Abstract
The Médecins Sans Frontiérs (MSF) established basic occupational health services to diagnose and treat work-related diseases among tannery, metal, plastics and garment workers and families in one of the more polluted areas of the world populated by 600 000 people. In spite of project limitations, an analysis of the 6-month data showed that of the original cohort of 5000, 3200 (64%) came for at least 1 consultation. Among them, 468 (14.6%) were diagnosed with suspected work-related diseases as per defined protocols. Follow-up consultation was performed for 1447 cases of occupational diseases and work-related injuries. The MSF experience begs the need for replication of such services in densely populated urban areas in developing nations like Bangladesh and India, where no specialty occupational health clinics exist in primary care but are desperately needed and where occupational health clinics on factory premises are exclusive to industry workers and are not accessible to communities.
Case presentation
The unique Médecins Sans Frontiérs Occupational Health Project in Kamrangirchar and Hazaribagh, Dhaka.
Médecins Sans Frontiérs (MSF) is an international humanitarian organisation started in 1971 and works in areas burdened by natural disasters and large-scale human conflicts in 70 countries.1 Though the mandate of MSF is primarily surgery, it has recently expanded its operations into acute emergencies during massive outbreaks of diseases like HIV/AIDS, cholera, malnutrition and Ebola.1
MSF has been working in Hazaribagh and Kamrangirchar since 2012,2 and designated those locations as a man-made disaster areas. Hence, they decided to intervene to provide basic healthcare to the suffering population. While the mandate of MSF is to provide medical assistance to people in disaster situations like earthquakes and war, this marks the first time they have intervened in an area for reasons other than natural disasters or war. The reason for this intervention developed from the widespread industrial negligence and apathy of owners of tanneries and other hazardous material factories towards a largely migrant population of ∼600 000 labourers with no government health service. After 40 years of service as an impartial humanitarian medical charity, MSF began providing basic occupational health services (BOHS).
The workers' plight in Bangladesh is similar to the plight of those working in other developing economies such as India. The Rana Plaza disaster, in which thousands of garment worker women were restrained like slaves and either died or became disabled, is a microcosm of how labourers and their families are exposed to extreme risks in their environment.3 Migrant labourers and their families stream into the city of Dhaka daily to work in one of the more toxic hotspots of the world at Kamrangirchar–Hazaribagh (see figures 1–6).4 5
Figure 1.

Workers without personal protective equipment immersed in a tank full of chemicals during the process of tanning at the Hazaribagh tanneries, Dhaka.
Figure 2.

Workers handling raw leather treated with chemicals at the Hazaribagh tanneries, Dhaka.
Figure 3.

A tank in one of the tanneries of Hazaribagh, Dhaka, contains a conglomerate of chemicals.
Figure 4.

A child metal worker is exposed to toxic metal dust in Kamrangirchar, Dhaka.
Figure 5.

Women plastic workers with no protective equipment rinse plastic materials in acid.
Figure 6.

Workers with no protective equipment process the waste from the tanneries as poultry feed.
