Abstract
Background:
On a pharmacologic basis, levobupivacaine is expected to last longer than ropivacaine. However, most reports of these anesthetics for brachial plexus block do not suggest a difference in analgesic effect. The aim of this study is to compare the postoperative analgesic effects of levobupivacaine and ropivacaine when used for treating ultrasound-guided brachial plexus block.
Methods:
A total of 62 patients undergoing orthopedic surgery procedures were prospectively enrolled and randomized to receive levobupivacaine (group L, N = 31) or ropivacaine (group R, N = 31). The duration of analgesia, offset time of motor block, need for rescue analgesics, and sleep disturbance on the night of surgery were recorded. Pain score was recorded on the day of surgery, and on postoperative days 1 and 2.
Results:
There was no difference in the time interval until the first request for pain medication comparing the two groups (group L: 15.6 [11.4, 16.8] hours; group R: 12.5 [9.4, 16.0] hours, P = 0.32). There was no difference in the duration of motor block (group L: 12.2 [7.6, 14.4] hours; group R: 9.4 [7.9, 13.2] hours, P = 0.44), pain score (P = 0.92), need for rescue analgesics (group L: 55%; group R: 65%, P = 0.6), or rate of sleep disturbance (group L: 61%, group R: 58%, P = 1.0) on comparing the two groups.
Conclusions:
There was no difference in postoperative analgesia comparing levobupivacaine and ropivacaine when used for brachial plexus block.
Keywords: brachial plexus block, levobupivacaine, postoperative analgesia, ropivacaine
1. Introduction
Levobupivacaine and ropivacaine are long-acting local anesthetics used for peripheral nerve blocks to provide prolonged postoperative analgesia. Levobupivacaine has been reported to have a longer duration of analgesic effect compared with ropivacaine when used for spinal and epidural anesthesia.[1–4] Levobupivacaine is more lipophilic compared with ropivacaine.[5] On a pharmacologic basis, levobupivacaine is considered to be more potent than ropivacaine with regard to providing postoperative analgesia. However, previous reports[6–8] have not shown a longer duration of postoperative analgesia when levobupivacaine is used for brachial plexus blocks compared with ropivacaine, except for a single report.[9]
Clinically, prolonged postoperative analgesia is important for postoperative pain management. Most appropriate local anesthetics are chosen for peripheral nerve block. We undertook this randomized prospective trial to compare the postoperative analgesic effects of levobupivacaine and ropivacaine when used for brachial plexus nerve blocks, performed with ultrasound guidance in patients undergoing orthopedic surgery procedures.
2. Methods
This study was reviewed and approved by the local ethics committee (Hino Municipal Hospital Ethical Review Board; Reception. No. 25-10) and was registered in the University Hospital Medical Information Network Center Clinical Trials Registration System (UMIN000012897). Written informed consent was obtained from patients scheduled to undergo surgery for upper limb fractures from April 2014 to March 2015. Exclusion criteria included allergy to local anesthetics, coagulation disorders, local skin infection at the block site, peripheral neuropathy, American Society of Anesthesiologists physical status ≥4, and patient refusal. Patients were randomly divided in two groups using levobupivacaine (group L) or ropivacaine (group R) for peripheral nerve block.
Brachial plexus block with an interscalene approach was performed in patients undergoing open reduction and internal fixation (ORIF) of humerus fracture and ORIF of elbow fracture. Brachial plexus blocks using an axillary approach were performed for patients undergoing ORIF of wrist fracture.
A randomized, double-blind selection of the groups was performed using the envelope method. A nurse not associated with the surgery shuffled and selected a sealed envelope from a box. The nurse prepared the solution for the nerve block after double checking with another nurse.
The solution for group L was a mixture of 15 mL of 0.5% levobupivacaine (Popscaine 5 mg/mL, Maruishi Pharmaceutical, Osaka, Japan) and 5 mL of saline (final concentration of the mixture was 0.375%). The solution for group R was a mixture of a mixture of 10 mL of 0.75% ropivacaine (Anapeine 7.5 mg/mL, AstraZeneca, Osaka, Japan) and 10 mL of saline (final concentration was 0.375%).
After preparing the solution, the nurse wrote down the operating room number and patient identification number, and placed this paper into another locked box. The key for this box was kept by an ethics committee member. In accordance with the rules of the protocol, these 2 nurses never met the anesthesiologist until completion of anesthesia, in order to ensure a blinded procedure. The anesthesiologists, orthopedic surgeons, and nurses in the ward remained blinded to the patients’ group allocation until the end of the study.
