Abstract
Background
Patients with advanced heart failure (HF) enroll in hospice at low rates and data on their acute medical service utilization following hospice enrollment is limited.
Methods and Results
We performed a descriptive analysis of Medicare fee-for-service beneficiaries, with at least one home health claim between 07/01/2009 and 06/30/2010, and at least two HF hospitalizations between 07/01/2009 and 12/31/2009, who subsequently enrolled in hospice between 07/01/2009 and 12/31/2009. We estimated panel negative binomial models on a subset of beneficiaries to compare their acute medical service utilization before and after enrollment. Our sample size included 5,073 beneficiaries: 55% were female, 45% were ≥ 85 years of age, 13% were non-white, and the mean comorbidity count was 2.38 (STD 1.22). The median number of days between the second HF hospital discharge and hospice enrollment was 45. The median number of days enrolled in hospice was 15, and 39% of the beneficiaries died within 7 days of enrollment. During the study period, 11% of the beneficiaries disenrolled from hospice at least once. The adjusted mean number of hospital, ICU, and ER admissions decreased from 2.56, 0.87, and 1.17 before hospice enrollment to 0.53, 0.19, and 0.76 after hospice enrollment.
Conclusions
Home health care Medicare beneficiaries with advanced HF who enrolled in hospice had lower acute medical service utilization following their enrollment. Their pattern of hospice use suggests that earlier referral and improved retention may benefit this population. Further research is necessary to understand hospice referral and palliative care needs of advanced HF patients.
Keywords: heart failure, hospice, Medicare
Heart failure (HF) is a chronic illness that often exhibits a progressive yet unpredictable disease course and largely affects older adults with multiple comorbidities.1,2 Older adults with HF are hospitalized frequently: in a large population-based study of HF patients with a mean age of 82 years at death, 81.5% were hospitalized at least once in the final year of life.3, 4 Medicare data from 2000–2007 demonstrate that approximately 80% of patients with HF are hospitalized in the last 6 months of life.5 Furthermore, Medicare patients with HF have higher use of acute medical services in the 30 days before death, when compared to cancer patients.6 Due to the high healthcare utilization of patients with HF, estimated total costs for HF treatment in the United States exceeds $32 billion per year,1 which is more than for any other diagnosis.7
Patients with advanced HF, or stage D HF, have marked symptoms at rest despite optimal medical management, as defined by the American College of Cardiology/the American Heart Association (ACC/AHA).3 These symptoms include fatigue, dyspnea, depression, edema and pain.2 In addition to a high symptom burden, these patients have high mortality of approximately 50% at one-year.8 Thus, ACC/AHA guidelines recommend clinicians introduce hospice as an option for patients who develop stage D HF while considering advanced therapies including ventricular assist device and transplant if appropriate.1, 3
Hospice, under the Medicare Hospice Benefit, delivers medical, physical, emotional, social and spiritual services to patients who have a prognosis of six months or less to live and who opt to forgo life-prolonging therapies.9, 10 Evidence demonstrates that in patients with advanced cancer, hospice improves survival11, patients’ physical and psychological symptoms11, caregiver well-being and family satisfaction12–15, and reduces healthcare costs.16–20
Although symptomatic HF confers a worse prognosis than most cancers, patients with advanced HF enroll in hospice at lower rates than those with cancer.19 Furthermore, patients with HF were more likely to enroll in hospice within three days of death.16 Though patients with HF are more likely to use emergency care services and disenroll from hospice than patients with cancer, evidence suggests there is little difference in caregiver satisfaction by diagnosis.21 Specifically, family caregivers are equally satisfied with hospice professionals’ care for patients with HF and cancer, especially in the area of symptom management.21 Data specific to patterns of hospice use in the HF population remains limited.22, 23
To improve our understanding of patients with advanced HF who enroll in hospice, we describe a sample of Medicare beneficiaries with advanced HF, including demographics, patterns of hospice use and acute medical service utilization (hospital admissions, intensive care unit (ICU) stays, and emergency room (ER) visits) before and after hospice enrollment. By establishing the advantages of hospice to patients with advanced HF, referral patterns could be changed so more individuals benefit from this model of comprehensive care at the end-of-life.
