Abstract
Background and Aims:
Undertreated pain can have negative consequences on patients' health as well as the health-care system. The present study was aimed at identifying the current trends in post-operative pain management and availability of acute pain services (APS). In addition, it is also an attempt to assess the availability of analgesia for non-surgical cases, and the attitudes, beliefs, and perceptions of clinicians regarding acute pain management in the tertiary hospitals in the state of Maharashtra (India).
Methods:
This was a cross-sectional, multicentre questionnaire survey involving the anaesthesiologists and surgeons. Percentages, median, interquartile ranges were calculated and compared by employing a Wilcoxon sign rank test.
Results:
Data from thirty centres revealed that the surgeons played a major role in treating pain, while most of the anaesthesiologists treated pain primarily in the operation theatre and recovery room. An APS was operational in seven hospitals. The most frequently employed techniques to achieve analgesia were the administration of non-steroidal anti-inflammatory drugs, opioids and epidural analgesia. The majority of the centres had no written protocol and dedicated staff for pain management, pain assessment was not adequately stressed, and only five out of the thirty centres included in the study provided ongoing pain education to health professionals even when the hospitals claimed to provide APS. The major hurdles in providing optimal analgesia and implementing APS were a lack of pain education, equipment and administrative problems.
Conclusion:
Thus, the tertiary centres in Maharashtra fall short of providing optimal acute post-operative pain management.
Key words: Acute pain, acute pain service, acute post-operative pain, multimodal analgesia
INTRODUCTION
Maharashtra is one of the largest states in India which has been in the forefront of healthcare and boasts of health-care indices above the national average.[1,2] However, there is inadequate literature on acute pain management in hospitals in the state – government or private. Less than 30% of patients in India receive adequate pain management.[3] Undertreated pain leads to increased post-operative morbidity and mortality,[4,5,6,7] prolonged hospital stay, overcrowding of wards which consequently adversely affects the quality of health care.[8] Therefore, a questionnaire survey was undertaken to assess the current practice of post-operative pain management in the tertiary hospitals in Maharashtra. The availability of the pain service for non-surgical cases, the roles, attitudes and perceptions of health-care professionals and the hurdles faced by them in delivering pain services were also surveyed.
METHODS
This non-interventional, descriptive, cross-sectional, multi-centre survey was undertaken (December 2013–February 2016) after taking the Ethics Committee approval from the parent institution. Out of the 47 government and private medical colleges and 10 corporate hospitals (teaching hospitals with more than 100 beds) that were approached, 35 agreed to participate in the survey. The procedures like taking permission from the Dean/Head of Department or the Ethics Committee of the participating centre were completed as per the norms of each institute. The participating centres and individuals were assured anonymity. Questionnaires were addressed to the respective Heads of Department. One questionnaire for the Anaesthesiology Department and one each for various surgical specialties was sent to each institute in printed form by post or in an electronic version by E-mail. If there was no response within 3 weeks, four telephonic reminders were given at weekly intervals after which follow-up was not done.
The questionnaires for anaesthesiologists and surgeons were identical and consisted of 24 questions with 4 questions having Likert scale responses as options, 3 open-ended questions, and the remaining had multiple choices or yes/no responses [Annexure I]. The questions sought information about the respondents' pain management policies, clinicians' attitudes, perceptions and beliefs about pain management, and hurdles faced by them in providing optimal pain management. Before the study, the questionnaire was validated by an experienced anaesthesiologist. A small pilot study initially was done in the parent institute to confirm face validity.
The data were analysed using the Statistical Package for the Social Sciences (IBM Corp. Released 2015, IBM SPSS Statistics for Windows, Version 23.0, Armonk, N.Y., U.S.A) and percentages, mean and standard deviation, median and interquartile range were calculated as applicable. The median values were compared using the Wilcoxon sign rank test. P < 0.05 was considered as statistically significant at 95% confidence interval.
