Abstract
Background and Aims:
Obese individuals are predisposed to difficult airway and intubation. They usually yield confusing or misleading auscultatory findings. We aimed to assess the rapidity and efficacy of ultrasonographic (USG) sliding lung sign for confirming endotracheal intubation in normal as well as overweight and obese surgical patients.
Methods:
This prospective, observational study was performed in forty surgical patients. Twenty patients with body mass index (BMI) <25 were recruited to Group A, whereas twenty patients with BMI ≥25 constituted Group B. Following induction and intubation, appearance of end-tidal carbon dioxide waveform was used to confirm endotracheal intubation. Presence of breath sounds bilaterally was sought by auscultation, and time taken for auscultatory confirmation was noted. The USG confirmation of air entry to the lung field as indicated by lung sliding was sought, and the time taken was noted. Chi-square test, independent t-test and paired t-test were used as applicable.
Results:
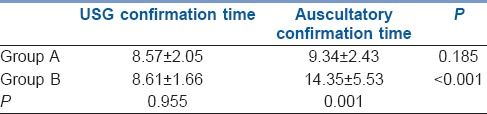
Auscultatory confirmation was more rapid in Group A as compared to Group B (9.34 ± 2.43 s vs. 14.35 ± 5.53 s, P = 0.001). However, there was no significant difference in USG confirmation time in both the groups (8.57 ± 2.05 s vs. 8.61 ± 1.66 s). Four patients in Group B had doubtful breath sounds against none in Group A. There was no doubtful lung slide with USG in both groups. One case of endobronchial intubation in Group B was diagnosed with USG which was doubtful by auscultation.
Conclusion:
Ultrasound directed confirmation of endotracheal tube placement in overweight and obese patients is superior in speed and accuracy in comparison to the standard auscultatory method.
Key words: Auscultation, endotracheal intubation, obesity, sliding lung sign, ultrasonography
INTRODUCTION
Obese individuals are predisposed to difficult airway and intubation in comparison to the non-obese patients.[1] The inherent increased risk of hypoxaemia during the induction of anaesthesia in these patients could be compounded by an increased time required for insertion of the tracheal tube,[1] besides reduction in functional residual capacity and compliance with an increase in airway resistance and pulmonary vascular resistance.[2] Delays in detecting improper endotracheal tube placement in the obese could, therefore, be catastrophic.
Among the various techniques available, the common ones usually adopted for the confirmation of endotracheal intubation are end tidal capnography and auscultation. Obese patients usually yield confusing or misleading auscultatory findings as the sound waves have to traverse large amount of tissues which represent a significant barrier. Ultrasonographic (USG) imaging of the sliding lung sign has been shown to be an accurate indicator of endotracheal intubation,[3,4,5,6,7] and hence can be used as an additional measure for confirming proper tracheal placement of the endotracheal tube.
The present study was aimed to assess the rapidity and efficacy of USG sliding lung sign for confirming correct endotracheal tube placement in normal as well as overweight and obese surgical patients.
METHODS
This prospective, unblinded, observational study was performed in patients undergoing various surgical procedures under general anaesthesia requiring endotracheal intubation.
Patients of both sex, aged 20–70 years, of American Society of Anesthesiologists (ASA) physical status 1 and 2, with Modified Mallampati class 1 and 2 having no pulmonary co-morbidities were included in the study after obtaining Hospital Ethical Committee approval and informed consent. Patients with significant cardiac illness and those requiring nasal intubation were excluded from the study.
Following a detailed pre-anaesthetic assessment, the patients were kept fasting for 6 h for solids and 2 h for clear fluids. On arrival in the theatre, an intravenous cannula was introduced and intravenous fluid was started. The patients were allotted to either of the two groups (20 in each group) based on their body mass index (BMI). Those with BMI <25 were recruited to Group A (auscultatory confirmation of intubation), whereas those with BMI ≥25 constituted Group B (ultrasonographic confirmation of intubation). Pre-induction monitors including a pulse-oximeter, non-invasive blood pressure, electrocardiograph and end-tidal carbon dioxide (ETCO2) were attached.
