Abstract
Rationale:
Anatomical characteristics, such as subcutaneous position and minimal muscle cover, contribute to the complexity of fractures of the distal third of the tibia and fibula. Severe damage to soft tissue and instability ensure high risk of delayed bone union and wound complications such as nonunion, infection, and necrosis.
Patient concerns:
This case report discusses management in a 54-year-old woman who sustained fractures of the distal third of the left tibia and fibula, with damage to overlying soft tissue (swelling and blisters). Plating is accepted as the first choice for this type of fracture as it ensures accurate reduction and rigid fixation, but it increases the risk of complications.
Diagnosis:
Closed fracture of the distal third of the left tibia and fibula (AO: 43-A3).
Interventions:
After the swelling was alleviated, the patient underwent closed reduction and fixation with an Acumed fibular nail and minimally invasive plating osteosynthesis (MIPO), ensuring a smaller incision and minimal soft-tissue dissection.
Outcomes:
At the 1-year follow-up, the patient had recovered well and had regained satisfactory function in the treated limb. The Kofoed score of the left ankle was 95.
Lessons:
Based on the experience from this case, the operation can be undertaken safely when the swelling has been alleviated. The minimal invasive technique represents the best approach. Considering the merits and good outcome in this case, we recommend the Acumed fibular nail and MIPO technique for treatment of distal tibial and fibular fractures.
Keywords: Acumed fibular nail, distal tibial and fibular fractures, minimally invasive plating osteosynthesis (MIPO)
1. Introduction
Anatomical characteristics, such as subcutaneous position and minimal muscle cover, contribute to the complexity of fractures of the distal third of the tibia and fibula. Severe damage to soft tissue and extreme instability ensure high risk of delayed bone union and wound complications such as dehiscence and infection.[1,2] Plating is accepted as the first choice of stabilization for this type of fracture and ensures accurate reduction and rigid fixation,[3] but increases the risk of complications due to the dissection of bone and soft tissue required in this technique. Recently, a novel technique—minimally invasive plating osteosynthesis (MIPO)—has been developed to alleviate soft tissue damage associated with plating.[4] Fibular fixation plays a positive role in reducing tibial displacement and improving mechanical stability of the entire lesion,[5] but the technique of plating the lateral malleolus has an associated with a complication rate of up to 30%.[6] Therefore, the fibular nail, which requires a smaller incision and minimal soft-tissue dissection, poses an alternative technique for fixation of the lateral malleolus.
We report a case with fractures of the distal third of the left tibia and fibula with associated severe damage to soft tissue. The fractures were successfully reduced and fixed with the Acumed fibular nail (Acumed LLC, Hillsboro, Oregon) using the MIPO technique, with satisfactory outcomes.
2. Case presentation
A 54-year-old woman sustained a fall and was admitted to our hospital 3 hours later with complaints of pain in the distal part of the left leg and limited mobility. On physical examination, the left distal leg showed severe swelling with several large blisters overlying the region; the distal pulses were palpable. The examination of the neurovascular system revealed no abnormalities of the lower extremities, and there was no compartment syndrome. She had no notable comorbidities. Radiography revealed fractures of the distal third of the left tibia and fibula, but the ankle articular surfaces were intact (Fig. 1A and B). Therefore diagnosis of a closed fracture of the distal third of the left tibia and fibula (AO: 43-A3) was made. Initially, strategies for detumescence and symptomatic treatment were administered. The left foot was elevated using a pillow, and oral detumescent drugs were used. A brace was used for temporary fracture fixation. Two weeks later, the swelling had alleviated and the blisters appeared wizened (Fig. 1C and D), and operative stabilization was conducted for early functional rehabilitation. The result of preoperative blood routine examination was normal.
Figure 1.
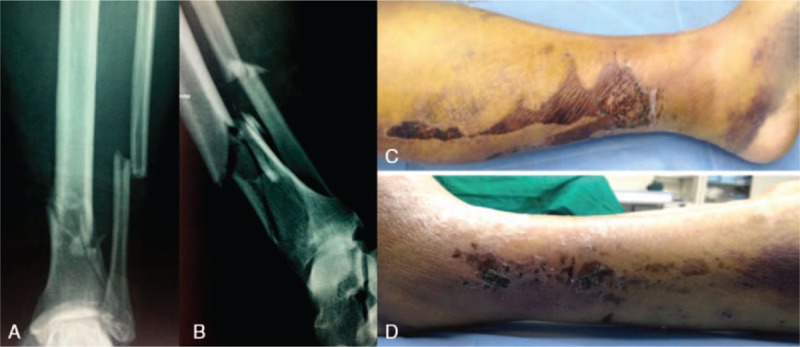
Preoperative plain radiographs and photographs. (A and B) Anteroposterior and lateral views showing fractures of the distal third of the tibia and fibula. (C and D) Photographs of medial and lateral appearance of soft-tissue injury showing the wizened blisters.
