Abstract
Objectives
To improve systems of care to advance implementation of the U.S. Preventive Services Task Force recommendations for childhood obesity treatment (i.e. clinicians offer/refer children with obesity to intensive, multicomponent behavioral interventions of >25 hours over 6–12 months to improve weight status) and to expand payment for these services.
Methods
In July 2015, forty-three cross-sector stakeholders attended a conference supported by the Agency for Healthcare Research and Quality, American Academy of Pediatrics Institute for Healthy Childhood Weight, and The Obesity Society. Plenary sessions presenting scientific evidence and clinical and payment practices were interspersed with breakout sessions to identify consensus recommendations.
Results
Consensus recommendations for childhood obesity treatment included: family-based multicomponent behavioral therapy; integrated care model; and multi-disciplinary care team. The use of evidence-based protocols, a well-trained healthcare team, medical oversight, and treatment at or above the minimum dose (e.g. >25 hours) are critical components to ensure effective delivery of high-quality care and to achieve clinically meaningful weight loss. Approaches to secure reimbursement for evidence-based obesity treatment within payment models were recommended.
Conclusion
Continued cross-sector collaboration is crucial to ensure a unified approach to increase payment and access for childhood obesity treatment and to scale-up training to ensure quality of care.
Keywords: childhood obesity, reimbursement, evidence-based treatment
Childhood obesity in the US has reached epidemic levels; nearly one in three children is overweight or has obesity.1,2 Obesity is a serious public health issue and is associated with immediate and long-term health problems for children.3–9 Childhood obesity incurs significant healthcare costs,10–12 and costs increase with the persistence of obesity into adolescence and adulthood.13–15 For example, children with obesity have more emergency room visits, higher prescription drug costs, and attend more specialist visits than peers who have normal weight.11,16 Indeed, childhood obesity appears to be driving increases in Medicaid spending.17
Most US children with obesity do not receive evidence-based care for obesity.18–23 In response to this problem, the United States Preventive Services Task Force (USPSTF), convened by the Agency for Healthcare Research and Quality (AHRQ) as authorized by Congress, conducted a rigorous literature review on childhood obesity screening (see Supplement 1) and recommended clinicians screen children aged 6 years and older for obesity and offer or refer them to comprehensive, intensive, behavioral interventions to promote improvements in weight status.24,25 This recommendation received a B grade from the USPSTF.26 As a result patients with obesity pay no deductibles or co-payments and do not participate in cost-sharing for these services as mandated by the Affordable Care Act (ACA) with the exception of grandfathered plans.27 Grandfathered plans are those that were in place as of March 23, 2010 and have remained in compliance with the criteria to maintain their grandfathered status. However, several barriers persist and impede widespread implementation of USPSTF-recommended care to treat childhood obesity. Improved care coordination, clinical-community integration, and inter-professional education to support care delivery within the healthcare system and community are needed to provide high-integrity, comprehensive, multicomponent treatment to the many children in need.19,20,22,28,29 Another important barrier to the implementation of recommended care is inadequate reimbursement for treatment.22,30 Despite substantial evidence that obesity warrants early and comprehensive treatment and is mandated by the ACA, many insurers do not provide coverage for childhood obesity treatment.21,23 When coverage is offered, it is often limited in scope and does not support treatments of adequate duration or breadth to effectively impact childhood obesity.21,23
To reduce barriers and realize the impact of effective treatment for childhood obesity, efforts are needed to accelerate implementation of the USPSTF recommendations and translate evidence into practice.24 To achieve this goal, multidisciplinary stakeholders in the fields of childhood obesity, policy, advocacy, and reimbursement must work collaboratively to: 1) develop feasible, acceptable, effective, and sustainable care delivery models supporting USPSTF recommendations and 2) create a unified strategy for policy change regarding reimbursement.
To this end, on July 9–10, 2015, the American Academy of Pediatrics (AAP) Institute for Healthy Childhood Weight, the Pediatric Obesity Section of The Obesity Society, and members of the Institute of Medicine’s Innovation Collaborative on Integrated Clinical and Social Systems for the Prevention and Treatment of Obesity hosted forty-three multidisciplinary, cross-sector stakeholders (clinicians, scientists, policy makers, representatives from advocacy organizations, and insurance industry leaders), plus a patient advocate and her parent at a meeting titled “Evidence-based childhood obesity treatment: Improving access and systems of care” (R13HS02281601). This working conference pursued the following aims: 1) advance the translation of evidence-based treatment for childhood obesity into routine clinical practice and 2) provide a forum in which key stakeholders could work collaboratively and partner with payers, foundations, professional organizations, and advocacy groups committed to forging a unified strategy for childhood obesity treatment reimbursement and disseminating the conference outcomes. The conference entailed pre-work (e.g., survey, webinar, state-of-the-field reading), a two-day meeting, and post-meeting synthesis.
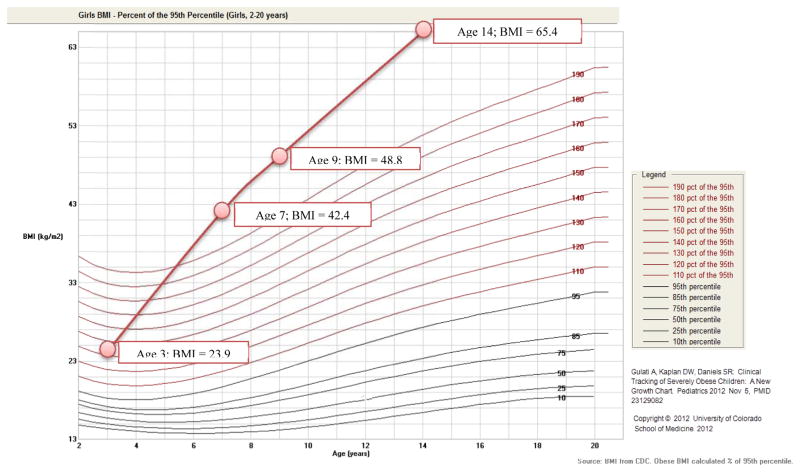
Figure 1 provides a case example from the conference’s patient advocate, Maria, illustrating the consequences of not receiving evidence-based care consistent with the USPSTF recommendations. Such consequences include psychosocial effects of bullying by peers and the experience of weight stigma from under-trained educational and healthcare professionals. Although Maria eventually advocated successfully for bariatric surgery, she and her mother describe how useful they found a multicomponent, family-based, behavioral intervention that they participated in when Maria was 9 years old. Unfortunately, program time limits prevented them from receiving the full dose of this intervention, and Maria continued to gain weight as illustrated by the growth chart reproduced in Figure 1.
Figure 1. The patient and parent perspective.
At 12 years old, Maria Caprigno* was told she would not live to see her 18th birthday because of her weight.
Maria’s story begins at 4 years old when she was told she had a “growth spurt” and was the size of a 7-year-old in her pediatrician’s office. This was the first notation in her medical record she was designated as “overweight.” Maria remembers feeling proud that day in her doctor’s office; at the time she did not understand “growth spurt” was the pediatrician’s positive spin on saying she was overweight. The figure below summarizes Maria’s childhood weight record graphed onto a BMI growth chart; all heights and weights were recorded at the pediatrician’s office.
Maria recalled the advice from her pediatrician and office staff being “nice and well-meaning” but provided no real guidance for weight management.
They would tell her to ride a bike, take a walk, and eat healthier, but Maria and her mother did not know how to implement that advice into their daily lives. At 4 years old, Maria and her mother started their pursuit of effective weight loss programs. During the next 7 years, Maria and her mother sought out treatment through four different hospital programs, two commercial programs, and one adult-centered gym, and all had limited results. All of Maria’s treatment was paid for out-of-pocket; none of the programs or interventions were reimbursable. The majority of programs she received were not evidence-based, and none were effective for Maria in maintaining weight loss long-term. Maria and her mother did complete one multicomponent, group- and family-based program for 12 weeks, which she and her mother found to be the most useful for making changes to their eating, exercise, and self-monitoring behaviors; however, they wished the program would have lasted longer. They participated in this program when Maria was 9 years old.
