Abstract
Colonoscopy is being widely used since the 1980s and is the leading diagnostic procedure for colorectal cancer. For many colorectal diseases, it is also a therapeutic tool. Like many other procedures in Medicine, it has its drawbacks and complications, some of which if not readily diagnosed can represent a serious risk to the patient's health and well-being. We describe a case of colon perforation during diagnostic colonoscopy in a patient, resulting in exuberant pneumoretroperitoneum, pneumoperitoneum, pneumomediastinum and subcutaneous emphysema, who successfully underwent laparoscopic colonic resection with primary anastomosis. There are only a few cases of combined intraperitoneal and retroperitoneal perforations described in the literature.
Background
Colonoscopy is the standard of care for screening of colorectal cancer (CCR) in patients over the age of 50.
It is no longer just a screening procedure; it has become a therapeutic option for many diseases, such as resection of neoplastic lesions, stenting of leaks, strictures and obstructions. Even surgery is nowadays doable through natural orifices due to endoscopy.1
Although the procedure is considered relatively safe,2 3 bleeding and especially perforation1 are the main complications, the latter being more common in therapeutic than in diagnostic procedures.
For the clinician in the emergency department (ED), it is extremely important to be aware of such complications and of its management possibilities.
Case presentation
A woman aged 73 years was brought to the ED within a few hours after a screening colonoscopy was performed in a private clinic. She had a known history of laparoscopic cholecystectomy and a family history of CCR, which led to her being submitted to uneventful colonoscopy with polypectomy 4 years before.
The attending surgical team immediately approached the patient who was calm and oriented, haemodynamically well and afebrile. She had no dyspnoea, despite having crepitus on palpation of the neck and abdominal wall. Her abdomen was slightly distended and painful, but she had no rebound tenderness.
According to the information from the gastroenterology consultant, although the colonic preparation was good, the colonoscope was introduced only 40 cm due to technical difficulties. At about 20 cm of the anal verge, the doctor suspected of perforation and sent the patient to the ED.
Investigations
Laboratory findings were within normal range.
A thoracic–abdominal–pelvic CT was requested and performed before and after using an intravenous contrast. An exuberant pneumoretroperitoneum was noted dissecting all the extraperitoneal spaces: from the abdomen to the pelvis, throughout the mediastinum. In addition, the muscles from the neck, scapula, thorax, abdomen and inguinal regions were also dissected. There was also pneumoperitoneum even though there was no free or collected fluid. The location of the perforation was not clear (figures 1–3).
Figure 1.
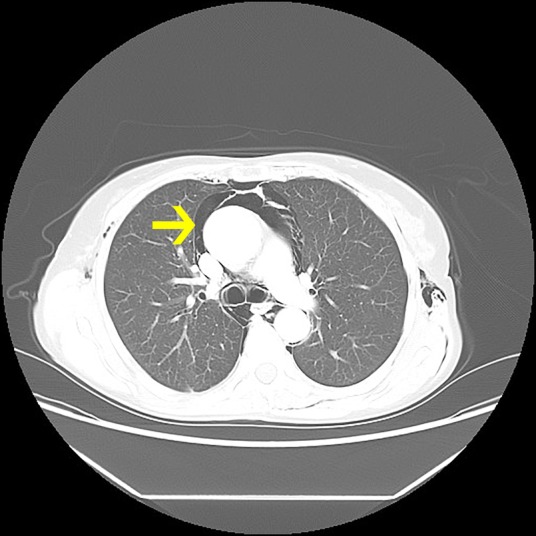
CT thoracic section. The arrow shows pneumomediastinum.
Figure 2.
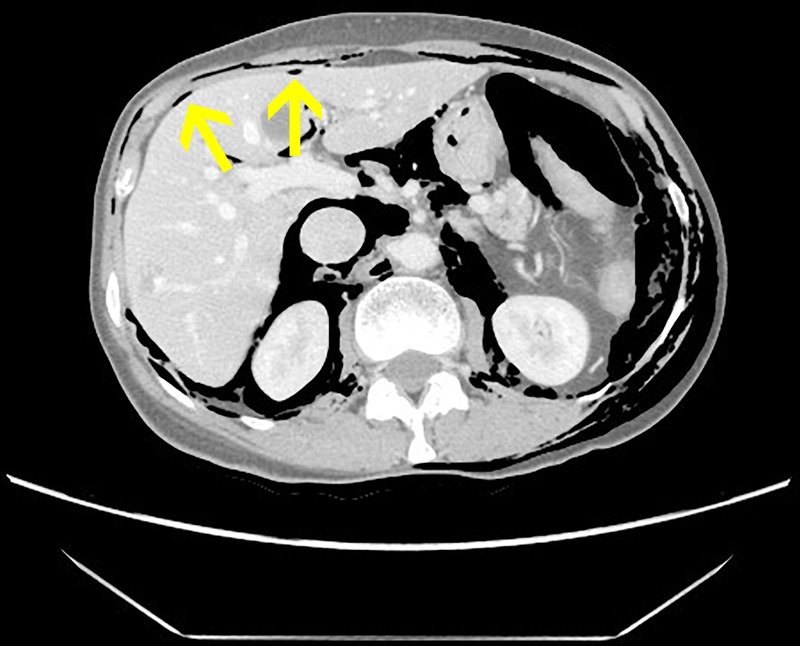
CT abdominal section. Arrows show pneumoperitoneum above the liver.
