Abstract
This paper aims to observe the effects of total flavonoids of Radix Ilicis pubescentis on mouse model of cerebral ischemia reperfusion. Mice were orally given different doses of total flavonoids of Radix Ilicis pubescentis 10 d, and were administered once daily. On the tenth day after the administration of 1 h in mice after anesthesia, we used needle to hook the bilateral common carotid artery (CCA) for 10 min, with 10 min ischemia reperfusion, 10 min ischemia. Then we restored their blood supply, copy the model of cerebral ischemia reperfusion; We then had all mice reperfused for 24 h, and then took their orbital blood samples and measured blood rheology. We quickly removed the brain, with half of the brain having sagittal incision. Then we fixed the brains and sectioned them to observe the pathological changes of brain cells in the hippocampus and cortex. We also measured the other half sample which was made of brain homogenate of NO, NOS, Na+-K+-, ATP enzyme Mg2+-ATPase and Ca2+-ATPase. Acupuncture needle hook occlusion of bilateral common carotid arteries can successfully establish the model of cerebral ischemia reperfusion. After comparing with the model mice, we concluded that Ilex pubescens flavonoids not only reduce damage to the brain nerve cells in the hippocampus and cortex, but also significantly reduce the content of NO in brain homogenate, the activity of nitric oxide synthase (NOS) and increases ATP enzyme activity (P < 0.05, P < 0.01). In this way, cerebral ischemia reperfusion injury is improved. Different dosages of Ilex pubescens flavonoids on mouse cerebral ischemia reperfusion model have good effects.
Keywords: Total flavonoids of Radix Ilicis pubescentis, Cerebral ischemia reperfusion, Animal model
1. Introduction
Cerebral ischemia–reperfusion injury (CIRI) refers to the cerebral ischemia after restoration of perfusion. It not only recovers the brain and brain cell function, but also leads to hazardous situations, such as further tissue damage and dysfunction. Therefore, the CIRI induces high morbidity, high mortality and high disability rate of people. So it is called “three high” suggesting the characteristics of such disease (Yang et al., 2015). Ilex pubescens promotes blood circulation and removes blood stasis drugs. It can promote blood circulation (in Chinese it refers as Huoxue Tongmai). Other functions include acetanilide detumescence, detoxification efficacy. Pharmacological studies have shown that, Ilex pubescens protects the brain, improves its anti-inflammatory and immune function, and thus serves as clinical treatment for ischemic cerebrovascular disease, coronary heart disease, and thrombotic occlusion of vein phlogistic etc. (Li and Mao, 2011, Peng et al., 2015). This paper will report on the effect of total flavonoids of Mao Dongqing on mice that have cerebral ischemia reperfusion.
2. Materials and method
2.1. Experimental animal
Kunming mice, male, weighing 28 ∼ 32 g, were provided by the Experimental Animal Center of Hebei Province, with the certificate number: 1006019, and laboratory Certificate No. SYXK (Henan 2010-001).
2.2. Experimental drugs and reagents
Mao Dongqing that contains 52% of flavonoids, with batch number: 20100312; Chemical Analysis Laboratory of Henan University of Traditional Chinese Medicine; extract of Ginkgo biloba tablets (Jin Naduo), by Dr. Willmar Schwabe, with the batch number: 0601209; Nimodipine was from Shandong Xinhua Pharmaceutical Limited by Share Ltd production, batch number: 808170.
Sodium chloride injection and production, were provided by Zhengzhou Yonghe Pharmaceutical Co. Ltd. with batch number: 10062121; Chloral hydrate products by Shanghai Yamaura Chemical Co., with batch number: 2010302; Sodium carboxymethyl cellulose, with batch number of Fuchen Chemical Reagent Factory of Tianjin City: 20090826; formaldehyde solution, produced by Tianjin Kermel Chemical Reagent Co. Ltd., with the batch number: 20100601; Kaumas bright blue kit from Nanjing Jiancheng Bioengineering Institute, batch number: 20100626; ATP (Adenosine-triphosphate) kit from Nanjing Jiancheng Bioengineering Institute, batch number: 20100613; NO (Nitric oxide) detection kit from Nanjing Jiancheng Bioengineering Institute, batch number: 20100626; NOS (Nitric oxide synthetase) detection kit from Nanjing Jiancheng Bioengineering Institute, batch number: 20100626.
