Abstract
Aim:
Large-scale population-based screening studies have identified lip lesions to be the most common oral mucosal lesions; however, few studies have been carried out to estimate the prevalence of lip lesions exclusively. The aim of present study is to highlight the diversity of lip lesions and determine their prevalence in an unbiased Indian population.
Materials and Methods:
Lip lesions were selected from 3009 patients who visited the department over a period of 3 years (January 2012 to December 2014). Age, sex, location of lip lesions, a detailed family and medical history, along with the history of any associated habit was recorded. Biopsy was carried out in necessary cases to reach a final diagnosis. The pathologies of the lip were classified based on the etiology.
Results:
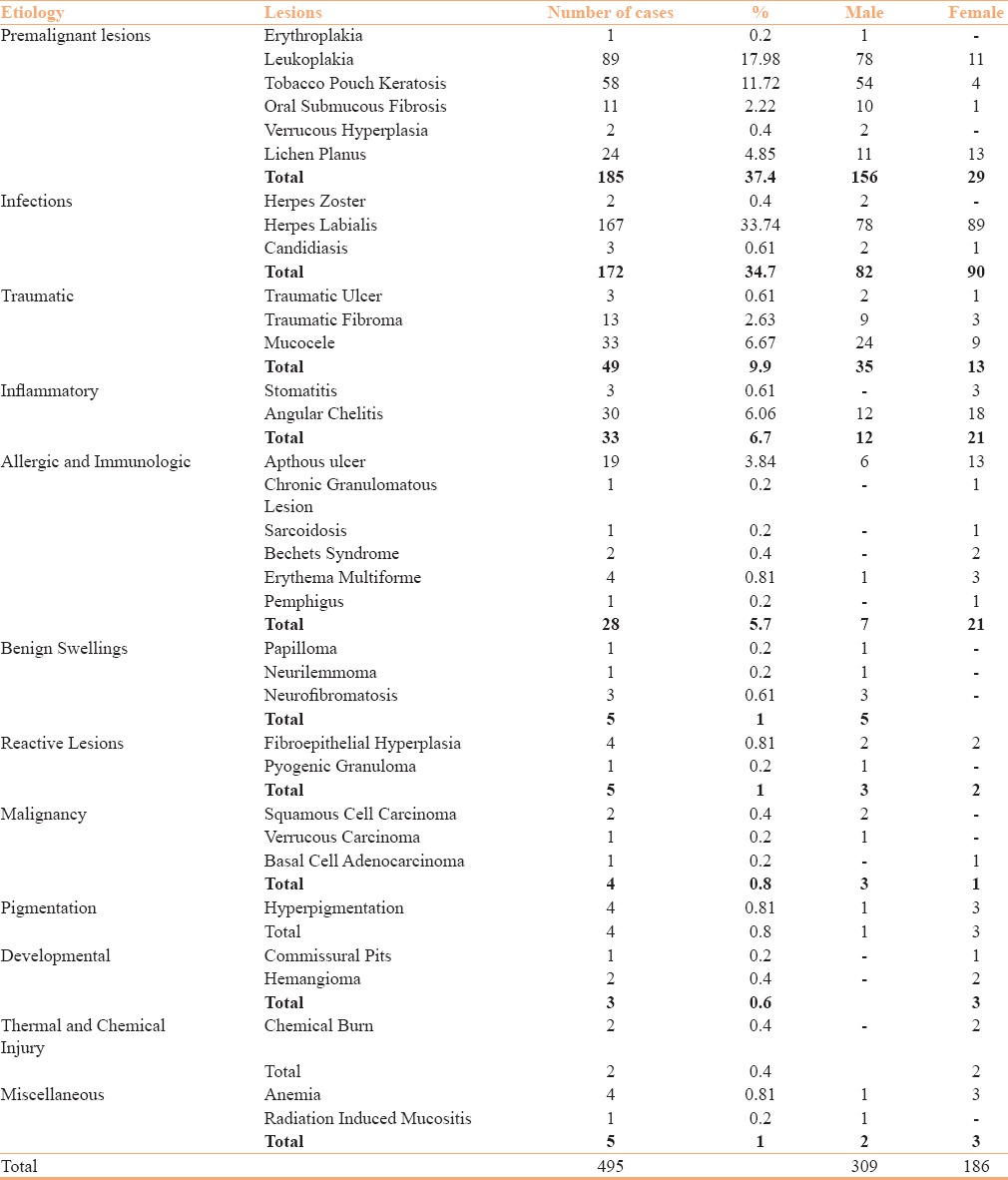
Among 3009 patients, 495 (16.5%) had lip lesions ranging from 4 years to 85 years with a mean age of 39.7 years. There were 309 (62.4%) males and 185 (31.9%) females. Lower lip was the most affected region (54.1%) followed by the corner of the mouth (30.9%) and upper lip (11.7%). In 3.2% of the cases, both the lips were involved. Of the 495 lip lesions, the most common were Potentially Malignant Disorders (PMDs) (37.4%), herpes labialis (33.7%), mucocele (6.7%), angular cheilitis (6.1%), and allergic and immunologic lesions (5.7%).
