Abstract
Purpose
To describe the transition from mentored to independent research funding for clinical and translational scholars supported by institutional KL2 Mentored Career Development programs.
Method
In 2013, faculty leaders at Clinical and Translational Science Award institutions completed an online survey, reporting characteristics of scholars in their KL2 programs from 2006–2013. The primary outcome variable was a report that the scholar had received independent research funding as a principal investigator. Data analysis included descriptive summaries and mixed effects regression models.
Results
Respondents from 48 institutions (of 62 eligible; 77%) provided information about 914 KL2 scholars. Of those, 620 (68%) were medical doctors, 114 (12%) had other clinical training, and 177 (19%) were non-clinician PhDs. Fifty-three percent (487) were female; 12% (108/865) were members of racial or ethnic groups underrepresented in medicine (URM). After completing KL2 training, 96% (558/582) remained engaged in research. Among scholars who completed KL2 training two or more years earlier, 39% (149/374) had received independent funding. Independent funding was from non-National Institutes of Health (NIH) sources (120 scholars) more often than from NIH (101 scholars). The odds of a non-clinician attaining independent funding were twice those of a clinician (odds ratio 2.05, 95% confidence interval 1.11–3.78). Female and URM scholars were equally as likely as male and non-URM scholars to attain independent funding.
Conclusions
KL2 programs supported the transition to independent funding for clinical and translational scientists. Female and URM scholars were well represented. Future studies should consider non-NIH funding sources when assessing the transition to research independence.
In the discussion of developing the clinical and translational researcher workforce,1–4 the transition from mentored to independent research funding has been recognized as a critical juncture in the career of an investigator.5,6 Starting in 2006, institutions that received the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) began implementing KL2 Mentored Career Development programs to support scholars through this transition.3,7 Individuals eligible for the KL2 award must have earned a health professional or research doctorate or equivalent and must not have received a current or past NIH or equivalent research project grant award.8 Through the KL2 award, scholars receive salary support for 75% effort and other support for research and career development activities.
KL2 scholars are selected by their institution and may be awarded support for two to five years. A KL2 scholar subsequently may apply for an individual mentored career development award (CDA) before transitioning to independent research funding or may apply for an independent research project grant directly following his or her period of KL2 support. The CTSA KL2 scholar population across institutions has been described with respect to supporting child health investigators,9 but other characteristics have not been comprehensively described. A survey conducted early in the program’s history found that only 10% of scholars had applied for NIH R01 funding through 201010; the source and type of peer-reviewed funding attained by KL2 scholars has not been further delineated.
Research evaluating the mentored-to-independent research funding transition has usually defined research independence based on one criterion--receipt of an NIH research project grant or R01 award.5,11–14 For example, within 10 years of the end of their K support, 50% of K08 and K23 scholars were reported to have attained NIH research project grant funding as principal investigators (PIs).12 However, most of the existing literature does not take into account non-NIH sources of independent funding for clinical and translational researchers, which may include foundation-funded awards and Veterans Health Administration (VHA) merit review awards.
We sought to characterize the population of scholars supported by the KL2 mechanism (1) to describe their attainment of both individual CDAs and independent peer-reviewed funding, including funding from non-NIH sources, and (2) to determine the factors associated with success in the transition from mentored to independent research funding.
Method
Survey development and content
The Mentored-to-Independent Investigator Transition working group, formed under the auspices of the CTSA Education and Career Development Key Function Committee, conceived of the study goals described above. There are no centralized sources of information on the demographics, training, and grant outcomes of KL2 scholars across institutions. Therefore, we developed a survey to collect these data. Survey items addressing the study goals were drafted based on a review of the existing literature on the mentored-to-independent funding transition and on the experiences of the working group members as mentors. The survey was beta-tested by the working group members and revised based on working group member feedback.
We administered the survey to research education and career development faculty leaders at CTSA institutions. One section of the survey requested information about each clinical and translational research scholar at the respondent’s institution who received mentored career development support through the KL2 program from 2006 to 2013. That information included the scholar’s prior clinical and PhD training, sex, race, and ethnicity. If the scholar had completed her or his KL2 training, the respondent was then asked “Is the scholar currently engaged in clinical or translational research?” They also were asked if the scholars had obtained one (or more) of three types of subsequent awards: (1) “Did the scholar go on to conduct further mentored research under an individual, peer-reviewed, training award mechanism? This would include an NIH K23, an NIH K08, a VHA Career Development Award, or other multi-year mentored research training grant.” (2) “Has the scholar been awarded funding as PI of an NIH R01 or as PI of a project within an NIH program project or center award, e.g. ‘P01’ mechanism?” (3) “Has the scholar been awarded funding as PI of an independent, externally-funded, non-NIH, peer-reviewed research project of 3 or more years duration? This would include, for example, a VHA merit award or a foundation-funded investigator-initiated research project award. Do not include mentored research projects or industry-funded trials.”
