Abstract
Fructooligosaccharides (FOS) can selectively stimulate the growth of bifidobacteria. Here, we investigated the effect of maternal FOS ingestion on maternal and neonatal gut bifidobacteria. In a randomized, double-blind, placebo-controlled study, we administered 8 g/day of FOS or sucrose to 84 women from the 26th week of gestation to one month after delivery. The bifidobacteria count was detected using quantitative PCR in maternal (26 and 36 weeks of gestation) and neonatal (one month after delivery) stools. Maternal stool frequency was recorded from 24 to 36 weeks of gestation. The number of fecal Bifidobacterium spp. and Bifidobacterium longum in the FOS group was significantly higher than that in the placebo group at 36 weeks of gestation (2.7 × 1010/g vs. 1.1 × 1010/g and 2.3 × 1010/g vs. 9.7 × 109/g). In their neonates, these numbers did not differ between the groups. Also, stool frequency in the FOS group was slightly higher than that in the placebo group two weeks after the intervention (1.0 vs. 0.8 times/day), suggesting a potential constipation alleviation effect. In conclusion, the maternal FOS ingestion showed a bifidogenic effect in pregnant women but not in their neonates.
Keywords: fructooligosaccharides, bifidobacteria, feces, infancy, pregnancy, prebiotic, constipation, stool frequency
1. Introduction
Bifidobacteria are the predominant commensal bacteria in neonates, and they colonize the neonatal gut immediately after birth [1]. Their colonization after birth occurs through the vertical transfer of gut microbiota from the mother to the neonate [2,3] and is influenced by several factors [4] such as gestational age at birth [5], the mode of delivery [6], use of perinatal antibiotics [7], or the mode of feeding [8]. Recent studies have shown that one of the main sources of bifidobacteria is breast milk [9,10,11]. This gut microbiota influences host nutrition, provides a natural defense mechanism against invading pathogenic bacteria [12], and may determine the development of the infant’s immune system [13,14]. Consequently, previous research has aimed to develop mechanisms to modify the composition of the neonatal gut microbiota, including the oral administration of prebiotics to pregnant women [15].
Fructooligosaccharides (FOS) are a type of prebiotics composed of 1-kestose, nystose, and 1F-ß-fructofuranosylnystose [16]. After ingestion, they enhance the growth of gut bifidobacteria in animals and humans [16]. In pregnant women, FOS ingestion alleviates constipation [17]; however, little is known about the effect of maternal FOS ingestion on maternal and neonatal gut bifidobacteria.
Here, we hypothesized that maternal FOS ingestion increases the number of bifidobacteria in the maternal gut, and these bifidobacteria can be vertically transferred from the mother to the neonate. Thus, we conducted a double-blind, randomized, placebo-controlled study to investigate the effect of maternal FOS ingestion on the number of gut bifidobacteria in both the maternal and neonatal gut. To evaluate the bifidobacterial transfer in detail, we focused on Bifidobacterium longum (B. longum) because it is the main species that inhabits both the infant and adult gut [1] and can multiply in both the maternal and neonatal gut by utilizing FOS or Human milk oligosaccharides (HMOs) [18,19]. In maternal feces, we also detected predominant bacteria present in adults, such as the Clostridium coccoides group, Clostridium leptum subgroup, Bacteroides spp., and Enterobacteriaceae [1,20,21], to monitor the prebiotic effect on the microbiota other than that of bifidobacteria. In addition, we evaluated whether FOS ingestion influences stool characteristics and the frequency of adverse events in pregnant women.
2. Materials and Methods
2.1. Subjects and Study Protocol
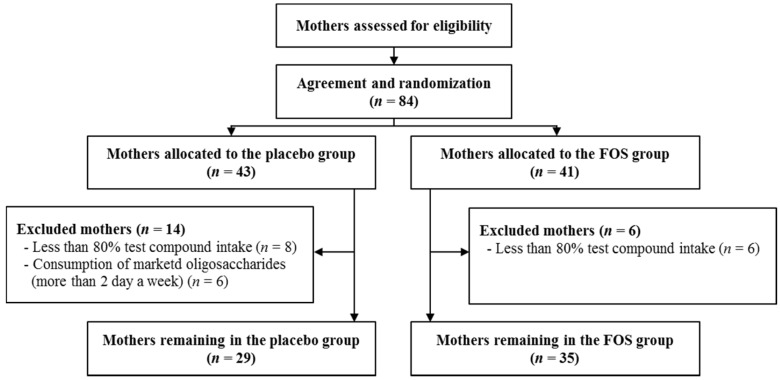
The present randomized, double-blind trial was registered in the UMIN Clinical Trial Registry (UMIN000008142) [22]. This trial was conducted at the Masuda Maternity Clinic in Chiba prefecture. Healthy pregnant woman were enrolled after they provided written informed consent from September 2009 to December 2011 [23]. Pregnant women with complications such as pregnancy-induced hypertension were excluded, although subjects with a history of allergic disease were included. The study was conducted according to the guidelines of the Declaration of Helsinki, and all the procedures were approved by the Ethics Committee of Chiba University. Subjects (84 pregnant women) were randomly assigned to the FOS (Meioligo-P, from Meiji Food Materia Company Limited, Tokyo, Japan) (FOS, n = 41) or sucrose (placebo, n = 43) intake groups (Figure 1). We administered 8 g of the trial compound as an oral daily dose between the 26th week of gestation and one month after delivery. The trial compound was divided into two 4 g doses. A 4 g dose was administered in each group twice daily. We did not impose a limit on the daily ingestion of oligosaccharides to the study subjects for ethical reasons. However, based on their diaries and food frequency questionnaire results, we excluded those subjects from the placebo group who ingest marketed oligosaccharide products for more than two days a week. In addition, we excluded those subjects from both groups with less than 80% test compound intake due to insufficient intervention (Figure 1).
Figure 1.
