Abstract
Objective
Accumulating evidence suggests cross-national differences in adults with bipolar disorder (BD), but also in the susceptibility of their offspring (bipolar offspring). This study aims to explore and clarify cross-national variation in the prevalence of categorical and dimensional psychopathology between bipolar offspring in the US and The Netherlands.
Methods
We compared levels of psychopathology in offspring of the Pittsburgh Bipolar Offspring Study (n=224) and the Dutch Bipolar Offspring Study (n=136) (age 10–18). Categorical psychopathology was ascertained through interviews using the Schedule for Affective Disorders and Schizophrenia for School Age Children (K-SADS-PL), dimensional psychopathology by parental reports using the Child Behavior Checklist (CBCL).
Results
Higher rates of categorical psychopathology were observed in the US versus the Dutch samples (66% versus 44%). We found no differences in the overall prevalence of mood disorders, including BD-I or -II, but more comorbidity in mood disorders in US versus Dutch offspring (80% versus 34%). The strongest predictors of categorical psychopathology were maternal BD (OR: 1.72, p<.05), older age of the offspring (OR: 1.19, p<.05), and country of origin (US; OR: 2.17, p<.001). Regarding comorbidity, only country of origin (OR: 7.84, p<.001) was a significant predictor. In general, we found no differences in dimensional psychopathology based on CBCL reports.
Limitations
Preliminary measure of inter-site reliability.
Conclusions
We found cross-national differences in prevalence of categorical diagnoses of non-mood disorders in bipolar offspring, but not in mood disorder diagnoses nor in parent-reported dimensional psychopathology. Cross-national variation was only partially explained by between-sample differences. Cultural and methodological explanations for these findings warrant further study.
Keywords: Bipolar offspring, High risk, Cross-national, Bipolar disorder, Mood disorder, Child Behavior Checklist
1. Background
Bipolar disorder (BD) is characterized by recurrent episodes of (hypo)mania and depression that affects on average 1.8% of youth across the world (Van Meter et al., 2011). Whereas prevalence of BD-I and -II in youth in the general population is not different between US and non-US countries (Van Meter et al., 2011), clinical studies have shown an increase in the “administrative” prevalence of outpatient visits and hospital admission rates of BD in youth in the United States (US) as compared to most other countries (Holtmann et al., 2010; James et al., 2014; Kozloff et al., 2010; Soutullo et al., 2005). Comparisons between US and European adult patients with BD have also shown higher prevalence, younger age of onset, more severe illnesses, and increased parental history of BD in the US (Bellivier et al., 2011; Post et al., 2008, 2014a, 2014b).
Numerous studies have consistently shown that offspring of adults with BD (hereafter referred to as bipolar offspring) are at increased risk to develop BD and other psychiatric disorders (Axelson et al., 2015; DelBello et al., 2001 ; Duffy et al., 2011; Hafeman et al., 2016; Mesman et al., 2013). Also among these offspring samples, the prevalence of BD and other psychiatric disorders and the age of onset of mood disorders varies significantly across studies and countries. The question is whether these cross-national variations are a real phenomenon or reflect demographic, illness (e.g. parental- or offspring characteristics), methodological (e.g. recruitment method, assessment instruments, information source, age at assessment) or cultural factors and differences (Carlson and Klein, 2014; Duffy et al., 2011; James et al., 2014; Merikangas et al., 2011; Soutullo et al., 2005). Thus far, cross-national variability in psychopathology among bipolar offspring has not been well studied. Recently, a first attempt on this issue was carried out by Post et al. (2016). In this study, BD adults completed a detailed questionnaire about their own illness and their offspring’s psychopathology (US: n= 365, Europe n = 132). Although based only on parent reports, the authors documented higher rates of psychopathology among US offspring in comparison to European offspring. This difference remained significant even when controlling for several prognostic factors including parental illness characteristics, childhood trauma and family history of psychiatric diagnoses. A better understanding of these cross-national differences is important for the interpretation of the scientific literature, and of course, development of effective mental health policies.
In the present study we aimed to evaluate the cross-national differences in categorical and dimensional psychopathology in US and Dutch bipolar offspring in two large and well characterized bipolar offspring studies: the Pittsburgh Bipolar Offspring Study (BIOS) (Birmaher et al., 2009) and the Dutch Bipolar Offspring Study (DBOS) (Wals et al., 2001) using direct interviews and parental reports. Categorical and dimensional psychopathology were examined in offspring aged 10–18 years through the direct interview the Schedule for Affective Disorders and Schizophrenia for School Age Children (K-SADS-PL) (Kaufman et al., 1996) and parental reports using the Child Behavior Checklist (CBCL) (Achenbach, 1991) respectively. Based on the offspring study by Post et al. (2016), we hypothesized cross-national variation in categorical and dimensional psychopathology. These differences would be least partly explained by demographic, parental and methodological variables.
2. Methods
2.1. Subjects
The US sample is based on BIOS (Birmaher et al., 2009), a sample of 388 offspring, aged 6–18 years, of parents with a bipolar I or II disorder. Families were recruited through advertisement and adult outpatient clinics. Study design and recruitment procedures have been described in detail elsewhere (Birmaher et al., 2009). The Dutch sample is based on two ongoing prospective bipolar offspring cohort studies: the DBOS (Wals et al., 2001) and a new yet unpublished cohort: the Dutch Bipolar and Schizophrenia Offspring Study (DBSOS) (for detailed information see Addendum 1). The DBOS recruited 140 offspring, aged 12–21 years old, of parents with BD-I or -II, from 86 families between 1997 and 1999 (Wals et al., 2001). The DBSOS is recruiting bipolar and schizophrenia offspring, aged 10–16 years; all available bipolar offspring (n=33) recruited between 2010 and 2012 were included in the present study. Both Dutch studies recruited through the Dutch Association for Manic Depressives and Relatives and outpatient clinics for patients with BD in different regions of the Netherlands. The DBOS and DBSOS were combined in order to enlarge the Dutch sample and to optimize equality in age range between the US and Dutch sample (age 6–18 versus 10–21). Only offspring aged 10–18 years were selected to optimally compare the US and the Dutch samples. Exclusion criteria in offspring for both the US and two Dutch studies were a severe physical disease or handicap and an IQ<70. Studies were approved by the institutional review board and written informed consent was obtained from parents and offspring (Wals et al., 2001). An overview of the sample selection is provided in Fig. 1.