As a 12-year-old, Maria suffered unbearable weight-based stigma. She was shamed by her school’s administration. After a difficult encounter with the school nurse, she went home crying and became inspired to find a bariatric surgeon. Within a short period of time, she was in touch with a bariatric surgeon who agreed to meet with her. Over the next two years, Maria continued her journey to leading a healthier life. She was followed closely by a medical center in Boston, MA but was unable to have a surgical intervention there. After insurance denied coverage of her surgical case because she was deemed a high risk, Maria appealed to her insurance company saying she was willing to be a “guinea pig” since the several programs she tried previously were unable to help her achieve successful weight loss. On February 9, 2010, at 14 years old, Maria weighed 443 pounds. Grateful that the insurance company had approved the bariatric surgery, Maria underwent a sleeve gastrectomy. Maria is now 21 years old and is excitedly preparing for graduation from college as a Communications major and hopes to continue as a strong patient advocate for other suffering with obesity and its related stigma. Her bariatric surgery was five years ago, and she has lost more than 140 pounds.
Maria’s story illustrated the numerous barriers faced by pediatric patients with obesity in the healthcare system. Whereas effective behavioral interventions for childhood obesity exist, none of these were made available to Maria and her mother, or they did not last long enough create sustainable weight loss. Furthermore, even if they had been offered effective intervention, they would likely have had to pay for it out-of-pocket. Without effective interventions offered or provided when she was first identified with overweight at 4 years old, Maria continued to gain weight rapidly until bariatric surgery became her only option. She also experienced devastating bullying and stigma, which are both common psychosocial consequences in children with obesity. This story illustrates the necessity to provide evidence-based intervention to all children with obesity as early as possible to prevent additional weight gain and associated comorbidities and costs.
* Note that the patient and parent gave permission to be identified.
Source: Gulati AK, Kaplan DW, Daniels SR. Clinical tracking of severely obese children: A new growth chart. Pediatrics. 2012;130(6):1136–40. PubMed PMID: 23129082.
This report presents a model for childhood obesity treatment consistent with USPSTF recommendations as envisioned by the stakeholders at the conference and a review of payment models and systems discussed at the conference. Areas of consensus and major themes that emerged during the conference are discussed, as well as relevant background evidence and future directions to improve access and systems of care for children with obesity and their families. For the purposes of this conference “consensus” was defined as the “absence of strong dissent.” Additionally, the meeting organizers and attendees adopted the Chatham House Rule to allow speakers and participants anonymity and to serve as an aid to free discussion. The Chatham House Rule stipulates that “participants are free to use the information received, but neither the identity nor the affiliation of the speaker(s), nor that of any other participant, may be revealed”.31
Consensus on Effective Implementation of Childhood Obesity Treatment into Clinical Practice
The first part of the conference established consensus on the components and structure of evidence-based childhood obesity intervention. The attendees agreed that multicomponent interventions including dietary modifications, physical activity changes, behavioral strategies, and active parental involvement should be made routinely available to children with obesity. Attendees further agreed that these interventions should be delivered at the intensity and in a format consistent with USPSTF recommendations. Specifically, the USPSTF recommends that clinicians screen children aged 6 years and older for obesity and offer or refer children to an intensive, comprehensive behavioral intervention to promote improvement in weight status.24 Early intervention is important because less weight change is needed at younger ages to achieve a healthy weight compared to the amount of weight loss necessary at older ages.32 Interventions should be of moderate-to-high intensity and include dietary, physical activity, and behavioral counseling components. Moderate intensity is defined as = 26–75 contact hours, and high intensity >75 hours over at least 6- to 12-months.24 Reviews conducted since the publication of the USPSTF recommendation support the effectiveness of multicomponent treatments for overweight/obesity in children and the positive impact of treatment intensity on outcomes,33–35 including the positive impact of these interventions on cardiometabolic outcomes.33 These reviews, and the 2010 USPSTF report, note the importance of parental involvement in the efficacy of children’s weight loss interventions. Conference attendees explored ways to improve systems for care delivery to implement these recommendations by examining patient perspectives and reviewing evidence around existing treatment models. Important observations and recommendations were made during the conference regarding treatment approach, measurements of success, setting, and team composition and team members’ roles and training, as summarized below.
Family-Based Behavioral Treatment
Conference attendees reached consensus on the critical components of a family-based treatment model for children with obesity. Because of the effectiveness of family-based therapy (FBT) and its consistency with USPSTF recommendations, FBT was more closely examined as a promising multicomponent, moderate-to-high intensity childhood obesity treatment for translation into clinical settings. FBT has been studied for over 30 years and has repeatedly been shown to be effective in treating childhood obesity despite increases in both the severity and prevalence of obesity in children in an increasingly obesogenic environment.36 FBT takes a family-centered, comprehensive approach to behavior change to improve nutrition/dietary behaviors, promote physical activity, and reduce sedentary behaviors.36–44 In FBT, parents who are overweight or have obesity are assisted in achieving their own weight-loss goals in addition to all parents being taught positive parenting techniques such as contingency management (e.g., praise and reinforcement of the child’s behavioral change successes) and environmental control (e.g. modification of the home environment to increase access to healthy food and activity choices and decrease access to unhealthy options) to support their child in achieving and maintaining a healthy weight.35–37,45,46 FBT is designed to help parents and their children build and establish lasting changes in these behaviors through the application of self-regulatory skills (e.g., self-monitoring), behavioral economics, and social and learning theory principles to the practice of weight maintenance behaviors across multiple socio-environmental contexts (home, school, community, work, etc.).35–38,47–51 Programs such as FBT, in which parents are active participants in the intervention, result in superior child weight outcomes compared to interventions in which the parent is not encouraged to make their own behavioral changes. In a seminal study of FBT, children who were treated together with their parents showed significant decreases in relative weight at 10-year follow up, whereas children treated separately from their parents increased their weights.37 Parental weight loss is a robust predictor of child success in FBT, with evidence suggesting that parental influences on child weight outcomes occur through parental modeling of healthy behaviors and changes to the home environment.52 Treating children together with their parents is a more cost-effective approach than treating the parent or child separately.53
Integrated Chronic Care Model
While the evidence reviewed for the USPSTF recommendations shows treatment consisting of > 25 contact hours over at least 6–12 months can effectively yield improvements in weight status, conference attendees agreed that the treatment of obesity does not occur as an acute episode of care, and as such, the chronic care model should frame treatment given the impact obesity has across the lifespan.54 The chronic care model allows for the integration of follow-up visits for medical monitoring and maintenance of behavior change as needed, facilitates the provision of an intensity and frequency of treatment sufficient to achieve meaningful outcomes,24,25 and calls for clinic-community linkages.54,55
Treatment Format
Individual family or mixed-format approaches (i.e., some time with individual families and some group time) produce better treatment effects than group-only approaches,34,37,45,56 perhaps because the behavioral change components of treatment are better implemented when working with individual families. Therefore, conference attendees reached consensus on the need for taking an individualized approach to care that allows for the tailoring of treatment to patient or family needs and preferences. However, it was noted that including some group sessions may offer the opportunity for social support with and amongst children, families, and parents, and may improve cost-effectiveness.57
Outcome Measures
Conference attendees recommended that a menu of evidence-based individual and system-level measures be considered for tracking success, with the treatment team choosing the best measures based on the individualized plan for the patient. The primary indicator of success should be stabilization or reduction of relative weight measures (e.g., body mass index [BMI], BMI z-score, % weight above the 95th percentile), depending on the child’s age and obesity status, with a focus on achieving clinically significant weight changes. Cut-offs for clinically significant changes have been proposed (e.g., 0.25 or 0.5 BMI z-score decrease56,58,59) because weight changes of this magnitude have been associated with improvements in indicators of cardiometabolic functioning such as blood pressure, cholesterol levels, and HbA1c values, and improved psychosocial health.33,60,61 However, additional research is needed to further establish the degree of weight change necessary in children to achieve sustainable clinical benefits. In addition to weight stabilization, the consensus of the conference stakeholders was that other relevant treatment outcomes should be assessed and monitored to provide feedback on treatment progress for the clinician and family including measures assessing psychosocial functioning, biomedical outcomes, behavioral change, systems-level variables, and patient perspectives or attitudes (see examples in Table 1).
Table 1.
Examples of outcome measures for evidence-based childhood obesity treatment.
| Outcome | Outcome Examples |
|---|---|
| Patient-level Metrics | |
| Psychosocial Functioning |
|
| Biomedical Outcomes |
|
| Behavior Change |
|
| Family Metrics | |
| Family-level |
|
| Process Metrics | |
| Systems-level |
|
| Patient Experience of Treatment |
|
Outcomes listed are for illustrative purposes; measurements should not be limited to only those listed above. It was further recommended that measures of treatment response or success should be collected regularly and shared with the patient and treatment team members throughout the course of treatment.