2.3. Experimental methods
2.3.1. Modeling and administration
We take the weight of 28 ∼ 32 g of Kunming mice 119, male, then evenly divide them into 7 groups, namely: sham operation group, model group, nimodipine group, Ginaton group, total flavonoids from Radix Ilecis pubescens large, medium and small dose group (n = 17). Except the sham operation group, the other 6 groups made transient cerebral ischemia–reperfusion model in mice. Large, small dose of Ilex pubescens flavonoids (300 mg/kg and 150 mg/kg, 75 mg/kg, with 0.1% CMC were prepared to 30 mg/ml, 15 mg/ml, 7.5 mg/ml suspension, volume 0.1 ml/10 g), Ginaton group (positive control drug, dosage is 40 mg/kg, 4 mg/ml in 0.1% CMC with mixed suspension, volume 0.1 ml/10 g), nimodipine group (positive control drug, dosage is 40 mg/kg, 4 mg/ml, 0.1% CMC, which is used for suspension, volume 0.1 ml/10 g), model group (fed with the same volume of 0.1% CMC), administered 1 times daily, administered continuously for 10 days. On the 10th day of fasting 12 h after the administration of 1 h and 10% chloral hydrate 0.03 ml/10 g intraperitoneal injection anesthesia (mice turn positive reflex), was used scissors to clip the neck hair and make the neck disinfected with alcohol. Then used a scalpel to median incision in the neck, gradually to separate the muscles around, until the bilateral common carotid artery (CCA), was seen and then bent tweezers stripping of peripheral nerve, separation of CCA, each artery with a diameter of about 0.3 mm acupuncture needle hook up, making approximately 90 degrees, 10 min of ischemia and restoration of perfusion for 10 min, ischemia reperfusion 10 min, and restoration of blood flow were done, and the mice were sutured. For sham operation group a surgical treatment in addition to blocking CCA was given, other operations being the same as of the model groups. In the first experiment on 119 mice, 32 rabbits died (death more complete second ischemia and 10 h after operation in the final 87), rats entered the result analysis.
2.3.2. Model evaluation criteria
The damage of mice cortical neurons by nerve injury was assessed. For each animal in Section 3, each slice section was similar. Then we selected the right hippocampus. Cortex was three times as high as that of the field (400 times) with the pathological scores of neural injury. Rating criteria are as follows: 0, no neuron injury; 1, scattered in the neuronal damage; 2, moderate degree of God the element damage (damaged neurons is less than the half); 3, severe neuronal damage (damaged neurons more than half); 4, extensive neuronal damage.
The results show: the display of a sham operation group cortical neurons in the reperfusion time points nerve have lower pathology scores; for ischemia again perfusion group mice cortex and hippocampus neurons appeared scattered arrangement of the cells, the nerve cell swelling obviously. It appears as deformation, its outline is not clear, with dark cytoplasm, nuclear pyknosis, nuclear week disappeared, neural cell autolysis and necrosis, a series of pathological changes of morphology, ischemia reperfusion group of nerve injury scores were increased (P < 0.05). Therefore, pathological outcome is that the animal model is the successful (Liu et al., 2010).
2.3.3. Observation items and indexes
After mice reperfusion for 24 h, we collected the orbital blood samples of all mice to measure their blood rheology. And then we euthanized mice by cervical dislocation by quickly taking the brain, and conducting sagittal incision on half of the brain. The we fixed the brain in 4% poly formaldehyde and 0.1 mol/L phosphate buffer (pH 7.4) for a week. Then we embedded the brain in paraffin and stained them by HE. The other half was put on a clean filter paper, and accurately weighed. We calculate the result according to the weight. Then we added cold saline volume, ratio of brain tissue (g): normal saline (ML) = 1:9 into 10% of brain homogenate, 4 DEG C, 3000r/min and the supernatant from – 20 DEG C cryopreservation were determined. No, NOS, Na+-K+-ATPase, Mg2+-ATPase and Ca2+-ATPase.
2.4. Statistical processing method
Data were analyzed with SPSS13.0 for windows medical statistics packages for data analysis. Measurement data between groups were compared using an analysis of variance. With the said, we use Ridit to test grade data.
3. Results
3.1. Effect on cerebral ischemia reperfusion injury in mice brain homogenate NO content
As what Table 1 shows when we compare the sham operation group with model group, we find that NO content in mice brain tissue has increased significantly (P < 0.01). It indicates that the modeling was successful. When we compare the Nimodipine group with the model group, the Ginaton group, relevant dose of total flavone can significantly reduce the content of nitric oxide (no) (P < 0.01).
