Abstract
Cancer immunotherapy has produced impressive clinical results in recent years. Despite the success of the checkpoint blockade strategies targeting cytotoxic T lymphocyte antigen 4 (CTLA-4) and programmed death receptor 1 (PD-1), a large portion of cancer patients have not yet benefited from this novel therapy. T cell immunoglobulin and mucin domain 3 (TIM-3) has been shown to mediate immune tolerance in mouse models of infectious diseases, alloimmunity, autoimmunity, and tumor Immunity. Thus, targeting TIM-3 emerges as a promising approach for further improvement of current immunotherapy. Despite a large amount of experimental data showing an immune suppressive function of TIM-3 in vivo, the exact mechanisms are not well understood. To enable effective targeting of TIM-3 for tumor immunotherapy, further in-depth mechanistic studies are warranted. These studies will also provide much-needed insight for the rational design of novel combination therapy with other checkpoint blockers. In this review, we summarize key evidence supporting an immune regulatory role of TIM-3 and discuss possible mechanisms of action.
Keywords: TIM-3, T cell subsets, tumor microenvironment, antitumor immune responses
1. Introduction
Immune checkpoint inhibitors targeting cytotoxic T lymphocyte antigen 4 (CTLA-4) and programmed death receptor 1 (PD-1) have been proven highly effective in fighting cancer. Ipilimumab—a fully humanized cytotoxic T-lymphocyte–associate-d antigen 4 (CTLA-4) antibody—was the first immune checkpoint inhibitor associated with an improvement in overall survival in a phase 3 study involving patients with metastatic melanoma [1,2]. Approximately 20% of patients treated with Ipilumumab had long-term survival [3,4]. Evidence suggests at least part of the mechanism of action of CTLA-4 monoclonal antibody (mAbs) functions by depleting regulartory T cells (Tregs) [5,6]. PD-1 is a key checkpoint molecule expressed in exhausted CD8+ T cells and Tregs. Blockade of PD-1 has achieved revolutionary clinical impact in many solid cancers [7,8,9,10,11,12,13,14,15,16,17,18]. Despite these encouraging results, large portions of cancer patients fail to respond to these therapies. One likely roadblock is the compensatory immune inhibitory pathways. Therefore, there is an urgent need to further improve these therapies by simultaneously targeting multiple immune checkpoint pathways.
T cell immunoglobulin and mucin domain 3 (TIM-3) has been recognized as a member of the TIM gene family, which includes TIM-1, TIM-3, TIM-4 in humans and Tim-1-8 in mice. TIM-3 is expressed on Th1, Th17, CD8+ T cells–cells of myeloid lineages [19,20,21] in mice. Engagement between TIM-3 and its ligands has been found to suppress Th1 and Th17 responses [22] and induce peripheral immune tolerance [23,24], supporting an inhibitory role of TIM-3 in T cell-mediated immune responses. TIM-3 expression also characterizes exhausted T cells during chronic infection [25,26,27,28]. In this setting, TIM-3-expressing CD4+ and CD8+ T cells produce reduced amounts of cytokine or are less proliferative in response to antigen [25,26,27,28]. Experiments with TIM-3 mAbs suggest that it plays a functional role in exhausted T cells. TIM-3 mAbs restores proliferation and enhances cytokine production in HIV-1-specific T cells in vitro [25]. Administration of TIM-3 and PD-1 mAbs synergistically control tumor growth [29,30,31,32]. These preclinical studies implicate an inhibitory role of TIM-3 in antitumor Immunity. However, the underlying mechanisms are not well understood and seemingly even contradictory to its well established T cell-stimulating function [33].
Herein, we summarize key evidence indicating an immune regulatory role of TIM-3. We further discuss possible mechanisms of action by which TIM-3 regulates immune responses in infectious immunity, autoimmunity, and tumor Immunity. We will discuss feasible approaches for targeting TIM-3 for cancer immunotherapy.
2. Molecular Characteristics of TIM-3, Its Ligands, and Signal Transduction
The TIM family is comprised of type I membrane proteins, which share a similar structure: a variable immunoglobulin domain (IgV), a glycosylated mucin domain of varying length in the extracellular region, and a single transmembrane domain [34,35,36,37,38,39]. With the exception of Tim-4, all TIM molecules also contain a C-terminal cytoplasmic tail with a conserved tyrosine-based signal motif [34,35,36,37,38,39]. There are six cysteines within the IgV domain of TIM-3, which makes this IgV domain different from others. Most TIM IgV regions contain four cysteines, which form two disulfide bridges that contribute to the formation of a unique binding surface [34]. In the classical IgV model, FG and CC’ loops are located at opposite ends of the domain, with a distance of 25 Å. However, in the TIM-3 protein, the CC’ loop is reoriented closer to the FG loop due to an additional disulfide bond [34,40]. Under this circumstance, a unique binding pocket (FG-CC′ cleft) is created, which is required for interactions with ligands of TIM-3 (Figure 1).
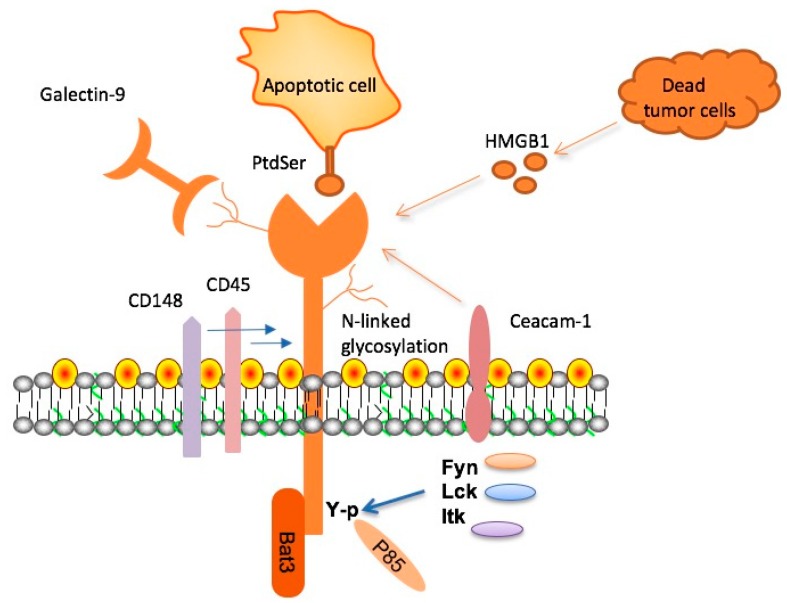
Figure 1.
T cell immunoglobulin and mucin domain 3 (TIM-3), its ligands, and signaling adaptor proteins. Four ligands—namely, galectin-9 (Gal-9), phosphatidylserine (PtdSer), high mobility group protein B1 (HMGB1), and carcinoembryonic antigen cell adhesion molecule 1 (Ceacam-1)—have been identified to bind to the variable immunoglobulin (IgV) domain of TIM-3. In terms of signaling, HLA-B associated transcript 3 (Bat-3) binds to the cytoplasmic tail of TIM-3 and inhibits TIM-3 function. Fyn, Lck, and Itk, three tyrosine kinases, bind and phosphorylate specific tyrosine residues within the cytoplasmic domain of TIM-3. The phosphorylated tyrosines within the cytoplasmic domain of TIM-3 can recruit other downstream signaling adaptors such as p85 adaptor protein. In addition, Gal-9 can mediate the formation of clusters containing TIM-3, CD45, and CD148.
