher prevalence of hoarseness than those with ACCF (3.0%, 95% CI 0.9%–4.2%) (Figs. 29, 30).
Figure 28.
Forest plot showing incidence of hoarseness. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 29.
Forest plot showing incidence of hoarseness after ACCF. ACCF = anterior cervical corpectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 30.
Forest plot showing incidence of hoarseness after ACDF. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
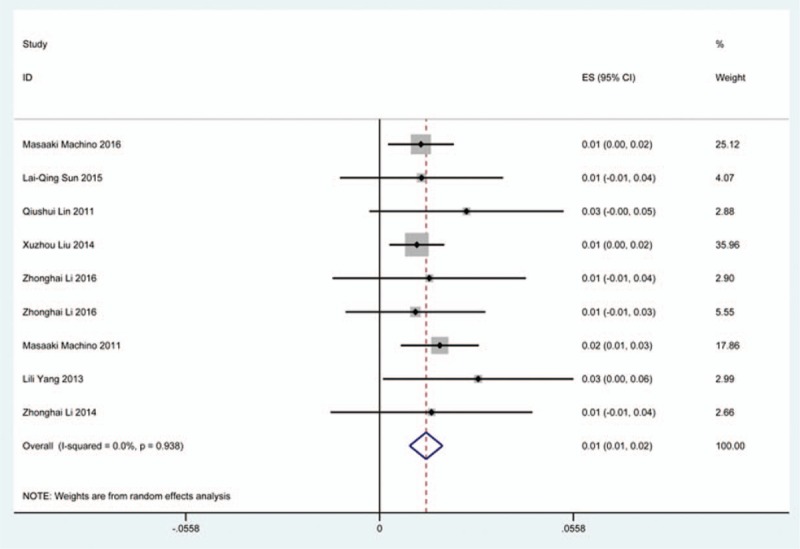
3.10. Epidural hematoma
Fourteen studies[22,23,33–35,38,39,56,61,65,74,79,81,120] containing 33 patients with epidural hematoma of 2185 patients after cervical surgery were included. Figure 31 shows that the incidence was 1.1% (95% CI 0.7%–1.5%), without substantial heterogeneity of incidence observed. The incidence varied between 0.5% and 5.3%. Incidence of axial pain for those following ACCF and ACDF was 3.1% (95% CI 1.0%–6.2%) and 2.0% (95% CI 0.9%–3.2%) (Figs. 32, 33).
Figure 31.
Forest plot showing incidence of epidural hematoma. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 32.
Forest plot showing incidence of epidural hematoma after ACCF. ACCF = anterior cervical corpectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
Figure 33.
Forest plot showing incidence of epidural hematoma after ACDF. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
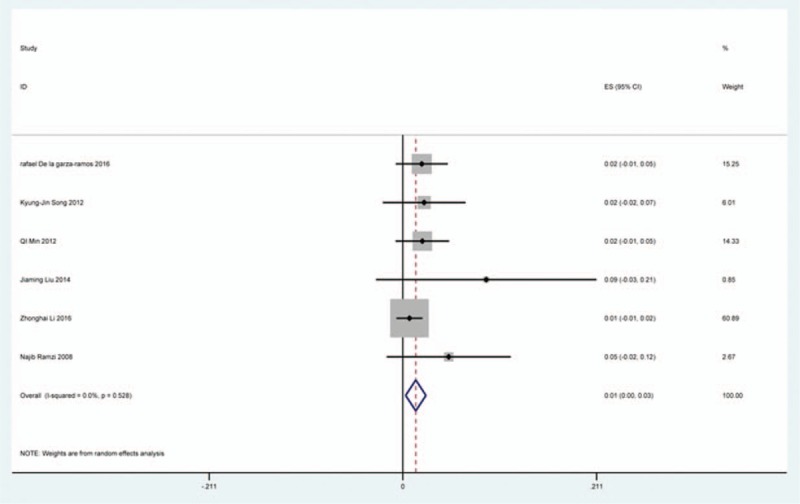
3.11. Graft dislodgment
Ten studies[35,38,40,45,62,64,69,81,82,121] containing 45 patients with graft dislodgment of 1102 patients after cervical surgery were included. Figure 34 shows that the incidence was 3.4% (95% CI 2.0%–4.8%), without substantial heterogeneity of incidence observed. The incidence among the studies varied between 1.4% and 8.2%.
Figure 34.
Forest plot showing incidence of graft dislodgment. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
3.12. Graft subsidence
Six studies[34,35,38,39,84,115] containing 26 patients with graft subsidence of 591 patients after cervical surgery were included. Figure 35 shows that the incidence of graft subsidence was 3.7% (95% CI 2.0%–5.5%), with substantial heterogeneity of incidence observed. The incidence varied between 2.2% and 11.1%.
Figure 35.
Forest plot showing incidence of graft subsidence. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
3.13. Fusion failure
Five studies[26,39,86,87,90] containing 21 patients with fusion failure of 689 patients after cervical surgery was included. Figure 36 shows that the incidence was 2.6% (95% CI 0.2%–4.9%), with substantial heterogeneity of incidence observed. The incidence varied between 0.2% and 12%.
Figure 36.