Table 1.
Determination of NO content in brain homogenate. Effect of nitric oxide level in brain homogenate of total flavonoids of 1 Mao Dongqing on cerebral ischemia reperfusion injury in mice ().
| Group | Animal (Each) | Dosage (mg kg−1) | NO (μmol/gprot) | Mortality (%) |
|---|---|---|---|---|
| Sham | 17 | – | 11.66 ± 1.52△△ | 0.0 |
| The model group | 9 | – | 18.58 ± 8.61 | 47.1 |
| Nimodipine group | 12 | 40 | 13.63 ± 3.38△△ | 29.4 |
| Ginaton group | 12 | 40 | 12.84 ± 0.83△△ | 29.4 |
| High dose of total flavonoids of Mao Dongqing group | 13 | 300 | 12.57 ± 0.72△△ | 23.5 |
| In the dose of Mao Dongqing total flavonoids group | 12 | 150 | 14.34 ± 0.79△△ | 29.4 |
| A small dose of total flavonoids of Mao Dongqing group | 12 | 75 | 18.36 ± 1.30 | 29.4 |
Compared with the model group (Delta P < 0.05, Delta P < 0.01).
3.2. Effect on cerebral ischemia reperfusion injury in mice NOS activity in brain homogenate
Table 2 shows that compared with the sham operation group, model mice brain tissue of TNOs and iNOS activity increased significantly (P < 0.01), indicating a successful model. Compared with the model group, total flavone in the middle dose group, Ginaton group, and nimodipine group can significantly reduce the TNOs, iNOS activity (P < 0.01); small dose of total flavonoids of Radix Ilicis pubescentis can significantly reduce the TNOs activity (P < 0.05).
Table 2.
Determination of NOS activity results. Total Flavonoids of Mao Dongqing on cerebral ischemia–reperfusion injury in mice of the same nitrogen synthase activity in brain homogenates ().
| Group | Animal (each) | Dosage (mg kg−1) | INOS (U/mgprot) | TNOS f (U/mgprot) |
|---|---|---|---|---|
| Sham | 17 | – | 0.739 ± 0.098△△ | 2.184 ± 0.263△△ |
| The model group | 9 | – | 1.457 ± 0.747 | 4.202 ± 1.522 |
| Nimodipine group | 12 | 40 | 0.786 ± 0.129△△ | 2.679 ± 0.510△△ |
| Ginaton group | 12 | 40 | 0.718 ± 0.132△△ | 2.574 ± 0.672△△ |
| High dose of total flavonoids of Mao Dongqing group | 13 | 300 | 0.751 ± 0.106△△ | 2.184 ± 0.281△△ |
| In the dose of Mao Dongqing total flavonoids group | 12 | 150 | 0.998 ± 0.054△△ | 2.591 ± 0.140△△ |
| A small dose of total flavonoids of Mao Dongqing group | 12 | 75 | 1.175 ± 0.152 | 3.683 ± 0.316△ |
Compared with the model group, Delta P < 0.05, Delta P < 0.01.
3.3. Effect of transient cerebral ischemia reperfusion injury in mice brain tissue ATP activity
Table 3 shows that, compared with the sham operation group, model group mice brain tissue Na+-K+-ATP enzyme, Ca2+-ATP enzyme and Mg2+-ATP enzyme activity was significantly decreased (P < 0.01), indicating that the model was successful. Compared with the model group, high dose group of total flavonoids from Radix Ilecis pubescens, nimodipine group of Na+-K+-ATP enzyme, and Ca2+-ATPase and Mg ∼ (2+)-ATPase activity increased significantly (P < 0.01); as for the Ginaton group, its Ca2+-ATPase, and Na+-K+-ATP enzyme activity significantly increased (P < 0.01); the total flavonoids from Radix Ilecis pubescens middle dose group of Na+-K+-ATP enzyme activity increased significantly (P < 0.01); Ginaton group Mg2+-ATPase activity increased significantly (P < 0.05); and for the total flavone small dose group of Ca2+-ATPase activity and Mg2+-AT, its enzyme activity of P significantly increased (P < 0.05).
Table 3.
