Abstract
Background
With diminishing reimbursement rates and strained public payer budgets, a high-volume inpatient procedure, such as total knee arthroplasty (TKA), is a common target for improving cost efficiencies.
Methods
This prospective case–control study compared the cost-minimization of same day discharge (SDD) versus inpatient TKA. We examined if and where cost savings can be realized and the magnitude of savings that can be achieved without compromising quality of care. Outcome variables, including detailed case costs, return to hospital rates and complications, were documented and compared between the first 20 SDD cases and 20 matched inpatient controls.
Results
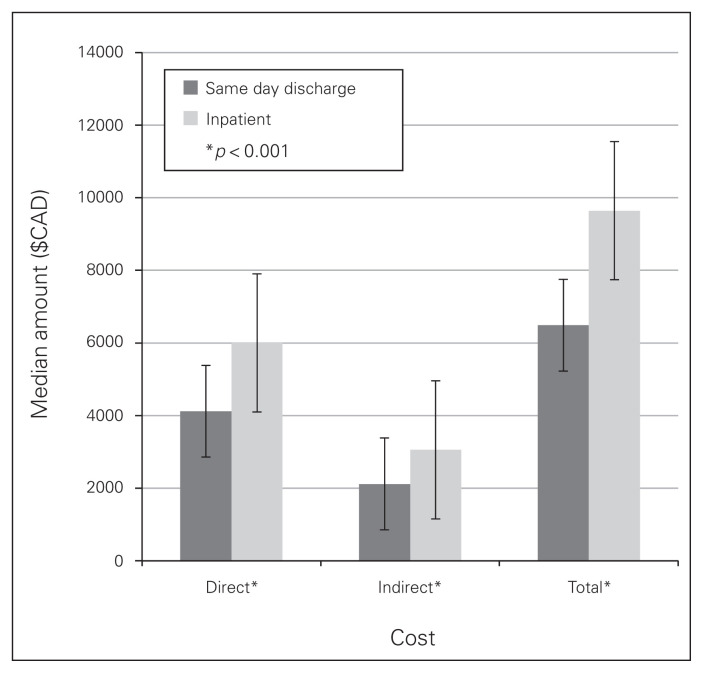
In every case–control match, the SDD TKA was less costly than the inpatient procedure and yielded a median cost savings of approximately 30%. The savings came primarily from costs associated with the inpatient encounter, such as surgical ward, pharmacy and patient meal costs. At 1 year, there were no major complications and no return to hospital or readmission encounters for either group.
Conclusion
Our results are consistent with previously published data on the cost savings associated with short stay or outpatient TKA. We have gone further by documenting where those savings were in a matched cohort design. Furthermore, we determined where cost savings could be realized during the patient encounter and to what degree. In carefully selected patients, outpatient TKA is a feasible alternative to traditional inpatient TKA and is significantly less costly. Furthermore, it was deemed to be safe in the perioperative period.
Abstract
Contexte
Dans le contexte de budgets publics serrés et de taux de remboursement à la baisse, une intervention chirurgicale en service interne à volume élevé, comme l’arthroplastie totale du genou, est souvent ciblée pour améliorer le rapport coût–efficacité.
Méthodes
Cette étude cas–témoins prospective a fait une analyse de minimisation des coûts de l’arthroplastie totale du genou en chirurgie d’un jour et en service interne. Nous avons examiné si et où des économies peuvent être réalisées et l’ampleur des économies pouvant être obtenues sans compromettre la qualité des soins. Les variables dépendantes, notamment les coûts détaillés des cas, le taux de retour à l’hôpital et les complications, ont été documentées, puis comparées entre les 20 premiers cas de chirurgie d’un jour et 20 cas–témoins appariés de chirurgie en service interne.
Résultats
Pour chaque appariement cas–témoins, l’arthroplastie totale du genou en chirurgie d’un jour était moins coûteuse que la chirurgie en service interne et a généré des économies médianes d’environ 30 %. Les économies découlaient principalement des coûts associés à l’hospitalisation du patient tels que les coûts de l’unité de soins chirurgicaux, de la pharmacie et des repas du patient. Après 1 an, ni l’un ni l’autre des 2 groupes ne présentait de complications majeures, de retours à l’hôpital ou de réadmissions.
