Abstract
The academician forms the backbone of any medical college, hospital or university and shoulders the quadruple responsibilities of patient care, teaching, administration and research. Of these, research, though long and difficult, is extremely fulfilling. Academicians often carry out research that is based on observations in practice or in response to their patient's needs. These are called as “Investigator- initiated studies” and these may not have the funding support of the pharmaceutical industry. Hence, the investigator must make sure that he/she complies with the country's regulatory requirements. In the past decade, several changes have dotted the regulatory landscape in the country and have changed the way in which academic research is carried out. The present article outlines regulatory requirements for academic research giving their historical evolution, the key bodies in India that govern or oversee research, along with “must know” and “good to know” facets for the conduct of clinical research in the country.
Key words: Academic research, clinical trials, compliance, India, regulations
INTRODUCTION
The academician is the life line of any medical college, hospital or university as he/she performs the quadruple functions of patient care, teaching, administration and research. While all of these can provide a great measure of satisfaction, a key driver to sating intellectual curiosity remains research. Good research contributes to evidence-based medicine and thus better and improved patient care with the ultimate goal of promoting health.
Research, however, is a laborious, time and labour intensive task that can take months or even years to reach fruition. Drug development research, in particular, is long and arduous and bringing a single new drug costs on an average USD 1.78 billion and takes approximately 13.5 years from discovery to the market.[1] Drug development research is primarily funded by the pharmaceutical industry including the process of human testing (Phase I-IV studies). These studies (called clinical trials or regulatory studies) are conducted with the academician as the principal investigator largely in academic centres. The pharmaceutical industry funds or 'sponsors' the studies and ensures compliance with the country's regulatory requirements. Academicians, however, also carry out their own research and these studies are called as 'Investigator initiated studies' (IISs). Here, the academician raises funds for the study through his efforts from various sources including possibly the pharmaceutical industry. In these IISs, he dons the dual mantle of an investigator and 'sponsor' and thus directly becomes responsible for ensuring regulatory compliance.
Anaesthesia as a speciality straddles several diverse disciplines that include various branches of surgery and medicine as well as critical care and pain management among others. The past three decades have also seen remarkable advances in the field of anaesthesia, some of which include pulse oximetry, end-tidal gas monitoring, introduction of propofol and the laryngeal mask airway. Anaesthesiologists are uniquely positioned to carry out translational research given the data-rich environment in which they practice[2] and this research can be used successfully to guide evidence-based practice of the discipline as also public health policy.[3] Regardless of the nature of the research (Regulatory Clinical Trials or IISs), knowledge of the regulatory requirements is an essential imperative for researchers. The present article details these requirements giving their historical evolution, the key bodies in India that govern or oversee research along with 'must know' and 'good to know' for the conduct of clinical trials in the country.
THE NATIONAL REGULATORY BODY – THE CENTRAL DRUGS STANDARD CONTROL ORGANISATION AND THE DRUGS CONTROLLER GENERAL OF INDIA
The Central Drugs Standard Control Organization (CDSCO) is the National Regulatory Authority in India. Its equivalent counterparts elsewhere include the United States Food and Drug Administration (US FDA), Health Canada and the European Medicines Agency. CDSCO is an arm of the Ministry of Health and Family Welfare, Government of India. Its mission is to safeguard and enhance public health by assuring the safety, efficacy and quality of drugs, cosmetics and medical devices.[4]
The Drugs Controller General of India (DCGI) is an official of the CDSCO who is the final regulatory authority for the approval of clinical trials in the country. His ambit, in addition, also extends to inspections of trial sites, inspections of sponsors of clinical research and manufacturing facilities in the country, oversight of the Central Drugs Testing Laboratory (Mumbai) and the Regional Drugs Testing Laboratory as also heading the Indian Pharmacopeia Commission among various other roles, responsibilities and functions.
