Abstract
The current climate in healthcare is increasingly emphasizing a value-based approach to diagnostic testing. Cardiac imaging, including echocardiography, has been a primary target of ongoing reforms in healthcare delivery and reimbursement. The Appropriate Use Criteria (AUC) for echocardiography is a physician-derived tool intended to guide utilization in optimal patient care. To date, the AUC have primarily been employed solely as justification for reimbursement, though evolving broader applications to guide clinical decision-making suggest a far more valuable role in the delivery of high-quality and high-value healthcare.
Keywords: Echocardiography, Healthcare policy, Appropriate use
Introduction
The Appropriate Use Criteria (AUC) were developed to guide optimal utilization of a variety of medical procedures for the delivery of high-quality care. Initial AUC focused on cardiac imaging, in response to marked increases in utilization and expenditures on cardiac imaging that had occurred over the last two decades. Echocardiography was a major contributor to this growth and remains the highest volume cardiac imaging test. AUC for echocardiography have now been tested and implemented in a variety of healthcare settings, and utilization trends in cardiac imaging have moderated since the AUC were first introduced. Concurrent with these changes in cardiac imaging, national healthcare reform has begun to shape a value-based approach to healthcare delivery. The purpose of this review is to discuss the role of the Appropriate Use Criteria for echocardiography in a new value-based era of utilization, delivery, and reimbursement.
Changing Trends in Cardiac Imaging Utilization
Medical diagnostic imaging experienced a cumulative growth of 85 % from 2000 to 2009, far exceeding any other physician service [1, 2•]. While not the fastest growing imaging modality, transthoracic echocardiography (TTE) volume nearly doubled in this time period and remains the highest volume cardiac imaging test. This growth garnered widespread concern from governmental and private payers regarding potential misuse or overuse of all cardiac imaging tests and served as the primary impetus for the development of AUC. To this day, these historic trends are referenced in the ongoing debate over healthcare reform.
But as we consider the role of AUC in today’s healthcare climate, it is important to understand the current reality of cardiac imaging utilization. As outlined in the annual Medicare Payment Advisory (MedPAC) reports, medical imaging as defined by procedures performed among Medicare beneficiaries has declined yearly from 2009 to 2013, with an overall 7 % cumulative decrease in volume [1] (Fig. 1). The correction in the utilization of echocardiographic procedures has been even more dramatic, with a 17 % cumulative decline (2009–2013), including a 7 % decline in 2012–2013, the most recent year for which data is available. The reasons for these changes in utilization are assuredly multifactorial. Prior authorization programs implemented by private payers, widespread reimbursement cuts for imaging procedures, and enhanced physician awareness and education about optimal utilization of imaging have all been likely contributors. The development and implementation of AUC have also played a major role, for the first time giving providers a physician-derived resource to guide optimal utilization of imaging tests.
Fig. 1.
