Abstract
Objectives
We evaluated the effectiveness of European chronic care programmes for type 2 diabetes mellitus (characterised by integrative care and a multicomponent framework for enhancing healthcare delivery), compared with usual diabetes care.
Design
Systematic review and meta-analysis.
Data sources
MEDLINE, Embase, CENTRAL and CINAHL from January 2000 to July 2015.
Eligibility criteria
Randomised controlled trials focussing on (1) adults with type 2 diabetes, (2) multifaceted diabetes care interventions specifically designed for type 2 diabetes and delivered in primary or secondary care, targeting patient, physician and healthcare organisation and (3) usual diabetes care as the control intervention.
Data extraction
Study characteristics, characteristics of the intervention, data on baseline demographics and changes in patient outcomes.
Data analysis
Weighted mean differences in change in HbA1c and total cholesterol levels between intervention and control patients (95% CI) were estimated using a random-effects model.
Results
Eight cluster randomised controlled trials were identified for inclusion (9529 patients). One year of multifaceted care improved HbA1c levels in patients with screen-detected and newly diagnosed diabetes, but not in patients with prevalent diabetes, compared to usual diabetes care. Across all seven included trials, the weighted mean difference in HbA1c change was −0.07% (95% CI −0.10 to −0.04) (−0.8 mmol/mol (95% CI −1.1 to −0.4)); I2=21%. The findings for total cholesterol, LDL-cholesterol and blood pressure were similar to HbA1c, albeit statistical heterogeneity between studies was considerably larger. Compared to usual care, multifaceted care did not significantly change quality of life of the diabetes patient. Finally, measured for screen-detected diabetes only, the risk of macrovascular and mircovascular complications at follow-up was not significantly different between intervention and control patients.
Conclusions
Effects of European multifaceted diabetes care patient outcomes are only small. Improvements are somewhat larger for screen-detected and newly diagnosed diabetes patients than for patients with prevalent diabetes.
Keywords: Type 2 diabetes mellitus, Managed care, Systematic review, Meta-analysis, Europe
Strengths and limitations of this study.
This is the first systematic review providing a comprehensive overview of studies that have evaluated the effectiveness of multifaceted diabetes care programmes addressing all their components together, rather than separately.
The focus in this systematic review was on European multifaceted diabetes care programmes only, to meet the need for efficient and established programmes to providing optimal chronic care due to the burden of increasing diabetes prevalence in Europe.
There is an important lack of studies which evaluate the effectiveness of implementing all chronic care model-components simultaneously.
Overall, the studies included in this systematic review provided insufficient details to fully understand the intensity of the intervention, and there was only little overlap in the wide range of outcome measures evaluated.
Introduction
Chronic disease management relies on the assumption that providing optimal chronic care requires changes of patients and professionals with regard to behaviour, culture, and communication.1 2 Indeed, with ageing of the population and the growing prevalence of chronic diseases, initiatives to improving quality of chronic care require more than evidence about effective diagnostic procedures and treatments in comparison to acute disorders.3 Aimed at describing essential elements for improving outcomes in care of chronic diseases, the chronic care model (CCM) was developed in the mid-1990s and was further refined in 1997.2 4 5 This primary care-based model is based on the assumption that improvements in care require an approach that incorporates patients, healthcare providers and system level interventions.4 6 The CCM comprises six interrelated components deemed essential for providing high-quality care to patients with chronic disease: (1) healthcare organisation (ie, providing leadership for securing resources and removing barriers to care), (2) self-management support (ie, facilitating skills-based learning and patient empowerment), (3) decision support (ie, providing guidance for implementing evidence-based care), (4) delivery system design (ie, coordinating care processes), (5) clinical information systems (ie, tracking progress through reporting outcomes to patients and providers and (6) community resources and policies (ie, sustaining care by using community-based resources and public health policy).7
The current literature indicates a widespread application of the CCM to multiple illnesses, and various studies have provided a rigorous evaluation of its individual components.5 8–14 In general, these studies have reported positive effects on patient outcomes and processes of care. The reported effect sizes, however, are relatively small, and many outcomes are flawed by a considerable level of statistical heterogeneity.10 13–25
An aspect that complicates the assessment of effectiveness of chronic care programmes is their inherent multicomponent nature.14 20 25 While some authors found that the total number of CCM elements incorporated in the interventions did not influence patient outcomes,9 10 others concluded that interventions containing more than one CCM component were more successful at improving the quality of care than single-component interventions.11 24 26 27
To date, no summative reviews have evaluated to which extent the complete CCM—thus all six components combined in interventions—improves diabetes care.
As such, the aim of the current review was to systematically identify studies of diabetes care assessing the effect of interventions addressing all six components of the CCM. We subsequently aimed to pool the effect of these models on biochemical outcomes (HbA1c, cholesterol levels, blood pressure, body mass index (BMI), fasting glucose, triglyceride and creatinine levels), patient-reported outcomes (health-related quality of life) and diabetes complications (macrovascular and microvascular complications, hypoglycaemia, cardiovascular risk, medication use and processes of care) in adult patients with type 2 diabetes compared to usual diabetes care by means of a meta-analysis.
Methods
Our systematic review was based on a protocol with input from experts in diabetes care, statistical methods and primary care. The protocol was composed according to the PRISMA-P guidelines (see online supplementary file S1).28
bmjopen-2016-013076supp1.pdf (77.9KB, pdf)
Data sources and searches
We identified studies by searching MEDLINE, Embase, CINAHL and CENTRAL from January 2000 until July 2015. Search syntaxes were developed in consultation with the Cochrane Metabolic and Endocrine Disorders Group by adapting and combining published search strategies from previous systematic reviews on chronic (diabetes) care management.10 12 Given that the CCM—and its terminology—had been introduced in the late 1990s, we restricted the search to publications from January 2000 onwards. In addition, reference lists of eligible studies and systematic reviews on multifaceted diabetes care were searched by hand to identify additional studies. The full MEDLINE search strategy is available in the online supplementary file S2.
bmjopen-2016-013076supp2.pdf (20.2KB, pdf)
Study selection
One reviewer (BWCB) identified potentially relevant studies for inclusion by screening title and abstract of all citations that resulted from our literature search. Two reviewers (BWCB and WR) then screened the full text of these articles. Only randomised controlled trials were considered eligible for inclusion. Non-randomised studies were excluded, as were studies written in a language other than English. Since this systematic review was part of a large European project on managed diabetes care that aimed at developing chronic care management standards and guidance for Europe,29 we further excluded all non-European CCM trials. Trials eligible for inclusion had to comply with the following inclusion criteria.
Type of participants
Individuals, regardless of gender and ethnicity, diagnosed with type 2 diabetes and with or without comorbidities.
Type of intervention
Previous systematic reviews on multifaceted chronic care have reported that randomised-controlled-trial-interventions are generally described poorly and incomprehensively, which complicates mapping the individual elements of the intervention to the six CCM components. To avoid mapping difficulties, we have reformulated the following inclusion criteria for the interventions: The intervention had to be described as a multifaceted CCM or programme that (1) was designed specifically for individuals with type 2 diabetes, (2) was based on guidelines, (3) provided multidisciplinary care, (4) addressed patient empowerment, (5) provided quality management (eg, patient registry systems, recording of process measurements and adherence to guidelines, achievement of treatment goals), (6) was delivered in primary or secondary care and (7) had a minimum duration of 6 months. The control intervention had to be defined as usual diabetes care as recommended in that particular country (eg, regular follow-up with the required health professional and a full diabetes annual review).
Type of outcome measures
We considered three categories of outcome measures: (1) biochemical outcomes, including HbA1c, cholesterol levels, blood pressure, BMI, fasting glucose, triglyceride and creatinine levels, (2) patient-reported outcomes, including health-related quality of life, and (3) diabetes complications, including macrovascular and microvascular complications, hypoglycaemia, cardiovascular risk, medication use and processes of care.
Any disagreements between the two reviewers regarding the inclusion or exclusion of studies were resolved by consensus.
Data extraction and quality assessment
Using a standard structured data abstraction form, one reviewer (BWCB) performed the data extraction which was confirmed by a second reviewer (WR). The extracted data included study design, length of intervention/follow-up, sample size, inclusion and exclusion criteria, mean or median age of the included sample, percentage males, study setting (ie, primary or secondary care), intervention details and mean differences in change for various outcomes. When important information or outcome data were missing, trial authors of the included studies were contacted. When unavailable, the particular data were not included in the analyses.
