Abstract
Background
Shift work is associated with health problems, including metabolic syndrome. This study investigated the association between shift work and metabolic syndrome in young workers.
Methods
A total of 3,317 subjects aged 20–40 years enrolled in the 2011–2012 Korean National Health and Nutrition Examination Survey were divided into shift and day workers. We conducted a cross-sectional study and calculated odds ratios using multivariate logistic regression analysis in order to examine the association between shift work and metabolic syndrome.
Results
The prevalence of metabolic syndrome was 14.3% and 7.1% among male and female shift workers, respectively. After adjusting for confounding factors, shift work was associated with metabolic syndrome in female workers (odds ratio, 2.53; 95% confidence interval, 1.12 to 5.70).
Conclusion
Shift work was associated with metabolic syndrome in young women. Timely efforts are necessary to manage metabolic syndrome in the workplace.
Keywords: Metabolic Syndrome, Female, Prevalence, Occupations, Workplace
INTRODUCTION
Shift work is a common form of work worldwide; it is utilized in various areas of business and is a characteristic of modern society. Shift work is defined as a job schedule in which working hours are outside of the standard daytime hours.1) In Korea, the number of shift workers is steadily growing,2) and a recent survey reported that approximately 10.9% of employees are shift workers.3)
The prevalence of metabolic syndrome in the modern world is high and increasing continuously. Alterations in socio-environmental factors have contributed to this trend.4) Metabolic syndrome refers to a group of metabolic conditions, including increased blood pressure, high blood glucose level, abdominal obesity, high triglyceride level, and low high-density lipoprotein cholesterol levels5) that, combined, increase the risk of type 2 diabetes, heart diseases, and stroke.6,7) In Korea, the prevalence of metabolic syndrome in adults over 30 years of age is 32.9% and 31.8% in men and women, respectively.8)
Shift work has been identified as a cause of many health problems due to disruption of circadian rhythm.9,10) Prolonged interruption of the circadian rhythm may lead to an array of disorders, including insomnia, impaired glucose tolerance, obesity, and high blood pressure, which are important determinants of cardiovascular disease.11,12) Because the majority of employees spend most of their time in the workplace, we believe that employers should develop prevention strategies and early interventions for metabolic syndrome in workplace settings.
Several studies have reported the association between shift work and risk of metabolic syndrome. A systematic review and meta-analysis13) of 10 original articles revealed that the association between metabolic syndrome and shift work varied among studies, and these studies showed discordant results. Consequently, the authors concluded that there was insufficient evidence on the relationship between shift work and the prevalence of metabolic syndrome. Moreover, few studies have evaluated the association between shift work and metabolic syndrome in younger adults, especially by using data from the Korean National Health and Nutrition Survey. Therefore, the current study examined the association between shift work and metabolic syndrome using a representative large-scale national database of workers.
METHODS
1. Data Source and Study Subjects
This study was based on data obtained from the fifth Korean National Health and Nutrition Survey (KNHANES) conducted in 2011 and 2012 by the Korean Ministry of Health and Welfare. The survey used a rolling sample design with stratified multistage cluster probability sampling of the South Korean population. The KNHANES was composed of three component surveys: a health interview survey, a health examination survey, and a nutritional survey. In 2011, the survey sample consisted of 3,840 households and 10,589 individuals (response rate 80.4%). In 2012, the survey sample consisted of 3,840 households and 10,069 individuals (response rate 80.0%). Individuals who had fasted for less than 8 hours and for whom hemoglobin A1c values were not available were excluded from the analysis. The present study included 3,317 individuals 20–40 years of age. The KNHANES was approved by the institutional review of board of the Korea Centers for Disease Control and Prevention. The approval code for 2011 was 2011-05CON-04-C and 2012 was 2012-07CON-01-2C. All study subjects provided written informed consent.
2. Assessment of Shift Work
Data concerning participants' work schedules were obtained from responses to the interview question, “Do you usually work during the day (between 6 am and 6 pm), or do you work at a different time?” There were eight possible answers: mainly daytime work, evening shift, night shift, regular day and night shift, 24-hour rotating shift, split shift, irregular shift, or other. Day workers were defined as subjects working mainly in the daytime, evening shift workers as subjects working between 2 pm to midnight, night shift workers as subjects working between 9 pm and 8 am the next day, and shift workers were defined as those subjects working in different time periods such as regular day and night rotating shifts, 24-hour rotating shifts, split shifts (working two shifts in one day), and irregular rotating shifts.
