Abstract
Objective
To examine whether baseline chronic stress, morning cortisol, and other appetite-related hormones (leptin, ghrelin, and insulin) predict future weight gain and food cravings in a naturalistic longitudinal 6-month follow-up study.
Methods
A prospective community cohort of three hundred and thirty-nine adults (age=29.1± 9.0 years; BMI=26.7±5.4 kg/m2; 56.9% female; 70.2% White) completed assessments at baseline and 6-month follow-up. Fasting blood draws were used to assess cortisol and other appetite-related hormones levels at baseline. At baseline and follow-up, body weight was measured and the Cumulative Adversity Interview and Food Craving Inventory were administered. Data were analyzed using linear mixed models adjusting for demographic and clinical covariates.
Results
Over the 6-month period, 49.9% of the sample gained weight. Food cravings and chronic stress decreased over 6 months (ps<0.05). However, after adjusting for covariates, individuals with higher baseline total ghrelin had significantly higher food cravings at 6 months (p=0.04). Furthermore, higher cortisol, insulin, and chronic stress were each predictive of greater future weight gain (ps<0.05).
Conclusions
These results suggest that ghrelin plays a role in increased food cravings and reward-driven eating behaviors. Studies are needed that examine the utility of stress reduction methods for normalizing disrupted cortisol responses and preventing future weight gain.
Keywords: Stress, food cravings, ghrelin, leptin, weight
Introduction
Energy intake and weight regulation in the modern food environment is challenging. In the United States, the prevalence of obesity is 37.7%.1 On average, American adults gain 0.2 to 0.9 kg each year.2,3 Energy and weight regulation involves complex homeostatic and non-homeostatic mechanisms including central regulatory systems, peripheral feedback from adipose and the gastrointestinal tract, and psychological factors.4 Among these mechanisms, stress, cortisol, and orexigenic and anorexigenic metabolic hormones have been identified as possible clinical targets. However, few studies have prospectively examined how these factors are related to weight gain.
Stress, a real or perceived disruption in homeostasis, influences eating behaviors and food choices. The effects of stress differ based on the type and duration of stressor. During acute stress, appetite is typically suppressed.5 Chronic stress generally promotes wanting, seeking, and intake of palatable high-fat and energy-dense foods.6 Stress, particularly chronic stress, has been linked with obesity and weight gain in several but not all studies.7,8 The effects of chronic stress on food intake and weight may be related to perturbations in the hypothalamic-pituitary-adrenal (HPA) axis. HPA axis activation results in secretion of cortisol, a glucocorticoid that stimulates appetite and increases intake of highly palatable foods.9 However, results of the relationship between cortisol and weight status are inconsistent and largely rely on cross-sectional data.
Other hormones such as ghrelin, leptin, and insulin communicate with the central nervous system (CNS) to signal information about energy homeostasis, though the precise role each of these hormones has in relation to weight changes is unclear. Ghrelin is secreted from the stomach as well as peripheral tissues and stimulates appetite and food intake.10 Cross-sectional analyses have demonstrated that obese individuals have lower fasting ghrelin levels and attenuated postprandial ghrelin suppression,11 though central and peripheral administration of ghrelin result in weight gain in pre-clinical models.12 Insulin and leptin are adiposity signals.13 The beta cells of the pancreas produce insulin to utilize glucose in peripheral tissues of the body. Leptin is an adipokine made in adipocytes and is involved in satiety signaling. Leptin and insulin levels are increased in individuals who are overweight/obese compared to individuals who are normal weight, but despite higher levels resistance to insulin, and possibly leptin, may contribute to dysregulation of hunger/satiety signaling and thus affect eating behavior. Little is known about the interactions between stress and appetite-related hormones, though it has been hypothesized that the effects of cortisol and stress may potentiate the rewarding value of food and increase food cravings, similar to the effects of stress on cravings in substance use disorders.
Craving, a strong desire or sense of compulsion to take a substance, is a central feature of addictions and has been added into the Diagnostic and Statistical Manual of Mental Disorders-5 criteria for substance use disorders. Stress and cortisol increase addiction vulnerability and are associated with cravings among individuals with drug and alcohol addictions. Chronic substance use results in neuroadaptations in brain reward and also stress pathways, including the HPA axis, that in turn contribute to increased cravings, drug intake and alteration of the reinforcing effects of substances.14,15 Brain reward pathways are involved in the reinforcing effects of drugs of abuse and also rewarding foods, however, the associations between stress, cortisol, appetitive hormones and food cravings are unclear.
Food cravings are an intense desire to consume a specific food or food type that is difficult to resist.16 Food cravings are common, with the majority of the population having experienced a food craving at some point. While all food cravings are not pathological, frequent food cravings are associated with greater intake of the respective craved foods and increased body mass index (BMI).17,18 We previously reported in a cross-sectional analysis that chronic psychosocial stress was associated with increased food cravings and BMI.19 In the present study, we report findings from the prospective 6-month follow-up data from a subsample of these participants who were followed longitudinally. Our aim was to examine whether higher chronic stress, cortisol, and circulating appetite-related hormones (ghrelin, leptin, and insulin) were predictive of future food cravings and weight 6-months later. We hypothesized that individuals with higher baseline cortisol, chronic stress, and appetite-related hormones would have more frequent food cravings and greater weight gain at follow-up.
Methods
Participants
This study reports on 6-month longitudinal changes in weight from a community cohort who participated in studies that examined the mechanisms underlying stress, self-control, and addictive behaviors.19 The longitudinal component was added in the third year of data collection and thus was available on a subsample of 339 participants who completed initial baseline measures and also attended a 6-month follow-up assessment. Participant inclusion criteria were age between 18 and 50 years, and able to read English at the sixth-grade level. Exclusion criteria were pregnancy, dependence on drugs other than nicotine, use of prescribed medications for any psychiatric disorders, and serious and chronic medical conditions.
Procedures
The Yale University Institutional Review Board approved the study. Study procedures were performed at the Yale Stress Center. Potential participants completed an initial screening over the telephone or in-person to determine eligibility. Following screening, eligible participants met with a research assistant for a 2-hour intake session to obtain informed consent and begin assessments. Participants had a morning biochemical evaluation session after fasting overnight. They also completed psychological measures and self-report questionnaires over three to four additional sessions. Participants attended a follow-up visit six months after their initial visit where weight was measured and assessments were completed. Participants were compensated for study participation.