Conclusion:
Lip lesions may act as an indicator for the presence of an underlying systemic disease. PMDs and infections were the most common lip lesions in the present study.
Keywords: Herpes labialis, Indian, lip, PMDs
Introduction
Lips are highly susceptible to environmental effects, such as wind, sun, smoking, and temperature extremes, because of their poor skin barrier function and low water retaining capacity.[1,2,3] Large-scale population-based screening studies have identified lip lesions to be the most common oral mucosal lesions; however, few studies have been carried out to estimate the prevalence of lip lesions exclusively.[4,5,6,7] The present study aims to highlight diversity of lip lesions and determine their prevalence in an unbiased Indian population.
Material and Methods
Patients with lip lesions were selected from a total of 3009 patients who visited the department over a period of 3 years (January 2012 to December 2014). Age, sex, location of lip lesions, a detailed family and medical history, along with the history of any associated habit such as smoking, tobacco chewing, and alcohol consumption was recorded.
Examination of lips
The classification proposed by Roed–Petersen and Renstrup[8] was used to understand the topography of lip. The color, texture, and any surface abnormalities of the vermillion border, lower labial mucosa, upper labial mucosa, labial commissures, and skin of the lip was noted. Regional nodes were also checked.
The pathologies of the lip were classified based on the etiology as (1) developmental, (2) inflammatory, (3) potentially malignant disorders (PMDs), (4) infection, (5) traumatic, (6) reactive, (7) thermal and chemical injury, (8) benign and malignant neoplasms, (9) allergic and immunologic, (10) pigmented, and (11) miscellaneous.
The Institutional Ethics Committee of Nair Hospital Dental College (IEC-NHDC) approved the study. It was designed according to the principles manifested in the Declaration of Helsinki and consistent with the guidelines of Good Clinical Practice given by the International Conference of Harmonization (ICH-GCP). A written informed consent was obtained from all patients.
Results
Among the 3009 examined patients, 495 (16.5%) had lip lesions, of which 257 were biopsied to identify the underlying cause.
The age of the patients ranged from 4 years to 85 years, with a mean age of 39.7 years. There were 309 (62.4%) males and 185 (31.9%) females. Lower lip was the most affected region (54.1%) followed by the corner of mouth (30.9%) and upper lip (11.7%). In 3.2% of the cases, both the lips were involved.
Of the 495 lip lesions, the most common were PMDs (37.4%) and herpes labialis (33.7%), followed by mucocele (6.7%), angular cheilitis (6.1%), allergic and immunologic lesions (5.7%), traumatic fibroma (2%), neoplasms (1.8%), pigmentation (0.8%), developmental (0.6%), thermal and chemical injury (0.4%), and miscellaneous (1%) [Table 1].
Table 1.
Prevalence and gender distribution of varied lip lesions in 3009 patients
Discussion
The prevalence of lip lesions in our study was found to be 16.5% similar to that reported from Brazil (16.6%);[6] however, lower than that observed in Caucasian Americans (18.5%)[4] and Indian patients (18.8%).[7] The reported difference may be due to geographical variations, ethnicity, social and cultural settings, study design, and diagnostic criteria.