3. Assessment of Metabolic Syndrome
The metabolic syndrome prevention and treatment for Korean adults proposed by the Korean Academy of Family Medicine defined metabolic syndrome as the presence of at least three of the following criteria:14) (1) increased waist circumference (≥90 cm for men, ≥85 cm for women), (2) elevated triglyceride levels (≥150 mg/dL), (3) low high-density lipoprotein cholesterol levels (<40 mg/dL in men, <50 mg/dL in women), (4) elevated blood pressure (systolic ≥130 mm Hg and/or diastolic ≥85 mm Hg), and (5) impaired fasting glucose levels (≥100 mg/dL).
4. Assessment of Covariates
The baseline physical examinations and laboratory findings included measurement of weight, waist circumference, blood pressure, blood lipid profile (total cholesterol, triglyceride, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol), and fasting glucose level after an eight-hour fast. Waist circumference was measured at the narrowest point of the torso between the base of the rib cage and the top of the iliac crest. Systolic and diastolic blood pressure were measured from the right arm in triplicate with the participant in a seated position following at least five minutes of rest, using a mercury sphygmomanometer (Baumanometer; WA Baum Co., Copague, NY, USA). The second and the third blood pressure measurements were averaged for a final blood pressure measurement used for analysis. Blood samples collected from the antecubital veins following an eight-hour fast were immediately processed, refrigerated, and transported in cold storage units to the central laboratory (NeoDIN Medical Institute, Seoul, Korea) and analyzed within 24-hour after transportation. In addition, serum levels of glucose, total cholesterol, high-density lipoprotein cholesterol, and triglycerides were measured using an automated enzyme technique (Hitachi Automatic Analyzer 7600; Hitachi, Tokyo, Japan).
Components of health-related behavior were recorded through self-reported questionnaires including questions on smoking status, alcohol consumption, exercise, water intake, and average number of hours of sleep. Smoking status was divided into three categories: current smokers, ex-smokers, and never smokers. Heavy drinking was defined as drinking more than seven drinks for men and five drinks for women two or more times per week. Regular and adequate exercise was defined as at least 30 minutes of moderate-intensity physical activity at least three days per week or at least 20 minutes of vigorous-intensity physical activity at least three days per week. An average of six to eight hours of sleep was defined as optimal for health. Data regarding daily water consumption were obtained in the health interview survey. Body mass index was divided into four categories, with under 18.5 kg/m2 defined as underweight, 18.5 to 22.9 kg/m2 as normal, 23.0 to 24.9 kg/m2 as overweight, and 25.0 kg/m2 and above as obese. Additionally, data regarding menstrual cycle regularity (regular or irregular) and degree of menstrual irregularity (once in three months or missed three or more months in a row more than one time) were obtained among female subjects.
5. Statistical Analysis
The data were analyzed by complex-samples analysis. Survey sample weights15) was used and the complex survey design was accounted for in the estimation of variance. The survey sample weights were calculated by taking the reciprocal of the probabilities of selection (the primary sample units, household), adjusting for non-response (household, person), and a post-stratification factor to make the resulting survey estimates for age, sex, metropolitan area, or province category approximately equal to the total population of Korea in order to calculate unbiased cross-sectional national estimates for the general Korean population. To analyze samples in multiple years, sampling weights were averaged over the sampled years. Generalized linear regression analyses and χ2 tests were used to compare continuous and categorical variables, respectively, between the two groups. Continuous variables were expressed as means±standard error, and categorical variables were expressed as frequencies and percentages. In order to evaluate independent associations between shift work and metabolic syndrome, we used multivariate logistic regression analyses. Model 1 adjusted for age; model 2 adjusted for age, education level and family income; and model 3 adjusted for age, education level, family income, smoking status, alcohol consumption, exercise, average sleep duration, and average daily water intake. In women, menstrual cycle regularity was also adjusted for along with the other variables in model 3. The results were expressed as odds ratios (ORs) and 95% confidence intervals (95% CIs). Data analysis was performed using PASW SPSS Statistics for Windows ver. 18.0 (SPSS Inc., Chicago, IL, USA). Statistically significant differences were assumed for two-tailed P-values less than 0.05.