Fig. 1.
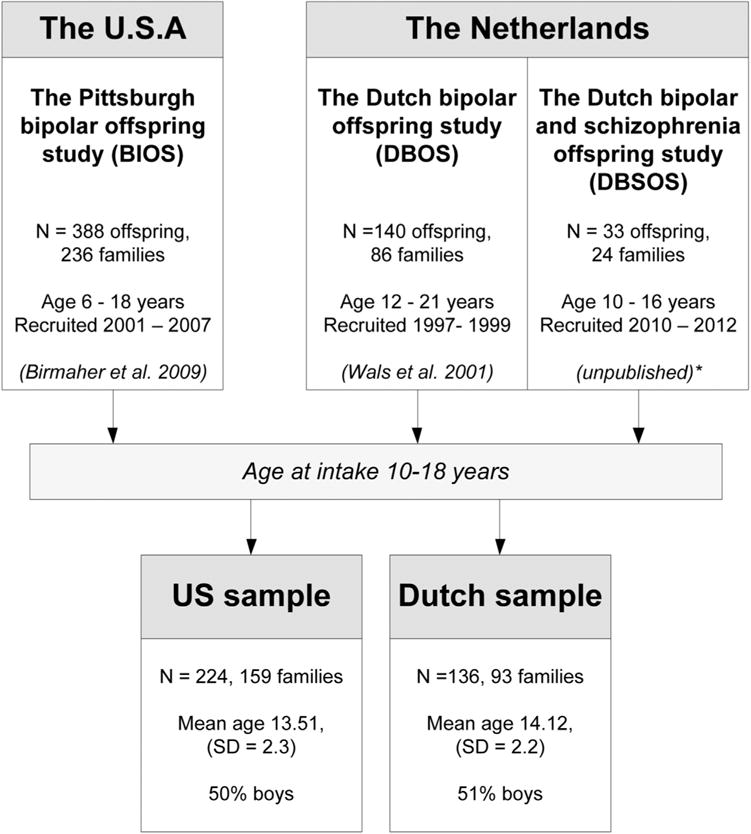
Origin bipolar offspring studies.
3. Instruments
3.1. Parental psychopathology
In the US-sample, DSM-IV axis I disorders for all BD probands and 30% of the biological co-parents were directly ascertained through the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (First, Spitzer, Gibbon and Williams, 1997). The psychopathology of the other biological co-parents was indirectly assessed using the Family History Research Diagnostic Criteria method (FH-RDC) (Andreasen et al., 1977) through the BD proband (Birmaher et al., 2009). Diagnoses were confirmed during diagnostic consensus conferences with a psychiatrist. In the DBOS, BD probands were directly evaluated using the International Diagnostic Checklists (IDCL) (Hiller et al., 1993) and diagnoses were confirmed by the treating psychiatrist or general practitioner. Biological co-parents were assessed by the FH-RDC directly, by phone interviews or through the bipolar proband. For the DBSOS, both the BD proband and biological co-parent were directly evaluated using the SCID-I. For the present analyses, both the US- and the Dutch samples, parental age of onset of the first mood episode of BD was classified as before age 19, between 19 and 25 years old or 26 years and older.
3.2. Categorical psychopathology in offspring
In both the US and the Dutch samples, all current (past 2 months) and past disorders in offspring were assessed using the Schedule for Affective Disorders and Schizophrenia for School Age Children Present and Lifetime Version (K-SADS-PL) (Kaufman et al., 1997). Children and their parents were interviewed separately. Diagnoses were established in accordance with DSM-IV criteria (American Psychiatric Association, 1994). Although both samples were evaluated using the K-SADS-PL, there were minor differences in the implementation of the K-SADS-PL mood section. With regard to BD not otherwise specified (BD-NOS) and cyclothymia, the Dutch sample did not include BD-NOS, but included cyclothymia. The US sample included an operationalized BD-NOS criteria developed for the Course and Outcome of Bipolar Youth (COBY) study (Birmaher et al., 2006). Cyclothymia was subsumed under the BD-NOS category. Although BD-NOS and cyclothymia were not comparably assessed in both studies, all these offspring had mood symptoms with a considerable burden; thus it was decided not to exclude them from the analyses, and rather to count them in the ‘any mood disorder’ category. For both samples, age at onset of first mood disorder was recorded and defined as the age when the subject first met the DSM-IV criteria for a mood disorder. Interviews were conducted by well-trained interviewers with a bachelor or graduate degree and clinical experience. US interviewers were blind to parental diagnosis (Birmaher et al., 2009). In both samples, lifetime psychiatric disorders were diagnosed in consensus with psychiatrists certified in child and adolescent as well as adult psychiatry. The US study kappas for all disorders were above .8. Kappas were not calculated for the Dutch site at the time, but all diagnoses were carefully discussed during consensus meetings reviewing video recordings of the interviews. Studies were conducted in different languages, precluding assessment of inter-site reliability. However, in preparation for this study, using the KSADS-PL, 5 audiotapes from BIOS were blindly rated by 4 interviewers from Pittsburgh and 4 interviewers from the Dutch site with the aim to present some preliminary, measure of inter-site reliability. Kappa statistics were calculated for bipolar I and II disorders and externalizing disorders: oppositional defiant disorder (ODD) and attention deficit hyperactivity disorder (ADHD), with an inter-site reliability of κ 1.00, 1.00 and.62, respectively.