Survey sample and administration
We defined our sample of survey recipients as one faculty representative to the Education and Career Development Committee from each CTSA institution. Contact information was obtained through committee membership lists. Following pre-notification of the survey during committee conference calls, each representative received an e-mail with an invitation to participate and a link to the online survey, which was available through REDCap.15 Non-respondents to the initial e-mail received follow-up communications. Surveys were completed from April through May 2013. Survey instructions encouraged respondents to respond to all items. The REDCap survey instrument was programmed so that if a response to any question was unknown, the respondent could still proceed with the rest of the survey. Respondents could exit the partially completed survey and return later. In addition, a copy of the survey was available in a downloadable, printable format so that respondents could refer to records for each scholar at their institution and compile information offline before returning to submit the completed survey online.
The institutional review boards at the University of Utah Health Sciences Center and Icahn School of Medicine at Mount Sinai determined this study to be non-human subjects research.
Data analysis
We categorized scholars who were reported to be Black or African American, American Indian or Alaska Native, Native Hawaiian or Pacific Islander, or Hispanic or Latino as belonging to racial and ethnic groups underrepresented in medicine (URM). We created an outcome variable for the successful transition to independent research funding, which represented a “yes” response to the question about receiving an NIH independent award as PI and/or a “yes” response to the question about receiving an independent research award from a non-NIH source. Institutions were categorized as being located in one of four geographic regions of the country (Northeast, Midwest, South, and West), as defined by the U.S. Census Bureau; additionally, we created a variable for the size of the institutions, which represented the amount of NIH funding they received, by tertile (small, medium, large).
Our primary analysis was descriptive; we used contingency tables and summary statistics to report our results. Differences in the distributions of scholars by sex and by URM status were assessed using Pearson’s chi square tests. We estimated associations between the transition to independence variable and characteristics of the individual scholars and institutions using odds ratios from mixed effects regression models; we addressed the clustering of scholars within institutions by treating the institution as a random effect. Stata software version 12 (Stata Corp., College Station, TX) was used for all analyses. P values less than .05 were described as significant.
Results
Respondents from 48 institutions (of 62 eligible institutions; 77%) provided information about 914 individuals supported by the KL2 mechanism from 2006–2013. Responding and non-responding institutions did not differ by size (i.e., NIH funding) or by region of the United States. The median number of scholars per institution was 13.5, the interquartile range was 9.5 – 24.5, with a minimum of 2 and a maximum of 78. Of these KL2 scholars, 68% (620/914) were medical doctors, 19% (177/914) were non-clinician PhDs, and the remainder were from a range of other health professions (see Table 1). Among clinicians who were not medical doctors, the largest group was nurses, followed by psychologists and pharmacists. Forty-one percent of scholars (368/897) held a PhD at the time of their appointment as a KL2 scholar.
Table 1.
Characteristics of Mentored Career Development (KL2) Scholars at 48 Clinical and Translational Science Award Institutions, 200–2013
| All scholars | Male scholars |
Female scholars |
URM scholarsa |
Non-URM scholars |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | no. | % | no. | % | no. | % | no. | % | no. | % |
| Totalb | 914 | 426 | 487 | 108 | 757 | |||||
| Clinical training | ||||||||||
| Medical doctor (MD, DO, MBBS) | 620 | 68.1 | 328 | 77.2 | 291 | 60.0 | 71 | 65.7 | 517 | 68.6 |
| Nurse | 32 | 3.5 | 3 | 0.7 | 29 | 6.0 | 5 | 4.6 | 27 | 3.6 |
| Psychologist | 24 | 2.5 | 7 | 1.7 | 17 | 3.5 | 5 | 4.6 | 17 | 2.3 |
| Pharmacist | 20 | 2.2 | 9 | 2.1 | 11 | 2.3 | 1 | 0.9 | 19 | 2.5 |
| Dentist | 9 | 1.0 | 1 | 0.2 | 8 | 1.7 | 3 | 2.8 | 6 | 0.8 |
| Occupational or physical therapist | 9 | 1.0 | 4 | 0.9 | 5 | 1.0 | 0 | 0.0 | 9 | 1.2 |
| Veterinarian | 5 | 0.5 | 2 | 0.5 | 3 | 0.6 | 1 | 0.9 | 4 | 0.5 |
| Social worker | 4 | 0.4 | 0 | 0.0 | 4 | 0.8 | 1 | 0.9 | 3 | 0.4 |
| Speech pathologist | 4 | 0.4 | 1 | 0.2 | 3 | 0.6 | 1 | 0.9 | 3 | 0.4 |
| Other clinical trainingc | 7 | 0.9 | 1 | 0.2 | 6 | 1.2 | 1 | 0.9 | 5 | 0.7 |
| Non-clinician PhD | 177 | 19.4 | 69 | 16.2 | 108 | 22.3 | 19 | 17.6 | 144 | 19.1 |
| PhD trainingd | ||||||||||
| No | 529 | 59.0 | 262 | 62.5 | 266 | 55.8 | 67 | 63.2 | 438 | 59.0 |
| Yes | 368 | 41.0 | 157 | 37.5 | 211 | 44.2 | 39 | 36.8 | 304 | 41.0 |
| Race | ||||||||||
| White | 593 | 68.7 | 290 | 71.8 | 302 | 65.9 | ||||
| Black or African American | 45 | 5.2 | 6 | 1.5 | 39 | 8.5 | ||||
| American Indian or Alaska Native | 2 | 0.2 | 1 | 0.3 | 1 | 0.2 | ||||
| Asian | 207 | 24.0 | 99 | 24.5 | 108 | 23.6 | ||||
| Native Hawaiian or Pacific Islander | 2 | 0.2 | 1 | 0.3 | 1 | 0.2 | ||||
| >1 race | 14 | 1.6 | 7 | 1.7 | 7 | 1.5 | ||||
| Ethnicity | ||||||||||
| Non-Hispanic | 809 | 93.4 | 381 | 94.1 | 427 | 92.8 | ||||
| Hispanic or Latino | 57 | 6.6 | 24 | 5.9 | 33 | 7.2 | ||||
Underrepresented in medicine (URM) includes Black or African American, American Indian or Alaska Native, Native Hawaiian or Pacific Islander, and Hispanic or Latino.