RESULTS
1. General Characteristics of the Study Population
Table 1 shows the subjects' baseline anthropometric measurements and the distribution of factors possibly related to metabolic syndrome. In both male and female subjects, shift workers were significantly younger than day workers (both P<0.001). There were no statistically significant differences in weight or waist circumference between day workers and shift workers in either sex.
Table 1. Characteristics of the study population.
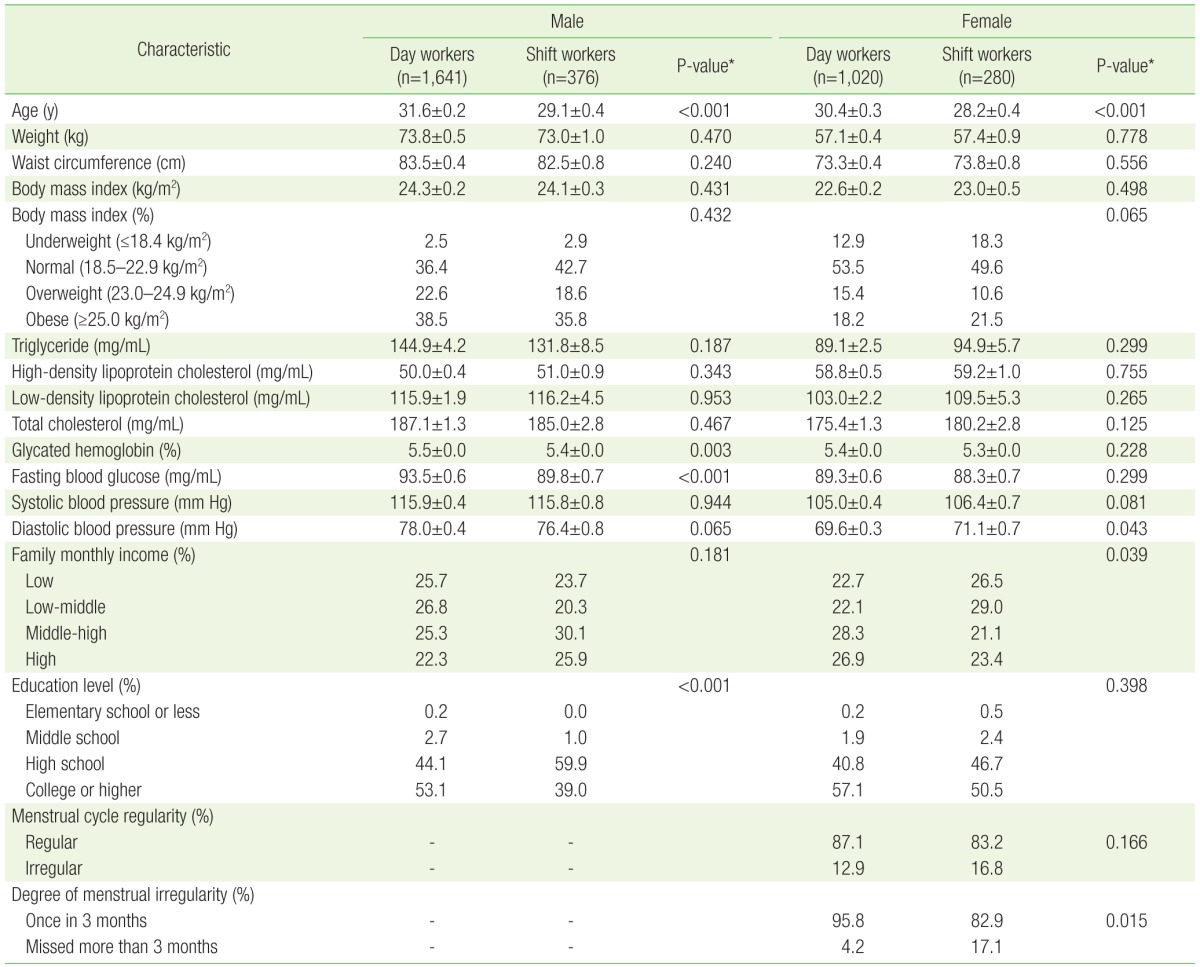
Values are presented as mean±standard error or frequency (%).