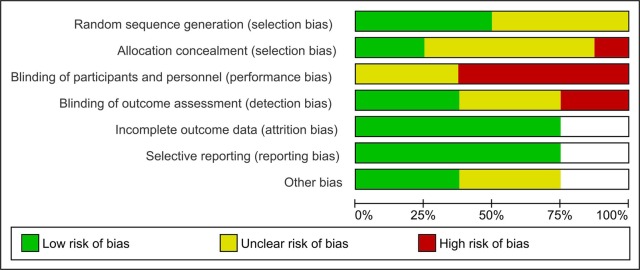
The standard Cochrane EPOC Risk of Bias Tool was used to assess risk of bias for each of the selected studies.30 Since all included studies were cluster-randomised controlled trials, additional attention was given to potential sources of bias specific to cluster-randomised trials: (1) recruitment bias: did recruitment of diabetes patients take place before or after randomisation of the clusters?, (2) did the intervention and control group differ in baseline characteristics?, (3) did any of the clusters drop out during follow-up?, (4) was clustering accounted for in the statistical analyses? If a certain domain could not be classified as ‘high’ or ‘low’ risk of bias due to inadequate reporting, it was deemed ‘unclear’ risk of bias.
Data synthesis and analysis
Owing to heterogeneity of the study populations and duration of the interventions, and owing to the small overlap in outcomes of the individual trials, an extensive meta-analysis and meta-regression of all reported outcome variables was not possible. The available data only allowed to statistically pool the results for HbA1c concentrations and total cholesterol levels. Review Manager (RevMan 5.2.0; the Cochrane Collaboration) was used to compute the weighted mean difference in change in HbA1c and total cholesterol between intervention and control groups, employing the generic inverse variance method. To incorporate between-study and within-study variance, we used a random effects model for estimating the weighted mean differences in change between intervention and control group across the included trials.31 Mean differences were pooled separately for the different types of diabetes patients (prevalent, screen-detected and newly diagnosed), and subsequently for the entire patient population. The consistency of the findings across the studies was assessed using forest plots. We evaluated statistical heterogeneity by calculating the I2 statistic, a measure independent of the number of studies and effect size metric.32 All outcome variables other than HbA1c and total cholesterol, we analysed descriptively.
Results
Figure 1 summarises the identification of relevant studies and the numbers of excluded and included studies. The search of the electronic databases identified 9464 abstracts of studies published between January 2000 and July 2015. After excluding duplicate citations (n=1227) and studies unrelated to the current review′’s topic (n=7801), we considered 436 articles for full-text review. Of these, 424 studies failed to meet our explicit inclusion criteria. In total, 12 articles met our inclusion criteria and were included in the current review.33–44 No relevant studies were retrieved by hand-search.
Figure 1.
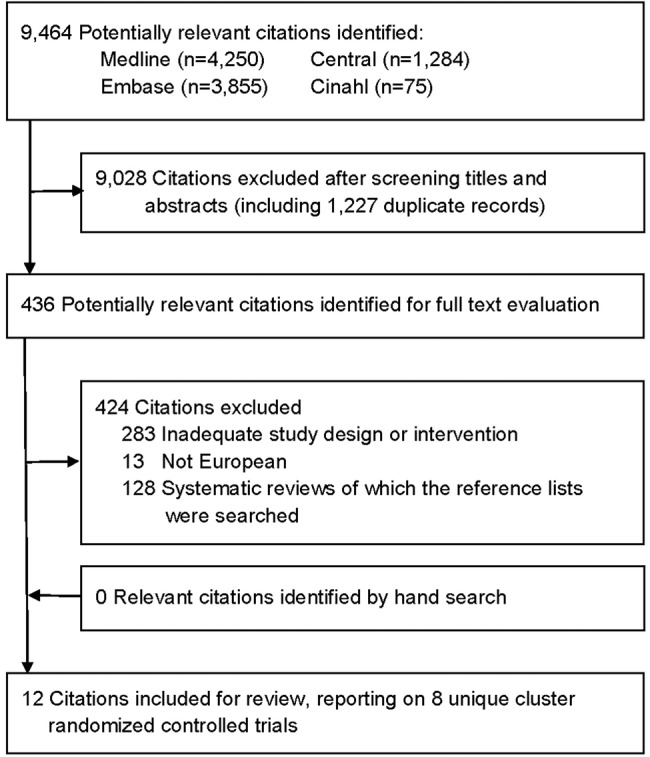
Flow chart summarising the identification of studies for inclusion in the review.
Study characteristics
The 12 included articles33–44 reported on eight unique cluster randomised controlled trials,33 35 39–41 43–45 carried out between 1989 and 2011. Two of these trials, Addition-Denmark40 and Addition-Cambridge,35 had not individually reported any follow-up results in sequel to their study protocols. Their 5-year data however were pooled in the Addition-Europe study46 together with the 5-year data of the Addition-Netherlands39 and Addition-Leicester43 trials. For the remainder of the ‘Methods’ section, we will describe the design features and assess risk of bias for the Addition-Denmark and Addition-Cambridge trials based on their published protocol, yet for the ‘Results’ section we will have to resort to the pooled five-year data from the Addition-Europe study. This means that although we identified eight unique trials,33 35 39–41 43–45 there are just seven publications to extract data from.33 39 41 43–46
All trials had recruited either general practitioners or physician practices which represented the cluster level (level of randomisation). In one study,45 however, first-level clusters were formed by district (characterised as urban, rural and mixed) and second-level clusters by the physicians. The total number of patients with type 2 diabetes enrolled by the physicians amounted to 9529, of whom 8921 (94%) had been included in the analyses.
The objective of each trial was the structured multifaceted management of diabetes, and the interventions were aimed at improving the patients’ cardiovascular risk profile44 45 and metabolic control,33 35 39 40 43 44 and assessing the effect of multifaceted care on the occurrence of cardiovascular events,35 39 40 43 overall mortality41 and risk factors for clinical complications.41 Interventions focused on all aspects of the CCM including more regular and frequent consultations, annual screening for diabetes complications, patient education/advice, guideline-based clinical treatment and physician education, regular/annual feedback reports to physicians, referrals, record keeping, formation of multidisciplinary (primary care provider) teams, delegation of routine diabetes tasks to a trained practice nurse, patient and physician reminders and patient–physician communication and decision-making. The interventions were largely delivered by general practitioners and physicians, yet specialised nurses or practice nurses were also involved in the intervention-programme as part of the practice team and to (partly) replace the physician in providing diabetes care.33 35 39 40 43 44
Two main aspects differed among the trials: the type of diabetes patient enrolled and the duration of the intervention. Three trials33 44 45 had included patients with prevalent diabetes and intervened for 1-year. The average diabetes duration in these studies ranged from 5.8 to 9.5 years. One trial41 had enrolled patients with newly diagnosed type 2 diabetes and assessed outcome measures after 6 years of intervention. Finally, there were four trials35 39 40 43 that first had initiated a diabetes screening programme and subsequently had recruited those with screen-detected diabetes to participate in the intervention study. Follow-up measurements were assessed at 1-year and at 5 years. Table 1 presents an overview of interventions and findings of the included publications. Tables 2 and 3 present the baseline patient characteristics for the trials that recruited patients with prevalent diabetes33 44 45 and for the trials that recruited patients with screen-detected39 43 46 and newly diagnosed diabetes,41 respectively.
Table 1.