3.3. Dimensional psychopathology in offspring
At both sites, dimensional psychopathology in offspring was ascertained using the CBCL completed by the mothers. The Child Behavior Checklist for Ages 6–18 (CBCL/6–18 ; Achenbach and Rescorla, 2001), assesses a broad range of children’s emotional, behavioral, and social problems. Informants rate each problem item 0 = not true (as far as you know), 1 = somewhat or sometimes true, or 2 = very true or often true, based on the preceding 6 months. Both the 1991 (BIOS, DBOS) and 2001 (DBSOS) versions of the CBCL were administered, and 114 overlapping problem items of both CBCL versions (6 problem items differed) were used for calculations, according to the CBCL manual (Achenbach, 1991; Achenbach et al., 2001). Cases with a CBCL missing value rate over 5% were excluded from the analyses. Total problems, internalizing and, externalizing problem scores (Achenbach, 1991; Achenbach et al., 2001) in addition to the CBCL mania scale (Papachristou et al., 2013) scores were calculated.
3.4. Socioeconomic status (SES)
As SES was measured differently in the US and Dutch sample and no reliable international standard for SES was available, a proxy for SES, the presence of an employed head of household, was utilized.
3.5. Statistical analyses
Differences in demographic characteristics and categorical and dimensional psychopathology across the US- and Dutch sample were compared using t-, χ2- and Fisher exact tests as appropriate. Age of onset of the first mood disorder was compared between the two samples using Kaplan-Meier survival analysis and Log-rank tests. Demographic, clinical and methodological variables that differed significantly (p < .05) between the two samples were included in univariate single predictor regression models. Logistic or Cox proportional regression analyses were applied as appropriate. All single predictors with a coefficient significance of p < .2 in univariate regression models were included in multiple (predictor) stepwise regression models. The final set of predictors were hierarchically organized starting with ‘country of origin’, followed by parental, offspring and environmental characteristics (e.g. living with both parents, employment of parents) consecutively added stepwise to the models. Goodness of fit for all models was determined by the Akaike Information Criterion (AIC). Smaller AIC values indicate better model fit. Missing values were treated as missing in the statistical analyses. Analyses were conducted using the Statistical Package for Social Sciences, version 20.0.
4. Results
4.1. Parent and family characteristics
In total, 93 families from the Dutch sample and 159 families from the US sample were included (Fig. 1). As shown in Table 1, compared to the Dutch sample, families from the US sample showed lower rates of employment. The BD proband in the US sample was more likely to be the mother, to have BD-II, to have substance use disorders and to have a younger age of onset. Prevalence of mood and substance use disorders in the co-parent was significantly higher in the US sample. In two US families and in one Dutch family, both parents were diagnosed with BD.
Table 1.
Demographic and Clinical characteristics US- and Dutch sample.
| US sample
|
Dutch sample
|
P | |||
|---|---|---|---|---|---|
| N | % | n | % | ||
| Offspring | |||||
| Bipolar offspring | 224 | 100 | 136 | 100 | |
| Mean age, sd | 13.51 | 2.3 | 14.12 | 2.2 | .02 |
| Sex, girls | 113 | 50.4 | 66 | 48.5 | .72 |
| Living with both biological parents | 92 | 41.1 | 100 | 73.5 | <.001 |
| Caucasian | 187 | 83.5 | 121 | 89.0 | .15 |
| Family | |||||
| Families | 159 | 100 | 93 | 100 | |
| Employment | 105 | 66.0 | 83 | 89.2 | <.001 |
| Bipolar parent | |||||
| Sex, female | 124 | 78.0 | 55 | 59.1 | .001 |
| Bipolar I disorder | 107 | 67.3 | 75 | 80.6 | .02 |
| Substance use disorder | 104 | 65.4 | 14 | 15.1 | <.001 |
| Age of BD onset: | |||||
| − < 19 | 80 | 50.3 | 24 | 25.8 | <.001 |
| − 19–25 | 41 | 25.8 | 31 | 33.3 | |
| − >25 | 33 | 20.8 | 38 | 40.9 | |
| Biological co-parent | |||||
| Mood disorder | 37 | 23.3 | 16 | 17.2 | .06 |
| Substance use disorder | 43 | 27.0 | 3 | 3.2 | <.001 |
| Mania | 2 | 1.6 | 1 | 1.1 | 1.00 |
| Psychosis | 0 | 0 | 1 | 1.1 | .423 |
| Source of recruitment | <.001 | ||||
| - Advertisement | 101 | 63.5 | 4 | 4.3 | |
| - Psychiatric clinics | 58 | 36.5 | 35 | 37.6 | |
| - Patient advocacy groups | 0 | 0 | 54 | 56.1 | |
| Informant Categorical psychopathology, K-SADS-PL | |||||
| Single informanta | 224 | 100 | 78 | 57.4 | <.001 |
| Motherb | 197 | 88.7 | 128 | 94.1 | .08 |
| Bipolar parent | 168 | 75.7 | 102 | 75.0 | .89 |
| Dimensional psychopathology, CBCLc | |||||
| Motherc | 169 | 79.0 | 75 | 67.0 | .02 |
| Bipolar parent | 214 | 95.5 | 112 | 82.3 | .01 |
One informant versus both parents.
Mother versus father or significant other (n = 7).
As the majority of CBCLs were completed by the bipolar proband; only CBCLs completed by the bipolar proband were selected for further analyses. In total, nine subjects in the US sample and one subject in the Dutch sample had a missing value rate over 5% and were excluded from the analyses.
4.2. Offspring
In total 360 offspring were selected for this study: 224 from the US and 136 from the Dutch sample. As illustrated in Fig. 1 and Table 1, there were no between-group differences in sex or ethnic background. The Dutch offspring were significantly older and resided more often in families with both biological parents than the US offspring.
4.3. Categorical psychopathology
As shown in Table 2, prevalence of any lifetime psychiatric disorder was significantly higher in the US offspring than in the Dutch offspring (66% versus 44%). Specifically, higher rates of anxiety, ADHD and disruptive behavior disorders were observed in the US sample. Higher rates of psychopathology were also reflected in current psychopathology with 51% for US offspring and 29% in Dutch offspring. Interestingly, the US and Dutch sample did not differ in lifetime and current prevalence of any mood disorders, BD-I or -II. However, higher rates of major depressive disorder were reported in the US (13% versus 4%). When focusing on comorbidity rates as a measure for illness severity in offspring with a mood disorder we found significantly higher rates of co-morbid disorders in US offspring: 80% (54% anxiety-, 44% disruptive-, 33% ADHD, 3% pervasive developmental-, and 13% substance use disorders) versus 35% in the Dutch sample (i.e. 12% anxiety-, 9% disruptive-, 9% ADHD, 9% pervasive developmental-and 0% substance use disorders) (χ2(1) = 19.76, p <.001). As illustrated in the survival curve of Fig. 2, age of onset of the first mood disorder was younger in the US offspring (mean age: 10.8 years, range 5–17) compared with the Dutch offspring (mean age: 12.8 years, range 6–18), χ2(1) = 3.97, p <.05).