Cells may not add up to the total due to information not provided, including n=1 missing sex, n=3 missing clinical training, n=17 missing PhD training, n=51 missing race, and n=48 missing ethnicity.
Includes audiologist, music therapist, naturopathic doctor, nutritionist, and not specified.
Includes clinicians and non-clinicians. Yes indicates the individual had a PhD when she or he was appointed as a KL2 scholar.
Fifty-three percent of KL2 scholars (487/913) were female. A larger percentage of male scholars were medical doctors (77% vs. 60%), whereas a larger percentage of female scholars had other backgrounds (40% vs. 23%; P < .001). Male and female scholars also differed in their distribution of race and ethnicity, with a larger percentage of female than male scholars being from URM groups (16% vs. 8%; P < .001). (See Table 1 for complete data.)
URM individuals represented 12% of scholars (108/865). The distribution of clinician versus non-clinician trained URM scholars was very similar to that of non-URM scholars (see Table 1). By region of the United States, the percentage of KL2 scholars who were from URM groups was somewhat higher in the South compared to the other regions, although this difference did not reach statistical significance (data not shown).
Among the 582 scholars who had completed their KL2 training at the time of this study and for whom their status as currently engaged in research or not was known, 558 (96%) remained engaged in clinical or translational research. Those who remained engaged in research did not differ from those who did not in terms of the type of clinician or non-clinician training, sex, or URM status (data not shown).
More than one third of scholars who had completed their KL2 training had transitioned to an individual mentored CDA (225/579; 39%), and nearly half of scholars who had completed their KL2 training two or more years before this study met this criterion (182/398; 46%) (see Table 2 and Figure 1). One hundred and one former KL2 scholars (of 587; 17%) had been awarded an NIH independent research project grant, and 120 (of 533; 23%) had received a non-NIH independent research project grant. Some scholars received both, so the total number of former KL2 scholars who had received independent funding was 190 (of 548; 35%). When time since completing KL2 training was considered, the percentage of scholars with independent funding rose from 23% (40/171) of those within two years of completing their KL2 training to 40% (149/374) among those who were two or more years beyond completing their KL2 training. The cohort of former KL2 scholars included 71 scholars who had received an individual CDA then transitioned to an independent research award and 119 scholars who had received an independent award without a period of individual CDA support.
Table 2.
Type of External, Peer-Reviewed Research Funding Awarded to 601 Mentored Career Development Scholars After Completing the KL2 Program at 48 Clinical and Translational Science Award Institutions, 2007–2013a
| All scholars | Scholars who completed KL2 training 2+ years earlier |
|||
|---|---|---|---|---|
| Type of award | no. | % | no. | % |
| Total | 601 | 412 | ||
| Individual career development award (CDA)b | ||||
| No | 354 | 61.1 | 216 | 54.3 |
| Yes | 225 | 38.9 | 182 | 45.7 |
|
National Institutes of Health (NIH) R01 or equivalent independent awardc |
||||
| No | 486 | 82.8 | 319 | 79.2 |
| Yes | 101 | 17.2 | 84 | 20.8 |
| Non-NIH independent awardd | ||||
| No | 413 | 77.5 | 266 | 74.1 |
| Yes | 120 | 22.5 | 93 | 25.9 |
|
Type of award by CDA, independent award, or both |
||||
| None | 217 | 38.7 | 122 | 31.5 |
| Individual CDA | 154 | 27.5 | 116 | 30.0 |
| Individual CDA and NIH or non-NIH independent award |
71 | 12.7 | 66 | 17.1 |
| NIH or non-NIH independent award | 119 | 21.2 | 83 | 21.4 |
Cells may not add up to the total due to information not provided, including n = 22 missing CDA status, n = 14 missing R01 award status, and n = 68 missing non-NIH independent award status.