Characteristics of the included cluster randomised controlled trials
| Study | Comparison | Effect on end points* | Notes |
|---|---|---|---|
| Cleveringa et al. (2008)33 | Intervention: Patient consultation by a practice nurse+use of a computerised decision support system+guideline-based care+physician support by practice nurse+interdisciplinary care by a specialist team+individualised treatment advice+patient education+physician feedback+recall system+regular patient consultations by practice nurse+physician feedback versus Usual diabetes care (not further specified) |
Biochemical outcomes HbA1c (0) Total cholesterol (+, i) HDL-cholesterol (0) LDL-cholesterol (+, i) Systolic blood pressure (+, i) Diastolic blood pressure (+, i) 10-year CHD risk (+, i) Diabetes complications and processes of care HbA1c below target value† (+, i) Total cholesterol below target value† (+, i) LDL-cholesterol below target value† (+, i) Systolic blood pressure below target value† (+, i) All treatment targets reached† (+, i) |
At baseline, patients in the intervention group had higher HDL-cholesterol levels, were more often smoker and more often had a history of CHD. Statistical analyses were conducted by intention-to-treat and for missing follow-up data the last observation was carried forward. Comparisons between the intervention and control group were adjusted for cluster structure. |
| Sönnichsen et al. (2008)45 | Intervention: Physician education+guideline-based care+patient education+use of a clinical information system tool+interdisciplinary care by a specialist team+patient reminders+physician reminders+goal setting+shared decision-making patient and physician+regular consultations versus Usual diabetes care (not further specified) |
Biochemical outcomes HbA1c (0) Total cholesterol (+, i) HDL-cholesterol (0) LDL-cholesterol (0) Systolic blood pressure (0) Diastolic blood pressure (0) Body mass index (+, i) Triglycerides (0) Creatinine (0) Diabetes complications and processes of care To the guidelines adherent: – number of eye examinations† (+, i) – number of foot examinations† (+, i) – provision of patient education† (+, i) – regular HbA1c checks† (+, i) |
At baseline, patients in the intervention group had a higher BMI and higher cholesterol levels than patients in the control group. Statistical analyses were conducted by intention-to-treat and for missing follow-up data the last observation was carried forward. Comparisons between the intervention and control groups were adjusted for cluster structure and baseline characteristics. |
| Frei et al. (2010)44 | Intervention: Specialist team involving a practice nurse+practice nurse education+physician education+physician support by practice nurse+regular independent patient consultations by practice nurse+use of a clinical information system tool+guideline-based care+physician feedback+patient information leaflets+self-management support for patient+patient treatment groups versus Usual diabetes care (not further specified) |
Biochemical outcomes HbA1c (0) Total cholesterol (0) HDL-cholesterol (0) LDL-cholesterol (+, i) Systolic blood pressure (+, i) Diastolic blood pressure (+, i) Body mass index (0) Fasting blood glucose (0) Patient-reported outcomes Diabetes complications and processes of care Number GP visits† (0) Change in antidiabetic therapy (0) Change in antihypertensive therapy (0) Change in lipid-lowering therapy (0) |
There were no baseline differences in patient characteristics between intervention and control group. Statistical analyses were conducted by intention-to-treat and for missing follow-up data the last observation was carried forward. Comparisons between intervention and control group were adjusted for cluster structure and baseline characteristics. |
| Webb et al. (2010)43 | Intervention: Structured patient education+lifestyle advice and self-management with ongoing (bimonthly) professional support+individualised management+guideline-based care+shared decision-making patient and healthcare professional+annual screening for diabetic complications+care delivered by a specialist team (specialty doctor, diabetes nurse educator, and a dietician)+patient reminders+physician reminders versus Usual diabetes care (not further specified) |
Biochemical outcomes HbA1c (+, i) Total cholesterol (+, i) LDL-cholesterol (+, i) HDL-cholesterol (0) Systolic blood pressure (+, i) Diastolic blood pressure (+, i) Body mass index (+, i) Weight (+, i) Waist circumference (0) Triglycerides (0) 5-year CHD risk (+, i) 5-year CVD risk (+, i) Patient-reported outcomes Health-related quality of life (0) Diabetes complications and processes of care Hypoglycaemia† (+, i) Use of antihypertensive drugs† (+, i) Use of lipid-lowering drugs† (+, i) Use of antiplatelet therapy† (+, i) Use of metformin† (0) Use of sulfonylurea† (0) |
At baseline, more patients in the intervention group were taking antihypertensive medication when entering the study and had higher total and LDL-cholesterol levels. Statistical analyses were conducted by intention-to-treat. It was not reported whether or not data were missing and how missing data were handled. Comparisons between intervention and control group were adjusted for cluster structure and baseline characteristics (except quality of life which had not been measured at baseline). |
| Janssen et al. (2009)39 | Intervention: Physician education+diabetes nurse education+lifestyle advice+guideline based care+physician support by diabetes nurse+evaluation and feed-back sessions diabetes nurse+frequent patient consultations with diabetes nurse+shared decision-making patient, physician and diabetes nurse+physician reminders+patient reminders versus Usual diabetes care (not further specified) |
Biochemical outcomesHbA1c (+, i) Total cholesterol (+, i) LDL-cholesterol (+, i) HDL-cholesterol (0) Systolic blood pressure (+, i) Diastolic blood pressure (+, i) Body mass index (+, i) Fasting blood glucose (+, i) Triglycerides (0) Patient-reported outcomes Health-related quality of life (0) Diabetes complications and processes of care Hypoglycaemia† (0) |
There were no baseline differences in patient characteristics between the intervention and control group. Statistical analyses were conducted by intention-to-treat and for missing follow-up data the last observation was carried forward. Comparisons between the intervention and control group were adjusted for baseline characteristics, and clustering at practice level. |
| Griffin et al. (2011)46 | This study combined the data after five years of a multifaceted care intervention from the (1) Addition-Denmark study (Lauritzen et al40), (2) the Addition-Netherlands study (Janssen et al39), (3) the Addition-Cambridge study (Echouffo et al35) and (4) the Addition-Leicester study (Webb et al43) in a meta-analysis. |
Biochemical outcomes HbA1c (+, i) Total cholesterol (+, i) LDL-cholesterol (+, i) HDL-cholesterol (0) Systolic blood pressure (+, i) Diastolic blood pressure (+, i) Body mass index (0) Weight (0) Waist circumference (0) Triglycerides (0) Creatinine (+, c) Patient-reported outcomes Health-related quality of life (0) Diabetes complications and processes of care All-cause mortality (0) CVD mortality (0) Myocardial infarction (0) Stroke (0) Revascularisation procedures (0) Hypoglycaemia† (0) Meeting target values for: HbA1c (+, i) Blood pressure (+, i) Total cholesterol (+, i) Use of any glucose-lowering drugs (+, i) Change in any antihypertensive drugs (+, i) Change in any cholesterol-lowering drugs (+, i) |
Baseline characteristics were well matched between intervention and control group. In Denmark however, more patients were identified in practices assigned to the intervention arm then in those assigned to control arm. And in the intervention group, more patients had a history of ischaemic heart disease. Statistical analyses were conducted by intention-to-treat and patients with missing outcome values at baseline were excluded from the analyses. Those with missing outcome baseline values were included according to the missing indicator method. Comparisons between intervention and control group were adjusted for cluster structure and baseline characteristics. |
| Olivarius et al. (2001)41 | Intervention: Patient follow-up every three months+annual screening for diabetes complications+shared decision-making patient and physician+physician feedback+goal setting+clinical guidelines+physician education+patient leaflets and folders+lifestyle advise+protocol based care+physician recall system versus Usual diabetes care (not further specified) |
Biochemical outcomes HbA1c (+, i) Total cholesterol (+, i) Systolic blood pressure (+, i) Diastolic blood pressure (0) Weight (0) Fasting blood glucose (+, i) Triglycerides (0) Creatinine (0) Diabetes complications and processes of care Overall mortality† (0) Severe hypoglycaemia† (0) Diabetic retinopathy† (0) Non-fatal myocardial infarction† (0) Non-fatal stroke† (0) Peripheral neuropathy† (0) Microalbuminuria† (0) Angina pectoris† (0) Intermittent claudication† (0) Number of consultations† (+, i) Number of referrals to diabetes clinic† (−, i) Number of hospital admissions† (0) Use of metformin† (+, i) Use of other glucose-lowering drugs† (0) Use of antihypertensive drugs† (0) Use of lipid-lowering drugs† (0) |
At baseline, more patients in the intervention group were excluded because of severe somatic disease than in the control group. Furthermore, occupation and smoking habits differed between the two groups. Statistical analyses were conducted by intention-to-treat. It was not reported whether or not data were missing or how missing data were handled. Comparisons between intervention and control group were adjusted for cluster structure and baseline characteristics. |
*+=positive effect; 0=no effect; −=negative effect; i=favouring intervention group; u=favouring control (usual care) group. The effects of the intervention are represented by the difference in change from baseline to follow-up between the intervention and control group.
† The effect of the intervention is represented by a difference in proportions of patients at follow-up between the intervention and control group.
CHD, coronary heart disease; CVD, cardiovascular (heart) disease; GP, general practitioner; T2DM, type 2 diabetes mellitus.
Table 2.