Demographics/BMI
Demographics including age, sex, smoking status and race/ethnicity were collected via a questionnaire designed for this study. A research nurse or trained research staff member measured participant’s weight at baseline and follow-up. These weights and measured heights were used to calculate BMI.
Chronic stress
Chronic stress was assessed using the chronic stress subscale of the Cumulative Adversity Interview administered at baseline and 6 months.20 The Cumulative Adversity Interview is a well-established, 140-item interview that assessed for the accumulation of stressful life events. The chronic stress subscale consisted of 62 items relating to the subjective experience of continuous stressors or ongoing life problems and hassles. Items were rated as not true, some to very true and referred to perceived difficulties with ongoing interpersonal, social, and financial relationships and responsibilities including difficulties in the work and home environment and relationships with family and significant others. The Cumulative Adversity Interview and its chronic stress subscale has excellent reliability ranging from an overall 0.86 and 0.82 for the chronic stress subscale.21
Food cravings
Food cravings were assessed at baseline and follow-up using the Food Craving Inventory (FCI), a 28-item measure of general and specific food cravings over the past month.22 The instrument defined craving as “an intense desire to consume a particular food (or food type) that is difficult to resist.” Participants rated how often each food was craved on a 5- point Likert scale ranging from 1 (never) to 5 (always/almost every day). Items were formed into a total score and 4 subscale scores: sweets, high fats, carbohydrates/starches and fast-food fats. The FCI has established content validity and reliability for assessing food cravings in adults.22
Biochemical evaluation
On a separate day from intake and baseline assessments and after overnight fasting, participants came to the laboratory at 7:30 AM, at which time an intravenous line was inserted and 4 repeated samples of cortisol were drawn 15 minutes apart over the course of 1 hour and then averaged across time points. In addition, circulating plasma total ghrelin, leptin, insulin, and plasma glucose levels were drawn once and tested in duplicate. All samples were immediately placed on ice, spun, and separated by centrifugation. Separated plasma was stored at −80°C. The homeostatic model assessment of insulin resistance (HOMAIR) was used as a surrogate measure for insulin resistance and calculated as [glucose (mg/dL) × insulin (µU/mL)]/405. Total ghrelin was measured because we were assessing basal levels and not hormonal response to short term manipulations of food intake or hunger.
Data Analysis
Descriptive statistics were computed using means, standard deviations and percentages. We calculated full and partial correlations (adjusting for baseline BMI) to examine the cross-sectional relationships among variables. We also assessed baseline relationships among morning levels of cortisol, ghrelin, leptin, insulin, and chronic stress and baseline values of our two primary outcomes (weight and food cravings). These analyses were conducted using general linear models adjusting for demographic factors (age, years of education, smoking status, sex, race/ethnicity). Models examining food cravings included baseline BMI.
Paired t-tests were used to assess changes in food cravings, BMI, and chronic stress over 6 months. Morning cortisol levels, ghrelin, leptin, insulin and chronic stress were used to predict changes in weight and the frequency of food cravings over the 6-month period. Longitudinal analyses were conducted using linear mixed-effects models. For analyses predicting weight change, covariates included baseline demographic factors and baseline weight. In analyses predicting changes in food cravings, covariates included demographic factors, baseline BMI, and baseline food cravings. Continuous variables were centered in models. Chronic stress was examined as a time-varying predictor while all other dependent variables were time-invariant. Post-hoc models were constructed to assess changes in specific types of food cravings using subscale scores from the FCI. Analyses were conducted using SPSS version 24 and a two-tailed significance level set at p<0.05.
Results
Cross-Sectional Analyses
Three hundred and thirty-nine adults completed the baseline and follow-up assessment. Sample characteristics are presented in Table 1. The sample had a mean age of 29.1±9.0 years and BMI of 26.7±5.4 kg/m2. On average, participants had 15.3±2.5 years of education. A little more than half of the sample (56.9%) was female. The majority of the sample (70.2%) identified as White. Current smokers comprised 27.4% of the sample. Males were heavier than females (p<0.001; Table 1). Males had significantly higher glucose (p=0.008) and cravings for high fats (p=0.02). Females had significantly higher baseline ghrelin (p=0.02), leptin (p<0.001), cortisol (p<0.001), chronic stress (p=0.003) and cravings for sweets (p=0.001).
Table 1.
Baseline descriptive characteristics and 6-month change scores in total sample and by sex (Mean(SD) or N(%))
| Total (N=339) | Male (n=146) | Female (n=193) | P-value | ||
|---|---|---|---|---|---|
| Age (years) | 29.09(8.97) | 28.57(8.04) | 29.48(9.60) | 0.34 | |
| Education (years) | 15.28(2.48) | 15.29(2.50) | 15.26(2.50) | 0.92 | |
| Race | White, Non-Hispanic | 238(70.2) | 108(74.5) | 130(67.4) | 0.14 |
| Black | 67(19.8) | 28(19.3) | 39(20.2) | ||
| Other | 34(10.0) | 9(6.2) | 24(12.4) | ||
| Current smokers | 93(27.4) | 46(33.6) | 47(26.6) | 0.18 | |
| Ghrelin (pg/mL) | 793.15(249.05) | 755.68(202.26) | 821.88(278.24) | 0.02 | |
| Leptin (ng/mL) | 13.15(11.29) | 6.36(6.44) | 18.23(11.54) | <0.001 | |
| Insulin (µU/mL) | 13.04(6.78) | 12.96(6.33) | 13.10(7.15) | 0.86 | |
| Glucose (mg/dL) | 92.58(8.82) | 94.10(7.54) | 91.38(9.37) | 0.008 | |
| HOMA-IR | 3.03(1.73) | 3.06(1.63) | 3.01(1.82) | 0.79 | |
| Cortisol (mcg/dL) | 17.03(8.87) | 15.01(4.60) | 18.85(10.06) | <0.001 | |
| Weight (kg) | 77.55(18.65) | 86.11(18.41) | 71.02(16.12) | <0.001 | |
| Δ Weight (kg)* | 0.82(4.23) | 1.12(4.28) | 0.61(4.18) | 0.29 | |
| BMI (kg/m2) | 26.65(5.37) | 27.13(5.28) | 26.28(5.42) | 0.15 | |
| Δ BMI (kg/m2)* | 0.18(1.50) | 0.22(1.39) | 0.15(1.58) | 0.72 | |
| Food | Total | 1.95(0.60) | 1.93(0.61) | 1.98(0.59) | 0.48 |
| cravings | Δ Total** | −0.15(0.50) | −0.15(0.53) | −0.14(0.48) | 0.94 |
| High fats | 1.67(0.66) | 1.77(0.70) | 1.59(0.63) | 0.02 | |
| Δ High fats** | −0.10(0.50) | −0.12(0.51) | −0.09(0.49) | 0.61 | |
| Sweets | 2.14(0.77) | 1.97(0.75) | 2.26(0.76) | 0.001 | |
| Δ Sweets** | −0.19(0.65) | −0.15(0.66) | −0.21(0.64) | 0.47 | |
| Carbs/starches | 1.89(0.70) | 1.86(0.70) | 1.92(0.71) | 0.47 | |
| Δ Carbs/starches** | −0.13(0.61) | −0.15(0.65) | −0.13(0.59) | 0.76 | |
| Fast-food fats | 2.28(0.77) | 2.28(0.75) | 2.28(0.79) | 0.95 | |
| Δ Fast-food fats** | −0.15(0.66) | −0.15(0.68) | −0.15(0.65) | 0.98 | |
| Chronic stress | 10.17(5.91) | 9.10(5.22) | 10.96(6.31) | 0.003 | |
| Δ Chronic stress** | −1.02(4.43) | −0.15(−0.60) | −0.11(0.48) | 0.54 | |
Note. For change scores, negative values indicate decreases from baseline to follow-up.