So far, four relevant ligands have been shown to interact with the IgV domain of TIM-3 (Figure 1) [41]. These include galectin-9 (Gal-9), high mobility group protein B1 (HMGB1), carcinoembryonic antigen cell adhesion molecule 1 (Ceacam-1), and phosphatidylserine (PtdSer). Gal-9, the first identified ligand, can bind to the carbohydrate motif on TIM-3 and incite an influx of calcium to the intracellular region of Th1 cells, inducing apoptosis [22]. It is important to note that glycosylation of the IgV is required for Gal-9 binding [22]. PtdSer, a molecule exposed on the surfaces of apoptotic cells, is another TIM-3 ligand. PtdSer was shown to bind to a pocket within the IgV domain of TIM-1, TIM-3, and TIM-4 [42]. This interaction facilitates the clearance of apoptotic bodies and also promotes the cross-presentation of antigens by dendritic cells (DCs) [43]. The third TIM-3 ligand identified is high mobility group protein B1 (HMGB1). TIM-3 is highly expressed on tumor infiltrating DCs and actively competes with nucleic acids released from dying tumor cells to bind HMGB1, effectively inhibiting stimulation of the innate immune response by nucleic acids [44]. As a result, activation of innate immunity and production of pro-inflammatory cytokines can be attenuated. Carcinoembryonic antigen cell adhesion molecule 1 (Ceacam-1) expressed on the cell surface is a more recently identified ligand for TIM-3. Ceacam-1 and TIM-3 are co-expressed, and the two molecules can form in trans a specific heterodimer which functions as a negative regulator of T cell responses [45]. The interaction between Ceacam-1 and TIM-3 can be either cis or trans, and both types of interactions can mediate T cell immune tolerance.
TIM-3 is involved in the proximal signaling events in T cells. However, there is evidence supporting both positive and negative effects of TIM-3 on TCR (T cell receoptor) signaling. Transient expression of TIM-3 increases TCR signaling to NFAT and NF-κB in Jurkat T cells and phosphorylation of tyrosines 256 and 263 is required, but the ecto domain of TIM-3 is not required for this function of TIM-3 [36]. Several members of the Src kinase family—such as Lck, Fyn and Itk—have been shown to bind and phosphorylate TIM-3 tyrosines [36,46]. The phosphorylated tyrosines within the cytoplasmic domain of TIM-3 can then recruit p85 adaptor protein, leading to the activation of PI3 kinases. TIM-3 has also been shown to inhibit TCR proximal signaling [47,48]. In TIM-3+ CD8+ effector T cells, Gal-9 is shown to induce co-localization of TIM-3 with receptor phosphatases CD45 and CD148, and thereby inhibits TCR signaling [49]. Another report shows that TIM-3 is stably expressed in Jurkat cells inhibits TCR-mediated NF-κB/NFAT activation [49]. Bat-3 has been shown to bind to the cytoplasmic tail of TIM-3, and Gal-9-triggered phosphorylation of tyrosines 256 and 263 leads to its release from TIM-3 [47]. Bat-3 reverses the negative effect of TIM-3 on TCR signaling, likely by recruiting active Lck or blocking the binding of Fyn to TIM-3 [41,47]. Therefore, the effect of TIM-3 on TCR signaling is dependent on cellular context (positive for naïve/effector/memory T cells versus negative for exhausted T cells) or the ligands it engages.
3. Tim-3 Mediates Immune Tolerance in Autoimmunity and Alloimmunity
In earlier studies, TIM-3 was shown to be involved in the regulation of autoimmune diseases in both mouse models and human patients. Treatment with TIM-3 mAb enhances the severity of experimental autoimmune encephalomyelitis (EAE) [21]. Lower expression of TIM-3 on T cells and higher production of interferon (IFN)-γ can be detected in patients suffering from multiple sclerosis (MS) [50]. TIM-3-Ig fusion protein or anti-TIM-3 mAb can accelerate autoimmune diabetes by blocking TIM-3-mediated immune tolerance [23]. These studies suggest that TIM-3 is an immune checkpoint molecule. Similar observations were also made in the transplantation setting. Administration of the TIM-3-Ig fusion protein prevented transplantation tolerance, and this function of TIM-3 is dependent on donor-specific CD4+CD25+ regulatory T cells [24]. Many other studies further support a critical role of TIM-3 in suppressing the rejection of transplanted skin [24], pancreatic islets [24], heart [51], and bone marrow allografts [52]. These studies indicate that TIM-3 signaling—or at least the immune cells expressing TIM-3—mediates immune tolerance. However, the in vivo mechanisms are still not clear.
4. TIM-3 in Immune Tolerance to Tumors
Recently, TIM-3 has been shown to be highly expressed on tumor antigen-specific T cells in the peripheral blood and among tumor infiltrating lymphocytes (TIL), suggesting a role of TIM-3 in tumor Immunity. Up-regulation of TIM-3 is associated with the exhaustion of tumor antigen-specific CD8+ T cells in melanoma patients, and administration of TIM-3 mAbs can reverse tumor-induced T cell exhaustion [29,53]. In human patients with non-small cell lung cancer (NSCLC), TIM-3 is predominantly expressed in tumor-infiltrating CD4+ and CD8+ T cells, but expressed at minimal levels on T cells from peripheral blood. In addition, among CD4+ TIL, TIM-3 is preferentially expressed on Foxp3+ CD4+ Treg cells, and the frequency of CD4+TIM-3+ TIL is correlated with poor patient survival [54]. TIM-3 was also shown to be expressed in TIL or tumor antigen-specific T cells in peripheral blood from many cancer types such as hepatocellular cancer, cervical cancer, colorectal cancer, ovarian cancer [55], NSCLC [56,57], head and neck cancer [58], renal cell carcinoma (RCC) [59], gastric cancer [60], esophageal cancer [61], prostate cancer [62], and non-Hodgkin lymphoma [63].