Baseline patient characteristics of the included cluster randomised controlled trials studying patients with prevalent diabetes
| Cleveringa et al33 * |
Sönnichsen et al45 † |
Frei et al44 ‡ |
||||
|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |
| N | 1699 | 1692 | 649 | 840 | 162 | 164 |
| Follow-up duration (years) | 1 | 1 | 1 | 1 | 1 | 1 |
| Type of diabetes patients | Prevalent diabetes | Prevalent diabetes | Prevalent diabetes | |||
| Country | Netherlands | Austria | Switzerland | |||
| Baseline patient characteristics | ||||||
| Age (years) | 65.2±11.3 | 65.0±11.0 | 65.4±10.4 | 65.5±10.4 | 65.7±10.4 | 68.3±10.6 |
| Sex (% men) | 48.2 | 49.8 | 51.0 | 53.1 | 54 | 60 |
| Ethnicity (% Caucasian) | 97.7 | 97.6 | − | − | − | − |
| Diabetes duration (years) | 5.8±5.7 | 5.4±5.8 | 7.0±6.5 | 9.5±7.4 | 10.3±7.8 | |
| Current smoking (% yes) | 22.6 | 16.6 | 13.4 | 14 | 9 | |
| Body mass index (kg/m2) | 30.0±5.3 | 30.2±5.3 | 30.4±5.1 | 29.7±4.9 | 30.5±5.3 | 30.7±5.9 |
| Systolic blood pressure (mm Hg) | 149±22 | 149±21 | 141±19 | 139±17 | 140±18 | 138±17 |
| Diastolic blood pressure (mm Hg) | 83±11 | 82±11 | 83±11 | 82±10 | 83±10 | 79±10 |
| UKDPS CHD risk (%) | 22.5±16.5§ | 21.7±15.8§ | − | − | − | − |
| HbA1c (%) | 7.1±1.3 | 7.0±1.1 | 7.46±1.53 | 7.34±1.31 | 7.8±1.5 | 7.6±1.1 |
| Total cholesterol (mmol/L) | 5.0±1.0 | 4.9±1.1 | 5.15±1.14 | 5.02±1.09 | 5.0±1.2 | 4.7±1.1 |
| HDL-cholesterol (mmol/L) | 1.36±0.36 | 1.32±0.35 | 1.35±0.39 | 1.32±0.36 | 1.2±0.3 | 1.3±0.4 |
| LDL-cholesterol (mmol/L) | 2.8±0.92 | 2.8±0.95 | 2.87±0.96 | 2·87±0·91 | 2·8±1·1 | 2·5±1·1 |
| Fasting glucose (mmol/L) | 8·0±2·4 | 7·8±2·2 | − | − | 8·4±2·5 | 7·7±2·2 |
| Creatinine (μmol/L) | 87.5±27.7 | 85.9±22.5 | 84.9±30.9 | 84.9±34.5 | − | − |
| Triglycerides (mmol/L) | 1.8±1.1 | 1.8±1.3 | 2.14±1.82 | 2.00±1.73 | − | − |
| Urinary albumin (mg/L) | − | − | − | − | − | − |
| Quality of life: PCS¶ | 43.9±10.9 | |||||
| Quality of life: MCS¶ | 50.1±11.3 | |||||
| History of myocardial infarction (%) | 47.1 | 63.3 | 8.4 | − | − | |
| History of stroke (%) | 7.0 | − | − | |||
| Diabetic retinopathy (%) | 2.9 | 3.3 | - | - | 9.3 | 8.1 |
| Peripheral neuropathy (%) | − | − | − | − | 18.6 | 13.4 |
Values are mean±sd, or percentages. Bold font indicates that the particular baseline characteristic differed statistically significantly between the intervention and control group.
*The information on BMI, fasting glucose, creatinine, triglycerides and retinopathy was obtained through contacting the authors.
†The information on diabetes duration, smoking, history of myocardial infarction and history of stroke was obtained from the publication describing baseline characteristics of the total study population and stratified by sex (Flamm et al60).
‡The quality of life summary scores for the physical and mental component were obtained from the publication describing baseline characteristics of the total study population (Frei et al61). Peripheral neuropathy is represented by ‘pathological foot status’ and diabetic retinopathy is represented by ‘annual eye exam: pathological’.
§Values concern the 10-year UKDPS CHD risk.
¶Quality of life was assessed with the 36-item Short Form Health Survey (SF-36).
CHD, coronary heart disease; MCS, Mental Component Summary Score; PCS, Physical Component Summary Score; UKPDS, UK Prospective Diabetes Study.
Table 3.
Baseline patient characteristics of the included cluster randomised controlled trials studying patients with screen-detected and newly diagnosed diabetes
| Webb et al43 |
Janssen et al39 |
Griffin et al46 |
Olivarius et al41 |
|||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | Intervention | Control | |
| N | 146 | 199 | 255 | 243 | 1678 | 1379 | 649 | 614 |
| Follow-up duration (years) | 1 | 1 | 1 | 1 | 5 | 5 | 6 | 6 |
| Type of diabetes patients | Screen-detected diabetes | Screen-detected diabetes | Screen-detected diabetes | Newly diagnosed diabetes | ||||
| Country | UK | Netherlands | UK, Netherlands, Denmark | Denmark | ||||
| Baseline patient characteristics | ||||||||
| Age (years) | 59.4±10.0 | 60.0±10.0 | 60.1±5.4 | 59.9±5.1 | 60.3±6.9 | 60.2±6.8 | 65.5 (55.3–74.0) | 65.3 (56.3–73.5) |
| Sex (% men) | 56.9 | 58.3 | 51.8 | 56.0 | 58.5 | 57.3 | 52.4 | 53.1 |
| Ethnicity (% Caucasian) | 52.7 | 62.3 | 98.0 | 98.7 | 95.8 | 93.4 | − | − |
| Diabetes duration (years) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Current smoking (% yes) | 15.2 | 10.2 | 26.3 | 21.4 | 26.9 | 27.8 | 35.5 | 34.5 |
| Body mass index (kg/m2) | 31.0±5.9 | 31.5±5.7 | 31.2±5.1 | 30.4±4.6 | 31.6±5.6 | 31.6±5.6 | 29.4 (26.2–33.0) | 28.8 (26.0–32.3) |
| Systolic blood pressure (mm Hg) | 145.7±18.5 | 148.4±20.5 | 166±23 | 163±23 | 148.5±22.1 | 149.8±21.3 | 150 (130–164) | 148 (130–160) |
| Diastolic blood pressure (mm Hg) | 87.8±10.4 | 89.5±10.7 | 90±11 | 89±10 | 86.1±11.1 | 86.5±11.3 | 85 (80–90) | 85 (80–90) |
| UKPDS CHD risk (%) | 8.5±5.8† | 9.3±7.1* | − | − | − | − | − | − |
| HbA1c (%) | 7.2±1.5 | 7.3±1.8 | 7.3±1.6 | 7.4±1.7 | 7.0±1.6 | 7.0±1.5 | 10.2 (8.6–11.6) | 10.2 (8.7–11.9) |
| Total cholesterol (mmol/L) | 5.3±1.2 | 5.6±1.3 | 5.6±1.1 | 5.6±1.1 | 5.5±1.1 | 5.6±1.2 | 6.2 (5.4–7.1) | 6.2 (5.5–7.2) |
| HDL-cholesterol (mmol/L) | 1.2±0.4 | 1.2±0.3 | 1.1±0.4 | 1.1±0.3 | 1.2 (1.0–1.5) | 1.2 (1.0–1.5) | − | − |
| LDL-cholesterol (mmol/L) | 3.2±1.0 | 3.5±1.0 | 3.7±1.0 | 3.7±1.0 | 3.4±1.0 | 3.5±1.0 | − | − |
| Fasting glucose (mmol/L) | − | − | 7.8±2.3 | 8.1±2.8 | − | − | 13.8 (10.7–17.0) | 13.7 (10.7–17.0) |
| Creatinine (μmol/L) | − | − | − | − | 83.4±17.1 | 84.9±18.6 | 90 (81–101) | 88 (79–100) |
| Triglycerides (mmol/L) | 2.1±1.9 | 2.1±1.4 | 1.9±1.0 | 2.0±1.6 | 1.6 (1.2–2.3) | 1.7 (1.2–2.4) | 2.03 (1.44–2.91) | 1.98 (1.39–2.95) |
| Urinary albumin (mg/L) | − | − | − | − | − | − | 11.7 (6.0–32.5) | 11.8 (5.7–27.5) |
| Quality of life: PCS† | 39.0 (37.4–40.5) | 38.5 (37.1-40.0) | No summary scores reported | − | − | − | − | |
| Quality of life: MCS† | 38.2 (35.2–41.2) | 39.2 (36.5–41.9) | No summary scores reported | − | − | − | − | |
| History of myocardial infarction (%) | 15.8* | 10.6‡ | − | − | 6.8 | 6.1 | 6.6 | 7.7 |
| History of stroke (%) | − | − | 2.9 | 1.9 | 3.5 | 4.2 | ||
| Diabetic retinopathy (%) | − | − | − | − | − | − | 5.0 | 4.5 |
| Peripheral neuropathy (%) | − | − | − | − | − | − | 18.8 | 19.7 |
Values are mean±sd, or median (IQR) or percentages. Bold font indicates that the comparison between the intervention and control group was statistically significant.
*Values concern the 5-year UKDPS CHD risk.
†Quality of life was assessed with the 12-item Short Form Health Survey (SF-12) in the study by Webb et al, and with the 36-item Short Form Health Survey (SF-36) in the study by Janssen et al.
‡Defined as ‘pre-existing CVD’, including myocardial infarction, stroke and angina.
CHD, coronary heart disease; MCS, Mental Component Summary Score; PCS, Physical Component Summary Score; UKPDS, UK Prospective Diabetes Study.
Data quality assessment
Figure 2 summarises the risk of bias for the trials included in this review. Although the Addition-Denmark40 and the Addition-Cambridge35 trials had not published 1-year data, they did provide 5-year data for the Addition-Europe meta-analysis46 and were thus included in the risk of bias assessment. However, since not having published actual trial data, we could not assess the domains of incomplete outcome data, selective reporting and other bias, which resulted in the occurrence of blanks in figure 2.
Figure 2.
Risk of bias graph. Review authors' judgements about each risk of bias item presented as percentages across all included studies. Studies included are Cleveringa et al (2008);33 Sönnichsen et al (2008),45 Frei et al (2010),44 Olivarius et al (2001),41 Janssen et al (2009),39 Webb et al (2010),43 Lauritzen et al (2000)40 and Echouffo et al (2009).35 The studies from Lauritzen and Echouffo were included in the risk of bias assessment since their 5-year follow-up data had been included in the Addition-Europe meta-analysis by Griffin et al.46 As the Addition-Europe publication only reported pooled data, no comprehensive overview of results was available for the studies by Lauritzen and Echouffo, which resulted in the blanks in the risk of bias graph.