Following pre-oxygenation with 100% oxygen for 3 min and induction with adequate doses of either thiopentone or propofol, the patients received a skeletal muscle relaxant (suxamethonium, vecuronium or atracurium) and were mask ventilated with isoflurane 1% in oxygen till the time of laryngoscopy. An ETCO2 trace was ensured at the time of mask ventilation. An experienced anaesthesiologist performed laryngoscopy, and intubation was accomplished with a single lumen endotracheal tube of size 7.0 or 8.0 mm internal diameter as appropriate. The endotracheal tube was introduced till the proximal part of the cuff had passed beyond the vocal cords. In those with poor visibility of the glottis on laryngoscopy, the tube was fixed at 19 cm in case of females and 21 cm for males at the angle of the mouth. Patients were manually ventilated with the reservoir bag of the breathing circuit, and the appearance of ETCO2 waveform was looked for and was used to confirm tracheal placement of endotracheal tube. Presence of breath sounds was sought by auscultation on the infra-clavicular and infra-axillary areas on both the sides by the same anaesthesiologist who performed the intubation. The presence of breath sounds, on each side were classified into definite, doubtful or absent and were documented. Time taken for auscultatory confirmation was also noted. Auscultatory time was defined as the time elapsed from beginning to the end of auscultation.
The USG confirmation was performed by a second anaesthesiologist who was trained to identify the lung sliding sign. A linear ultrasound probe (SonoSite S-Nerve™ Ultrasound, Bothell, WA 98021 USA with a frequency of 13.6MHz) was placed in the midclavicular line in the sagittal plane with the arrow mark just below the clavicle so that the upper part of the probe was over the second intercostal space. First, the ribs and then the pleural line were identified. Air entry to the lung field as indicated by lung sliding and comet tails were sought [Figure 1] (Normally, the pleura moves with respect to the ribs and the comet tail artefacts). The presence or absence of these signs were noticed and documented on both the sides. Anticipating an increased anterior chest wall thickness in Group B, the depth setting of the ultrasound machine was kept at 2.7cm for Group A and 4.9cm for Group B patients.
Figure 1.
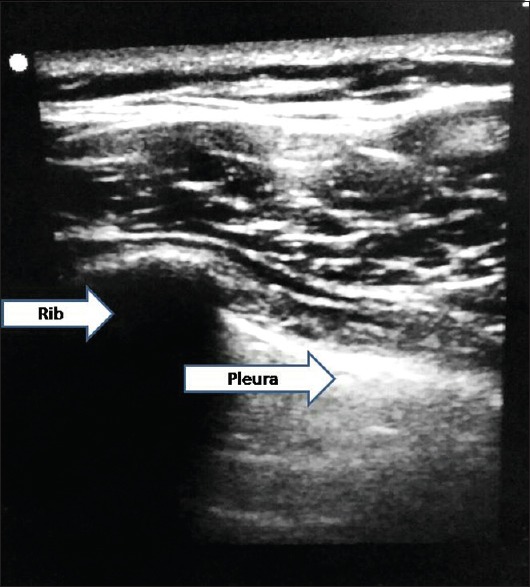
Ultrasonographic appearance of rib and pleura
Despite the presence of ETCO2 waveforms, if there was absent or doubtful air entry by auscultation on one side, lung sliding sign was sought. If the lung sliding was also absent, it was considered as endobronchial intubation. The tube was then withdrawn till positive lung sliding was obtained which was confirmed again by auscultation.
The time taken for USG confirmation was calculated from the time of placing the ultrasound probe on the chest till evaluation on both sides was complete. Both auscultatory and USG confirmation time periods were recorded using a stopwatch by an anaesthesia technician who was not actively involved with the anaesthetic procedure. After confirmation of bilateral air entry mechanical ventilation was initiated, and anaesthesia was continued. Use of gum elastic bougie, attempts at intubation and failure to intubate were also documented as obese patients were expected to pose difficulty in performing direct laryngoscopy and intubation.