Methods
Study Population
In collaboration with the Visiting Nurse Service of New York Center for Home Care Policy and Research (VNSNY), we conducted a secondary analysis using data from a longitudinal, observational study that examined patterns of care in a cohort of HF patients using Medicare claims and patient assessment data.24 This existing dataset used 2009 and 2010 Medicare administrative claims and home health patient assessment data to identify all HF hospitalizations with discharge to home health care (HHC) between July 1, 2009 and June 30, 2010.24 To identify HF hospitalizations, we included patients admitted with a principal diagnosis of HF using the ICD-9 CM codes employed by the federal Chronic Conditions Data Warehouse (CCW) and a medical Medicare Severity Diagnosis Related Group (MS-DRG).24 HF hospitalizations assigned to a surgical MS-DRG were excluded because wound care, rather than HF management, was likely the primary reason for care. To examine beneficiaries with advanced HF, we selected a sub-sample of individuals with two or more HF hospitalizations within a six-month period (07/01/2009 to 12/31/2009), as a marker of increased HF severity or worse prognosis.25 Only patients enrolled in hospice after the second HF discharge between 07/01/2009 and 12/31/2009 using follow-up data between 01/01/2010 and 12/31/2010 were included for analysis.
Demographics
We conducted descriptive analyses of the beneficiary demographics. We identified age, sex, and race from the Medicare data. A simple count of the number of comorbidities was our measure of comorbidity burden. By linking beneficiary zip codes to Census data, we obtained the median family income in the patient’s area of residence.
Patterns of Hospice Use
To characterize the timing of hospice referral we calculated: 1) number of days from second HF hospitalization discharge to hospice enrollment; 2) number of days from hospice enrollment to death; and 3) number of days from hospice enrollment to disenrollment, for those who disenrolled. We report the median number of days between the second HF hospital discharge and hospice enrollment and the median number of days enrolled in hospice. Hospice disenrollment may be initiated either by the patient or the hospice.22 Patients may revoke their election of hospice due to dissatisfaction with care, change in preferences for hospice care, or the desire to pursue treatments not covered under the Medicare Hospice Benefit. A hospice may discharge a patient if the hospice deems the patient no longer eligible for hospice, the patient moves out of the hospice’s service area, or the hospice can no longer safely provide care. We identified hospice disenrollment as a condition code of “patient discharged for cause” or patient status code of “discharge to home, revoked or decertified” on their last Medicare hospice claim. Finally, we examined the location of death using the place of service for those enrolled in hospice on their last Medicare hospice claim and for those not enrolled in hospice on their last Medicare claim.
Acute Medical Service Utilization: Hospital Admissions, ICU stays and ER visits
Hospital admissions, ICU stays, and ER visits that ended in hospital admission were identified from the Medicare Provider Analysis and Review (MEDPAR) file while ER visits that did not end in hospital admission were identified from Medicare Outpatient Standard Analytical Files. Because individual beneficiaries died at different time points after hospice enrollment, we used population-averaged generalized estimating equations (GEE) negative binomial models, also known as panel negative binomial models26, to account for differences in length of exposure and possible correlation between the before and after measurements for the same patients, when calculating acute medical service utilization six months before and after hospice enrollment. We calculated unadjusted and adjusted marginal means of the number of hospital admissions, ICU stays and ER visits, and compared the differences in means before and after enrollment. We used Stata 12 to estimate these models.
The VNSNY and the Icahn School of Medicine at Mount Sinai institutional review boards approved conduct of this study.
Results
Demographics
Of the 234,301 Medicare beneficiaries with HF hospitalizations with discharge to HHC between July 1, 2009 and June 30, 2010, 59,405 beneficiaries had at least two HF hospital discharges within a six-month period (07/01/2009 to 12/31/2009). Our sample includes the 5,073 (8.54%) beneficiaries who enrolled in hospice after the second HF hospital discharge (Figure 1). The socio-demographic and clinical characteristics of the beneficiaries are shown in Table 1. The mean age of beneficiaries was 82 years at the time of death, 55% were female, and 87% were White non-Hispanic. The mean comorbidity count was 2.38 (standard deviation of 1.22 with a range of 0–6), and 45% had a mean comorbidity count of three or more.
Figure 1.