Seven trials had at least one domain judged as unclear risk of bias. Five trials had at least one domain judged as high risk of bias. Only one study44 had explicitly described that their physicians were unaware of being allocated to the intervention or control group when recruiting eligible patients. For the remaining studies, prior knowledge of treatment allocation cannot be ruled out (recruitment bias). Furthermore, the Addition studies35 39 40 43 were the only trials in which patients remained unaware of group assignment throughout the study.
In four studies,35 39 40 43 outcome assessment was performed completely blinded for patient allocation. In one study,45 only laboratory outcomes were assessed blinded, whereas clinical outcomes were obtained by contacting the general practitioner, introducing possible bias. No substantial baseline differences between the intervention and control groups existed with regard to the outcomes of interest.
Biochemical outcomes
All studies had assessed biochemical outcomes at follow-up, including HbA1c level, blood lipid levels, blood pressure and BMI.
HbA1c levels
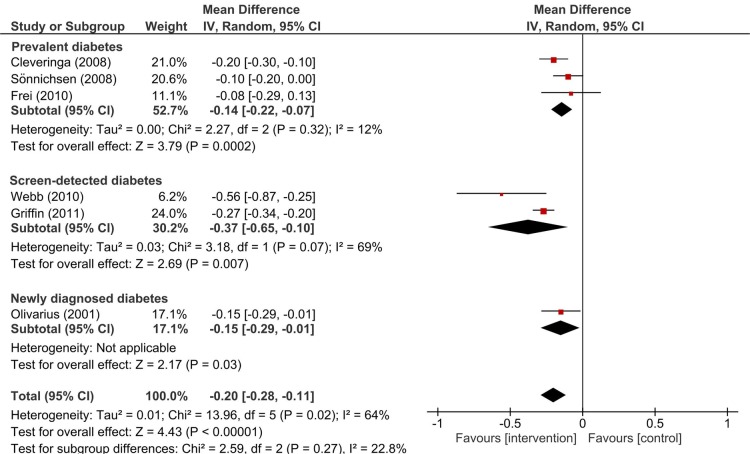
All studies assessed HbA1c values at follow-up. For six33 39 43–46 of the seven study populations glycaemic control at baseline was moderate to good, as expressed by the mean HbA1c concentrations ranging from 7.0 to 7.8% (53 to 62 mmol/mol). The three trials with prevalent type 2 diabetes patients33 44 45 observed no statistically significant difference in change in HbA1c levels between the intervention and control group after 1-year of intervention (figure 3). There was no statistical heterogeneity between these three trials (I2=0%) and the weighted mean difference in change between intervention and control groups was −0.06% (95% CI −0.13 to 0.01) (−0.7 mmol/mol (95% CI −1.4 to 0.1)), in favour of the intervention group. Using a similarly short intervention period, yet studying patients with screen-detected type 2 diabetes, the Addition-Leicester trial43 observed a significant difference in change in HbA1c between the two trial arms of −0.20% (95% CI −0.32 to −0.08) (−2.2 mmol/mol (95% CI −3.4 to −0.9)). Whereas the Addition-Netherlands authors39 did not report the actual difference in HbA1c change between the two groups, they stated in their paper that the improvement in HbA1c was significantly better in the intervention group, compared to the control group. The pooled 5-year data from all four Addition-trials46 showed a somewhat smaller, yet significantly greater improvement in HbA1c concentration in intervention patients, compared to control patients (−0.08% (95% CI −0.14 to −0.02)) (−0.9 mmol/mol (95% CI −1.5 to −0·2)) (figure 3). Finally, the effect of multifaceted care in Danish patients with newly diagnosed diabetes41 after 6 years of intervention was comparable to that in screen-detected patients after 5 years of intervention46 (−0.06% (95% CI −0.08 to −0.03)) (−0.7 mmol/mol (95% CI −0.9 to −0.3)).
Figure 3.
Mean difference in change (95% CI) in HbA1c levels (%) after multifaceted care between intervention and control groups. Results are stratified by type of diabetes patient. IV, generic inverse variance method. The three studies including patients with prevalent diabetes has an intervention duration of 1-year. The methodology for calculating the difference in change between intervention and control group that Cleveringa et al.33 have used (subtracting the HbA1c change over time for the control group from the change over time for the intervention group) was the opposite of that used by the other trials (subtracting the HbA1c change over time for the intervention group from the change over time for the control group). Since this would result in a misleading visual presentation of the findings from Cleveringa et al.,33 we have recalculated their HbA1c results according to the methodology used by the other studies. The study of Webb et al.43 had an intervention duration of one year and the study of Griffin et al.46 combined the 5-year intervention data from all four Addition studies, including the five-year data from Webb et al.43 The study including patients with newly detected diabetes had an intervention duration of six years.
Pooling all seven trials, multifaceted care improved HbA1c concentration with −0.07% (95% CI −0.10 to −0.04) (−0.8 mmol/mol (95% CI −1.1 to −0.4)) (figure 3). Statistical heterogeneity across the seven trials was small to moderate (I2=21%).
Cholesterol levels
Figure 4 presents the mean differences in change in total cholesterol levels for all seven trials. Of the three trials that studied prevalent diabetes patients, only the Dutch trial33 observed multifaceted care to significantly improve total cholesterol concentrations. In the remaining two studies,44 45 cholesterol levels were similar between intervention and control arm. Statistical heterogeneity across the three studies was low (I2=12%) and their weighted mean difference in change between intervention and control groups amounted to −0.14 mmol/L (95% CI −0.22 to −0.07). Similar to HbA1c, the effect of multifaceted care on cholesterol seemed larger in screen-detected patients than in patients with prevalent diabetes. After 1-year of intervention, Addition-Leicester43 found a mean difference in change between the intervention and control group of −0.56 mmol/L (95% CI −0.87 to −0.25). The pooled 5-year data from all four Addition trials also showed a significantly greater improvement in total cholesterol levels in intervention patients, compared to control patients (−0.27 mmol/L (95% CI −0.34 to −0.20)). Finally, in Danish patients with newly diagnosed diabetes,41 6 years of multifaceted care had caused cholesterol levels to improve (−0.15 mmol/L (95% CI −0.29 to −0.01)).
Figure 4.
Mean difference in change (95% CI) in total cholesterol levels (mmol/L) after multifaceted care between intervention and control groups. Results are stratified by type of diabetes patient. IV, generic inverse variance method. The three studies including patients with prevalent diabetes has an intervention duration of 1-year. The methodology for calculating the difference in change between intervention and control group that Cleveringa et al.33 have used (subtracting the HbA1c change over time for the control group from the change over time for the intervention group) was the opposite of that used by the other trials (subtracting the HbA1c change over time for the intervention group from the change over time for the control group). Since this would result in a misleading visual presentation of the findings from Cleveringa et al.,33 we have recalculated their HbA1c results according to the methodology used by the other studies. The study of Webb et al.43 had an intervention duration of one year and the study of Griffin et al.46 combined the 5-year intervention data from all four Addition studies, including the five-year data from Webb et al.43 The study including patients with newly detected diabetes had an intervention duration of six years.
Pooling all trials, the effect of multifaceted care on improvement of total cholesterol resulted in a weighted difference in change between intervention and control patients of −0.20 mmol/L (95% CI −0.28 to −0.11); I2=64%.
In addition to improvements in total cholesterol levels, HDL-cholesterol levels appeared to be unaffected by multifaceted care in patients with prevalent diabetes.33 44 45 LDL-cholesterol levels on the other hand did improve (see online supplementary figure S1 and S2). The Dutch33 and the Swiss44 study found significantly better improvements in LDL-cholesterol for the intervention group, when compared to the control group. The Addition-Netherlands39 and Addition-Leicester43 studies observed that multifaceted care significantly improved LDL-cholesterol levels after 1-year, while HDL-cholesterol remained largely unchanged. Similar results were reported for 5 years of intervention by the Addition-Europe study.46 The Danish study41 with newly diagnosed diabetes patients had not measured HDL and LDL-cholesterol levels.
bmjopen-2016-013076supp_figures.pdf (272.6KB, pdf)
Blood pressure
Two33 44 out of the three trials with patients with prevalent diabetes reported a difference in change in diastolic and systolic blood pressure, both being in favour of the intervention group (see online supplementary figures S3 and S4). Better improvements in blood pressure were also seen in intervention patients with screen-detected diabetes, compared to control patients.39 43 46 Improvements after 1-year of intervention43 were larger than those after 5 years of intervention.46 In patients with newly diagnosed diabetes41 6 years of multifaceted care significantly improved systolic, but not diastolic, blood pressure when compared to usual diabetes care. Similar to HbA1c and total cholesterol, the results for blood pressure were stronger for patients with screen-detected and newly diagnosed diabetes than for those with prevalent, long-standing diabetes.