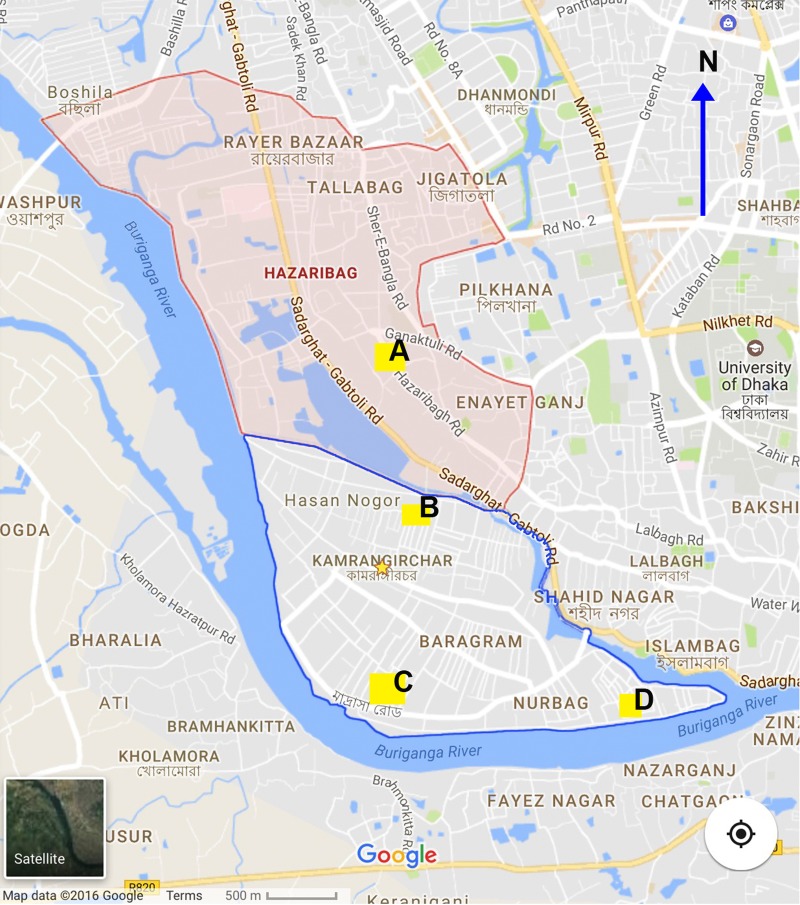
MSF provided diagnosis and treatment services to the cohort of 5000 workers in a BOHS situated in the community. Four main clinics were located in the centre of a community tied to tannery, plastics, garment and metal factories (see figure 7). The selection was equally divided among the 4 industries with 1250 each from the tannery, garment, metal and plastics industries. The criteria were the willingness of the owner to use the MSF health facilities and allow the worker 30 min during the day for a health consultation. The diagnosis, treatment and investigations were free. Investigations were contracted out to a local laboratory. Secondary and tertiary level treatment was by referral to public hospitals in Dhaka, and any expenses incurred from this are reimbursed. A basal chest X-ray, complete blood counts and renal and liver function tests were performed for all the workers present for consultations. The staff (total 80) consisted of 6 doctors, 14 nurses, 34 outreach workers (ORWs), 4 laboratory assistants, 15 registers and 6 cleaners headed by an international expert in occupational medicine. We conducted training in occupational medicine every week for all the staff. The training consisted of hands-on training (eg, audiometer), didactics lectures, field visits, and case presentations and discussions. The initial diagnosis was made by the expert, and follow-ups were performed by the other doctors and nurses using the same criteria.
Figure 7.
Hazaribagh (red outline) and Kamrangirchar (blue outline). The locations of the clinics and the main industries they serve are (A) Hazaribagh, tannery; (B) Aminbagh, garments; (C) Huzurpada, metals and plastics; and (D) Thoda, plastics and metals.
Global health problem list
Industry workers and their families in developing countries suffer work-related diseases, trauma and death in the tannery, metal, plastics and garment industries.
There are no specialty occupational health clinics in primary care in these areas, leaving workers and family members at risk for work-related diseases, trauma and accidents to go without treatment for the adverse effects of industrial operations.