*Calculated using generalized linear regression analysis via complex sampling or χ2 test via complex sampling.
There were also no statistically significant differences in total cholesterol, triglyceride, and fasting glucose levels in either sex. In female subjects, however, diastolic blood pressures were significantly higher in shift workers than those in day workers (P=0.04). The prevalence of menstrual cycle irregularity was also higher in female shift workers (16.8%) than in day workers (12.9%), and compared with day workers, shift workers had a significantly higher prevalence of a missed menstrual cycles over the previous three months (4.2% and 17.1%, respectively; P=0.015).
2. Health-Related Behaviors of the Study Population
Table 2 shows health-related behaviors among subjects. There were no statistically significant differences in rates of current cigarette smoking and heavy drinking, average sleep duration, and average water intake between day workers and shift workers in either sex. The proportions of female subjects who performed adequate exercise were higher among shift workers than that of day workers.
Table 2. Distribution of health-related behaviors in the study population.
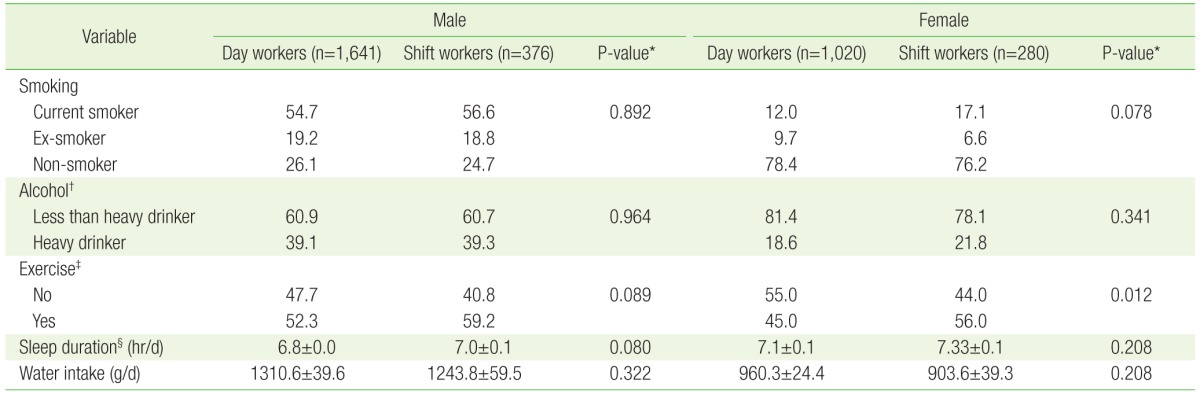
Values are presented as frequency % or mean±standard error.
*Calculated using generalized linear regression analysis via complex sampling or χ2 test via complex sampling. †Heavy drinking was defined as drinking more than 7 drinks for men and 5 drinks for women two or more times per week. ‡Exercise was defined as at least 30 minutes of moderate-intensity physical activity at least 3 days per week or at least 20 minutes of vigorous-intensity physical activity at least 3 days per week. §Six to eight hours of sleep was defined as optimal for health.
3. Association Between Shift Work and Metabolic Syndrome
Table 3 shows the ORs of metabolic syndrome according to type of work. Unadjusted, there were no statistically significant relationships between shift work and metabolic syndrome in either sex. After adjusting for age (model 1), the ORs for metabolic syndrome in female and male shift workers were 2.34 (95% CI, 1.11 to 4.94) and 1.06 (95% CI, 0.07 to 1.67), respectively. After adjusting for age, education level, and family income (model 2), the ORs in female and male shift workers were 2.25 (95% CI, 1.05 to 4.79) and 1.07 (95% CI, 0.07 to 1.70), respectively. After adjusting for age, education level, family income, education level, family income, smoking status, alcohol consumption, exercise, average sleep duration, and average water intake (model 3), the OR for metabolic syndrome in male shift workers was 0.93 (95% CI, 0.51 to 1.58). In female subjects, model 3 plus additional adjustment for menstrual cycle regularity resulted in an OR for metabolic syndrome of 2.53 (95% CI, 1.12 to 5.70). The association became statistically significant after adjusting for age, education level, family income, health-related behaviors, and menstrual cycle regularity. However, in male subjects, no significant association between shift work and metabolic syndrome was observed, even after adjustment.