P<0.01 or
p<0.001 for paired t-tests comparing baseline to follow-up scores.
Full and partial correlations (adjusting for BMI) are shown in Table 2. Baseline BMI was significantly positively correlated with chronic stress (r=0.18, p=0.001), total and specific food cravings (r=0.16 to 0.24, ps<0.05), leptin (r=0.55, p<0.001), insulin (r=0.48, p<0.001), fasting plasma glucose (r=0.30, p<0.001), and HOMA-IR (r=0.49, p<0.001). BMI was inversely associated with fasting total ghrelin (r= −0.18, p=0.002) and morning cortisol (r= −0.29, p<0.001). In unadjusted analyses, total food cravings were positively associated with leptin (r=0.18, p=0.002), insulin (r=0.26, p<0.001), glucose (r=0.16, p=0.008), and HOMA-IR (r=0.26, p<0.001). Morning cortisol was inversely associated with chronic stress (r= −0.14, p=0.01), cravings for high-fat foods (r= −0.12, p=0.04), leptin (r= −0.14, p=0.02), insulin (r= −0.12, p=0.048) and HOMA-IR (r= −0.12, p=0.04) in unadjusted correlations. Leptin was positively associated with total food cravings (r=0.19, p=0.002) and insulin (r=0.41, p<0.001). Ghrelin was not associated with food cravings in cross-sectional analyses (ps>0.05).
Table 2.
Cross-sectional full and partial correlations (adjusting for BMI) among study variables (N=339)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. BMI | --- | ||||||||||||
| 2. Chronic stress | 0.18* | --- | 0.22** | 0.13* | 0.30** | 0.12 | 0.17* | −0.02 | 0.19* | −0.01 | 0.02 | 0.00 | −0.07 |
| 3. Food cravings-Total | 0.24** | 0.25** | --- | 0.80** | 0.81** | 0.87** | 0.82** | 0.04 | 0.04 | 0.14* | 0.09 | 0.14* | 0.05 |
| 4. Food cravings-High fats | 0.22** | 0.16* | 0.82** | --- | 0.42** | 0.63** | 0.64** | 0.01 | −0.06 | 0.12* | 0.13* | 0.14* | −0.06 |
| 5. Food cravings-Sweets | 0.21** | 0.31** | 0.82** | 0.46** | --- | 0.58** | 0.57** | 0.08 | 0.11 | 0.09 | 0.01 | 0.09 | 0.09 |
| 6. Food cravings-Carbs/starches | 0.20** | 0.17* | 0.88** | 0.63** | 0.61** | --- | 0.63** | 0.00 | 0.05 | 0.12* | 0.06 | 0.12** | 0.11 |
| 7. Food cravings-Fast-food fats | 0.16* | 0.19** | 0.83** | 0.67** | 0.59** | 0.65** | --- | 0.07 | 0.01 | 0.12* | 0.13* | 0.14* | 0.02 |
| 8. Ghrelin | −0.18* | −0.03 | −0.03 | −0.06 | 0.01 | −0.04 | 0.02 | --- | 0.06 | −0.10 | −0.01 | −0.09 | 0.07 |
| 9. Leptin | 0.55** | 0.25** | 0.18* | 0.09 | 0.22** | 0.17* | 0.11 | −0.04 | --- | 0.24** | −0.10 | 0.20** | 0.01 |
| 10. Insulin | 0.48** | 0.08 | 0.26** | 0.24** | 0.19* | 0.22** | 0.20* | −0.18* | 0.41** | --- | 0.20* | 0.98** | 0.03 |
| 11. Glucose | 0.30** | 0.04 | 0.16* | 0.20* | 0.08 | 0.12 | 0.16* | −0.08 | 0.08 | 0.33** | --- | 0.38** | −0.01 |
| 12. HOMA-IR | 0.49** | 0.08 | 0.26** | 0.25** | 0.19* | 0.22** | 0.21** | −0.18* | 0.39** | 0.98** | 0.48** | --- | 0.03 |
| 13. Cortisol | −0.29** | −0.14* | −0.04 | −0.12* | −0.01 | 0.03 | −0.03 | 0.11 | −0.14* | −0.12* | −0.08 | −0.12* | --- |
Note. Full correlations are shown in the lower left corner. Partial correlations, adjusting for BMI, are displayed in the upper right corner.
p<0.05;
p<0.001.
In cross-sectional analyses, adjusting for demographic characteristics, BMI was positively associated with leptin (B=0.34, SE=0.03, p<0.001) and insulin (B=0.10, SE=0.04, p=0.01) and was negatively associated with ghrelin (B= −0.003, SE= 0.001, p=0.01). Cortisol and chronic stress were not significantly associated with weight in the cross-sectional model (ps>0.05). Insulin was replaced with HOMA-IR and was also significant (B=0.39, SE=0.15, p=0.01). In models examining food cravings, there were significant relationships with chronic stress (B=0.22, SE=0.06, p<0.001) and HOMA-IR (B=0.05, SE=0.02, p=0.048). Ghrelin, leptin, insulin, and cortisol were not significant (ps>0.05).