RESULTS
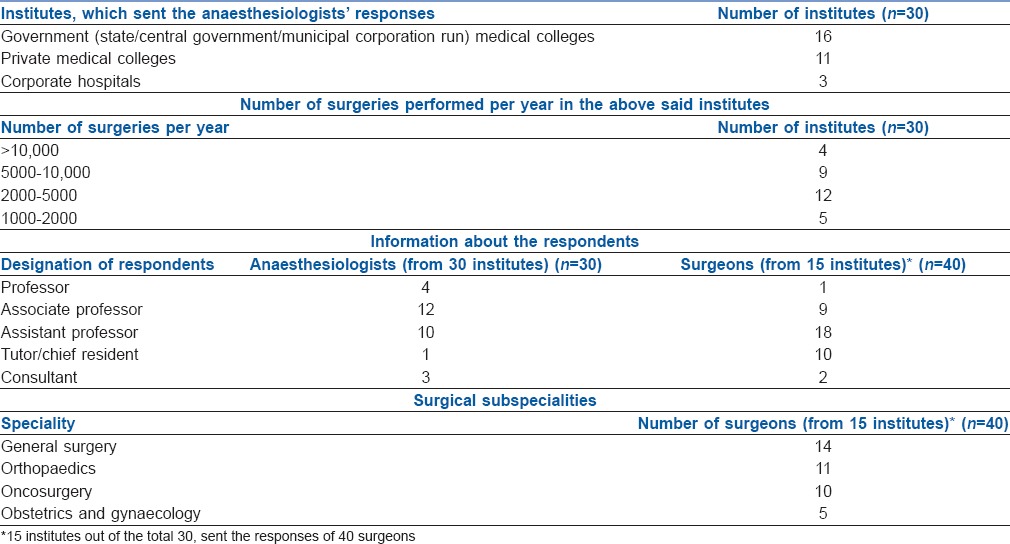
We got one response each from the Anaesthesiology Departments of thirty institutes, while 15 institutes sent the responses of forty surgeons of different specialties such as General Surgery, Orthopaedics, Obstetrics and Gynaecology, and Oncosurgery (one response from each department of an institute). The demographic profiles of the hospitals and the respondents are depicted in Table 1.
Table 1.
Demographic data
Out of the 30 hospitals, 7 had an operational acute pain service (APS), 2 had a formal pain management program and 4 had a chronic pain clinic. The surgeons played a major role in pain management throughout the patients' stay in the hospital while the role of most of the anaesthesiologists was confined to treating pain primarily in the operation theatre and post-operative recovery room. However, anaesthesiologists from 17 centres agreed that they managed pain, even in wards for a selected group of patients or if requested by the surgeons [Table 2]. Dedicated staff for acute pain management was available in 7 centres and 6 hospitals provided round-the-clock pain services. The facility for treating acute pain in non-surgical patients was available in 13 hospitals on demand. Written protocol for pain management was developed in 4 hospitals. Five institutes had on-going pain education for the health care professionals out of which 2 centres were also providing training for nursing staff. Intermittent non-steroidal anti-inflammatory drugs (NSAIDs), opioids and epidural analgesia were used most commonly for treating post-operative pain, while patient-controlled analgesia (PCA) was the least commonly used modality. Nine institutes claimed to use non-pharmacological methods such as physiotherapy, psychological counselling, and change in position which were resorted to more frequently by the orthopaedic surgeons [Table 2].
Table 2.
Current post-operative pain management practices in various tertiary hospitals in Maharashtra
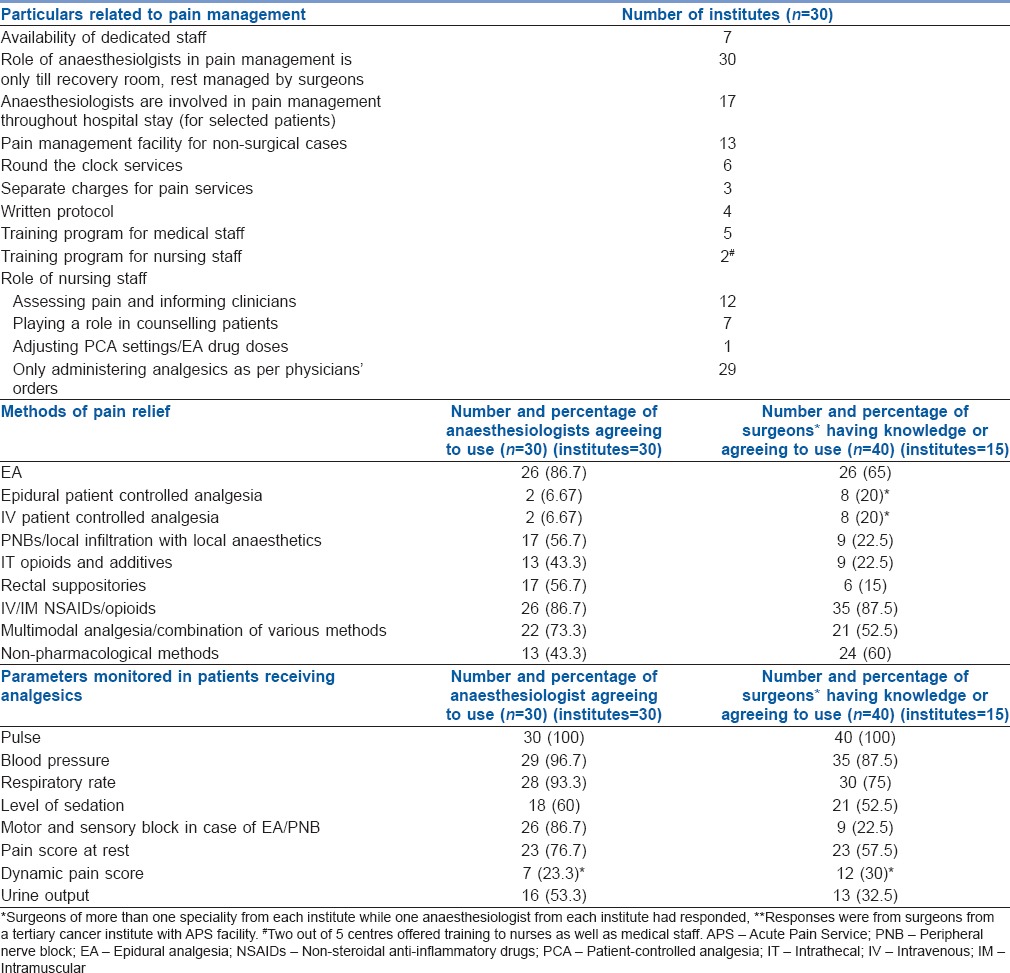
Anaesthesiologists and resident doctors were responsible for the follow-up of the patients with epidural catheters and peripheral nerve blocks. In patients receiving potent analgesics, the vital parameters were routinely monitored in all the hospitals. Pain scores at rest were measured routinely in 23 hospitals, and dynamic pain scores were routinely measured in only 7 hospitals [Table 2].