Global health problem analysis
Global statistics
Authors of the global report of empirical assessments of the causes of death state that there are no authentic data available from India, and, hence, the mortality and morbidity cannot be computed with accuracy.6 Reliable country-wide data on occupational diseases are not available from most of the countries of the world.7 Hence, it is not surprising that there are no authentic data on the number of work-related diseases and accidents in India. Nevertheless, many authors have attempted to extrapolate small studies into larger, national-level data which is fraught with uncertainties and underestimates.7–10 In India, it is estimated that there are ∼20 million occupational diseases with an estimated 1 million deaths resulting from disease. It is also estimated that there are ∼17 million occupational accidents with 50 000 accident-related deaths each year in India.7 9 Similarly, another study extrapolating data from Thailand calculated that 11.47% of mortality from injuries are due to work-related trauma. The study concluded that, of the working population of the world (∼3 billion), 3.5 years of healthy life is lost per 1000 workers. The authors of that study believe the results are an underestimation of actual mortality.11 Ten million people are affected by mining activities in India.10 Infants and children are brought to the site by their mothers, exposing developing lungs to hazardous dust. The families live close to the mines, leading to silicosis and tuberculosis due to primary and secondary exposure. The nearest health facility is many miles away. In summary, the majority of people in the community are workers and family members who are at risk of work-related diseases and accidents. To the best of my knowledge, India does not have a dedicated specialised occupational health clinic established in a primary care setting.
Risk factors
Risk factor assessment on a global scale is severely limited; even in developed countries, data are available only for a limited number of diseases.12 The WHO report did not estimate the vast population of workers in the informal sector (eg, workers under age 14) in developing countries like India. Nevertheless, the report provides insight into the risk factors affecting half of the worlds' working population. Of the nearly 100 occupational diseases classified in the International Classification of Diseases (ie, ICD-10), the report provided insight into the contribution of work-related risk factors for the following major occupational diseases: low back pain (37%), work-related asthma (11%), hearing loss (16%), chronic obstructive pulmonary disease (COPD; 13%), lung cancer (9%) and leukaemia (2%).12 The main cause of death due to occupational risk was injury (41%), followed by COPD (40%), and lung cancer (13%).12 The WHO report estimated that occupationally acquired lung cancer comprises 10.3% and leukaemia comprises 2.4% of all cancers.13 A WHO report on environmental risk contribution to neuropsychiatric diseases based on the opinions of 100 experts showed that 13% of risk fraction is associated with migraine, Parkinson's disease, Alzheimer's disease, depression, epilepsy and migraine.14
In summary, the majority of workers and families living in developing communities are at risk from developing diseases and injuries due to occupational and environmental exposures. Most of them live in crowded urban communities and develop work-related diseases or suffer unintentional injuries related to their occupations.
Kamrangirchar and Hazaribagh urban slums, Dhaka.
Kamrangirchar is not officially part of Dhaka city but is an urban slum with a population of around 600 000 people with no government structures.2 Hazaribagh has around 250 tanneries which are 30–35 years old and discharge 6000 m3 of toxic effluents and 10 t of solid waste daily.15 WHO reports that 90% of the workers and families living there die within 50 years of age, suffering from diseases of occupation and environmental toxicity, including chronic dermatological and lung diseases.16 Apart from heavy metals like chromium, cadmium, lead and mercury, a conglomerate of chemicals are discharged by the tanneries into the environment. Workers aged 8 and older are soaked to the skin, breathing the fumes for most of the day and eat and live in these surroundings throughout the year. Personal protective equipment are not provided (figures 1–2 and 4–6).The main chemical exposures are formaldehyde, hydrogen sulfide, sulfuric acid, ammonium sulfates, ammonia, sodium chlorite, sodium chloride, non-ionic wetting agents, waxes, dyes, emulsions, pigments, binders and liquors (figures 1–3). Solid waste from the tanneries are processed as poultry feed (figure 6).15 17
The other major industries in Kamrangirchar are plastic recycling, garments and metals. In these, there are complex risk hazards from cotton dust, heavy metals, and chemicals like mercury, phthalates, acids, and dioxins, and ergonomic hazards (figures 4 and 5). The major risk factors are listed in table 1. Medical care is provided by pharmacies and a few non-governmental organisations. From 2013 to 2015, MSF mapped the area and decided to treat a dedicated cohort of 5000 workers. They appointed an international expert to plan, organise and run the project in June 2015.
Table 1.