Prospective Longitudinal Analyses of 6-month Food Craving and Weight Outcomes
Food cravings
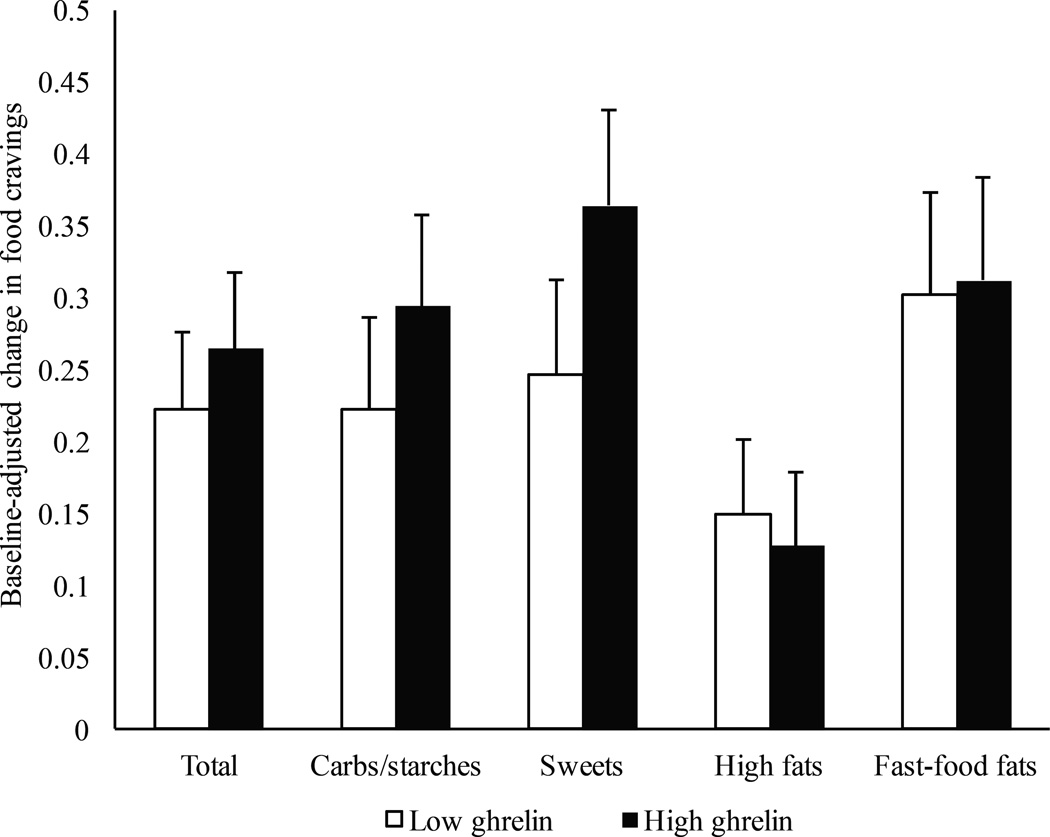
Total and specific food cravings and chronic stress significantly decreased from baseline to follow-up (ps<0.001; Table 1). After adjusting for demographic and baseline BMI and food cravings, higher baseline levels of total ghrelin predicted having higher total food cravings over 6 months (p=0.04; Table 3 and Figure 1). Cortisol (p=0.09) leptin (p=0.06), insulin (p=0.85), and chronic stress (p=0.17) did not predict change in food cravings over time (Table 3). Total food craving at 6 months was positively correlated with BMI at 6 months (r=0.14, p=0.02). However, neither baseline food craving nor change in food cravings was associated with weight change (ps=0.63, 0.69, respectively).
Table 3.
Linear mixed-effects models estimating change in food cravings and weight over 6 months (N=339)
| Food cravingsa | Weight (kgs)b | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | High fats | Sweets | Carbs/starches | Fast-food fats | ||||||||||||||
| Predictor | Estimate | SE | P | Estimate | SE | P | Estimate | SE | P | Estimate | SE | P | Estimate | SE | P | Estimate | SE | P |
| Cortisol | −0.005 | 0.003 | 0.093 | −0.003 | 0.003 | 0.374 | −0.002 | 0.004 | 0.557 | −0.009 | 0.003 | 0.013 | −0.008 | 0.004 | 0.049 | 0.056 | 0.024 | 0.024 |
| Ghrelin | 0.001 | 0.0001 | 0.038 | 0.0001 | 0.0001 | 0.399 | 0.002 | 0.001 | 0.053 | 0.001 | 0.001 | 0.002 | 0.001 | 0.001 | 0.303 | 0.001 | 0.001 | 0.322 |
| Leptin | −0.005 | 0.002 | 0.061 | −0.003 | 0.002 | 0.210 | −0.006 | 0.003 | 0.056 | −0.007 | 0.003 | 0.020 | −0.001 | 0.003 | 0.879 | −0.031 | 0.021 | 0.142 |
| Insulin | 0.001 | 0.004 | 0.910 | 0.0001 | 0.004 | 0.965 | 0.001 | 0.005 | 0.763 | 0.001 | 0.005 | 0.798 | −0.001 | 0.005 | 0.870 | 0.852 | 0.032 | 0.008 |
| Chronic stress | −0.051 | 0.004 | 0.174 | −0.643 | 0.037 | 0.083 | −0.119 | 0.048 | 0.013 | −0.007 | 0.046 | 0.885 | −0.055 | 0.049 | 0.266 | 0.679 | 0.310 | 0.029 |
Note.
p<0.05,
p<0.001;
Adjusted for baseline demographic variables (age, years of education, race/ethnicity, smoking status, sex), baseline BMI and baseline food cravings (total or specific type);
Adjusted for baseline demographic factors and baseline weight.
Figure 1.
Mean±SE of baseline-adjusted changes in food cravings over 6 months using a sample-median split of high (≥762 pg/mL) and low ghrelin (<762 pg/mL). A median split was used for graphical display only.
Post-hoc analyses were conducted with each of the FCI subscales using a Bonferroni correction of p<0.0125. Higher baseline ghrelin predicted increases in the frequency of cravings for carbohydrates/starches over 6 months (p=0.002). Baseline ghrelin was not significant in models predicting changes in cravings for high fats, sweets, or fast-food fats (ps>0.05).