General anesthesia was induced with 2 mg/kg of propofol and 100–200 mcg of fentanyl intravenously. A laryngeal mask (ProSeal, Teleflex, San Diego, CA) was used, and anesthesia maintained with 4–6% desflurane. An ultrasound-guided peripheral nerve block was performed after placement of the laryngeal mask.[10] We used a 6–13 Hz high-frequency linear probe (HFL 38x EDGE, SonoSite Co., Bothell, WA) and a 22-G needle (Stimplex Ultra, B. Braun, Melsungen, Germany). We routinely used ultrasound guidance and nerve stimulators (Rasin Plex HRP-10, Hakko Co., Japan). Brachial plexus blocks with an interscalene approach or axillary approach were performed using 20 mL of 0.375% levobupivacaine (group L) or ropivacaine (group R). All nerve blocks were performed by anesthesiologists with extensive experience in ultrasound-guided nerve blocks. During surgery, ephedrine and/or phenylephrine were administered to maintain appropriate hemodynamics. At the end of surgery, 50 mg of flurbiprofen was routinely administered intravenously. On the first postoperative day, administration of 4 mg of oral lornoxicam after each meal was started and continued until the fifth postoperative day.
Postoperative pain was scored using the verbal rating scale (scale range: 0–5; 0: no pain, 5: strongest pain) on the day of surgery, as well as on the first and second postoperative days. Motor block was assessed using the modified Lovett rating scale[11] (0: complete paralysis, 1: almost complete paralysis, 2: pronounced mobility impairment, 3: slightly impaired mobility, 4: pronounced reduction of muscular force, 5: slightly reduced muscular force, 6: normal muscular force). The duration of analgesia (time interval until the first request for pain medication), offset time of motor block, need for rescue analgesics, and sleep disturbances during the night of surgery were recorded. Nurses were educated to assess pain score and neurologic evaluation before starting the study.
After surgery, patients were allowed to request rescue analgesics at any time, which included diclofenac (25 mg p.r.) with at least a 6-hour interval before re-administration. If the diclofenac did not relieve the pain, patients received pentazocine (15 mg i.v.) at an interval of at least 30 minutes. Administration time and amount of analgesic used were recorded.
2.1. Statistical analysis
A pilot study showed a mean difference in the time interval until the first request for pain medication using levobupivacaine and ropivacaine of 4.5 hours (standard deviation 6 hours). The sample size required for 80% power at ɑ = 0.05 was estimated to be 29 patients each for the experimental and control groups based on this pilot study. We planned for a total of 40 patients in each group.
The Wilcoxon rank test was used to compare continuous variables in the patient demographic data. Bonferroni correction to the multiple-comparison correction was used for pain scores. Time interval until the first request of pain medication and motor block were analyzed with the log-rank test using Kaplan–Meier survival curves. Fisher's exact test was used for American Society of Anesthesiologists physical status, rate of rescue analgesic requirement, and incidence of sleep disturbance. Numerical values are expressed as ratios (%) or as the median (interquartile range). P values <0.05 are considered statistically significant. Statistical analyses were performed with JMP 11 statistical software (JMP Statistical Discovery, Cary, NC).
3. Results
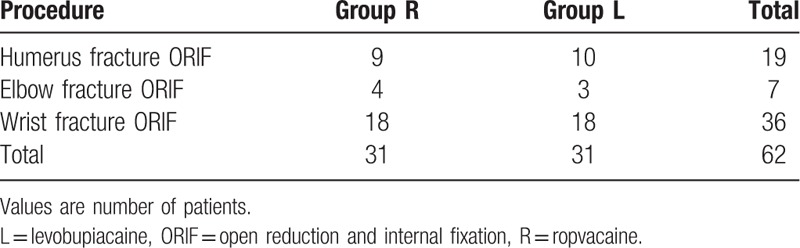
Sixty-two patients were enrolled in this study (Fig. 1). There was no difference in the demographic data comparing the two groups (Tables 1 and 2). There was no technical difficulty in performing ultrasound-guided peripheral nerve block in any patient.
Figure 1.