Treatment Setting
There was a consensus that obesity treatment is ideally provided within an integrated system of care, which can be housed within a primary care practice medical home, a tertiary care center, or a community setting as part of the medical neighborhood.62 In 2011, the Centers for Medicare and Medicaid Services issued a Decision Memo for Intensive Behavioral Therapy for Obesity (CAG-00423N) which covers telephone-based counseling.63 Thus, virtual or telehealth technology may also be used to reach families who cannot easily travel for care as evidence emerges for its adherence and efficacy.54
Composition of the Care Delivery Team
A team approach should be adopted to facilitate an integrated system of care. Table 2 describes the team composition and roles of team members as envisioned by conference stakeholders. The core team members are a primary care provider with medical credentials who provides medical oversight, partnered with a behavioral interventionist trained in childhood obesity management who provides weight loss counseling. Access to sub-specialty care is critical,64 and sub-specialists can follow the AAP recommendations for monitoring comorbidities.65 Importantly, the sub-specialist interaction can be virtual to facilitate access to those geographically distant from the sub-specialty clinic so as not to widen health disparities.66 Conference attendees suggested that a care coordinator could facilitate the integration of care and communication from the referring primary care provider to the behavioral interventionist and sub-specialists as well as reduce fragmentation that can occur when multiple providers are involved in a patient’s care. Effective training practices are available for treatment teams, particularly behavioral interventionists, to deliver family-based childhood obesity treatments in a consistent and robust manner, but these must be scaled-up to increase access to evidence-based care.
Table 2.
Identified team roles for delivering family-based obesity treatment for children and adolescents.
| Team Member | Role | Suggested Types of Providers** |
|---|---|---|
| Pediatrician or primary care provider* |
|
|
| Behavioral interventionist* |
|
|
| Sub-specialist(s)* |
|
|
| Care coordinator |
|
|
Although required roles for treatment delivery are not explicitly stated in the USPSTF recommendations, these roles were identified among treatments deemed successful (i.e., >25 contact hours within 6 to 12 months, multicomponent, comprehensive).
Supervision or ongoing consultation might not be needed for all providers; however, implementation of evidence-based interventions in clinical settings have resulted in better treatment outcomes with implementation plans that include training to competency with ongoing supervision or consultation with an expert in the intervention. Additional roles that are not required but may be helpful include community outreach liaison, parent/patient advisory committee, and a business manager.
Provider Training
A lack of providers trained in evidence-based care for childhood obesity was listed in the pre-conference survey as a major barrier to the implementation of treatment consistent with USPSTF recommendations. Therefore, there was general agreement that comprehensive and consistent training should be made widely available to obesity treatment teams, with training specialized based on role (see Table 2). Although educational backgrounds for the behavioral interventionists were not explicitly detailed, cultural and developmental competencies were highlighted as requisites. Because effective methods for training interventionists have been employed in clinical research trials resulting in a reliable and reproducible intervention,35,36,46,67 the development of a standardized training, certification, and monitoring system to deliver evidence-based treatment in multiple settings was discussed. A number of dissemination and implementation studies have demonstrated that training novice providers to competency combined with ongoing consultation or supervision and coaching from experts can result in treatment outcomes consistent with those obtained in carefully controlled clinical trials.68–76
Consensus on the Access to and Payment for Effective Childhood Obesity Treatment
The second part of the conference established a consensus that despite the USPSTF recommendations, access to and reimbursement for evidence-based childhood obesity treatment is inconsistent and/or insufficient. Lack of reimbursement for childhood obesity treatment services was noted as a significant barrier to widespread implementation of childhood obesity treatment that complies with USPSTF recommendations. Conference attendees agreed that action-oriented dialog on the topic of childhood obesity treatment and reimbursement was long overdue. Indeed, one conference participant noted: “We feel and know that our children and families need better care – we need to push the field.” In response to the pre-conference survey, stakeholders agreed that the current reimbursement/insurance system, available financial resources and operating costs of the organization, and limited availability of quality training in USPSTF-recommended care are the most significant barriers to implementation (see Supplement 2), highlighting the need to create a unified strategy for policy change regarding payment for childhood obesity services, a primary focus of the conference.
Evidence for the Current Provision of Childhood Obesity Services
Evidence regarding the current provision and reimbursement of childhood obesity treatment services was reviewed during the conference. Despite the Affordable Care Act’s focus on prevention,77 obesity treatment services for children and adolescents remain scattered with little uniformity in the healthcare system. The lack of uptake or provision of such services by appropriate pediatric centers parallels the un-reimbursed or under-reimbursed financial history of services.22,23,78 Conference attendees reviewed data that examined the current landscape of childhood obesity treatment delivery. Specifically, the Children’s Hospital Association conducted a survey of children’s hospitals and pediatric departments in 2013 to assess the availability of comprehensive, multidisciplinary weight management services.78 Surveys were returned by 54% of the 218 children’s hospitals contacted, and of these, only 52 reported providing comprehensive, multidisciplinary weight management services for children consistent with USPSTF recommendations. However, there was little uniformity in program length. For example, 52% of programs reported treatment length of less than 20 weeks,78 illustrating the challenges to deliver the recommended duration of care. A major barrier highlighted by the survey was lack of payment for these services. For example, physicians were fully reimbursed by Medicaid 58% of the time and by commercial insurance 41% of the time. Other childhood obesity care team members (e.g., registered dietitians, behavioral counselors, exercise specialists) were reimbursed at significantly lower rates.78 Indeed, 84% of respondents reported that their weight management services ran at a financial loss, leading to the conclusion that weight management services are not financially self-sustaining.78
Reimbursement for behavioral health services affects both access to care and effectiveness, as illustrated by a study comparing different forms of coverage for smoking cessation.79 Full insurance coverage, including removal of copayments except those required for prescriptions, improved both access to smoking cessation programs and quit rates. These results highlight the importance of securing adequate payment for childhood obesity services to facilitate widespread and sustainable access to effective care. Accordingly, the remainder of the conference focused on: 1) understanding current payment models and their implications for childhood obesity services; 2) examining novel payment and treatment delivery systems from adult obesity and analogous childhood chronic conditions; 3) describing current and emerging payers; and 4) understanding how to advocate for payment for evidence-based care for childhood obesity through current payer systems.
Payment Models
In an effort to contain healthcare costs while improving quality of care, payment systems are evolving.20 Payment systems are moving from fee-for-service (FFS) models, which incentivize providers to perform more services leaving payers to shoulder financial risks, to payment models that emphasize quality over quantity of services and shift some financial risk to the provider80 (see Table 3). The evolution from FFS to shared risk payment models is illustrated by Medicare’s decision to boost the percentage of its payments devoted to alternative payment models from 20% in 2014 to 50% in 2018 while also increasing the proportion of FFS payments tied to quality or value (85% in 2016 and 90% in 2018).81
Table 3.
Post-conference synthesis on payment models and their application to childhood obesity.
| Category 1: Fee-For-Service (No Link to Quality) | Category 2: Fee-For-Service (Linked to Quality) | Category 3: Alternate Payment Models on Fee-For-Service Architecture (e.g., Bundled Payment) | Category 4: Population-Based Payment (e.g., Comprehensive Care Payment) | |
|---|---|---|---|---|
| Description |
|
|
|
|
| Application to Childhood Obesity |
|
|
|
|
Adapted from “Center for Medicaid Innovation Center Update”; Rajkumar R, Conway PH, Tavenner M. The CMS – Engaging Multiple Payers in Risk-Sharing Models. JAMA. Doi:10.1001/jama.2014.3703).
During the conference, rich discussions among participants were facilitated in multiple small breakout groups (see Supplement 3 for discussions guides). Conference attendees concluded that alternative payment models could better support the integration of behavioral health and medical care related to childhood obesity treatment than traditional FFS models.82 Conference stakeholders explored the design and implementation of new payment models conducive to reimbursement for evidence-based obesity treatment for children within a chronic care model. However, multiple challenges to designing and implementing new payment systems were identified at the conference. These include how best to bundle payments, settle the payment amount, assure quality healthcare for patients, and align incentives through multiple payers,83 all of which will need to be addressed as they apply to childhood obesity.
Relevant Examples of Current and Future Delivery Models
Whereas conference attendees noted that alternative payment models would best facilitate the routine delivery of USPSTF-recommended care for childhood obesity, it was acknowledged that such changes require concomitant shifts in care delivery systems. Thus, during the conference, attendees discussed recent innovations in payment models and systems of care from adult obesity and analogous conditions that can be applied to the evidence-based intervention for childhood obesity. Three examples were highlighted at the conference, as follows.