Defined as an individual peer-reviewed training award such as an NIH K23, NIH K08, or Veterans Health Administration CDA.
Defined as the principal investigator of an NIH R01 award or the principal investigator of a project within an NIH program project or center award (e.g., P01).
Defined as the principal investigator of an independent, externally-funded, non-NIH, peer-reviewed research project of 3 or more years duration (e.g., a Veterans Health Administration merit award or a foundation-funded research project award). Does not include mentored research or industry-funded trials.
Figure 1.
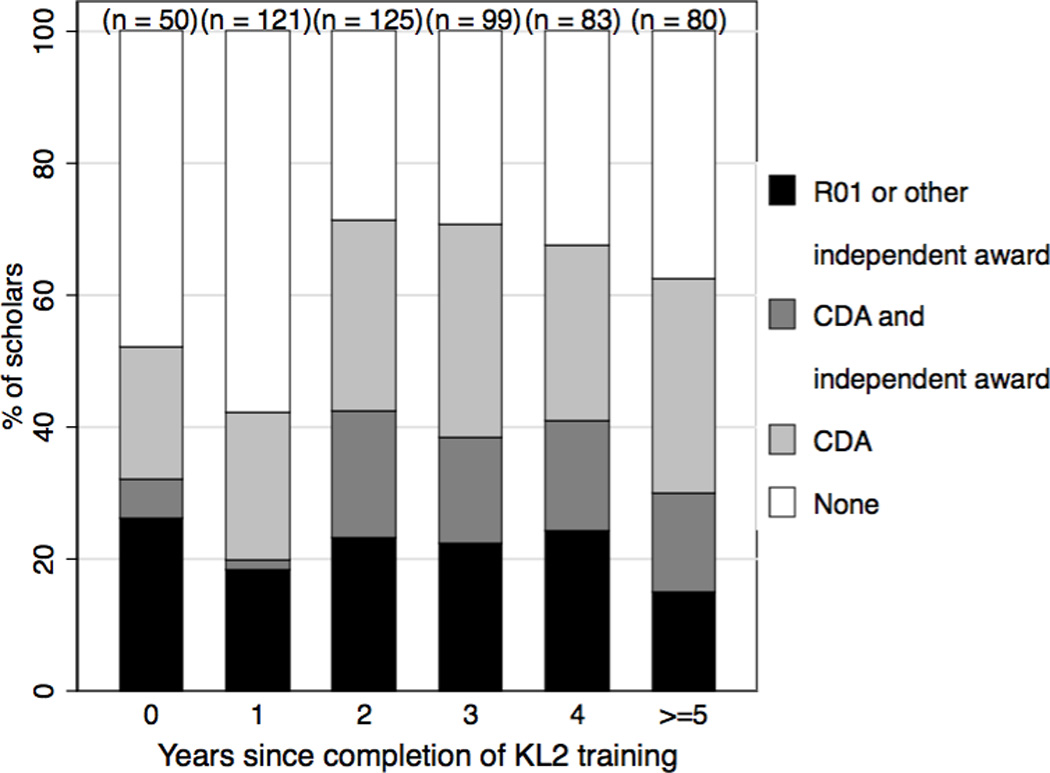
Grants awarded to mentored clinical and translational scholars who completed their KL2 training from 2007–2013, by year since completion of KL2 training. Based on data from 601 scholars; excluded are 40 scholars for whom incomplete grant information was reported and 3 scholars with missing data on the year of completion of KL2 training.
Compared to clinicians, non-clinicians differed somewhat in the types of grants they were awarded (see Figure 2). A larger percentage of non-clinician PhDs than of clinicians had received independent awards (42% vs. 32%), but a smaller percentage had received individual CDAs (33% vs. 42%). Non-clinicians more frequently transitioned directly from KL2 support to independent funding without a period of individual CDA support.
Figure 2.