Table 3. Odds ratios of metabolic syndrome according to type of work.
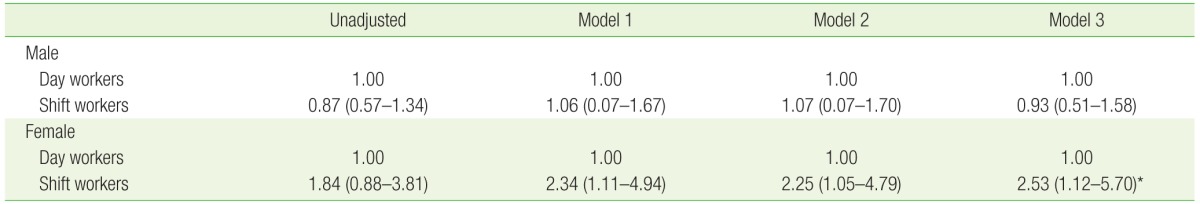
Values are presented as odds ratio (95% confidence interval). Odds ratios were calculated using multivariate logistic regression analyses via complex sampling. Model 1: adjusted for age; model 2: adjusted for age, education level, and family income; model 3: adjusted for age, education level, family income, smoking status, alcohol consumption, exercise, average sleep duration, and average water intake.
*Model 3 plus additional adjustment for menstrual cycle regularity in females.
DISCUSSION
This cross-sectional study was designed to determine the association between shift work and metabolic syndrome in young adults using data from the 2011–2012 KNHANES. Although previous studies16,17) have examined the association between shift work and metabolic syndrome, they included small sample sizes or broad age ranges, and thus did not adequately evaluate the association between shift work and metabolic syndrome at young ages.
To our knowledge, the present study is the first to evaluate the relationship between shift work and metabolic syndrome in young workers. Several prospective studies have indicated that shift work may be an independent risk factor for metabolic syndrome. One such study found that rotating shift work increases the risk for developing metabolic syndrome over a period of six years.18) Another study of male and female nurses reported that the risk of developing metabolic syndrome was strongly associated with night-shift work over a four-year follow-up.19)
One possible explanation for the connection between shift work and metabolic syndrome is disruption of normal circadian rhythms.20) Circadian rhythms control several biological processes, including hormone secretion, body temperature, feeding, sleep-wake cycles, and metabolic homeostasis.21) Shift work promotes chronic misalignment between endogenous circadian oscillation and behavior cycles. This persistent circadian misalignment causes metabolic and cardiovascular events, including increased glucose and insulin levels, as well as increased mean arterial blood pressure and reduced sleep efficiency.22) Another possible explanation for this study finding could be socioeconomic status related to shift workers such as education level or family monthly income. In the present study, among male subjects with middle school or less education levels, the prevalence of metabolic syndrome was higher among shift workers compared with day workers; similarly, among female subjects with low-middle or lower family monthly income, the prevalence was higher among shift workers compared with day workers. Socioeconomic status has been reported to be associated with metabolic syndrome.23,24) Education and family income may influence access and use of health services, and may affect health-related behaviors. In shift workers, lower levels of education or income may act as a significant barrier to access to health care and health publicity.
In the present study, shift work was associated with metabolic syndrome in female workers but not in male workers. In female workers, a high prevalence of menstrual irregularity was reported among shift workers and prevalence rates of obesity in shift workers was approximately 5% higher than that in day workers, although shift workers exercised regularly and received adequate sleep. One prospective study reported that menstrual cycle irregularity might be a risk factor for metabolic abnormalities that predispose individuals to the development of cardiovascular disease.25) Another cross-sectional survey reported that night shift work was associated with the development of obesity among night shift-working females.26) A possible explanation for this relationship is that many women with menstrual irregularities have polycystic ovary syndrome (PCOS), which has been associated with metabolic abnormalities that increase the risk of cardiovascular disease.27) Because the KNHANES data do not include manifestations of clinical and biochemical androgen excess, we cannot determine whether menstrual cycle irregularities were caused by PCOS in the present study. However, PCOS is the most common female endocrine hormonal disorder and a frequent cause of irregular menstrual cycles among young women.28) Many women with PCOS have features of metabolic syndrome such as central obesity,29) dyslipidemia,30) high blood glucose level,31) and high blood pressure.29) Therefore, menstrual cycle irregularity related to hormonal imbalances such as PCOS may be attributable to higher prevalence rates of obesity and metabolic syndrome in female shift workers. However, further prospective studies are required in order to investigate these associations.