Major risk factors and work-related diseases*
| Industry | Hazards | Work-related disease |
|---|---|---|
| Tannery | Chromium, sodium sulfite and basic chromium sulfate including non-ionic wetting agents, bactericides, soda ash, CaO, ammonium sulpfide, ammonium chloride and enzymes. Others are sodium bisulfate, sodium chlorite, NaCl, H2SO4, formic acid, sodium formate, sodium bicarbonate, vegetable tannins, syntans, resins, polyurethane, dyes, fat emulsions, pigments, binders, waxes, lacquers and formaldehyde | Injury, contact-dermatitis, work-related asthma, reactive airway dysfunction syndrome due to acute inhalation of chemicals, acute and chronic effects of chemicals |
| Plastic recycling | Hydrogen chloride, formaldehyde, styrene, acrolein, acetone, phenol, butadiene, other alkanes and alkenes, bisphenol A, butane, cadmium, phthalates, mercury, lead dioxins, polyvinyl chloride, heat, electric shock | Injury, work-related asthma, acute and chronic effects of chemicals |
| Metal | Noise, aluminium, copper, lead, iron, heat, chromium, asbestos, electric shock, light, heat and ionising radiation | Injury, noise-induced hearing loss, corneal injury, blindness, metal fume fever, acute and chronic effects of metals |
| Garment | Cotton, noise, dyes and chemicals used in printing | Injury, byssinosis, noise-induced hearing loss, acute and chronic effects of chemicals |
*Ergonomic factors due to cramped, dimly lit spaces, wet floors, absent ventilation, a lack of toilet and water, long hours of work and food contamination are common hazards to all the four categories of work listed in the table. Moreover, specific hazard depends on the type of raw material used in plastic recycling and metal scraps in metal work processes.
Outreach workers
ORWs are very important in primary care.18 They played an important role in the MSF project in enabling labourers to seek medical help for acute and chronic work-related diseases.
Nurses and doctors
Like in India, there is no formal postgraduate teaching in environmental and occupational health for nurses and doctors in Bangladesh. Moreover, bias exists in not being able to diagnose an occupational disease.19 They need training on a daily basis, and the work-related disease diagnosis and treatment needs to be validated. More importantly, the nurses and doctors need to visit the workplace to understand that work-related disease correlates occupation. Even nurses and doctors working in this hazardous environment can develop industry-specific diseases.20
Equipment and medicines
Audiometers and spirometers needed to be procured and installed, and protocols needed to be developed. While there are no special medications for work-related diseases, doctors needed clear protocols for treatment. For example, if physicians did not diagnose conjunctivitis as allergic and work-related, they might treat the condition with antibiotic eye drops instead of antihistamines.
Diagnostic criteria
The suspected work-related diseases are the ones listed in the US Department of Labour, Occupational Safety and Health (OSH) classification and in the International Classification of Diseases, work-related diseases (ICD 10).21 22 Lung diseases were diagnosed based on work history, clinical history, associated morbidity (especially tuberculosis) and symptoms and signs including the presence of Rhonchi in suspected occupational asthma, medications history (including relief of symptoms from bronchodilator use).23 24 PFT is needed for confirmation. Skin diseases were diagnosed by work history, inspection, palpation and temporary relief with treatment. Patch tests were not performed due to the infeasibility to isolate the offending chemical(s), and they can potentially cause an irritant reaction for which the worker needs cessation from exposure. Moreover, the aim of a patch test is to treat the person with avoidance of further exposure which is not an option for the worker. He will continue to work 7 days a week, 365 days a year until death or disability. Allergic conjunctivitis, allergic rhinitis, lower back pain and irritable bowel disease were diagnosed by standard guidelines.25–28 Injuries were recorded in a separate proforma and treated accordingly. Peptic disease was diagnosed based on classical symptoms of epigastric pains relieved or aggravated by food and/or signs of epigastric tenderness. Malaise and pruritus were diagnosed after a detailed occupational history and basic investigations to rule out comorbidities. The noise-induced hearing loss was diagnosed on occupational history and by an audiometry showing classical bilateral sensorineural deafness.29
Results
Diagnoses of work-related disease started emerging after 6 months. The collated data at the 6-month mark showed that 3200 (64%) of the original cohort of 5000 had come for consultation. Among the 3200 workers who were consulted, 2843 were men, and 357 were women. Female workers came from the plastic and garment industries only. Workers do not possess birth certificates and do not know their exact age. Moreover, child workers are told by the management to report their ages as 14 to escape legal issues. Therefore, the entries of age in the database are not accurate.