THE DEPARTMENT OF HEALTH RESEARCH AND THE INDIAN COUNCIL OF MEDICAL RESEARCH
The Indian Council of Medical Research (ICMR) is the apex body that is responsible for the formulation, coordination and promotion of biomedical research. It receives funding from the Ministry of Health and Family Welfare and the Department of Health Research, Government of India.[5]
KEY DOCUMENTS IN CLINICAL RESEARCH
Drugs and Cosmetics Act (1940) and Drugs and Cosmetics Rules (1945)
This act first came into being in 1940 and regulates the import, manufacture and distribution of drugs in the country to ensure that drugs and cosmetics sold in the country are safe, effective and conform to essential quality standards. It has Chapters, Rules and Schedules[6,7] and is amended at regular intervals to ensure greater safety, efficacy and drug quality. The Schedule Y along with rules 122A, 122B, 122D, 122DA, 122DAC and 122E (see below) is the key document that governs clinical research in the country. Per law, it is mandatory that all clinical research that falls under the ambit of Schedule Y complies with the necessary requirements. It has 12 appendices, formats for clinical trial protocols, informed consent forms, ethics committee (EC) approval templates and a format for serious adverse event (SAE) reporting.
Ethical Guidelines of the Indian Council of Medical Research (2006)
The revised ICMR guidelines released in 2006 is called the 'Ethical Guidelines for Biomedical Research on Human Participants' and remains valid as of today, and a revised version is expected in 2017. This guideline covers two broad aspects of clinical research – the general principles that need to be followed and guidance regarding special areas of research (e.g., research in children or herbal research).[8] Researchers are expected to be familiar with both these documents and abide by the requirements in the former and the guidance in the latter.
Indian Good Clinical Practice Guideline (2001)
A good clinical practice (GCP) guideline was released in 2001 by the CDSCO that attempted to be India specific, but unlike the ICH GCP guideline, has not been revised since.[9]
REGULATORY CHANGES IN INDIA'S LANDSCAPE (2005–2016)
The Schedule Y amendment released on 20th January, 2005 saw dramatic changes that attempted to bring India on par with internationally prevalent regulations.[7] Some of the key changes included the definition of a clinical trial, permitting trials in India to be conducted in the same phase of drug development as elsewhere in the world, demarcation of clear roles and responsibilities of the sponsor, investigator and ECs, underscoring the importance of informed consent, requirement for studies in special populations and mandating that protocol amendments need approval from the office of the DCGI.[10] Over the next 10 years, a slew of changes and reforms dotted the regulatory landscape as outlined in Table 1.
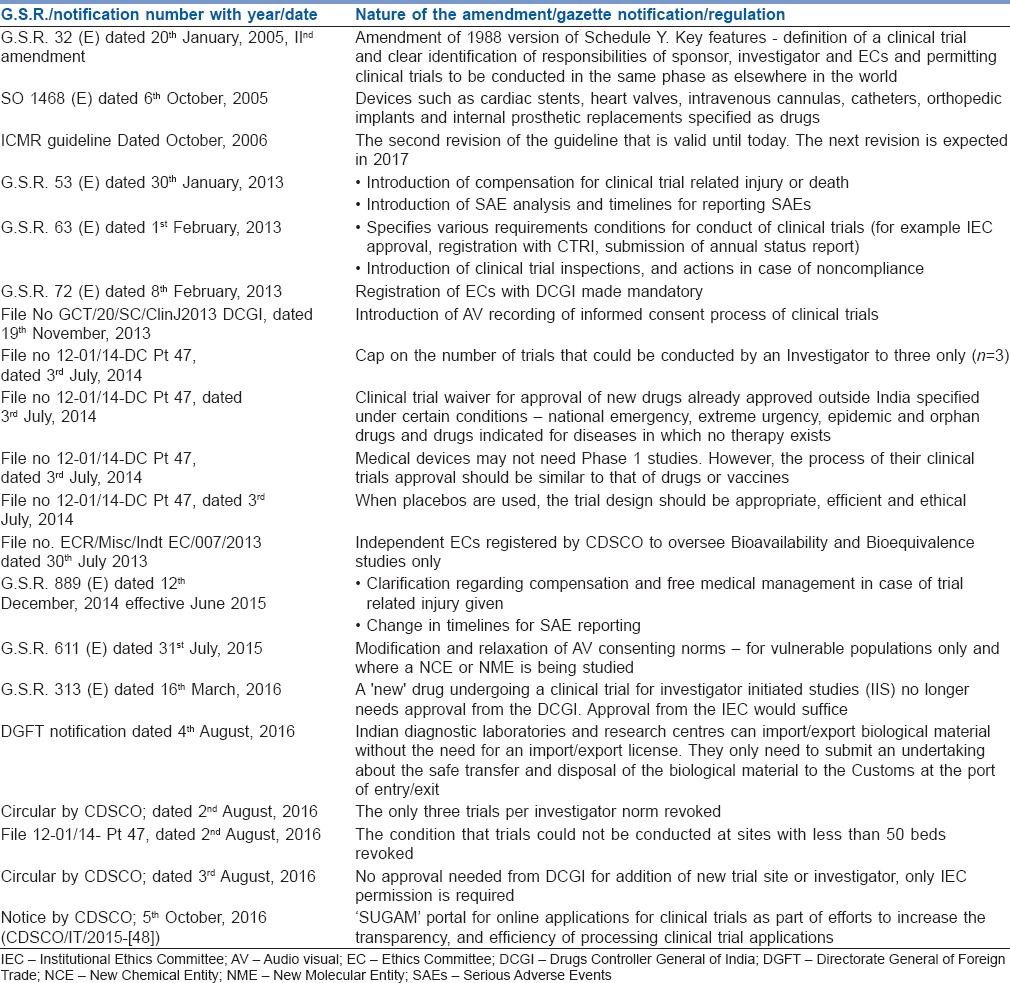
Table 1.
Evolution of regulatory changes in India (2005–2016 as relevant to clinical trials)
REGULATORY REQUIREMENTS FOR THE CONDUCT OF CLINICAL TRIALS IN INDIA – WHAT THE INDIAN RESEARCHER MUST KNOW
A - Regulatory definitions
What is a 'clinical trial'