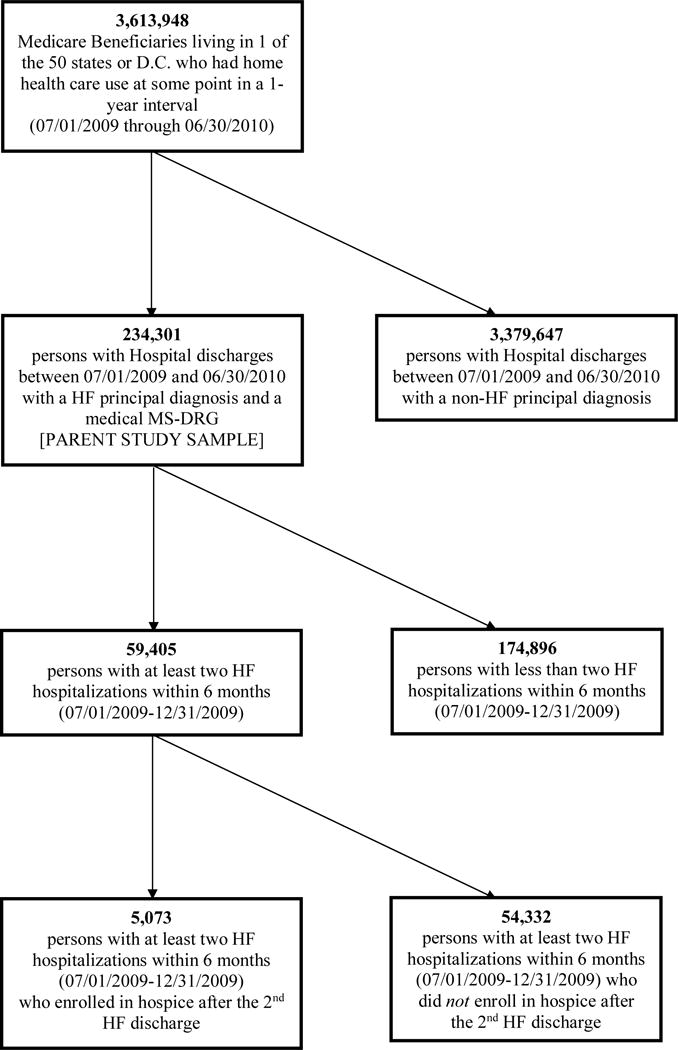
Selection of Sample (N= 5,073).
Table 1.
Demographics of Study Population: Home Health Care Medicare beneficiaries with advanced HF who were hospitalized at least twice in six months and enrolled in hospice (N = 5,073 beneficiaries).
| Characteristic | N (%) |
|---|---|
| Age (years) | |
| <65 | 236 (5%) |
| 65–74 | 721 (14%) |
| 75–84 | 1859 (37%) |
| 85 years and older | 2257 (45%) |
| Sex | |
| Female | 2811 (55%) |
| Race | |
| White non-Hispanic | 4410 (87%) |
| White Hispanic | 81 (2%) |
| Black | 524 (10%) |
| Asian | 20 (<1%) |
| Other & Pacific Islander | 21 (<1%) |
| North American Native | 11 (<1%) |
| Comorbidity Count, mean (SD) | 2.38 (1.22) |
| Comorbidity Count ≥ 3 | 2273 (45%) |
| Family Income, Median | $48,000 |
Patterns of Hospice Use
The median and mean number of days from second HF hospital discharge to enrollment in hospice was 45 days and 70 days, respectively (standard deviation of 73 days) (Figure 2). Figure 2 also shows 24% of our sample enrolling in hospice within 0–7 days after second HF hospital discharge and another 23% enrolling up to 91–180 days after second HF hospital discharge. The mean number of days from hospice enrollment to death was 71 days (SD 112 days) (Figure 3). Half of the patients died after 16 days of hospice care and 39% died within 7 days (Figure 4). Four hundred fifty-four individuals (8.9%) were still alive at one year after hospice enrollment. Five hundred and fifty-five beneficiaries (11%) disenrolled from hospice at least once in the one-year after hospice enrollment. Of those, 38% disenrolled in the first 30 days after hospice enrollment.
Figure 2.
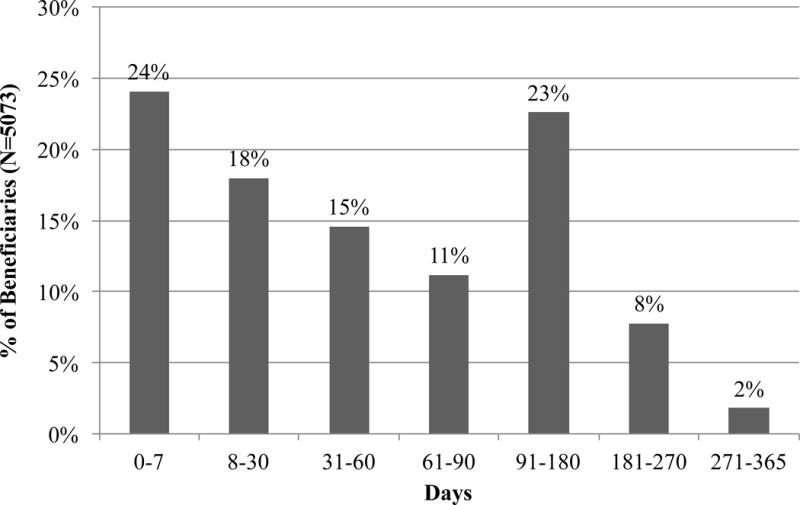
Percentage of beneficiaries (N = 5,073) who enrolled in hospice by time interval (days = 0–7, 8–30, 31–60, 61–90, 91–180, 181–270, 271–365 from 2nd hospitalization discharge).