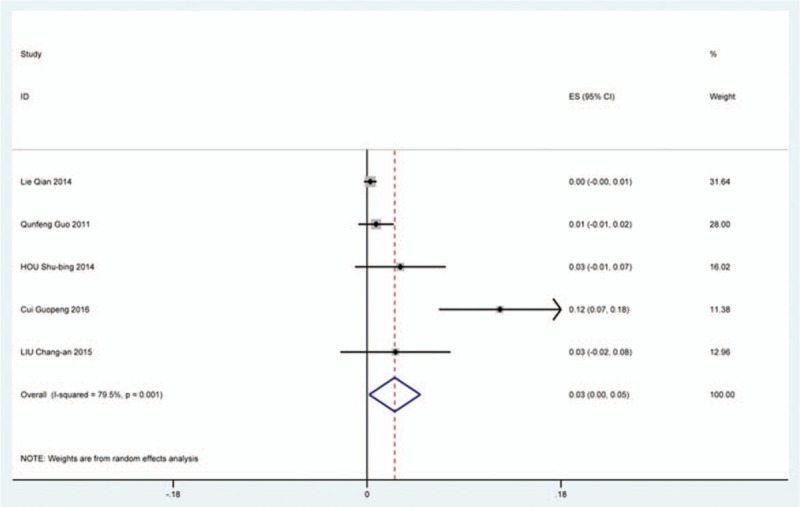
Forest plot showing incidence of fusion failure. CI = confidence interval, df = degrees of freedom, M–H = Mantel–Haenszel.
3.14. Publication bias
We performed funnel plot for publication bias, as shown in Fig. 37, after a detection of publication bias by Egger and Begg tests using STATA 12.0, there was no publication bias found for all included studies (all P > 0.05).
Figure 37.
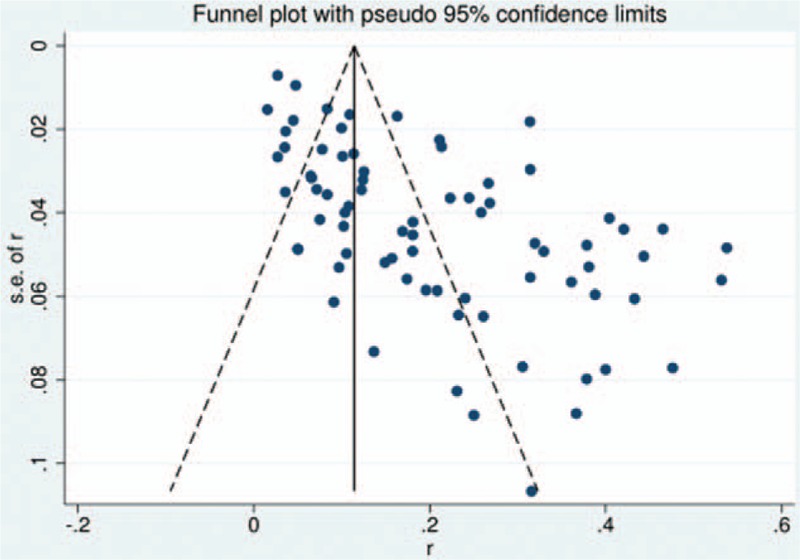
Funnel plot showing incidence of all complications after cervical surgery.
4. Discussion
Increasing studies focused on surgical selection for cervical compressive myelopathy (CCM), which usually caused by CSM or OPLL.[3–5,33] Nearly half a century, surgical procedures were widely applied from posterior approaches including LF and LP to anterior approaches containing ACDF, ACCF, and ACCDF.[47,78] Nevertheless, the option of surgical approach remains debated. Especially, the inevitable complications of anterior and posterior approaches cause our attention.[22,36,48] Anterior approaches had a higher rate of postoperative hoarseness, dysphagia.[55,81] Similarly, C5 palsy and cervical kyphosis may limit the use of posterior surgery.[26] The complications in our study included overall complications, C5 plasy, cerebrospinal fluid (CSF), infection, axial pain, dysphagia, hoarseness, fusion failure, graft subsidence, graft dislodgment, and epidural hematoma. As we know, this is the first meta-analysis on prevalence of various complications after cervical surgery. The aim of the study is to compute prevalence of each complication according to previous studies. We hope that our work can give some suggestions to assess incidence of complications before surgery.
Our results showed that the rates for total complications, C5 plasy, CSF, infection, axial pain, dysphagia, hoarseness, fusion failure, graft subsidence, graft dislodgment and epidural hematoma were 20.1%, 5.3%, 1.9%, 2.8%, 15.6%, 16.8%, 4.0%, 2.6%, 3.7%, 3.4%, 1.1%, respectively. Compared with patients with CSM, patients with OPLL have a higher incidence of C5 plasy (4.1% vs 6.3%) and CSF (0.9% vs 12.2%). In terms of C5 plasy, patients after LP had the highest rate (15.2%), while those after ACDF had the lowest rate (2.0%). As for dysphagia, patients who underwent ACCDF and ACDF were 16.8% and 16.2%, which are higher than those who received ACCF (9.9%). For CSF, patients who underwent ACCF had the highest rate (4.2%), while those who received ACDF had the lowest rate (1.9%), and the same trend for infection between ACCF group (14.2%) and ACDF group (0.9%). While it was opposite for hoarseness between ACDF (4.8%) and ACCF (3.0%).