Conclusion
Nos résultats concordent avec les données antérieures publiées sur les économies associées à l’arthroplastie totale du genou pratiquée en chirurgie d’un jour ou en service interne de courte durée. Nous sommes allés plus loin en documentant également où les économies se situaient dans un modèle cas–témoins. De plus, nous avons déterminé les aspects de la rencontre avec le patient où des économies pourraient être réalisées et l’ampleur de ces économies. Chez des patients soigneusement choisis, l’arthroplastie totale du genou en chirurgie d’un jour est une solution de rechange envisageable à l’arthroplastie totale du genou traditionnelle en service interne et est beaucoup moins coûteuse. De plus, elle a été jugée sécuritaire en période périopératoire.
Total knee arthroplasty (TKA) is considered a highly cost-effective procedure, on par with procedures such as hemodialysis.1 There was an increase of 250 000 cases of TKA performed between 1991 and 2010 in the U.S. Medicare population, accounting for a 160% increase in volume.2 Similarly, in Canada the number of hip and knee replacements increased by 13% between 2006 and 2011 and by 87% in the 10 years preceding that.3 Diminishing third party payer reimbursement rates and strained public payer budgets have made procedures such as TKA a common target for improving cost efficiencies. Bundled payment programs are also providing substantial incentives to create more efficient TKA protocols, which include standardized care pathways in most major centres.
Since its establishment, inpatient hospital stay has been and continues to be the standard of care following TKA. However, within the past decade, the concept of outpatient TKA programs has been reported. Berger and colleagues showed promising results with an outpatient TKA program first in selected patients4 and then in an unselected cohort.5 In both studies, the authors showed successful discharges within 24 hours following TKA with low hospital readmission rates.
Given the demonstrated safety of outpatient TKA, there is great interest among health care providers and hospital administrators in characterizing its financial impact. The purpose of this study was to compare the cost minimization of a pilot outpatient same-day discharge (SDD) TKA program to that of standard inpatient TKA in matched patients. Specifically, we sought to determine both the nature and extent of any cost savings.
Methods
This prospective case–control study was conducted in accordance with the Declaration of Helsinki6 with the aim to compare the cost minimization of outpatient versus inpatient TKA. Accordingly, we obtained institutional ethics approval before the study began. Outpatient, as described in the study, refers to discharge on the same day of surgery with no overnight stay (SDD). Data from both SDD and inpatient TKA cases from a single surgeon’s practice in a tertiary academic medical centre were prospectively collected between September 2012 and October 2013. Outcome variables, including detailed case costs, patient-centred satisfaction scores, return to hospital rates and 90-day complications, were documented and compared between the first 20 SDD cases and 20 matched inpatient controls.
Patient selection
Same-day discharge patients were selected preoperatively based on low age-adjusted Charlson Comorbidity Index7 (CCI), age younger than 75 years, stable medical health with a willing caregiver at home, and patient willingness to participate in the voluntary SDD TKA program. They also had to live within 45 minutes of the hospital and have access to standardized, government-funded home care. These patients were then matched to control patients from the same surgeon’s practice who were undergoing TKA at the same site in the same fiscal year and who were enrolled in the standard inpatient clinical pathway, which was a typical contemporary rapid rehabilitation program aiming for a length of stay (LOS) of 48 hours. Patients were matched based on fiscal year, age, sex, body mass index (BMI) and comorbid conditions according to the age-adjusted CCI.