In preclinical models, administration of TIM-3 mAbs alone has produced variable antitumor effects. TIM-3 has been shown to be upregulated in TIL in mouse tumor models such as CT26 colon adenocarcinoma, 4T1 mammary adenocarcinoma, and B16F10 melanoma [64]. On its own, administration of TIM-3 mAbs did not inhibit tumor growth in the CT26 model. However, combination of TIM-3 and PD-1 mAbs had a much greater antitumor effect than administration of TIM-3 or PD-1 mAbs alone [64]. Another study showed that TIM-3 mAbs injection slowed tumor progression in many mouse tumor models, such as MC38 colon carcinoma, WT3 sarcoma, CT26 colon adenocarcinoma, and TRAMP-C1 prostate tumor [65]. Furthermore, combination of TIM-3 mAbs and CTLA4 mAbs, or TIM-3 mAbs and PD-1 mAbs has had much greater antitumor effects [65]. These studies have established that targeting TIM-3 with monoclonal antibodies is a viable new immunotherapy for cancer. In addition, rational combinations of TIM-3 mAbs with the PD-1 mAbs and/or CTLA4 mAbs have great potential to further improve the current immunotherapeutic approaches to cancer. Currently, a Phase I-Ib/II open-label multi-center study of the safety and efficacy of TIM-3 mAbs as single agent and in combination with PD-1 mAbs in adult patients with advanced malignancies is ongoing (ClinicalTrials.gov Identifier: NCT02608268).
5. Targeting TIM-3 for Immunotherapy of Cancer
TIM-3 signaling directly regulates the function of Th1 and CD8+ T cells through various mechanisms (Figure 2). TIM-3 is induced in Th1 cells and inhibits Th1-mediated immune responses by directly triggering apoptosis [22]. TIM-3 has also been identified as a marker for exhausted CD8+ T cells in patients with chronic infections such as HIV or hepatitis C virus [25,27]. In cancer patients, TIM-3 is upregulated on tumor antigen-specific CD8+ T cells and CD8+ TIL [29,53,54,64]. Administration of TIM-3 mAbs increases proliferation and cytokine production by tumor antigen-specific T cells [29,53,54,64,65]. These data support the idea that the exhaustion of T cells is involved in the establishment of an immune suppressive state in cancer.
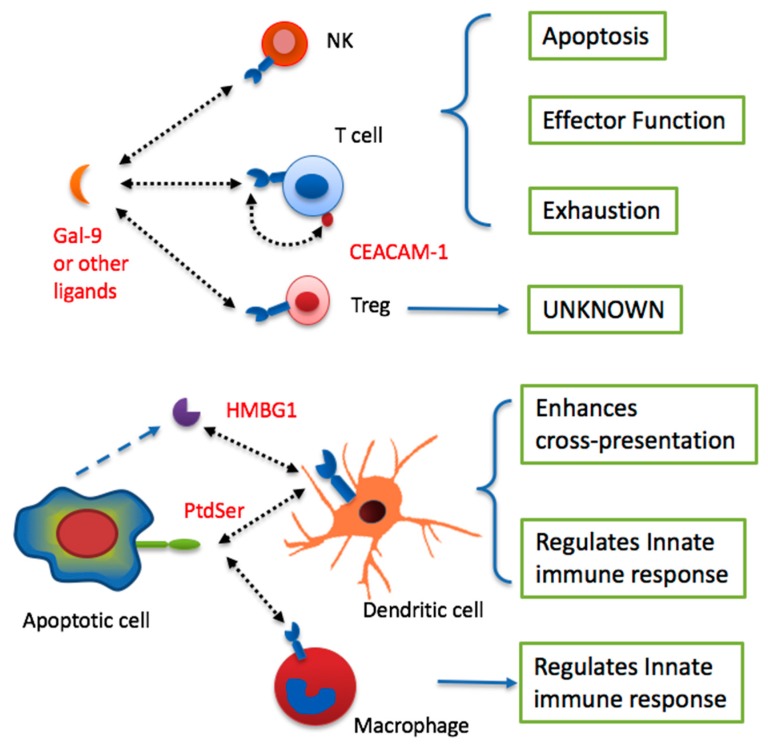
Figure 2.
Summary of multiple biological functions of TIM-3 on various immune cells. TIM-3 signaling in T cells and NK cells leads to the development of effector functions, apoptosis, or exhaustion. The effect on Tregs remains unknown. Likely dependent on the cellular context, TIM-3 signaling can enhance cross-presentation of dendritic cells (DC) or inhibit innate immune responses of DC and macrophages.
However, one must be cautious when considering TIM-3 for the purpose of boosting CD8+ T cell-mediated immune responses. Despite the antitumor efficacy seen with TIM-3 mAbs, TIM-3 has been shown to promote CD8+ T cells function in the setting of listeria infection [33]. It is possible that although TIM-3 expression is associated with CD8+ T cell exhaustion during chronic infection and tumor immune suppression, it may also promote the initial generation of effector CD8+ T cells during acute infection.
TIM-3 is also found to be upregulated on CD4+ T cells in patients with chronic infection and cancer [25,27,54,64]. It is possible that TIM-3 is an exhaustion marker for Th1 cells [25,27]. It is important to note that a substantial proportion of CD4+TIM-3+ TIL are Foxp3+, suggesting a role for TIM-3 in Treg within the tumor microenvironment (TME) [64]. Besides tumor tissues, TIM-3 has also been found in many tissue-resident Tregs [66], and plays an important role in both maintaining immune tolerance as well as tissue repair [67,68,69,70]. It remains to be determined whether or not TIM-3 mAbs function in tumor immunotherapy—at least in part—by inhibiting the function of tumor-infiltrating Treg (Figure 2).
Ample evidence supports a role for TIM-3 as an inhibitory receptor on NK cells. TIM-3 is highly expressed on mature human NK cells and is variably expressed on immature NK cells [71]. TIM-3 marks NK cells with greater effector function, including cytokine production and cytotoxicity. However, cross-linking of TIM-3 inhibits NK cell-mediated cytotoxicity, suggesting that interaction of TIM-3 with one or more of its ligands negatively regulates NK cell activity [71]. In another study, TIM-3 expression was increased on NK cells from patients infected chronically with hepatitis B [72]. TIM-3 blockade ex vivo increased cytotoxicity of NK cells from these patients, suggesting that TIM-3 inhibits NK function in chronic infection. Many other studies further support an inhibitory role of TIM-3 in NK cell-mediated immune responses [73,74,75,76]. In contrast, some studies demonstrated a positive role of TIM-3 in NK function [77]. Therefore, TIM-3 might play both stimulatory and inhibitory roles in NK cells, depending on cellular and pathological context. The role of TIM-3 on NK cells in the tumor microenvironment remains to be examined (Figure 2).
Besides lymphocytes, TIM-3 has been shown to be expressed by various myeloid cells (e.g., DCs, monocytes, and macrophages), and to play an important role in regulating innate immune cell-mediated anti-viral infection and antitumor immune responses (Figure 2) [78]. TIM-3 is expressed on splenic CD8+ DCs [19,43]. Both Gal-9 and an agonistic TIM-3 mAb were reported to promote DC maturation and increase proinflammatory cytokine production [19,79]. TIM-3 mediates the uptake of apoptotic cells and the cross-presentation of antigen by DCs via TIM-3 binding to PtdSer [43]. TIM-3 mAbs inhibit this function of TIM-3 and inhibit cross-presentation of tumor antigens [43]. Despite evidence of a positive role for TIM-3 in DC function, other studies suggest that TIM-3 mediates inhibitory signals in DC, particularly in the TME. TIM-3 mAbs inhibited the activation and maturation of bone marrow-derived DCs by blocking the NF-κB pathway [80]. In tumor tissues, HMGB1—a ligand of TIM-3—is believed to act together with tumor-derived nucleic acids to gain access to endosomal vesicles and activate innate immune responses by DCs [81]. Through direct interaction with HMGB1, TIM-3—which is highly expressed on tumoral DCs—circumvents the stimulatory effects of nucleic acids in tumor immunity [81]. It is possible that the exact role of TIM-3 is dependent on the type of DC where it is expressed and the specific ligand through which it primarily engages these cells.