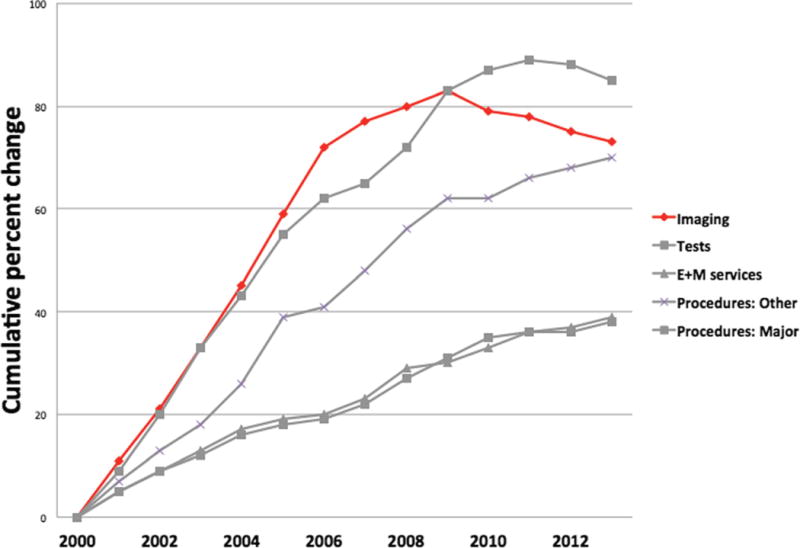
2000–2013 trend in growth of Medicare service for beneficiaries. Cardiac imaging volume trends are depicted in red (adapted from: MedPac Report to Congress: 2015 Medicare Payment Policy Update). Adapted from MedPac Report to Congress: 2015 Medicare Payment Policy Update
Despite the new utilization trends, it is evident that more work needs to be done to optimize imaging utilization. For example, recent reports have shown geographic variations in patterns of ordering echocardiography, as high as an 8.5-fold difference, raising the possibility of geographic pockets of ongoing overutilization of imaging [3]. Factors that may increase the susceptibility to overuse include financial incentives of fee-for-service reimbursement models, cultural factors such as the desire to reassure a patient with a diagnostic test, and concerns over malpractice liability. On the contrary, there may also be instances in which echocardiography is underutilized. In a study by Ballo and colleagues, 16 % of inpatients admitted with a clear indication for echocardiography did not have one performed. Further study will be needed to determine if these represent “missed opportunities” where an echocardiogram may contribute to optimal patient care [4].
In sum, while the era of unfettered growth of cardiac imaging has ended, additional study is needed to fine-tune the optimal utilization of echocardiography and better define its role in a value-based healthcare environment.
AUC in the Era of Value-Based Healthcare
The Affordable Care Act (ACA) was passed in March of 2010, in the midst of rising healthcare expenditures, and it continues to alter the landscape of current clinical care. In the ACA era, the focus has shifted to “value-based” healthcare, in which utilization of individual components requires justifying improvements in patient outcomes and/or demonstrable reductions in cost. Healthcare expenditures and reimbursements are increasingly being “bundled” into global payments for the complete care of a particular disease state or illness, so called episodes of care. For any individual test to be justified in an “episode of care,” it must provide “value” by reducing overall cost or through demonstrable improvements in patient care or health outcomes.
A recent summit convened by the American Society of Echocardiography Foundation sought to address the pending changes in the structure of healthcare payments, with a specific focus on echocardiography. In the proceedings, the trifecta of an ideal healthcare system in this current atmosphere was proposed, underscoring the importance of (a) the achievement of a higher quality of care for the patient population and (b) an improved patient experience while (c) accomplishing all of this at a lower cost [2•]. The pressure to enhance cost-conscious healthcare utilization, particularly within the realm of cardiac imaging, has been hugely emphasized in the media and among governmental and private payers over the last decade. With this attention came fee reimbursement cuts and prior authorization programs, both with the primary intention to constrain the utilization of echocardiography. Concurrently, the physician-derived AUC were developed and released [5]. While most early implementation of the AUC was similarly aimed solely at eliminating overuse of cardiac imaging, this circumscribed application was not the intended purpose of the AUC.
The AUC’s clearly stated aim is “to improve patient care and health outcomes in a cost effective manner [5].” Similarly, value in healthcare is commonly defined as healthcare outcomes achieved per dollar spent. Thus, the initial intended purpose of the AUC was to help define how and when an imaging test could provide the greatest value in optimal patient care. Despite this noble goal, it remains difficult to definitively “prove” the value of an imaging test. Historically, there has been a paucity of evidence that cardiac imaging tests directly improve patient outcomes. More recently, a growing number of studies have demonstrated that the integration of AUC by educational and computer-assisted interventions can help to inform and potentially optimize ordering patterns and downstream patient outcomes.