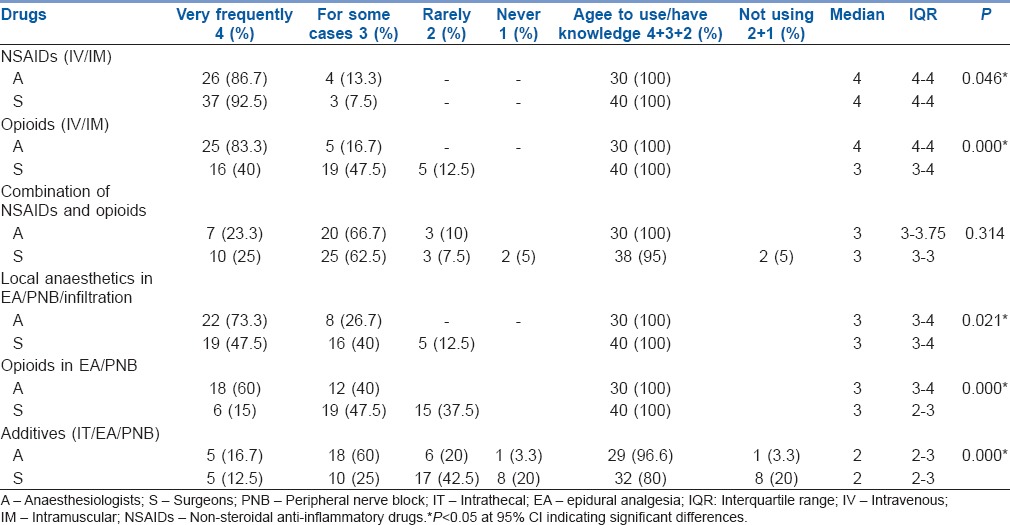
There were significant differences in pain management practices of anaesthesiologists and surgeons [Table 3]. While surgeons (92.5%) used NSAIDs more frequently, (P = 0.046), the anaesthesiologists (83.3%) used opioids more frequently (P = 0.000). Furthermore, other modalities such as epidurals, nerve blocks, intrathecal additives and multimodal approach were used more frequently by the anaesthesiologists.
Table 3.
Comparison of pain management practice by anaesthesiologists and surgeons: Drugs used for post-operative pain management
With the existing pain management strategies, about 40% of anaesthesiologists and an equal percentage of surgeons believed that they had succeeded in bringing a moderate degree of pain relief in the post-operative patients. Regarding the benefits of pain management and APS, there were significant differences of perception between anaesthesiologists and surgeons. Ninety-four per cent of anaesthesiologists agreed that optimal pain management in the form of APS would bring down the post-operative complications as against 85% of surgeons who concurred (P = 0.039, P < 0.05). There was a consensus between the anaesthesiologists (43.3%) and surgeons (42.5%) that treating post-operative pain prevented chronic post-operative pain (P = 0.793) [Figure 1].
Figure 1.
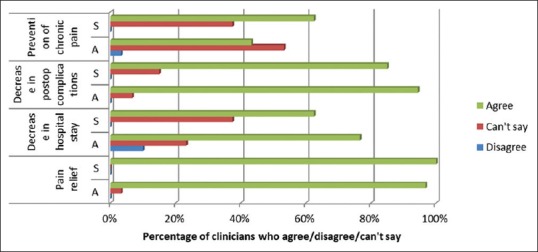
Knowledge/perception of clinicians about the goals of acute post-operative pain management. A – Anaesthesiologists; S – Surgeons
Thirty per cent of the anaesthesiologists and 47.5% of surgeons believed that patients should 'expect to have some amount of pain' after surgery. All surgeons (100%) and 96.7% of anaesthesiologists agreed that the patients should be counselled preoperatively about post-operative pain. All the anaesthesiologists (100%) agreed that they should have a role in managing pain even in the wards while 80% of surgeons agreed to this. Most of the clinicians accepted that a multidisciplinary approach and an APS would be required for optimal pain management [Figure 2].