TIM-3 has been shown to be involved in both promoting and inhibiting the function of monocytes and macrophages. It was reported that antibodies to TIM-3 led to increased activation of macrophages and aggravated autoimmune disease [21]. In the same vein, TIM3-specific mAbs and TIM-3 overexpression in macrophages inhibited TLR4-stimulated inflammatory cytokine production and promoted sepsis in vivo [82]. TIM-3 is constitutively expressed by primary CD14+ monocytes, and blockade of TIM-3 signaling or silencing of TIM-3 expression led to a significant increase in interleukin (IL)-12 and IL-10 production and a decrease in PD-1 [83,84]. These findings suggest that TIM-3 acts as a negative regulator of macrophages and monocytes during innate immune responses. In contrast, several studies indicated that interaction of Gal-9 and TIM-3 resulted in the activation of macrophages and promoted antibacterial activity, though still-undefined mechanisms [85,86,87,88].
The phenotype of myeloid cells is highly influenced by tumor progression. Tumor-associated macrophages (TAMs) and myeloid-derived suppressor cells are highly increased in the TME. TIM-3 is expressed on TAMs in a variety of tumors, including hepatocellular carcinoma, lung cancer, clear cell renal cell carcinoma, osteosarcoma, Langerhans cell sarcoma, and neoplasms derived from histiocytic and dendritic cells [89,90,91,92,93]. Interestingly, transgenic overexpression of TIM-3 driven by the CD2 promoter on some T cells resulted in an increase in systemic levels of CD11b+Ly-6G+ granulocytic myeloid-derived suppressor cells (MDSC) and inhibition of immune responses [94]. These data are consistent with a role for TIM-3 in immune suppression. Mechanisms by which TIM-3 affects the generation and function of TAMs and MDSCs remain to be elucidated.
6. Conclusions and Perspective
At present, TIM-3 is generally acknowledged as a negative regulator of antitumor Immunity. Several properties of TIM-3 make it an ideal target for the next generation of immunotherapy. For example, its selective expression on intratumoral T cells may allow for more precise therapy via the targeting of tumor-infiltrating T cells, potentially reducing non-specific toxicity. In addition, signaling downstream of TIM-3 is rather distinct from that of CTLA-4 and PD-1, which have reasonably well-defined inhibitory mechanisms. By contrast, TIM-3 can both enhance and inhibit proximal signaling in T cells, depending on the cellular context. Therefore, the distinctive expression and intracellular signaling suggest a great potential for targeting TIM-3 alone and in combination with current PD-1 and CTLA-4-based immunotherapy of cancer.
Accumulating data support the concept that TIM-3 blockade can increase cell-mediated antitumor immune responses. In addition, TIM-3 mAbs may synergize with other immunotherapy modalities to increase antitumor efficacy. However, due to the expression of TIM-3 in both myeloid cells and lymphocytes, the exact cellular mechanisms underlying the in vivo antitumor activity of TIM-3 mAbs are still not understood. This issue is particularly critical because TIM-3 has been shown to both promote and inhibit cellular immune responses, depending on the models used. A thorough understanding of the roles of different cell types that express TIM-3 in various tumors and tumor immunotherapy models is crucial for further drug development targeting TIM-3 and design of combination therapy with PD-1 or CTLA-4 mAbs.
Acknowledgments
This work was supported in part by R21CA205727 (to Binfeng Lu), a Head and Neck Cancer Spore Development award (to Binfeng Lu), a pilot grant of Roswell Park Cancer Institute/University of Pittsburgh Cancer Institute Ovarian Cancer Specialized Programs of Research Excellence Grants P50CA159981 (to Binfeng Lu), and National Natural Science Foundation of China Grant 31428005 (to Binfeng Lu).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Hodi F.S., O’Day S.J., McDermott D.F., Weber R.W., Sosman J.A., Haanen J.B., Gonzalez R., Robert C., Schadendorf D., Hassel J.C., et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robert C., Thomas L., Bondarenko I., O’Day S., Weber J., Garbe C., Lebbe C., Baurain J.F., Testori A., Grob J.J., et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N. Engl. J. Med. 2011;364:2517–2526. doi: 10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- 3.Maio M., Grob J.J., Aamdal S., Bondarenko I., Robert C., Thomas L., Garbe C., Chiarion-Sileni V., Testori A., Chen T.T., et al. Five-year survival rates for treatment-naive patients with advanced melanoma who received ipilimumab plus dacarbazine in a phase III trial. J. Clin. Oncol. 2015;33:1191–1196. doi: 10.1200/JCO.2014.56.6018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schadendorf D., Hodi F.S., Robert C., Weber J.S., Margolin K., Hamid O., Patt D., Chen T.T., Berman D.M., Wolchok J.D. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J. Clin. Oncol. 2015;33:1889–1894. doi: 10.1200/JCO.2014.56.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Selby M.J., Engelhardt J.J., Quigley M., Henning K.A., Chen T., Srinivasan M., Korman A.J. Anti-CTLA-4 antibodies of IgG2a isotype enhance antitumor activity through reduction of intratumoral regulatory T cells. Cancer Immunol. Res. 2013;1:32–42. doi: 10.1158/2326-6066.CIR-13-0013. [DOI] [PubMed] [Google Scholar]
- 6.Romano E., Kusio-Kobialka M., Foukas P.G., Baumgaertner P., Meyer C., Ballabeni P., Michielin O., Weide B., Romero P., Speiser D.E. Ipilimumab-dependent cell-mediated cytotoxicity of regulatory T cells ex vivo by nonclassical monocytes in melanoma patients. Proc. Natl. Acad. Sci. USA. 2015;112:6140–6145. doi: 10.1073/pnas.1417320112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong H., Zhu G., Tamada K., Chen L. B7-H1, a third member of the B7 family, co-stimulates T cell proliferation and interleukin-10 secretion. Nat. Med. 1999;5:1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]