PMDs were found to be the most common lip pathology in the present study, with a prevalence rate of 37.4%, which is significantly higher than that reported in Caucasian Americans (31.4%)[4] and Indians (20.6%).[7] Our study showed that leukoplakias [Figure 1a and b], oral submucous fibrosis (OSMF), verrucous hyperplasia [Figure 1c and d] and tobacco pouch keratosis was more prevalent in males whereas oral lichen planus (OLP) [Figure 1e and f] was more common in females. Burning sensation and inability to open mouth to its normal range was the most common presenting sign associated with OLP and OSMF.
Figure 1.
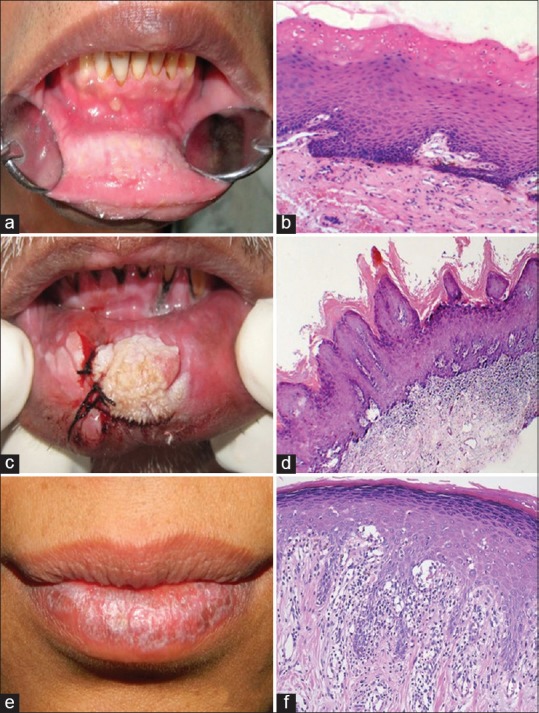
(a) Oral leukoplakia: A non-scrapable, fissured gray-white lesion; (b) parakeratotic hyperkeratosis with acanthosis (Hematoxylin and eosin; 100×); (c) verrucous hyperplasia; fissured gray-white lesion; (d) hyperplastic orthokeratinized squamous epithelium thrown into verrucous folds suggestive of verrucous hyperplasia. (Hematoxylin and eosin; 40×); (e) oral Lichen Planus; White reticular striae seen on lower lip; (f) basal cell layer degeneartion with sub-epithelial inflammatory cell infiltrate suggestive of lichen planus. (Hematoxylin and eosin; 100×)
Clinically, leukoplakia and OLP may sometimes resemble each other. Leukoplakia is a tobacco associated lesion, which clinically presents as a non-scrapable white patch, whereas OLP is an autoimmune, mucocutaneous disease with a bilateral occurrence clinically presenting as a white striation, papule, plaque, or erosion.[9] Population based studies from across the globe have shown that leukoplakias have a relatively high rate of malignant transformation because of its strong correlation with tobacco and alcohol use.[10] In the present study, incidence of smokeless tobacco was found to be higher as compared to smoked tobacco.
Infection (34.7%) was found to be the second most common lip pathology in the present study, similar to 32.6% observed by Patil and Maheshwari.[7] Herpes labialis (33.7%) [Figure 2a] with predominance in females (53.9%) presented with unilateral (87%) distribution of ruptured and ulcerated vesicles. In Caucasian Americans, prevalence of 8.5% for herpes labialis was reported.[4] Herpes Zoster [Figure 2b], a localized, painful, cutaneous eruption, was seen in two patients. Oral candidiasis, most common oral fungal infection,[11] was observed in 3 cases, with history of asthma and tuberculosis, thereby revealing the underlying cause for the infection.
Figure 2.