Table 2.
Categorical psychopathology outcome as assigned by the clinician (K-SADS-PL) and dimensional ratings by the bipolar proband (CBCL).
| Categorical psychopathology | US sample, n = 224
|
Dutch sample, n = 136
|
p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Lifetime | |||||
| Any DSM-IV axis-I disorder | 147 | 65.6 | 60 | 44.1 | <.001 |
| Any mood disorder | 69 | 30.8 | 34 | 25 | .24 |
| - Bipolar I disorder | 5 | 2.2 | 2 | 1.5 | .71 |
| - Bipolar II disorder | 4 | 1.8 | 1 | .7 | .65 |
| - BD-NOSa | 15 | 6.7 | ND | ND | ND |
| - Cyclothymiaa | ND | ND | 2 | 1.5 | ND |
| - Major depressive disorder | 30 | 13.4 | 6 | 4.4 | .006 |
| - Dysthymic disorder | 5 | 2.2 | 7 | 5.1 | .14 |
| - Depression NOS | 18 | 8.0 | 17 | 12.5 | .17 |
| Any psychotic disorder | 1 | .4 | 0 | .0 | 1.0 |
| Any anxiety disorderb | 70 | 31.3 | 12 | 8.8 | <.001 |
| ADHD | 50 | 22.3 | 11 | 8.1 | <.001 |
| Disruptive behavior disordersc | 43 | 19.2 | 8 | 5.9 | <.001 |
| Autism spectrum disordersd | 4 | 1.8 | 7 | 5.1 | .11 |
| Substance use disorders | 12 | 5.4 | 3 | 2.2 | .18 |
| Other disorderse | 51 | 22.8 | 17 | 12.5 | .02 |
| Current | |||||
| Any DSM-IV axis-I disorder | 115 | 51.3 | 40 | 29.4 | <.001 |
| Any mood disorder | 44 | 19.6 | 18 | 13.2 | .12 |
| Dimensional psychopathology |
US sample, n = 214
|
Dutch sample, n = 112
|
p | ||
| Mean | SD | Mean | SD | ||
|
| |||||
| Total problems | 32.22 | 24.9 | 27.49 | 20.7 | .09 |
| Internalizing problems | 10.44 | 8.8 | 8.82 | 8.2 | .11 |
| Externalizing problems | 9.58 | 8.5 | 8.11 | 6.4 | .08 |
| Mania scale | 4.96 | 4.7 | 4.12 | 3.9 | .09 |
| Offspring with mood disorders | n = 65 | n = 27 | |||
| Total problems | 47.66 | 29.0 | 42.63 | 23.2 | .42 |
| Internalizing problems | 15.57 | 11.1 | 14.44 | 9.0 | .64 |
| Externalizing problems | 15.00 | 9.7 | 10.81 | 7.6 | .03 |
| Mania scale | 7.82 | 5.5 | 7.11 | 5.2 | .57 |
Lifetime and current categorical psychopathology. Current categorical psycho-pathology is defined as the past 2 months.
Note: ND = not determined; BD = bipolar disorder; NOS = not otherwise specified; ADHD = Attention Deficit Hyperactivity Disorder.
BD-NOS was not assessed in the Dutch sample. In the US-sample cyclothymia was subsumed under the BD-NOS category (see methods section).
Any anxiety disorder includes: generalized anxiety disorder, separation anxiety disorder, social-, agora- and specific phobia’s, posttraumatic stress disorder, panic disorder, obsessive-compulsive disorder, anxiety nos.
Disruptive behavior disorders includes: opposition defiant-, conduct-, tic-disorder and disruptive disorder nos.
Autism Spectrum disorders includes: Autism-, PDD-NOS or Asperger disorder.
Other disorders includes: lifetime: eating-, body dismorphic-, elimination-, adjustment- and somatization disorders.
Fig. 2.
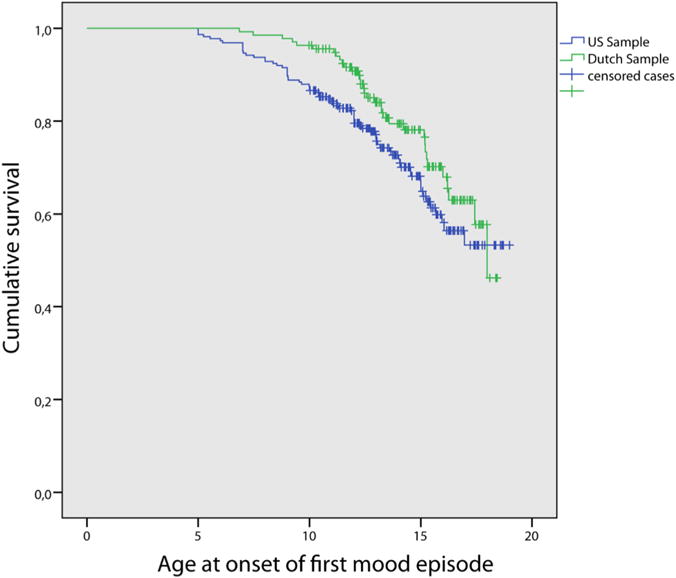
Survival curve age of onset of the first mood episode in US and Dutch bipolar offspring.
4.4. Dimensional psychopathology
In contrast to the categorical K-SADS-PL findings, there were no overall significant between-group differences in the parental ratings on the CBCL scales (Table 2). Among offspring with mood disorders as defined by the K-SADS-PL, categorical findings were partly mirrored on the dimensional assessment as reflected in significantly higher scores on the CBCL externalizing problem subscale. No differences were found on the mania scale or internalizing problem scale.