- 8.Freeman G.J., Long A.J., Iwai Y., Bourque K., Chernova T., Nishimura H., Fitz L.J., Malenkovich N., Okazaki T., Byrne M.C., et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J. Exp. Med. 2000;192:1027–1034. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Topalian S.L., Hodi F.S., Brahmer J.R., Gettinger S.N., Smith D.C., McDermott D.F., Powderly J.D., Carvajal R.D., Sosman J.A., Atkins M.B., et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brahmer J.R., Tykodi S.S., Chow L.Q., Hwu W.J., Topalian S.L., Hwu P., Drake C.G., Camacho L.H., Kauh J., Odunsi K., et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N. Engl. J. Med. 2012;366:2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolchok J.D., Kluger H., Callahan M.K., Postow M.A., Rizvi N.A., Lesokhin A.M., Segal N.H., Ariyan C.E., Gordon R.A., Reed K., et al. Nivolumab plus ipilimumab in advanced melanoma. N. Engl. J. Med. 2013;369:122–133. doi: 10.1056/NEJMoa1302369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ansell S.M., Lesokhin A.M., Borrello I., Halwani A., Scott E.C., Gutierrez M., Schuster S.J., Millenson M.M., Cattry D., Freeman G.J., et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N. Engl. J. Med. 2015;372:311–319. doi: 10.1056/NEJMoa1411087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robert C., Schachter J., Long G.V., Arance A., Grob J.J., Mortier L., Daud A., Carlino M.S., McNeil C., Lotem M., et al. Pembrolizumab versus ipilimumab in advanced melanoma. N. Engl. J. Med. 2015;372:2521–2532. doi: 10.1056/NEJMoa1503093. [DOI] [PubMed] [Google Scholar]
- 14.Garon E.B., Rizvi N.A., Hui R., Leighl N., Balmanoukian A.S., Eder J.P., Patnaik A., Aggarwal C., Gubens M., Horn L., et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N. Engl. J. Med. 2015;372:2018–2028. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 15.Larkin J., Chiarion-Sileni V., Gonzalez R., Grob J.J., Cowey C.L., Lao C.D., Schadendorf D., Dummer R., Smylie M., Rutkowski P., et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med. 2015;373:23–34. doi: 10.1056/NEJMoa1504030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Le D.T., Uram J.N., Wang H., Bartlett B.R., Kemberling H., Eyring A.D., Skora A.D., Luber B.S., Azad N.S., Laheru D., et al. PD-1 blockade in tumors with mismatch-repair deficiency. N. Engl. J. Med. 2015;372:2509–2520. doi: 10.1056/NEJMoa1500596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brahmer J., Reckamp K.L., Baas P., Crino L., Eberhardt W.E., Poddubskaya E., Antonia S., Pluzanski A., Vokes E.E., Holgado E., et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N. Engl. J. Med. 2015;373:123–135. doi: 10.1056/NEJMoa1504627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Motzer R.J., Escudier B., McDermott D.F., George S., Hammers H.J., Srinivas S., Tykodi S.S., Sosman J.A., Procopio G., Plimack E.R., et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 2015;373:1803–1813. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson A.C., Anderson D.E., Bregoli L., Hastings W.D., Kassam N., Lei C., Chandwaskar R., Karman J., Su E.W., Hirashima M., et al. Promotion of tissue inflammation by the immune receptor TIM-3 expressed on innate immune cells. Science. 2007;318:1141–1143. doi: 10.1126/science.1148536. [DOI] [PubMed] [Google Scholar]
- 20.Hastings W.D., Anderson D.E., Kassam N., Koguchi K., Greenfield E.A., Kent S.C., Zheng X.X., Strom T.B., Hafler D.A., Kuchroo V.K. TIM-3 is expressed on activated human CD4+ T cells and regulates Th1 and Th17 cytokines. Eur. J. Immunol. 2009;39:2492–2501. doi: 10.1002/eji.200939274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monney L., Sabatos C.A., Gaglia J.L., Ryu A., Waldner H., Chernova T., Manning S., Greenfield E.A., Coyle A.J., Sobel R.A., et al. Th1-specific cell surface protein TIM-3 regulates macrophage activation and severity of an autoimmune disease. Nature. 2002;415:536–541. doi: 10.1038/415536a. [DOI] [PubMed] [Google Scholar]
- 22.Zhu C., Anderson A.C., Schubart A., Xiong H., Imitola J., Khoury S.J., Zheng X.X., Strom T.B., Kuchroo V.K. The TIM-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat. Immunol. 2005;6:1245–1252. doi: 10.1038/ni1271. [DOI] [PubMed] [Google Scholar]
- 23.Sabatos C.A., Chakravarti S., Cha E., Schubart A., Sanchez-Fueyo A., Zheng X.X., Coyle A.J., Strom T.B., Freeman G.J., Kuchroo V.K. Interaction of TIM-3 and TIM-3 ligand regulates T helper type 1 responses and induction of peripheral tolerance. Nat. Immunol. 2003;4:1102–1110. doi: 10.1038/ni988. [DOI] [PubMed] [Google Scholar]
- 24.Sanchez-Fueyo A., Tian J., Picarella D., Domenig C., Zheng X.X., Sabatos C.A., Manlongat N., Bender O., Kamradt T., Kuchroo V.K., et al. TIM-3 inhibits T helper type 1-mediated auto- and alloimmune responses and promotes immunological tolerance. Nat. Immunol. 2003;4:1093–1101. doi: 10.1038/ni987. [DOI] [PubMed] [Google Scholar]
- 25.Jones R.B., Ndhlovu L.C., Barbour J.D., Sheth P.M., Jha A.R., Long B.R., Wong J.C., Satkunarajah M., Schweneker M., Chapman J.M., et al. TIM-3 expression defines a novel population of dysfunctional T cells with highly elevated frequencies in progressive HIV-1 infection. J. Exp. Med. 2008;205:2763–2779. doi: 10.1084/jem.20081398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hafler D.A., Kuchroo V. TIMs: Central regulators of immune responses. J. Exp. Med. 2008;205:2699–2701. doi: 10.1084/jem.20082429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Golden-Mason L., Palmer B.E., Kassam N., Townshend-Bulson L., Livingston S., McMahon B.J., Castelblanco N., Kuchroo V., Gretch D.R., Rosen H.R. Negative immune regulator TIM-3 is overexpressed on T cells in hepatitis C virus infection and its blockade rescues dysfunctional CD4+ and CD8+ T cells. J. Virol. 2009;83:9122–9130. doi: 10.1128/JVI.00639-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takamura S., Tsuji-Kawahara S., Yagita H., Akiba H., Sakamoto M., Chikaishi T., Kato M., Miyazawa M. Premature terminal exhaustion of friend virus-specific effector CD8+ T cells by rapid induction of multiple inhibitory receptors. J. Immunol. 2010;184:4696–4707. doi: 10.4049/jimmunol.0903478. [DOI] [PubMed] [Google Scholar]