Based on the results on sensitivity of ultrasound with clinical assessment reported in an earlier publication (Sustic et al.[6]), with 95% confidence and 20% allowable error, the minimum sample size was calculated as 40. Chi-square test was used to compare the gender and the presence or absence of breath sounds and the lung sliding in both the groups. Independent t-test was used to compare the USG and auscultatory confirmation time, age, height, weight and BMI. To compare the average confirmation time by ultrasound and auscultation between groups, Paired t-test was used. The statistical analysis was performed using IBM SPSS software version 20.0 (Bengaluru, India) for windows 8.
RESULTS
Patients in Group B had a significantly higher age (50.60 ± 11.24 vs. 32.90 ± 13.92) and BMI (30.57 ± 3.75 vs. 21.75 ± 2.24) as compared to those in Group A. The gender distribution was comparable between the groups with 9 out of 20 patients in Group A and 10 out of 20 in Group B being females (P = 1.000). Intragroup comparison of rapidity of auscultatory and USG confirmation showed comparable results in Group A [Table 1]. But, in Group B, the USG confirmation took significantly longer time than auscultation [Table 1, P ≤ 0.001]. Intergroup analysis had shown that auscultatory confirmation time was shorter in Group A as compared to Group B. But, there was no significant difference in the USG confirmation time in both the groups [Table 1].
Table 1.
information can be rewritten as provided below
On auscultation, four patients in Group B had doubtful breath sounds against none in Group A. There was no doubtful lung sliding with USG in both groups, though there was one case of absent lung sliding in Group B. The percentage comparison of breath sounds by auscultation (present and doubtful) between groups yielded similar results [Table 2, P = 0.106]. Similarly, the percentage comparison of lung sliding sign (present and absent) between groups was comparable [Table 2, P = 1.000]. All patients were intubated in the first attempt itself and none in both the groups required gum elastic bougie for intubation.
Table 2.
Comparison of breath sounds and lung sliding sign in both groups

DISCUSSION
Major mishaps during general anaesthesia result from inability to intubate the trachea following administration of a muscle relaxant and failure to detect it in time. Proper endotracheal intubation is usually confirmed by adequate bilateral chest expansion, presence of bilateral breath sounds, endotracheal tube fogging, colorimetric ETCO2, continuous waveform capnography and absence of gurgling sound over the epigastrium.[8,9] Though the most commonly employed techniques are ETCO2 and auscultation, sometimes, confirmation remains doubtful. Increased thickness of anterior chest wall as in the obese and females occasionally pose difficulty with auscultatory confirmation. Blockage of gas sampling tube or auto zeroing at the time of intubation may delay confirmation by ETCO2. Although the presence of ETCO2 is definitely the most reliable confirmatory test, it may not always be available in remote locations or in Intensive Care Units.
The sliding lung sign has shown to be an accurate indicator of endotracheal intubation,[3] therefore this technique is of help in difficult situations. The normal lung surface associates lung sliding with horizontal repetitions of the pleural line which indicate gas. The to-and-fro movement observed at the pleural line, spreading below is called the lung sliding which, in turn, reflects that the pleural line consists of the visceral pleura also. Physiologically, this sign is most discrete at the upper parts of the lungs.[10]
Prolonged auscultatory confirmation time observed in Group B in our study could be because of the increased thickness of the anterior chest wall which hindered the passage of sound waves. Comparable auscultatory and ultrasonographic confirmation time in non-obese patients was anticipatory. In our study, for auscultatory confirmation, four lung areas were auscultated, whereas for USG confirmation, only two areas were examined. This reflects in the slightly higher mean auscultatory confirmation time even in the non-obese. It was also noted that the patients' mean age in the obese group was significantly higher. This could be because obesity is more prevalent in older age groups as many people who reach old age are already overweight.[11]
The time consumed for performing bilateral lung ultrasound had been compared with auscultation and capnography for confirming endotracheal intubation in elective surgical patients by Pfeiffer et al.[12] It was noted that verification with ultrasound was as fast as auscultation alone and faster than the standard method of auscultation and capnography. Similar conclusions were derived in obese patients also.[13] Anticipating thicker anterior chest wall in these patients and keeping the depth setting of the ultrasound machine at higher values from the beginning itself will facilitate faster identification of lung sliding.