Development of AUC
The AUC for echocardiography were initially released in 2007 (transthoracic echocardiography) and 2008 (stress echocardiography) and later revised in 2011 in to a comprehensive AUC addressing all echocardiographic procedures [5–7]. The initial 2007 AUC categorized appropriateness by a relative score, with 7 to 9 defined as “appropriate,” 4 to 6 defined as “uncertain,” and 1 to 3 defined as “inappropriate” [6].
The 2011 update broadened the AUC to include 202 clinical indications for transthoracic, transesophageal, and stress echocardiography. Recently, nomenclature has been revised such that the AUC now establish procedures as appropriate, “may be appropriate,” and “rarely appropriate.” The new nomenclature was adopted in an attempt to acknowledge that in rare instances, additional clinical factors not accounted for in the AUC indications may make an echocardiographic procedure reasonable to perform in optimal patient care. Thus, due to the necessary nuances of clinical care, even rarely appropriate studies may occasionally warrant reimbursement.
Early studies of the AUC allowed the first objective description of the appropriateness of the clinical practice of echocardiography and confirmed the AUC’s ability to stratify practice. A prospective evaluation of the 2007 AUC criteria in a university hospital setting demonstrated that in over 1500 studies, 89 % were deemed appropriate, with 89 % of the indications addressed by the AUC [8]. Subsequent investigations of the 2007 AUC in a variety of practice settings identified additional clinical scenarios for which echocardiography is commonly ordered in clinical practice, but that were not covered by the AUC [8, 9].
These “gaps” were addressed by the 2011 revision of the AUC for echocardiography. A study of the 2011 AUC found that it represented a comprehensive summary of echocardiography practice, addressing 98 % of indications for studies in a consecutive cohort of 2000 transthoracic, transesophageal, and stress echocardiograms [10]. A large-scale meta-analysis also demonstrated an improvement in rates of reported appropriateness as a result of the 2011 AUC, with TTE performing among the best among multimodality imaging techniques [11]. These studies helped to establish the AUC as a feasible and representative tool for clinical application.
Rarely Appropriate Echocardiograms
While AUC implementation studies demonstrated the vast majority of echocardiograms performed in clinical practice to be appropriate, they also identified the most common clinical scenarios for which rarely appropriate echocardiograms are ordered. There has been great interest in identifying characteristics of these rarely appropriate studies, so that efforts can be targeted to reduce inappropriate utilization of echocardiography, optimize clinical practice, and constrain costs (Table 1). Factors such as practice setting (community vs. academic) have not been shown to significantly affect appropriateness [12, 13]. Depending on the population studied, physician ordering specialty (cardiologist vs. non-cardiologist) may or may not affect the appropriateness of echo ordering [9]. The two characteristics that are consistently found in the vast majority of rarely appropriate TTEs are outpatient status and repeat studies (Table 1). Outpatient TTEs are less commonly appropriate than are inpatient studies because hospitalized patients generally have new symptoms or a “change in clinical status,” a key feature establishing many AUC indications as “appropriate” [13]. Similarly, repeat TTEs are more likely to be rarely appropriate than first-time TTEs because of the time intervals specified in the AUC for the reevaluation of heart disease to establish appropriateness. For example, the AUC indication addressing routine follow-up of mild valvular heart disease reads “routine surveillance (<3 years) of mild valvular heart disease without a change in clinical status or cardiac exam” [5]. Thus, an echocardiogram performed within 3 years of the prior study would not be appropriate, in the absence of a clinical change. Routine-repeat TTEs to follow up mild heart disease are among the most common rarely appropriate indications for TTE in clinical practice and represent a primary target to optimize utilization.
Table 1.
Most common “rarely appropriate” (formerly termed “inappropriate”) indications for which transthoracic echocardiograms are performed in clinical practice according to the 2011 AUC
|
AUC and Clinical Impact
Justifying the value of an echocardiogram using demonstrable improvements in patient outcomes as the only metric is challenging and oversimplifies the true meaning of a useful diagnostic test in clinical practice. A number of studies have sought to evaluate the value of echocardiography by tracking new abnormalities on the echocardiogram and/or changes in active clinical management. These investigative techniques attempt to establish the “clinical impact” of the echocardiogram, using it as a surrogate for clinical outcomes.