Determination of ATP enzyme activity results.
| Group | Animal (each) | Dosage (mg·kg−1) | Ca2+-ATPase (μmolPi/mgprot/h) | Mg2+-ATP enzyme (μmolPi/mgprot/h) | Na+-K+-ATP enzyme (μmolPi/mgprot/h) |
|---|---|---|---|---|---|
| Sham | 17 | – | 23.644 ± 3.015△△ | 16.650 ± 3.018△△ | 12.017 ± 0.943△△ |
| The model group | 9 | – | 11.726 ± 5.122 | 9.809 ± 3.934 | 5.879 ± 3.071 |
| Nimodipine group | 12 | 40 | 23.862 ± 5.814△△ | 16.761 ± 5.444△△ | 10.749 ± 1.661△△ |
| Ginaton | 12 | 40 | 21.344 ± 5.667△△ | 15.066 ± 2.095△△ | 10.377 ± 1.188△△ |
| High dose of total flavonoids of Mao Dongqing group | 13 | 300 | 24.569 ± 2.658△△ | 18.518 ± 3.117△△ | 12.449 ± 2.762△△ |
| In the dose of Mao Dongqing total flavonoids group | 12 | 150 | 21.447 ± 2.678△△ | 17.577 ± 2.483△△ | 10.583 ± 2.135△△ |
| A small dose of total flavonoids of Mao Dongqing group | 12 | 75 | 15.998 ± 2.192△ | 13.067 ± 1.782△ | 8.085 ± 1.474△ |
Compared with the model group (Delta P < 0.05, Delta P < 0.01).
3.4. Effect on cerebral ischemia reperfusion injury in mice model of pathomorphology
3.4.1. Effect of total flavonoids of Mao Dongqing mice brain nerve cells in the hippocampus pathological changes induced by cerebral ischemia reperfusion in Table 4, Fig. 1
Table 4.
Effect of total flavonoids of Mao Dongqing on mice brain nerve cells in the hippocampus pathological changes induced by cerebral ischemia reperfusion.
| Group | Animal (each) | Dosage (mg·kg−1) | − | + | ++ | +++ |
|---|---|---|---|---|---|---|
| Sham | 17 | – | 17 | 0 | 0 | 0 |
| The model group | 9 | – | 0 | 0 | 2 | 7 |
| Nimodipine group | 12 | 40 | 9 | 2 | 1 | 0 |
| Ginaton | 12 | 40 | 10 | 1 | 1 | 0 |
| High dose of total flavonoids of Mao Dongqing group | 12 | 300 | 10 | 1 | 1 | 0 |
| In the dose of Mao Dongqing total flavonoids group | 12 | 150 | 6 | 3 | 2 | 1 |
| A small dose of total flavonoids of Mao Dongqing group | 11 | 75 | 4 | 1 | 2 | 4 |
“−” nerve cells were normal. “+” few nerve cells mildly atrophy; “++” part of the nerve cells moderately atrophy with a few of cells with mild edema; “+++” all nerve cells severely atrophy or with partial cell moderate edema.
Figure 1.
Mao Dongqing flavonoids on cerebral ischemia reperfusion model in mouse hippocampus HE staining.
Effect of ATP enzyme activities in brain homogenate of total flavonoids in 3 Mao Dongqing on cerebral ischemia reperfusion injury in mice ().
By Ridit test, compared with sham operated group, the model group has significant pathological changes in the hippocampus nerve cells (P < 0.01), indicating that the model was successful. Compared with the model group, high dose of Ilex pubescens total flavone group, Ginaton group and nimodipine group can significantly reduce mouse brain nerve cells and induce pathological changes of the hippocampus (P < 0.05); small dose of Ilex pubescens flavonoid group of mouse brain nerve cells in the hippocampus of the physical changes only has a trend to reduce.
The hippocampus pathological observation showed: sham operation group showed no cerebral pathological changes in nerve cells of hippocampus. They were normal, neuronal nuclei. The nuclear chromatin is fluffy, clear nucleolus, as what can be seen in the photo 1of nerve cells of the hippocampus. Nerve cells of the hippocampus in the nimodipine group have the protective effect. Ginaton group, large dose of Ilex pubescens flavonoid group also has the protective effect as can be seen in.photo 3,4,5; it has a role in promoting a small dose of Ilex pubescens total flavone group, as can be seen photo 6,7.