Clinical pathways
The patients were placed and treated in their respective pathways following standardized patient care maps, which included patient physiotherapy starting on postoperative day (POD) 1 and standardized clinical follow-up. All patients attended a mandatory preoperative clinic assessment with multidisciplinary resources, including social work and physiotherapy, to educate them about their upcoming procedure and address pertinent questions. This assessment occurred 4–10 weeks before the scheduled surgery date and was distinct from the preoperative assessment with the nursing and anesthesia teams which occurred 2–4 weeks before surgery. At both visits, expectation on LOS was reinforced for outpatient and inpatient protocols. All patients received similar anesthetic regimens, including spinal anesthetic where possible and standardized postoperative analgesic and antiemetic treatments. Specifically, the SDD protocol was geared to the patient being discharged on the same day of surgery after receiving a second dose of intravenous cefazolin at 8 h or vancomycin (if there was a documented allergy to cefazolin) at 10 h postoperative. Patients also had to successfully complete a mobilization test with a physical therapist that included the use of stairs. The SDD protocol included a postoperative visit from a home care nurse for a wound dressing evaluation on POD 1 and standardized physiotherapy on POD 2 followed by outpatient physiotherapy. In contrast, the inpatient group received daily physiotherapy starting on POD 1 and a wound dressing change. They were discharged once they were able to safely ambulate independently and remained stable medically with only oral analgesic requirements. Both groups had standardized follow-up clinic visits at 2 weeks, at which time the skin staples were removed, and at 6 weeks, 3 months and 1 and 2 years.
Cost data
We obtained detailed case costs, including comprehensive financial breakdown of direct, indirect and total costs, from the hospital’s finance department. Direct costs included all costs related directly to patient care, such as labour and supply costs; indirect costs comprised general operating expenses and overhead. A detailed description of the various cost components is provided in Appendix 1, available at canjsurg. ca. All hospital costs were collected in accordance with the Ontario Case Costing Initiative (OCCI), a standardized medical case costing system for Ontario hospitals based on Management Information Systems (MIS) and Ontario Healthcare Reporting Standards (OHRS) standards.8
Cost-centred outcomes
We compared median costs and differences among indirect, direct and total costs between SDD cases and matched inpatient controls. Any failure to discharge, with subsequent overnight stays or admission to hospital, and any return to hospital encounters within 90 days, regardless of whether the patient was admitted, were included into the patient’s cost. The cost of the home care visit from the nurse was also included in the SDD group. A home visit from physical therapy was provided to all patients in both groups as part of a rapid rehabilitation and discharge incentive program and was therefore considered cost-neutral.
Statistical analysis
Basic descriptive statistics (means and standard deviations for normalized data, and medians and ranges for skewed data) are reported as appropriate. For each variable, normality was assessed with a Shapiro–Wilk test, and nonparametric tests were used when necessary. We compared aggregate costs for both cohorts, including a breakdown of direct and indirect components. All statistical analyses were conducted using SPSS software version 22 (IBM).
Results
Demographic characteristics of the study sample are presented in Table 1. There were no significant differences between the groups for age, sex, BMI or CCI, suggesting they were homogeneous comparison cohorts.
Table 1.
Demographic and clinical characteristics of the study sample
| Characteristic | Group; mean ± SD or median (IQR) | p value | |
|---|---|---|---|
| SDD, n = 20 | Inpatient, n = 20 | ||
| Sex, male:female | 14:6 | 14:6 | > 0.99 |
| Age, yr | 58.5 ± 5.6 | 61.5 ± 5.9 | 0.40 |
| BMI | 29.0 ± 3.7 | 30.6 ± 5.3 | 0.27 |
| CCI | 2 (1–3) | 2 (1–6) | 0.30 |
| LOS, d | 0 | 3 (1–5) | NA |
BMI = body mass index; CCI = Charlson Comorbidity Index; IQR = interquartile range; LOS = length of stay; NA = not applicable; SD = standard deviation; SDD = same-day discharge.