Centers of Excellence
The treatment of autism spectrum disorders (ASD) provides an analog condition because the need for ongoing, dedicated, specialized interdisciplinary services is similar to the needs required to successfully address childhood obesity. For instance, significant strides have been made to improve access to care for children living in Missouri with ASD through a state-level model of collaborative care using a Centers of Excellence (COE) approach. Developing a COE for the treatment of childhood obesity could be an important next step to improving availability of high-quality care. The expansion of current regional centers and creation of new centers for childhood obesity could tailor care to include more intensive services for complex cases of childhood obesity while possibly containing costs, as was illustrated in the treatment of ASD in Missouri.84 The development of the COE for ASD involved state leaders targeting legislative action to improve funding for ASD services in part due to advocacy from parents/caregivers and healthcare professionals. The conference attendees discussed the importance of securing similarly comprehensive, integrated services for childhood obesity that will require parents, providers, and other advocates working to counter societal weight bias and stigma and other barriers to these services.
Integrating Community-Based Services with Healthcare
A promising example of incorporating chronic disease prevention into routine practice is the effort to adapt the Diabetes Prevention Program (DPP) for use in YMCAs85 and other settings. The DPP is an intensive lifestyle intervention for adults at risk of developing diabetes. DPP has demonstrated efficacy86; however, its intensity makes it difficult to implement in busy healthcare settings. Investigators thus examined the feasibility of implementing the program in YMCAs, and a pilot program demonstrated its feasibility and effectiveness,87 which led to an expansion of the program to more than 70 YMCA organizations as well as a partnership between the YMCA and the UnitedHealthcare group. The partnership in turn created a system of payment for participants in the YMCA’s program to help ensure program sustainability.87–89 Importantly, in this adult prevention program, care is delivered by trained instructors who receive on-going supervision. Conference attendees identified this training model as an extension of care that holds promise for childhood obesity services as long as interventionists are trained by experts in the treatment and have on-going treatment oversight. Additionally, the value-based payment from some insurers may be successfully applied with a key to reimbursement being patients meeting weight loss goals.
Integrated Behavioral and Physical Healthcare
An example of an innovative payment model comes from New York State’s Medicaid Waiver.90 In April 2014, the Centers for Medicare and Medicaid Services (CMS) and New York created a groundbreaking waiver allowing the State to reinvest eight billion dollars generated by Medicaid Redesign Team reforms into a Delivery System Reform Incentive Payment program. The intention of this Medicaid redesign was to create a Value-Based Payment system. The Roadmap for this plan presents a model for three types of integrated care: Integrated Primary Care (e.g., Patient-Centered Medical Home, behavioral health primary care, management of chronic illness); Episodic Care Services (specialized services for a particular condition and time such as maternity care, hip replacement); and Specialized Continuous Care Services for individuals needing ongoing, dedicated, specialized multidisciplinary services for a health problem/condition. Supplement 4 illustrates how the New York Medicaid program will implement value-based payment and offers a population health focus. The model depicted in the supplement includes specific areas where childhood obesity care could be implemented and be eligible for payment. Because the conference consensus was that evidence-based obesity treatment services for children/adolescents could be both episodic and chronic, these services could be delivered and reimbursed the same way as other chronic diseases.
Current Payer Systems
Payers for healthcare services fall into four broad categories: government-sponsored such as Medicaid; commercial plans such as those offered through employers; Accountable Care Organizations (ACOs); and large employer groups. Each is defined in Table 4. The potential capacity or motivation of each healthcare service to address childhood obesity is described in more detail below. Addressing obesity is imperative for the health and well-being of all children with obesity and their families. Importantly, minority populations are disproportionately affected with obesity (i.e., for 6–11 year-old children, Latinos have a 25.0% obesity prevalence, African Americans, 21.4%, and Whites, 13.6%,91 thus confronting these disparities could help contain the increasing healthcare costs associated with obesity.
Table 4.
Defining payer or payment systems involved with child healthcare.
| Payer or System | Definition |
|---|---|
| Medicaid |
|
| Children’s Health Insurance Program (CHIP) & Medicaid Managed Care |
|
| Commercial |
|
| Accountable Care Organizations (ACO) |
|
| Large Employer Groups |
|
Medicaid
Medicaid pays for some treatment services for children with obesity, but the amount or frequency of those payments is historically lower than that of commercial plans.80,92 Also, Medicaid programs vary across states with respect to benefit coverage, delivery systems, and administration.93 The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit represents a viable means to cover most, if not all, of childhood obesity treatment services94 (see Supplement 5). Ultimately, the goal of EPSDT is to deliver the right care to the right child at the right time in the right setting. Many states are not leveraging EPSDT programs to treat childhood overweight and obesity95 and exclude some sub-specialists (e.g., registered dietitians) and settings from coverage.
Children’s Health Insurance Program (CHIP)
CMS administers the Children’s Health Insurance Program (CHIP), which provides low-cost healthcare to children in households that earn too much to qualify for regular Medicaid. The income levels vary by state, and care can be paid directly by state Medicaid or by a private insurer’s managed care organization. Both Medicaid and CHIP programs cover a range of services to prevent and reduce obesity, including behavioral counseling, medication, and surgery.96,97 CHIP and Medicaid Managed Care plans typically have a more narrow scope of coverage than the EPSDT services defined under Medicaid. Medicaid and CHIP represent the payers covering the greatest number of underserved and minority children, who are also the children with the highest obesity prevalence. Therefore, it was acknowledged that these programs would have more challenges providing the full amount of reimbursement for delivery of the level of care that has been associated with the most robust weight loss outcomes (i.e., intensive, family-based behavioral interventions).
Commercial Plans
Approximately 50% of children nationwide are covered as dependents by employer-sponsored health insurance.98 Basic services including well-child visits are covered under these plans. Diet and nutrition counseling services for weight management are typically covered as routine visits; however, these visits may be reimbursed only at routine physician visit rates. Nutrition counseling and weight loss services are sometimes excluded from coverage, and multispecialty comprehensive programs still face barriers to coverage. For example, currently only 48% of large firms and 18% of small firms provide weight loss services for employees.98 These services are often provided as an add-on benefit outside of regular coverage (e.g., through contract with a health plan or third party). Offering services to children is rare. Conference attendees discussed that to facilitate payment for childhood obesity services from commercial payers, it is necessary to explain that childhood obesity treatment is an important family health intervention to reduce childhood morbidity and chronic adult disease.
Accountable Care Organizations
Accountable Care Organizations (ACOs) are groups of doctors, hospitals, and other healthcare providers who come together voluntarily and accept shared accountability for the cost and quality of care provided to a population of patients.99 Accordingly, the focus of ACOs is on containing high-cost services, such as emergency room visits, especially among chronically ill patients.100 Because untreated or undertreated childhood obesity is associated with increased short-term medical costs (e.g., medications, specialty care),10 and because these costs continue to rise as obesity tracks into adulthood for these children,101 reimbursing for childhood obesity treatment presents an opportunity for ACOs to invest in care that would potentially lead to lower lifetime medical costs. Moreover, the demonstrated cost savings of treating both the child with obesity and adults in the child’s family52 could provide financial incentive for ACOs to provide payment for evidence-based childhood obesity treatment.
Large Employer Groups
Large employer groups represent companies or collections of businesses that choose to self-insure with or without the use of a commercial plan as a third party administrator of their health benefit. Therefore, similar to commercial plans, they typically cover children as dependents. Employer groups are interested in a more productive work force; thus, it may be helpful to frame obesity treatment as an opportunity to target parents’ weight loss in treatment along with their children37,53 and thus employees will likely experience health benefits as well.
Summary of Payment Discussion
Access to and reimbursement for evidence-based childhood obesity treatment is inconsistent and/or insufficient despite the fact that the USPSTF has endorsed obesity screening and either offering or referring intensive behavioral interventions for the treatment of childhood obesity with a grade B recommendation. The ACA specifically states that all services designated with a grade A or B MUST be covered without copayment by private health insurance plans,26 with exception to grandfathered plans. Healthcare reform is creating opportunities for moving rapidly toward payment models and care delivery systems conducive to the provision of evidence-based childhood obesity treatment, and all payers have a stake in this discussion. Demonstration projects involving full fee-for-service payment of the USPSTF recommended level of care should be conducted by all payers (Medicaid and private) in a region or state to allow for the determination of baseline costs from which to build alternative payment models. At the meeting, the parent advocate noted that all of the programs were paid for out-of-pocket and “at times I stopped looking for programs due to the expense.”