Figure 3.
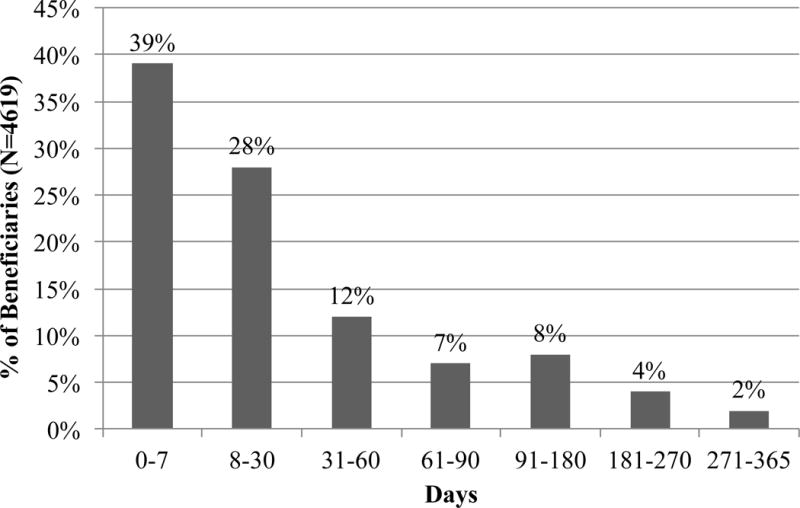
Percentage of beneficiaries (N = 4,619) who died by time interval (days = 0–7, 8–30, 31–60, 61–90, 91–180, 181–270, 271–365 from hospice enrollment).
Figure 4.
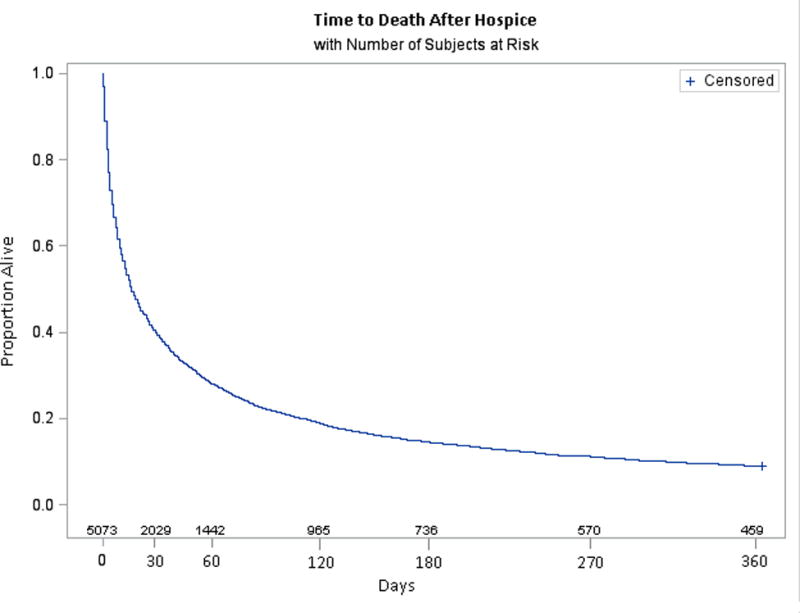
Kaplan-Meier survival curve of beneficiaries from hospice enrollment to death or one year.
By the end of the study period, 4,619 beneficiaries (91%) had died. Of those, 4,051 (88%) died while enrolled in hospice. Of the 568 beneficiaries who disenrolled from hospice and died while not receiving hospice care, 48.6% died in an acute hospital facility, 17.6% died in a skilled nursing facility or rehabilitation center, 2% died receiving HHC, and 31.9% died outside of these settings of care.
Acute Medical Service Utilization: Hospital Admissions, ICU stays and ER visits
Table 2 reports the unadjusted and adjusted mean number of hospital admissions, ICU stays, and ER visits before and after hospice enrollment. Following hospice enrollment, there was significant reduction in hospital admissions (2.56 vs. 0.53, p<0.001), ICU admissions (0.87 vs. 0.19, p<0.001) and ER visits (1.17 vs. 0.76, p<0.001).
Table 2.