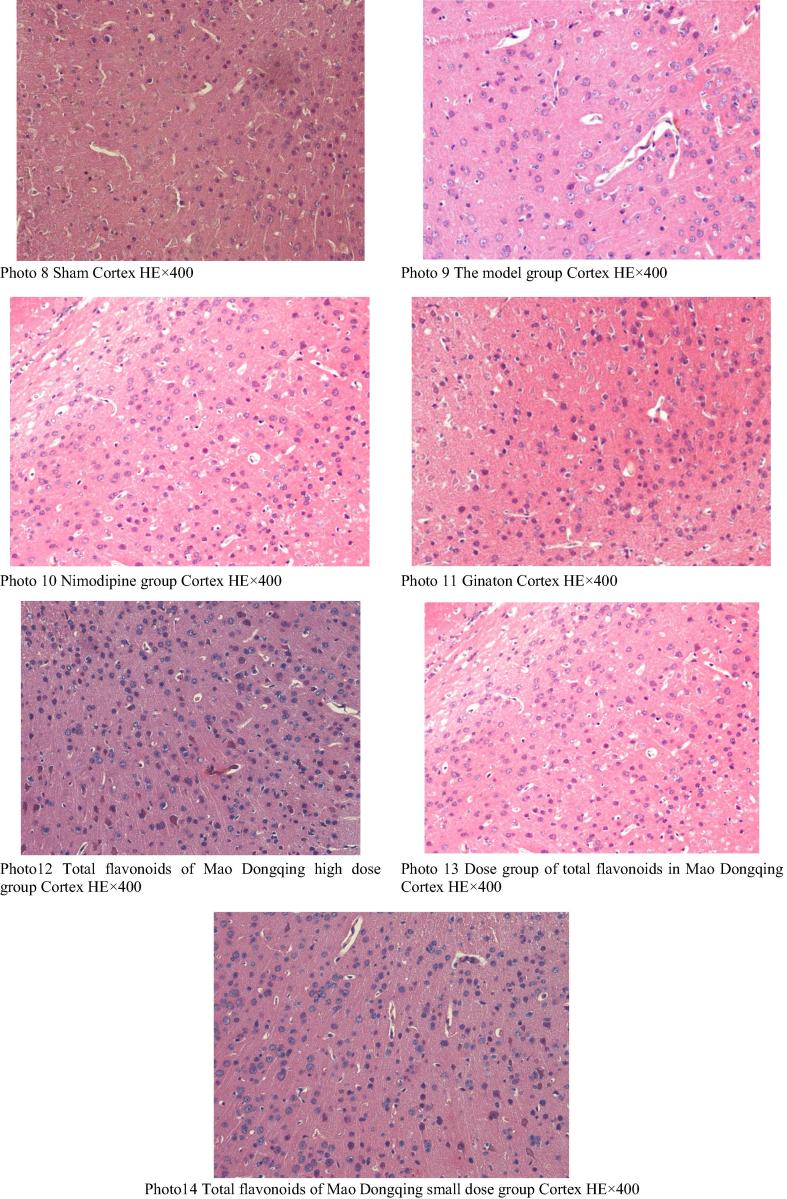
3.4.2. Effect of total flavonoids of Mao Dongqing on pathological changes of mice cerebral cortex nerve cells and on cerebral ischemia reperfusion in Table 5, Fig. 2
Table 5.
Effect of total flavonoids of Mao Dongqing mice cerebral cortex nerve cell pathological changes of cerebral ischemia reperfusion.
| Group | Animal (each) | Dosage (mg kg−1) | − | + | ++ | +++ |
|---|---|---|---|---|---|---|
| Sham | 17 | – | 17 | 0 | 0 | 0 |
| The model group | 9 | – | 0 | 0 | 2 | 7 |
| Nimodipine group | 12 | 40 | 10 | 2 | 0 | 0 |
| Ginaton | 12 | 40 | 9 | 1 | 2 | 0 |
| High dose of total flavonoids of Mao Dongqing group | 12 | 300 | 10 | 1 | 1 | 0 |
| In the dose of Mao Dongqing total flavonoids group | 12 | 150 | 8 | 2 | 1 | 1 |
| A small dose of total flavonoids of Mao Dongqing group | 11 | 75 | 5 | 2 | 2 | 2 |
“−” nerve cells was normal. “+” few nerve cells appeared mild atrophy; “++” part of the nerve cells appear moderate atrophy with a few of cells with mild edema; “+++” all nerve cells appeared severe atrophy or with partial cell moderate edema.
Figure 2.
Mao Dongqing flavonoids on cerebral ischemia reperfusion model in mouse cerebral cortex HE staining.