Of the original cohort of 5000, 3200 (64%) came for at least 1 consultation. Among them, 468 (14.6%) were diagnosed with suspected work-related diseases, and 30 (0.9%) had work-related injuries. Follow-up consultation was performed for 1447 cases of occupational diseases and work-related injuries. The audiometer and spirometer arrived during the last month of the 6-month period. The clinics were open only 4 days in a week and only during regular working hours. If the clinics were open every day and available during after-work hours, the number of cases diagnosed as work-related would likely be higher. Nevertheless, the above data show that, in a cohort of working people in a dense urban community, there would be many occupational injuries and/or diseases that need to be treated at primary care. The number of cases diagnosed as work-related should positively correlate with increased and focused work by ORWs, daily available clinic hours, access to the clinic during non-industry working hours and further training of nurses and doctors. The diseases diagnosed and treated at the clinic are shown in table 2, which shows the major diseases are contact dermatitis, work-related asthma, peptic disease, low back pain, malaise and injuries. The majority of the cases of contact dermatitis were from the tannery (72%). Occupational asthma was mainly detected in the plastics (40%) and tannery (45%) workers. Since the audiometer only arrived in the final month of the period analysed, the number is small; the two cases noted were from the garment industry.
Table 2.
Suspected work-related diseases (6 months) from November 2015 to April 2016
| Work-related disease | New | Follow-up | Total (n) |
|---|---|---|---|
| Noise-induced hearing loss | 2 | 0 | 2 |
| No disease | 4 | 58 | 62 |
| Peptic disease | 85 | 299 | 384 |
| Work-related asthma | 28 | 144 | 172 |
| COPD | 4 | 0 | 4 |
| Allergic rhinitis | 15 | 30 | 45 |
| Contact dermatitis | 99 | 294 | 393 |
| Contact urticaria | 2 | 20 | 22 |
| Folliculitis and acne | 6 | 19 | 25 |
| Pruritus | 49 | 56 | 105 |
| Tendonitis | 0 | 1 | 1 |
| Low back pain | 59 | 243 | 302 |
| Allergic conjunctivitis | 3 | 11 | 14 |
| IBS | 0 | 3 | 3 |
| Malaise | 82 | 158 | 240 |
| Injuries | 30 | 111 | 141 |
| Total | 468 | 1447 | 1915 |
Basic occupational health service.
COPD, chronic obstructive pulmonary disease; IBS, irritable bowel syndrome.
The above data show that work-related diseases are common in a densely populated urban community and need a specialised clinic within the context of primary care to correctly diagnose and treat such diseases. The WHO established and outlined the standard BOHS in 2005.30 In India as well as in Bangladesh, there are no specialised occupational health clinics in the primary care setting.8 31 The concept of BOHS is exemplary in its simplicity. Briefly, BOHS integrated in the primary care setting should be financed by the public sector and provided to all working people in the community irrespective of the type or location. The MSF experience also highlights the importance of providing these services for labourers' families whose lives are interlinked with work and the environment.32
Learning points.
Work-related diseases and accidents frequently occur among workers and families in densely populated urban communities in developing countries like Bangladesh and India, where the majority of work is informal, and the entire population is exposed to multiple hazards at the workplace and from exposure to the environment.