Mean Acute Medical Service Utilization in the Six Months Before and After Hospice Enrollment Hospice Enrollment.
| Unadjusted Means (95% CI) |
Adjusted Means* (95% CI) |
|||||
|---|---|---|---|---|---|---|
| Before Hospice | After Hospice | p-value | Before Hospice | After Hospice | p-value | |
| Number of hospital admissions | 3.98 (3.93, 4.03) |
0.23 (0.21, 0.25) |
<0.001 | 2.56 (2.48, 2.63) |
0.53 (0.49, 0.57) |
<0.001 |
| Number of ICU admissions | 1.36 (1.32, 1.40) |
0.08 (0.07, 0.09) |
<0.001 | 0.87 (0.84, 0.91) |
0.19 (0.17, 0.21) |
<0.001 |
| Number of ER visits | 1.82 (1.73, 1.90) |
0.35 (0.30, 0.40) |
<0.001 | 1.17 (1.13, 1.21) |
0.76 (0.71, 0.81) |
<0.001 |
The adjusted means were calculated from the negative binomial regression; these results are adjusted for the number of days enrolled in hospice, which varies for each beneficiary.
Discussion
We describe the demographics, patterns of hospice use, and acute medical service utilization in the six months before and after hospice enrollment for Medicare beneficiaries with advanced HF. We aimed to focus on the benefits to HF patients once they are enrolled in hospice. Specifically, we were interested in describing the trajectory of patients with HF enrolled in hospice, rather than describing their hospice enrollment patterns, so we only studied the sample that enrolled in hospice (N = 5,073 from Figure 1).
Demographics of this sample of older adults with HF who used hospice–45% were older than 85 years of age, a slight majority were female, and 87% were White–are similar to national trends regarding characteristics of hospice users across all diagnoses.10 In addition, although advanced HF patients are referred to hospice less often, this sample’s time to hospice enrollment, high prevalence of short hospice enrollment periods, and hospice disenrollment rate of this sample parallel that of hospice users across all diagnoses nationally.23
Time to referral to hospice
Earlier referral to hospice has been demonstrated to improve the quality of end-of-life care received by patients and their families.11 Patients may not receive the full benefit of hospice services when enrollment periods are ≤1 week, and this has been associated with poor outcomes for patients and their families.27–30 A study by the US Department of Health and Human Services suggests that a patient must receive hospice care for at least 30 days to minimally experience its benefits.31 Timing of referral is challenging because of the unpredictable clinical course of patients with HF. Additionally, stage D patients are potential candidates for advanced therapies.32 The bimodal distribution of days until hospice enrollment following second HF hospital discharge (Figure 2) may reflect the clinical trajectory of HF.33, 34 The later peak in hospice enrollment may be due to patients who initially return to their clinical baseline and later experienced a clinical decline.
Given that 39% of the beneficiaries in our sample died within seven days of hospice enrollment and half died within 16 days, this population may be referred to hospice too late. This duration of hospice enrollment is comparable to national trends: 32.4% of all Medicare decedents in 2011 used hospice for less than seven days.35 Similar to other seriously ill patients, patients with advanced HF could benefit from earlier hospice enrollment, and therefore receive improved symptom control. The barriers to earlier hospice referral in this population remain unstudied. With earlier hospice referral, advanced HF patients would receive the beneficial effects of hospice.
The unpredictable trajectory of HF makes prognostication challenging, leading to variable hospice enrollment periods [short enrollment (≤1 week) versus long enrollment period (> 6 months)].22 In our sample, 281 (5.54%) beneficiaries had a long enrollment period, compared to 10.3% reported in the National Hospice and Palliative Care Organization10 and 13.9% in Medicare hospice claims.22
Rates of Hospice Disenrollment
Another opportunity to improve the quality of hospice care received by patients with advanced HF would be reducing the rate of hospice disenrollment, which impacts quality of care received, healthcare utilization and cost. Eleven percent of the beneficiaries in our sample disenrolled at least once following hospice enrollment, which is comparable to other reports on hospice disenrollment.36–38 In patients with cancer, hospice disenrollment is associated with higher healthcare use, including higher rates of hospitalization, ED and ICU admissions, and increased length of stay once hospitalized.38 On average, patients with advanced cancer who disenroll cost Medicare almost five times as much as those who remain with hospice until death.37 Additionally, disenrollees were more likely to die in the hospital.37, 38 In our sample, of those who died, 88% died while receiving hospice care, which is consistent with patient preferences for death.2 Of the 568 beneficiaries (11%) who died without hospice care, nearly half died in an acute hospital facility, and 17.6% died in a skilled nursing facility or rehabilitation center, which is inconsistent with data on patient and caregiver preferences.39
Acute Medical Service Utilization Before and After Hospice Enrollment
We found that the mean number of hospital admissions, ICU admissions, and ER visits all decreased after hospice enrollment, consistent with other populations.40 These findings are significant because there is a growing body of literature demonstrating an increase in acute medical service utilization as HF clinical trajectory progresses and symptom burden worsens.34, 41–43 In addition, these findings are timely given the policy efforts to reduce HF readmission rates and healthcare costs; if eligible patients are referred to hospice, significant reductions in cost and utilization are possible.