A number of studies focused on the occurrence of C5 palsy after cervical surgery. Even though some mechanisms trying to explain this common complication have been proposed, it remained a controversial issue. C5 palsy after cervical surgery is considered to be a result of nerve root injury or segmental spinal cord disorder.[36–41,51–55] We reviewed 57 studies and the rate of C5 plasy was 5.3%. We also found that patients with CSM (4.1%) have a lower incidence of C5 palsy than patients with OPLL (6.3%). The reason is still unclear. In all surgical options, LF had the highest rate, ACDF had the lowest incidence. Nakashima[72] reported that C5 palsy was caused by posterior shift of the spinal cord, and additional iatrogenic foraminal stenosis due to cervical alignment correction after posterior instrumentation with fusion. It was obvious that posterior shift of the spinal cord in LF was largest, which was similar to our results.
Dysphagia is a relatively common complication after cervical surgery. Smith-Hammond et al[121] found that the prevalence of dysphagia on the first postoperative day was approximately 50% in the anterior cervical group. As Fig. 11 has shown, the rate was 16.8% (95% CI 13.6%–19.9%). According to included articles in our series, the rate for this complication ranged from 1.4% to 58.1%. Patients after ACCDF (16.8%, 95% CI 6.9%–27.2%) and ACDF (16.2%, 95% CI 11.7%–19.8%) had higher incidence than those who received ACCF (9.9%, 95% CI 4.8%–15.9%). Multifactors as reported by recent studies,[63,68–71,75–80] hematoma, pharyngeal plexus denervation, vocal cord paralysis, adhesion formation, plate profile, and swelling due to biologic agents, may be related to dysphagia. Brad[99] indicated that a no-profile cervical disc arthroplasty had a significantly lower rate of dysphagia compared with ACDF. Due to few included articles on disc arthroplasty, we did not assess rate of dysphagia in arthroplasty group.
CSF is a serious complication of cervical surgery,[87,88] which may cause wound infection, purulent meningitis, or even high risk of death. Rate of CSF after cervical operation ranged from 0.4% and 21.1%[122]. As the same with previous reports, our results implied that patients with OPLL had a higher rate compared with those with CSM. We surprisingly found that patients after ACCF (4.2%) had a higher rate than those who received ACDF (1.9%), which was possibly different with our thinking. Compared with ACCF, operative field of ACDF was smaller, which was more likely to cause CSF. Large sample studies are needed to further investigate this issue. Figure 21 shows that the rate of infection was 2.8%. The same trend as CSF, individual who underwent ACCF (14.2%) had higher than those who received ACDF (0.9%) and LP (2.1%).
As for axial pain, which is terrible complication after posterior approaches, the results show that LP (22.2%) and LF (23.2%) are similar. Muscles were widely dissected and ligamentous structures transected in both techniques resulting in axial pain to some extent. Hoarseness and epidural hematoma had relatively low rate. Overstretch or improper handing may lead to these complications. We also estimated implant-related complications, but the rate on these complications in various surgical options were not assessed due to lack relevant data. The rates of graft dislodgment, graft subsidence, and fusion failure were 3.7%, 3.4%, and 1.1%.
There are several limitations of this study. First, there was no RCT on all complications, we need RCT to further study; second, the statistical power could be improved in the future by including more studies. Some parameters, like one-level, two-level, or multilevel CSM for C5 palsy, due to lack of data could not be analyzed by subgroups to avoid a high heterogeneity which may exert instability on the consistency of the outcomes; third, the searching strategy was restricted to articles published in the English and Chinese languages. Articles with potentially high-quality data published in other languages were not included because of anticipated difficulties in obtaining accurate medical translations. Fourth, it is difficult to avoid that many figures presented high heterogeneity due to relative large sample.
In summary, the rate of overall complications was 21%, patients with OPLL have a higher incidence of C5 palsy and CSF. Patients after LF have a higher incidence of C5 palsy, ACCDF have a higher incidence of dysphagia, ACCF have a higher incidence of CSF and infection, and ACDF have a higher incidence of hoarseness. Considering the limitations noted above, a further well-designed, large population-based study on the topic of the prevalence of complications after cervical surgery should be conducted.
Footnotes
Abbreviations: ACCDF = anterior corpectomy combined with discectomy, ACCF = anterior cervical corpectomy and fusion, ACDF = anterior cervical discectomy and fusion, C5 palsy = C5 nerve root palsy, CI = confidence intervals, CSF = cerebrospinal fluid, CSM = cervical spondylotic myelopathy, LF = laminectomy and fusion, LP = laminoplasty, OPLL = ossification of posterior longitudinal ligament.
TW, X-MT, S-KL, and HW are co-first authors.
Authors’ contributions—conceived and designed the study: W-YD; collected data: TW, HW; analyzed the data: TW, X-MT; wrote the paper: TW and S-KL.
The authors have no conflicts of interest to disclose.