A clinical trial[11] is defined as the systematic study of new drug(s) (see below for the definition of a new drug) in human subject(s) to generate data for discovering and/or verifying:
The clinical pharmacological (including pharmacodynamic and pharmacokinetic) effects
And/or adverse effects
With the objective of determining safety and/or efficacy of the new drug
What is a 'new drug'
A 'new' drug[12] is one:
That has not been used to a significant extent in the country
An already approved drug that is now proposed to be used in a different dosage, different dosage form, a new route or a new indication. An example of this would be the intrathecal or epidural route of use of dexmedetomidine
Approved for use but has been on the market for <4 years after approval
A fixed-dose combination of two or more drugs, individually approved earlier for certain claims, which are now proposed to be combined for the first time in a fixed ratio
All vaccines
Drugs made using the recombinant DNA technology
B - Conduct of the clinical trial
Conduct of the clinical trial
The investigator must ensure that clinical trials are conducted as per the rules outlined below[13]
In compliance with an EC and a DCGI approved protocol
In the case of IISs with 'new drugs', DCGI approval is no longer needed; only an EC approval is required – 16th March, 2016 G.S.R. 313 (E)[14]
In compliance with GCP guidelines
All applicable regulations
Registration of Ethics Committees that approve studies (Rule 122DD)[15]
Investigators and Administrators of Academic Institutes should ensure that their Institutional Ethics Committees (IECs) are registered with the central licensing authority and the registration renewed at the end of 3 years.[15] This is mandatory for Regulatory Clinical Trials
Approval from Institutional Ethics Committee
All clinical trials need to have approval from the IEC
A recent regulatory change with respect to IISs is that academicians who carry out trials with 'new drugs' no longer need approval from the DCGI for the conduct of the trial and IEC approval would suffice. This is provided that these studies are not intended for generating data to make a regulatory submission.[14]
In the event that the IEC feels that there could be a potential overlap between the academic and regulatory purposes of the trial, they should notify the office of the DCGI. If the IEC does not hear from the DCGI within 30 days, it should be presumed that no permission is needed from the licensing authority
Understand the three types of review carried out by the Institutional Ethics Committee and the nature of the research proposal/s in each category of review
Institutional Ethics Committees function according to standard operating procedures [SOPS] that are usually available on their websites. Projects submitted essentially undergo two broad types of review- Full board or full committee review [for all projects that present more than minimal risk] or expedited review [for projects that pose no more than minimal risk; e.g., left over clinical samples]. Projects may also be “exempted from review” [research on data in public domain as for example with systematic reviews or meta-analysis]. Investigators who make submissions to the IEC should be familiar with the IEC SOPs and understand the category that their trial/study fits into and the nature of the review that it is likely to undergo.