In the Ridit test, sham operation group, and the model group mice cerebral cortex nerve cells have significant pathological changes (P < 0.01), indicating a successful model. Compared with the model group, high dose of Ilex pubescens total flavone group, nimodipine group and Ginaton group had significantly less injury of nerve cells (P < 0.01). Small dose of Ilex pubescens flavonoid group in mouse cerebral cortex nerve cells had no significant effect (P < 0.05).
Cortex pathological observation showed that: the brain neurons in the cortex of the sham operation group and cells in the hippocampus had normal pathological changes, as what can be seen in photos 8; nerve cells of the hippocampus in the brains of the model group obviously atrophied or disappeared, associated with pathological changes such as obvious edema of nerve cells in the cerebral cortex, as can be seen in photo 9; as for Ginaton group, and high dose of total flavonoids from Radix Ilecis pubescens group, few nerve cells in their cerebral cortex had mild edema, and the nucleus was clear and their normal glial cells appear normal as can be, seen in photo 11, and photo 12; Few parts of the compared group, their brain cortex’s nerve cell will have obvious pathological changes. Such changes will be restored, mostly recovered to a certain extent, see photo. As for the small dose of hair total flavonoids of brain pathology group, a few parts of the nerve cells that had been changed were obviously recovered. Most of them have been restored, see photo 13, 14.
4. Discussions
Epidemiological studies show that as China’s aging population expands, deaths caused by cerebrovascular disease increase. Cerebrovascular disease now ranks the top three. Ischemic cerebrovascular disease accounts for 80% of all the cerebral vascular disease, not only affects the patient's daily work and life, but also increases the family and social burden of medical treatment (Wang et al., 2013). Inhibiting the ischemia and reperfusion injury has become the key link in the treatment of ischemic cerebrovascular diseases.
Cerebral ischemia reperfusion injury (CIRI) leads to neurological damage. In Chinese medicine, a “stroke” category (Zhao and Zhu, 2015) is the ischemic semi dark band visible for blood micro indications. Edema can be observed through the indication of phlegm. Therefore, we are able to differentiate two syndromes, such as “phlegm” and “blood stasis”. The treatments of blood and phlegm are Shu and Tongluo respectively. In recent years, with further researches on Ciri rats, and rapid development of modern pharmacology in traditional Chinese medicine, the study variety has been extended to include expectorant Xingshen, (breathing and resuscitation), Yiqi Bushen (replenishing qi and tonifying the kidney), Huazhuo Jiedu (resolving turbidity and toxin) (Zhao et al., 2011). The efficacy of traditional Chinese medicine, even the development of many new Chinese herbal medicines and its extract are also included in these areas.
Modern research shows that cerebral ischemia, reperfusion injury appears as calcium overload, brain edema, excitotoxicity, and oxidative stress (Yu et al., 2015). Energy metabolism disorder is believed to be ischemia and reperfusion cell injury is the initiating factor. Metabolic toxins trigger a chain reaction, and intracellular Ca2+ overload will lead to neuronal death. Main drugs for this disease include cerebral protection agents, calcium antagonistic agent (such as the Nimmo equality) and free radical scavenger (e.g., edaravone, mannitol, etc.) (Wang et al., 2014, Fu et al., 2014), nerve growth factor, excitatory amino acid receptor antagonist, mitochondrial protection agent (such as butyl benzene skin) and others. Most of them belong to the single-factor protective agent. Clinical applications have strict indications, so we have not yet determined which drug or treatment obtains the ideal effect.
The dry roots of Ilex pubescens plant (or holly of Ilex genus) are able to promote blood circulation and remove blood stasis. This is a kind of traditional Chinese medicine. The main effective components of hairy holly roots contain flavonoid glycosides, phenols, sterol, tannins, triterpenes and numerous other chemical constituents. Pharmacological studies have shown that, holly (or Mao Dongqing) has the effect of promoting blood circulation and removing blood stasis. It soothes swelling and pain, and has heat clearing and detoxifying effect (Lv, 2015), it is antihypertensive, anticoagulation and protects cerebral tissue. It is anti-inflammatory and improves immune system. In a word, Mao Dongqing is one clinical treatment of ischemic cerebrovascular disease. The study showed that total flavonoids from Radix Ilecis pubescens significantly reduced the blood stasis associated with cerebral ischemia in model rats. It has good effect on rats’ whole blood viscosity, and improves their brain nerve cells in the hippocampus. All in all total flavonoids from Radix Ilecis pubescens have a good effect on the model rats that have cerebral ischemia (Cheng et al., 2012).