Advocacy Recommendations and Next Steps for the Field
The synergy of multiple stakeholders across the continuum of research, clinical care, policy, payment, and patients was clearly evident at the conference and produced consensus on the steps needed to operationalize the USPSTF treatment recommendations. Our parent advocate stated she often felt medical professionals did not discuss obesity because of discomfort with parental obesity. However, it will be important for parents/caregivers, employers, and policy makers to overcome the weight stigma and bias that can interfere with the vigorous advocacy needed to improve access to evidence-based care for childhood obesity.102,103 An important outcome of this conference was the development of advocacy strategies that can be developed into tools to support efforts for improved reimbursement for evidence-based childhood obesity treatment (see Table 5). When advocating for greater access to care, key talking points will need to be adjusted to fit the payer being approached,104,105 especially in the case of Medicaid because coverage varies across states. However, some general critical points to highlight across payers when advocating for greater access to care include: 1) the adverse effects of childhood obesity on health and healthcare costs; 2) existence of an evidence-based, effective behavioral intervention for childhood obesity; 3) treatment results that produce clinically significant weight change and other patient-centered improvements, such as physical functioning and quality of life; and 4) parents are actively targeted in family-based treatment and therefore the parent who is overweight or has obesity also may lose weight,106 expanding the reach of the intervention beyond the target child and likely further improving the cost-effectiveness of treatment.
Table 5.
Key points for use when advocating for the reimbursement of childhood obesity treatment with payers.
| Key Advocacy Points | |
|---|---|
| Efficacy |
|
| Patient-Related Variables |
|
| Return on Investment |
|
| Mandate |
|
USPSTF = United States Preventive Services Task Force; EPSDT = Early and Periodic Screening, Diagnostic and Treatment
As evidence-based care is translated and implemented in clinical settings, it is critical to use systematic methods including the use of standardized curricula, training of interventionists, and ongoing fidelity checks and medical oversight to ensure effective delivery of high quality care. Healthcare providers play an important role in engaging parents and patients in advocating for better access to and reimbursement for childhood obesity treatment. Providers must first engage the healthcare system (e.g. pediatric departments, children’s hospitals) to advocate for assembling the appropriate obesity management resources needed to develop and offer these services to their pediatric patients. Advocates (i.e. patients/families, providers, private and public payers, and health systems) must work together to encourage full coverage of these required services. Clinical care needs to be delivered by a well-trained team which includes supervised, and perhaps certified, behavioral interventionists to achieve clinically significant weight outcomes. To this end, conference consensus identified the skills needed to deliver the treatment and suggested types of providers (see Table 2), with training to competency being the most critical component for providers. Finally, in discussions with payers, it is critical to highlight the long-term payoff of providing treatment to children to prevent obesity tracking into adulthood, the prevention of which benefits both population health and cost savings. Advocating for the inclusion of an evaluative component to any payment or healthcare system innovation should also be considered to better understand and document the impact and effectiveness of these innovations on childhood obesity treatment.20
Conclusion
This conference and the present report represent an important first step in assuring that children and their families have access to evidence-based behavioral treatment for obesity. As one participant noted during discussion, the primary reason for attending this conference was to bring forward the passion and drive for translating what we know into what we do and forging the link between health and clinical medicine. Continued collaboration between stakeholders will be crucial to create a unified approach to payment for childhood obesity treatment that is of sufficient intensity and to scale-up training in the delivery of treatment with competency and consistency. Advancing efforts to secure payment for USPSTF-recommended childhood obesity care is critical, and this conference report provides a necessary first step towards achieving this goal. The AAP and many of the organizations participating in this conference have expressed commitment to continuing the implementation, dissemination, training, and advocacy needed to improve access to effective care for childhood obesity.
Supplementary Material
Acknowledgments
FUNDING:
-
Conference supported by R13HS02281601: “Evidence-based childhood obesity treatment: Improving access and systems of care” from the Agency for Healthcare Research and Quality.
Funding amount matched by American Academy of Pediatrics—Institute for Healthy Childhood Weight.
DEW and MA are supported by T32HL00745629: “Nutrition-behavioral cardiovascular disease prevention” from the National Heart, Lung, and Blood Institute of the National Institutes of Health.
DEW is supported by K24MH07044610: “Clinical research in eating disorders and obesity” from the National Institute of Mental Health of the National Institutes of Health.
DEW and AL are supported by the Scott Rudolph Endowed University Professorship from the Washington University School of Medicine in St. Louis.
AES is supported, in part, by the U54GM104940 grant from the National Institute of General Medical Sciences of the National Institutes of Health which funds the Louisiana Clinical and Translational Science Center.
The Improving Access and Systems of Care for Evidence-Based Childhood Obesity Treatment Conference Workgroup consisted of the following:
Foundations/Institutes: Ryan Barker, MSW, MPPA, VP of Health Policy, Missouri Foundation of Health; Romana Hasnain-Wynia, MS, PhD, Program Director for Addressing Disparities, Patient-Centered Outcomes Research Institute; Elizabeth Vegas, Director, Industry initiative, attended on behalf of Jenny Bogard, Director, Healthcare Initiative; Shale Wong, MD, MSPH, Senior Program Consultant & Professor of Pediatrics, Robert Wood Johnson Foundation & University of Colorado School of Medicine.
Government/Payers: Douglas G. Fish, MD, Medical Director, Division of Program Development & Management, New York State Department of Health; Jennifer Foltz, MD, MPH, USPHS Medical Epidemiologist, Centers for Disease Control & Prevention; Stewart Gordon, MD, FAAP, Chief Medical Officer, Louisiana Healthcare Connections/Centene; Robert Mendonsa, MBA, CPA, Deputy Administrator Care Coordination for Rate and Finance, Illinois Department of Healthcare & Family Services; Samar Muzaffar, MD, MPH, Medical Director, Missouri HealthNet; Elizabeth O’Connor, PhD, Kaiser Permanente Research Affiliates Evidence-Based Practice Center, The Center for Health Research, Kaiser Permanente; Edmund Pezalla, MD, MPH, VP, National Medical Director for Pharmacy Policy and Strategy, Aetna; Darshak Sanghavi, MD, Director, Preventive and Population Health Models Group, Center for Medicare and Medicaid Innovation/Centers for Medicare & Medicaid Services; Deirdra Stockmann, PhD, Presidential Management Fellow & Health Insurance Specialist, Centers for Medicare and Medicaid Services; Barry Zallen, MD, Chief Medical Officer, Children’s Hospital Integrated Care Organization (CHICO).
Hospitals: Ihuoma Eneli, MD, Professor of Pediatrics, Director of the Center for Healthy Weight & Nutrition, The Ohio State University/Nationwide Children’s Hospital; Sarah Hampl, MD, General Pediatrics and Weight Management, Children’s Mercy Kansas City, Associate Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Susan Schuh, Director, Planning & Business Development, Physician Services, and Transplant Financial Services, St. Louis Children’s Hospital; Karen Seaver Hill, Director, Community and Child Health, Children’s Hospital Association.
Non-profit Organizations and Professional Associations: Cedric Bryant, PhD, FACSM, Chief Science Officer, American Council on Exercise; Lynn Bufka, PhD, Associate Executive Director of Practice, Research and Policy, American Psychological Association; Matt Longjohn, MD, MPH, National Health Officer, YMCA of the USA; Annalia Glenn Michelman, JD, MPP, Senior Legislative Attorney, American Medical Association; Francesca M. Dea, MBA, CAE, Executive Director, The Obesity Society; Marsha Schofield, MS, RD, LD, FAND, Director, Nutrition Services Coverage, Academy of Nutrition and Dietetics.
Policy/Advocacy: Alison Baker, MS, Director, Division of Safety & Health Promotion, American Academy of Pediatrics; Maria Caprigno, Patient Advocate; Terry Caprigno, Patient Advocate; Christine Ferguson, JD, Principal, Leverage Global Consulting; Chris Gallagher, Washington Coordinator, Obesity Care Continuum; Janice Liebhart, MS, Evaluation Manager, American Academy of Pediatrics Institute for Childhood Healthy Weight; Joe Nadglowski, President/CEO, Obesity Action Coalition; Corrie Pierce, Program Coordinator, American Academy of Pediatrics Institute for Childhood Healthy Weight.