Basic occupational health services (BOHS) integrated into the primary healthcare setting will benefit workers and families by diagnosing and treating occupational diseases at a clinic situated within the community.
BOHS is to be provided to all workers and their families irrespective of the type and location of the work. BOHS should be financed by the public sector and integrated into the primary healthcare structure.
Much needed data on occupational diseases and accidents will be generated at the community level.
Acknowledgments
The author wish to acknowledge all members of the team. MSF administrators: Emily, Andrea and Flavia; OH Medical Doctor: Shifa Mahjebin; OH Nurses: Masudur Rahman, Sayfur Rahman, Md. Shafiq, Md. Billal, Wazedul Islam Tushar, Shuvashish Das Bala, Noor Mohammad, Kimi Chakma, Amena Khatun and Samir Chandra; OH registrars: Kaniz runa, Fatema Shila and Masud Kaisar; OH Cleaners: Rukhsana, Shumon, Marzina and Rekha; OH Outreach Workers: Manimoy, Tushar, Fateema and others.
Footnotes
Contributors: VM worked with MSF in Dhaka as an MD from June 2015 to June 2016. VM saw all the cases and validated them as occupational disease. VM analysed the data, made tables and wrote the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Chu K, Rosseel P, Trelles M et al. Surgeons without borders: a brief history of surgery at Medecins Sans Frontieres. World J Surg 2010;34:411–14. 10.1007/s00268-009-0187-z [DOI] [PubMed] [Google Scholar]
- 2.Ali E, Zachariah R, Shams Z et al. Is mid-upper arm circumference alone sufficient for deciding admission to a nutritional programme for childhood severe acute malnutrition in Bangladesh? Trans R Soc Trop Med Hyg 2013;107:319–23. 10.1093/trstmh/trt018 [DOI] [PubMed] [Google Scholar]
- 3.Hobson J. To die for? The health and safety of fast fashion . Occup Med 2013;63:317–19. 10.1093/occmed/kqt079 [DOI] [PubMed] [Google Scholar]
- 4.Al Amin MM. Factors behind internal migration and migrant aspects internal migrant's livelihood aspects [Master program in economic demography] Dhaka City, Bangladesh. Lund, Sweden: Lund University. School of Economics and Management, Department of Economic History, 2010. [Google Scholar]
- 5. Bangladesh's toxic tanneries turning a profit at an intolerable human price. http://www.theguardian.com/global-development/2012/dec/13/bangladesh-toxic-tanneries-intolerable-human-price.
- 6.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–71. 10.1016/S0140-6736(14)61682-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leigh J, Macaskill P, Kuosma E et al. Global burden of disease and injury due to occupational factors. Epidemiology 1999;10:626–31. 10.1097/00001648-199909000-00032 [DOI] [PubMed] [Google Scholar]
- 8.Pingle S. Basic occupational health services. Indian J Occup Environ Med 2009;13:1–2. 10.4103/0019-5278.50715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saiyed HN, Tiwari RR. Occupational health research in India. Ind Health 2004;42:141–8. 10.2486/indhealth.42.141 [DOI] [PubMed] [Google Scholar]
- 10.Murlidhar V. An 11-year-old boy with silico-tuberculosis attributable to secondary exposure to sandstone mining in central India. BMJ Case Rep 2015;2015:pii: bcr2015209315 10.1136/bcr-2015-209315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Concha-Barrientos M, Nelson DI, Fingerhut M et al. The global burden due to occupational injury. Am J Ind Med 2005;48:470–81. 10.1002/ajim.20226 [DOI] [PubMed] [Google Scholar]
- 12.Concha-Barrientos M. Chapter 21: Selected occupational risk factors. In: Ezzati M, Lopez A, Rodgers A et al., eds. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organisation, 2004:1651. [Google Scholar]
- 13.2002. The world health report 2002—reducing risks, promoting healthy life. http://www.who.int/entity/whr/2002/en/whr02_en.pdf?ua=1.