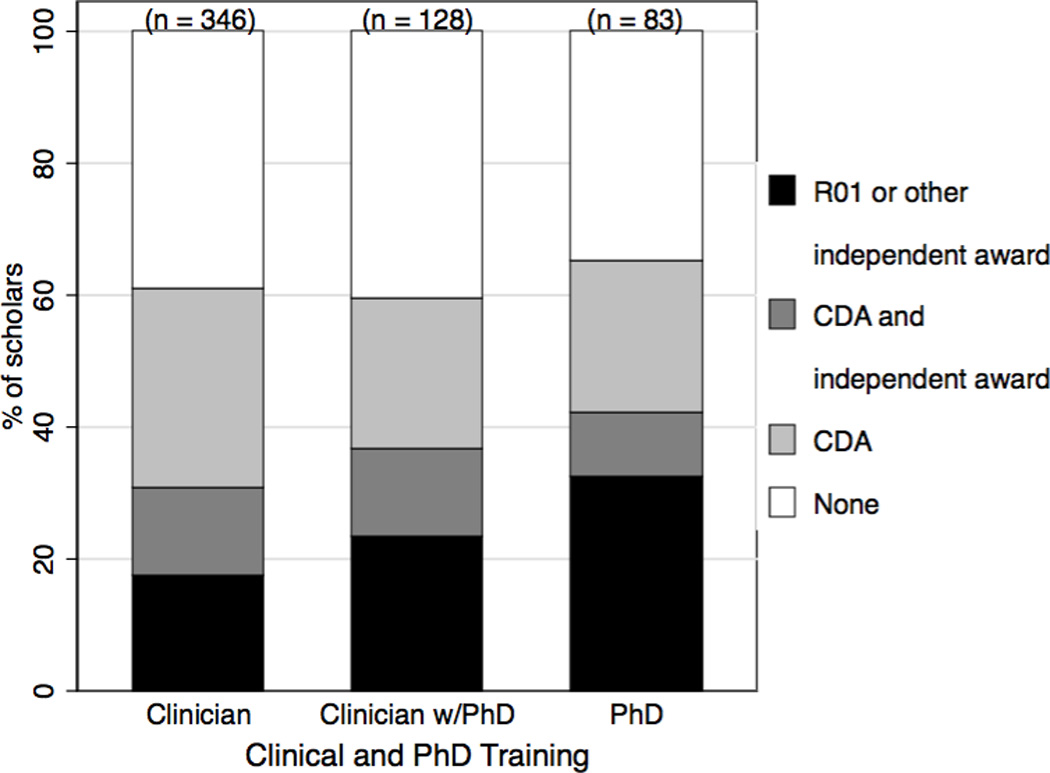
Grants awarded to mentored clinical and translational scholars who completed their KL2 training from 2007–2013, by type of previous clinical and/or PhD training. Based on data from 601 scholars; excluded are 40 scholars for whom incomplete grant information was reported and 4 scholars with missing data on previous clinical and/or PhD training.
In a multivariable analysis accounting for multiple scholar characteristics and for clustering by institution, the odds of non-clinician PhDs attaining independent funding were approximately twice those of clinicians doing so, whereas the difference between clinicians with and without a PhD was modest (see Table 3). Pursuing an advanced degree during KL2 training was not associated with obtaining independent research funding, and success did not differ significantly by sex or URM status. We also considered possible associations between characteristics of the institution and scholar success. The amount of NIH funding an institution received was not a predictor of an individual scholar’s success in transitioning to independent research funding (data not shown).
Table 3.
The Relationship between the Characteristics of Mentored Career Development (KL2) Scholars and Their Transition to Independent Research Funding
| Received an independent research award?a | Odds ratiob |
95% confidence interval |
||||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| Characteristic | no. | % | no. | % | ||
| Clinical and PhD trainingc | ||||||
| Clinician, no PhD | 233 | 65.4 | 106 | 56.4 | 1 | ref |
| Clinician with PhD | 76 | 21.3 | 47 | 25.0 | 1.17 | 0.69 – 1.96 |
| Non-clinician PhD | 47 | 13.2 | 35 | 18.6 | 2.05 | 1.11 – 3.78 |
| Pursued MS or PhD during KL2 training | ||||||
| No | 198 | 55.9 | 127 | 67.6 | 1 | ref |
| Yes | 156 | 44.1 | 61 | 32.4 | 0.83 | 0.49 – 1.41 |
| Sex | ||||||
| Male | 165 | 46.2 | 91 | 47.9 | 1 | ref |
| Female | 192 | 53.8 | 99 | 52.1 | 0.87 | 0.57 – 1.31 |
| URM statusd | ||||||
| Not URM | 305 | 86.2 | 167 | 90.8 | 1 | ref |
| URM | 49 | 13.8 | 17 | 9.2 | 0.81 | 0.42 – 1.58 |
| When completed KL2 training | ||||||
| Within the last 2 years | 131 | 36.8 | 40 | 21.2 | 1 | ref |
| 2–3 years earlier | 127 | 35.7 | 91 | 48.2 | 2.47 | 1.46 – 4.16 |
| 4+ years earlier | 98 | 27.5 | 58 | 30.7 | 2.51 | 1.40 – 4.51 |
Defined as the principal investigator (PI) of a National Institutes of Health (NIH) R01 award, PI of a project within an NIH program project or right award (e.g., P01), or PI of an independent, externally-funded, non-NIH, peer-reviewed research project of 3 or more years duration. Does not include mentored research awardsor industry-funded trials.
Odds ratios are from a mixed effects regression analysis, which treated the institution as a random effect and included all variables listed in this table as covariates.
Defined as training prior to appointment as a KL2 scholar.
Underrepresented in medicine (URM) includes Black or African American, American Indian or Alaska Native, Native Hawaiianor Pacific Islander, and Hispanic or Latino.
Discussion
In this study, approximately one-third of scholars within six years of completing their KL2 training had successfully transitioned to independence, as defined by being awarded independent research funding as a PI. This percentage was greater among scholars who had completed their KL2 training two or more years earlier than among scholars within two years of completing their training.