Figure 2.
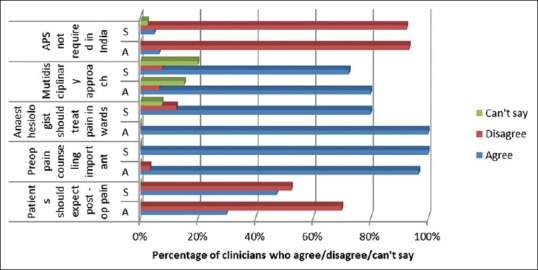
Attitudes and beliefs of clinicians about acute post-operative pain management. A – Anaesthesiologists; S – Surgeons
In spite of having the willingness to run an APS, they were faced with many hurdles. The biggest hurdle, as cited by both anaesthesiologists (83.3%) and surgeons (72.5%) was a lack of pain education at all levels of health-care professionals. The other obstacles were lack of equipment and workforce and lack of priority from hospital administration [Figure 3].
Figure 3.
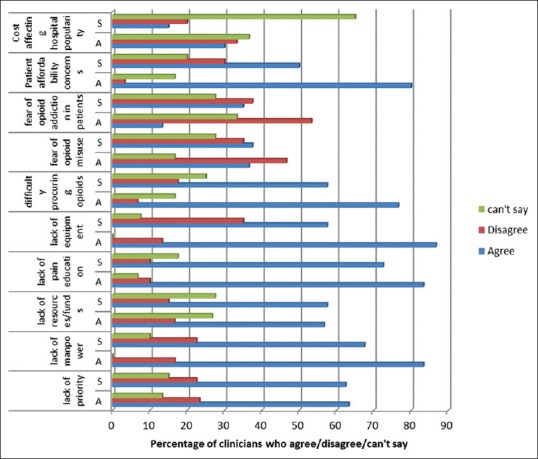
Hurdles in acute pain management. A – Anaesthesiologists; S = Surgeons
DISCUSSION
The 24-item questionnaire was designed on the basis of the questionnaire surveys done before,[9,10,11,12,13,14,15,16,17,18,19] to get a comprehensive idea about the existing acute pain management practices and availability of APS. An APS is a rapidly evolving health-care service for managing post-operative pain which may also be tasked with consultation related to non-surgical pain like trauma, burns and other cases.[9,20] Besides the post-operative pain, treatment for non-surgical pain was provided by anaesthesiologists in 13 hospitals out of 30, on request by surgeons, irrespective of the presence of APS.
Many guidelines have been issued by the pain medicine associations of different countries, but no such guidelines exist in India. The 2005 American Pain Society recommendations for post-operative pain management suggest that an interdisciplinary process should be used to improve pain management.[21] The Association of Anaesthetists of Great Britain and Ireland has recommended that all hospitals performing major surgeries should have a multidisciplinary pain team with an anaesthesiologist in charge.[6] Anaesthesiologists are a logical choice to provide pain relief because of their knowledge and technical expertise in managing pain.[22] The results of our survey showed that the surgeons played a key role in post-operative pain management with the help of anaesthesiologists. In most of the institutes, leadership on the part of the anaesthesiologists and involvement of nursing staff, physiotherapist and pharmacists was limited. Our survey showed that the role of nurses in almost all the hospitals was limited mostly to administering the analgesics as per clinicians' orders. This scenario must change, and nurses should play a more active role as they have the most frequent contact with patients. This can be done by training them adequately and giving them responsibilities of pain assessment, counselling the patients, adjusting the drug infusions, PCA, etc.[23] As early mobilisation and less post-operative pulmonary complications are proven benefits of treating pain, the physiotherapists should also be involved.[10,23] However, only 7 (23.3%) hospitals take the help of a physiotherapist for pain management. The personnel like pharmacists and clinical psychologist should also be recruited as a part of the pain management team to provide better pain relief.[10,23]
Besides the multidisciplinary approach, the other recommendations include good physician-patient communication to encourage patients' involvement in decision-making in their treatment, on-going pain education of health providers with interventions in the health-care system like use of synergistic analgesia, minimally invasive surgery, 24 hours/day pain service, pain protocols, increased use of patient reported outcomes and patient education regarding prompt reporting of pain.[6,24,25,26,27] However, our survey showed that there was a paucity of organised pain services, written protocols, round the clock services and training programs.