Body mass index
With regard to the studies on prevalent diabetes, only the Austrian study45 found a significant difference in change in BMI between the intervention group and control group after 1-year of intervention (see online supplementary figure S5). In screen-detected diabetes patients,39 43 multifaceted care resulted in a significantly higher reduction in BMI, compared to usual diabetes care. Furthermore, Addition-Leicester43 reported a higher reduction in BMI and body weight (kg) for the intervention group compared to the control group, but observed no difference in reduction of waist circumference. After an intervention duration of 5 years, the pooled reduction in weight and waist circumference, but not in BMI, in screen-detected diabetes was significantly higher in the intervention group compared to the control group.46 The Danish trial41 with newly diagnosed diabetes patients observed no difference in weight change after 6 years of intervention, yet BMI had not been measured.
For further biochemical outcomes, see online supplementary file S3 and figures S6–S8.
bmjopen-2016-013076supp3.pdf (17.1KB, pdf)
Patient-reported outcomes
The effect of a multifaceted care intervention on the patients’ quality of life accounted for the only patient-reported outcome assessed by the included trials.
Health-related quality of life
Quality of life was reported by five33 39 43 44 46 of the seven trials, most of which had used the 36-item Short Form Health Survey (SF-36) to assess the different domains of health-related quality of life. In patients with prevalent diabetes,33 44 significant changes over time were absent for all scores of the SF-36 subscales for the intervention and control arms. A superior effect of multifaceted care was observed only on the SF-36 subscale ‘health change’ in the Dutch trial with prevalent diabetes patients.33 For the two Addition studies reporting results after 1-year of intervention,39 43 as for the pooled 5-year data by Addition-Europe,46 no significant changes in the physical and mental summary scores of the SF-36, or the abbreviated SF-12 version that was used in the Addition-Leicester trial,43 could be demonstrated.
Diabetes complications
Only few trials had reported diabetes complications, including cardiovascular disease and mortality. Closely related to the prevention and occurrence of complications, some studies evaluated the effect of their intervention on processes of care, such as reaching target values for HbA1c and receiving regular eye and foot examinations.
Macrovascular and microvascular complications
Macrovascular and microvascular diabetes complications during follow-up were reported by the two studies41 46 with the longer intervention periods. The Addition-Europe study46 had assessed myocardial infarction, stroke, coronary and peripheral revascularisation procedures, cardiovascular death and total mortality and non-traumatic amputation in screen-diagnosed diabetes patients. Although the estimated HRs for these events all favoured the intervention group, none of the estimates reached statistical significance. In newly diagnosed diabetes patients,41 multifaceted care had not resulted in differences between intervention and control group regarding the risk of diabetic retinopathy, peripheral neuropathy, microalbuminuria, non-fatal myocardial infarction and stroke, angina pectoris or intermittent claudication at 6 years.
Processes of care
Only three studies assessed processes of care or process quality measures.33 45 46 The Dutch study33 with prevalent diabetes patients observed that multifaceted care resulted in significantly more patients reaching treatment targets (18.9%) than usual diabetes care (13.4%) (treatment targets were defined as HbA1c ≤7% (53 mmol/mol), systolic blood pressure ≤140 mm Hg, total cholesterol ≤4.5 mmol/L and LDL-cholesterol ≤2.5 mmol/L). Process quality measures at 1-year, defined as the percentage of patients receiving guideline-adherent foot-examinations, eye-examinations and HbA1c-examinations, were reported by the Austrian study with prevalent diabetes patients45 to be significantly higher in the intervention group. The pooled 5-year results from the four Addition studies46 showed that in both trial arms more patients had values below target thresholds for HbA1c (<7% (53 mmol/mol)), blood pressure (≤135/85 mm Hg) and cholesterol level (<4.5 mmol/L), yet proportions were higher in the intervention group than in the control group.
For further diabetes complications and related outcomes, see online supplementary file S3.
Discussion
This review assessed the effectiveness of chronic disease management models for type 2 diabetes on the improvement of patient outcomes, in Europe. In general, the effects of multifaceted care on patient outcomes were rather small and their magnitude seemed to differ according to the type of diabetes patient being studied. Our analysis suggested that in comparison to usual diabetes care, multifaceted care improves HbA1c levels for patients with screen-detected diabetes and patients with newly diagnosed diabetes, but not for patients with prevalent type 2 diabetes. Similar findings were observed for total cholesterol, LDL-cholesterol, BMI and body weight. The resulting improvements in blood pressure seemed less strongly related to the type of diabetes patient studied. Other outcomes, such as fasting glucose levels, triglycerides, quality of life and diabetes complications, had been reported inconsequently, and results varied widely across the included trials.
The few cluster randomised controlled trials that we identified from the literature were relatively heterogeneous with regard to the individual components of the implemented intervention, duration of the intervention, type of diabetes patient and reported outcomes. For each trial, methodological quality was acceptable and there were very low rates of dropout among the enrolled patients. Still, details on the randomisation procedure were frequently missing as well as information concerning concealment of allocation from general practitioners and physicians in advance to recruitment of eligible patients. Since the currently performed meta-analysis included only a small number of trials, caution is warranted not to overinterpret its results. The χ2 statistic for example, indicating homogeneity of the effect of the intervention on HbA1c and total cholesterol, has low power when based on only few, and small-sized, studies.47 When interpreting the data, we thus prefer to look at the direction of the individual effect estimates and CIs, rather than let the calculated statistics guide our conclusions. As such, given the current literature, it is not possible to draw an unequivocal conclusion about the effectiveness of chronic multifaceted care on diabetes patient outcomes.
Overall, previous systematic reviews have reported that an integrated approach to diabetes care versus usual diabetes care may improve clinical and biochemical outcomes,9 10 19 20 23 24 48 including HbA1c levels, blood pressure and blood lipid concentrations. Those reviews that included a meta-analysis reported mean differences in HbA1c reduction between intervention and control groups ranging from −0.14% (95% CI −0.25 to −0.05) to −0.5% (95% CI −0.6 to −0.3). Mean differences in total cholesterol have only been estimated by one meta-analysis, which reported a reduction of −0.24 mmol/L (95% CI −0.41 to −0.06) in favour of the intervention group.10 This study also reported a mean difference in diastolic blood pressure reduction of −1.3 mm Hg (95% CI −0.21 to −0.6) and a mean difference in systolic blood pressure reduction of −2.2 mm Hg (95% CI −3.5 to −0.9), comparable with the summary estimate for systolic blood pressure from Elissen et al (−2.8 mm Hg (95% CI −4.7 to −0.9)).20 All other outcomes of multifaceted care interventions were described narratively. Improvements have been observed for frequency of retinopathy screening,20 48 49 screening for peripheral polyneuropathy and foot lesions,20 48 49 proteinuria measurements49 and the monitoring frequency of lipid and HbA1c levels.49 In addition, there seems to be an economic benefit of integrated diabetes care.50 Yet, other systematic reviews have found no impact on patients outcomes and processes of care18 25 49 or have disputed the clinical relevance of statistically significant findings.19 A comparison of the reported effect estimates with our summary estimates for HbA1c and total cholesterol warrants caution, given the varying number of CCM elements the estimates were based on, the heterogeneity among the included diabetes patients, the different restrictions to geographical region and the number of included studies in each review.
The novelty of the current systematic review is that it provides a comprehensive overview of diabetes care trials that have evaluated the effectiveness of the all the six components of the CCM combined, instead of one or more components. Overall, we found there is an important lack of studies which evaluate the implementation of all six CCM-components simultaneously. In the current literature, findings on the issue of whether multifaceted chronic care is to be preferred over single-faceted care are conflicting.9–12 24–26 51 However, improving the management of a complex disease like diabetes is a challenging goal which, we believe, may not be achieved by targeting single care aspects only. Another novel aspect of the current review is the focus on state-of-the-art diabetes management in Europe only. The narrow view relates to the enormous burden that type 2 diabetes represents in Europe, in individual and in societal terms.52 The prevalence of diabetes in Europe is expected to increase from 59.8 million adults in 2015 to 71.1 million in 2040.53
As reflected by recent guidelines for the management of patients with type 2 diabetes,54 healthcare providers have increasingly focused at improving and controlling cardiovascular risk factors to improve patient outcomes, including hyperglycaemia, overweight or obesity, elevated blood pressure and dyslipidemia. Results from the Steno-2 trial support the view that even in high-risk patients with type 2 diabetes multifaceted care has the potential to reduce the risk of complications and mortality.55 Randomising 160 patients with type 2 diabetes and persistent microalbuminuria to an intensive multifactorial treatment and conventional therapy, the authors found that the multifactorial treatment was associated with a lower risk of cardiovascular events after 13.3 years of follow-up, as well as with a lower risk of death from cardiovascular disease, compared to conventional treatment. And while the CCM has been proposed as a tool to improve the quality of diabetes care and, subsequently, patient outcomes, the current review indicates that at least the existing programmes have not been as successful in this respect as intended. The challenge thus remains to translate results from landmark studies like Steno-2, into primary care, where the majority of type 2 diabetes patients are being treated.