Figure 3.
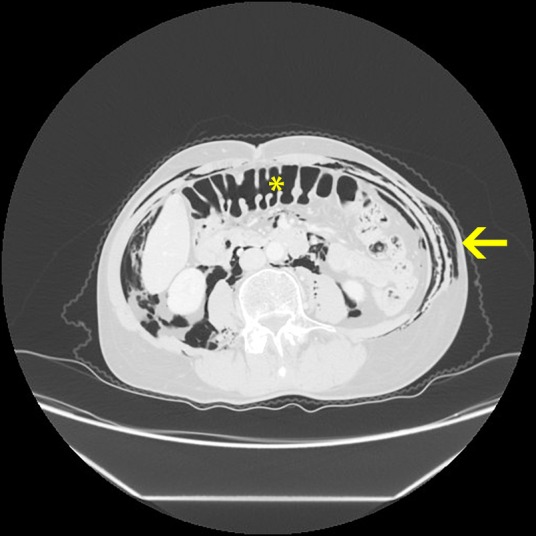
CT abdominal section. *Inflated colon; the arrow shows the dissected abdominal wall.
Treatment
The patient was proposed for emergency surgery and signed the informed consent.
The surgical team decided to perform a diagnostic laparoscopy. The perforation on the sigmoid wall appeared to be about 1 cm wide, near to the mesenteric insertion. They did not find free fluid, abscesses or intra-abdominal contamination.
A laparoscopic sigmoidectomy was carried out with primary anastomosis and a subaquatic anastomosis test was performed (figures 4 and 5).
Figure 4.
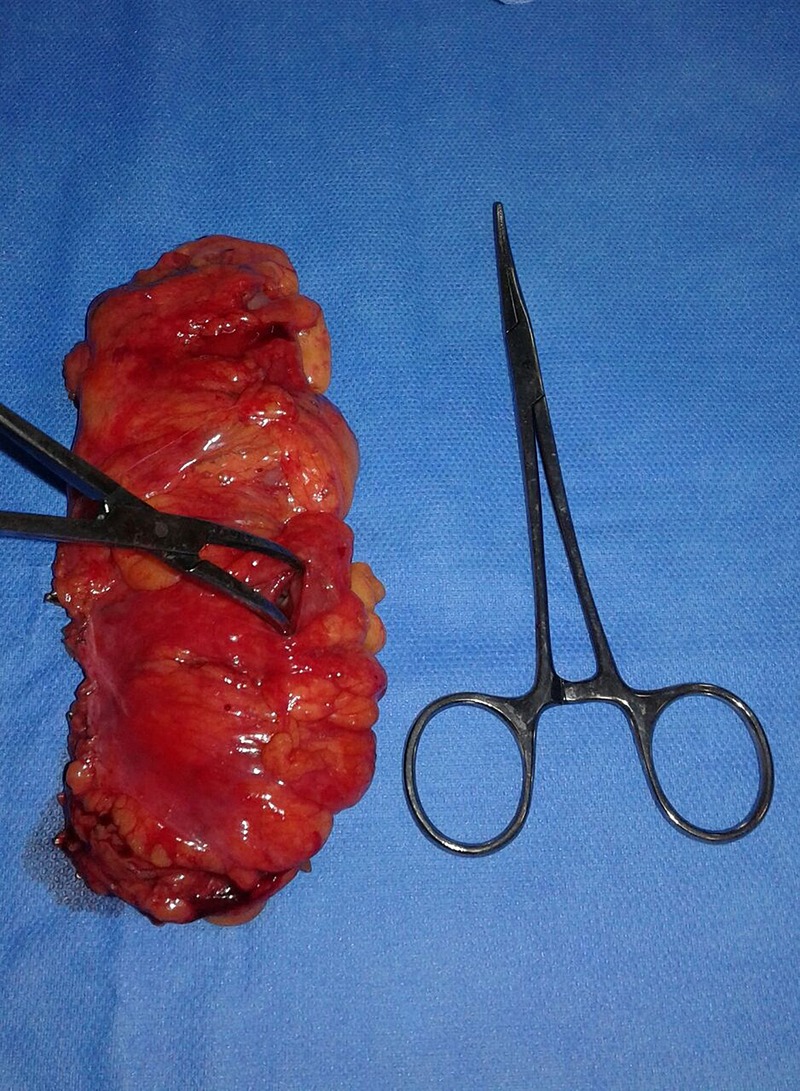
Sigmoid section, forceps inside perforation.