4.5. Regression analyses
The most apparent differences between US and Dutch bipolar offspring were the prevalence rates of lifetime non-mood disorders, comorbid disorders among offspring with mood disorders and age of onset of mood disorders. Multiple regression analyses were carried out to evaluate whether the observed cross-national differences remained significant after controlling for the significant between-group differences noted in Table 1. First, univariate single predictor analyses were performed as presented in Table S1. Predictors selected for the final regression models included for the parents: maternal bipolarity, BD-II and an early age of onset of BD (< 18 years), substance use in the parents; predictors for the offspring included: age at assessment and environmental factors including unemployment of the parents and not living with both biological parents. Source of recruitment and number of informants were significant predictors, but were excluded from further analyses because of the high specificity for sample of origin (Table 1) causing a problem of multicollinearity in the multiple regression models.
Multiple stepwise regression models are presented in Table 3. The strongest predictors of lifetime psychopathology were maternal BD (OR: 1.72, p < .05), older age of the offspring at assessment (OR: 1.19, p < .05), and also country of origin remained a significant predictor (US; OR: 2.17, p < .001). Comorbidity in mood disorders was best predicted by country of origin (US; OR: 7.84, p < .001). None of the other predictors contributed significantly to the observed cross-national variation. Observed cross-national differences in age of onset of mood disorder did not remain significant (OR: 1.43, p = n.s.). when controlling for the selected variables from the univariate analyses (maternal BD and age of the offspring) (see Table 1).
Table 3.
Stepwise multiple regression analyses: categorical outcome.
| Any psychopathology, n = 318
|
Mood disorders & comorbidity, n = 91
|
Age of onset mood disorder, n = 330b
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors ↓ Model → | 1 | 2 | 3a | 4 | 1a | 2 | 3 | 4 | 1 | 2 | 3a | 4 |
| Step 1: Country of Origin (US) | 2.39*** | 1.92* | 2.17** | 2.06* | 7.84*** | 4.21* | 4.22* | 3.74* | 1.53* | 1.48 | 1.43 | 1.27 |
| Step 2: Parental characteristics | ||||||||||||
| - Bipolar parent (mother) | 1.46 | 1.72* | 1.68 | 1.16 | 1.12 | 1.14 | 1.60 | 1.54 | 1.38 | |||
| - Bipolar disorder (type I) | .76 | .73 | .72 | – | – | – | – | – | – | |||
| - Age of BD onset (< 18 years) | ||||||||||||
| - 19–25 years | .64 | .61 | .62 | 1.37 | 1.41 | 1.43 | – | – | – | |||
| - > = 26 years | 1.00 | .94 | .93 | .79 | .81 | .78 | – | – | – | |||
| - SUD bipolar parent (yes) | – | – | – | 1.90 | 1.90 | 1.76 | – | – | – | |||
| - SUD co-parent (yes) | 1.60 | 1.52 | 1.46 | 2.40 | 2.41 | 2.69 | – | – | – | |||
| Step 3: Age offspring (per year) | 1.1 9 ** | 1.19 ** | .98 | .99 | .91 | .92 | ||||||
| Step 4: Environmental char. | ||||||||||||
| Employment (not employed) | 1.56 | 1.66 | 1.32 | |||||||||
| Not living with both biological Parents | .96 | .93 | 1.30 | |||||||||
| Model fit index: AIC | 425.4 | 424.9 | 416.2a | 418.2 | 105.5a | 111.8 | 113.8 | 117.2 | 1038.3 | 1036.2 | 1035.9a | 1036.1 |
Stepwise procedure multiple regression analyses. Values per predictor represent odds ratio’s or hazard ratio (age of onset mood disorder). When no values presented, predictors were not included in the model (see also Table S1 online). With regard to the reference category: US origin means that the odds presented are increased in comparison to Dutch origin etc. Note: BD = bipolar disorder, SUD = Substance use disorder. AIC = Akaike Information Criterion.
p <.001.
p-value < = 0.05.
p <.01.
Model with best model fit according to Akaike’s Information Criterion (AIC).
Because of the pH assumption of the cox-regression analyses, only offspring aged <17.4 years were selected for further analyses.
5. Discussion
This is the first study to systematically compare two bipolar offspring samples from the US and the Netherlands using direct interviews and parental-reports to assess categorical and dimensional psychopathology. Based on the K-SADS-PL, US offspring showed higher rates of categorical diagnoses, mainly accounted for by non-mood disorders. Moreover, more comorbid psychopathology in mood affected offspring was observed in US offspring. The strongest predictors of psychopathology were maternal BD, older age of the offspring at assessment, and also country of origin. As regards comorbidity, only country of origin was a significant predictor. We found no difference in the prevalence of mood disorders, including BD-I and -II, age of onset, nor parental-reported dimensional psychopathology.
Overall, in line with previous offspring studies, we found higher rates of categorical psychopathology in US offspring (for review see Duffy et al., 2011; Post et al., 2016). In subsequent regression analyses, “country of origin” remained the strongest predictor of psychopathology and comorbidity in mood affected offspring, even after controlling for between-group sample differences. These findings suggest that cross-national variation exists, however no significant differences in dimensional psychopathology across samples were observed when measured via parent-reports (CBCL). Therefore, the question remains whether this is ‘real’ cross-national variation or rather methodological or cultural issues are involved. For example, cross-national differences in prevailing attitudes and beliefs regarding specific psychiatric diagnoses in youth may be involved. Cultural context may impact how clinical information is expressed by individuals, parents and/or interpreted by the clinician (Bird, 1996; Draguns and Tanaka-Matsumi, 2003; Reichart and Nolen, 2004). The preliminary measure of inter-site reliability of this study suggests the possibility that there are differences in which the sites ascertained and/or interpreted non-mood disorders and explain, at least in part, the differences in the rates of these disorders between the two sites. Moreover, other unmeasured variables may have contributed to the noted differences between the two samples. Early trauma and stressful life events may be such an example, as adult bipolar studies have shown that US patients experienced more stressors, both prior to and during the course of their illness, than European patients (Post et al., 2014a).