2.1. Surgical technique
Under general anesthesia, with tourniquet application, and in the supine position on a radiolucent table the patient underwent fracture reduction. In the distal tibia, a medial distal tibia locking compression plate (LCP, size: 10 holes, DePuy Synthes, Oberdorf, Switzerland) of adequate length was applied over the medial surface and we performed closed indirect reduction using fluoroscopic guidance. The reduced fracture of the tibia was fixed temporarily by K-wires. Thereafter, a 4-cm vertical incision was made at the center of the medial malleolus and a subcutaneous tunnel was opened with a periosteal dissector. The selected plate was tunneled proximally and subcutaneously across the fracture site and positioned anteriorly over the tibial crest. Thereafter, 3.5-mm locking screws were inserted after ensuring satisfactory reduction by orientation using a similar-sized LCP. Then, the fibular fracture was fixed after closed reduction; a 1 cm incision was made just below the lateral end of the distal fibula. The distal fibular metaphysis was prepared with a cannulated 6.1 mm drill over a 1.6 mm guide wire. The diaphysis was then reamed by hand using a 3.1 mm reamer and the Acumed fibular nail (diameter: 3 mm, length: 180 mm) was inserted in a retrograde manner. Two 5 mm incisions were made at the ankle laterally and the nail was locked using two 2.7 mm screws through the eyelet of the nail in the lateral malleolus. The tourniquet was removed and all incisions were sutured after ensuring hemostasis. Intraoperative radiographs showed correct reduction of the fractures (Fig. 2A–D).
Figure 2.

Intraoperative radiographs and clinical postoperative pictures. (A–D) Anteroposterior and lateral intraoperative views showing correct reduction of fractures. (E and F) At 1 week after surgery, clinical pictures reveal the incisions are healing well.
Intravenous antibiotic prophylaxis was initiated routinely 30 minutes before surgery and was then continued for another 24 hours postoperatively. We followed standard institutional protocols of postoperative routine dressing change, infection prevention measures, and symptomatic therapy. Results of blood routine examination at postoperative day 3 were normal. The patient was instructed to undergo physiotherapy with muscle strengthening and joint function exercises. One week after surgery, the incisions were healing well (Fig. 2E and F). Two weeks postoperatively the patient was discharged. Partial weight-bearing was commenced at 6 weeks postoperatively and full weight-bearing was permitted 3 months after the surgery. Radiographs taken postoperatively revealed correct fracture reduction (Fig. 3A and B). At the 1-year follow-up, there were no localized tenderness, axial knocking pain, or abnormal movement; radiography revealed good fracture healing with abundant callus across the fracture site and obliteration of the fracture line (Fig. 3C and D) and the patient had attained satisfactory restoration of function in the injured leg. The patient could walk freely. The Kofoed score of the left ankle was 95.
Figure 3.

Postoperative radiographs. (A and B) Anteroposterior and lateral views showing correct reduction of fractures. (C and D) At 1 year after surgery, radiographs revealed that the fracture healed well with abundant callus formation.
3. Discussion
Distal tibial fractures remain among the most substantial therapeutic challenges that confront the orthopedic traumatologist. Although conservative management of these fractures has been described,[7,8] unstable distal tibial and fibular fractures are most often treated by open reduction and internal fixation (ORIF) techniques that have not changed significantly for many years and are associated with a high rate of complications including infection, soft-tissue necrosis, and nonunion because of the poor blood supply and a thin layer of soft-tissue cover, especially in patients with osteoporosis. The incidence of complications following ORIF in the elderly is up to 40%,[9] and is much higher in patients with systemic disease, particularly diabetes and neuropathy,[10] and in smokers.[11]
The MIPO technique is established for managing fractures of the distal third of the tibia that has a reliable fixation approach while preserving the osseous vascularity and hematoma, thus facilitating better biological repair. The technique can be used for the fractures with vertical split where nailing is not suitable. Due to the preserved vascularity and limited exposure, there is a lower incidence of delayed union, nonunion, or infection.[1]
For the distal fibular fracture, minimally invasive plating techniques, which are carried out through smaller wounds (3–4 cm), are more technically challenging.[12] The fibular nail may be an alternative method of fixing the distal fibular fracture as it requires a smaller incision (1 cm[13] vs 8 cm[14] for lateral plating) and less extensive soft-tissue dissection. Successful outcomes have been reported with different nails. Bugler et al[15] reported good 8-year follow-up results in 105 patients treated with the Acumed fibular nail. Both the MIPO technique and fibular nail have the same minimally invasive advantage and, therefore, are suitable for fractures with poor soft-tissue conditions.