In contrast to some previous studies, in which research independence was defined according to one criterion, being awarded an NIH R01 grant, we expanded the criteria to include being awarded comparable grants from other sources. We found that more KL2 scholars received their first independent award from a non-NIH source than from NIH. A 2008 report, based on a study at a single large institution, also observed that clinical investigator trainees were more likely to obtain grants from non-NIH sources.16 Recognition of the need to consider the impact of biomedical research funding from non-governmental, not-for-profit organizations in addition to that from the government led to the initiation of the Grants in the Health Research Alliance Shared Portfolio.17 Such collaboration and data sharing between governmental and non-governmental research organizations in the future may contribute to improved understanding of research career development.
Although we found that the percentage of scholars with NIH independent research awards was less than 20% of those who had completed their KL2 training, we expect this percentage to increase over time. Many former KL2 scholars were participating in further mentored training under individual CDA mechanisms at the time this study was conducted and may continue on to pursue independent funding after their CDA is complete.
We found that scholars receiving a KL2 award included individuals from a range of clinical disciplines, including medicine, nursing, psychology, pharmacy, and others. Approximately one-fifth were translational science researchers with no clinical training. Female scholars were slightly more numerous than male scholars in the KL2 cohort. In contrast, male scholars represented 53% and 70% respectively of awardees receiving NIH individual K23 and K08 grants for the somewhat earlier period from 2000–2005.18 Female scholars have been underrepresented among physician-scientists,12 although the gap is closing.5
The percentage of KL2 scholars who were from URM groups (12%) was essentially identical to the percentage of URM physicians reported in the U.S. physician workforce19 and was greater than the percentage of URM faculty at U.S. medical schools (7.1%).20 Among U.S. medical school faculty with a rank comparable to KL2 scholars (i.e., instructors and assistant professors), the percentage of physicians from URM groups is estimated to be 8.4%. The percentages of African-Americans (5.2%) and Hispanics (6.6%) in the KL2 scholar population are slightly higher than the percentages reported for those groups in the NIH physician-scientist research project grant applicant pool (2.4% and 4.5%, respectively).5
The CTSA program’s emphasis on diversity and on participation by underrepresented groups8 may contribute to the greater representation of women and URM researchers we observed among KL2 scholars. In addition, the processes for recruiting and selecting KL2 awardees from within an institution, in contrast to the processes for awarding individual NIH career development grants for which an individual’s application is peer-reviewed by an external panel, may support identifying qualified individuals who are members of underrepresented groups.
We found that male and female KL2 scholars were similar in their success in attaining independent funding and that URM individuals and their non-URM colleagues also had similar success rates. These findings are in contrast to those of prior studies, which reported that, NIH-wide, female and URM recipients of individual K awards had lower likelihoods of applying for and obtaining R01 awards compared to their male and non-URM counterparts.11–14 Our findings may reflect continued progress over time for female and URM researchers in clinical and translational science. However, we also saw differences in our findings relative to 2012 data from the Physician-Scientist Workforce Working Group, which found persistent disparities, including by sex and race/ethnicity, among physician-scientist grant awardees.5 The institutional KL2 selection process can take into account firsthand knowledge of the applicant and his or her mentor and fit between the applicant’s interests and institutional strengths. This process may support female and URM scholars in the transition to independence. Prior research indicates that mentoring and career development support play a role in the success of female and URM scholars.21,22 The integrated mentoring and support provided to KL2 scholars through the CTSA core resources may play a role in the success of female and URM awardees compared to individual CDA mechanisms. We cannot rule out that characteristics of the institutions with CTSAs in general, rather than those of the KL2 programs specifically, also may contribute to the greater success of female and URM applicants in attaining independent funding.
The pattern of transition to independent research funding for many individuals from clinical disciplines was to first obtain an individual CDA following the period of KL2 support, whereas non-clinician PhDs more often obtained independent funding directly following the period of KL2 support without a period of individual CDA support. Individuals with non-clinician PhDs likely have devoted more years to research training prior to participating in the KL2 program. While having a PhD degree at the time of KL2 appointment was positively associated with success attaining independent funding (significantly for non-clinicians, non-significantly for clinicians), we detected no significant association between pursuing a clinical research MS or PhD degree during KL2 training and the subsequent transition to independent research funding. Many scholars already have advanced degrees at the time of their appointment to the KL2 program and may not need further didactic research training. The absence of an association between pursuing an MS or PhD degree and success attaining independent funding may reflect a selection process; scholars who are identified as needing additional didactic training are directed to pursue a clinical research MS or PhD degree during their KL2 support period, whereas those with adequate preparation prior to KL2 appointment do not pursue an additional formal degree.