Other than cross-national variation, also age of the offspring was an important predictor lifetime psychopathology. Age, naturally, is an important predictor of increased rates of lifetime psychopathology. This finding stresses the importance of taking into account age at assessment when interpreting reported differences in the literature. Also maternal BD was significantly associated with psychopathology. Only a few reports on maternal BD exist. Since mothers often are the primary care-givers, impact of mood disorders on parenting can be profound. It has been suggested that maternal BD is associated with an impaired parent-child interaction, an unstable environment and more physical and/or psychological abuse. This may negatively affect the susceptibility for psychopathology in their offspring (Alloy et al., 2006; Moreno et al., 2012; Mowbray et al., 2006). In addition, an informant bias for mothers cannot be ruled out, which may lead to over-estimation of their offspring’s psychopathology (Müller and Furniss, 2013).
The finding that bipolar offspring from the US and the Netherlands have a similar prevalence of BD–I and -II is in line with previous epidemiological cross-national comparison studies (Van Meter et al., 2011; Weissman et al., 1996). Moreover, this study suggests that the liability for mood disorders in general, in terms of prevalence, was similar across samples. These findings contrast with those of the offspring study by Post et al. (2016) who report increased rates of BD (17% versus 4%) and depression (25% and 8%) in US versus European offspring of BD parents. However, this is probably primarily due to methodological differences including reliance on parent-report as opposed to direct interview and the absence of detailed demographic information on the offspring. The difference in age of onset of the first mood episode did not remain significant after controlling for other characteristics. Once again, this finding contrasts the existing literature on adults with BD in which earlier onset of BD is consistently reported among US patients as compared to European patients (Bellivier et al., 2011; Leboyer et al., 2005; Post et al., 2014b) suggesting that previous reported differences may also be driven by retrospective bias, selection bias and/or other sample differences.
Findings of the dimensional assessment as completed by the parent did not converge completely with categorical assessment by the clinician. Although we found higher rates of categorical psychopathology in US offspring, we found no significant overall differences in dimensional psychopathology as reported by the BD parent between the US and Dutch offspring. There are several potential reasons for the difference between categorical diagnoses and dimensional psychopathology. Previous studies have shown that CBCL scores and the K-SADS-PL based DSM-IV diagnoses significantly correlate but that both approaches do not converge completely (Kasius et al., 1997; Rishel et al., 2005). It is possible that trained interviewers using the K-SADS-PL were able to more accurately ascertain psychopathology. Furthermore, the K-SADS-PL evaluated both current and lifetime psychopathology, while the CBCL only ascertained psychopathology for the prior 6 months before parents completed this questionnaire. However, as indicated in Table 2, cross-national differences in lifetime psycho-pathology were also present in current psychopathology as obtained with the K-SADS-PL, mitigating this concern to some extent. Finally, as discussed above, it is possible that there were discrepancies in the scoring and/or interpretation of the data collected through the K-SADS-PL. In fact, the preliminary inter rater reliability between the two sites showed lower kappas for the externalizing disorders.
Findings of this study must be interpreted in the context of the following limitations. As this study was carried out in two different languages and the comparison was post-hoc only a preliminary measure of intersite-reliability could be obtained based on US and -because of the need to understand the language spoken - not on Dutch offspring. Also, although we attempted to take into account type of recruitment as possible source of interference, recruitment was too sample specific and could not be included in our analyses. However, there is a possibility that recruitment plays a significant role, for example recruitment through advocacy groups (the Dutch sample) may have led to a selection of a better functioning and informed families. More systematic studies are needed to further elucidate this issue. Furthermore, as noted in the methods section, BD-NOS was not assessed in Dutch offspring and could therefore not be compared directly. Cross-national variation may be especially an issue with BD-NOS, as both administrative studies and epidemiological studies show more variation when BD-NOS is included (James et al., 2014; Van Meter et al., 2011). However, it is interesting to note that we found no differences on the mania scale as obtained with the CBCL across samples. Future studies could benefit from including more specifically defined BD-NOS criteria such as those used in the COBY study. Despite the limitations, this study adds meaningful preliminary insights regarding cross-national differences in psychopathology among bipolar offspring. A clinically and scientifically important topic for which there is a paucity of data. These findings are based on a comparison that benefits from using standardized direct interviews, similar well validated instruments, multiple informants and offspring within the same age range. Future studies are warranted to improve our understanding of cross-national variation in bipolar offspring and adult BD studies. The current study provides important heuristics to guide the hypotheses and designs of future studies.
In conclusion, we found cross-national differences in the prevalence of non-mood disorders in adolescent offspring of BD parents but not in the prevalence of BD or mood disorders in general or parent-reported dimensional psychopathology. The differences in psychopathology were accounted for by country of origin, maternal BD and older age at assessment. Potential explanations for cross-national variation and the discrepancy in categorical versus dimensional ratings were discussed. Despite the preliminary character of this study, present findings emphasize the need to take into account these variables when comparing psychopathology prevalence rates in BD offspring across countries and warrant continued attention for cross-national variation in study outcomes.
Supplementary Material
Acknowledgments
Grant support
The Dutch Bipolar Offspring Study was financially supported by the Netherlands Organization for Scientific Research (Grant #9120818) and 7FP of the European Commission (Grant #22963). The Pittsburgh bipolar offspring study was financially supported by the National Institute of Mental Health (Grant #MH60952). The funding had no role in the conduct of the study or in the presentation and interpretation of results.
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.jad.2016.06.011.
Footnotes
Presented in part at the 61st annual meeting of the American Academy of Child Adolescent Psychiatry, San Diego, October 22, 2014.
Contributor’s statement
Study concept and design: Hillegers, Nolen, Birmaher, Axelson.
Acquisition of data: Wals, Reichart, Hillegers, Vleeschouwer, Axelson, Hickey, Diler, Sakolsky.
Analyses and interpretation of the data: Mesman, Derks, Axelson, Goldstein, Hickey.
Drafting of the manuscript: Mesman, Birmaher, Hillegers.
Critical revision of the manuscript: Hillegers, Birmaher, Goldstein, Goldstein, Axelson, Diler, Hafeman, Derks, Verhulst Reichart, Nolen.