There are five recognised quality criteria for an APS: dedicated personnel, 24 hours/day service, written protocols, regular assessment/documentation of pain scores and on-going pain education.[15,20,22,27] Although 7 centres claimed to have an APS, only 2 hospitals had an organised APS according to the set criteria. The observation that there is a paucity of APS in Maharashtra is a reflection of a previous national level survey by Jain et al.[9] in which it was observed that there were only 68 functioning APS in India. The advantages of having an APS are an improvement in the quality of pain management and lower incidence of side effects. In addition, with an APS in place, patients are more likely to receive pain education, are more satisfied, are discharged earlier and perceive fewer barriers to pain management.[27]
There was no written protocol in majority of the centres. A written protocol ensures a more consistent standard of care and provides detailed instructions on when and whom to call for unrelieved pain, treatment of special groups of patients and standard orders for PCA pumps, epidurals, nursing care and so on.[10]
Analgesics like NSAIDs and opioids given by intramuscular and intravenous routes were widely used, but they may not provide optimal analgesia unless the intermittent analgesics are tailored according to individual patient's needs with regular pain scoring. Multimodal analgesia was used by 73.3% of anaesthesiologists and 52.5% of surgeons. The use of epidurals was observed in 26 out of 30 institutes, and PCA pumps were used in only 2 institutes. Non-pharmacological methods which are cost-effective and useful adjuncts for pain management[20,28] were used by 43.3% of anaesthesiologists and 60% of surgeons [Table 2].
Regular pain assessment was lacking in many hospitals, which is an important tool to individualise treatment.[11] Our questionnaire had no direct question about the awareness about pain as a 5th vital sign. Furthermore, we have not asked about the frequency of pain assessment, which is a limitation of our study.
The survey revealed important facts about the beliefs of anaesthesiologists and surgeons. The perception in the anaesthesiologists (30%) and surgeons (47.5%) that the patients should 'expect to have some pain' after surgery may contribute to suboptimal pain management.[13] However, a positive finding was that many of them were aware of the benefits of optimal pain management and were convinced of the need for a multidisciplinary approach and special pain services for post-operative pain management. Despite this, APS is not available in most of the medical centres.
The frequently cited reason for this by both anaesthesiologists (83.3%) and surgeons (72.5%) was lack of pain education at all levels of health-care professionals. The other reasons were lack of equipment (86.7%), workforce (83.3%), concerns regarding affordability of patients (80%), difficulty in procuring opioids (76.6%), lack of priority from hospital administration (63.3%), etc., This is a very important take-home message of this study as it provides directions for improvement in the area of post-operative pain management. In the national survey by Jain et al.,[9] lack of initiative and funds were the major reasons cited by the anaesthesiologists. In this study,[9] 'lack of pain education' as a hurdle in starting APS was not included. However, it has been cited as one of the biggest hurdles in pain management in our study. In the Italian survey by Coluzzi et al.,[15] the inadequate training of nurses and surgeons, poor organisation and lack of equipment were the biggest hurdles. In a Canadian survey by Zimmerman and Stewart, 'time commitment' and financial constraints have been cited as the top reasons for failure to institute APS.[14] In another study, Jain and Chatterjee[29] have described several barriers which were overcome while implementing APS in a tertiary hospital in India. These were lack of workforce, pain education, and administrative problems. These were similar to those highlighted in our study.
The questionnaire surveys have their own limitations. The information gathered may be skewed[11] and there may be a recall bias and a social desirability bias, which means the responders, may give responses which appear more desirable socially.[10] This survey was done only in the academic tertiary institutes. However, clinicians in other sectors may have a different perspective on post-operative pain management and APS. Thus, still larger scale surveys are needed to evaluate the practices and attitudes of the clinicians in other sectors.
CONCLUSION
The study shows that the tertiary hospitals in Maharashtra face many challenges in acute post-operative pain management. To improve it, on-going education programs, policy changes at government as well as institutional levels, procuring funds, equipment, improving accessibility to opioids, continued research and establishment of APS needs to be done.[6,30] In addition, procedure-specific, evidence-based, acute post-operative pain management guidelines-based practice must be promoted in all the tertiary hospitals.[31]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
ANNEXURE
Annexure I: Questionnaire for anaesthesiologists and surgeons
The following questionnaire is for research purpose, the name, identity and the institute of the responders will not be revealed when the study is published.
Multiple choice questions are given, you may select the option/options you feel is/are the most appropriate. You can express your opinion in the blank spaces provided.
Name: ....... email i.d: ................ Contact no:................
Speciality: ◻ anaesthesiologist ◻ surgeon, specify the subspeciality if surgeon........
Designation: ◻ Running own private clinic ◻ free lancing ◻ consultant in a private institute If you are in a medical college-◻ Chief resident, ◻ assistant professor, ◻ associate professor ◻ Professor and head of department ◻ other (specify)..........