Diagram showing the flow of participants in the placebo and FOS groups.
2.2. Fecal Sample Collection
We collected two maternal stool samples from each subject immediately before the first treatment (at 26 weeks of gestation) and 10 weeks after the start of the treatment (at 36 weeks of gestation). In addition, we collected one neonatal stool sample per infant at one month of age. The mothers were asked to freeze the samples immediately after collection. The samples were subsequently kept frozen during transport and stored at −20 °C until further analyses.
2.3. Analysis of Fecal Microbiota
Bacterial DNA was extracted from the stool samples using a QIAamp stool mini kit (QIAGEN; Valencia, CA, USA). Briefly, 20 mg of stool samples were disrupted in 700 μL of ASL Buffer with zirconia beads (0.1 and 0.3 mm) using a tissue lyser at a frequency of 25.0 Hz for 15 min. The samples were subsequently incubated at 70 °C for 15 min. Impurities and PCR inhibitors were removed by adding InhibitEX Tablets to each sample. The DNA in the supernatants was then purified using QIAamp mini-spin columns. This procedure included protein digestion, a wash to remove any impurities, and an elution step to obtain a purified DNA sample. We used quantitative real-time polymerase chain reaction (q-RT-PCR) to quantify the number of gut microbiota using locus-specific primers, as previously described [21,24]. The primer sequences were as follows: Bifidobacterium spp. sense primer: 5′-CTCCTGGAAACGGGTGG-3′; Bifidobacterium spp. antisense primer: 5′-GGTGTTCTTCCCGATATCTACA-3′; Bacteroides spp. sense primer: 5′-ATAGCCTTTCGAAAGRAAGAT-3′; Bacteroides spp. antisense primer: 5′-CCAGTATCAACTGCAATTTTA-3′. Enterobacteriaceae sense primer: 5′-CATTGACGTTACCCGCAGAAGAAGC-3′; Enterobacteriaceae antisense primer: 5′-CTCTACGAGACTCAAGCTTGC-3′; Clostridium coccoides group sense primer: 5′-AAATGACGGTACCTGACTAA-3′; Clostridium coccoides group antisense primer: 5′-CTTTGAGTTTCATTCTTGCGAA-3′; Clostridium leptum subgroup sense primer: 5′-GCACAAGCAGTGGAGT-3′; Clostridium leptum subgroup antisense primer: 5′-CTTCCTCCGTTTTGTCAA-3′; and Bifidobacterium longum (B. longum) sense primer: 5′-TTCCAGTTGATCGCATGGTC-3′; Bifidobacterium longum antisense primer: 5′-GGGAAGCCGTATCTCTACGA-3′; Each PCR reaction mixture contained 22.5 pmol of each primer, 12.5 μL of 2× QuantiFast SYBR Green PCR Master Mix (QIAGEN; Valencia, CA, USA), and a DNA template in a total volume of 25 μL. To quantify the number of Bifidobacterium spp. in maternal and neonatal guts, we used a PCR amplification protocol comprising an initial denaturation step for 15 min at 95 °C followed by 45 cycles of melting, annealing, and extension at 94 °C for 15 s, 60 °C for 30 s, and 72 °C for 30 s, respectively. To quantify Bacteroides spp. and Clostridium leptum subgroup numbers, we used the following PCR amplification protocol: initial denaturation for 15 min at 95 °C followed by 45 cycles of melting, annealing, and extension at 94 °C for 15 s, 50 °C for 30 s, and 72 °C for 30 s, respectively. To quantify the Enterobacteriaceae number, we used the following PCR amplification protocol: initial denaturation for 15 min at 95 °C followed by 45 cycles of melting, annealing, and extension at 94 °C for 15 s, 58 °C for 30 s, and 72 °C for 30 s, respectively. To quantify the Clostridium coccoides number, we used the following PCR amplification protocol: initial denaturation for 15 min at 95 °C followed by 45 cycles of melting, annealing, and extension at 94 °C for 15 s, 50 °C for 30 s, and 72 °C for 45 s, respectively. To quantify the B. longum number, we used the following PCR amplification protocol: initial denaturation for 15 min at 95 °C followed by 45 cycles of melting, annealing, and extension at 94 °C for 15 s, 55 °C for 30 s, and 72 °C for 30 s, respectively. Calibration curves for quantification were performed with genomic DNA isolated from a known number of each species of bacteria.
2.4. Stool Characteristics and Delivery and Feeding Modes
At 24, 28, 32, and 36 weeks of gestation, we collected daily data on stool consistency and frequency, diarrhea, and abdominal pain. The outcome parameters were stool frequency per day, stool consistency according to the Bristol Stool Form Scale (stools are rated based on the water content of the feces on a scale from 1 to 7, with 1 meaning hard stools and 7 meaning liquid stools) [25], frequency of abdominal pain per week, and frequency of diarrhea per week. The mode of delivery was recorded in the hospital. The mode of feeding (i.e., breast-feeding or formula-feeding) was reported by the mothers.
2.5. Exclusion from the Analyses
In the analysis of maternal feces, we excluded one subject from the FOS group because we did not receive her stool samples. In the analysis of the neonatal feces, we excluded those neonates born by cesarean delivery (C-section) were excluded (n = 2 and n = 3 for the placebo and FOS group, respectively) because the mode of delivery influences the compositon of neonatal microbiota [26,27]. We also excluded two neonates from the placebo group because we did not receive their stool samples. In the analysis of B. longum of neonatal feces, one neonate was additionally excluded because of the absence of the sample. Finally, in the stool characteristic and adverse event analyses, we excluded those mothers who did provide with less than four daily records per week.
2.6. Statistics
The values are expressed as medians or means, depending on their distribution. We compared the differences between groups using Student’s t-test for parametric data, Mann-Whitney U test for nonparametric data and chi-squared tests for categorical data. To determine the relation between the number of fecal bifidobacteria in mothers and neonates, we used the Spearman’s rank correlation coefficient. For all tests, p < 0.05 was considered statistically significant. The statistical analyses were performed using the Bell Curve for Excel (Social Survey Research Information Co., Ltd., Tokyo, Japan).