Conflict of interest
Boris Birmaher, MD has received royalties for publications from Random House, Inc., Lippincott Williams & Wilkins and UpToDate. Dr. Frank C. Verhulst is the contributing editor of the Achenbach System of Empirically Based Assessment, from which he receives remuneration. Manon H.J. Hillegers was part of the Benecke Advisory Board. W. A. Nolen has received grants from the Netherlands Organization for Health Research and Development, the European Union; has received honoraria/speaker’s fees from Astra Zeneca, Lundbeck, and has served as consultant for Daleco Pharma. For the other authors, no competing financial interest exists.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profiles. University of Vermont, Department of Psychiatry; Burlington: 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington: University of Vermont, Department of Psychiatry; 2001. [Google Scholar]
- Alloy LB, Abramson LY, Smith JM, Gibb BE, Neeren AM. Role of parenting and maltreatment histories in unipolar and bipolar mood disorders: mediation by cognitive vulnerability to depression. Clin Child Fam Psychol Rev. 2006;9:23–64. doi: 10.1007/s10567-006-0002-4. http://dx.doi.org/10.1007/s10567-006-0002-4. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; Washington DC: 1994. [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliability and validity. Arch Gen Psychiatry. 1977;34:1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. http://dx.doi.org/10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- Axelson D, Goldstein B, Goldstein T, Monk K, Yu H, Hickey MB, Sakolsky D, Diler R, Hafeman D, Merranko J, Iyengar S, Brent D, Kupfer D, Birmaher B. Diagnostic precursors to bipolar disorder in offspring of parents with bipolar disorder: a longitudinal study. Am J Psychiatry. 2015;172 doi: 10.1176/appi.ajp.2014.14010035. http://dx.doi.org/10.1176/appi.ajp.2014.14010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellivier F, Etain B, Malafosse A, Henry C, Kahn JP, Elgrabli-Wajsbrot O, Ja-main S, Azorin JM, Frank E, Scott J, Grochocinski V, Kupfer DJ, Golmard JL, Leboyer M. Age at onset in bipolar I affective disorder in the USA and Europe. World J Biol Psychiatry. 2011 doi: 10.3109/15622975.2011.639801. [DOI] [PubMed] [Google Scholar]
- Bird HR. Epidemiology of childhood disorders in a cross-cultural context. J Child Psychol Psychiatry Allied Discip. 1996 doi: 10.1111/j.1469-7610.1996.tb01379.x. http://dx.doi.org/10.1111/j.1469-7610.1996.tb01379.x. [DOI] [PubMed]
- Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, Obreja M, Ehmann M, Iyengar S, Shamseddeen W, Kupfer D, Brent D. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the Pittsburgh bipolar offspring study. Arch Gen Psychiatry. 2009;66:287–296. doi: 10.1001/archgenpsychiatry.2008.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson GA, Klein DN. How to understand divergent views on bipolar disorder in youth. Annu Rev Clin Psychol. 2014;10:529–551. doi: 10.1146/annurev-clinpsy-032813-153702. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Soutullo CA, Hendricks W, Niemeier RT, McElroy SL, Strakowski SM. Prior stimulant treatment in adolescents with bipolar disorder: association with age at onset. Bipolar Disord. 2001;3:53–57. doi: 10.1034/j.1399-5618.2001.030201.x. [DOI] [PubMed] [Google Scholar]
- Draguns JG, Tanaka-Matsumi J. Assessment of psychopathology across and within cultures: issues and findings. Behav Res Ther. 2003;41:755–776. doi: 10.1016/s0005-7967(02)00190-0. [DOI] [PubMed] [Google Scholar]
- Duffy A, Doucette S, Lewitzka U, Alda M, Hajek T, Grof P. Findings from bipolar offspring studies: methodology matters. Early Interv. Psychiatry. 2011;5:181–191. doi: 10.1111/j.1751-7893.2011.00276.x. http://dx.doi.org/10.1111/j.1751-7893.2011.00276.x. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. User’s Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders - Clinical Version (SCID-CV) American Psychiatric Press; Washingtion DC: 1997. [Google Scholar]
- Hafeman DM, Merranko J, Axelson D, Goldstein BI, Goldstein T, Monk K, Hickey MB, Sakolsky D, Diler R, Iyengar S, Brent D, Kupfer D, Birmaher B. Toward the definition of a bipolar prodrome: dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. 2016 doi: 10.1176/appi.ajp.2015.15040414. http://dx.doi.org/10.1176/appi.ajp.2015.15040414 (appi.ajp.2015.1.) [DOI] [PMC free article] [PubMed]
- Hiller W, Zaudig M, Mombour W, Bronisch T. Routine psychiatric examinations guided by ICD-10 diagnostic checklists (international diagnostic checklists) Eur Arch Psychiatry Clin Neurosci. 1993;242:218–223. doi: 10.1007/BF02189966. [DOI] [PubMed] [Google Scholar]
- Holtmann M, Duketis E, Poustka L, Zepf FD, Poustka F, Bolte S. Bipolar disorder in children and adolescents in Germany: national trends in the rates of inpatients, 2000–2007. Bipolar Disord. 2010;12:155–163. doi: 10.1111/j.1399-5618.2010.00794.x. [DOI] [PubMed] [Google Scholar]
- James A, Hoang U, Seagroatt V, Clacey J, Goldacre M, Leibenluft E. A comparison of American and English hospital discharge rates for pediatric bipolar disorder, 2000–2010. J Am Acad Child Adolesc Psychiatry. 2014;53:614–624. doi: 10.1016/j.jaac.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasius MC, Ferdinand RF, van den Berg H, Verhulst FC. Associations between different diagnostic approaches for child and adolescent psychopathology. J Child Psychol Psychiatry. 1997;38:625–632. doi: 10.1111/j.1469-7610.1997.tb01689.x. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kaufman Birmaher, Rao R. Diagnostic Interview Kiddie-Sads-Present and Lifetime Version (K-SADS-PL) 1996 Oct;135:153–162. doi: http://dx.doi.org/10.1097/00004583-199707000-00021. [Google Scholar]