Weight
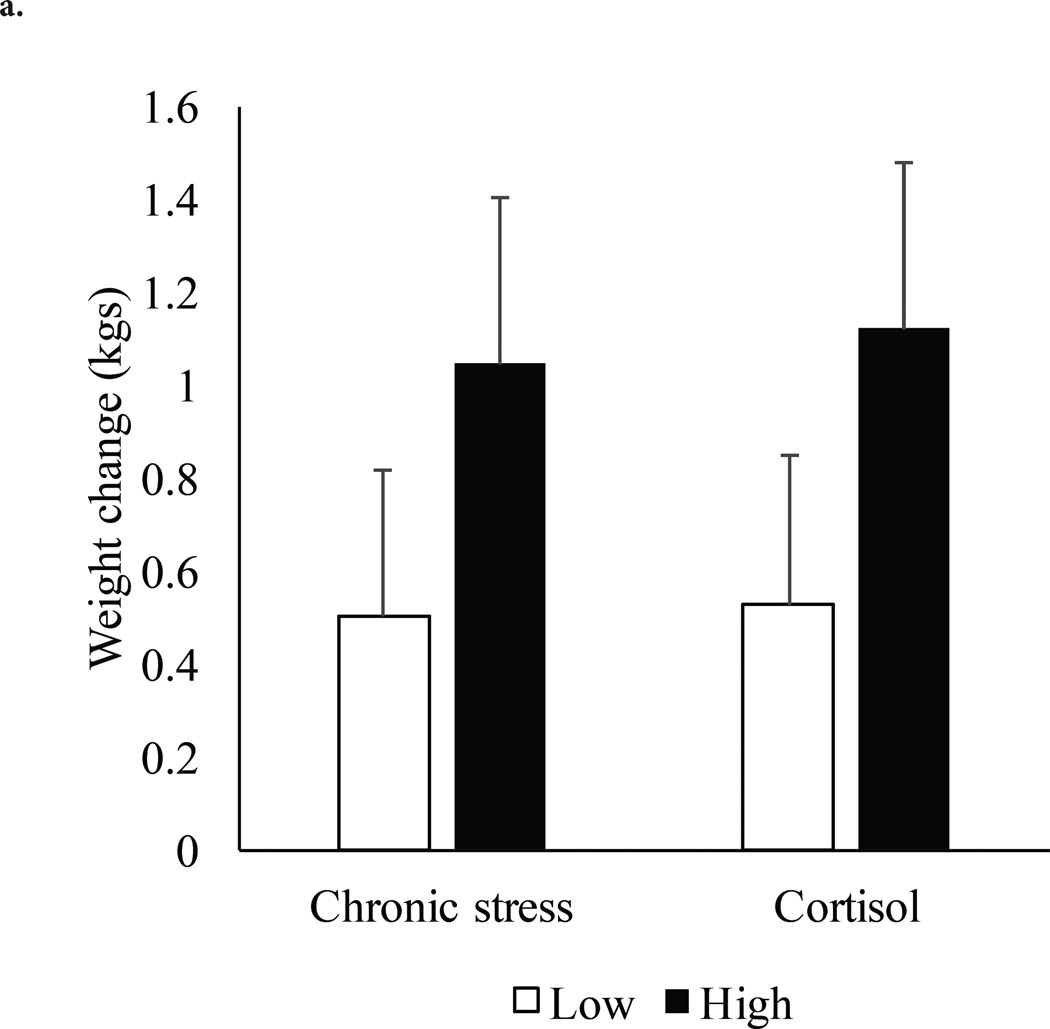
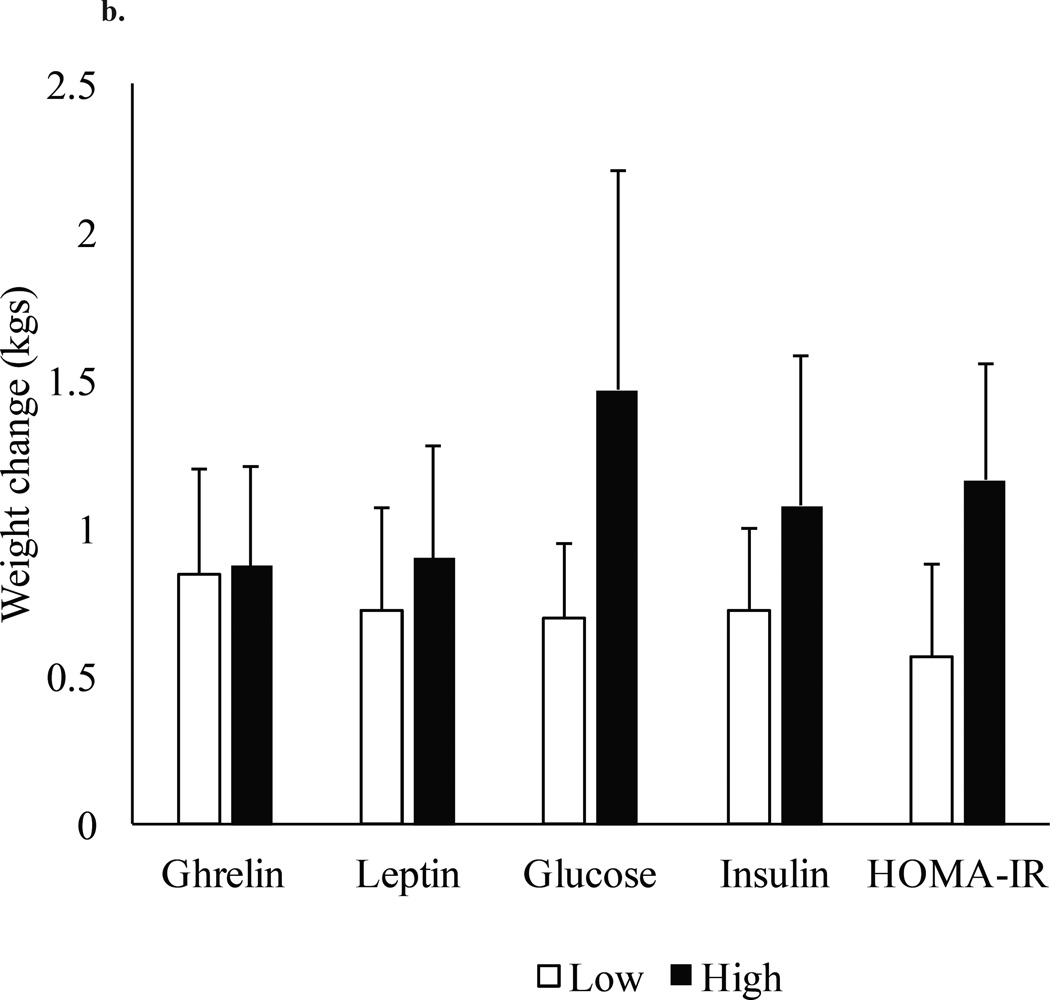
Of the total sample, 49.9% gained weight over 6 months. Among individuals who gained weight, the average gain was 3.54±3.16 kgs and 4.63±4.08% of initial body weight. Of individuals who stayed the same or lost weight, the average loss was 2.54±2.67 kgs and 3.26±3.36% of initial body weight. Weight gain did not differ between males (1.12±4.28 kgs; 1.28±4.63%) and females (0.61±4.18 kgs; 1.00±5.98%; ps=0.29, 0.62). Using a median-sample split, participants with higher baseline chronic stress had a mean 6-month weight gain of 1.05±0.36 kgs compared to 0.50±0.32 kgs for those with lower chronic stress (Figure 2). Individuals with higher baseline cortisol gained an average of 1.12±0.33 kgs whereas those with lower baseline cortisol gained 0.53±0.37 kgs. In adjusted models, higher baseline cortisol, insulin, and increases in chronic stress predicted greater weight gain from baseline to 6 months (p=0.02, 0.008, 0.03, respectively; Table 3). As a post-hoc analysis, we replaced insulin with HOMA-IR in mixed models. Higher HOMA-IR was associated with greater weight gain (B=0.34, SE=0.01, p=0.007).