3. Results
After exclusions, we included 29 subjects in the placebo group and 35 in the FOS group (Figure 1). As previously reported, no significant differences were observed in the characteristics and dietary habits of the subjects between the groups (Table 1) [23].
Table 1.
Characteristics of the mothers and the neonates.
| Placebo Group n = 29 | FOS Group n = 35 | p | |
|---|---|---|---|
| Mothers’ characteristics | |||
| Age (median, years) | 33 | 30 | N.S.* |
| Primipara (n) | 13 | 16 | N.S. † |
| Pollen disease (n) | 8 | 10 | N.S. † |
| History of atopic diseases (n) | 1 | 6 | N.S. † |
| History of other allergic diseases (n) | 10 | 20 | N.S. † |
| Smoking during pregnancy (n) | 6 | 3 | N.S. † |
| BMI during prepregnancy (median) | 21.2 | 20.3 | N.S. * |
| BMI during pregnancy (median) | 25.3 | 24.6 | N.S. * |
| Neonates’ characteristics | |||
| Fetus week number (median, weeks) | 39.1 | 39.3 | N.S. * |
| Birth weight (median, g) | 2990 | 3165 | N.S. * |
| Caesarean section (n) | 2 | 3 | N.S. † |
| Exclusively breastfed (n) | 14 | 16 | N.S. † |
| Exclusively formula-fed (n) | 0 | 0 | N.S. † |
FOS, fructo-oligosaccharides. BMI, body mass index. * Mann–Whitney U-test. † Pearson’s x2 test.
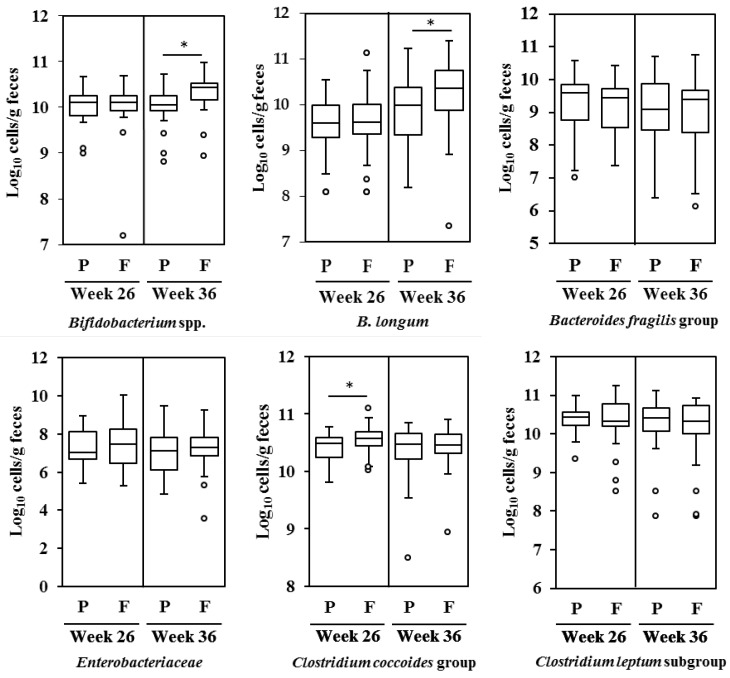
Figure 2 shows the estimated number of Bifidobacterium spp., B. longum, the Bacteroides fragilis group, Enterobacteriaceae, the Clostridium coccoides group, and the Clostridium leptum subgroup in maternal feces at 26 and 36 weeks of gestation (before intervention and 10 weeks after intervention, respectively), based on q-RT-PCR data. The number of fecal Bifidobacterium spp. in the FOS group at 36 weeks of gestation (2.7 × 1010/g) was significantly higher than that in the placebo group (1.1 × 1010/g, Mann-Whitney U test, p < 0.05, Figure 2). Also, the number of fecal B. longum in the FOS group at 36 weeks of gestation (2.3 × 1010/g) was significantly higher than that in the placebo group (9.7 × 109/g, Mann-Whitney U test, p < 0.05, Figure 2). The number of fecal Clostridium coccoides before the intervention was also higher in the FOS group than that in the placebo group (Mann-Whitney U test, p < 0.05, Figure 2).
Figure 2.
The number of gut microbiota, expressed as the logarithm of cell numbers, in maternal feces at 26 and 36 weeks of gestation. Microbiota were quantified using q-RT-PCR (n = 29 and 34 for the placebo and FOS group, respectively). Box and whiskers plot, with the black horizontal line representing the median value and the boxes the interquartile ranges. The T-bars represent the data range, and the open circles indicate the presence of outliers (data points more than 1.5 interquartile ranges below the first quartile or above the third quartile). * Statistically different based on a Mann-Whitney U test (p < 0.05). P: Placebo group; F: FOS group.