References
- [1].Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg 2001;9:376–88. [DOI] [PubMed] [Google Scholar]
- [2].Geck MJ, Eismont FJ. Surgical options for the treatment of cervical spondylotic myelopathy. Orthop Clin North Am 2002;33:329–48. [DOI] [PubMed] [Google Scholar]
- [3].Yalamanchili PK, Vives MJ, Chaudhary SB. Cervical spondylotic myelopathy: factors in choosing the surgical approach. Adv Orthop 2012;2012:783762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Liu G, Buchowski JM, Bunmaprasert T, et al. Revision surgery following cervical laminoplasty: etiology and treatment strategies. Spine 2009;34:2760–8. [DOI] [PubMed] [Google Scholar]
- [5].Chiba K, Ogawa Y, Ishii K, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy—average 14-year follow-up study. Spine 2006;31:2998–3005. [DOI] [PubMed] [Google Scholar]
- [6].Takeuchi T, Shono Y. Importance of preserving the C7 spinous process and attached nuchal ligament in French-door laminoplasty to reduce postoperative axial symptoms. Eur Spine J 2007;16:1417–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Liu J, Ebraheim NA, Sanford CG, Jr, et al. Preservation of the spinous process-ligament-muscle complex to prevent kyphotic deformity following laminoplasty. Spine J 2007;7:159–64. [DOI] [PubMed] [Google Scholar]
- [8].Ogawa Y, Toyama Y, Chiba K, et al. Long-term results of expansive open door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 2004;1:168–74. [DOI] [PubMed] [Google Scholar]
- [9].Brons S, Becking AG, Tuinzing DB. Value of informed consent in surgical orthodontics. Oral Maxillofac Surg 2009;67:1021–5. [DOI] [PubMed] [Google Scholar]
- [10].Betti S, Sironi A, Saino G, et al. Effect of the informed consent process on anxiety and comprehension of patients undergoing esophageal and gastrointestinal surgery. Gastrointest Surg 2011;15:922–7. [DOI] [PubMed] [Google Scholar]
- [11].Falagas ME, Korbila IP, Giannopoulou KP, et al. Informed consent: how much and what do patients understand? Am J Surg 2009;198:420–35. [DOI] [PubMed] [Google Scholar]
- [12].Sakaura H, Hosono N, Mukai Y, et al. Preservation of the nuchal ligament plays an important role in preventing unfavorable radiologic changes after laminoplasty. J Spinal Disord Tech 2008;21:338–43. [DOI] [PubMed] [Google Scholar]
- [13].Ono A, Tonosaki Y, Yokoyama T, et al. Surgical anatomy of the nuchal muscles in the posterior cervicothoracic junction. Significance of the preservation of the C7 spinous process in cervical laminoplasty. Spine 2008;33:E349–54. [DOI] [PubMed] [Google Scholar]
- [14].Satomi K, Ogawa J, Ishii Y, et al. Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine J 2001;1:26–30. [DOI] [PubMed] [Google Scholar]
- [15].Minamide A, Yoshida M, Yamada H, et al. Clinical outcomes of microendoscopic decompression surgery for cervical myelopathy. Eur Spine J 2010;19:487–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Nikaido T, Kikuchi S, Yabuki S, et al. Surgical treatment assessment using the Japanese orthopedic association cervical myelopathy evaluation questionnaire in patients with cervical myelopathy: a new outcome measure for cervical myelopathy. Spine (Phila Pa 1976) 2009;34:2568–72. [DOI] [PubMed] [Google Scholar]
- [17].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959;22:719–48. [PubMed] [Google Scholar]
- [19].Yeh KT, Lee RP, Chen IH, et al. The midterm surgical outcome of modified expansive open-door laminoplasty. Biomed Res Int 2016;2016:8069354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Yang L, Gu Y, Shi J, et al. Modified plate-only open-door laminoplasty versus laminectomy and fusion for the treatment of cervical stenotic myelopathy. Orthopedics 2013;36:e79–87. [DOI] [PubMed] [Google Scholar]
- [21].Tanaka S, Tashiro T, Gomi A, et al. Cervical unilateral open-door laminoplasty with titanium miniplates through newly designed hydroxyapatite spacers. Neurol Med Chir (Tokyo) 2011;51:673–7. [DOI] [PubMed] [Google Scholar]
- [22].Chen Y, Guo Y, Lu X, et al. Surgical strategy for multilevel severe ossification of posterior longitudinal ligament in the cervical spine. J Spinal Disord Tech 2011;24:24–30. [DOI] [PubMed] [Google Scholar]
- [23].Lee DG, Lee SH, Park SJ, et al. Comparison of surgical outcomes after cervical laminoplasty: open-door technique versus French-door technique. J Spinal Disord Tech 2013;26:E198–203. [DOI] [PubMed] [Google Scholar]
- [24].Chen H, Liu H, Deng Y, et al. Multivariate analysis of factors associated with axial symptoms in unilateral expansive open-door cervical laminoplasty with miniplate fixation. Medicine (Baltimore) 2016;95:e2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].De la Garza-Ramos R, Xu R, Ramhmdani S, et al. Long-term clinical outcomes following 3- and 4-level anterior cervical discectomy and fusion. J Neurosurg Spine 2016;24:885–91. [DOI] [PubMed] [Google Scholar]
- [26].Qian L, Shao J, Liu Z, et al. Comparison of the safety and efficacy of anterior 'skip’ corpectomy versus posterior decompression in the treatment of cervical spondylotic myelopathy. J Orthop Surg Res 2014;9:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wang L, Song Y, Liu L, et al. Clinical outcomes of two different types of open-door laminoplasties for cervical compressive myelopathy: a prospective study. Neurol India 2012;60:210–6. [DOI] [PubMed] [Google Scholar]