Number of surgeries performed per year: ◻ <1000 ◻ 1000-5000 ◻ 5001-10,000 ◻ >10,000
Do you have a special pain management service/(APS)/formal pain management program in your hospital? ◻ Yes ◻ no
If yes, when was it established?...............
Do you have dedicated staff for pain management? ◻ yes ◻ no
-
Describe the nature of APS/pain management in your institute
-
(i)Managed by anaesthesiologists till the patient is discharged from recovery room to ward, later managed by surgeons in ward ◻ yes ◻ no
-
(ii)Managed by a dedicated multidisciplinary pain team from recovery room till the time pain management is required during hospital stay ◻ yes ◻ no
-
(iii)Available to patients in acute pain other than those operated like trauma, burns, cancer, etc., ◻ yes ◻ no
-
(iv)Available round the clock on all week days ◻ yes ◻ no
-
(v)Separate charges for pain services ◻ yes ◻ no
-
(i)
-
Describe the degree of pain relief achieved by the pain management provided in your institute-(select any one option)
- ◻ Complete pain relief even with movement
- ◻ enough relief that pain is noticed
- ◻ Moderate relief with a small degree of distress but not distressing
- ◻ Pain relief only at peak periods of pain
- ◻ Can’ft say
-
Describe the goals achieved by post-operative pain management in your institute-(you may select the appropriate option)-
-
(i)Pain relief ◻ Strongly agree ◻ agree ◻ strongly disagree ◻ disagree ◻ can’t say
-
(ii)Decreased length of stay in hospital ◻ Strongly agree ◻ agree ◻ strongly disagree ◻ disagree ◻ can’t say
-
(iii)Decreased post.operative respiratory complication ◻ Strongly agree ◻ agree ◻ strongly disagree ◻ disagree ◻ can’t say
-
(iv)Prevention of chronic pain ◻ Strongly agree ◻ agree ◻ strongly disagree ◻ disagree ◻ can’t say
-
(v)Any other-................................................
-
(i)
-
Do you have written protocol for pain management?
◻ yes ◻ no
-
If there is written protocol, which of the following is included?(you may select more than one option)
◻ Instructions on when/whom to call for unrelieved pain
◻ Pharmacologic intervention (e.g for epidural, intramuscular, PCA etc...)
◻ Non-pharmacologic intervention
◻ Emergency call orders (in case of emergency surgery requiring pain management/complications regarding analgesic drugs etc.)
Others.............................
-
Personnel involved in developing the protocol-(you may select more than one option if appropriate)
◻ Anaesthesiologist ◻ surgeon ◻ general physicians/paediatrician
◻ pharmacist ◻ nursing staff ◻ specialist pain physician
◻ physiotherapist ◻ clinical psychologist ◻ other
-
Personnel involved in pain management in your institute
◻ Anaesthesiologist ◻ surgeon ◻ general physicians/paediatrician
◻ pharmacist ◻ nursing staff ◻ specialist pain physician
◻ physiotherapist ◻ clinical psychologist ◻ other
-
Do you run regular training program for pain management in your hospital?
For medical staff- ◻ yes ◻ no
For nursing staff – ◻ yes ◻ no
-
Which drugs do you use in your institute for post-operative pain management? (Select appropriate answer from the options placed in front of each drug)
NSAIDS (i.v/i.m) ◻ Very frequently ◻ for some cases ◻ rarely ◻ never
OPIOIDS (i.v/i.m) ◻ Very frequently ◻ for some cases ◻ rarely ◻ never
Combination of above two ◻ Very frequently ◻ for some cases ◻ rarely ◻ never
For epidural/PNB/infiltration
Local anaesthetics ◻ Very frequently ◻ for some cases ◻ rarely ◻ never
Opioids ◻ Very frequently ◻ for some cases ◻ rarely ◻ never
Additives like clonidine ◻ Very frequently ◻ for some cases ◻ rarely ◻ never
Other drugs-......................................
-
What methods of pain relief do you know/use for major surgeries in post-operative period? (select one or more than one if appropriate)-
◻ Epidural analgesia ◻ Epidural patient controlled analgesia
◻ Intravenous patient controlled analgesia
◻ Peripheral nerve blocks
◻ Intrathecal opioids/additives ◻ Rectal suppositories
◻ i.v/i.m NSAIDS and narcotic analgesics
◻ Combination of different methods
-
What parameters do you evaluate in patients receiving analgesics?
◻ Pulse ◻ blood pressure ◻ respiratory rate
◻ level of sedation ◻ motor/sensory block in case of epidural/peripheral nerve block ◻ pain score at rest ◻ pain score during movement
◻ urine output
-
Are non-pharmacologic measures included as a part of post-operative pain management?
◻ Yes ◻ No
-
If yes, which of the following are included?