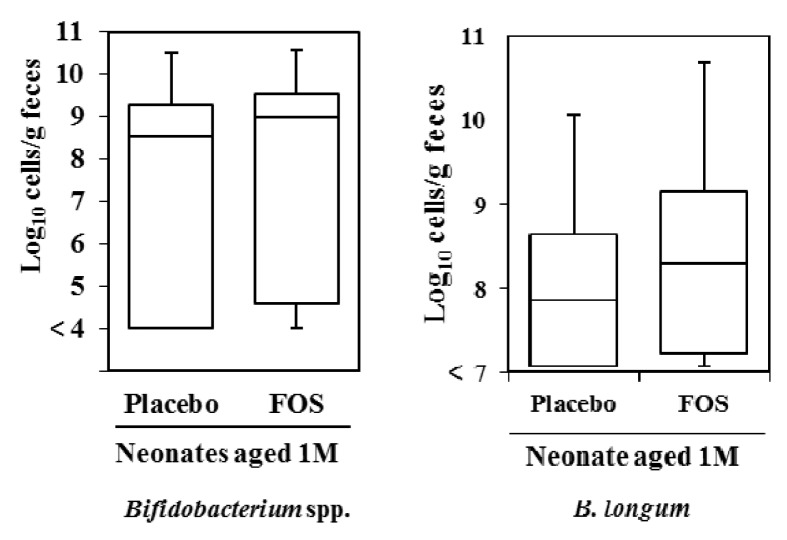
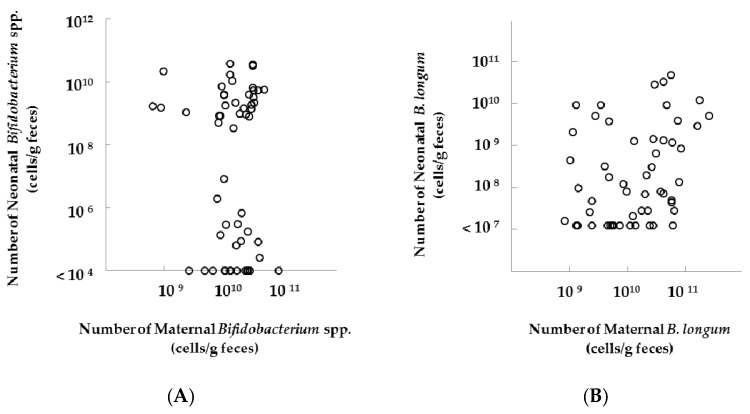
In the analyses of neonatal feces, we did not observe any differences in the number of Bifidobacterium spp. and B. longum in neonates at one month of age between groups, after excluding neonates born by C-section (Figure 3). Additionally, we found no correlation in the number of fecal Bifidobacterium spp. (ρ = 0.09, p = 0.50, Figure 4) and a significant correlation in the number of fecal B. longum (ρ = 0.33, p = 0.01, Figure 4) between mothers and their neonates (Spearman’s rank correlation coefficient, Figure 4). In the subgroup analysis, the significant positive correlation in the fecal number of B. longum was observed between mothers and their neonates in the FOS group (Spearman’s rank correlation coefficient, ρ = 0.52, p < 0.05, Table 2).
Figure 3.
Infant fecal Bifidobacterium spp. and B. longum at one month of age, excluding neonates born by C-section. The number of Bifidobacterium spp. was quantified using q-RT-PCR (n = 25 and 30 in the analysis of B. longum) for the placebo and FOS group, respectively). Box and whiskers plot, with the black horizontal line representing the median value and the boxes the interquartile ranges. The T-bars represent the data range, and the open circles indicate the presence of outliers (data points more than 1.5 interquartile ranges below the first quartile or above the third quartile). No significant difference was observed between the groups (Mann-Whitney U test).
Figure 4.
Relations between the number of fecal (A) Bifidobacterium spp. or (B) B. longum in mothers (at 36 weeks of gestation) and their neonates (one month after delivery), excluding neonates born by C-section. The number of Bifidobacterium spp. was quantified using q-RT-PCR (n = 25 and 31 in placebo and FOS group, respectively). Data were analyzed using the Spearman’s rank correlation coefficient ((A): ρ = 0.09, p = 0.50; (B): ρ = 0.33, p = 0.01).
Table 2.
Subgroup analysis for relation between the number of fecal bifidobacteria in mothers and their neonates.
| Subgroup | Bifidobacterium spp. | B. longum | |||||
|---|---|---|---|---|---|---|---|
| n | ρ | p | n | ρ | p | ||
| Placebo-group | All infants | 25 | 0.19 | 0.37 | 25 | −0.22 | 0.25 |
| Exclusively breastfed infants | 13 | 0.41 | 0.16 | 13 | 0.14 | 0.64 | |
| FOS-group | All infants | 31 | −0.02 | 0.94 | 30 | 0.49 | 0.01 |
| Exclusively breastfed infants | 16 | 0.15 | 0.56 | 16 | 0.40 | 0.17 | |
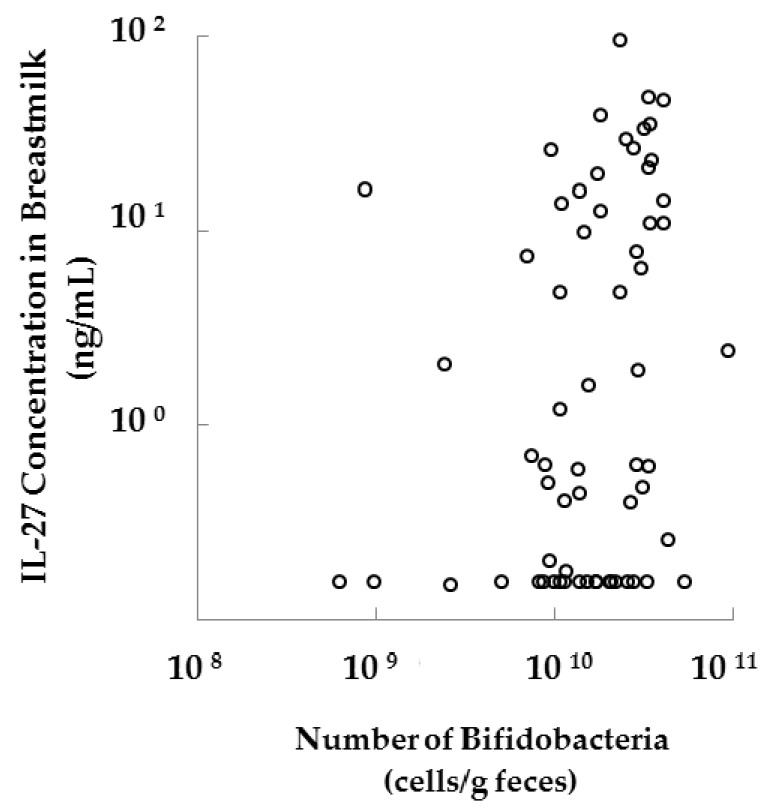
We did not find any significant difference between groups regarding the stool form score, frequency of abdominal pain, and frequency of diarrhea two weeks before the intervention or two, six, and 10 weeks after the intervention (at 24, 28, 32, 36 weeks of gestation, respectively) (Table 3). Stool frequency in the FOS group was significantly higher only two weeks after the intervention (28 weeks of gestation) than in the placebo group (1.0 vs. 0.8 times per day, Mann-Whitney U test, p < 0.05). In addition, a significant correlation was observed between the fecal bifidobacterial count in mothers and the interleukin-27 (IL-27) concentration in their breast milk (IL-27 concentration was shown in our previous report [23]) (Spearman’s rank correlation coefficient, p < 0.05, Figure A1).