Of concern is the lower success rate for clinician scholars relative to non-clinician PhDs in achieving independent funding. Clinicians without PhDs are likely to have no more than one or two years of research experience before their appointment as K scholars, whereas non-clinician PhDs have at least four years of pre-doctoral mentored research and several years of post-doctoral research experience. It has been proposed that NIH consider a longer mentored program that would combine three years of KL2-equivalent training with five years of K08/K23-equivalent training to fully prepare clinician scholars for independent funding.23
Also of note is our finding that more than 95% of the individuals who had completed their KL2 training were described as currently engaged in research. Participation in team science, holding roles other than PI, is increasingly recognized as making a significant contribution in clinical research,3,24 and our data are consistent with former KL2 scholars taking on these roles.
With a high survey response rate, we were able to present a fairly complete and representative description of the cohort of scholars appointed in the first six years of the CTSA KL2 Mentored Career Development program. In designing this study, we considered that survey length adds to respondent burden and potentially affects response rates.25 We therefore elected to limit the number of survey items used to describe each scholar. A resulting limitation is that the data we collected did not include full career details nor grant award details for each scholar. Further, we did not obtain data on team science metrics, such as participation as a co-investigator on grants or publications. We also did not assess the different processes each institution used to select scholars. We relied on research education and career development faculty leaders to accurately report their scholars’ progress during their post-award period. Each CTSA institution is responsible for tracking KL2 scholars’ outcomes and for reporting them to the funding agency. Thus, respondents to our survey likely were able to refer to those tracking data to complete the survey. We used several strategies to maximize the quality of our data, including providing a form respondents could use to compile responses offline and carefully wording and beta-testing the survey. Nonetheless, we acknowledge that respondent errors in reporting may be present. No other existing cross-institutional data was available to validate responses.
It should be noted that due to the survey structure, the metrics of success we used to denote independent funding differed somewhat from the “award rate” and “success rate” data provided in NIH reports.18 We obtained information regarding whether each scholar had received an award but not whether she or he had applied for an award but was unsuccessful.
In conclusion, the CTSA KL2 award program supports the transition to independent research funding for physician-scientists, other clinician-scientists, and non-clinician PhDs interested in clinical and translational research. Female and URM scholars are well represented in this program and have similar success as male and non-URM scholars in the transition to independence. Many KL2 scholars first attain independent funding from non-NIH sources, so future research on the transition to independent funding should capture multiple sources.
Acknowledgments
The authors acknowledge Maureen Goode, PhD, Center for Clinical and Translational Science, University of Texas Health Science Center at Houston, Jennifer D. Kusch, PhD, Medical College of Wisconsin, and Jasjit Ahluwalla, MD, MPH, University of Minnesota School of Public Health who provided useful feedback on the survey draft.
Funding/Support: Support from the National Center for Advancing Translational Sciences-sponsored Clinical and Translational Science Award program to the following institutions supported this work: University of Texas Southwestern Center for Translational Medicine (UL1TR000451), Icahn School of Medicine at Mount Sinai (UL1TR000067-05S1), Utah Center for Clinical and Translational Science (ULTR001067), Clinical and Translational Science Institute at Children's National/George Washington (UL1TR000075), and the Vanderbilt Institute for Clinical Translational Research (UL1TR000445). The contents of this report are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health. REDCap electronic research tools were provided by the Vanderbilt Institute for Clinical Translational Research (UL1TR000445).
Footnotes
Other disclosures: None reported.
Ethical approval: The institutional review boards at the University of Utah Health Sciences Centers and Icahn School of Medicine at Mount Sinai determined this study to be non-human subjects research.
Previous presentations: A portion of the results reported here were presented in the form of a poster at the 2014 meeting of the Association for Clinical and Translational Science (Washington, DC; April 2014).
Contributor Information
Carol Sweeney, Department of Internal Medicine, and Center for Clinical & Translational Science, University of Utah Health Sciences Center, Salt Lake City, Utah.
Lisa S. Schwartz, Department of Clinical Research and Leadership, George Washington University School of Medicine and Health Sciences, Washington, DC.
Robert Toto, Department of Internal Medicine, associate dean for clinical and translational research, and director, The Center for Translational Medicine, University of Texas Southwestern Medical Center, Dallas, Texas.
Carol Merchant, Extramural Career Development Programs, National Center for Advancing Translational Sciences, National Institutes of Health, Bethesda, Maryland.
Alecia S. Fair, Vanderbilt Institute for Clinical and Translational Research, Vanderbilt University Medical Center, Nashville, Tennessee.
Janice L. Gabrilove, James F. Holland Professor of Medicine and Oncological Sciences, associate director for education and training, Tisch Cancer Institute, and director, Clinical Research Education Programs, Icahn School of Medicine at Mount Sinai & Graduate School of Biomedical Sciences, New York, New York.