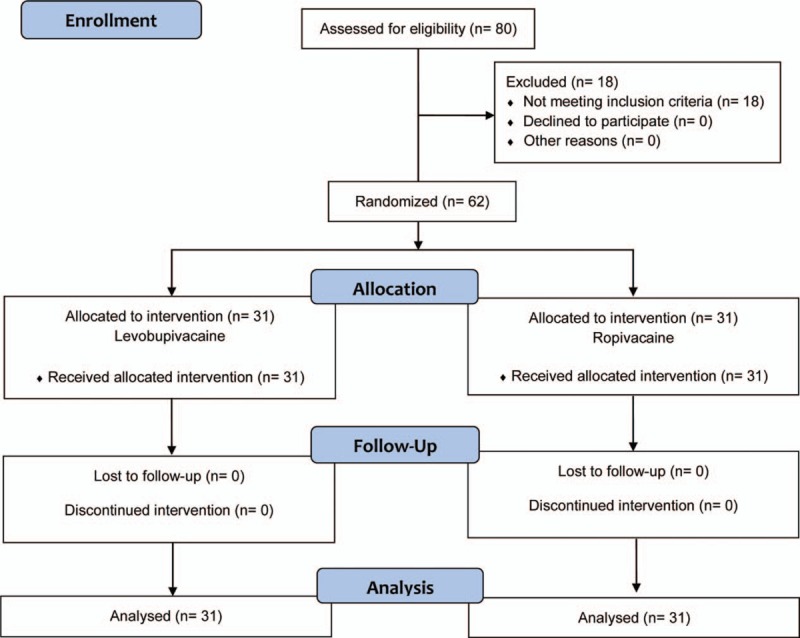
Study flow diagram.
Table 1.
Patient demographic data.
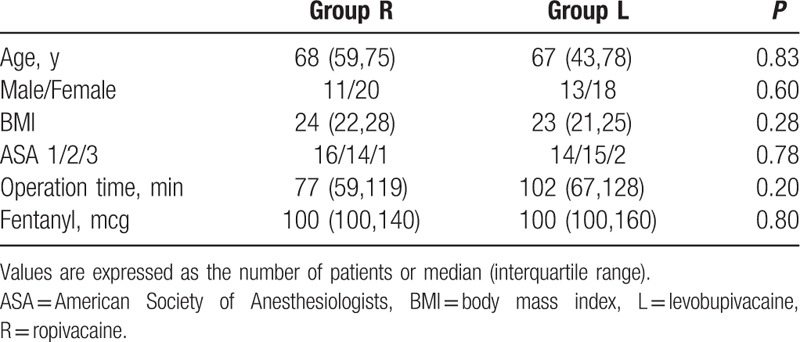
Table 2.
Surgical procedures.
There was no difference in time interval until the first request for pain medication comparing the 2 groups (group L: 15.6 [11.4, 16.8] hours; group R: 12.5 [9.4, 16.0] hours, P = 0.32) (Fig. 2). There was no difference in the duration of motor block comparing the two groups (group L: 12.2 [7.6, 14.4] hours; group R: 9.4 [7.9, 13.2] hours, P = 0.44). There were no differences in pain scores at each time point after surgery comparing the two groups (P = 0.92) (Fig. 3). There were no differences in the need for rescue analgesics comparing the two groups (group L: 55%; group R: 65%, P = 0.6). There were no differences in the rate of sleep disturbance comparing the 2 groups (group L: 61%; group R: 58%, P = 1.0).
Figure 2.
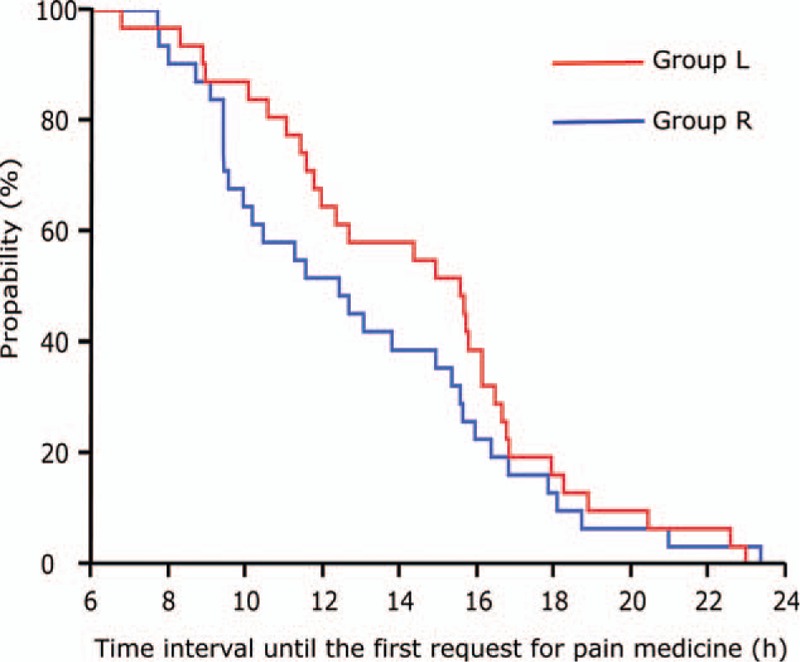
Duration of analgesia. There is no difference in the time interval until the first request for pain medication on comparing the 2 groups (P = 0.32): group R = ropivacaine, group L = levobupivacaine.