Table 3.
Stool characteristics and adverse events recorded in pregnant women two weeks before the intervention and two, six, and 10 weeks after the intervention.
| Weeks of Gestation | 24 | 28 | 32 | 36 | ||||
| Weeks from the Start of Supplementation | −2 | 2 | 6 | 10 | ||||
| Group | P | F | P | F | P | F | P | F |
| n | 25 | 27 | 26 | 31 | 24 | 33 | 25 | 32 |
| Stool frequency (times per day), median | 0.9 | 1.0 | 0.8 | 1.0 * | 1.1 | 1.0 | 1.2 | 1.0 |
| Stool form score, mean | 3.9 | 4.2 | 3.9 | 4.2 | 3.9 | 4.0 | 3.9 | 4.3 |
| Frequency of abdominal pain (days per week), median | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| frequency of diarrhea (days per week), median | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
P = Placebo-group, F = Fructooligosaccharides-group. * P < 0.05 (Mann-Whitney U test).
4. Discussion
The present clinical trial investigated the effects of maternal prebiotic ingestion on maternal and neonatal gut bifidobacteria. Here, we show that the daily FOS intake (8 g/day) increased the number of fecal bifidobacteria in pregnant women, consistent with previous reports describing FOS bifidogenic activity at doses ranging from 2.5 to 10 g/day in healthy humans [28]. However, there was no difference in the number of fecal bifidobacteria between neonates whose mothers received FOS and those whose mothers did not take FOS (control). Also, stool frequency in the FOS group was slightly higher than that in the placebo group two weeks after the intervention (1.0 vs. 0.8 times/day), suggesting a potential constipation alleviation effect.
The present study showed that the FOS-mediated increase in maternal fecal bifidobacteria did not affect the number of Bifidobacterium spp. in the feces of neonates aged one month. These results are also supported by a previous study on maternal supplementation with another prebiotic (galactooligosaccharides/long-chain FOS) [15], which showed that the proportion of bifidobacteria found in neonatal feces did not differ between the placebo and the supplemented groups. In addition, we find no significant correlations between the number of fecal Bifidobacterium spp. in mothers and their neonates, which is also consistent with previous non-interventional studies [3,29]. There are some aspects that could explain these results. First, the effect of maternal FOS ingestion in neonates might appear earlier (within the first month after birth). Second, maternal FOS ingestion might not lead to a significant increase in the number of vaginal bifidobacteria to be detected as transferred to the neonate because dietary FOS cannot reach the vagina. Third, the bifidobacterial species that were transferred to infants could not increase in the individual intestinal microbiome because neonatal stable engraftment of bifidobacteria was shown to depend on the individual microbiome [30]. Fourth, if the bifidobacterial species that were transferred to infants were not genetically capable of utilizing or degrading HMOs in breast milk, then the neonatal bifidobacterial number would not increase. In fact, the abundance of fecal bifidobacteria in neonates was shown to be greatly influenced by the utilization of HMOs [18]. To consider the fourth aspect, we quantified the number of B. longum in the maternal and neonatal feces. Here, maternal FOS ingestion resulted in high levels of B. longum in the mothers but not in their neonates, although it is capable of utilizing HMOs [18]. Thus, we found no evidence of a bifidogenic effect on the neonates by maternal FOS ingestion.
In the present study, 30 of 64 infants were exclusively breastfed at one month (Table 1). This low percentage for exclusive breastfeeding may have influenced the low correlation between maternal and infant fecal bifidobacteria. To clarify the effect of breastfeeding on the bifidobacterial transfer, we performed subgroup analyses on the number of Bifidobacterium spp. in exclusively breastfed infants of each group. Then, we did not find any significant correlation in exclusively breastfeeding pairs (Table 2). Meanwhile, the correlation seems to be higher in exclusively breastfed infants than in all infants. Interestingly, this correlation was low in the FOS group. It might be because bifidobacteria species that can utilize FOS but not HMOs increased in the maternal feces of the FOS group. Further research is required to investigate the effect of breastfeeding on the bacterial transfer.
The present study showed that FOS was well tolerated by pregnant women at a dose of 8 g/day. Previous clinical trials assessing an FOS intake of ≤10 g/day have been reported for adult women [31,32,33,34,35]; however, the number of reports on FOS perinatal ingestion in women has reduced [17]. In the present study, we found no differences in the frequency of abdominal symptoms in the FOS group compared with those in the placebo group until 10 weeks after the start of the intervention. Additionally, the maternal FOS intake (8 g/day) was shown to increase the number of fecal bifidobacteria. These findings suggested that the ingested dose of FOS (8 g/day) was appropriate for pregnant women.