Registration of the clinical trial with the Clinical Trials Registry of India
The CTRI[16,17] is a free, online portal that allows both investigator-initiated and regulatory studies to be registered. It is recommended that all studies are registered at a public portal. However, for Regulatory Clinical Trials, registration in CTRI is mandatory from June 2009.
Registration must be done before the first participant is enrolled
Registration is important from a publication standpoint point as editors of many Biomedical Journals will not accept papers that have interventional studies not registered with a Clinical Trials Registry
Obtain informed consent from participants
Investigators must ensure that written, informed consent is obtained from all participants in a clinical trial
For trials that involve vulnerable participants (children or mentally challenged patients for example) and involve a new chemical entity or a new molecular entity, the investigators in addition have to ensure audio visual recording of the informed consent process (gazette notification dated 19th November, 2013).[18]
Report serious adverse events that occur during a clinical trial
An SAE is defined as an untoward medical occurrence during a clinical trial that is associated with death, in patient hospitalisation (if the study was done on outpatient basis), prolongation of hospitalisation (if the study was conducted on in-patient basis), persistent or significant disability or incapacity, a congenital anomaly or birth defect or is otherwise life-threatening.[19] The timelines for reporting SAEs are given below
- The investigator should report all SAEs to the DCGI (for regulatory studies), the sponsor and the IEC, within 24 h of their occurrence (for academic studies, these should be reported only to the IEC within 24 h)[20]
- If unable to do so, the reason for delay in reporting the SAE along with the report should be submitted to the DCGI
- Send SAE report to DCGI after due analysis. In addition, send to Chairman of IEC and the Head of the institution where the trial has been conducted within 14 calendar days of occurrence of the event
- IEC should submit its report on the SAE, after due analysis, along with its opinion on the financial compensation (if any) to be paid by the sponsor or his representative, and to the DCGI within 30 calendar days of occurrence of the event
Understand that compensation for trial related death and injury is now required and the implications of compensation particularly when academic studies with 'new drugs' are carried out
Compensation in a clinical trial is needed both when death occurs or when there is clinical trial-related injury. The formulae for compensation for both are described below.[21]
Compensation for death: B × F × R/99.37, where 'B' is a base amount of 8 lakhs, 'F' is a age factor based on the Workmen Compensation Act and 'R' a risk factor that takes into account the severity, duration of disease and co-morbidities
Compensation for permanent disability: (C × D × 90)/(100 × 100), where 'C' is the quantum of compensation which would have been given to the nominee in case of death of the participant and 'D' is the percentage disability suffered by the subject
Compensation for an SAE leading to life-threatening disease: 2 × W × N, where 'W' is the minimum wage per day of the unskilled worker (in Delhi) and ‘N’ is the number of days of hospitalisation
Compensation for birth defect or congenital anomaly: Medical care to be provided as long as required and a lumpsum amount to be kept in a fixed deposit that would bring in a monthly interest equal to half of the minimum wage of an unskilled worker in Delhi
Addressing SAEs and compensation: For dealing with SAEs, some institutions have a SAE subcommittee (over and above the IEC) that meets regularly to review and evaluate SAEs. For institutes that do not have them, this would be a good committee to constitute. Since clinical trial related injury or death is equally possible both with pharmaceutical industry and investigator-initiated (academic) studies, budgetary provisions need to be in place at the institutional level for the medical management of adverse events [AEs], SAEs and provision of insurance to trial participants.