Figure 3.
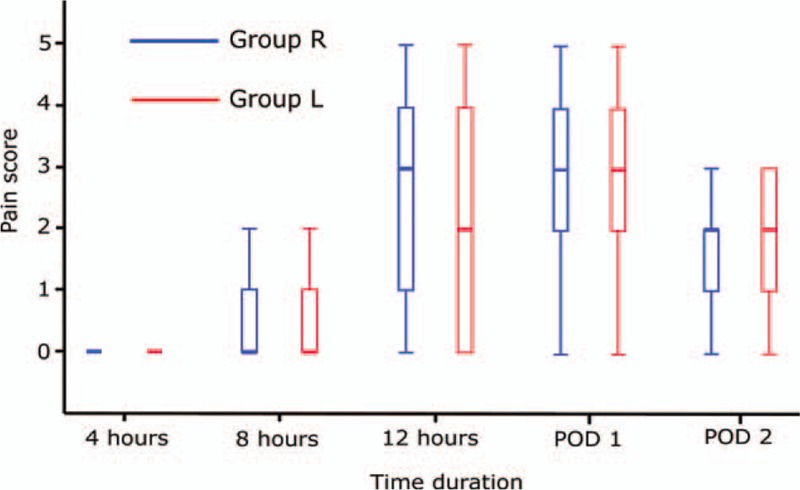
Postoperative pain scores. There is no difference in the postoperative pain scores on comparing the 2 groups (P = 0.92): group R = ropivacaine, group L = levobupivacaine. POD = postoperative day.
4. Discussion
This study shows that the postoperative analgesic effects of levobupivacaine and ropivacaine used for brachial plexus blocks are similar. Based on the pharmacology, levobupivacaine is expected to be associated with a longer duration of analgesia compared with ropivacaine.[5] Studies comparing postoperative analgesia in sciatic nerve block showed that levobupivacaine had a longer duration of postoperative analgesia compared with ropivacaine.[12–14] There are four previous studies comparing levobupivacaine and ropivacaine in the same concentrations used for brachial plexus blocks. However, 3 of the studies of brachial plexus block report no difference between these 2 agents. Liisanantti et al[6] reported that the duration of analgesia when using levobupivacaine for brachial plexus block was the same as that when using ropivicaine. Mageswaran and Choy[7] reported that patients receiving levobupivacaine and ropivicaine reported almost the same pain level at 6 hours after the operation. Casati et al[8] reported that there were no difference in postoperative pain scores comparing levobupivacaine and ropivacaine. However, Cline et al[9] showed a longer analgesic effect of levobupivacaine compared with ropivacaine.
The duration of postoperative analgesia after brachial plexous block is shorter than after sciatic nerve block. The reason for the difference in analgesic duration may be explained by pharmacodynamics. Serum levels of local anesthetics injected into the tissue rapidly increased after brachial plexus block compared with sciatic nerve block.[15,16] This suggests that local anesthetics used in brachial plexus block are rapidly absorbed. Therefore, a longer analgesic effect of levobupivacaine may be attenuated when used for brachial plexus block.
In the study we used 2 approaches to the brachial plexus block, the interscalene approach and an axillary approach. However, a previous report utilized another approach, the infraclavicular approach.[7] This may limit the ability to compare the results of this study with previous studies of brachial plexus block. We performed a subgroup analysis for the interscalene and axillary approaches, and found no statistically significant difference in all outcome measures.
This study shows that the analgesic effects of levobupivacaine and ropivacaine are not statistically significant when used for ultrasound guided brachial plexus block. This unexpected result may be explained by the pharmacodynamics of local anesthetics used for bracahal plexus blocks.
Acknowledgments
The authors thank contribution for the study to Dr. Shohei Siono (Hino Municipal Hospital), Dr. Kenji Nanao (Hino Municipal Hospital), and Toshiko Maeda (Hino Municipal Hospital).