This study has several strengths, including its large sample size and nationally representative sample of young working adults. However, it also has some limitations. First, because of its cross-sectional design, we were not able to establish a causal relationship between shift work and metabolic syndrome. Second, we did not collect information about eating habits and dietary patterns among the subjects and therefore could not assess their relationships with metabolic syndrome. Third, we did not perform a detailed analysis of occupational qualitative data, such as the duration of shift work, intensity of work, and job categories. The KNHANES does not include occupational qualitative data; therefore, we could not assess the effect of occupational qualitative variables that could be additional risk factors of metabolic syndrome. Further high-quality, prospective longitudinal studies are necessary to overcome these limitations.
ACKNOWLEDGMENTS
The findings and conclusions in this document are those of the authors and do not necessarily represent the views of the Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency. This work was supported by a 2016 clinical research grant from Pusan National University Hospital.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Hedstrom AK, Akerstedt T, Olsson T, Alfredsson L. Shift work influences multiple sclerosis risk. Mult Scler. 2015;21:1195–1199. doi: 10.1177/1352458514563592. [DOI] [PubMed] [Google Scholar]
- 2.Kim C, Cho Y. Working conditions and leisure-time physical activity among waged workers in South Korea: a cross-sectional study. J Occup Health. 2015;57:259–267. doi: 10.1539/joh.14-0028-OA. [DOI] [PubMed] [Google Scholar]
- 3.Jeong H, Hong S, Heo Y, Chun H, Kim D, Park J, et al. Vitamin D status and associated occupational factors in Korean wage workers: data from the 5th Korea national health and nutrition examination survey (KNHANES 2010-2012) Ann Occup Environ Med. 2014;26:28. doi: 10.1186/s40557-014-0028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim S, Shin H, Song JH, Kwak SH, Kang SM, Yoon JW, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011;34:1323–1328. doi: 10.2337/dc10-2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 6.Frost P, Kolstad HA, Bonde JP. Shift work and the risk of ischemic heart disease: a systematic review of the epidemiologic evidence. Scand J Work Environ Health. 2009;35:163–179. doi: 10.5271/sjweh.1319. [DOI] [PubMed] [Google Scholar]
- 7.Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC. Shift work and chronic disease: the epidemiological evidence. Occup Med (Lond) 2011;61:78–89. doi: 10.1093/occmed/kqr001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee JH, Um MH, Park YK. The association of metabolic syndrome and serum γ-glutamyl transpeptidase: a 4-year cohort study of 3,698 Korean male workers. Clin Nutr Res. 2013;2:67–75. doi: 10.7762/cnr.2013.2.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ohlander J, Keskin MC, Stork J, Radon K. Shift work and hypertension: prevalence and analysis of disease pathways in a German car manufacturing company. Am J Ind Med. 2015;58:549–560. doi: 10.1002/ajim.22437. [DOI] [PubMed] [Google Scholar]
- 10.Taniyama Y, Nakamura A, Yamauchi T, Takeuchi S, Kuroda Y. Shift-work disorder and sleep-related environmental factors in the manufacturing industry. J UOEH. 2015;37:1–10. doi: 10.7888/juoeh.37.1. [DOI] [PubMed] [Google Scholar]
- 11.Rajaratnam SM, Howard ME, Grunstein RR. Sleep loss and circadian disruption in shift work: health burden and management. Med J Aust. 2013;199:S11–S15. doi: 10.5694/mja13.10561. [DOI] [PubMed] [Google Scholar]