Figure 2.
a. Mean±SE of weight change (kgs) over 6 months using sample-median splits of high and low cortisol and chronic stress. The median splits were as follows: cortisol≥14.67 mcg/dL and chronic stress≥9.
b. Mean±SE of weight change (kgs) over 6 months using sample-splits of high and low values of appetite-related hormones. The median splits were as follows: ghrelin≥762 pg/mL; leptin≥8.56 ng/mL. A clinical-cut off was used for insulin≥15 µU/mL; glucose≥100 mg/dL; HOMA-IR≥3. Splits were used for graphical display only.
Discussion
To our knowledge, this is the first prospective naturalistic study in a community sample which demonstrates that higher levels of fasting total ghrelin were predictive of future food cravings. These results suggest that ghrelin plays a role in increasing motivation and subjective craving for foods and in reward-based eating, particularly for complex carbohydrates and starches. Ghrelin has well known homeostatic functions on feeding. Ghrelin increases with fasting, peaking prior to meal ingestion, and decreases after eating. Peripheral administration of ghrelin promotes food intake and stimulates food intake by activating homeostatic hypothalamic circuits.23 More recently, it has been demonstrated that ghrelin plays a role in hedonically motivated food behavior, partially by its effects on mesolimbic reward circuits.23 Ghrelin can shift preferences to high palatable foods and increase the motivational aspects of food reward. Administration of ghrelin stimulates more vivid imagination of food compared to a placebo.24 Neuroimaging studies have demonstrated that ghrelin administration increases the neural response to food pictures in areas associated with hedonic eating (i.e., amygdala, hippocampus, orbitofrontal cortex, striatum, and ventral tegmental area).25 Additionally, there is growing evidence that feed-forward and feed-back circuitry between stress and food reward are partly mediated by ghrelin.26 It is important to note that the majority of this previous research reported total ghrelin levels, as in our study. Total ghrelin values include the most abundant form of unacylated ghrelin and the less stable and active, acylated ghrelin.27 Acylated ghrelin may be more responsive and active in response to food intake and motivational aspects and is associated with obesity.28 In the current study, the effect size was small. It is possible that measurement of acylated ghrelin alone would have been a more robust and sensitive predictor of future food cravings and weight gain. Despite this caveat, the previous research cited above together with the present study findings, suggests that ghrelin increases food craving and possibly the hedonic value of food over time, thereby contributing to increased food intake. Development of therapies targeting the ghrelin system may help individuals with high levels of food cravings.
The present study extends findings from cross-sectional studies by examining relationships among appetite-related hormones, stress, and weight change in a large community sample of healthy adults followed prospectively and naturalistically. Similar to some previous studies,29 we observed an inverse relationship between cortisol and BMI, as well as cortisol and stress, in cross-sectional analyses. However, higher baseline cortisol, chronic stress, insulin and HOMA-IR (a measure of insulin resistance) predicted short-term weight gain over a 6-month period. These findings are consistent with studies that demonstrated increased cortisol and self-reported stress promote weight gain.30,31 Our results indicate that while morning cortisol may be blunted among individuals with higher BMI when examined in cross-sectional analyses, future weight gain may be related to complex feedforward and feedback HPA axis dynamics wherein individuals may use food to regulate stress and HPA axis responses.32 Cortisol also helps to regulate feeding behavior and choice, with higher levels of cortisol predicting stress-induced eating as well as binge-eating.33 These results may be due to the direct effects of cortisol and insulin on lipid accumulation through activation of lipoprotein lipase.34 Insulin and cortisol may also act synergistically to upregulate lipogenesis.35 Elevated cortisol stimulates gluconeogenesis, which can result in insulin resistance.36 In previous neuroimaging work, we have shown cortisol increases under the physiologic stress of mild hypoglycemia, which in turn increased brain activation in stress and reward motivation pathways and also increased wanting for high calorie foods.37 We also recently showed that lower dynamic prefrontal activation during stress predicted emotional eating scores in a community sample38 and that higher insulin was associated with greater brain activation in reward regions in response to stress and to food cue exposure, but only in overweight individuals.39 These findings suggest that dynamic stress-related cortisol changes as well as adaptations in cortisol and insulin may modulate brain extrahypothalamic reward and motivation regions to influence future weight gain. Future experimental studies are necessary to elucidate the relationships among cortisol, insulin, and eating behavior to fully understand their role in weight gain. Furthermore, our findings suggest the potential relevance of interventions targeting stress and/or disrupted cortisol responses for weight management. For example, in a recent 8-week trial, 52 participants were randomized to placebo or treatment with Ashwagandha, a standardized root extract that has been suggested to help counteract the negative effects of stress.40 Relative to placebo, treatment with Ashwagandha resulted in significant improvements in perceived stress, food cravings, cortisol, and weight.