References
- 1.Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med. 1979;301:1254–1259. doi: 10.1056/NEJM197912063012303. [DOI] [PubMed] [Google Scholar]
- 2.Schafer AI. The vanishing physician-scientist? Transl Res. 2010;155:1–2. doi: 10.1016/j.trsl.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meyers FJ, Begg MD, Fleming M, Merchant C. Strengthening the career development of clinical translational scientist trainees: A consensus statement of the Clinical Translational Science Award (CTSA) Research Education and Career Development Committees. Clin Transl Sci. 2012;5:132–137. doi: 10.1111/j.1752-8062.2011.00392.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: Continuing challenges in the 21st century. FASEB J. 2014;28:1049–1058. doi: 10.1096/fj.13-241687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institutes of Health. Physician-Scientist Workforce Working Group Report. Bethesda, MD: National Institutes of Health; 2014. Office of Extramural Research. [Google Scholar]
- 6.Yin HL, Gabrilove J, Jackson R, Sweeney C, Fair AM, Toto R. Sustaining the clinical and translational research workforce: Training and empowering the next generation of investigators. Acad Med. 2015;90:861–865. doi: 10.1097/ACM.0000000000000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine. The CTSA Program at NIH: Opportunities for Advancing Clinical and Translational Research. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 8.National Center for Advancing Translational Sciences. Clinical and Translational Science Award (U54). RFA-TR-14-009. [Accessed August 29, 2016];Overview Information. 2009 http://grants.nih.gov/grants/guide/rfa-files/RFA-TR-14-009.html.
- 9.Byington CL, Higgins S, Kaskel FJ, Purucker M, Davis JM, Smoyer WE. The CTSA mentored career development program: Supporting the careers of child health investigators. Clin Transl Sci. 2014;7:44–47. doi: 10.1111/cts.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miyaoka A, Spiegelman M, Rau K, Frechtling J. Findings from the CTSA National Evaluation Education and Training Study. Rockville, MD: Westat; 2011. [Google Scholar]
- 11.Jagsi R, DeCastro R, Griffith KA, et al. Similarities and differences in the career trajectories of male and female career development award recipients. Acad Med. 2011;86:1415–1421. doi: 10.1097/ACM.0b013e3182305aa6. [DOI] [PubMed] [Google Scholar]
- 12.Jagsi R, Motomura AR, Griffith KA, Rangarajan S, Ubel PA. Sex differences in attainment of independent funding by career development awardees. Ann Intern Med. 2009;151:804–811. doi: 10.7326/0003-4819-151-11-200912010-00009. [DOI] [PubMed] [Google Scholar]
- 13.Pohlhaus JR, Jiang H, Wagner RM, Schaffer WT, Pinn VW. Sex differences in application, success, and funding rates for NIH extramural programs. Acad Med. 2011;86:759–767. doi: 10.1097/ACM.0b013e31821836ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pohlhaus JR, Jiang H, Sutton J. Sex differences in career development awardees’ subsequent grant attainment. Ann Intern Med. 2010;152:616–617. doi: 10.7326/0003-4819-152-9-201005040-00019. author reply 617. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dyrbye LN, Lindor KD, LaRusso NF, Cook DA. Research productivity of graduates from 3 physician-scientist training programs. Am J Med. 2008;121:1107–1113. doi: 10.1016/j.amjmed.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 17.Myers ER, Alciati MH, Ahlport KN, Sung NS. Similarities and differences in philanthropic and federal support for medical research in the United States: An analysis of funding by nonprofits in 2006–2008. Acad Med. 2012;87:1574–1581. doi: 10.1097/ACM.0b013e31826762f4. [DOI] [PubMed] [Google Scholar]
- 18.National Institutes of Health Individual Mentored Career Development Awards Program Evaluation Working Group. Bethesda, MD: National Institutes of Health; 2011. National Institutes of Health Individual Mentored Career Development Awards Program. http://grants.nih.gov/training/K_Awards_Evaluation_FinalReport_20110901.pdf. [Google Scholar]
- 19.Association of American Medical Colleges. Facts and Figures 2010. Washington, DC: Association of American Medical Colleges; 2010. Diversity in the Physician Workforce. [Google Scholar]
- 20.Association of American Medical Colleges. Diversity in Medical Education: Facts & Figures 2012. Washington, DC: Association of American Medical Colleges; 2012. [Google Scholar]
- 21.Daley S, Wingard DL, Reznik V. Improving the retention of underrepresented minority faculty in academic medicine. J Natl Med Assoc. 2006;98:1435–1440. [PMC free article] [PubMed] [Google Scholar]
- 22.Wingard DL, Reznik VM, Daley SP. Career experiences and perceptions of underrepresented minority medical school faculty. J Natl Med Assoc. 2008;100:1084–1087. doi: 10.1016/s0027-9684(15)31449-8. [DOI] [PubMed] [Google Scholar]
- 23.Hoots WK, Abkowitz JL, Coller BS, DiMichele DM. Planning for the future workforce in hematology research. Blood. 2015;125:2745–2752. doi: 10.1182/blood-2015-01-617811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Begg MD, Crumley G, Fair AM, et al. Approaches to preparing young scholars for careers in interdisciplinary team science. J Investig Med. 2014;62:14–25. doi: 10.231/JIM.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edwards PJ, Roberts I, Clarke MJ, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009;(3) doi: 10.1002/14651858.MR000008.pub4. MR000008. [DOI] [PMC free article] [PubMed] [Google Scholar]