A recent retrospective study of an academic population at UT Southwestern reported that despite an appropriateness rate of 91 %, only 25 % of studies demonstrated a new echo abnormality, with no significant difference in new abnormalities detected between “appropriate” and “rarely appropriate” studies [14•, 15]. This contradicts a prior larger prospective study, in which appropriate studies were found to have significantly more new important echo abnormalities than did inappropriate studies [8]. Furthermore, in the UT Southwestern population, the impact of these findings resulted in active changes in care in less than one third of patients’ clinical courses [15]. A similar study of inpatient TTE published this year showed more promising results, with 48 % of TTE results leading to changes in active management and 20 % of ordering physicians obtaining further studies for diagnostic evaluation [16•]. The inclusion of both active management changes and downstream diagnostic testing is perhaps a more inclusive and realistic measure of the clinical impact of echocardiography.
These studies illustrate the pitfall of focusing on outcome-based studies of AUC in echocardiography, due to the obscuration of the concept of “hidden” (i.e., indirect) clinical value. This could be highlighted by a patient who presents with shortness of breath, for whom an echocardiogram would be a standard and appropriate part of the evaluation. If the TTE is abnormal, then the value of the test is readily apparent. However, if the TTE is unremarkable, it would be expected to prompt additional testing to provide an alternate diagnosis and guide treatment to improve a patient’s symptoms and outcome. This indirect effect of a normal TTE, which leads to the pursuit of other diagnostic testing, is a fundamental step in clinical reasoning and meets every reasonable definition of clinical appropriateness but is not always captured by AUC validation studies which lack downstream clinical decision making as part of the primary outcome.
A recent study performed at our institution attempted to quantify the effect of echocardiography’s “hidden value” in 1525 patients referred for TTE. Clinical indications were assessed by AUC, and a clinical impact score including both direct impact (based upon new TTE abnormalities) and indirect impact (normal or unchanged TTE result prompted further workup or testing) was determined [17]. The majority of appropriate studies were found to have clinical impact, but what was perhaps most striking was that one half of these appropriate studies demonstrated clinical impact, which qualified as indirect.
AUC Versus Practice Guidelines: Different Purpose and Different Goal
While the 2011 revision of AUC has proven successful in its capacity to address a wide spectrum of clinical scenarios, there are limitations worth noting. Critiques of the 2007 and 2011 AUC documents cite that in contrast with the heavily evidence-based format of clinical practice guidelines, the AUC rely more heavily upon consensus and expert opinion, largely due to the limited available evidence on the effect of echocardiography on patient outcomes. However, this criticism belies the differential purpose of the AUC, which are meant to guide clinicians regarding a reasonable scenario for utilization of echocardiography and not impose a rigid definition of the standard of care. A strict implementation of the AUC in clinical decision-making, no matter how comprehensive the indications, may be prohibitive and overlook situations where testing should be considered, even if the impact may be indirect or result in continuation of current care. Furthermore, it can be challenging to glean the true impact of an echocardiogram from the medical record. A good example of this case is the patient undergoing chemotherapy with agents capable of cardiotoxicity; in this scenario, there may be no obvious change in symptomatology, and an unchanged echocardiogram does not obviously change clinical care, but insidious myocardial dysfunction is a feared complication and serial cardiac imaging is required for detection. Any diagnostic test should be weighed with its attendant risk-benefit ratio, but the inherent non-invasive nature of echocardiography may skew toward benefit and result in a lower threshold for obtaining a test.
“Teaching” the AUC: Interventions Used to Improve the Application of AUC
A number of strategies have been incorporated in an effort to improve AUC application in everyday practice. Commonly used methods include echocardiography lab auditing to meet laboratory certification requirements and prior-authorization programs by private payers. More recent educational initiatives and point-of-care ordering algorithms have been reported as successful methods as well, particularly effective at targeting individual practice.