Despite cross-sectional associations between food cravings and BMI, neither baseline nor change in food cravings were predictive of weight change. Our sample mean on the FCI was low which may have resulted in floor effects. The low scores are possibly related to the use of a community cohort and geographical differences in food preferences between items on the FCI, which was developed in the Southern region of the US, and the current sample from the Northeast. It is also possible that visual or olfactory food stimuli to provoke craving may be a more sensitive predictor of weight relative to self-report. The effects of food cravings on weight status may be subtle and take a longer duration of time to manifest.
In this sample recruited from the community, 49.9% of participants gained weight over the 6 months and the average weight gain was 3.5±3.2 kgs. This weight gain is significantly higher than the 0.2 to 0.9 kg each year (i.e., 0.1 kg to 0.45 kg over 6 months) reported in previous studies. This is possibly because the average age of our participants was 29.1 years. College-aged individuals and young adults between the ages of 25 to 34 years are particularly susceptible to weight gain, which may have contributed to the large weight increases seen in this sample. If this rate of weight gain continued, it would be significant in terms of obesity risk and population health.
There are several limitations to this study. While the effect sizes of the findings were small, it is important to note that we studied the natural course and outcome of a community sample and individuals were generally healthy. Results may not generalize to other groups. There may have been floor effects as there were low levels of chronic stress, and metabolic parameters were largely within normal limits. Several laboratory-based stress paradigms have been used to investigate the effect of stress on eating and weight. We chose to use participant’s naturalistic self-report of chronic stress and circulating hormone measures while participants were fasting. It is possible that different responses would be seen during acute or laboratory-based stress or feeding paradigms. Our results included a prospective short-term (6-month) follow-up assessment for prediction of future food cravings and weight gain. The longer-term effects of cortisol, stress and appetitive hormones and their associated weight outcomes are unknown and longer follow-up studies are needed. Biochemical data were collected under fasting conditions but only at baseline and at a single time point for the metabolic hormones. We were not able to assess how the dynamics of 24-hour cortisol profiles or changes in cortisol or appetite-related hormones may effect changes in weight or food cravings.
In conclusion, ghrelin was associated with future higher frequencies of food cravings over the 6-month follow-up period, suggesting its role in motivation for food and reward-based eating. Chronic stress, cortisol levels, insulin levels, and HOMA-IR each predicted future weight gain over the 6-month assessment period in a sample of adult volunteers recruited from the community. Future research is needed to test whether interventions targeting stress and disrupted cortisol responses may help to mitigate weight gain in community samples.
Study Importance.
What is already known about this subject?
Stress, cortisol, and other metabolic hormones have been identified as possible clinical targets related to eating behaviors and weight regulation.
Findings on the relationships between cortisol and weight status are inconsistent and largely rely on cross-sectional data.
Little is known about the prospective effects of stress and appetite-related hormones on food cravings and weight.
What does your study add?
In this naturalistic longitudinal cohort of participants recruited from the community, 49.9% of individuals gained weight over 6 months.
Individuals with higher baseline ghrelin had significantly higher food cravings at follow-up.
Higher baseline cortisol, insulin, HOMA-IR and chronic stress predicted greater weight gain from baseline to 6 months.
Acknowledgments
Funding: This work was supported by the National Institutes of Health (NIH; PL1-DA024859; UL1-DE019586; R01-DK099039 and the Yale CTSA UL1TR001863). AMC was funded by a postdoctoral fellowship from the National Institutes of Nursing Research/NIH (T32NR007100-17). AMJ was funded by the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK)/NIH (K23DK101694). CMG was funded, in part by, the NIDDK/NIH (K24DK070052). The contents of this work are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Disclosures: Dr. Chao reports receiving grant support on behalf of the University of Pennsylvania from Shire Pharmaceuticals. Dr. White has a patent Copyright: Food Craving Inventory (copyright owned by Pennington Biomedical Research Center) with royalties paid. Dr. Sinha serves on the Scientific Advisory Board of Embera Neurotherapeutics and has received honorarium for consultation to them. Dr. Grilo reports personal fees from Shire, personal fees from Sunovion, other from American Psychological Association, other from Guilford Press Publishers, other from Taylor & Francis Publishers, other from American Academy CME, other from Vindico CME, other from Global Medical Education, other from Medscape CME, other from Professional and Scientific Conferences (various), outside the submitted work.