- 12.Boivin DB, Boudreau P. Impacts of shift work on sleep and circadian rhythms. Pathol Biol (Paris) 2014;62:292–301. doi: 10.1016/j.patbio.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Canuto R, Garcez AS, Olinto MT. Metabolic syndrome and shift work: a systematic review. Sleep Med Rev. 2013;17:425–431. doi: 10.1016/j.smrv.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 14.Shim JY. The metabolic syndrome prevention and treatment for Korean adults. Korean J Fam Pract. 2015;5:375–420. [Google Scholar]
- 15.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sookoian S, Gemma C, Fernandez Gianotti T, Burgueno A, Alvarez A, Gonzalez CD, et al. Effects of rotating shift work on biomarkers of metabolic syndrome and inflammation. J Intern Med. 2007;261:285–292. doi: 10.1111/j.1365-2796.2007.01766.x. [DOI] [PubMed] [Google Scholar]
- 17.Guo Y, Rong Y, Huang X, Lai H, Luo X, Zhang Z, et al. Shift work and the relationship with metabolic syndrome in Chinese aged workers. PLoS One. 2015;10:e0120632. doi: 10.1371/journal.pone.0120632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Bacquer D, Van Risseghem M, Clays E, Kittel F, De Backer G, Braeckman L. Rotating shift work and the metabolic syndrome: a prospective study. Int J Epidemiol. 2009;38:848–854. doi: 10.1093/ije/dyn360. [DOI] [PubMed] [Google Scholar]
- 19.Pietroiusti A, Neri A, Somma G, Coppeta L, Iavicoli I, Bergamaschi A, et al. Incidence of metabolic syndrome among night-shift healthcare workers. Occup Environ Med. 2010;67:54–57. doi: 10.1136/oem.2009.046797. [DOI] [PubMed] [Google Scholar]
- 20.Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;8:e1001141. doi: 10.1371/journal.pmed.1001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maury E, Ramsey KM, Bass J. Circadian rhythms and metabolic syndrome: from experimental genetics to human disease. Circ Res. 2010;106:447–462. doi: 10.1161/CIRCRESAHA.109.208355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leproult R, Holmback U, van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014;63:1860–1869. doi: 10.2337/db13-1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park MJ, Yun KE, Lee GE, Cho HJ, Park HS. A cross-sectional study of socioeconomic status and the metabolic syndrome in Korean adults. Ann Epidemiol. 2007;17:320–326. doi: 10.1016/j.annepidem.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Zuo H, Shi Z, Hu X, Wu M, Guo Z, Hussain A. Prevalence of metabolic syndrome and factors associated with its components in Chinese adults. Metabolism. 2009;58:1102–1108. doi: 10.1016/j.metabol.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Solomon CG, Hu FB, Dunaif A, Rich-Edwards JE, Stampfer MJ, Willett WC, et al. Menstrual cycle irregularity and risk for future cardiovascular disease. J Clin Endocrinol Metab. 2002;87:2013–2017. doi: 10.1210/jcem.87.5.8471. [DOI] [PubMed] [Google Scholar]
- 26.Peplonska B, Bukowska A, Sobala W. Association of rotating night shift work with BMI and abdominal obesity among nurses and midwives. PLoS One. 2015;10:e0133761. doi: 10.1371/journal.pone.0133761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:41. doi: 10.1186/1741-7015-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jayasena CN, Franks S. The management of patients with polycystic ovary syndrome. Nat Rev Endocrinol. 2014;10:624–636. doi: 10.1038/nrendo.2014.102. [DOI] [PubMed] [Google Scholar]
- 29.Joham AE, Boyle JA, Zoungas S, Teede HJ. Hypertension in reproductive-aged women with polycystic ovary syndrome and association with obesity. Am J Hypertens. 2015;28:847–851. doi: 10.1093/ajh/hpu251. [DOI] [PubMed] [Google Scholar]
- 30.Kim JJ, Choi YM. Dyslipidemia in women with polycystic ovary syndrome. Obstet Gynecol Sci. 2013;56:137–142. doi: 10.5468/ogs.2013.56.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palomba S, Falbo A, Russo T, Rivoli L, Orio M, Cosco AG, et al. The risk of a persistent glucose metabolism impairment after gestational diabetes mellitus is increased in patients with polycystic ovary syndrome. Diabetes Care. 2012;35:861–867. doi: 10.2337/dc11-1971. [DOI] [PMC free article] [PubMed] [Google Scholar]