Figure 5.
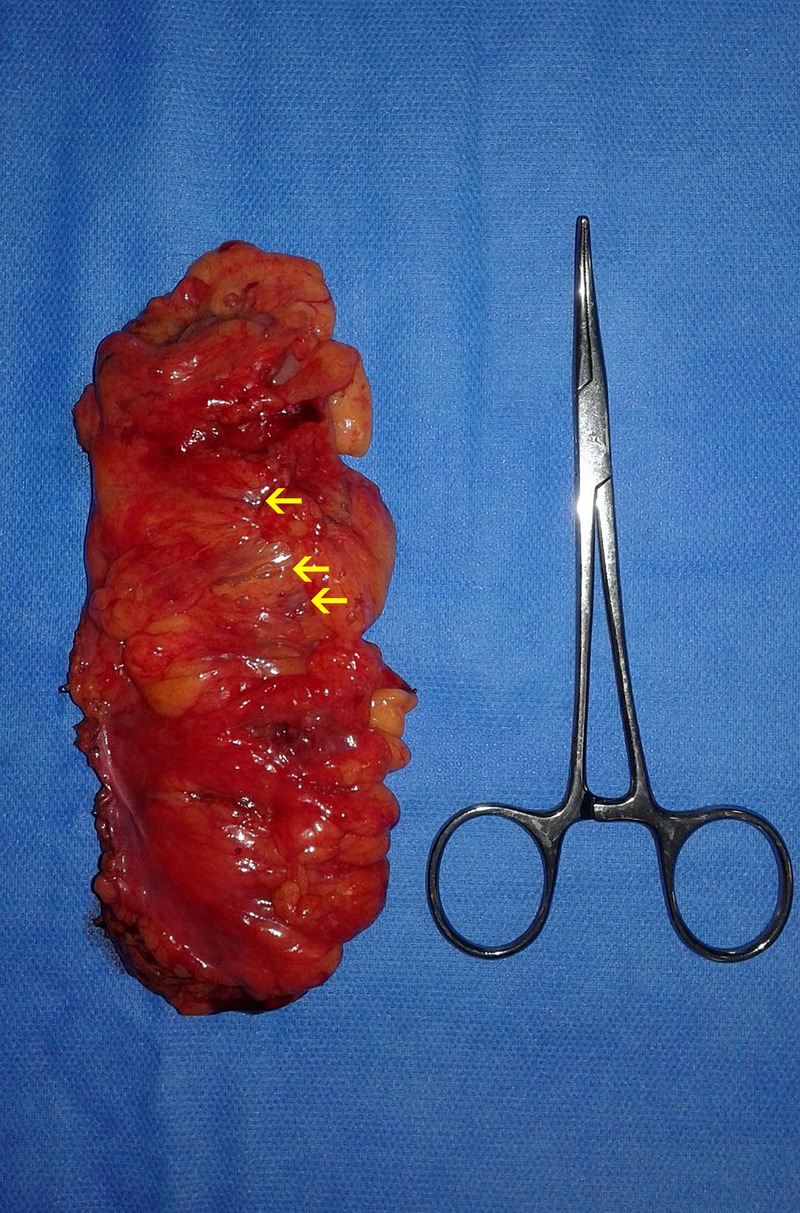
Sigmoid section, the arrow shows air trapped along the mesentery.
During the surgery, the patient was haemodynamically stable.
The anatomopathological examination revealed a sigmoid colon perforation 0.7 cm wide with congestion, transmural inflammatory infiltrate and signs of local peritonitis. The presence of diverticula was not referred.
Outcome and follow-up
The postoperative period was uneventful and the patient was discharged to the outpatient clinic at day 7.
Discussion
Colonic perforation after colonoscopy has been described as having a range of 0.016–5%.4 Several authors seem to agree that complication rates are inferior in diagnostic procedures (<0.5%) versus therapeutic ones, which are associated with a perforation rate of 2–5%.1–5
If undiagnosed, such complications can present with serious threats to patient's life. They are also associated with a high rate of morbidity, such as stoma formation, sepsis and long hospital stays.4
The injuries can happen due to three mechanisms: pneumatic (barotrauma due to inflated air), mechanical (direct trauma with the colonoscope) or as a consequence of the therapeutic procedure itself (polypectomy, stenting, etc). The intraluminal pressure caused by the sharp endoscope or tip manipulation is thought to be responsible for the majority of perforations,2 3 especially if there are kinks or adhesions to the colon.