- [28].Wang LN, Wang L, Song YM, et al. Clinical and radiographic outcome of unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation for cervical compressive myelopathy: a five-year follow-up study. Int Orthop 2016;40:1267–74. [DOI] [PubMed] [Google Scholar]
- [29].Williams KE, Paul R, Dewan Y, et al. Functional outcome of corpectomy in cervical spondylotic myelopathy. Indian J Orthop 2009;43:205–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Yeh KT, Chen IH, Yu TC, et al. Modified expansive open-door laminoplasty technique improved postoperative neck pain and cervical range of motion. J Formos Med Assoc 2015;114:1225–32. [DOI] [PubMed] [Google Scholar]
- [31].Kamani MM, Ballal A, Shetty V, et al. A prospective study of the functional outcome of anterior cervical discectomy with fusion in single level degenerative cervical disc prolapse. J Clin Diagn Res 2016;10:RC01–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Schroeder GD, Kurd MF, Kepler CK, et al. Comparing the treatment algorithm and complications for patients undergoing an anterior cervical discectomy and fusion at a physician-owned specialty hospital and a university-owned tertiary care hospital. Am J Med Qual 2015;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [33].Skeppholm M, Lindgren L, Henriques T, et al. The Discover artificial disc replacement versus fusion in cervical radiculopathy—a randomized controlled outcome trial with 2-year follow-up. Spine J 2015;15:1284–94. [DOI] [PubMed] [Google Scholar]
- [34].Li Z, Huang J, Zhang Z, et al. A comparison of multilevel anterior cervical discectomy and corpectomy in patients with 4-level cervical spondylotic myelopathy: a minimum 2-year follow-up study. Clin Spine Surg 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [35].Liu Y, Hou Y, Yang L, et al. Comparison of 3 reconstructive techniques in the surgical management of multilevel cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2012;37:E1450–8. [DOI] [PubMed] [Google Scholar]
- [36].Song KJ, Yoon SJ, Lee KB. Three- and four-level anterior cervical discectomy and fusion with a PEEK cage and plate construct. Eur Spine J 2012;21:2492–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kim S, Lee SH, Kim ES, et al. Clinical and radiographic analysis of c5 palsy after anterior cervical decompression and fusion for cervical degenerative disease. J Spinal Disord Tech 2014;27:436–41. [DOI] [PubMed] [Google Scholar]
- [38].Lin Q, Zhou X, Wang X, et al. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. Eur Spine J 2012;21:474–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Guo Q, Bi X, Ni B, et al. Outcomes of three anterior decompression and fusion techniques in the treatment of three-level cervical spondylosis. Eur Spine J 2011;20:1539–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ramzi N, Ribeiro-Vaz G, Fomekong E, et al. Long term outcome of anterior cervical discectomy and fusion using coral grafts. Acta Neurochir (Wien) 2008;150:1249–56. [DOI] [PubMed] [Google Scholar]
- [41].Fernández-Fairen M, Sala P, Dufoo M, Jr, et al. Anterior cervical fusion with tantalum implant: a prospective randomized controlled study. Spine (Phila Pa 1976) 2008;33:465–72. [DOI] [PubMed] [Google Scholar]
- [42].Kimura A, Endo T, Inoue H, et al. Preoperative predictors of patient satisfaction with outcome after cervical laminoplasty. Global Spine J 2014;4:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Chang V, Lu DC, Hoffman H, et al. Clinical results of cervical laminectomy and fusion for the treatment of cervical spondylotic myelopathyin 58 consecutive patients. Surg Neurol Int 2014;5suppl 3:S133–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Zhang H, Zhu R, Yang H, et al. Multifactor analysis on the outcomes of cervical spondylotic myelopathy with expansive open-door laminoplasty. J Int Med Res 2012;40:1608–16. [DOI] [PubMed] [Google Scholar]
- [45].Kimura A, Seichi A, Hoshino Y, et al. Perioperative complications of anterior cervical decompression with fusion in patients with ossification of the posterior longitudinal ligament: a retrospective, multi-institutional study. J Orthop Sci 2012;17:667–72. [DOI] [PubMed] [Google Scholar]
- [46].Jiang JL, Li XL, Zhou XG, et al. Plate-only open-door laminoplasty with fusion for treatment of multilevel degenerative cervical disease. J Clin Neurosci 2012;19:804–9. [DOI] [PubMed] [Google Scholar]
- [47].Machino M, Yukawa Y, Hida T, et al. Modified double-door laminoplasty in managing multilevel cervical spondylotic myelopathy: surgical outcome in 520 patients and technique description. J Spinal Disord Tech 2013;26:135–40. [DOI] [PubMed] [Google Scholar]