Before using rats, in recent years, people try to use different kinds of animal models of cerebral ischemia reperfusion injury. Due to the small difference in the body weight of the mice, the success rate of the mice model is high. What’s more mice models have brains that are close to human brains as for cerebral ischemia or cerebral infarction reperfusion. Brain tissues of mice and human have similar pathological and physiological evolution process, so scholars have used mice to make cerebral ischemia reperfusion model (Wang and Tension, 2011). And because male mice have less estrogen which has a protective effect on brain injury, many scholars choose male mice. (Guo and Xiao, 2012).
The research showed that on cerebral ischemia stage, the metabolism of the body generated large amounts of NO, and increased the activity of NOS. This phenomenon was induced by glutamate excitotoxicity, which aggravated the injury of ischemia reperfusion (Chen et al., 2012). The study found that NO content decreased and the aged rats with cerebral ischemia reperfusion injury on brain tissues were damaged. The experimental results show that the total flavonoids from Radix Ilecis pubescens reduced NO level and NOS in mice with cerebral ischemia and reperfusion injury, reducing transient cerebral ischemia reperfusion injury of the mice. From observing each mouse and their death, the mortality of the model group was higher than that of the treatment group and high dose group of Ilex pubescens flavonoids had the lowest mortality rate. It showed that the medication in each group of ischemia and reperfusion in mice has a protective effect.
Energy metabolism disorder is one of the main pathological mechanisms of cerebral ischemia (Liu et al., 2011). Cerebral ischemia and reperfusion appears microcirculation, inadequate supply of oxygen and glucose, ATP was rapidly depleted, mitochondrial ATP synthase failure, resulting in ATP dependent enzymes (including Ca2-ATP enzyme and Na+-K+-ATPase enzyme activity decreased, resulting in a massive outflow of intracellular K+, Na+, Cl− and Ca2+ large inflows of cells, resulting in cell, ion imbalance. In addition, the brain ischemia leads to the significant increase of lactic acid, metabolic acidosis. It also increased intracellular H+ content, promoted Na+, H+ exchange. As a result, more Na+ flowed into cells. Sodium and water retention were caused by cytotoxic cerebral edema (Genovese et al., 2011, Wen et al., 2016). This experiment is affected by determination of ATP enzyme activity reaction Mao Dongqing flavonoids on cerebral ischemia reperfusion injury. The results showed that total flavonoids of Ilex pubescens can improve the ATP activity of brain tissue in mice, improving brain energy metabolism. So Mao Dongqing has a good effect on cerebral ischemia reperfusion injury.
Brain tissue sections can be intuitive reaction of brain cell volume size and cause changes in the cytoplasm, nucleus, cytoplasm and so on. Transient cerebral ischemia will lead to damaged neurons in the brain. More serious phase will cause cell apoptosis. Hippocampus CAI area is the most sensitive to ischemia and hypoxia of brain tissue. The damage can cause the decline of learning ability and bad memory. The hippocampus was dissected in fiber position and contact, suggesting that in brain function, it plays a key role (Li and Li, 2015). So in this study we took HE staining method, choosing the CA1 region of the hippocampus and the cortex for pathological view observation. And the objective study and the pathological observation showed: Mao Dongqing flavonoids can improve the histopathological changes in brain, improving the cerebral ischemia reperfusion injury.
The long-term experimental results of Ilex pubescens show, Ilex pubescens flavonoids can reduce brain tissue in the hippocampus and reduce the cortex nerve cell damage. It can also significantly reduce brain homogenate of No and NOS. It increases brain homogenate ATP enzyme activity, by improving cerebral tissue pathology change and regulation related biochemical indexes. In this way, cerebral ischemia reperfusion injury is improved, and the high dose effect is the best. The laboratory study shows that, Mao Dongqing has both heat clearing and detoxifying, effect. It not only promotes blood circulation and removes blood stasis. As one of the traditional Chinese medicines, it can prevent cerebral ischemia and provide a new train of thoughts on cerebral ischemia reperfusion injury treatments. The use of drugs on cerebral ischemia reperfusion injury has certain change. The good effect of the treatment of cerebral ischemic reperfusion injury is of great significance, and will become a new Mao Dongqing clinic.
Acknowledgement
This research is supported by the national major new drug “Special Science and Technology” (batch number: 2009ZX09103-324); the team of outstanding scientific and technological innovation in Henan province (TCJ2014-391); as well as the science and technology innovation team of Zhengzhou City (131PCXTD612).