References
- 1.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malhotra R, Østbye T, Riley CM, Finkelstein EA. Young adult weight trajectories through midlife by body mass category. Obesity. 2013;21(9):1923–1934. doi: 10.1002/oby.20318. [DOI] [PubMed] [Google Scholar]
- 4.Hopkins M, Blundell JE. Energy balance, body composition, sedentariness and appetite regulation: pathways to obesity. Clin Sci. 2016;130(18):1615–1628. doi: 10.1042/CS20160006. [DOI] [PubMed] [Google Scholar]
- 5.Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response 1. Annu Rev Physiol. 2005;67:259–284. doi: 10.1146/annurev.physiol.67.040403.120816. [DOI] [PubMed] [Google Scholar]
- 6.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 7.Wardle J, Chida Y, Gibson EL, Whitaker KL, Steptoe A. Stress and adiposity: A meta-analysis of longitudinal studies. Obesity. 2011;19(4):771–778. doi: 10.1038/oby.2010.241. [DOI] [PubMed] [Google Scholar]
- 8.Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21(3):159–165. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11):887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Klok M, Jakobsdottir S, Drent M. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: A review. Obes Rev. 2007;8(1):21–34. doi: 10.1111/j.1467-789X.2006.00270.x. [DOI] [PubMed] [Google Scholar]
- 11.Le Roux C, Patterson M, Vincent R, Hunt C, Ghatei M, Bloom S. Postprandial plasma ghrelin is suppressed proportional to meal calorie content in normal-weight but not obese subjects. The Journal of Clinical Endocrinology & Metabolism. 2005;90(2):1068–1071. doi: 10.1210/jc.2004-1216. [DOI] [PubMed] [Google Scholar]
- 12.Tschöp M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000;407(6806):908–913. doi: 10.1038/35038090. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404(6778):661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 14.Stephens MAC, Wand G. Stress and the HPA axis: role of glucocorticoids in alcohol dependence. Alcohol Research-Current Reviews. 2012;34(4):468. doi: 10.35946/arcr.v34.4.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry. 2013;73(9):827–835. doi: 10.1016/j.biopsych.2013.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weingarten HP, Elston D. The phenomenology of food cravings. Appetite. 1990;15(3):231–246. doi: 10.1016/0195-6663(90)90023-2. [DOI] [PubMed] [Google Scholar]
- 17.Chao A, Grilo CM, White MA, Sinha R. Food cravings, food intake, and weight status in a community-based sample. Eating Behaviors. 2014;15(3):478–482. doi: 10.1016/j.eatbeh.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin CK, O’Neil PM, Tollefson G, Greenway FL, White MA. The association between food cravings and consumption of specific foods in a laboratory taste test. Appetite. 2008;51(2):324–326. doi: 10.1016/j.appet.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chao A, Grilo CM, White MA, Sinha R. Food cravings mediate the relationship between chronic stress and body mass index. J Health Psychol. 2015;20(6):721–729. doi: 10.1177/1359105315573448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. J Health Soc Behav. 1995:360–376. [PubMed] [Google Scholar]
- 21.Ansell EB, Rando K, Tuit K, Guarnaccia J, Sinha R. Cumulative adversity and smaller gray matter volume in medial prefrontal, anterior cingulate, and insula regions. Biol Psychiatry. 2012;72(1):57–64. doi: 10.1016/j.biopsych.2011.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White MA, Whisenhunt BL, Williamson DA, Greenway FL, Netemeyer RG. Development and validation of the Food-Craving Inventory. Obes Res. 2002;10(2):107–114. doi: 10.1038/oby.2002.17. [DOI] [PubMed] [Google Scholar]
- 23.Nakazato M, Murakami N, Date Y, et al. A role for ghrelin in the central regulation of feeding. Nature. 2001;409(6817):194–198. doi: 10.1038/35051587. [DOI] [PubMed] [Google Scholar]
- 24.Schmid DA, Held K, Ising M, Uhr M, Weikel JC, Steiger A. Ghrelin stimulates appetite, imagination of food, GH, ACTH, and cortisol, but does not affect leptin in normal controls. Neuropsychopharmacology. 2005;30(6):1187–1192. doi: 10.1038/sj.npp.1300670. [DOI] [PubMed] [Google Scholar]
- 25.Malik S, McGlone F, Bedrossian D, Dagher A. Ghrelin modulates brain activity in areas that control appetitive behavior. Cell Metab. 2008;7(5):400–409. doi: 10.1016/j.cmet.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Schellekens H, Finger BC, Dinan TG, Cryan JF. Ghrelin signalling and obesity: at the interface of stress, mood and food reward. Pharmacol Ther. 2012;135(3):316–326. doi: 10.1016/j.pharmthera.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Staes E, Rozet E, Učakar B, Hubert P, Préat V. Validation of a method for the quantitation of ghrelin and unacylated ghrelin by HPLC. J Pharm Biomed Anal. 2010;51(3):633–639. doi: 10.1016/j.jpba.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 28.Castaneda T, Tong J, Datta R, Culler M, Tschöp M. Ghrelin in the regulation of body weight and metabolism. Front Neuroendocrinol. 2010;31(1):44–60. doi: 10.1016/j.yfrne.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 29.Rodriguez ACI, Epel ES, White ML, Standen EC, Seckl JR, Tomiyama AJ. Hypothalamic-pituitary-adrenal axis dysregulation and cortisol activity in obesity: a systematic review. Psychoneuroendocrinology. 2015;62:301–318. doi: 10.1016/j.psyneuen.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 30.Roberts CJ, Campbell IC, Troop N. Increases in weight during chronic stress are partially associated with a switch in food choice towards increased carbohydrate and saturated fat intake. Eur Eat Disord Rev. 2014;22(1):77–82. doi: 10.1002/erv.2264. [DOI] [PubMed] [Google Scholar]
- 31.Kivimäki M, Head J, Ferrie J, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes. 2006;30(6):982–987. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- 32.Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF. Chronic stress promotes palatable feeding, which reduces signs of stress: feedforward and feedback effects of chronic stress. Endocrinology. 2004;145(8):3754–3762. doi: 10.1210/en.2004-0305. [DOI] [PubMed] [Google Scholar]
- 33.Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26(1):37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- 34.Gathercole LL, Morgan SA, Bujalska IJ, Hauton D, Stewart PM, Tomlinson JW. Regulation of lipogenesis by glucocorticoids and insulin in human adipose tissue. PLoS One. 2011;6(10):e26223. doi: 10.1371/journal.pone.0026223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Björntorp P. Hormonal control of regional fat distribution. Hum Reprod. 1997;12(suppl 1):21–25. doi: 10.1093/humrep/12.suppl_1.21. [DOI] [PubMed] [Google Scholar]
- 36.Asensio C, Muzzin P, Rohner-Jeanrenaud F. Role of glucocorticoids in the physiopathology of excessive fat deposition and insulin resistance. Int J Obes. 2004;28:S45–S52. doi: 10.1038/sj.ijo.0802856. [DOI] [PubMed] [Google Scholar]
- 37.Page KA, Seo D, Belfort-DeAguiar R, et al. Circulating glucose levels modulate neural control of desire for high-calorie foods in humans. J Clin Invest. 2011;121(10):4161–4169. doi: 10.1172/JCI57873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sinha R, Lacadie CM, Constable RT, Seo D. Dynamic neural activity during stress signals resilient coping. Proc Natl Acad Sci. 2016;113(31):8837–8842. doi: 10.1073/pnas.1600965113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jastreboff AM, Sinha R, Lacadie C, Small DM, Sherwin RS, Potenza MN. Neural correlates of stress-and food cue–induced food craving in obesity association with insulin levels. Diabetes Care. 2013;36(2):394–402. doi: 10.2337/dc12-1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Choudhary D, Bhattacharyya S, Joshi K. Body weight management in adults under chronic stress through treatment with ashwagandha root extract a double-blind, randomized, placebo-controlled trial. J Evid Based Complementary Altern Med. 2017;22(1):96–106. doi: 10.1177/2156587216641830. [DOI] [PMC free article] [PubMed] [Google Scholar]