◻ Physiotherapy ◻ Psychological counseling
◻ Acupressure/acupuncture ◻ Hot/cold fomentation ◻ Other
-
Role of nursing staff in your institute (select one or more)
◻ Assessing pain and informing clinicians
◻ Playing role in counseling the patients
◻ Adjusting patient controlled analgesia (PCA) settings/epidural analgesia drug doses
◻ Administering drugs as per clinicians’ orders
◻ Other........................................
-
Who provides follow-up for post-operative epidurals/nerve block/PCA/PCEAS?
◻ Anaesthesiologist ◻ surgeons ◻ pain specialists
◻ residents ◻ nurses ◻ others
-
Please select the appropriate answer – (agree/disagree/can’t say) for each question
-
(i)Patients after an operation should expect to have some pain.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
(ii)It is important to counsel the patient regarding post-operative pain prior to surgery.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
(iii)The anaesthesiologists should be involved in pain management even after the patient goes toward.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
(iv)Special pain services are not required for Indian set up.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t sayIf you agree- select reason/s-◻ Because patients have very good pain tolerance◻ The resources and workforce can instead be utilized for other health problems in our country◻ It is neither an affordable concept in India nor is it feasible.◻ We are managing the pain efficiently even if there is no special setup
-
(i)
-
What are the hurdles in managing acute post-operative pain and/or developing acute pain services?
-
Lack of priority for pain management from hospital administration.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Lack of workforce. ◻ Strongly agree ◻ agree◻ strongly disagree ◻ disagree ◻ can’t say
-
Lack of resources/funds.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Lack of pain education in nurses and doctors.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Lack of equipment (non-availability of PCA pumps, special monitors, other equipment)◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Difficulty in procuring opioids due to strict regulatory laws.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Fear about misuse of opioids among residents, nurses etc.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Concern about addiction in patients.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Common patients may not afford the sophisticated services.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
-
Hospital may lose its popularity if bills of patients are hiked.◻ Strongly agree ◻ agree ◻ strongly disagree◻ disagree ◻ can’t say
- Other ..........................
-
REFERENCES
- 1.Economic Survey of Maharashtra 2015-2016. Directorate of Economics and Statistics, Planning Department. Government of Maharashtra. [Last accessed on 2016 Nov 10]. Available from: https://www.mahades.maharashtra.gov.in/files/publication/ESM_1516_Eng.pdf .
- 2.Duggal R, Dilip TR, Raymus P. Health and Healthcare in Maharashtra. A Status Report. [Last accessed on 2016 Nov 10]. Available from: http://www.cehat.org/publications/PDf%20files/r53.pdf .
- 3.Vijayan R. Managing acute pain in the developing world. Pain Clin Updat. 2011;19:1–7. [Google Scholar]
- 4.Macintyre PE, Walker S, Power I, Schug SA. Acute pain management: Scientific evidence revisited. Br J Anaesth. 2006;96:1–4. doi: 10.1093/bja/aei295. [DOI] [PubMed] [Google Scholar]
- 5.Carr EC, Nicky Thomas V, Wilson-Barnet J. Patient experiences of anxiety, depression and acute pain after surgery: A longitudinal perspective. Int J Nurs Stud. 2005;42:521–30. doi: 10.1016/j.ijnurstu.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 6.Meissner W, Coluzzi F, Fletcher D, Huygen F, Morlion B, Neugebauer E, et al. Improving the management of post-operative acute pain: Priorities for change. Curr Med Res Opin. 2015;31:2131–43. doi: 10.1185/03007995.2015.1092122. [DOI] [PubMed] [Google Scholar]
- 7.Iverson RE. Discussion: Clinical consequences of inadequate pain relief: Barriers to optimal pain management. Plast Reconstr Surg. 2014;134(4 Suppl 2):22S–3S. doi: 10.1097/PRS.0000000000000688. [DOI] [PubMed] [Google Scholar]
- 8.Masigati HG, Chilonga KS. Postoperative pain management outcomes among adults treated at a tertiary hospital in Moshi, Tanzania. Tanzan J Health Res. 2014;16:47–53. doi: 10.4314/thrb.v16i1.7. [DOI] [PubMed] [Google Scholar]