- Kozloff N, Cheung AH, Schaffer A, Cairney J, Dewa CS, Veldhuizen S, Kurdyak P, Levitt AJ. Bipolar disorder among adolescents and young adults: results from an epidemiological sample. J Affect Disord. 2010;125:350–354. doi: 10.1016/j.jad.2010.02.120. [DOI] [PubMed] [Google Scholar]
- Leboyer M, Henry C, Paillere-Martinot ML, Bellivier F. Age at onset in bipolar affective disorders: a review. Bipolar Disord. 2005;7:111–118. doi: 10.1111/j.1399-5618.2005.00181.x. [DOI] [PubMed] [Google Scholar]
- Müller JM, Furniss T. Correction of distortions in distressed mothers’ ratings of their preschool children’s psychopathology. Psychiatry Res. 2013;210:294–301. doi: 10.1016/j.psychres.2013.03.025. http://dx.doi.org/10.1016/j.psychres.2013.03.025. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, Viana MC, Andrade LH, Hu C, Karam EG, Ladea M, Medina-Mora ME, Ono Y, Posada-Villa J, Sagar R, Wells JE, Zarkov Z. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68:241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesman E, Nolen WA, Reichart CG, Wals M, Hillegers MHJ. The dutch bipolar offspring study: 12-year follow-up. Am J Psychiatry. 2013:542–549. doi: 10.1176/appi.ajp.2012.12030401. http://dx.doi.org/10.1176/appi.ajp.2012.12030401. [DOI] [PubMed]
- Moreno DH, Bio DS, Petresco S, Petresco D, Gutt EK, Soeiro-De-Souza MG, Moreno RA. Burden of maternal bipolar disorder on at-risk offspring: a controlled study on family planning and maternal care. J Affect Disord. 2012;143:172–178. doi: 10.1016/j.jad.2012.05.050. http://dx.doi.org/10.1016/j.jad.2012.05.050. [DOI] [PubMed] [Google Scholar]
- Mowbray CT, Bybee D, Oyserman D, MacFarlane P, Bowersox N. Psychosocial outcomes for adult children of parents with severe mental illnesses: demographic and clinical history predictors. Health Soc Work. 2006;31:99–108. doi: 10.1093/hsw/31.2.99. http://dx.doi.org/10.1093/hsw/31.2.99. [DOI] [PubMed] [Google Scholar]
- Papachristou E, Ormel J, Oldehinkel AJ, Kyriakopoulos M, Reinares M, Reichenberg A, Frangou S. Child behavior checklist-mania scale (CBCL-MS): development and evaluation of a population-based screening scale for bipolar disorder. PLoS One. 2013;8:e69459. doi: 10.1371/journal.pone.0069459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM, Altshuler L, Kupka R, McElroy S, Frye M, Rowe M, Leverich GS, Grunze H, Suppes T, Keck PE, Jr, Nolen WA. More pernicious course of bipolar disorder in the United States than in many European countries: implications for policy and treatment. J Affect Disord. 2014a;160:27–33. doi: 10.1016/j.jad.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Post RM, Altshuler LL, Kupka R, McElroy SL, Frye MA, Rowe M, Grunze H, Suppes T, Keck PE, Leverich GS, Nolen WA. More illness in offspring of bipolar patients from the U.S. compared to Europe. J Affect Disord. 2016;191:180–186. doi: 10.1016/j.jad.2015.11.038. http://dx.doi.org/10.1016/j.jad.2015.11.038. [DOI] [PubMed] [Google Scholar]
- Post RM, Luckenbaugh DA, Leverich GS, Altshuler LL, Frye MA, Suppes T, Keck PE, McElroy SL, Nolen WA, Kupka R, Grunze H, Walden J. Incidence of childhood-onset bipolar illness in the USA and Europe. Br J Psychiatry. 2008;192:150–151. doi: 10.1192/bjp.bp.107.037820. http://dx.doi.org/10.1192/bjp.bp.107.037820. [DOI] [PubMed] [Google Scholar]
- Post RM, Leverich GS, Kupka R, Keck P, McElroy S, Altshuler L, Frye MA, Luckenbaugh DA, Rowe M, Grunze H, Suppes T, Nolen WA. Increased parental history of bipolar disorder in the United States: association with early age of onset. Acta Psychiatr Scand. 2014b;129:375–382. doi: 10.1111/acps.12208. http://dx.doi.org/10.1111/acps.12208. [DOI] [PubMed] [Google Scholar]
- Reichart CG, Nolen WA. Earlier onset of bipolar disorder in children by antidepressants or stimulants? An hypothesis. J Affect Disord. 2004;78:81–84. doi: 10.1016/s0165-0327(02)00180-5. [DOI] [PubMed] [Google Scholar]
- Rishel CW, Greeno C, Marcus SC, Shear MK, Anderson C. Use of the child behavior checklist as a diagnostic screening tool in community mental health. Res Soc Work Pract. 2005;15:195–203. [Google Scholar]
- Soutullo CA, Chang KD, Diez-Suarez A, Figueroa-Quintana A, Escamilla-Canales I, Rapado-Castro M, Ortuno F. Bipolar disorder in children and adolescents: international perspective on epidemiology and phenomenology. Bipolar Disord. 2005;7:497–506. doi: 10.1111/j.1399-5618.2005.00262.x. [DOI] [PubMed] [Google Scholar]
- Van Meter AR, Moreira AL, Youngstrom EA. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J Clin Psychiatry. 2011;72:1250–1256. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- Wals M, Hillegers MH, Reichart CG, Ormel J, Nolen WA, Verhulst FC. Prevalence of psychopathology in children of a bipolar parent. J Am Acad Child Adolesc Psychiatry. 2001;40:1094–1102. doi: 10.1097/00004583-200109000-00019. http://dx.doi.org/10.1097/00004583-200109000-00019. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, Joyce PR, Karam EG, Lee CK, Lellouch J, Lepine JP, Newman SC, Rubio-Stipec M, Wells JE, Wickramaratne PJ, Wittchen H, Yeh EK. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:293–299. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