(a) Acute outbreak of clusters of herpetic vesicles; (b) unilateral presentation of vesicles on the left commissure of mouth and left half of palate associated with pain suggestive of herpes zoster; (c) aphthous ulcers; (d) Behcet's Syndrome-Recurrent multiple painful apthous ulceration of the oral cavity with genital ulcers
On the lip, we found recurrent apthous ulcers (RAUs) [Figure 2c] and angular cheilitis with a prevalence of 3.8% and 6.1%, respectively. Among Caucasian Americans,[4] a prevalence of 6.3% was observed for angular cheilitis. In our patients, various causes for angular cheilitis could be attributed to iron deficiency anemia, reduced vertical dimensions, pooling of saliva at the corner of the mouth, and immunosuppresion. RAUs are one of the most common oral mucosal pathologies triggered by a variety of causative agents, primary being stress.[12] Two diagnosed cases of Behcet's syndrome [Figure 2d], multisystemic chronic inflammatory disease[13] characterized by recurrent oral and genital ulcers, and other manifestations were included in the present study.
Oral vesiculobullous diseases may be immunologically mediated, viral, drug induced, hereditary, or traumatic in origin, and may occur independently or precede cutaneous involvement.[14] We report 4 cases of erythema multiforme (EM) and a case of pemphigus vulgaris occuring in the oral cavity with no cutaneous involvement. Characteristic target lesions and edema of the lips were seen in EM. In another study conducted in an Indian population, a prevalence rate of 0.2% was observed, which was lower than that seen in the present study (1%).[7]
Ntomouchtsis et al.[5] reported 27.6% of benign lip lesions in Greek patients, which included actinic keratosis, hemangioma, pyogenic granuloma, and mucocele as a benign neoplasm. Researchers have included various lesions in the category of benign oral neoplasms which are not true benign lesions, making a comparative study difficult. In the present study, 1% of the cases (n = 5) of lip were benign neoplasms, which included 3 neurofibromas, including a case of neurofibromatosis [Figure 3a and b] and a case each of neurilemmoma [Figure 3c and d] and papilloma. Studies have shown a prevalence of 3.4% and 7.9% for papilloma on lip in Greek and Caucasian American patients, respectively.[4,5]
Figure 3.
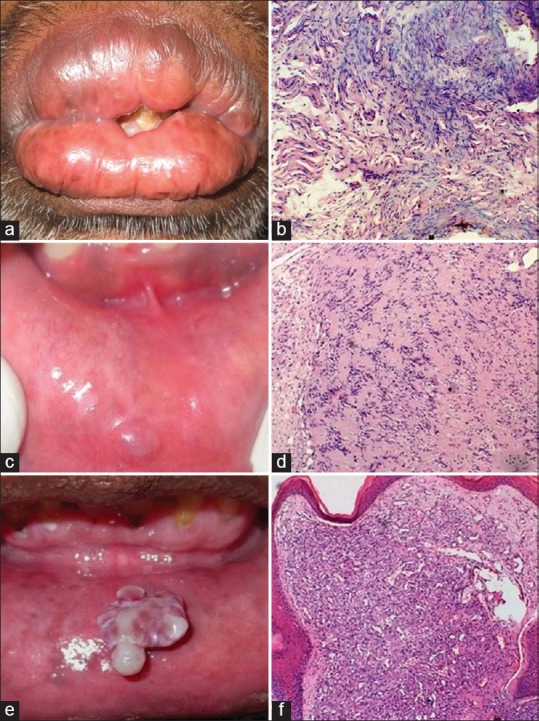
(a) Diffuse fibrous enlargement of the lips in a 42-year-old male in a case of neurofibromatosis, (b) spindle-shaped cells with wavy nuclei confirming the diagnosis of neurofibromatosis (Hematoxylin and eosin; 100×), (c) soft painless nodular growth on the lower lip of a 51-year-old male patient since 1 year with a history of trauma; (d) streaming fascicles of spindle-shaped cell arranged in Antoni A and Antoni B arrangement suggestive of neurilemmoma. (Hematoxylin and eosin; 100×); (e) ulcerated and lobulated mass on lower labial mucosa; (f) lobular pattern with multiple dilated capillaries and inflammatory cell infiltrate suggestive of pyogenic granuloma (Hematoxylin and eosin; 40×)
Localized fibrous tissue overgrowths are very common in oral mucosa due to constant irritation, majority being fibrous hyperplasia.[15] We found 13 cases of fibrous hyperplasia, which were not considered as true fibromas and were thus included in traumatic lesions category. The extremely low frequency of occurrence of true fibromas was also highlighted by Barker and Lucas[16] and Bouquot et al.[17] in their study.