The implementation of an AUC web-based application in one study was an expedient and accurate method to assess the appropriateness of an echocardiogram study [18]. A second VA study showed that the effect of a computerized ordering prompt which provides AUC information did not diminish the rate of TTE ordering in a significant manner, signifying there is opportunity to help guide clinicians without curtailing the ability to order studies [19]. Not surprisingly, a small “rebound” effect was noted following the intervention. Early trends showed small decreases in TTE ordering after intervention but by 6-month rates and ordering returned to preintervention levels. This may suggest some initial resistance to AUC prompts by ordering providers, which dissipate quickly over time. An advantage of these types of applications has been the ability to incorporate the AUC to not just determine the appropriateness of echocardiography as a diagnostic test but also to integrate myocardial perfusion studies (MPS) and coronary computed tomography angiography (CCTA) to help clinicians identify the optimal test for the individual patient at the time of care. There is a suggestion that clinical decision-making support tools can increase the relative proportion of several different imaging tests designated as appropriate, even within a year of implementation [20, 21]. This could also fulfill a role as an additional quality improvement measure, while helping to streamline utilization of noninvasive imaging techniques [22].
A number of educational studies have been reported in the outpatient and inpatient setting, with mixed results. Two educational interventions at the same center employed a combination of a lecture on the 2011 AUC for TTE, a pocket card for guidance on the application of AUC to various clinical situations, and biweekly feedback on individual ordering behavior and followed the ratio of appropriate to inappropriate studies ordered. Both studies used a control group and found that the house staff improved their rates of appropriate echocardiogram ordering as a result of the educational initiatives [23, 24]. A current multicenter randomized controlled trial of an AUC-based educational intervention is underway in the Echo Will Inappropriate Scenarios for Echocardiography Lessen Significantly in an education RCT (WISELY) study [25•]. Set to conclude in July 2016, this trial is examining the rates of inappropriate TTE ordering by attending cardiologists and primary care physicians in an ambulatory setting following an educational intervention [25•].
Whether educational interventions can truly alter the ordering patterns for better, more cost-effective and impactful care is yet to be determined. However, recent studies opine there is ample room for growth within imaging. Stress echocardiography is a prime example, as few studies have shown an improvement beyond an appropriateness rate of about 61 % [11, 26]. While awareness of appropriateness has been heightened by the availability of AUC, continued and diligent efforts are needed to help transition them into daily clinical use, which translates into more cost-effective, care.
AUC Beyond North America: the Next Step?
The development of AUC in North America has set a precedent for a clinician-led approach to guide resource utilization in cardiology. At present, the only AUC published for clinical application come from the documents cited in this paper, but in 2014, the European Society of Cardiology (ESC) announced their intention to develop their own consensus statement using a similar scoring system to allocate studies as inappropriate, “uncertain” (more evidence needed), or appropriate [27]. Since the release of the ESC statement, a set of appropriateness criteria have been published to guide the utilization of imaging in the diagnosis and management of heart failure; this document was developed by an ESC Imaging Task Force reflecting an expert consensus approach with supporting literature review and addresses the use of echocardiography, cardiac CT, cardiac magnetic resonance imaging (MRI), and MPS [28]. This publication highlights the importance of a collaborative effort among cardiac imagers with the ultimate goal to help not just guide clinical decision-making but also support the choice of an appropriate imaging modality for patient care.
Employing AUC as a quality improvement metric to help pinpoint groups or scenarios susceptible to inappropriate use has also been highlighted by the application of AUC in a handful of international studies, in which the study authors were able to identify rates of inappropriate echocardiograms, the associated indications, and the ordering patterns of individual physicians [29–32]. One Portuguese study reported an overall appropriate indication in 79 % of echocardiograms audited with AUC; this value is less than what has been reported in US-based studies but may not be generalizable given the differences in healthcare costs and delivery systems [30].