Universities: Eric Armbrecht, PhD, Associate Professor, Saint Louis University Center for Outcomes Research, School of Medicine, College for Public Health & Social Justice; Sarah Barlow, MD, MPH, Director of the Center for Childhood Obesity, Associate Professor of Pediatrics, Texas Children’s Hospital and Baylor College of Medicine; Sue Curry, PhD, Dean, College of Public Health Distinguished Professor of Health Management and Policy, University of Iowa; Leonard Epstein, PhD, SUNY Distinguished Professor and Chief of Behavioral Medicine, University at Buffalo-SUNY; Janet Farmer, PhD, Associate Dean for Research, School of Health Professions, University of Missouri; Tim McBride, PhD, Professor, Brown School, Washington University in Saint Louis; Sara McMullin, BA, Clinical Research Coordinator, Washington University School of Medicine; Deborah Parra-Medina, PhD, MPH, Professor of Epidemiology and Biostatistics, University of Texas Health Science Center at San Antonio; Dana Rofey, PhD, Assistant Professor of Psychiatry, Pediatrics & Psychology, University of Pittsburgh School of Medicine; Dorothy Van Buren, PhD, Assistant Professor, Washington University School of Medicine.
We would like to thank Brad Sperber of the Keystone Policy Center, our conference facilitator, for his efforts in guiding our conversations in an efficient and effective manner.
We also thank and acknowledge Tim McBride, PhD, for his work in conjunction with the Center for Diabetes Translation Research and Center for Health Economics and Policy at Washington University.
Footnotes
AUTHOR CONTRIBUTIONS: DEW and SC equally contributed to the implementation of the conference and the corresponding materials created as a result of the conference.
DISCLOSURE: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. JLF’s participation does not constitute an endorsement for any advocacy or funding statements.
Contributor Information
Denise E. Wilfley, Department of Psychiatry, Washington University School of Medicine, St. Louis, MO.
Amanda E. Staiano, Pennington Biomedical Research Center; Baton Rouge, LA.
Myra Altman, Department of Psychiatry, Washington University School of Medicine, St. Louis, MO.
Jeanne Lindros, Institute for Healthy Childhood Weight, American Academy of Pediatrics, Chicago, IL.
Angela Lima, Department of Psychiatry, Washington University School of Medicine, St. Louis, MO.
Sandra G. Hassink, American Academy of Pediatrics Institute for Healthy Childhood Weight, Chicago, IL.
William H. Dietz, Redstone Global Center for Prevention and Wellness, Milken Institute School of Public Health, Washington, D.C..
Stephen Cook, Golisano Children’s Hospital, University of Rochester Medical Center, Rochester, NY.
References
- 1.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8. [PubMed] [Google Scholar]
- 2.Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999–2014. Obesity (Silver Spring) 2016;24(5):1116–1123. doi: 10.1002/oby.21497. [DOI] [PubMed] [Google Scholar]
- 3.BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: effects of race and ethnicity. Pediatrics. 2009;123:697–702. doi: 10.1542/peds.2008-0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dietz WH. Health Consequences of Obesity in Youth: Childhood Predictors of Adult Disease. Pediatrics. 1998;101(Supplement 2):518–525. [PubMed] [Google Scholar]
- 5.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6):1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 6.Gilliland FD, Berhane K, Islam T, et al. Obesity and the risk of newly diagnosed asthma in school-age children. Am J Epidemiol. 2003;158(5):406–415. doi: 10.1093/aje/kwg175. [DOI] [PubMed] [Google Scholar]
- 7.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx WJH, Zitman FG. Overweight, Obesity, and Depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2013;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 8.Reilly JJ, Methven E, McDowell ZC, et al. Health consequences of obesity. Arch Dis Child. 2003;88(9):748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360(9331):473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 10.Hampl SE, Carroll Ca, Simon SD, Sharma V. Resource utilization and expenditures for overweight and obese children. Arch Pediatr Adolesc Med. 2007;161:11–14. doi: 10.1001/archpedi.161.1.11. [DOI] [PubMed] [Google Scholar]
- 11.Trasande L, Samprit C. The Impact of Obesity on Health Service Utilization and Costs in Childhood. Obesity (Silver Spring) 2009;17(9):1749–1754. doi: 10.1038/oby.2009.67. [DOI] [PubMed] [Google Scholar]
- 12.Finkelstein EA, Graham WC, Malhotra R. Lifetime direct medical costs of childhood obesity. Pediatrics. 2014;133(5):854–862. doi: 10.1542/peds.2014-0063. [DOI] [PubMed] [Google Scholar]
- 13.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: The Bogalusa Heart Study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 14.Lynch BA, Finney Rutten LJ, Jacobson RM, et al. Health Care Utilization by Body Mass Index in a Pediatric Population. Acad Pediatr. 2015;15(6):644–650. doi: 10.1016/j.acap.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang LY, Chyen D, Lee S, Lowry R. The association between body mass index in adolescence and obesity in adulthood. J Adolesc Health. 2008;42(5):512–518. doi: 10.1016/j.jadohealth.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Buescher PA, Whitmire JT, Plescia M. Relationship between body mass index and medical care expenditures for North Carolina adolescents enrolled in Medicaid in 2004. Prev Chronic Dis. 2008;5(1):A04. [PMC free article] [PubMed] [Google Scholar]
- 17.Trasande L, Liu Y, Fryer G, Weitzman M. Effects of childhood obesity on hospital care and costs, 1999–2005. Health Aff (Millwood) 2009;28(4):w751–760. doi: 10.1377/hlthaff.28.4.w751. [DOI] [PubMed] [Google Scholar]
- 18.Cook S, Weitzman M, Auinger P, Barlow SE. Screening and counseling associated with obesity diagnosis in a national survey of ambulatory pediatric visits. Pediatrics. 2005;116(1):112–116. doi: 10.1542/peds.2004-1517. [DOI] [PubMed] [Google Scholar]
- 19.Kolagotla L, Adams William. Ambulatory management of childhood obesity. Obes Res. 2004;12(2):275–283. doi: 10.1038/oby.2004.35. [DOI] [PubMed] [Google Scholar]
- 20.Perrin EM, Flower KB, Garrett J, Ammerman AS. Preventing and treating obesity: pediatricians’ self-efficacy, barriers, resources, and advocacy. Ambul Pediatr. 2005;5(3):150–156. doi: 10.1367/A04-104R.1. [DOI] [PubMed] [Google Scholar]
- 21.Simpson LA, Cooper J. Paying for obesity: a changing landscape. Pediatrics. 2009;123(Suppl 5):S301–307. doi: 10.1542/peds.2008-2780I. [DOI] [PubMed] [Google Scholar]
- 22.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110(1 Pt 2):210–214. [PubMed] [Google Scholar]
- 23.Tershakovec AM, Watson MH, Wenner WJ, Jr, Marx AL. Insurance reimbursement for the treatment of obesity in children. J Pediatr. 1999;134(5):573–578. doi: 10.1016/s0022-3476(99)70243-x. [DOI] [PubMed] [Google Scholar]
- 24.Barton M. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125(2):361–367. doi: 10.1542/peds.2009-2037. [DOI] [PubMed] [Google Scholar]
- 25.Whitlock EP, O’Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125(2):e396–418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 26.Melnyk BM, Grossman DC, Chou R, et al. USPSTF perspective on evidence-based preventive recommendations for children. Pediatrics. 2012;130(2):e399–407. doi: 10.1542/peds.2011-2087. [DOI] [PubMed] [Google Scholar]
- 27.Tolbert J. The Coverage Provisions in the Affordable Care Act: An Update. Kaiser Family Foundation; 2015. [Google Scholar]
- 28.Klein JD, Sesselberg TS, Johnson MS, et al. Adoption of Body Mass Index Guidelines for Screening and Counseling In Pediatric Practice. Pediatrics. 2010;125(2):265–272. doi: 10.1542/peds.2008-2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Gerwen M, Franc C, Rosman S, Le Vaillant M, Pelletier-Fleury N. Primary care physicians’ knowledge, attitudes, beliefs and practices regarding childhood obesity: a systematic review. Obes Rev. 2009;10(2):227–236. doi: 10.1111/j.1467-789X.2008.00532.x. [DOI] [PubMed] [Google Scholar]
- 30.Caprio S. Treating child obesity and associated medical conditions. Future Child. 2006;16(1):209–224. doi: 10.1353/foc.2006.0002. [DOI] [PubMed] [Google Scholar]