Footnotes
Peer review under responsibility of King Saud University.
References
- Chen Y.M., Chen T.P., Feng H.L. Present situation of injury mechanism and treatment of cerebral ischemia reperfusion. Med. Res. Educ. 2012;06:47–54. [Google Scholar]
- Cheng X., Zhang X.L., Miao M.T. The influence of Mao Dongqing flavonoids on rat cerebral ischemia model. Clin. Pharmacol. 2012;06:640–643. [Google Scholar]
- Fu W., Liu Z.L., Feng B. Electrospun gelatin/PCL and collagen/PLCL scaffolds for vascular tissue engineering. Int. J. Nanomed. 2014;9:2335–2344. doi: 10.2147/IJN.S61375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genovese T., Mazzon E., Paterniti I. Neuroprotective effects of olprinone after cerebral ischemia/reperfusion injury in rats. Neurosci. Lett. 2011;503(2):93–99. doi: 10.1016/j.neulet.2011.08.015. [DOI] [PubMed] [Google Scholar]
- Guo X.L., Xiao W. Analysis of influence factors of arterial occlusion of cerebral ischemia animal model with suture method in rats. J. Clin. Med. 2012;03:239–241. [Google Scholar]
- Li M.F., Li Z.J. Study on the model of ischemic brain injury. Apoplexy Nerv. Dis. 2015;06:385–388. [Google Scholar]
- Li X.R., Mao D.Q. Review on pharmacological effects of. Glob. Chin. Med. 2011;03:238–240. [Google Scholar]
- Liu P.G., Du Y., Zhao X.F., Wang S. Cerebral ischemia animal model evaluation method of. Liaoning J. Trad. Chin. Med. 2010;(7):1396–1397. [Google Scholar]
- Liu M., Sun J.N., Dong S.F., Liu Y., Xuan Z.Y. Study on the changes of cerebral energy metabolism in different time after cerebral ischemia reperfusion in rats. J. Clin. Exp. Pathol. 2011;05:216–218. [Google Scholar]
- Lv Y.Y. Study on the clinical application of Mao Dongqing. Inner Mongolia Trad. Chin. Med. 2015;07:148–149. [Google Scholar]
- Peng W.X., Lin Z., Wang L.S., Wu J.G. Effect of weakly alkaline salt pretreatment on bio-boards for medicine safety. J. Pure Appl. Microbiol. 2015;9(3):1913–1917. [Google Scholar]
- Wang Tension S. Preparation and evaluation of animal model of cerebral ischemia and cerebral ischemia reperfusion injury. Neuropharmacol. Sinica. 2011;03:31–40. [Google Scholar]
- Wang J.M., Zhou W.H., Cheng G.Q. Maximum length sequences brainstem auditory evoked potential changes in head hypothermia in newborn piglets with hypoxic ischemic brain injury in. China J. Contemp. Pediatr. 2013;6:484–489. [Google Scholar]
- Wang H.M., He Y.G., eosin L., Li H.B. Cerebral ischemia/reperfusion injury and treatment of. J. Hebei Union Univ. (Medical Science Edition) 2014;02:186–188. [Google Scholar]
- Wen, H.X., Liu, X.J., Wang, H., Caputo, Y., 2016. The influence of financial constraint and agency cost on investment inefficiency of GEM Listed Firms-Based on Two-Tier stochastic frontier model, 39(2), 584-592
- Yang W., Liu S., Fan X.J. Effect of huatantongluo in acute cerebral ischemia reperfusion injury TNAF-2 and Ask1 protein. Liaoning J. Trad. Chin. Med. 2015;12:2439–2441. [Google Scholar]
- Yu H.J., Feng X.Y., Xin S.M., Li H. Protective effect of pretreatment by NF- B signaling pathway in rat cerebral ischemia reperfusion injury of dl-3-n-butylphthalide injection. J. Apoplexy Nervous Dis. 2015;12:1119–1121. [Google Scholar]
- Zhao X.X., Zhu M.Z. Research overview of kidney and brain Tongzhi prevention and treatment of ischemic stroke. Lishizhen Med. Chinese Med. 2015;12:2988–2990. [Google Scholar]
- Zhao J.W., Tian J.B., Li D.G. Huazhuo Jiedu Huoxue Tongluo method on cerebral ischemia reperfusion injury in rats and to study the small sea horse nerve cell morphology influence. Med. J. 2011;5217:1492–1495. [Google Scholar]