Conclusions
Echocardiography remains a cornerstone in the diagnosis, management, and risk stratification of many cardiovascular diseases. With the shifting emphasis on defining the value of diagnostic imaging tests, echocardiography as guided by the AUC has an even greater potential to impact clinical care. Contrary to trends in the early 2000s, cardiac imaging utilization rates, including echocardiography, have experienced a correction, now declining over the last half decade. Thus, interventions aimed solely at limiting utilization will not advance the goal of optimizing the clinical practice of echocardiography. On the contrary, the purpose of the AUC is to refine cardiac imaging, limiting its use in clinical scenarios where value is not achieved, while increasing its use in scenarios where it may facilitate cost-effective optimal care. The AUC have been shown to comprehensively represent current clinical practice, and their implementation has proven feasible and effective in a variety of practice settings. There is room for improvement in their application, with educational and web-based interventions showing promise for how to augment physician awareness and perhaps offer quality metrics for health systems and payers. Emerging evidence is also supporting the use of AUC to define and quantify the value of echocardiography in optimal patient care. In summary, the AUC for echocardiography are our best available vehicle to guide optimal use of echocardiography in a value-based healthcare environment.
Footnotes
This article is part of the Topical Collection on Echocardiography
Conflict of Interest Amita Singh and R. Parker Ward declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.MEDPAC. Report to the congress: Medicare payment policy. Washington, DC: MEDPAC; 2015. [Google Scholar]
- 2•.Byrd BF, 3rd, Abraham TP, Buxton DB, et al. A summary of the American society of echocardiography foundation value-based healthcare: summit 2014: the role of cardiovascular ultrasound in the new paradigm. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2015;28:755–69. doi: 10.1016/j.echo.2015.05.007. A review of the economic, political and clinical implications of health care reform and the effect on the field of echocardiography. [DOI] [PubMed] [Google Scholar]
- 3.Huang X, Rosenthal MB. Overuse of cardiovascular services: evidence, causes, and opportunities for reform. Circulation. 2015;132:205–14. doi: 10.1161/CIRCULATIONAHA.114.012668. [DOI] [PubMed] [Google Scholar]
- 4.Ballo P, Bandini F, Capecchi I, et al. Application of 2011 American College of Cardiology Foundation/American Society of Echocardiography appropriateness use criteria in hospitalized patients referred for transthoracic echocardiography in a community setting. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2012;25:589–98. doi: 10.1016/j.echo.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 5.American College of Cardiology Foundation Appropriate Use Criteria Task F, American Society of E, American Heart A et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropriate use criteria for echocardiography. A report of the American College of Cardiology foundation appropriate use criteria task force, American Society of Echocardiography, American Heart Association, American Society Of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance American College of Chest Physicians. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2011;24:229–67. doi: 10.1016/j.echo.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Douglas PS, Khandheria B, Stainback RF, et al. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians and The Society of Critical Care Medicine. J Am Coll Cardiol. 2007;50:187–204. doi: 10.1016/j.jacc.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Douglas PS, Khandheria B, Stainback RF, et al. ACCF/ASE/ACEP/AHA/ASNC/SCAI/SCCT/SCMR 2008 appropriateness criteria for stress echocardiography: a report of the American College of Cardiology Foundation Appropriateness Criteria Task Force, American Society of Echocardiography, American College of Emergency Physicians, American Heart Association, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society For Cardiovascular Magnetic Resonance: endorsed by the Heart Rhythm Society and the Society of Critical Care Medicine. Circulation. 2008;117:1478–97. doi: 10.1161/CIRCULATIONAHA.107.189097. [DOI] [PubMed] [Google Scholar]