- 14.2006. Preventing disease through healthy environments: towards an estimate of the environmental burden of disease. http://www.who.int/quantifying_ehimpacts/publications/preventingdisease.pdf.
- 15.Azom M, Mahmud K, Yahya S et al. Environmental impact assessment of tanneries: a case study of Hazaribag in Bangladesh. Int J Environ Sci Dev 2012;3:152–6. 10.7763/IJESD.2012.V3.206 [DOI] [Google Scholar]
- 16.Maurice J. Tannery pollution threatens health of half-million Bangladesh residents. Bull World Health Organ 2001;79:78–9.11217673 [Google Scholar]
- 17.Islam GM, Khan FE, Hoque MM et al. Consumption of unsafe food in the adjacent area of Hazaribag tannery campus and Buriganga River embankments of Bangladesh: heavy metal contamination. Environ Monit Assess 2014;186:7233–44. 10.1007/s10661-014-3923-2 [DOI] [PubMed] [Google Scholar]
- 18.Roodenbeke ED, Lucas S, Rouzaut A et al. Outreach services as a strategy to increase access to health workers in remote and rural areas. Geneva: World Health organisation (WHO), 2011. [PubMed] [Google Scholar]
- 19.Murlidhar V. Occupational health physicians: unwilling or unable to practise ethically. Indian J Med Ethics 2002;10:26. [Google Scholar]
- 20.Murlidhar V. Occupationally acquired asbestosis in a healthcare worker. BMJ Case Rep 2015;2015:pii: bcr2015211670 10.1136/bcr-2015-211670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karjalainen A. International statistical classification of diseases and related health problems (ICD-10) in occupational health. Geneva: World Health Organisation, 1999. [Google Scholar]
- 22.United Department of Labour. Occupational injury and illness classification manual. Washington, DC: US Bureau of Labor Statistics, 2014. [Google Scholar]
- 23.Murlidhar V, Kanhere V. Asbestosis in an asbestos composite mill at Mumbai: a prevalence study. Environ Health 2005;4:24 10.1186/1476-069X-4-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murlidhar V, Murlidhar VJ, Kanhere V. Byssinosis in a Bombay textile mill. Natl Med J India 1995;8:204–7. [PubMed] [Google Scholar]
- 25.Longstreth GF, Thompson WG, Chey WD et al. Functional bowel disorders. Gastroenterology 2006;130:1480–91. 10.1053/j.gastro.2005.11.061 [DOI] [PubMed] [Google Scholar]
- 26.Greiner AN, Hellings PW, Rotiroti G et al. Allergic rhinitis. Lancet 2016;378:2112–22. 10.1016/S0140-6736(11)60130-X [DOI] [PubMed] [Google Scholar]
- 27.Bielory L, Lien KW, Bigelsen S. Efficacy and tolerability of newer antihistamines in the treatment of allergic conjunctivitis. Drugs 2005;65:215–28. 10.2165/00003495-200565020-00004 [DOI] [PubMed] [Google Scholar]
- 28.Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332:1430–4. 10.1136/bmj.332.7555.1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murlidhar V, Kanhere V. Occupational noise-induced hearing loss: the first two cases compensated in India. Natl Med J India 1998;11:150. [PubMed] [Google Scholar]
- 30.Rantanen J. Basic occupational health services. 3rd edn Helsinki: ILO/WHO/ICOH collaboration: Finnish Institute of Occupational Health, 2007. [Google Scholar]
- 31.Tasnim F, Rahman I, Rahman M et al. A review on occupational health safety in Bangladesh with respect to Asian Continent. Int J Pub Health Safe 2016;1:102. [Google Scholar]
- 32.Rantanen J. Basic occupational health services, their structure, content and objectives. SJWEH Suppl 2005;1:5–15. [Google Scholar]