We found a single case of pyogenic granuloma [Figure 3e and f] on the lower lip. Mucocele [Figure 4a and b] (33/495, 6.7%) was the most common sequelae to lip biting with a prevalence of 94% on the lower lip. Other studies have reported 4.7%, 7.1%, and 29.8% occurrence.[4,5,6,7]
Figure 4.
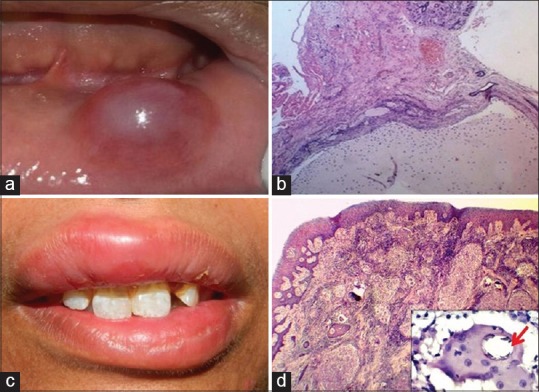
(a) Dome-shaped translucent swelling on the lower lip with a history of lip biting suggestive of mucocele; (b) well-circumscribed cyst-like cavity filled with spilled mucin and devoid of epithelial lining suggestive of mucocele (Hematoxylin and eosin; 40×); (c) persistent, nontender, diffuse enlargement of the lips and gingiva of a 19-year-old female since a year; (d) connective tissue showing dense chronic inflammatory cell infiltrate with Langhan's type of giant cells attempting to form granulomas (Hematoxylin and eosin; 40×). Inset shows calcified Schaumann body suggestive of sarcoidosis (Hematoxylin and eosin; 400×)
The lips account for 12% of all head and neck cancers.[18] We found 0.8% cases (4/495) of lip malignancies, which is lower than that reported by Patil and Maheshwari (2.24%),[7] whereas Bouquot and Gundlach reported a prevalence rates of 0.8/1000 among Caucasian American population.[4] We came across a case of basal cell adenocarcinoma in the upper lip.
Other lesions observed were hyperpigmented lesions (0.8%), anemia (0.8%), traumatic ulcer (0.6%), and radiation-induced mucositis (0.2%). Developmental lesions were seen in 0.6% of the study group. No clefts of lip were observed because they are surgically corrected early in life. Though we found only 2 cases of hemangiomas of lip, Bouquot and Gundlach[4] observed 12.6% of hemangiomas on the lip, the second most common surface alterations in their study.
Along with histopathological examination, few investigative procedures were carried out to reach a definitive diagnosis for treatment planning and better prognosis. Elevated serum anti-desmoglein 1 and 3 antibody levels along with suprabasilar split of the epithelium on histopathology confirmed pemphigus vulgaris, C3 and IgM deposition on direct immunofluorescence established the diagnosis of erythema multiforme, presence of hilar lymphadenopathies on chest radiograph (PA view), elevated serum angiotensin converting enzyme levels in addition to the presence of Schauman Bodies [Figure 4c and d] were diagnostic of sarcoidosis and ultrasonography was performed to diagnose the case of hemangioma. Special stains such as periodic acid Schiff stain for candidiasis, acid fast bacilli stain to rule out the presence of Mycobacterium in chronic granulomatous lesions were carried out. Blood investigations were conducted to confirm anemia.