- 8.Ward RP, Mansour IN, Lemieux N, Gera N, Mehta R, Lang RM. Prospective evaluation of the clinical application of the American College of Cardiology Foundation/American Society of Echocardiography Appropriateness Criteria for transthoracic echocardiography. J Am Coll Cardiol Img. 2008;1:663–71. doi: 10.1016/j.jcmg.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Aggarwal NR, Wuthiwaropas P, Karon BL, Miller FA, Pellikka PA, American College of Cardiology F Application of the appropriateness criteria for echocardiography in an academic medical center. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2010;23:267–74. doi: 10.1016/j.echo.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Mansour IN, Razi RR, Bhave NM, Ward RP. Comparison of the updated 2011 appropriate use criteria for echocardiography to the original criteria for transthoracic, transesophageal, and stress echocardiography. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2012;25:1153–61. doi: 10.1016/j.echo.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Fonseca R, Negishi K, Otahal P, Marwick TH. Temporal changes in appropriateness of cardiac imaging. J Am Coll Cardiol. 2015;65:763–73. doi: 10.1016/j.jacc.2014.11.057. [DOI] [PubMed] [Google Scholar]
- 12.Bhatia RS, Carne DM, Picard MH, Weiner RB. Comparison of the 2007 and 2011 appropriate use criteria for transthoracic echocardiography in various clinical settings. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2012;25:1162–9. doi: 10.1016/j.echo.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Ward RP, Krauss D, Mansour IN, et al. Comparison of the clinical application of the American College of Cardiology Foundation/American Society of Echocardiography Appropriateness Criteria for outpatient transthoracic echocardiography in academic and community practice settings. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2009;22:1375–81. doi: 10.1016/j.echo.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 14•.Matulevicius SA, Rohatgi A, Das SR, Price AL, DeLuna A, Reimold SC. Appropriate use and clinical impact of transthoracic echocardiography. JAMA Intern Med. 2013;173:1600–7. doi: 10.1001/jamainternmed.2013.8972. Recent clinical study which emphasizes the importance of clinical decision making in ordering and interpreting echocardiography in the context of AUC. [DOI] [PubMed] [Google Scholar]
- 15.Koshy TP, Rohatgi A, Das SR, et al. The association of abnormal findings on transthoracic echocardiography with 2011 appropriate use criteria and clinical impact. Int J Cardiovasc Imaging. 2015;31:521–8. doi: 10.1007/s10554-014-0582-x. [DOI] [PubMed] [Google Scholar]
- 16•.Chiriac A, Kadkhodayan A, Pislaru SV, et al. Clinical importance of transthoracic echocardiography with direct input from treating physicians. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2016;29:195–204. doi: 10.1016/j.echo.2015.11.009. Recent study highlighting the value of echocardiographic data in real-world clinical practice, including results which changed clinical decision making by indirect value. [DOI] [PubMed] [Google Scholar]
- 17.Levy A, Singh A, Ward RP. The association between appropriate use criteria and impact on patient care for transthoracic echocardiography. Portland: American Society of Echocardiography Scientific Sessions; 2014. [Google Scholar]
- 18.Bhave NM, Mansour IN, Veronesi F, Razi RR, Lang RM, Ward RP. Use of a web-based application of the American College of Cardiology Foundation/American Society of Echocardiography Appropriateness Use Criteria for transthoracic echocardiography: a pilot study. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2011;24:271–6. doi: 10.1016/j.echo.2010.12.027. [DOI] [PubMed] [Google Scholar]