- 29.Fourcade J., Sun Z., Benallaoua M., Guillaume P., Luescher I.F., Sander C., Kirkwood J.M., Kuchroo V., Zarour H.M. Upregulation of TIM-3 and PD-1 expression is associated with tumor antigen-specific CD8+ T cell dysfunction in melanoma patients. J. Exp. Med. 2010;207:2175–2186. doi: 10.1084/jem.20100637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sakuishi K., Jayaraman P., Behar S.M., Anderson A.C., Kuchroo V.K. Emerging Tim-3 functions in antimicrobial and tumor immunity. Trends Immunol. 2011;32:345–349. doi: 10.1016/j.it.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koyama S., Akbay E.A., Li Y.Y., Herter-Sprie G.S., Buczkowski K.A., Richards W.G., Gandhi L., Redig A.J., Rodig S.J., Asahina H., et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat. Commun. 2016;7:10501. doi: 10.1038/ncomms10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu J., Zhang S., Hu Y., Yang Z., Li J., Liu X., Deng L., Wang Y., Zhang X., Jiang T., Lu X. Targeting PD-1 and TIM-3 pathways to reverse CD8 T cell exhaustion and enhance ex vivo T cell responses to autologous dendritic/tumor vaccines. J. Immunother. 2016;39:171–180. doi: 10.1097/CJI.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 33.Gorman J.V., Starbeck-Miller G., Pham N.L., Traver G.L., Rothman P.B., Harty J.T., Colgan J.D. TIM-3 directly enhances CD8 T cell responses to acute Listeria monocytogenes infection. J. Immunol. 2014;192:3133–3142. doi: 10.4049/jimmunol.1302290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cao E., Zang X., Ramagopal U.A., Mukhopadhaya A., Fedorov A., Fedorov E., Zencheck W.D., Lary J.W., Cole J.L., Deng H., et al. T cell immunoglobulin mucin-3 crystal structure reveals a galectin-9-independent ligand-binding surface. Immunity. 2007;26:311–321. doi: 10.1016/j.immuni.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 35.Anderson A.C., Xiao S., Kuchroo V.K. TIM protein structures reveal a unique face for ligand binding. Immunity. 2007;26:273–275. doi: 10.1016/j.immuni.2007.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee J., Su E.W., Zhu C., Hainline S., Phuah J., Moroco J.A., Smithgall T.E., Kuchroo V.K., Kane L.P. Phosphotyrosine-dependent coupling of TIM-3 to T cell receptor signaling pathways. Mol. Cell Biol. 2011;31:3963–3974. doi: 10.1128/MCB.05297-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferris R.L., Lu B., Kane L.P. Too much of a good thing? TIM-3 and TCR signaling in T cell exhaustion. J. Immunol. 2014;193:1525–1530. doi: 10.4049/jimmunol.1400557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kane L.P. Antigen receptor kinase two-step. J. Immunol. 2014;193:4277–4278. doi: 10.4049/jimmunol.1402287. [DOI] [PubMed] [Google Scholar]
- 39.Phong B.L., Avery L., Sumpter T.L., Gorman J.V., Watkins S.C., Colgan J.D., Kane L.P. TIM-3 enhances FcεRI-proximal signaling to modulate mast cell activation. J. Exp. Med. 2015;212:2289–2304. doi: 10.1084/jem.20150388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Santiago C., Ballesteros A., Tami C., Martinez-Munoz L., Kaplan G.G., Casasnovas J.M. Structures of T cell immunoglobulin mucin receptors 1 and 2 reveal mechanisms for regulation of immune responses by the TIM receptor family. Immunity. 2007;26:299–310. doi: 10.1016/j.immuni.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anderson A.C., Joller N., Kuchroo V.K. Lag-3, TIM-3, and TIGIT: Co-inhibitory receptors with specialized functions in immune regulation. Immunity. 2016;44:989–1004. doi: 10.1016/j.immuni.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeKruyff R.H., Bu X., Ballesteros A., Santiago C., Chim Y.L., Lee H.H., Karisola P., Pichavant M., Kaplan G.G., Umetsu D.T., et al. T cell/transmembrane, Ig, and mucin-3 allelic variants differentially recognize phosphatidylserine and mediate phagocytosis of apoptotic cells. J. Immunol. 2010;184:1918–1930. doi: 10.4049/jimmunol.0903059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakayama M., Akiba H., Takeda K., Kojima Y., Hashiguchi M., Azuma M., Yagita H., Okumura K. TIM-3 mediates phagocytosis of apoptotic cells and cross-presentation. Blood. 2009;113:3821–3830. doi: 10.1182/blood-2008-10-185884. [DOI] [PubMed] [Google Scholar]
- 44.Tang D., Lotze M.T. Tumor immunity times out: TIM-3 and HMGB1. Nat. Immunol. 2012;13:808–810. doi: 10.1038/ni.2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang Y.H., Zhu C., Kondo Y., Anderson A.C., Gandhi A., Russell A., Dougan S.K., Petersen B.S., Melum E., Pertel T., et al. CEACAM1 regulates TIM-3-mediated tolerance and exhaustion. Nature. 2015;517:386–390. doi: 10.1038/nature13848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Van de Weyer P.S., Muehlfeit M., Klose C., Bonventre J.V., Walz G., Kuehn E.W. A highly conserved tyrosine of TIM-3 is phosphorylated upon stimulation by its ligand galectin-9. Biochem. Biophys. Res. Commun. 2006;351:571–576. doi: 10.1016/j.bbrc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 47.Clayton K.L., Haaland M.S., Douglas-Vail M.B., Mujib S., Chew G.M., Ndhlovu L.C., Ostrowski M.A. T cell Ig and mucin domain-containing protein 3 is recruited to the immune synapse, disrupts stable synapse formation, and associates with receptor phosphatases. J. Immunol. 2014;192:782–791. doi: 10.4049/jimmunol.1302663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tomkowicz B., Walsh E., Cotty A., Verona R., Sabins N., Kaplan F., Santulli-Marotto S., Chin C.N., Mooney J., Lingham R.B., et al. TIM-3 suppresses anti-CD3/CD28-induced TCR activation and IL-2 expression through the NFAT signaling pathway. PLoS ONE. 2015;10:e0140694. doi: 10.1371/journal.pone.0140694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rangachari M., Zhu C., Sakuishi K., Xiao S., Karman J., Chen A., Angin M., Wakeham A., Greenfield E.A., Sobel R.A., et al. Bat3 promotes T cell responses and autoimmunity by repressing TIM-3-mediated cell death and exhaustion. Nat. Med. 2012;18:1394–1400. doi: 10.1038/nm.2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang L., Anderson D.E., Kuchroo J., Hafler D.A. Lack of TIM-3 immunoregulation in multiple sclerosis. J. Immunol. 2008;180:4409–4414. doi: 10.4049/jimmunol.180.7.4409. [DOI] [PubMed] [Google Scholar]