When aiming to improve chronic healthcare, it has been proposed that only assessing the effects of a multifaceted care intervention on patient outcomes is not sufficient. In order to gain insights into why and when certain interventions are effective, it is also important to focus on barriers and facilitators to the implementation process of the intervention and their effect on the interplay between intervention and outcomes.56 This latter aspect is usually not evaluated or reported on by randomised controlled trials implementing a multifaceted care intervention.57 As such, it has not yet been possible to analyse the relationships between context, mechanisms and outcomes of multifaceted diabetes care interventions and to subsequently provide meaningful insights into how these have influenced the outcomes achieved.57
There are some limitations of our work that need to be considered. First, many studies provided insufficient detail in their methods section to fully understand the intensity of (specific components of) the intervention. This complicated our appraisal of whether all components of the CCM were fully covered. Also, the different interventions that the trials have used to represent a given component of the CCM have possibly resulted in some heterogeneity across the trials. In addition to the insufficiently described interventions, standards for usual diabetes care were not elaborated on in any of the trials. Online versions of diabetes care guidelines were found to be published in the country’s native language and represented current versions only. However, most European countries define their standards according to the recommendations made by the joint task force convened by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD).54 58 Indeed, identified guidelines from the Netherlands, Austria, and the UK did comply with the ADA/EASD recommendations. We do therefore not expect that practices of usual diabetes care in the individual trials have differed to the extent of causing a significant increase in heterogeneity. Second, whereas the aim of the current review was to investigate the effectiveness of CCMs in Europe, the trials available for this review only represented the Western part of Europe. Countries with the highest prevalence of diabetes lie in Eastern Europe, that is, Turkey, Montenegro, Macedonia and Serbia.52 The top-three countries in Western Europe with the highest diabetes prevalence are Germany, Spain and Italy,52 none of which were represented in this review. And third, the procedure of selecting relevant studies for the current review was largely performed by only one person. However, two reviewers subsequently screened the full text of all potentially relevant papers such that the final decision on inclusion was based on two opinions.
In conclusion, the available scientific evidence regarding the effectiveness of multifaceted chronic care programmes for type 2 diabetes in older patients in Europe is low. In general, the current findings support the concept of the CCM, yet the improvements in patient outcomes and processes of care are only small. While key aspects of type 2 diabetes can be improved by a multifactorial intervention, it is not yet clear if these improvements will subsequently lower diabetes-related complications, such as cardiovascular disease and overall mortality. Furthermore, the effect of the interventions seemed, at least partly, to depend on the type of diabetes patient, which could suggest effect modification by disease duration and/or disease severity. Another aspect that could add to the differences in effectiveness between the individual interventions is the degree in which they facilitate changes in social behaviour. This implies that more attention in trials should be spent to factors like adherence to treatment strategies, level of self-management skills and patients’ knowledge on their disease. These traits need to be positively affected before an improvement in clinical measures can even occur,1 yet studies generally reveal little on person-centred factors. And finally, there is a lack of knowledge (on information) on effective methods to address important pragmatic questions about improvement of care, for example, which specific mechanism or procedure of a CCM works, for which patients and under which circumstances?59 Future research would need to incorporate the measurement of context, mechanisms and outcomes of multifaceted care into study designs in order to deliver the full extent of insights needed to improve chronic diabetes care and, ultimately, patient outcomes.
Acknowledgments
The authors thank Trials Search Co-ordinator Maria-Inti Metzendorf and Professor Bernd Richter (MD) from the Cochrane Metabolic and Endocrine Disorders group (University Hospital Düsseldorf, Germany) for their valuable assistance, guidance and advice offered while developing the literature search strategy. The authors thank the trial authors of the Dutch Diabetes Care Implementation Study, the Swiss Chronic CARE for diAbeTes Study (CARAT) and the Danish Diabetes Care in General Practice study for kindly providing us additional trial results. Furthermore, we are grateful to Professor Oliver Kuß (PhD) from the Institute for Biometrics and Epidemiology of the German Diabetes Center (Düsseldorf, Germany) for his useful contributions to developing the review protocol.
Footnotes
Contributors: BWCB designed the review by writing the review protocol, identified studies for inclusion, extracted and interpreted the data and drafted and revised the article. KM contributed to the review protocol and to the discussion. He further revised the draft paper for intellectual content. JW involved in conception of the review and he contributed to the review protocol, to interpretation of the data and to the discussion. Furthermore, JW revised the draft paper for intellectual content. CL contributed to the review protocol and to the discussion, and she revised the draft paper for intellectual content. PS conceived and initiated the review, contributed to the review protocol and contributed to the interpretation of the data, to the discussion and to revision of the draft paper. MR involved in conception of the review and revised the draft paper for intellectual content. WR contributed to the review protocol, identified studies for inclusion, extracted and interpreted the data and revised the draft paper for intellectual content. All authors approved the final completed article.
Funding: The MANAGE-CARE project—of which this systematic review was part—was supported by grants from the European Commission (Grant Agreement 2012 12 03). The funding body had no influence on the design and conduct of the study, interpretation of the data and contents and publication of this manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Lemmens KM, Nieboer AP, van Schayck CP et al. . A model to evaluate quality and effectiveness of disease management. Qual Saf Health Care 2008;17:447–53. 10.1136/qshc.2006.021865 [DOI] [PubMed] [Google Scholar]
- 2.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q 1996;74:511–44. 10.2307/3350391 [DOI] [PubMed] [Google Scholar]
- 3.Clark CM, Fradkin JE, Hiss RG et al. . Promoting early diagnosis and treatment of type 2 diabetes: The National Diabetes Education Program. JAMA 2000;284:363–5. 10.1001/jama.284.3.363 [DOI] [PubMed] [Google Scholar]
- 4.Wagner EH, Davis C, Schaefer J et al. . A survey of leading chronic disease management programs: are they consistent with the literature? Manag Care Q 1999;7:56–66. [PubMed] [Google Scholar]
- 5.Wagner EH, Austin BT, Davis C et al. . Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78. 10.1377/hlthaff.20.6.64 [DOI] [PubMed] [Google Scholar]
- 6.Glasgow RE, Orleans CT, Wagner EH. Does the chronic care model serve also as a template for improving prevention? Milbank Q 2001;79:579–612, iv–v 10.1111/1468-0009.00222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.http://www.improvingchroniccare.org, 09-07-2015.
- 8.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002;288:1775–9. 10.1001/jama.288.14.1775 [DOI] [PubMed] [Google Scholar]
- 9.Tsai AC, Morton SC, Mangione CM et al. . A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care 2005;11:478–88. [PMC free article] [PubMed] [Google Scholar]
- 10.Si D, Bailie R, Weeramanthri T. Effectiveness of chronic care models-oriented interventions to improve quality of diabetes care: a systematic review. Prim Health Care Res Dev 2008;9:25–40. [Google Scholar]
- 11.Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis 2013;10:E26 10.5888/pcd10.120180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zwar N, Harris M, Griffiths R et al. . A systematic review of chronic disease management. Research Centre for Primary Health Care and Equity, School of Public Health and Community Medicine, University of New South Wales, 2006. [Google Scholar]
- 13.Tricco AC, Ivers NM, Grimshaw JM et al. . Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet 2012;379:2252–61. 10.1016/S0140-6736(12)60480-2 [DOI] [PubMed] [Google Scholar]
- 14.Shojania KG, Ranji SR, McDonald KM et al. . Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA 2006;296:427–40. 10.1001/jama.296.4.427 [DOI] [PubMed] [Google Scholar]
- 15.Glazier RH, Bajcar J, Kennie NR et al. . A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care 2006;29:1675–88. 10.2337/dc05-1942 [DOI] [PubMed] [Google Scholar]
- 16.Loveman E, Royle P, Waugh N. Specialist nurses in diabetes mellitus. Cochrane Database Syst Rev 2003;(2):CD003286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norris SL, Chowdhury FM, Van Le K et al. . Effectiveness of community health workers in the care of persons with diabetes. Diabet Med 2006;23:544–56. 10.1111/j.1464-5491.2006.01845.x [DOI] [PubMed] [Google Scholar]
- 18.Renders CM, Valk GD, Griffin S et al. . Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev 2001;(1):CD001481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Egginton JS, Ridgeway JL, Shah ND et al. . Care management for type 2 diabetes in the United States: a systematic review and meta-analysis. BMC Health Serv Res 2012;12:72 10.1186/1472-6963-12-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elissen AM, Steuten LM, Lemmens LC et al. . Meta-analysis of the effectiveness of chronic care management for diabetes: investigating heterogeneity in outcomes. J Eval Clin Pract 2013;19:753–62. [DOI] [PubMed] [Google Scholar]
- 21.Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ 2013;185:E635–644. 10.1503/cmaj.130053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ivers NM, Tricco AC, Taljaard M et al. . Quality improvement needed in quality improvement randomised trials: systematic review of interventions to improve care in diabetes. BMJ Open 2013;3:pii: e002727 10.1136/bmjopen-2013-002727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pimouguet C, Le Goff M, Thiebaut R et al. . Effectiveness of disease-management programs for improving diabetes care: a meta-analysis. CMAJ 2011;183:E115–127. 10.1503/cmaj.091786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shojania KG, Ranji SR, Shaw LK et al. . Closing the quality gap: a critical analysis of quality improvement strategies (Vol 2: Diabetes Care). Rockville, MD: Agency for Healthcare Research and Quality; 2004. September. Technical Review no. 9. AHRQ publication no. 04-0051-2. [PubMed] [Google Scholar]
- 25.Baptista DR, Wiens A, Pontarolo R et al. . The chronic care model for type 2 diabetes: a systematic review. Diabetol Metab Syndr 2016;8:7 10.1186/s13098-015-0119-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boaz A, Baeza J, Fraser A et al. . Effective implementation of research into practice: an overview of systematic reviews of the health literature. BMC Res Notes 2011;4:212 10.1186/1756-0500-4-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brusamento S, Legido-Quigley H, Panteli D et al. . Assessing the effectiveness of strategies to implement clinical guidelines for the management of chronic diseases at primary care level in EU Member States: a systematic review. Health Policy 2012;107:168–83. 10.1016/j.healthpol.2012.08.005 [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Shamseer L, Clarke M et al. . Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.http://www.managecare-project.eu/.