Site preparedness (rule 122DAC)
Understand that the regulator can inspect the site at any time and that he can cancel the trial permission and discontinue the study. Therefore preparedness of the study site at all times must be ensured
Studies with medical devices
A draft notification [Medical Devices Rules, 2016] dated 17th October 2016, has been issued for medical devices by the Ministry of Health and Family Welfare, Department of Health and Family Welfare, Government of India [GSR 983 (E)]. Per this notification, medical devices are broadly classified as investigational medical devices and registered or approved medical devices. Chapter VII of this notification states that clinical trials with the former need both IEC and DCGI approval, while academic studies [studies not intended for manufacturing or marketing the device] with the latter, need only IEC approval.[22]
Interventional studies in Anaesthesia that are not “drug” trials
Clinical studies/trials that are investigator – initiated and involve procedures as interventions [e.g., comparison of effectiveness of two different techniques of brachial plexus block] would need Institutional Ethics committee approval and CTRI registration.
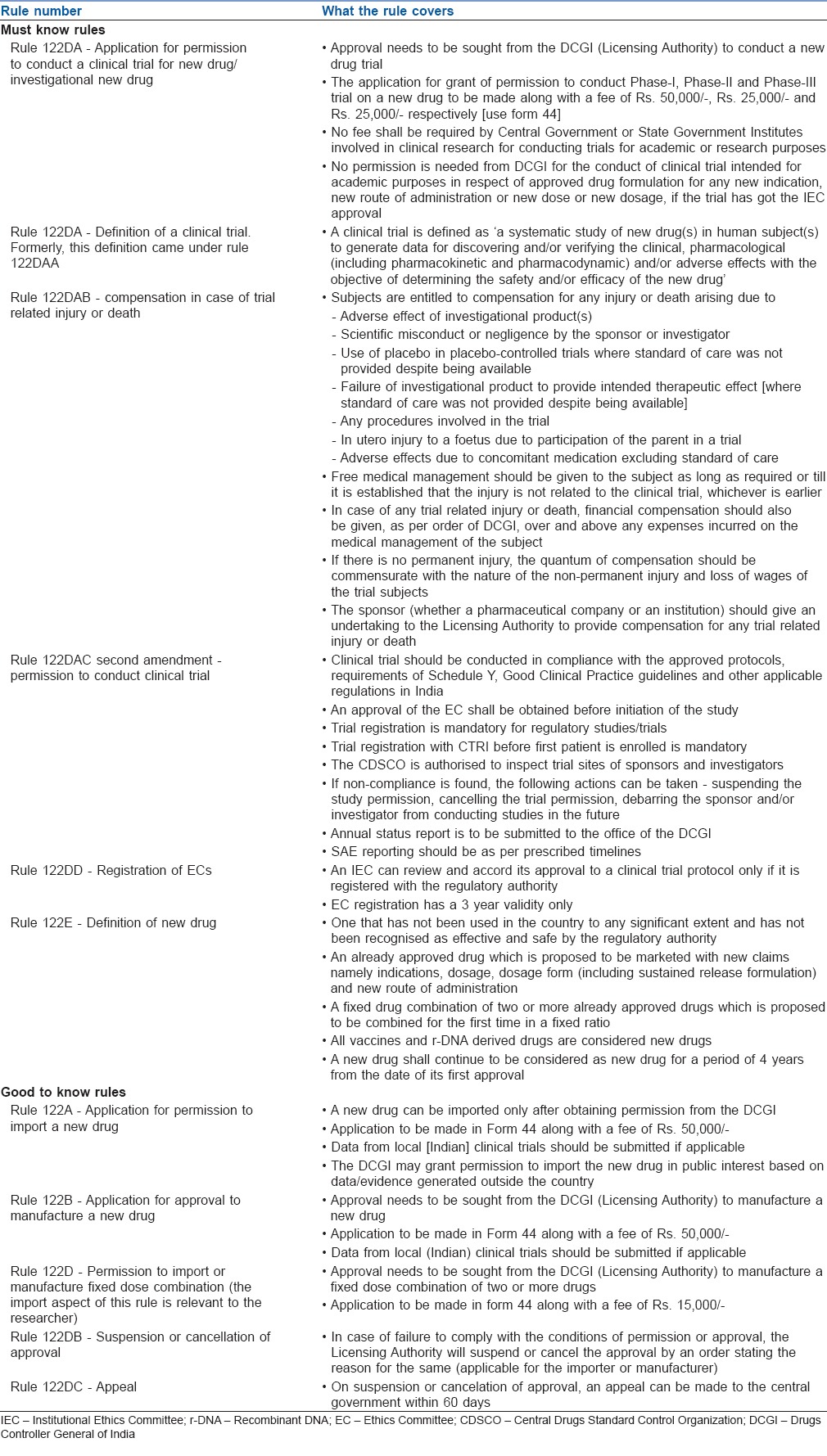
Table 2 covers must know and good to know aspects of clinical trial research.