- 51.Boenisch O., D’Addio F., Watanabe T., Elyaman W., Magee C.N., Yeung M.Y., Padera R.F., Rodig S.J., Murayama T., Tanaka K., et al. TIM-3: A novel regulatory molecule of alloimmune activation. J. Immunol. 2010;185:5806–5819. doi: 10.4049/jimmunol.0903435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Veenstra R.G., Taylor P.A., Zhou Q., Panoskaltsis-Mortari A., Hirashima M., Flynn R., Liu D., Anderson A.C., Strom T.B., Kuchroo V.K., et al. Contrasting acute graft-versus-host disease effects of TIM-3/galectin-9 pathway blockade dependent upon the presence of donor regulatory T cells. Blood. 2012;120:682–690. doi: 10.1182/blood-2011-10-387977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baitsch L., Baumgaertner P., Devevre E., Raghav S.K., Legat A., Barba L., Wieckowski S., Bouzourene H., Deplancke B., Romero P., et al. Exhaustion of tumor-specific CD8+ T cells in metastases from melanoma patients. J. Clin. Investig. 2011;121:2350–2360. doi: 10.1172/JCI46102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gao X., Zhu Y., Li G., Huang H., Zhang G., Wang F., Sun J., Yang Q., Zhang X., Lu B. TIM-3 expression characterizes regulatory T cells in tumor tissues and is associated with lung cancer progression. PLoS ONE. 2012;7:e30676. doi: 10.1371/journal.pone.0030676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yan J., Zhang Y., Zhang J.P., Liang J., Li L., Zheng L. TIM-3 expression defines regulatory T cells in human tumors. PLoS ONE. 2013;8:e58006. doi: 10.1371/journal.pone.0058006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ji P., Chen D., Bian J., Xia R., Song X., Wen W., Zhang X., Zhu Y. Up-regulation of TIM-3 on CD4+ tumor infiltrating lymphocytes predicts poor prognosis in human non-small-cell lung cancer. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2015;31:808–811. [PubMed] [Google Scholar]
- 57.Thommen D.S., Schreiner J., Muller P., Herzig P., Roller A., Belousov A., Umana P., Pisa P., Klein C., Bacac M., et al. Progression of lung cancer is associated with increased dysfunction of T cells defined by coexpression of multiple inhibitory receptors. Cancer Immunol. Res. 2015;3:1344–1355. doi: 10.1158/2326-6066.CIR-15-0097. [DOI] [PubMed] [Google Scholar]
- 58.Jie H.B., Gildener-Leapman N., Li J., Srivastava R.M., Gibson S.P., Whiteside T.L., Ferris R.L. Intratumoral regulatory T cells upregulate immunosuppressive molecules in head and neck cancer patients. Br. J. Cancer. 2013;109:2629–2635. doi: 10.1038/bjc.2013.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cai C., Xu Y.F., Wu Z.J., Dong Q., Li M.Y., Olson J.C., Rabinowitz Y.M., Wang L.H., Sun Y. TIM-3 expression represents dysfunctional tumor infiltrating T cells in renal cell carcinoma. World J. Urol. 2016;34:561–567. doi: 10.1007/s00345-015-1656-7. [DOI] [PubMed] [Google Scholar]
- 60.Cheng G., Li M., Wu J., Ji M., Fang C., Shi H., Zhu D., Chen L., Zhao J., Shi L., et al. Expression of TIM-3 in gastric cancer tissue and its relationship with prognosis. Int. J. Clin. Exp. Pathol. 2015;8:9452–9457. [PMC free article] [PubMed] [Google Scholar]
- 61.Jinhua X., Ji W., Shouliang C., Liangfeng Z., Feiyue J., Lin Y., Yan Z., Haoming J. Expression of immune checkpoints in T cells of esophageal cancer patients. Oncotarget. 2016;7:63669–63678. doi: 10.18632/oncotarget.11611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Japp A.S., Kursunel M.A., Meier S., Malzer J.N., Li X., Rahman N.A., Jekabsons W., Krause H., Magheli A., Klopf C., et al. Dysfunction of PSA-specific CD8+ T cells in prostate cancer patients correlates with CD38 and TIM-3 expression. Cancer Immunol. Immunother. 2015;64:1487–1494. doi: 10.1007/s00262-015-1752-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang Z.Z., Grote D.M., Ziesmer S.C., Niki T., Hirashima M., Novak A.J., Witzig T.E., Ansell S.M. IL-12 upregulates TIM-3 expression and induces T cell exhaustion in patients with follicular B cell non-Hodgkin lymphoma. J. Clin. Investig. 2012;122:1271–1282. doi: 10.1172/JCI59806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sakuishi K., Apetoh L., Sullivan J.M., Blazar B.R., Kuchroo V.K., Anderson A.C. Targeting TIM-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J. Exp. Med. 2010;207:2187–2194. doi: 10.1084/jem.20100643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ngiow S.F., von Scheidt B., Akiba H., Yagita H., Teng M.W., Smyth M.J. Anti-TIM-3 antibody promotes T cell IFN-gamma-mediated antitumor immunity and suppresses established tumors. Cancer Res. 2011;71:3540–3551. doi: 10.1158/0008-5472.CAN-11-0096. [DOI] [PubMed] [Google Scholar]
- 66.Panduro M., Benoist C., Mathis D. Tissue Tregs. Annu. Rev. Immunol. 2016;34:609–633. doi: 10.1146/annurev-immunol-032712-095948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gupta S., Thornley T.B., Gao W., Larocca R., Turka L.A., Kuchroo V.K., Strom T.B. Allograft rejection is restrained by short-lived TIM-3+PD-1+Foxp3+ Tregs. J. Clin. Investig. 2012;122:2395–2404. doi: 10.1172/JCI45138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schiering C., Krausgruber T., Chomka A., Frohlich A., Adelmann K., Wohlfert E.A., Pott J., Griseri T., Bollrath J., Hegazy A.N., et al. The alarmin IL-33 promotes regulatory T cell function in the intestine. Nature. 2014;513:564–568. doi: 10.1038/nature13577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burzyn D., Kuswanto W., Kolodin D., Shadrach J.L., Cerletti M., Jang Y., Sefik E., Tan T.G., Wagers A.J., Benoist C., et al. A special population of regulatory T cells potentiates muscle repair. Cell. 2013;155:1282–1295. doi: 10.1016/j.cell.2013.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Odegaard J.I., Lee M.W., Sogawa Y., Bertholet A.M., Locksley R.M., Weinberg D.E., Kirichok Y., Deo R.C., Chawla A. Perinatal licensing of thermogenesis by IL-33 and ST2. Cell. 2016;166:841–854. doi: 10.1016/j.cell.2016.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ndhlovu L.C., Lopez-Verges S., Barbour J.D., Jones R.B., Jha A.R., Long B.R., Schoeffler E.C., Fujita T., Nixon D.F., Lanier L.L. TIM-3 marks human natural killer cell maturation and suppresses cell-mediated cytotoxicity. Blood. 2012;119:3734–3743. doi: 10.1182/blood-2011-11-392951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ju Y., Hou N., Meng J., Wang X., Zhang X., Zhao D., Liu Y., Zhu F., Zhang L., Sun W., et al. T cell immunoglobulin- and mucin-domain-containing molecule-3 (TIM-3) mediates natural killer cell suppression in chronic hepatitis B. J. Hepatol. 2010;52:322–329. doi: 10.1016/j.jhep.