- [48].Kimura A, Seichi A, Inoue H, et al. Long-term results of double-door laminoplasty using hydroxyapatite spacers in patients with compressive cervical myelopathy. Eur Spine J 2011;20:1560–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Sakaura H, Hosono N, Mukai Y, et al. Medium-term outcomes of C3-6 laminoplasty for cervical myelopathy: a prospective study with a minimum 5-year follow-up. Eur Spine J 2011;20:928–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Liu Y, Yu KY, Hu JH. Hybrid decompression technique and two-level corpectomy are effective treatments for three-level cervical spondylotic myelopathy. J Zhejiang Univ Sci B 2009;10:696–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Kristof RA, Kiefer T, Thudium M, et al. Comparison of ventral corpectomy and plate-screw-instrumented fusion with dorsal laminectomy and rod-screw-instrumented fusion for treatment of at least two vertebral-level spondylotic cervical myelopathy. Eur Spine J 2009;18:1951–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Konya D, Ozgen S, Gercek A, et al. Outcomes for combined anterior and posterior surgical approaches for patients with multisegmental cervical spondylotic myelopathy. J Clin Neurosci 2009;16:404–9. [DOI] [PubMed] [Google Scholar]
- [53].Ishii M, Wada E, Ishii T, et al. Laminoplasty for patients aged 75 years or older with cervical myelopathy. J Orthop Surg (Hong Kong) 2008;16:211–4. [DOI] [PubMed] [Google Scholar]
- [54].Chen Y, Guo Y, Chen D, et al. Long-term outcome of laminectomy and instrumented fusion for cervical ossification of the posterior longitudinal ligament. Int Orthop 2009;33:1075–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Lee CH, Jahng TA, Hyun SJ, et al. Expansive laminoplasty versus laminectomy alone versus laminectomy and fusion for cervical ossification of the posterior longitudinal ligament: is there a difference in the clinical outcome and sagittal alignment? Clin Spine Surg 2016;29:E9–15. [DOI] [PubMed] [Google Scholar]
- [56].Li Z, Wang H, Tang J, et al. Comparison of 3 reconstructive techniques in the surgical management of patients with 4-level cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [57].Koehler S, Raslan F, Stetter C, et al. Autologous bone graft versus PEKK cage for vertebral replacement after 1- or 2-level anterior median corpectomy. J Neurosurg Spine 2015;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [58].Lau D, Chou D, Mummaneni PV, et al. Two-level corpectomy versus three-level discectomy for cervical spondylotic myelopathy: a comparison of perioperative, radiographic, and clinical outcomes. J Neurosurg Spine 2015;23:280–9. [DOI] [PubMed] [Google Scholar]
- [59].Liu J, Chen X, Liu Z, et al. Anterior cervical discectomy and fusion versus corpectomy and fusion in treating two-level adjacent cervical spondylotic myelopathy: a minimum 5-year follow-up study. Arch Orthop Trauma Surg 2015;135:149–53. [DOI] [PubMed] [Google Scholar]
- [60].Liu X, Wang H, Zhou Z, et al. Anterior decompression and fusion versus posterior laminoplasty for multilevel cervical compressive myelopathy. Orthopedics 2014;37:e117–22. [DOI] [PubMed] [Google Scholar]
- [61].Li Z, Guo Z, Hou S, et al. Segmental anterior cervical corpectomy and fusion with preservation of middle vertebrae in the surgical management of 4-level cervical spondylotic myelopathy. Eur Spine J 2014;23:1472–9. [DOI] [PubMed] [Google Scholar]
- [62].Liu Y, Qi M, Chen H, et al. Comparative analysis of complications of different reconstructive techniques following anteriorde compression for multilevel cervical spondylotic myelopathy. Eur Spine J 2012;21:2428–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Gandhoke G, Wu JC, Rowland NC, et al. Anterior corpectomy versus posterior laminoplasty: is the risk of postoperative C-5 palsy different? Neurosurg Focus 2011;31:E12. [DOI] [PubMed] [Google Scholar]
- [64].Okawa A, Sakai K, Hirai T, et al. Risk factors for early reconstruction failure of multilevel cervical corpectomy with dynamic plate fixation. Spine (Phila Pa 1976) 2011;36:E582–7. [DOI] [PubMed] [Google Scholar]
- [65].Chen Y, Chen D, Wang X, et al. Anterior corpectomy and fusion for severe ossification of posterior longitudinal ligament in the cervical spine. Int Orthop 2009;33:477–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Chen H, Li H, Wang B, et al. Facet joint disturbance induced by miniscrews in plated cervical laminoplasty: dose it influence the clinical and radiologic outcomes? Medicine (Baltimore) 2016;95:e4666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Zhou H, Liu ZJ, Wang SB, et al. Laminoplasty with lateral mass screw fixation for cervical spondylotic myelopathy in patients with athetoid cerebral palsy: a retrospective study. Medicine (Baltimore) 2016;95:e5033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Blizzard DJ, Caputo AM, Sheets CZ, et al. Laminoplasty versus laminectomy with fusion for the treatment of spondylotic cervical myelopathy: short-term follow-up. Eur Spine J 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [69].Yoshii T, Sakai K, Hirai T, et al. Anterior decompression with fusion versus posterior decompression with fusion for massive cervical ossification of the posterior longitudinal ligament with a ≥50% canal occupying ratio: a multicenter retrospective study. Spine J 2016;16:1351–7. [DOI] [PubMed] [Google Scholar]
- [70].Kim B, Yoon DH, Shin HC, et al. Surgical outcome and prognostic factors of anterior decompression and fusion for cervical compressive myelopathy due to ossification of the posterior longitudinal ligament. Spine J 2015;15:875–84. [DOI] [PubMed] [Google Scholar]
- [71].Sun LQ, Li M, Li YM, et al. Predictors for surgical outcome of laminoplasty for cervical spondylotic myelopathy. World Neurosurg 2016;94:89–96. [DOI] [PubMed] [Google Scholar]