Limitations
Our study population includes only Medicare beneficiaries who received HHC prior to the two HF hospitalizations, so this sample may not be generalizable to other populations. In spite of this limitation, patients who required HHC are likely to have a more severe illness course and thus have greater need for skilled services such as those provided by hospice. However, patients receiving HHC, by virtue of having an informal home caregiver, may have both a better social safety net and function, thereby preventing admission to a skilled nursing facility.
Additionally, HHC agencies with embedded hospice services may have different referral patterns than those without, and this was a difference we could not account for. There is a potential threat to external validity of the study given the overlap of our inclusion criteria of two or more HF hospitalizations and the outcome variable of hospital admissions.
Another limitation is in how we categorized those who disenrolled from hospice. Because Medicare claims data does not include information about patient preferences, we are unable to distinguish those who disenrolled from hospice due to improved clinical stability from those who disenrolled due to change in treatment preference for hospice. Finally, without standard HF severity indicators, such as HF stage or New York Heart Association HF class, we examined only those with at least two HF hospitalizations within a six-month period as a surrogate for disease severity.
Conclusions
This sample of HHC Medicare beneficiaries with advanced HF who enroll in hospice reflects the national trends in hospice enrollment across all diagnoses. The clinical marker of two HF hospitalizations within a six-month period could serve as an opportunity to initiate earlier conversations about advance care planning and hospice enrollment. These results highlight the need for timelier hospice referral in this population, thereby allowing for longer enrollment periods and decreased disenrollment rates; in turn, patients with advanced HF and their families would benefit from the spectrum of hospice services and improved quality of end-of-life care. Ultimately, further research is necessary, so we can better tailor hospice to the needs of older adults with advanced HF.
Clinical Perspective.
Heart failure (HF) is a chronic illness, which often affects older adults with multiple co-morbidities, who experience a high symptom burden leading to frequent hospitalizations, as well as high mortality rates. Although there is a growing body of literature about patterns of hospice use, HF specific data remains limited. Our study examined the demographics, patterns of hospice use, and acute medical service utilization of a population of Medicare beneficiaries who received home health care followed by two or more HF admissions within 6 months, and subsequently enrolled in hospice. We found that this sample shared similar demographic characteristics to national trends in hospice enrollment across all diagnoses. In addition to possible delay in hospice referral, this population had short hospice stays: 39% died within a week. In contrast with literature demonstrating an increase in acute medical service use as HF disease progresses, there was a reduction in acute medical service utilization (hospital admissions, ICU stays, and ER visits) following hospice enrollment in this sample. Patients with advanced HF could benefit from an earlier hospice enrollment. The clinical marker of 2 HF hospitalizations in six months may serve as an opportunity to engage patients with HF and their families in earlier conversations about hospice enrollment. In turn, these patients and their families could benefit from the full range of hospice services and improve the quality of their end-of-life care.
Acknowledgments
Sources of Funding: CY received support from the Medical Student Training in Aging Research (MSTAR) Fellowship administered by American Federation for Aging (AFAR) and National Institute on Aging (NIA). LPG received support from the National Institute on Aging (NIA) (1K23AG049930), The Mount Sinai Older Adults Independence Center (P30AG028741), the American Federation on Aging Research, and the National Palliative Care Research Center. The core dataset analyzed in this study was developed as part of a project supported by grant number R01HS020257 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily reflect the official view of the Agency for Healthcare Research and Quality.