- 9.Jain PN, Bakshi SG, Thota RS. Acute pain services in India: A glimpse of the current scenario. J Anaesthesiol Clin Pharmacol. 2015;31:554–7. doi: 10.4103/0970-9185.169088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagi H. Acute pain services in the United Kingdom. Acute Pain. 2004;5:89–107. [Google Scholar]
- 11.Nasir D, Howard JE, Joshi GP, Hill GE. A survey of acute pain service structure and function in United States hospitals. Pain Res Treat. 2011;2011:934932. doi: 10.1155/2011/934932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan SK, Chui PT, Lee A, Lai PB, Li TY, Gin T. Surgeons' attitudes and perception of an acute pain service. Hong Kong Med J. 2008;14:342–7. [PubMed] [Google Scholar]
- 13.Manzoni D, Pizabella ML, Beltramelli V, Severgnini C, Balicco B. Attitudes on pain change when acute pain services are introduced. J Anaesth Clin Res. 2012;4:280. [Google Scholar]
- 14.Zimmermann DL, Stewart J. Postoperative pain management and acute pain service activity in Canada. Can J Anaesth. 1993;40:568–75. doi: 10.1007/BF03009742. [DOI] [PubMed] [Google Scholar]
- 15.Coluzzi F, Savoia G, Paoletti F, Costantini A, Mattia C. Postoperative pain survey in Italy (POPSI): A snapshot of current national practices. Minerva Anestesiol. 2009;75:622–31. [PubMed] [Google Scholar]
- 16.Windsor AM, Glynn CJ, Mason DG. National provision of acute pain services. Anaesthesia. 1996;51:228–31. doi: 10.1111/j.1365-2044.1996.tb13638.x. [DOI] [PubMed] [Google Scholar]
- 17.Ready LB. How many acute pain services are there in the United States, and who is managing patient-controlled analgesia? Anesthesiology. 1995;82:322. doi: 10.1097/00000542-199501000-00055. [DOI] [PubMed] [Google Scholar]
- 18.Harmer M, Davies KA, Lunn JN. A survey of acute pain services in the United Kingdom. BMJ. 1995;311:360–1. doi: 10.1136/bmj.311.7001.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rawal N, Allvin R. Acute pain services in Europe: A 17-nation survey of 105 hospitals. The EuroPain acute pain working party. Eur J Anaesthesiol. 1998;15:354–63. doi: 10.1046/j.1365-2346.1998.00306.x. [DOI] [PubMed] [Google Scholar]
- 20.Upp J, Kent M, Tighe PJ. The evolution and practice of acute pain medicine. Pain Med. 2013;14:124–44. doi: 10.1111/pme.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gordon DB, Dahl JL, Miaskowski C, McCarberg B, Todd KH, Paice JA, et al. American Pain Society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med. 2005;165:1574–80. doi: 10.1001/archinte.165.14.1574. [DOI] [PubMed] [Google Scholar]
- 22.Ready LB, Oden R, Chadwick HS, Benedetti C, Rooke GA, Caplan R, et al. Development of an anesthesiology-based postoperative pain management service. Anesthesiology. 1988;68:100–6. doi: 10.1097/00000542-198801000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Engelman E, Salengros JC, Paquot MC, Barvais L. The acute pain service (APS): How we should have done it. Acta Anaesthesiol Belg. 2006;57:233–8. [PubMed] [Google Scholar]
- 24.Savoia G, Alampi D, Amantea B, Ambrosio F, Arcioni R, Berti M, et al. Postoperative pain treatment SIAARTI recommendations 2010.Short version. Minerva Anestesiol. 2010;76:657–67. [PubMed] [Google Scholar]
- 25.Schug SA, Palmer GM, Scott DA, Hallivell R, Trinca J. Acute Pain Management: Scientific Evidence. 4th ed. Melbourne: ANZCA and FPM; 2015. [Last accessed on 2016 Oct 05]. APM: Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine. Available from: http://www.anzca.edu.au/resources/college.publications . [Google Scholar]
- 26.Apfelbaum JL, Ashburn MA, Connis RT, Gan TJ, Nickinovich DG. Practice guidelines for acute pain management in the perioperative setting. An updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116:248–73. doi: 10.1097/ALN.0b013e31823c1030. [DOI] [PubMed] [Google Scholar]
- 27.Miaskowski C, Crews J, Ready LB, Paul SM, Ginsberg B. Anesthesia-based pain services improve the quality of postoperative pain management. Pain. 1999;80:23–9. doi: 10.1016/s0304-3959(98)00192-4. [DOI] [PubMed] [Google Scholar]
- 28.Rao M. Acute postoperative pain. Indian J Anaesth. 2006;50:340–4. [Google Scholar]
- 29.Jain PN, Chatterjee A. Development of acute pain service in an Indian cancer hospital. J Pain Palliat Care Pharmacother. 2010;24:129–35. doi: 10.3109/15360281003713842. [DOI] [PubMed] [Google Scholar]
- 30.Khatib SK, Kulkarni SS, Razvi SS. Acute pain services in India: A long and challenging journey ahead. Indian J Pain. 2016;30:83–9. [Google Scholar]
- 31.Joshi GP, Kehlet H. Procedure-specific pain management: The road to improve postsurgical pain management? Anesthesiology. 2013;118:780–2. doi: 10.1097/ALN.0b013e31828866e1. [DOI] [PubMed] [Google Scholar]