The positive predictive value of bilateral lung sliding for confirming proper endotracheal intubation in patients following cardiac arrest is well established[4]: So is its efficacy in ensuring precise placement of the left-sided double lumen tubes.[5,6,14] The use of ultrasound becomes important during cardiopulmonary resuscitation as capnography is less reliable in confirmation of endotracheal intubation in this situation.
The usefulness of upper airway sonography for the verification of endotracheal tube location after intubation has been well proven.[6,7,14,15,16,17,18,19] It reduces the incidence of unrecognised oesophageal intubation and prevents morbidity and mortality. However, this technique may be of limited use in patients with large swellings of anterior neck, gross tracheal shift, short and stout neck, especially in the presence of extreme obesity. In these situations, identification of the trachea at the neck using sonography might be time-consuming and could delay detection of an oeophageal intubation, the chance of which is more in this subset of patients.
As ultrasound is as effective and quicker than X-ray for assessing the depth of tube insertion, especially in paediatric patients, the routine use of X-ray after tracheal intubation in the Intensive Care Units can be avoided.[20] Lung sonography is considered more sensitive than traditional upright chest radiography in detecting pneumothorax and it allows a rapid bedside evaluation of an unstable patient.[21]
Although M-mode of the ultrasound machine has been more often described to identify pneumothorax easily, it is useful to demonstrate the lung sliding also. The advantage being, with a single image the lung sliding can be documented. This is because, during respiration, the anterior chest wall moves less as compared to the lung. Hence, the chest wall above the pleura produces flat lines ('waves') on M-mode whereas normal lung sliding below pleural line will create a grainy appearance ('sand'), mimicking the appearance of waves on a beach or 'seashore sign'.[22,23]
As ultrasound machine is now considered an essential commodity in the field of practice of anaesthesia, either for aiding the performance of nerve blocks or for obtaining vascular access, the availability and accessibility of it to the anaesthesiologist have increased many folds. Since ultrasound machines are costly, it cannot be recommended as a mandatory monitor to be used routinely in obese and overweight patients. But as we increasingly come across overweight and obese patients in our daily practice nowadays, the use of ultrasound, if available, as an additional aid to confirm endotracheal intubation should be encouraged especially in the obese. Anaesthesia personnel can be easily trained to identify the lung sliding sign as it is not a difficult skill to attain.
One of the drawbacks of our study was the lack of randomisation, as recruitment into each group was based on BMI. Although the ultrasound was performed after auscultation, as both were performed by two different anaesthesiologists, the possibility of the ultrasound results being biased was minimal. But, observation of other signs such as expansion of chest during ventilation could have influenced the results.
CONCLUSION
Ultrasound-directed confirmation of endotracheal tube placement using sliding lung sign in overweight and obese patients can be superior in speed and accuracy as compared to the standard auscultatory method.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Juvin P, Lavaut E, Dupont H, Lefevre P, Demetriou M, Dumoulin JL, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003;97:595–600. doi: 10.1213/01.ANE.0000072547.75928.B0. [DOI] [PubMed] [Google Scholar]
- 2.Adams JP, Murphy PG. Obesity in anaesthesia and intensive care. Br J Anaesth. 2000;85:91–108. doi: 10.1093/bja/85.1.91. [DOI] [PubMed] [Google Scholar]