- 19.Boggan JC, Schulteis RD, Donahue M, Simel DL. Guideline-based decision support has a small, non-sustained effect on transthoracic echocardiography ordering frequency. BMJ Qual Saf. 2016;25:57–62. doi: 10.1136/bmjqs-2015-004284. [DOI] [PubMed] [Google Scholar]
- 20.Lin FY, Dunning AM, Narula J, et al. Impact of an automated multimodality point-of-order decision support tool on rates of appropriate testing and clinical decision making for individuals with suspected coronary artery disease: a prospective multicenter study. J Am Coll Cardiol. 2013;62:308–16. doi: 10.1016/j.jacc.2013.04.059. [DOI] [PubMed] [Google Scholar]
- 21.Levitt K, Edwards J, Chow CM, Bhatia RS. Development of an educational strategy and decision support tool to enhance appropriate use of stress echocardiography at a large academic medical center: a prospective, pre- and postintervention analysis. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr. 2015;28:1401–9. doi: 10.1016/j.echo.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Remfry A, Abrams H, Dudzinski DM, Weiner RB, Bhatia RS. Assessment of inpatient multimodal cardiac imaging appropriateness at large academic medical centers. Cardiovasc Ultrasound. 2015;13:44. doi: 10.1186/s12947-015-0037-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhatia RS, Milford CE, Picard MH, Weiner RB. An educational intervention reduces the rate of inappropriate echocardiograms on an inpatient medical service. J Am Coll Cardiol Img. 2013;6:545–55. doi: 10.1016/j.jcmg.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 24.Bhatia RS, Dudzinski DM, Malhotra R, et al. Educational intervention to reduce outpatient inappropriate echocardiograms: a randomized control trial. J Am Coll Cardiol Img. 2014;7:857–66. doi: 10.1016/j.jcmg.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 25•.Bhatia RS, Ivers N, Yin CX, et al. Design and methods of the echo WISELY (Will Inappropriate Scenarios for Echocardiography Lessen SignificantlY) study: an investigator-blinded randomized controlled trial of education and feedback intervention to reduce inappropriate echocardiograms. Am Heart J. 2015;170:202–9. doi: 10.1016/j.ahj.2015.04.022. Study design of a large prospective randomized trial to determine whether educational interventions for AUC use among physicians across multiple centers can improve appropriateness of physician ordering. [DOI] [PubMed] [Google Scholar]
- 26.Fonseca R, Marwick TH. Appropriateness and outcomes: is it time to adopt appropriate use criteria outside of North America? Heart. 2014;100:357–8. doi: 10.1136/heartjnl-2013-305273. [DOI] [PubMed] [Google Scholar]
- 27.Garbi M, Habib G, Plein S, et al. Appropriateness criteria for cardiovascular imaging use in clinical practice: a position statement of the ESC/EACVI taskforce. Eur Heart J Cardiovasc Imaging. 2014;15:477–82. doi: 10.1093/ehjci/jeu031. [DOI] [PubMed] [Google Scholar]
- 28.Garbi M, McDonagh T, Cosyns B, et al. Appropriateness criteria for cardiovascular imaging use in heart failure: report of literature review. Eur Heart J Cardiovasc Imaging. 2015;16:147–53. doi: 10.1093/ehjci/jeu299. [DOI] [PubMed] [Google Scholar]
- 29.Fonseca R, Negishi K, Marwick TH. What is the evidence status of appropriate use criteria (AUC)? Insight from a matching exercise with the guidelines for echocardiography. Intern Med J. 2015;45:864–9. doi: 10.1111/imj.12829. [DOI] [PubMed] [Google Scholar]
- 30.Fonseca P, Sampaio F, Ribeiro J, Goncalves H, Gama V. Appropriate use criteria for transthoracic echocardiography at a tertiary care center. Revista Port Cardiol: Orgao Of Soc Port Cardiol = Port J Cardiol: Off J Port Soc Cardiol. 2015;34:713–8. doi: 10.1016/j.repc.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 31.Gurzun MM, Ionescu A. Appropriateness of use criteria for transthoracic echocardiography: are they relevant outside the USA? Eur Heart J Cardiovasc Imaging. 2014;15:450–5. doi: 10.1093/ehjci/jet186. [DOI] [PubMed] [Google Scholar]
- 32.Rameh V, Kossaify A. Appropriate use criteria in echocardiography: an observational institutional study with the perspective of a quality improvement project. Clin Med Insights Cardiol. 2016;10:23–8. doi: 10.4137/CMC.S36504. [DOI] [PMC free article] [PubMed] [Google Scholar]