Footnotes
Disclosures: None.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Executive summary: Heart disease and stroke statistics–2014 update: A report from the american heart association. Circulation. 2014;129:399–410. doi: 10.1161/01.cir.0000442015.53336.12. [DOI] [PubMed] [Google Scholar]
- 2.LeMond L, Allen LA. Palliative care and hospice in advanced heart failure. Prog Cardiovasc Dis. 2011;54:168–178. doi: 10.1016/j.pcad.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJV, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WHW, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;62:e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 4.Dunlay SM, Redfield MM, Jiang R, Weston SA, Roger VL. Care in the last year of life for community patients with heart failure. Circ Heart Fail. 2015;8:489–496. doi: 10.1161/CIRCHEARTFAILURE.114.001826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unroe KT, Greiner MA, Hernandez AF, Whellan DJ, Kaul P, Schulman KA, Peterson ED, Curtis LH. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000–2007. Arch Intern Med. 2011;171:196–203. doi: 10.1001/archinternmed.2010.371. [DOI] [PubMed] [Google Scholar]
- 6.Setoguchi S, Glynn RJ, Stedman M, Flavell CM, Levin R, Stevenson LW. Hospice, opiates, and acute care service use among the elderly before death from heart failure or cancer. Am Heart J. 2010;160:139–144. doi: 10.1016/j.ahj.2010.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: A report of the american college of cardiology/american heart association task force on practice guidelines (writing committee to update the 2001 guidelines for the evaluation and management of heart failure): Developed in collaboration with the american college of chest physicians and the international society for heart and lung transplantation: Endorsed by the heart rhythm society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 8.Friedrich EB, Bohm M. Management of end stage heart failure. Heart. 2007;93:626–631. doi: 10.1136/hrt.2006.098814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services (CMS), HHS. Medicare and medicaid programs: Hospice conditions of participation. Final rule. Fed Regist. 2008;73:32087–32220. [PubMed] [Google Scholar]
- 10.National Hospice and Palliative Care Organization. NHPCO’s Facts and Figures: Hospice Care in America. 2015. Alexandria (VA): NHPCO; 2015. Internet. [Google Scholar]
- 11.Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 12.Jordhoy MS, Fayers P, Loge JH, Ahlner-Elmqvist M, Kaasa S. Quality of life in palliative cancer care: Results from a cluster randomized trial. J Clin Oncol. 2001;19:3884–3894. doi: 10.1200/JCO.2001.19.18.3884. [DOI] [PubMed] [Google Scholar]
- 13.Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 14.Casarett D, Pickard A, Bailey FA, Ritchie C, Furman C, Rosenfeld K, Shreve S, Chen Z, Shea JA. Do palliative consultations improve patient outcomes? J Am Geriatr Soc. 2008;56:593–599. doi: 10.1111/j.1532-5415.2007.01610.x. [DOI] [PubMed] [Google Scholar]
- 15.Gelfman LP, Meier DE, Morrison RS. Does palliative care improve quality? A survey of bereaved family members. J Pain Symptom Manage. 2008;36:22–28. doi: 10.1016/j.jpainsymman.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung WY, Schaefer K, May CW, Glynn RJ, Curtis LH, Stevenson LW, Setoguchi S. Enrollment and events of hospice patients with heart failure vs. Cancer. J Pain Symptom Manage. 2013;45:552–560. doi: 10.1016/j.jpainsymman.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Morrison RS, Dietrich J, Ladwig S, Quill T, Sacco J, Tangeman J, Meier DE. Palliative care consultation teams cut hospital costs for medicaid beneficiaries. Health Aff (Millwood) 2011;30:454–463. doi: 10.1377/hlthaff.2010.0929. [DOI] [PubMed] [Google Scholar]
- 18.Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, Spragens L, Meier DE. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783–1790. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 19.Penrod JD, Deb P, Dellenbaugh C, Burgess JF, Jr, Zhu CW, Christiansen CL, Luhrs CA, Cortez T, Livote E, Allen V, Morrison RS. Hospital-based palliative care consultation: Effects on hospital cost. J Palliat Med. 2010;13:973–979. doi: 10.1089/jpm.2010.0038. [DOI] [PubMed] [Google Scholar]
- 20.Back AL, Li YF, Sales AE. Impact of palliative care case management on resource use by patients dying of cancer at a veterans affairs medical center. J Palliat Med. 2005;8:26–35. doi: 10.1089/jpm.2005.8.26. [DOI] [PubMed] [Google Scholar]
- 21.MacKenzie MA, Meghani SH, Buck HG, Riegel B. Does diagnosis make a difference? Comparing hospice care satisfaction in matched cohorts of heart failure and cancer caregivers. J Palliat Med. 2015;18:1008–1014. doi: 10.1089/jpm.2015.0078. [DOI] [PubMed] [Google Scholar]
- 22.Aldridge MD, Canavan M, Cherlin E, Bradley EH. Has hospice use changed? 2000–2010 utilization patterns. Med Care. 2015;53:95–101. doi: 10.1097/MLR.0000000000000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khand A, Gemmel I, Clark A, Cleland J. Is the prognosis of heart failure improving? J Am Coll Cardiol. 2000;36:2284–2286. doi: 10.1016/s0735-1097(00)00995-5. [DOI] [PubMed] [Google Scholar]