- 3.Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006;13:239–44. doi: 10.1197/j.aem.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Sim SS, Lien WC, Chou HC, Chong KM, Liu SH, Wang CH, et al. Ultrasonographic lung sliding sign in confirming proper endotracheal intubation during emergency intubation. Resuscitation. 2012;83:307–12. doi: 10.1016/j.resuscitation.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Álvarez-Díaz N, Amador-García I, Fuentes-Hernández M, Dorta-Guerra R. Comparison between transthoracic lung ultrasound and a clinical method in confirming the position of double-lumen tube in thoracic anaesthesia. A pilot study. Rev Esp Anestesiol Reanim. 2015;62:305–12. doi: 10.1016/j.redar.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Sustic A, Protic A, Cicvaric T, Zupan Z. The addition of a brief ultrasound examination to clinical assessment increases the ability to confirm placement of double-lumen endotracheal tubes. J Clin Anesth. 2010;22:246–9. doi: 10.1016/j.jclinane.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Kundra P, Mishra SK, Ramesh A. Ultrasound of the airway. Indian J Anaesth. 2011;55:456–62. doi: 10.4103/0019-5049.89868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002;28:701–4. doi: 10.1007/s00134-002-1290-x. [DOI] [PubMed] [Google Scholar]
- 9.Leone TA, Lange A, Rich W, Finer NN. Disposable colorimetric carbon dioxide detector use as an indicator of a patent airway during noninvasive mask ventilation. Pediatrics. 2006;118:e202–4. doi: 10.1542/peds.2005-2493. [DOI] [PubMed] [Google Scholar]
- 10.Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care. 2014;4:1. doi: 10.1186/2110-5820-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chapman IM. Obesity in old age. Front Horm Res. 2008;36:97–106. doi: 10.1159/000115358. [DOI] [PubMed] [Google Scholar]
- 12.Pfeiffer P, Rudolph SS, Børglum J, Isbye DL. Temporal comparison of ultrasound vs. auscultation and capnography in verification of endotracheal tube placement. Acta Anaesthesiol Scand. 2011;55:1190–5. doi: 10.1111/j.1399-6576.2011.02501.x. [DOI] [PubMed] [Google Scholar]
- 13.Pfeiffer P, Bache S, Isbye DL, Rudolph SS, Rovsing L, Børglum J. Verification of endotracheal intubation in obese patients – Temporal comparison of ultrasound vs. auscultation and capnography. Acta Anaesthesiol Scand. 2012;56:571–6. doi: 10.1111/j.1399-6576.2011.02630.x. [DOI] [PubMed] [Google Scholar]
- 14.Parab SY, Divatia JV, Chogle A. A prospective comparative study to evaluate the utility of lung ultrasonography to improve the accuracy of traditional clinical methods to confirm position of left sided double lumen tube in elective thoracic surgeries. Indian J Anaesth. 2015;59:476–81. doi: 10.4103/0019-5049.162983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adi O, Chuan TW, Rishya MA. Feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J. 2013;5:7. doi: 10.1186/2036-7902-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chou HC, Chong KM, Sim SS, Ma MH, Liu SH, Chen NC, et al. Real-time tracheal ultrasonography for confirmation of endotracheal tube placement during cardiopulmonary resuscitation. Resuscitation. 2013;84:1708–12. doi: 10.1016/j.resuscitation.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 17.Chou HC, Tseng WP, Wang CH, Ma MH, Wang HP, Huang PC, et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82:1279–84. doi: 10.1016/j.resuscitation.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 18.Abbasi S, Farsi D, Zare MA, Hajimohammadi M, Rezai M, Hafezimoghadam P. Direct ultrasound methods: A confirmatory technique for proper endotracheal intubation in the emergency department. Eur J Emerg Med. 2015;22:10–6. doi: 10.1097/MEJ.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 19.Galicinao J, Bush AJ, Godambe SA. Use of bedside ultrasonography for endotracheal tube placement in pediatric patients: A feasibility study. Pediatrics. 2007;120:1297–303. doi: 10.1542/peds.2006-2959. [DOI] [PubMed] [Google Scholar]
- 20.Alonso Quintela P, Oulego Erroz I, Mora Matilla M, Rodríguez Blanco S, Mata Zubillaga D, Regueras Santos L. Usefulness of bedside ultrasound compared to capnography and X-ray for tracheal intubation. An Pediatr (Barc) 2014;81:283–8. doi: 10.1016/j.anpedi.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 21.Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012;5:76–81. doi: 10.4103/0974-2700.93116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barillari A, Kiuru S. Detection of spontaneous pneumothorax with chest ultrasound in the emergency department. Intern Emerg Med. 2010;5:253–5. doi: 10.1007/s11739-010-0347-z. [DOI] [PubMed] [Google Scholar]
- 23.Johnson A. Emergency department diagnosis of pneumothorax using goal-directed ultrasound. Acad Emerg Med. 2009;16:1379–80. doi: 10.1111/j.1553-2712.2009.00542.x. [DOI] [PubMed] [Google Scholar]