- 31.Chatham House Rule. Chathamhouse.org; [Accessed 8/17/2016]. Chatham House: The Royal Institute of International Affairs. https://www.chathamhouse.org/about/chatham-house-rule. [Google Scholar]
- 32.Goldschmidt AB, Wilfley DE, Paluch RA, Roemmich JN, Epstein LH. Indicated prevention of adult obesity: how much weight change is necessary for normalization of weight status in children? JAMA Pediatr. 2012:1–6. doi: 10.1001/jamapediatrics.2013.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ho M, Garnett SP, Baur L, et al. Effectiveness of Lifestyle Interventions in Child Obesity: Systematic Review With Meta-analysis. Pediatrics. 2012;130(6):e1647–e1671. doi: 10.1542/peds.2012-1176. [DOI] [PubMed] [Google Scholar]
- 34.Janicke DM, Steele RG, Gayes LA, et al. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. J Pediatr Psychol. 2014;39(8):809–825. doi: 10.1093/jpepsy/jsu023. [DOI] [PubMed] [Google Scholar]
- 35.Wilfley DE, Stein RI, Saelens BE, et al. Efficacy of maintenance treatment approaches for childhood overweight: a randomized controlled trial. JAMA. 2007;298(14):1661–1673. doi: 10.1001/jama.298.14.1661. [DOI] [PubMed] [Google Scholar]
- 36.Epstein LH, Paluch RA, Roemmich JN, Beecher MD. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychol. 2007;26(4):381–391. doi: 10.1037/0278-6133.26.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA. 1990;264:2519–2523. [PubMed] [Google Scholar]
- 38.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154(3):220–226. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 39.Epstein LH, Valoski AM, Vara LS, et al. Effects of decreasing sedentary behavior and increasing activity on weight change in obese children. Health Psychol. 1995;14(2):109–115. doi: 10.1037//0278-6133.14.2.109. [DOI] [PubMed] [Google Scholar]
- 40.Epstein LH, Paluch RA, Beecher MD, Roemmich JN. Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity (Silver Spring) 2008;16(2):318–326. doi: 10.1038/oby.2007.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Epstein LH, Paluch RA, Gordy CC, Saelens BE, Ernst MM. Problem solving in the treatment of childhood obesity. J Consult Clin Psychol. 2000;68(4):717–721. [PubMed] [Google Scholar]
- 42.Epstein LH. Development of evidence-based treatments for pediatric obesity. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford Publications; 2003. pp. 374–388. [Google Scholar]
- 43.Epstein LH, Wing RR, Koeske R, Ossip DJ, Beck S. A comparison of lifestyle change and programmed aerobic exercise on weight and fitness changes in obese children. Behavior Therapy. 1982;13:651–665. [Google Scholar]
- 44.Epstein LH, Wing RR, Koeske R, Valoski A. A comparison of lifestyle exercise, aerobic exercise and calisthenics on weight loss in obese children. Behavior Therapy. 1985;16:345–356. [Google Scholar]
- 45.Altman M, Cahill Holland J, Lundeen D, et al. Reduction in food away from home is associated with improved child relative weight and body composition outcomes and this relation is mediated by changes in diet quality. J Acad Nutr Diet. 2015;115(9):1400–1407. doi: 10.1016/j.jand.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Holland JC, Kolko RP, Stein RI, et al. Modifications in parent feeding practices and child diet during family-based behavioral treatment improve child zBMI. Obesity (Silver Spring) 2014;22(5):E119–126. doi: 10.1002/oby.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Daniel TO, Stanton CM, Epstein LH. The future is now: comparing the effect of episodic future thinking on impulsivity in lean and obese individuals. Appetite. 2013;71:120–125. doi: 10.1016/j.appet.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Daniel TO, Stanton CM, Epstein LH. The future is now: reducing impulsivity and energy intake using episodic future thinking. Psychol Sci. 2013;24(11):2339–2342. doi: 10.1177/0956797613488780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Daniel TO, Said M, Stanton CM, Epstein LH. Episodic future thinking reduces delay discounting and energy intake in children. Eat Behav. 2015;18:20–24. doi: 10.1016/j.eatbeh.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lin H, Epstein LH. Living in the moment: effects of time perspective and emotional valence of episodic thinking on delay discounting. Behav Neurosci. 2014;128(1):12–19. doi: 10.1037/a0035705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilfley DE. Using basic behavioral science to develop more effective obesity treatments. Academy of Behavioral Medicine Research annual meeting; 2015; Cambridge, MD. [Google Scholar]
- 52.Best JR, Goldschmidt AB, Mockus-Valenzuela DS, Stein RI, Epstein LH, Wilfley DE. Shared weight and dietary changes in parent-child dyads following family-based obesity treatment. Health Psychol. 2016;35(1):92–95. doi: 10.1037/hea0000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Epstein LH, Paluch RA, Wrotniak BH, et al. Cost-effectiveness of family-based group treatment for child and parental obesity. Child Obes. 2014;10(2):114–121. doi: 10.1089/chi.2013.0123. [DOI] [PubMed] [Google Scholar]
- 54.Dietz WH, Solomon LS, Pronk N, et al. An Integrated Framework For The Prevention And Treatment Of Obesity And Its Related Chronic Diseases. Health Aff (Millwood) 2015;34(9):1456–1463. doi: 10.1377/hlthaff.2015.0371. [DOI] [PubMed] [Google Scholar]
- 55.Foltz JL, Belay B, Dooyema CA, Williams N, Blanck HM. Childhood Obesity Research Demonstration (CORD): the cross-site overview and opportunities for interventions addressing obesity community-wide. Child Obes. 2015;11(1):4–10. doi: 10.1089/chi.2014.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reinehr T, Andler W. Changes in the atherogenic risk factor profile according to degree of weight loss. Arch Dis Child. 2004;89(5):419–422. doi: 10.1136/adc.2003.028803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hayes JF, Altman M, Coppock JH, Wilfley DE, Goldschmidt AB. Recent Updates on the Efficacy of Group-Based Treatments for Pediatric Obesity. Curr Cardiovasc Risk Rep. 2015;9(4):1–10. doi: 10.1007/s12170-015-0443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ford AL, Hunt LP, Cooper A, Shield JP. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child. 2010;95(4):256–261. doi: 10.1136/adc.2009.165340. [DOI] [PubMed] [Google Scholar]
- 59.Hunt LP, Ford AL, Sabin MA, Crowne EC, Shield JPH. Clinical measures of adiposity and percentage fat loss: which measure most accurately reflects fat loss and what should we aim for? Arch Dis Child. 2007;92(5):399–403. doi: 10.1136/adc.2006.103986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kalarchian MA, Levine MD, Arslanian SA, et al. Family-Based Treatment of Severe Pediatric Obesity: Randomized, Controlled Trial. Pediatrics. 2009;124(4):1060–1068. doi: 10.1542/peds.2008-3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wilfley D, Berkowitz R, Goebel-Fabbri A, et al. Binge eating, mood, and quality of life in youth with type 2 diabetes: baseline data from the today study. Diabetes Care. 2011;34(4):858–860. doi: 10.2337/dc10-1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cheak-Zamora NC, Farmer JE. The impact of the medical home on access to care for children with autism spectrum disorders. J Autism Dev Disord. 2015;45(3):636–644. doi: 10.1007/s10803-014-2218-3. [DOI] [PubMed] [Google Scholar]
- 63.Centers for Medicare & Medicaid Services. Decision Memo for Intensive Behavioral Therapy for Obesity (CAG-00423N) [Accessed 8/17/2016];CMS.gov. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=253.
- 64.Kirk S, Woo JG, Jones MN, Siegel RM. Increased frequency of dietitian visits is associated with improved body mass index outcomes in obese youth participating in a comprehensive pediatric weight management program. Child Obes. 2015;11(2):202–208. doi: 10.1089/chi.2014.0079. [DOI] [PubMed] [Google Scholar]
- 65.American Academy of Pediatrics Institute for Healthy Childhood Weight. [Accessed: 8/17/16];Algorithm for the Assessment and Management of Childhood Obesity in Patients 2 Years and Older. 2015 https://ihcw.aap.org/Documents/Assessment%20and%20Management%20of%20Childhood%20Obesity%20Algorithm_v1015.pdf.