- 30.Higgins JP, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions, Version 510 [updated March 2011] The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org [Google Scholar]
- 31.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 32.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 33.Cleveringa FGW, Gorter KJ, van den Donk M et al. . Combined task delegation, computerized decision support, and feedback improve cardiovascular risk for type 2 diabetic patients: a cluster randomized trial in primary care. Diabetes care 2008;31:2273–5. 10.2337/dc08-0312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cleveringa FGW, Minkman MH, Gorter KJ et al. . Diabetes Care Protocol: effects on patient-important outcomes. A cluster randomized, non-inferiority trial in primary care. Diabet Med 2010;27:442–50. 10.1111/j.1464-5491.2010.02968.x [DOI] [PubMed] [Google Scholar]
- 35.Echouffo-Tcheugui JB, Simmons RK, Williams KM et al. . The ADDITION-Cambridge trial protocol: a cluster—randomised controlled trial of screening for type 2 diabetes and intensive treatment for screen-detected patients. BMC Public Health 2009;9:136 10.1186/1471-2458-9-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flamm M, Panisch S, Winkler H et al. . Effectiveness of the Austrian disease management programme ‘Therapie Aktiv’ for type 2 diabetes regarding the improvement of metabolic control, risk profile and guideline adherence: 2 years of follow up. Wien Klin Wochenschr 2012;124:639–46. 10.1007/s00508-012-0226-x [DOI] [PubMed] [Google Scholar]
- 37.Flamm M, Panisch S, Winkler H et al. . Impact of a randomized control group on perceived effectiveness of a disease management programme for diabetes type 2. Eur J Public Health 2012;22:625–9. 10.1093/eurpub/ckr147 [DOI] [PubMed] [Google Scholar]
- 38.Frei A, Senn O, Chmiel C et al. . Implementation of the chronic care model in small medical practices improves cardiovascular risk but not glycemic control. Diabetes Care 2014;37:1039–47. 10.2337/dc13-1429 [DOI] [PubMed] [Google Scholar]
- 39.Janssen PG, Gorter KJ, Stolk RP et al. . Randomised controlled trial of intensive multifactorial treatment for cardiovascular risk in patients with screen-detected type 2 diabetes: 1-year data from the ADDITION Netherlands study. Br J Gen Pract 2009;59:43–8. 10.3399/bjgp09X394851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lauritzen T, Griffin S, Borch-Johnsen K et al. . The ADDITION study: proposed trial of the cost-effectiveness of an intensive multifactorial intervention on morbidity and mortality among people with type 2 diabetes detected by screening. Int J Obes Relat Metab Disord 2000;24(Suppl 3):S6–11. 10.1038/sj.ijo.0801420 [DOI] [PubMed] [Google Scholar]
- 41.Olivarius NF, Beck-Nielsen H, Andreasen AH et al. . Randomised controlled trial of structured personal care of type 2 diabetes mellitus. BMJ 2001;323:970–5. 10.1136/bmj.323.7319.970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sönnichsen AC, Winkler H, Flamm M et al. . The effectiveness of the Austrian disease management programme for type 2 diabetes: a cluster-randomised controlled trial. BMC Fam Pract 2010;11:86 10.1186/1471-2296-11-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Webb DR, Khunti K, Srinivasan B et al. . Rationale and design of the ADDITION-Leicester study, a systematic screening programme and randomised controlled trial of multi-factorial cardiovascular risk intervention in people with type 2 diabetes mellitus detected by screening. Trials 2010;11:16 10.1186/1745-6215-11-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frei A, Chmiel C, Schläpfer H et al. . The Chronic CARe for diAbeTes study (CARAT): a cluster randomized controlled trial. Cardiovasc Diabetol 2010;9:23 10.1186/1475-2840-9-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sönnichsen AC, Rinnerberger A, Url MG et al. . Effectiveness of the Austrian disease-management-programme for type 2 diabetes: study protocol of a cluster-randomized controlled trial. Trials 2008;9:38 10.1186/1745-6215-9-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Griffin SJ, Borch-Johnsen K, Davies MJ et al. . Effect of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with type 2 diabetes detected by screening (ADDITION-Europe): a cluster-randomised trial. Lancet 2011;378:156–67. 10.1016/S0140-6736(11)60698-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Deeks JJ, Higgins JP, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JP, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 510 [updated March 2011] The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org. [Google Scholar]
- 48.Knight K, Badamgarav E, Henning JM et al. . A systematic review of diabetes disease management programs. Am J Manag Care 2005;11:242–50. [PubMed] [Google Scholar]
- 49.Norris SL, Nichols PJ, Caspersen CJ et al. . The effectiveness of disease and case management for people with diabetes. A systematic review. Am J Prev Med 2002;22:15–38. 10.1016/S0749-3797(02)00423-3 [DOI] [PubMed] [Google Scholar]
- 50.de Bruin SR, Heijink R, Lemmens LC et al. . Impact of disease management programs on healthcare expenditures for patients with diabetes, depression, heart failure or chronic obstructive pulmonary disease: a systematic review of the literature. Health Policy 2011;101:105–21. 10.1016/j.healthpol.2011.03.006 [DOI] [PubMed] [Google Scholar]
- 51.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA 2002;288:1909–14. 10.1001/jama.288.15.1909 [DOI] [PubMed] [Google Scholar]
- 52.International Diabetes Federation. IDF Diabetes Atlas. 6th edn Brussels, Belgium: International Diabetes Federation, 2013. http://www.idf.org/diabetesatlas. [Google Scholar]
- 53.International Diabetes Federation . IDF Diabetes Atlas . 7th edn Brussels, Belgium: International Diabetes Federation, 2015. http://www.idf.org/diabetesatlas. [Google Scholar]
- 54.Inzucchi SE, Bergenstal RM, Buse JB et al. . Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140–9. 10.2337/dc14-2441 [DOI] [PubMed] [Google Scholar]
- 55.Gaede P, Lund-Andersen H, Parving HH et al. . Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580–91. 10.1056/NEJMoa0706245 [DOI] [PubMed] [Google Scholar]
- 56.Berwick DM. The science of improvement. JAMA 2008;299:1182–4. 10.1001/jama.299.10.1182 [DOI] [PubMed] [Google Scholar]
- 57.Busetto L, Luijkx KG, Elissen AM et al. . Context, mechanisms and outcomes of integrated care for diabetes mellitus type 2: a systematic review. BMC Health Serv Res 2016;16:18 10.1186/s12913-015-1231-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Inzucchi SE, Bergenstal RM, Buse JB et al. . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–79. 10.2337/dc12-0413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Davidoff F, Batalden P, Stevens D et al. . Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ 2009;338:a3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Flamm M, Winkler H, Panisch S et al. . Quality of diabetes care in Austrian diabetic patients willing to participate in a DMP - at baseline. Wien Klin Wochenschr 2011;123:436–43. [DOI] [PubMed] [Google Scholar]
- 61.Frei A, Herzog S, Woitzek K et al. . Characteristics of poorly controlled Type 2 diabetes patients in Swiss primary care. Cardiovasc Diabetol 2012;11:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-013076supp1.pdf (77.9KB, pdf)
bmjopen-2016-013076supp2.pdf (20.2KB, pdf)
bmjopen-2016-013076supp_figures.pdf (272.6KB, pdf)
bmjopen-2016-013076supp3.pdf (17.1KB, pdf)