Numerous treatment options are available for distal fractures of the tibia and fibula—plating for both the bones, nailing for tibial fracture combined with plating for fibular fractures, nailing for both the bones, plating for the tibial fracture combined with nailing for fibular fractures. The most appropriate treatment option is selected based on fracture type, soft-tissue condition, and stability of the fracture. In the reported case with the poor condition of the overlying soft tissue (blisters) we choose the least invasive technique (Acumed fibular nail) for the stabilization of the fibular fracture. Due to the lower fracture line of the tibia, we selected the MIPO technique with LCP for stabilization. At present, the patient has recovered very well with restoration of good function in the injured leg without any complication. Based on the experience from this case, the operation can be undertaken safely after the swelling is alleviated. Considering the good outcome in this case, we recommend use of the Acumed fibular nail and MIPO technique for treatment of distal tibial and fibular fractures.
Footnotes
Abbreviations: LCP = locking compression plate, MIPO = minimally invasive plating osteosynthesis.
T-JW and W-NJ contributed equally to this work.
Funding: This work was supported by the Academy & Research Foundation for Young Scientists (grant no. MJR20160015), the National Natural Science Foundation of China (grant no. 81500911), and AOTrauma Asia Pacific (Ref: AOTAP15-01).
Consent: The Institutional Review Board of Jilin University approved the publication of this case report. Informed consent was obtained from the patient.
The authors have no conflicts of interest to disclose.
References
- [1].Paluvadi SV, Lal H, Mittal D, et al. Management of fractures of the distal third tibia by minimally invasive plate osteosynthesis—a prospective series of 50 patients. J Clin Orthop Trauma 2014;5:129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Xue XH, Yan SG, Cai XZ, et al. Intramedullary nailing versus plating for extra-articular distal tibial metaphyseal fracture: a systematic review and meta-analysis. Injury 2014;45:667–76. [DOI] [PubMed] [Google Scholar]
- [3].Zelle BA, Bhandari M, Espiritu M, et al. Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma 2006;20:76–9. [DOI] [PubMed] [Google Scholar]
- [4].Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg 2006;14:406–16. [DOI] [PubMed] [Google Scholar]
- [5].Bonnevialle P, Lafosse JM, Pidhorz L, et al. Distal leg fractures: how critical is the fibular fracture and its fixation? Orthop Traumatol Surg Res 2010;96:667–73. [DOI] [PubMed] [Google Scholar]
- [6].Lamontagne J, Blachut PA, Broekhuyse HM, et al. Surgical treatment of a displaced lateral malleolus fracture: the antiglide technique versus lateral plate fixation. J Orthop Trauma 2002;16:498–502. [DOI] [PubMed] [Google Scholar]
- [7].Digby JM, Holloway GM, Webb JK. A study of function after tibial cast bracing. Injury 1983;14:432–9. [DOI] [PubMed] [Google Scholar]
- [8].Sarmiento A, Latta LL. 450 closed fractures of the distal third of the tibia treated with a functional brace. Clin Orthop Relat Res 2004;261–71. [DOI] [PubMed] [Google Scholar]
- [9].Anderson SA, Li X, Franklin P, et al. Ankle fractures in the elderly: initial and long-term outcomes. Foot Ankle Int 2008;29:1184–8. [DOI] [PubMed] [Google Scholar]
- [10].Wukich DK, Joseph A, Ryan M, et al. Outcomes of ankle fractures in patients with uncomplicated versus complicated diabetes. Foot Ankle Int 2011;32:120–30. [DOI] [PubMed] [Google Scholar]
- [11].Nasell H, Ottosson C, Tornqvist H, et al. The impact of smoking on complications after operatively treated ankle fractures—a follow-up study of 906 patients. J Orthop Trauma 2011;25:748–55. [DOI] [PubMed] [Google Scholar]
- [12].Hess F, Sommer C. Minimally invasive plate osteosynthesis of the distal fibula with the locking compression plate: first experience of 20 cases. J Orthop Trauma 2011;25:110–5. [DOI] [PubMed] [Google Scholar]
- [13].Appleton P, McQueen M, Court-Brown C. The fibula nail for treatment of ankle fractures in elderly and high risk patients. Tech Foot Ankle 2006;5:204–8. [Google Scholar]
- [14].Lee YS, Huang HL, Lo TY, et al. Lateral fixation of AO type-B2 ankle fractures in the elderly: the Knowles pin versus the plate. Int Orthop 2007;31:817–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bugler KE, Watson CD, Hardie AR, et al. The treatment of unstable fractures of the ankle using the Acumed fibular nail: development of a technique. J Bone Joint Surg Br 2012;94:1107–12. [DOI] [PubMed] [Google Scholar]