Table 2.
Key rules of the Drugs and Cosmetics Act and what they mean for the researcher
SOURCES OF FUNDING FOR ACADEMIC INVESTIGATOR INITIATED RESEARCH
Several governmental and non-governmental organisations within the country fund academic research and the academician needs to make an application to them with application formats and timelines being available on their home pages. Some of these include – ICMR, Department of Biotechnology, Department of Science and Technology and the Council for Scientific and Industrial Research. In addition, several pharmaceutical companies in the country also fund investigator initiated research. The funding from the industry could be by way of provision of drug supplies or monetary support or both. The control of the study including its conception, conduct and analysis remains exclusively with the investigator in these studies and would need a clear memorandum of understanding with the industry funder.
WORKING WITH A COLLABORATOR OUTSIDE THE COUNTRY
Studies that involve a collaborator from outside India need an additional approval from the Health Ministry Screening Committee, a committee that works out of ICMR and meets quarterly to assess these projects for collaborative merit.[23]
THE ROAD AHEAD
India accounts for 17% of the world's population and 20% of the global disease burden expressed as disability adjusted life years.[24] The scope for clinical research in the country thus is enormous as it faces the dual burden of both communicable and non-communicable diseases.[25] A recent study has also shown that the regulatory studies done in the country are not commensurate with their health care needs.[26] An understanding of both the disease burden coupled with the regulatory requirements by the researcher will go a long way in alleviating disease associated burden and suffering in the country.
CONCLUSIONS
The academic investigator needs to be up to speed in reading, understanding and applying regulations and work in tandem with the pharmaceutical industry for greater patient benefit. The ECs now have a larger than ever onus need to appreciate and understand risk – benefit and to empower themselves through repeated training and use of standard operating procedures given that it is known that the quality of IEC review across the country remains variable.[27] Finally, the empowering of IECs by the regulator towards approving studies with 'new' drugs without the need for regulatory approval means that researchers, IECs and institutional administrators should have mechanisms in place for greater participant protection, assessment and analysis of SAEs and budgetary provisions in place for insurance and compensation of participants in these trials.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Paul SM, Mytelka DS, Dunwiddie CT, Persinger CC, Munos BH, Lindborg SR, et al. How to improve R and D productivity: The pharmaceutical industry's grand challenge. Nat Rev Drug Discov. 2010;9:203–14. doi: 10.1038/nrd3078. [DOI] [PubMed] [Google Scholar]
- 2.Sanders RD, Maze M. Translational research: Addressing problems facing the anesthesiologist. Anesth Analg. 2007;105:899–901. doi: 10.1213/01.ane.0000278624.55746.29. [DOI] [PubMed] [Google Scholar]
- 3.Amin P, Fox-Robichaud A, Divatia JV, Pelosi P, Altintas D, Eryüksel E, et al. The Intensive Care Unit specialist: Report from the Task Force of World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2016;35:223–8. doi: 10.1016/j.jcrc.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Central Drugs Standard Control Organization. [Last accessed on 2017 Feb 20]. Available from: https://www.cdscoonline.gov.in/CDSCO/homepage .
- 5.Indian Council of Medical Research, New Delhi. [Last accessed on 2017 Feb 20]. Available from: http://www.icmr.nic.in/
- 6.Imran M, Najmi AK, Rashid MF, Tabrez S, Shah MA. Clinical research regulation in India-history, development, initiatives, challenges and controversies: Still long way to go. J Pharm Bioallied Sci. 2013;5:2–9. doi: 10.4103/0975-7406.106553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drugs and Cosmetics Act. [Last accessed on 2017 Feb 20]. Available from: https://www.rgcb.res.in/uploads/2014/07/Schedule-Y.pdf .
- 8.Indian Council of Medical Research, New Delhi. [Last accessed on 2017 Feb 20]. Available from: http://www.icmr.nic.in/ethical_guidelines.pdf .