Our results suggest a potential constipation alleviation effect of FOS in pregnant women. The prevalence of constipation in pregnancy ranges from 11% to 44% [36] and has been associated with a decrease in the quality of life for pregnant women. Dietary supplementation composed of FOS, Lactobacillus, and Bifidobacterium has been shown to increase stool frequency in constipated adult women [32]. A similar effect has been observed for probiotics [37] or FOS [38]. However, little is known about the effect of FOS on stool frequency in pregnant women [17]. The increased stool frequency observed in our results suggested that dietary FOS helps alleviate the gastrointestinal discomfort in pregnant women. Further research in pregnant women with constipation should investigate the effect of FOS ingestion on constipation during pregnancy.
Maternal prebiotic consumption may also affect immunoactive constituents in breast milk by altering the gut microbiota. In a previous report on this clinical trial, we showed that the IL-27 concentration in breast milk increased in the FOS group compared with that in the placebo group [23]. A further analysis also showed a significant correlation between the IL-27 concentration in breast milk and bifidobacterial counts in maternal feces (Figure A1; the Spearman’s rank correlation coefficient, p < 0.05). Dietary FOS has been shown to increase the number of gut Bifidobacterium spp. and Bacteroides spp. as well as the total IgA concentration in both the intestine and milk in mice, and the IgA concentration in milk was correlated with the number of gut Bacteroides spp. [39]. In the present study, however, the IgA concentration in the colostrum did not differ between the groups [23]. A possible cause is the presence of a large individual diversity in the gut microbiota that utilize prebiotics. In fact, the IgA concentration did not change in response to dietary FOS in some subjects [40]. Thus, the choice of prebiotics may be important to provide the appropriate immunomodulating effect in neonates through breast milk.
There are some limitations of this study. First, we did not control the daily consumption of oligosaccharides in pregnant women for ethical reasons. Consequently, we excluded those subjects who consumed marketed oligosaccharide products for more than two days a week from the placebo group. Thus, the increases in the number of fecal bifidobacteria and stool frequency found in the FOS group might partly result from the consumption of other oligosaccharides. Second, we quantified the number of bacteria by using q-RT-PCR. A 16S rRNA gene-based metagenomic analysis would add a great deal to the study results.
5. Conclusions
In conclusion, the present study showed a bifidogenic effect of FOS in pregnant women at a dose of 8 g/d with no evidence of adverse effects. Also, no evidence was obtained about a bifidogenic effect on the neonates by maternal FOS ingestion.
Acknowledgments
The authors are extremely grateful to the pregnant women for their participation. They also thank Takehiro Yokoo for measuring the number of fecal microbiota and Kae Yamazaki for preparing daily record of stool characteristics. The present study was partly supported by a grant of Program for Fostering Regional Innovation from the MEXT (Ministry of Education, Culture, Sports, Science and Technology). MEXT had no role in the design and analysis of the study.
Appendix A
Figure A1.
A significant correlation between the fecal bifidobacterial count in mothers and IL-27 concentration in their breast milk. The number of Bifidobacterium spp. was quantified by q-RT-PCR (n = 29 and 34 for the placebo and FOS group, respectively). IL-27 in colostrum whey was detected using The Human IL-27 DuoSet ELISA kit (R&D Systems). Data were analyzed using the Spearman’s rank correlation coefficient (p < 0.05).
Author Contributions
Y.N., S.S., Y.K., K.M. and N.S. designed the study; T.K., Y.I, N.O., T.N., Y.M., T.A., F.Y. and K.M. conducted the study; S.J. and T.T. analyzed stool samples; S.J., Y.N. and N.S. analyzed the data and S.J. wrote the paper. All authors read and approved the final manuscript.
Conflicts of Interest
S.J., T.T. and Y.N. are employed by Meiji Co., Ltd. The authors declare no conflict of interest.
References
- 1.Mitsuoka T. Establishment of intestinal bacteriology. Biosci. Microbiota Food Health. 2014;33:99–116. doi: 10.12938/bmfh.33.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tannock G.W., Fuller R., Smith S.L., Hall M.A. Plasmid profiling of members of the family Enterobacteriaceae, lactobacilli, and bifidobacteria to study the transmission of bacteria from mother to infant. J. Clin. Microbiol. 1990;28:1225–1228. doi: 10.1128/jcm.28.6.1225-1228.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mikami K., Takahashi H., Kimura M., Isozaki M., Izuchi K., Shibata R., Sudo N., Matsumoto H., Koga Y. Influence of maternal bifidobacteria on the establishment of bifidobacteria colonizing the gut in infants. Pediatr. Res. 2009;65:669–674. doi: 10.1203/PDR.0b013e31819ed7a8. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz L., Moles L., Gueimonde M., Rodriguez J.M. Perinatal microbiomes influence on preterm birth and preterms’ health: Influencing factors and modulation strategies. J. Pediatr. Gastroenterol. Nutr. 2016;63:e193–e203. doi: 10.1097/MPG.0000000000001196. [DOI] [PubMed] [Google Scholar]