Perforations due to excess inflation are usually associated with other underlying morbidities, such as diverticulosis or inflammatory intestinal disease. The sigmoid colon seems to be the most common location for perforation, followed by the caecum. The angulation of the sigmoid combined with the presence of diverticula and the fact that the caecum walls are thinner and fragile explain the occurrence of perforation in those locations.
To the best of our knowledge, there are very few cases of colonic perforation after colonoscopy that has resulted in such an exuberant form of ‘all over-the-place-pneumo’ (figure 6). Combined intraperitoneal and extraperitoneal perforations are rare because perforations usually occur in the antimesenteric colonic wall resulting in pneumoperitoneum. In our case, as you can see in the pictures (figure 4), the perforation starts in the mesentery, which explains the retroperitoneal air dissection.
Figure 6.

CT coronal section, arrows show air in the different spaces.
Air passes through the soft tissues of the mesentery, along the vessels and through pneumatosis coli.5 The fascial planes separate into four regions that are common to the neck, thorax and abdomen: previsceral space, visceral space, paravertebral tissue and subcutaneous tissue. If air leaks in one space, it can spread elsewhere.2 3
According to the information from the gastroenterologist and from the anatomopathological examination, the authors think that mechanical injury is the most likely cause in our case.
With our experience in advanced laparoscopic surgery, we decided to carry out diagnostic laparoscopy.
Our patient was an otherwise healthy woman and the time since injury to diagnosis to treatment was <6 hours. The colon was clean, due to preparation for the colonoscopy. She had no clinical signs of sepsis and no contamination of the abdomen was found, the laparoscopic resection and the primary anastomosis seemed to be a suitable approach.
Laparoscopic operations are linked to less morbidity, less hospital stay and better cosmetic results.1 5 However, such approach may not be feasible in every patient who suffers a colonic perforation.
Patients who present with perforations in more than 24–48 hours, with intra-abdominal contamination and signs of sepsis, primary anastomosis may not be feasible and colostomy could be necessary.6
Some patients may actually be managed with a conservative approach,1 4 6 if there are no signs of clinical peritonitis or haemodynamical instability, even in the presence of pneumoperitoneum or retroperitoneum.1 6
Advances in endoscopic techniques have also allowed for management of complications due to endoscopy.6 7 Clipping of colon perforations was first described in the 1990s6 7 and it is now feasible even for large perforations wider than 3 cm.6 An experienced endoscopist is the most important person for clipping closure success and could prevent additional surgery.6 7
There are wide-ranging possibilities for the management of colonoscopy perforations. Treatment must be individualised to the patient and her/his disease, as well as the resources available in the hospitals and clinics.
Learning points.
We describe a rare case of combined intraperitoneal and retroperitoneal perforation after diagnostic colonoscopy.
Contact with the gastroenterologist is important to acknowledge why the procedure was performed, the type of injure, its location and time until diagnosis.
Laparoscopic approach is feasible and safe in the emergency setting depending on the injury characteristics but especially on the patient comorbidities and clinical condition.
Footnotes
Contributors: CB is the senior doctor, responsible for all the decision-making. CS and HC were the surgeons who operated on the patient. AVA was responsible for the data acquisition and writing of the paper.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zinner MJ, Ashley SW. Maingot's abdominal operations. In: Marks JM, Ponsky JL. Endoscopy and endoscopic intervention. 12th edn McGraw-Hill, 2013:31–61. [Google Scholar]
- 2.Dehal A, Tessier DJ. Intraperitoneal and extraperitoneal colonic perforation following diagnostic colonoscopy. JSLS 2014;18:136–41. 10.4293/108680813X13693422521638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park NS, Choi JH, Lee DH et al. Pneumoretroperitoneum, pneumomediastinum, peumopericardium, and subcutaneous emphysema after colonoscopic examination. Gut Liver 2007;1:79–81. 10.5009/gnl.2007.1.1.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lohsiriwat V. Colonoscopic perforation: incidence, risk factors, management and outcome. World J Gastroenterol 2010;16:425–30. 10.3748/wjg.v16.i4.425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marwan K, Farmer KC, Varley C et al. Pneumothorax, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum and subcutaneous emphysema following diagnostic colonoscopy. Ann R Coll Surg Engl 2007;89:W20–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai SL, Chen T, Yao LQ et al. Management of iatrogenic colorectal perforation: from surgery to endoscopy. World J Gastrointest Endosc 2015;7:819–23. 10.4253/wjge.v7.i8.819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mana F, De Vogelaere K, Urban D. Iatrogenic perforation of the colon during diagnostic colonoscopy: endoscopic treatment with clips. Gastrointest Endosc 2001;54:258–9. 10.1067/mge.2001.114959 [DOI] [PubMed] [Google Scholar]