- [72].Nakashima H, Tetreault L, Nagoshi N, et al. Comparison of outcomes of surgical treatment for ossification of the posterior longitudinal ligament versus other forms of degenerative cervical myelopathy: results from the prospective, multicenter AO Spine CSM-International Study of 479 Patients. J Bone Joint Surg Am 2016;98:370–8. [DOI] [PubMed] [Google Scholar]
- [73].Chen H, Liu H, Deng Y, et al. Multivariate analysis of factors associated with axial symptoms in unilateral expansive open-door cervical laminoplasty with miniplate fixation. Medicine (Baltimore) 2016;95:e2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Machino M, Yukawa Y, Imagama S, et al. Surgical treatment assessment of cervical laminoplasty using quantitative performance evaluation in elderly patients: a prospective comparative study in 505 patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2016;41:757–63. [DOI] [PubMed] [Google Scholar]
- [75].Oshima Y, Miyoshi K, Mikami Y, et al. Long-term outcomes of cervical laminoplasty in the elderly. Biomed Res Int 2015;2015:713952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Yeh KT, Lee RP, Chen IH, et al. Laminoplasty instead of laminectomy as a decompression method in posterior instrumented fusion for degenerative cervical kyphosis with stenosis. J Orthop Surg Res 2015;10:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Maeno T, Okuda S, Yamashita T, et al. Age-related surgical outcomes of laminoplasty for cervical spondylotic myelopathy. Global Spine J 2015;5:118–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Nakashima H, Yukawa Y, Imagama S, et al. Complications of cervical pedicle screw fixation for nontraumatic lesions: a multicenter study of 84patients. J Neurosurg Spine 2012;16:238–47. [DOI] [PubMed] [Google Scholar]
- [79].Lu DC, Tumialán LM, Chou D. Multilevel anterior cervical discectomy and fusion with and without rhBMP-2: a comparison of dysphagiarates and outcomes in 150 patients. J Neurosurg Spine 2013;18:43–9. [DOI] [PubMed] [Google Scholar]
- [80].Wu B, Song F, Zhu S. Reasons of dysphagia after operation of anterior cervical decompression and fusion. Clin Spine Surg 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [81].Li Z, Zhao Y, Tang J, et al. A comparison of a new zero-profile, stand-alone Fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [82].Lee SH, Ahn Y, Lee JH. Laser-assisted anterior cervical corpectomy versus posterior laminoplasty for cervical myelopathic patients with multilevel ossification of the posterior longitudinal ligament. Photomed Laser Surg 2008;26:119–27. [DOI] [PubMed] [Google Scholar]
- [83].Gao H, Chen X, Qiang W. Long-term efficacy of cervical posterior decompressions for cervical spondylotic myelopathy: a comparison between two kinds of surgical procedures. ACTA Acad Med Qingdao Univ 2014;50:509–15. [Google Scholar]
- [84].Li WF, Han DT. Clinical analysis of anterior and posterior cervical approaches in treatment for multilevel cervical spondylotic myelopathy. Fujian Med J 2015;37:39–42. [Google Scholar]
- [85].Qi M, Wang X, Liu Y, et al. Comparative analysis of complications of different anterior decompression procedures for treating multilevel cervical spondylotic myelopathy. Chin J Spine Spinal Cord 2012;22:963–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Hou SB, Shen Y, Wang LF, et al. A follow-up study of two anterior surgical interventions for multi-segmental cervical spondylotic myelopath. Orthopedic J China 2014;22:594–600. [Google Scholar]
- [87].Cui GP, Zhang LY, Zheng CW, et al. Comparative analysis of two different anterior combined approaches for treating multilevel cervical spondylotic myelopathy. Modern Pract Med 2016;28:716–8. [Google Scholar]
- [88].Jia B, Zhang CJ, Zhou XQ, et al. Modified cervical open -door laminoplasty versus cervical laminectomy and fusion for treatment of multilevel cervical myelopathy. China Med Herald 2016;13:69–73. [Google Scholar]
- [89].Hu Y, Zhao H-y, Dong W-x. Comparative study of laminoplasty and laminectomy combined fusion for treatment of multi-level cervical myelopathy. J Spinal Surg 2014;12:226–30. [Google Scholar]
- [90].Liu C-a, Zhang W-p, Wang L-y. Anterior decompression by subtotal vertebrectomy combined with bone grafting and internal fixation in treatment of multilevel cervical spondylotic myelopathy. Med Pharm J Chin PLA 2015;27:24–8. [Google Scholar]
- [91].Zhang B, Dai M, Tang Y-m, et al. Surgical treatment of ossification of the posterior longitudinal ligament of cervical spine. Orthop J China 2011;19:1601–4. [Google Scholar]
- [92].Wang L, Wang GH. Clinical analysis of posterior cervical laminectomy and fusion in the treatment for multilevel cervical spondylotic myelopathy. Hainan Med J 2014;25:1498–9. [Google Scholar]
- [93].Cherian J, Mayer RR, Haroun KB, et al. Contribution of lordotic correction on C5 palsy following cervical laminectomy and fusion. Neurosurgery 2016;79:816–22. [DOI] [PubMed] [Google Scholar]
- [94].Lee SH, Suk KS, Kang KC, et al. Outcomes and related factors of C5 palsy following cervical laminectomy with instrumented fusion compared with laminoplasty. Spine (Phila Pa 1976) 2016;41:E574–9. [DOI] [PubMed] [Google Scholar]