- 9.Central Drugs Standard Control Organization. [Last accessed on 2017 Feb 20]. Available from: http://www.cdsco.nic.in/html/GCP1.html .
- 10.Bhave A, Menon S. Regulatory environment for clinical research: Recent past and expected future. Perspect Clin Res. 2017;8:11–6. doi: 10.4103/2229-3485.198551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. [Last accessed on 2017 Feb 25]. Available from: https://www.rgcb.res.in/uploads/2014/07/Schedule-Y.pdf .
- 12. [Last accessed on 2017 Feb 25]. Available from: https://www.indiankanoon.org/doc/50800010/
- 13.Government of India. Ministry of Health and Family Welfare. [Last accessed on 2017 Feb 26]. Available from: http://www.mohfw.nic.in/index1.php?lang=1&level=5&sublinkid=4481&lid=2641 .
- 14.G.S.R 313. [Last accessed on 2017 Feb 26]. Available from: http://www.cdsco.nic.in/writereaddata/GSR%20313%20(E)%20dated%2016_03_2016.pdf .
- 15.Registration of Ethics Committees. GSR72E. 2013. Feb 08, [Last accessed on 2017 Feb 25]. Available from: http://www.cdsco.nic.in/writereaddata/G.S.R%2072(E)%20dated%2008.02.2013.pdf .
- 16.Clinical Trials Registry – India. Which Clinical Trials are Required to Be Registered? [Last accessed on 2017 Feb 21]. Available from: http://www.ctri.nic.in/Clinicaltrials/faq.php .
- 17.Satyanarayana K, Sharma A, Parikh P, Vijayan VK, Sahu DK, Nayak BK, et al. Statement on publishing clinical trials in Indian biomedical journals. J Postgrad Med. 2008;54:78–9. doi: 10.4103/0022-3859.40766. [DOI] [PubMed] [Google Scholar]
- 18.Office Order. Audio-visual Recording of Informed Consent of Process. 2013. Nov 19, [Last accessed on 2017 Feb 26]. Available from: http://www.cdsco.nic.in/writereaddata/Office%20Order%20dated%2019.11.2013.pdf .
- 19.ICH Harmonized Tripartite Guideline. [Last accessed on 2017 Feb 27]. Available from: http://www.cdsco.nic.in/writereaddata/GSR%20313%20(E)%20dated%2016_03_2016.pdf .
- 20.G.S.R 292 (E). Ministry of Health and Family Welfare. [Last accessed on 2017 Feb 26]. Available from: http://www.cdsco.nic.in/writereaddata/1Draft%20Rules%20on%20compensation.pdf .
- 21.Government of India. Ministry of Health and Family Welfare. [Last accessed on 2017 Feb 20]. Available from: http://www.cdsco.nic.in/writereaddata/ORDER%20and%20Formula%20to%20Determine%20the%20quantum%20of%20compensation%20in%20the%20 cases%20of%20Clinical%20Trial%20related%20serious%20Adverse%20Events (SAEs)%20of%20Injury%20other%20than%20Death.pdf .
- 22.G.S.R 983 (E). Ministry of Health and Family Welfare. [Last accessed on 2017 Feb 28]. Available from: http://www.cdsco.nic.in/writereaddata/grsoct17983.pdf .
- 23.Indian Council of Medical Research, New Delhi. [Last accessed on 2017 Feb 22]. Available from: http://www.icmr.nic.in/hmsc_document/hmsc_project2/introduction.pdf .
- 24.Country Cooperation Strategy at a Glance, World Health Organization. [Last accessed on 2017 Feb 20]. Available from: http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_ind_en.pdf .
- 25.Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100:191–9. doi: 10.1016/j.trstmh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 26.Chaturvedi M, Gogtay NJ, Thatte UM. Do clinical trials conducted in India match its healthcare needs? An audit of the clinical trials registry of India [CTRI] Perspect Clin Res. 2017 doi: 10.4103/2229-3485.215970. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muthuswamy V. Status of ethical review and challenges in India. Indian Pediatr. 2005;42:1189–90. [PubMed] [Google Scholar]