- 5.Arboleya S., Binetti A., Salazar N., Fernández N., Solís G., Hernández-Barranco A., Margolles A., de los Reyes-Gavilán C.G., Gueimonde M. Establishment and development of intestinal microbiota in preterm neonates. FEMS Microbiol. Ecol. 2012;79:763–772. doi: 10.1111/j.1574-6941.2011.01261.x. [DOI] [PubMed] [Google Scholar]
- 6.Jakobsson H.E., Abrahamsson T.R., Jenmalm M.C., Harris K., Quince C., Jernberg C., Björkstén B., Engstrand L., Andersson A.F. Decreased gut microbiota diversity, delayed Bacteroidetes colonisation and reduced Th1 responses in infants delivered by caesarean section. Gut. 2014;63:559–566. doi: 10.1136/gutjnl-2012-303249. [DOI] [PubMed] [Google Scholar]
- 7.Arboleya S., Sánchez B., Milani C., Duranti S., Solís G., Fernández N., De Los Reyes-Gavilán C.G., Ventura M., Margolles A., Gueimonde M. Intestinal microbiota development in preterm neonates and effect of perinatal antibiotics. J. Pediatr. 2015;166:538–544. doi: 10.1016/j.jpeds.2014.09.041. [DOI] [PubMed] [Google Scholar]
- 8.Gomez-Llorente C., Plaza-Diaz J., Aguilera M., Muñoz-Quezada S., Bermudez-Brito M., Peso-Echarri P., Martinez-Silla R., Vasallo-Morillas M.I., Campaña-Martin L., Vives-Piñera I., et al. Three main factors define changes in fecal microbiota associated with feeding modality in infants. J. Pediatr. Gastroenterol. Nutr. 2013;57:461–466. doi: 10.1097/MPG.0b013e31829d519a. [DOI] [PubMed] [Google Scholar]
- 9.Soto A., Martín V., Jiménez E., Mader I., Rodríguez J.M., Fernández L. Lactobacilli and Bifidobacteria in Human Breast Milk. J. Pediatr. Gastroenterol. Nutr. 2014;59:78–88. doi: 10.1097/MPG.0000000000000347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar H., du Toit E., Kulkarni A., Aakko J., Linderborg K.M., Zhang Y., Nicol M.P., Isolauri E., Yang B., Collado M.C., et al. Distinct Patterns in Human Milk Microbiota and Fatty Acid Profiles Across Specific Geographic Locations. Front. Microbiol. 2016;7:1619. doi: 10.3389/fmicb.2016.01619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gomez-Gallego C., Garcia-Mantrana I., Salminen S., Collado M.C. The human milk microbiome and factors influencing its composition and activity. Semin. Fetal Neonatal Med. 2016;21:400–405. doi: 10.1016/j.siny.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Cummings J.H., Antoine J., Azpiroz F., Bourdet-Sicard R., Brandtzaeg P., Calder P.C., Gibson G.R., Guarner F., Isolauri E., Pannemans D., et al. PASSCLAIM—Gut health and immunity. Eur. J. Nutr. 2004;43(Suppl. 2):II118–II173. doi: 10.1007/s00394-004-1205-4. [DOI] [PubMed] [Google Scholar]
- 13.Grönlund M.M., Arvilommi H., Kero P., Lehtonen O.P., Isolauri E. Importance of intestinal colonisation in the maturation of humoral immunity in early infancy: A prospective follow up study of healthy infants aged 0–6 months. Arch. Dis. Child. Fetal Neonatal Ed. 2000;83:F186–F192. doi: 10.1136/fn.83.3.F186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gomez de Agüero M., Ganal-Vonarburg S.C., Fuhrer T., Rupp S., Uchimura Y., Li H., Steinert A., Heikenwalder M., Hapfelmeier S., Sauer U., et al. The maternal microbiota drives early postnatal innate immune development. Science. 2016;351:1296–1302. doi: 10.1126/science.aad2571. [DOI] [PubMed] [Google Scholar]
- 15.Shadid R., Haarman M., Knol J., Theis W., Beermann C., Rjosk-Dendorfer D., Schendel D.J., Koletzko B.V., Krauss-Etschmann S. Effects of galactooligosaccharide and long-chain fructooligosaccharide supplementation during pregnancy on maternal and neonatal microbiota and immunity—A randomized, double-blind, placebo-controlled study. Am. J. Clin. Nutr. 2007;86:1426–1437. doi: 10.1093/ajcn/86.5.1426. [DOI] [PubMed] [Google Scholar]
- 16.Bornet F.R.J., Brouns F. Immune-stimulating and gut health-promoting properties of short-chain fructo-oligosaccharides. Nutr. Rev. 2002;60:326–334. doi: 10.1301/002966402320583442. [DOI] [PubMed] [Google Scholar]
- 17.Tani M. Effect of Fructooligosaccharides on conspitaion in pregnant and lying-in women. Matern. Health. 1990;31:352–357. [Google Scholar]
- 18.Matsuki T., Yahagi K., Mori H., Matsumoto H., Hara T., Tajima S., Ogawa E., Kodama H., Yamamoto K., Yamada T., et al. A key genetic factor for fucosyllactose utilization affects infant gut microbiota development. Nat. Commun. 2016;7:11939. doi: 10.1038/ncomms11939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitsuoka T., Hidaka H., Eida T. Effect of fructo-oligosaccharides on intestinal microflora. Nahrung. 1987;31:427–436. doi: 10.1002/food.19870310528. [DOI] [PubMed] [Google Scholar]
- 20.Matsuki T., Watanabe K., Fujimoto J., Miyamoto Y., Takada T., Matsumoto K., Oyaizu H., Tanaka R. Development of 16S rRNA-gene-targeted group-specific primers for the detection and identification of predominant bacteria in human feces. Appl. Environ. Microbiol. 2002;68:5445–5451. doi: 10.1128/AEM.68.11.5445-5451.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsuki T., Watanabe K., Fujimoto J., Takada T. Use of 16S rRNA Gene-Targeted Group-Specific Primers for Real-Time PCR Analysis of Predominant Bacteria in Human Feces Use of 16S rRNA Gene-Targeted Group-Specific Primers for Real-Time PCR Analysis of Predominant Bacteria in Human Feces. Appl. Environ. Microbiol. 2004;70:7220–7228. doi: 10.1128/AEM.70.12.7220-7228.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.University Hospital Medical Information Network (UMIN) Center. [(accessed on 25 February 2016)]. Available online: http://www.umin.ac.jp/