- 66.Barlow SE Committee atE. Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics. 2007;120(Supplement 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 67.Saelens BE, Grow HM, Stark LJ, Seeley RJ, Roehrig H. Efficacy of increasing physical activity to reduce children’s visceral fat: a pilot randomized controlled trial. Int J Pediatr Obes. 2011;6(2):102–112. doi: 10.3109/17477166.2010.482157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Edmunds JM, Beidas RS, Kendall PC. Dissemination and Implementation of Evidence-Based Practices: Training and Consultation as Implementation Strategies. Clin Psychol (New York) 2013;20(2):152–165. doi: 10.1111/cpsp.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nadeem E, Gleacher A, Beidas RS. Consultation as an implementation strategy for evidence-based practices across multiple contexts: unpacking the black box. Adm Policy Ment Health. 2013;40(6):439–450. doi: 10.1007/s10488-013-0502-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ringle VA, Read KL, Edmunds JM, et al. Barriers to and Facilitators in the Implementation of Cognitive-Behavioral Therapy for Youth Anxiety in the Community. Psychiatr Serv. 2015;66(9):938–945. doi: 10.1176/appi.ps.201400134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Webster-Stratton CH, Reid MJ, Marsenich L. Improving therapist fidelity during implementation of evidence-based practices: Incredible years program. Psychiatr Serv. 2014;65(6):789–795. doi: 10.1176/appi.ps.201200177. [DOI] [PubMed] [Google Scholar]
- 72.Karlin BE, Brown GK, Trockel M, Cunning D, Zeiss AM, Taylor CB. National dissemination of cognitive behavioral therapy for depression in the Department of Veterans Affairs health care system: therapist and patient-level outcomes. J Consult Clin Psychol. 2012;80(5):707–718. doi: 10.1037/a0029328. [DOI] [PubMed] [Google Scholar]
- 73.Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69(1):19–33. doi: 10.1037/a0033888. [DOI] [PubMed] [Google Scholar]
- 74.Karlin BE, Trockel M, Taylor CB, Gimeno J, Manber R. National dissemination of cognitive behavioral therapy for insomnia in veterans: therapist- and patient-level outcomes. J Consult Clin Psychol. 2013;81(5):912–917. doi: 10.1037/a0032554. [DOI] [PubMed] [Google Scholar]
- 75.Stewart MO, Raffa SD, Steele JL, et al. National dissemination of interpersonal psychotherapy for depression in veterans: therapist and patient-level outcomes. J Consult Clin Psychol. 2014;82(6):1201–1206. doi: 10.1037/a0037410. [DOI] [PubMed] [Google Scholar]
- 76.Walser RD, Karlin BE, Trockel M, Mazina B, Barr Taylor C. Training in and implementation of Acceptance and Commitment Therapy for depression in the Veterans Health Administration: therapist and patient outcomes. Behav Res Ther. 2013;51(9):555–563. doi: 10.1016/j.brat.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 77.Pilkey D, Skopec L, Gee E, Finegold K, Amaya K, Robinson W. The Affordable Care Act and Adolescents. [Accessed 8/17/2016];ASPE.hhs.gov. https://aspe.hhs.gov/sites/default/files/pdf/180281/rb_adolescent.pdf.
- 78.Children’s Hospitals Association. 2013 Survey Findings of Children’s Hospitals Obesity Services. 2013. [Google Scholar]
- 79.Curry SJ, Grothaus LC, McAfee T, Pabiniak C. Use and cost effectiveness of smoking-cessation services under four insurance plans in a health maintenance organization. N Engl J Med. 1998;339(10):673–679. doi: 10.1056/NEJM199809033391006. [DOI] [PubMed] [Google Scholar]
- 80.Rajkumar R, Conway PH, Tavenner M. CMS—engaging multiple payers in payment reform. JAMA. 2014;311(19):1967–1968. doi: 10.1001/jama.2014.3703. [DOI] [PubMed] [Google Scholar]
- 81.Choudhury JS. From Fee-for-Service to Fee-for-Value. [Accessed 8/17/2016];Strategy+business. http://www.strategy-business.com/blog/From-Fee-for-Service-to-Fee-for-Value?gko=30f2e.
- 82.Hubley SH, Miller BF. Implications of Healthcare Payment Reform for Clinical Psychologists in Medical Settings. J Clin Psychol Med Settings. 2016;23(1):3–10. doi: 10.1007/s10880-016-9451-1. [DOI] [PubMed] [Google Scholar]
- 83.Miller HD. From volume to value: better ways to pay for health care. Health Aff (Millwood) 2009;28(5):1418–1428. doi: 10.1377/hlthaff.28.5.1418. [DOI] [PubMed] [Google Scholar]
- 84.Nixon JW. [Accessed 8/17/16];Annual Report to the Missouri Legislature: Insurance Coverage for Autism Treatment & Applied Behavior Analysis. 2015 http://insurance.mo.gov/consumers/autismFAQ/documents/2015AutismReport.pdf.
- 85.YMCA. Measurable Success, Unlimited Support: Diabetes Prevention Program Fact Sheet: January 2016. 2016. [Google Scholar]
- 86.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community. The DEPLOY Pilot Study. Am J Prev Med. 2008;35(4):357–363. doi: 10.1016/j.amepre.2008.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff (Millwood) 2012;31(1):67–75. doi: 10.1377/hlthaff.2011.1009. [DOI] [PubMed] [Google Scholar]
- 89.Vojta D, Koehler TB, Longjohn M, Lever JA, Caputo NF. A coordinated national model for diabetes prevention: linking health systems to an evidence-based community program. Am J Prev Med. 2013;44(4 Suppl 4):S301–306. doi: 10.1016/j.amepre.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 90.New York State Department of Health Medicaid Redesign Team. [Accessed 8/17/16];A Path toward Value Based Payment: New York State Roadmap for Medicaid Payment Reform. https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/vbp_roadmap_final.pdf.
- 91.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Moffit RE. [Accessed 8/17/16];Obamacare: Impact on Doctors.Heritage.org. http://www.heritage.org/research/reports/2010/05/obamacare-impact-on-doctors.
- 93.Snyder L, Rudowitz R, Garfield R, Gordon T. Why does medicaid spending vary across states: a chart book of factors driving state spending. [Accessed 8/17/16];Kff.org. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8378.pdf.
- 94.Centers for Medicaid & Medicare Services. EPSDT - A Guide for States: Coverage in the Medicaid Benefit for Children and Adolescents. [Accessed 8/17/16];Medicaid.gov. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Benefits/Downloads/EPSDT_Coverage_Guide.pdf.
- 95.Lee JS, Sheer JL, Lopez N, Rosenbaum S. Coverage of obesity treatment: a state-by-state analysis of Medicaid and state insurance laws. Public Health Rep. 2010;125(4):596–604. doi: 10.1177/003335491012500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Centers for Medicaid & Medicare Services. CHIP Reports and Evaluations. [Accessed 8/17/16];Medicaid.gov. https://www.medicaid.gov/chip/reports-and-evaluations/reports-and-evaluations.html.
- 97.Kaiser Family Foundation. Medicaid and its Role in State/Federal Budgets & Health Reform. [Accessed 8/17/16];Kff.org. https://kaiserfamilyfoundation.files.wordpress.com/2012/05/8139-03.pdf.
- 98.Kaiser Family Foundation. 2014 Employer Health Benefits Survey. [Accessed 8/17/16];Kff.org. http://files.kff.org/attachment/2014-employer-health-benefits-survey-full-report.
- 99.Burke T. Accountable Care Organizations. Public Health Rep. 2011;126(6):875–878. doi: 10.1177/003335491112600614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kocher R, Sahni NR. Physicians versus hospitals as leaders of accountable care organizations. N Engl J Med. 2010;363(27):2579–2582. doi: 10.1056/NEJMp1011712. [DOI] [PubMed] [Google Scholar]
- 101.Trasande L. How much should we invest in preventing childhood obesity? Health Aff (Millwood) 2010;29(3):372–278. doi: 10.1377/hlthaff.2009.0691. [DOI] [PubMed] [Google Scholar]
- 102.Puhl RM, Suh Y, Li X. Improving anti-bullying laws and policies to protect youth from weight-based victimization: parental support for action. Pediatr Obes. 2016 doi: 10.1111/ijpo.12129. [DOI] [PubMed] [Google Scholar]
- 103.Puhl RM, Suh Y, Li X. Legislating for weight-based equality: national trends in public support for laws to prohibit weight discrimination. Int J Obes (Lond) 2016 doi: 10.1038/ijo.2016.49. [DOI] [PubMed] [Google Scholar]
- 104.Hampl SE, Davis AM, Sampilo ML, Stephens KL, Dean K. Insurer and employer views on pediatric obesity treatment: a qualitative study. Obesity (Silver Spring) 2013;21(4):795–799. doi: 10.1002/oby.20112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rask KJ, Gazmararian JA, Kohler SS, Hawley JN, Bogard J, Brown VA. Designing insurance to promote use of childhood obesity prevention services. J Obes. 2013;2013:379513. doi: 10.1155/2013/379513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Boutelle KN, Cafri G, Crow SJ. Parent-only treatment for childhood obesity: a randomized controlled trial. Obesity (Silver Spring) 2011;19(3):574–580. doi: 10.1038/oby.2010.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.