- [95].Blizzard DJ, Gallizzi MA, Sheets C, et al. The role of iatrogenic for aminal stenosis from lordotic correction in the development of C5 palsy after posterior laminectomy and fusion. J Orthop Surg Res 2015;10:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Li Q, Hu J, Tian Y, et al. Clinical observation and analysis of C5 plasy after cervical surgery. Chin J Bone Joint Surg 2012;5:433–7. [Google Scholar]
- [97].Olsson EC, Jobson M, Lim MR. Risk factors for persistent dysphagia after anterior cervical spine surgery. Orthopedics 2015;38:e319–23. [DOI] [PubMed] [Google Scholar]
- [98].Arnold PM, Rice LR, Anderson KK, et al. Factors affecting hospital length of stay following anterior cervical discectomy and fusion. Evid Based Spine Care J 2011;2:11–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Segebarth B, Datta JC, Darden B, et al. Incidence of dysphagia comparing cervical arthroplasty and ACDF. SAS J 2010;4:3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Vaidya R, Carp J, Sethi A, et al. Complications of anterior cervical discectomy and fusion using recombinant human bone morphogenetic protein-2. Eur Spine J 2007;16:1257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].McAfee PC, Cappuccino A, Cunningham BW, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech 2010;23:1–8. [DOI] [PubMed] [Google Scholar]
- [102].Kang SH, Kim DK, Seo KM, et al. Multi-level spinal fusion and postoperative prevertebral thickness increase the risk of dysphagia after anterior cervical spine surgery. J Clin Neurosci 2011;18:1369–73. [DOI] [PubMed] [Google Scholar]
- [103].Kalb S, Reis MT, Cowperthwaite MC, et al. Dysphagia after anterior cervical spine surgery: incidence and risk factors. World Neurosurg 2012;77:183–7. [DOI] [PubMed] [Google Scholar]
- [104].Kepler CK, Rihn JA, Bennett JD, et al. Dysphagia and soft-tissue swelling after anterior cervical surgery: a radiographic analysis. Spine J 2012;12:639–44. [DOI] [PubMed] [Google Scholar]
- [105].Zeng JH, Zhong ZM, Chen JT. Early dysphagia complicating anterior cervical spine surgery: incidence and risk factors. Arch Orthop Trauma Surg 2013;133:1067–71. [DOI] [PubMed] [Google Scholar]
- [106].Reinard KA, Cook DM, Zakaria HM, et al. A cohort study of the morbidity of combined anterior-posterior cervical spinal fusions: incidence and predictors of postoperative dysphagia. Eur Spine J 2016;25:2068–77. [DOI] [PubMed] [Google Scholar]
- [107].Chen Z, Huang X, Li F, et al. Related factors to dysphagia after anterior cervical spine surgery. Chin J Spine Spinal Cord 2012;22:979–83. [Google Scholar]
- [108].Sang P-m, Zhang M, Chen B-h. Cause analysis of dysphagia after anterior cervical spine surgery. China J Orthop Traum 2016;29:350–4. [Google Scholar]
- [109].Ma J-x, Xiang L-b, Yu H-l, et al. Comparison of the extent of prevertebral soft tissue swelling and incidence of dysphagia after low- and high-level anterior cervical decompression and fusion. Orthop J China 2014;22:1921–5. [Google Scholar]
- [110].Yu J, Tao X-H, Jin P-H, et al. Risk factors for dysphagia after posterior cervical surgery. Shandong Med 2016;56:40–1. [Google Scholar]
- [111].Tao X-h, Tian W, Liu B. Risk factors of dysphagia following cervical spine surgery. Shandong Med 2013;53:19–21. [Google Scholar]
- [112].Wu B, Zhu S, Wang Y. Patients with dysphagia after anterior cervical discectomy and fusion: an analysis of 36 cases. Acad J Chin PLA Med Sch 2015;36:121–3. [Google Scholar]
- [113].Chen B, Qu X, Yang Y. Risk factors for dysphagia after single-level anterior cervical fusion. Chin J Tissue Eng Res 2015;19:2028–33. [Google Scholar]
- [114].Gu Y, Yang L, Yuan W, et al. A comparison of anterior artificial disc insertion and anterior cervical discectomy and fusion in postoperative dysphagia. Chin J Spine Spinal Cord 2013;23:25–9. [Google Scholar]
- [115].Jia X, Liu S, Wang Y. Observation on the therapeutic effects of ACCF and ACDF on cervical spondylotic myelopathy and evaluation on the postoperative complications. Chongqi Med 2014;43:3201–3. [Google Scholar]
- [116].Lin W, Xue Y, Zhao Y, et al. Disc associating axial pain were indicated by PLL resection in ACDF surgery. Eur Spine J 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [117].Nassr A, Khan MH, Ali MH, et al. Donor-site complications of autogenous nonvascularized fibula strut graft harvest for anterior cervical corpectomy and fusion surgery: experience with 163 consecutive cases. Spine J 2009;9:893–8. [DOI] [PubMed] [Google Scholar]
- [118].Fujibayashi S, Neo M, Yoshida M, et al. Neck muscle strength before and after cervical laminoplasty: relation to axial symptoms. J Spinal Disord Tech 2010;23:197–202. [DOI] [PubMed] [Google Scholar]
- [119].Sakaura H, Hosono N, Mukai Y, et al. C3-6 laminoplasty for cervical spondylotic myelopathy maintains satisfactory long-term surgical outcomes. Global Spine J 2014;4:169–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Goldstein CL, Bains I, Hurlbert RJ, et al. Symptomatic spinal epidural hematoma after posterior cervical surgery: incidence and risk factors. Spine J 2015;15:1179–87. [DOI] [PubMed] [Google Scholar]
- [121].Smith-Hammond CA, New KC, Pietrobon R, et al. Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients. Spine (Phila Pa 1976) 2004;29:1441–6. [DOI] [PubMed] [Google Scholar]
- [122].Yue W-M, Brodner W, Highland TR. Longterm results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138–44. [DOI] [PubMed] [Google Scholar]