Our study highlights the fact that lip lesions may act as an indicator for the presence of an underlying systemic disease. Granulomatous lesions manifesting on the lip can be biopsied to rule out underlying systemic cause such as sarcoidosis or tuberculosis. Early diagnosis and treatment of labial dermatoses can usually lead to complete cure. This helps to maintain patients’ social acceptance and self-esteem. In the present study, habit associated white lesions, herpes labialis, and mucocele were found to be more common in the lower lip. Angular cheilitis, herpes labialis were located at the commissures of the mouth with bilateral and unilateral involvement, respectively.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ya-Xian Z, Suetake T, Tagami H. Number of cell layers of the stratum corneum in normal skin-Relationship to the anatomical location on the body, age, sex and physical parameters. Arch Dermatol Res. 1999;291:555–9. doi: 10.1007/s004030050453. [DOI] [PubMed] [Google Scholar]
- 2.Kobayashi H, Tagami H. Functional properties of the surface of the vermilion border of the lips are distinct from those of the facial skin. Br J Dermatol. 2004;150:563–7. doi: 10.1046/j.1365-2133.2003.05741.x. [DOI] [PubMed] [Google Scholar]
- 3.Zugerman C. The lips: Anatomy and differential diagnosis. Cutis. 1986;38:116–20. [PubMed] [Google Scholar]
- 4.Bouquot JE, Gundlach KK. Odd lips: The prevalence of common lip lesions in 23,616 white Americans over 35 years of age. Quintessence Int. 1987;18:277–84. [PubMed] [Google Scholar]
- 5.Ntomouchtsis A1, Karakinaris G, Poulolpoulos A, Kechagias N, Kittikidou K, Tsompanidou C, et al. Benign lip lesions. A 10-year retrospective study. Oral Maxillofac Surg. 2010;14:115–8. doi: 10.1007/s10006-009-0196-y. [DOI] [PubMed] [Google Scholar]
- 6.Osterne RL, Costa FW, Mota MR, Vidal Patrocínio RM, Alves AP, Soares EC, et al. Lip lesions in a Brazilian population. J Craniofac Surg. 2011;22:2421–5. doi: 10.1097/SCS.0b013e318232a7dc. [DOI] [PubMed] [Google Scholar]
- 7.Patil S, Maheshwari S. Prevalence of lip lesions in an Indian population. J Clin Exp Dent. 2014;6:e374–8. doi: 10.4317/jced.51597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roed-Petersen B, Renstrup G. A topographical classification of the oral mucosa suitable for electronic data processing. Its application to 560 leukoplakias. Acta Odontol Scand. 1969;27:681–95. doi: 10.3109/00016356909026317. [DOI] [PubMed] [Google Scholar]
- 9.Shafer W, Hine M, Levy B. Textbook of Oral Pathology. 6th ed. India: Elsevier Publication; 2009. pp. 799–800. [Google Scholar]
- 10.Van der Waal I. Potentially malignant disorders of the oral and pharyngeal mucosa; Terminology, classification and present concepts of management. Oral Oncol. 2009;45:317–23. doi: 10.1016/j.oraloncology.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 11.Muzyka BC. Oral fungal infections. Dent Clin North Am. 2005;49:49–65. doi: 10.1016/j.cden.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Preeti L, Magesh K, Rajkumar K, Karthik R. Recurrent aphthousstomatitis. J Oral Maxillofac Pathol. 2011;15:252–6. doi: 10.4103/0973-029X.86669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhee SH, Kim YB, Lee ES. Comparison of Behçet's Disease and Recurrent Aphthous Ulcer According to Characteristics of Gastrointestinal Symptoms. J Korean Med Sci. 2005;20:971–6. doi: 10.3346/jkms.2005.20.6.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zunt SL. Vesiculobullous disease of the oral cavity. Dermatol Clin. 1996;14:291–302. doi: 10.1016/s0733-8635(05)70357-0. [DOI] [PubMed] [Google Scholar]
- 15.Scully C. Swellings: Reactive Lesions. 1st ed. England: Wiley Blackwell; 2010. Oral Medicine and Pathology at a Glance; p. 49. [Google Scholar]
- 16.Barker DN, Lucas RB. Localised fibrous overgrowths of the oral mucosa. Br J Oral Surg. 1967;5:86–92. doi: 10.1016/s0007-117x(67)80031-3. [DOI] [PubMed] [Google Scholar]
- 17.Bouquot JE, Kanrste KH. Oral exophytic lesions in 23 616 white Americans over 35 years of age. Oral Surg Oral Med Oral Pathol. 1986;62:284–91. doi: 10.1016/0030-4220(86)90010-1. [DOI] [PubMed] [Google Scholar]
- 18.Padmavathy L, Rao L, Ethirajan N, Gunasekaran K, Krishnaswamy B. Verrucous carcinoma-Report on two cases. Indian J Dermatol. 2009;54:68–70. [Google Scholar]