- 23.Kubota T., Shimojo N., Nonaka K., Yamashita M., Ohara O., Igoshi Y., Ozawa N., Nakano T., Morita Y., Inoue Y., et al. Prebiotic consumption in pregnant and lactating women increases IL-27 expression in human milk. Br. J. Nutr. 2013;18:1–8. doi: 10.1017/S0007114513003036. [DOI] [PubMed] [Google Scholar]
- 24.Matsuki T., Watanabe K., Fujimoto J., Takada T., Matsumoto K., Kado Y. Quantitative PCR with 16S Primers for Analysis of Human Intestinal Bifidobacteria. Appl. Environ. Microbiol. 2004;70:167–173. doi: 10.1128/AEM.70.1.167-173.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewis S.J., Heaton K.W. Stool form scale as a useful guide to intestinal transit time. Scand. J. Gastroenterol. 1997;32:920–924. doi: 10.3109/00365529709011203. [DOI] [PubMed] [Google Scholar]
- 26.Grönlund M.M., Lehtonen O.-P.P., Eerola E., Kero P. Fecal microflora in healthy infants born by different methods of delivery: Permanent changes in intestinal flora after cesarean delivery. J. Pediatr. Gastroenterol. Nutr. 1999;28:19–25. doi: 10.1097/00005176-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Bennet R., Nord C.E. R bennet development of the faecal anaerobic microflora. Infection. 1987;15:332–336. doi: 10.1007/BF01647733. [DOI] [PubMed] [Google Scholar]
- 28.Bouhnik Y., Raskine L., Simoneau G., Paineau D., Bornet F. The capacity of short-chain fructo-oligosaccharides to stimulate faecal bifidobacteria: A dose-response relationship study in healthy humans. Nutr. J. 2006;5:8. doi: 10.1186/1475-2891-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grönlund M., Gueimonde M., Laitinen K., Kociubinski G., Gronroos T., Salminen S., Isolauri E. Maternal breast-milk and intestinal bifidobacteria guide the compositional development of the bifidobacterium microbiota in infants at risk of allergic disease. Clin. Exp. Allergy. 2007;37:1764–1772. doi: 10.1111/j.1365-2222.2007.02849.x. [DOI] [PubMed] [Google Scholar]
- 30.Maldonado-Gomez M.X., Ines M., Bottacini F., O’Callaghan A., Ventura M., van Sinderen D., Hillmann B., Vangay P., Knights D., Hutkins R.W., et al. Stable engraftment of Bifidobacterium longum AH1206 in the human gut depends on individualized features of the resident microbiome. Cell Host Microbe. 2016;20:515–526. doi: 10.1016/j.chom.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Tahiri M., Tressol J.C., Arnaud J., Bornet F., Ducros R., Bouteloup-demange C., Feillet-coudray C., Pin D.P.E., Brouns F., Roussel A.M., et al. Five-Week Intake of Short-Chain Fructo-Oligosaccharides Increases Intestinal Absorption and Status of Magnesium in Postmenopausal Women. J. Bone Miner. Res. 2001;16:2152–2160. doi: 10.1359/jbmr.2001.16.11.2152. [DOI] [PubMed] [Google Scholar]
- 32.Waitzberg D.L., Logullo L.C., Bittencourt A.F., Torrinhas R.S., Shiroma G.M., Paulino N.P., Teixeira-da-silva M.L. Effect of synbiotic in constipated adult women e A randomized, double-blind, placebo-controlled study of clinical response q. Clin. Nutr. 2013;32:27–33. doi: 10.1016/j.clnu.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 33.Tousen Y., Uehara M., Abe F., Kimira Y., Ishimi Y. Effects of short-term fructooligosaccharide intake on equol production in Japanese postmenopausal women consuming soy isoflavone supplements: A pilot study. Nutr. J. 2013;12:127. doi: 10.1186/1475-2891-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ducros V., Arnaud J., Tahiri M., Coudray C., Bornet F., Bouteloup-Demange C., Brouns F., Rayssiguier Y., Roussel A.M. Influence of short-chain fructo-oligosaccharides (sc-FOS) on absorption of Cu, Zn, and Se in healthy postmenopausal women. J. Am. Coll. Nutr. 2005;24:30–37. doi: 10.1080/07315724.2005.10719440. [DOI] [PubMed] [Google Scholar]
- 35.Tahiri M., Tressol J.C., Arnaud J., Bornet F.R.J., Bouteloup-Demange C., Feillet-Coudray C., Brandolini M., Ducros V., Pépin D., Brouns F., et al. Effect of short-chain fructooligosaccharides on intestinal calcium absorption and calcium status in postmenopausal women: A stable-isotope study. Am. J. Clin. Nutr. 2003;77:449–457. doi: 10.1093/ajcn/77.2.449. [DOI] [PubMed] [Google Scholar]
- 36.Rungsiprakarn P., Laopaiboon M., Sangkomkamhang U.S., Lumbiganon P., Pratt J.J. Interventions for treating constipation in pregnancy. Cochrane Database Syst. Rev. 2015;9:CD011448. doi: 10.1002/14651858.CD011448.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dimidi E., Christodoulides S., Fragkos K.C., Scott S.M., Whelan K. The effect of probiotics on functional constipation in adults: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2014;100:1075–1084. doi: 10.3945/ajcn.114.089151. [DOI] [PubMed] [Google Scholar]
- 38.Tominaga S., Hirayama M., Adachi T., Tokunaga T., Iino H. Effects of Ingested Fructooligosaccharides on Stool Frequency in Healthy Female Volunteers: A Placebo-Controlled Study. Biosci. Microflora. 1999;18:49–53. doi: 10.12938/bifidus1996.18.49. [DOI] [Google Scholar]
- 39.Jinno S., Nakamura Y., Nagata M., Takahashi T. 1-Kestose consumption during pregnancy and lactation increases the levels of IgA in the milk of lactating mice. Biosci. Biotechnol. Biochem. 2014;78:861–866. doi: 10.1080/09168451.2014.905179. [DOI] [PubMed] [Google Scholar]
- 40.Kato T., Fukuda S., Fujiwara A., Suda W., Hattori M., Kikuchi J., Ohno H. Multiple omics uncovers host-gut microbial mutualism during prebiotic fructooligosaccharide supplementation. DNA Res. 2014;21:469–480. doi: 10.1093/dnares/dsu013. [DOI] [PMC free article] [PubMed] [Google Scholar]