Footnotes
Abbreviation: ORIF = open reduction and internal fixation.
This study was presented as an abstract at the Japanese Society of Regional Anesthesia 3rd Annual Congress 2015, Hirosaki, Japan.
The authors have no conflicts of interest to disclose.
References
- [1].Sia AT, Goy RW, Lim Y, et al. A comparison of median effective doses of intrathecal levobupivacaine and ropivacaine for labor analgesia. Anesthesiology 2005;102:651–6. [DOI] [PubMed] [Google Scholar]
- [2].Kopacz DJ, Allen HW, Thompson GE. A comparison of epidural levobupivacaine 0.75% with racemic bupivacaine for lower abdominal surgery. Anesth Analg 2000;90:642–8. [DOI] [PubMed] [Google Scholar]
- [3].Egashira T, Fukasaki M, Araki H, et al. Comparative efficacy of levobupivacaine and ropivacaine for epidural block in outpatients with degenerative spinal disease. Pain Physician 2014;17:525–9. [PubMed] [Google Scholar]
- [4].Perotti L, Cusato M, Ingelmo P, et al. A comparison of differences between the systemic pharmacokinetics of levobupivacaine and ropivacaine during continuous epidural infusion: a prospective, randomized, multicenter, double-blind controlled trial. Anesth Analg 2015;121:348–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Leone S, Di Cianni S, Casati A, et al. Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed 2008;79:92–105. [PubMed] [Google Scholar]
- [6].Liisanantti O, Luukkonen J, Rosenberg PH. High-dose bupivacaine, levobupivacaine and ropivacaine in axillary brachial plexus block. Acta Anaesthesiol Scand 2004;48:601–6. [DOI] [PubMed] [Google Scholar]
- [7].Mageswaran R, Choy YC. Comparison of 0.5% ropivacaine and 0.5% levobupivacaine for infraclavicular brachial plexus block. Med J Malaysia 2010;65:300–3. [PubMed] [Google Scholar]
- [8].Casati A, Borghi B, Fanelli G, et al. Interscalene brachial plexus anesthesia and analgesia for open shoulder surgery: a randomized, double-blinded comparison between levobupivacaine and ropivacaine. Anesth Analg 2003;96:253–9. [DOI] [PubMed] [Google Scholar]
- [9].Cline E, Franz D, Polley RD, et al. Analgesia and effectiveness of levobupivacaine compared with ropivacaine in patients undergoing an axillary brachial plexus block. AANA J 2004;72:339–45. [PubMed] [Google Scholar]
- [10].Misamore G, Webb B, McMurray S, et al. A prospective analysis of interscalene brachial plexus blocks performed under general anesthesia. J Shoulder Elbow Surg 2011;20:308–14. [DOI] [PubMed] [Google Scholar]
- [11].Biradar PA, Kaimar P, Gopalakrishna K. Effect of dexamethasone added to lidocaine in supraclavicular brachial plexus block: A prospective, randomised, double-blind study. Indian J Anaesth 2013;57:180–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Casati A, Vinciguerra F, Santorsola R, et al. Sciatic nerve block with 0.5% levobupivacaine, 0.75% levobupivacaine or 0. 75% ropivacaine: a double-blind, randomized comparison. Eur J Anaesthesiol 2005;22:452–6. [DOI] [PubMed] [Google Scholar]
- [13].Fournier R, Faust A, Chassot O, et al. Levobupivacaine 0.5% provides longer analgesia after sciatic nerve block using the Labat approach than the same dose of ropivacaine in foot and ankle surgery. Anesth Analg 2010;110:1486–9. [DOI] [PubMed] [Google Scholar]
- [14].Pham Dang C, Langlois C, Lambert C, et al. 0.5% levobupivacaine versus 0.5% ropivacaine: are they different in ultrasound-guided sciatic block? Saudi J Anaesth 2015;9:3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Schoenmakers KP, Vree TB, Jack NT, et al. Pharmacokinetics of 450 mg ropivacaine with and without epinephrine for combined femoral and sciatic nerve block in lower extremity surgery. A pilot study. Br J Clin Pharmacol 2013;75:1321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Rettig HC, Lerou JG, Gielen MJ, et al. The pharmacokinetics of ropivacaine after four different techniques of brachial plexus blockade. Anaesthesia 2007;62:1008–14. [DOI] [PubMed] [Google Scholar]