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 73.Hou H., Liu W., Wu S., Lu Y., Peng J., Zhu Y., Wang F., Sun Z. TIM-3 negatively mediates natural killer cell function in LPS-induced endotoxic shock. PLoS ONE. 2014;9:e110585. doi: 10.1371/journal.pone.0110585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gallois A., Silva I., Osman I., Bhardwaj N. Reversal of natural killer cell exhaustion by TIM-3 blockade. Oncoimmunology. 2014;3:e946365. doi: 10.4161/21624011.2014.946365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tripathi S., Chabtini L., Dakle P.J., Smith B., Akiba H., Yagita H., Guleria I. Effect of TIM-3 blockade on the immunophenotype and cytokine profile of murine uterine NK cells. PLoS ONE. 2015;10:e0123439. doi: 10.1371/journal.pone.0123439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Da Silva I.P., Gallois A., Jimenez-Baranda S., Khan S., Anderson A.C., Kuchroo V.K., Osman I., Bhardwaj N. Reversal of NK cell exhaustion in advanced melanoma by TIM-3 blockade. Cancer Immunol. Res. 2014;2:410–422. doi: 10.1158/2326-6066.CIR-13-0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gleason M.K., Lenvik T.R., McCullar V., Felices M., O’Brien M.S., Cooley S.A., Verneris M.R., Cichocki F., Holman C.J., Panoskaltsis-Mortari A., et al. TIM-3 is an inducible human natural killer cell receptor that enhances interferon gamma production in response to galectin-9. Blood. 2012;119:3064–3072. doi: 10.1182/blood-2011-06-360321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Han G., Chen G., Shen B., Li Y. TIM-3: An activation marker and activation limiter of innate immune cells. Front. Immunol. 2013;4:449. doi: 10.3389/fimmu.2013.00449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dai S.Y., Nakagawa R., Itoh A., Murakami H., Kashio Y., Abe H., Katoh S., Kontani K., Kihara M., Zhang S.L., et al. Galectin-9 induces maturation of human monocyte-derived dendritic cells. J. Immunol. 2005;175:2974–2981. doi: 10.4049/jimmunol.175.5.2974. [DOI] [PubMed] [Google Scholar]
- 80.Maurya N., Gujar R., Gupta M., Yadav V., Verma S., Sen P. Immunoregulation of dendritic cells by the receptor T cell Ig and mucin protein-3 via Bruton’s tyrosine kinase and c-Src. J. Immunol. 2014;193:3417–3425. doi: 10.4049/jimmunol.1400395. [DOI] [PubMed] [Google Scholar]
- 81.Chiba S., Baghdadi M., Akiba H., Yoshiyama H., Kinoshita I., Dosaka-Akita H., Fujioka Y., Ohba Y., Gorman J.V., Colgan J.D., et al. Tumor-infiltrating DCs suppress nucleic acid-mediated innate immune responses through interactions between the receptor TIM-3 and the alarmin HMGB1. Nat. Immunol. 2012;13:832–842. doi: 10.1038/ni.2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yang X., Jiang X., Chen G., Xiao Y., Geng S., Kang C., Zhou T., Li Y., Guo X., Xiao H., et al. T cell Ig mucin-3 promotes homeostasis of sepsis by negatively regulating the TLR response. J. Immunol. 2013;190:2068–2079. doi: 10.4049/jimmunol.1202661. [DOI] [PubMed] [Google Scholar]
- 83.Zhang Y., Ma C.J., Wang J.M., Ji X.J., Wu X.Y., Moorman J.P., Yao Z.Q. TIM-3 regulates pro- and anti-inflammatory cytokine expression in human CD14+ monocytes. J. Leukoc. Biol. 2012;91:189–196. doi: 10.1189/jlb.1010591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang Y., Ma C.J., Wang J.M., Ji X.J., Wu X.Y., Jia Z.S., Moorman J.P., Yao Z.Q. TIM-3 negatively regulates IL-12 expression by monocytes in HCV infection. PLoS ONE. 2011;6:e19664. doi: 10.1371/journal.pone.0019664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sada-Ovalle I., Chavez-Galan L., Torre-Bouscoulet L., Nava-Gamino L., Barrera L., Jayaraman P., Torres-Rojas M., Salazar-Lezama M.A., Behar S.M. The TIM-3-galectin 9 pathway induces antibacterial activity in human macrophages infected with Mycobacterium tuberculosis. J. Immunol. 2012;189:5896–5902. doi: 10.4049/jimmunol.1200990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jayaraman P., Sada-Ovalle I., Nishimura T., Anderson A.C., Kuchroo V.K., Remold H.G., Behar S.M. IL-1β promotes antimicrobial immunity in macrophages by regulating TNFR signaling and caspase-3 activation. J. Immunol. 2013;190:4196–4204. doi: 10.4049/jimmunol.1202688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jayaraman P., Sada-Ovalle I., Beladi S., Anderson A.C., Dardalhon V., Hotta C., Kuchroo V.K., Behar S.M. TIM-3 binding to galectin-9 stimulates antimicrobial immunity. J. Exp. Med. 2010;207:2343–2354. doi: 10.1084/jem.20100687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ocana-Guzman R., Torre-Bouscoulet L., Sada-Ovalle I. TIM-3 regulates distinct functions in macrophages. Front. Immunol. 2016;7:229. doi: 10.3389/fimmu.2016.00229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dannenmann S.R., Thielicke J., Stockli M., Matter C., von Boehmer L., Cecconi V., Hermanns T., Hefermehl L., Schraml P., Moch H., et al. Tumor-associated macrophages subvert T cell function and correlate with reduced survival in clear cell renal cell carcinoma. Oncoimmunology. 2013;2:e23562. doi: 10.4161/onci.23562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Flecken T., Sarobe P. TIM-3 expression in tumour-associated macrophages: A new player in HCC progression. Gut. 2015;64:1502–1503. doi: 10.1136/gutjnl-2014-309094. [DOI] [PubMed] [Google Scholar]
- 91.Han Q., Shi H., Liu F. CD163+ M2-type tumor-associated macrophage support the suppression of tumor-infiltrating T cells in osteosarcoma. Int. Immunopharmacol. 2016;34:101–106. doi: 10.1016/j.intimp.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 92.Li J., Cao D., Guo G., Wu Y., Chen Y. Expression and anatomical distribution of TIM-containing molecules in Langerhans cell sarcoma. J. Mol. Histol. 2013;44:213–220. doi: 10.1007/s10735-012-9475-2. [DOI] [PubMed] [Google Scholar]
- 93.Yan W., Liu X., Ma H., Zhang H., Song X., Gao L., Liang X., Ma C. TIM-3 fosters HCC development by enhancing TGF-β-mediated alternative activation of macrophages. Gut. 2015;64:1593–1604. doi: 10.1136/gutjnl-2014-307671. [DOI] [PubMed] [Google Scholar]
- 94.Dardalhon V., Anderson A.C., Karman J., Apetoh L., Chandwaskar R., Lee D.H., Cornejo M., Nishi N., Yamauchi A., Quintana F.J., et al. TIM-3/galectin-9 pathway: Regulation of Th1 immunity through promotion of CD11b+Ly-6G+ myeloid cells. J. Immunol. 2010;185:1383–1392. doi: 10.4049/jimmunol.0903275. [DOI] [PMC free article] [PubMed] [Google Scholar]