- 24.Murtaugh CM, Deb P, Zhu C, Peng TR, Barron Y, Shah S, Moore SM, Bowles KH, Kalman J, Feldman PH, Siu AL. Reducing readmissions among heart failure patients discharged to home health care: Effectiveness of early and intensive nursing services and early physician follow-up. Health Serv Res. 2016 doi: 10.1111/1475-6773.12537. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J. 2007;154:260–266. doi: 10.1016/j.ahj.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 26.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using stata. STATA Press; College Station, TX: 2008. [Google Scholar]
- 27.Miller SC, Mor V, Teno J. Hospice enrollment and pain assessment and management in nursing homes. J Pain Symptom Manage. 2003;26:791–799. doi: 10.1016/s0885-3924(03)00284-7. [DOI] [PubMed] [Google Scholar]
- 28.Bradley EH, Prigerson H, Carlson MD, Cherlin E, Johnson-Hurzeler R, Kasl SV. Depression among surviving caregivers: Does length of hospice enrollment matter? Am J Psychiatry. 2004;161:2257–2262. doi: 10.1176/appi.ajp.161.12.2257. [DOI] [PubMed] [Google Scholar]
- 29.Kris AE, Cherlin EJ, Prigerson H, Carlson MD, Johnson-Hurzeler R, Kasl SV, Bradley EH. Length of hospice enrollment and subsequent depression in family caregivers: 13-month follow-up study. Am J Geriatr Psychiatry. 2006;14:264–269. doi: 10.1097/01.JGP.0000194642.86116.ce. [DOI] [PubMed] [Google Scholar]
- 30.Rickerson E, Harrold J, Kapo J, Carroll JT, Casarett D. Timing of hospice referral and families’ perceptions of services: Are earlier hospice referrals better? J Am Geriatr Soc. 2005;53:819–823. doi: 10.1111/j.1532-5415.2005.53259.x. [DOI] [PubMed] [Google Scholar]
- 31.Miller SC, Gozalo P, Mor V. Outcomes and utilization for hospice and non-hospice nursing facility decedents. US Department of Health and Human Services, Office of Disability, Aging, and Long-Term Care Policy, Washington, DC. 2000 [Google Scholar]
- 32.Gelfman LP, Kalman J, Goldstein NE. Engaging heart failure clinicians to increase palliative care referrals: Overcoming barriers, improving techniques. J Palliat Med. 2014;17:753–760. doi: 10.1089/jpm.2013.0675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teno JM, Weitzen S, Fennell ML, Mor V. Dying trajectory in the last year of life: Does cancer trajectory fit other diseases? J Palliat Med. 2001;4:457–464. doi: 10.1089/109662101753381593. [DOI] [PubMed] [Google Scholar]
- 34.Udelson JE, Stevenson LW. The future of heart failure diagnosis, therapy, and management. Circulation. 2016;133:2671–2686. doi: 10.1161/CIRCULATIONAHA.116.023518. [DOI] [PubMed] [Google Scholar]
- 35.Wang SY, Aldridge MD, Gross CP, Canavan M, Cherlin E, Johnson-Hurzeler R, Bradley E. Geographic variation of hospice use patterns at the end of life. J Palliat Med. 2015;18:771–780. doi: 10.1089/jpm.2014.0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Casarett DJ, Marenberg ME, Karlawish JH. Predictors of withdrawal from hospice. J Palliat Med. 2001;4:491–497. doi: 10.1089/109662101753381638. [DOI] [PubMed] [Google Scholar]
- 37.Carlson MD, Herrin J, Du Q, Epstein AJ, Barry CL, Morrison RS, Back AL, Bradley EH. Impact of hospice disenrollment on health care use and medicare expenditures for patients with cancer. J Clin Oncol. 2010;28:4371–4375. doi: 10.1200/JCO.2009.26.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carlson MD, Herrin J, Du Q, Epstein AJ, Cherlin E, Morrison RS, Bradley EH. Hospice characteristics and the disenrollment of patients with cancer. Health Serv Res. 2009;44:2004–2021. doi: 10.1111/j.1475-6773.2009.01002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: A qualitative systematic literature review of patient preferences. J Palliat Med. 2000;3:287–300. doi: 10.1089/jpm.2000.3.287. [DOI] [PubMed] [Google Scholar]
- 40.Blecker S, Anderson GF, Herbert R, Wang NY, Brancati FL. Hospice care and resource utilization in medicare beneficiaries with heart failure. Med Care. 2011;49:985–991. doi: 10.1097/MLR.0b013e318235c221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Colvin MM, Drazner MH, Filippatos G, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: An update of the 2013 accf/aha guideline for the management of heart failure: A report of the american college of cardiology/american heart association task force on clinical practice guidelines and the heart failure society of america. J Am Coll Cardiol. 2016;68:1476–1488. doi: 10.1016/j.jacc.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 42.Goldstein NE, Lynn J. Trajectory of end-stage heart failure: The influence of technology and implications for policy change. Perspect Biol Med. 2006;49:10–18. doi: 10.1353/pbm.2006.0008. [DOI] [PubMed] [Google Scholar]
- 43.Kheirbek RE, Alemi F, Citron BA, Afaq MA, Wu H, Fletcher RD. Trajectory of illness for patients with congestive heart failure. J Palliat Med. 2013;16:478–484. doi: 10.1089/jpm.2012.0510. [DOI] [PubMed] [Google Scholar]