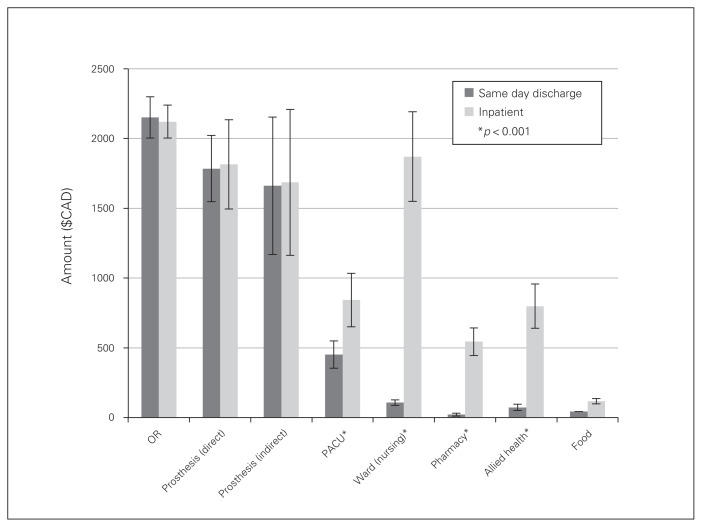
The median LOS was 2.8 (range 1–5) days for the inpatient group, which was less than the median discharge times in 2012–2013 in the province of Ontario, in keeping with an accelerated inpatient protocol. All patients in the SDD group were discharged within 10 h of surgery as planned. In every case–control match, the SDD TKA procedure was less costly than the inpatient procedure and yielded a 30% median cost savings (Appendix 1 gives representative costing for an outpatient case). Specifically, the total hospital median costs for an inpatient case was $9643.06 (range $6458.54–$14 201.67) compared with $6487.50 (range $5168–$11 490.36) for the SDD group, for a difference in median costs of $3155.56 or 32.7%. This cost reduction was shared between both direct and indirect cost attributes (Fig. 1). A more specific cost breakdown of the various aspects of patient care between the 2 groups is shown in Figure 2. The inpatient group spent more time in the postanesthesia care unit (PACU) than the SDD group, leading to a significant difference in costs between the groups. This variable was negatively influenced for the inpatient group by hospital occupancy; inpatients typically had prolonged stays in the PACU while waiting for their beds on the ward owing to delayed discharges and hospital occupancy levels above capacity. This was not captured directly for this study, but it is important to note that medical discharge criteria from the PACU were identical for both cohorts. As expected, other significant contributing costs unique to the inpatient group included surgical floor care costs (mean $1869 per inpatient), pharmacy costs (mean $543 per inpatient) and patient meals (mean $117 per patient). The high outlier SDD case was due to an additional augment component and a prolonged PACU stay corresponding to additional indirect cost inflation.
Fig. 1.
Direct, indirect and total costs comparison between same-day discharge and inpatient groups. The solid bars indicate median amounts and errors bars indicate interquartile range (IQR). *p < 0.001.
Fig. 2.
Cost breakdown between same-day discharge and inpatient groups. The solid bars indicate mean amounts and error bars indicate standard deviation. *p < 0.001. OR = operating room; PACU = postanesthesia care unit.
At 1 year, there were no major complications and no return to hospital encounters for either group and no readmissions. Minor complications included 2 patients within the first 10 cases in the SDD group with transient vasovagal episodes occurring on the day of surgery, which resolved with fluid resuscitation; no patients among the latter 10 SDD cases experienced complicatitons. No patients failed discharge or returned to hospital.
Discussion
While the merits of same day unicompartmental arthroplasty (UKA)9,10 are well documented and accepted, outpatient TKA has been much less frequently reported, likely owing to concerns of patient safety and questions surrounding its true cost minimization once societal costs have been factored in. Berger and colleagues5 reported a discharge rate within 24 hours of operation of 94% in an unselected cohort of patients undergoing same-day TKA. We have confirmed the safety of outpatient TKA and further demonstrated savings of 30% of the inpatient costs, which averaged approximately $3100 per patient in the Canadian system. There was a reduction in both direct and indirect costs with a majority of the savings coming from surgical floor care, patient meals and inpatient pharmacy costs and physiotherapy.
Our study also had no readmissions and no major complications in the outpatient cohort. Two outpatients (within the first 10 SDD cases) experienced vasovagal episodes postoperatively before discharge. There were no recurrences after modifications to the anesthetic and postoperative analgesia protocol, and neither episode prevented SDD. Although the study clearly showed a significant cost differential, it remains a pilot study and is underpowered to detect any added complication risk, specifically because the outpatient cohort was carefully selected preoperatively. The nursing visit was established to reassure patients and the surgical team that the wound dressing could be changed within 24 hours and that a general assessment could be performed for any medical concerns.
Our findings are on par with those of previous studies of outpatient arthroplasty patients. Lovald and colleagues11 performed a comparison in the US Medicare population of outpatient TKA versus short (1–2 d) inpatient stay, standard (3–4 d) inpatient stay, or extended (≥ 5 d) inpatient stay. There were mean cost savings of $8527 USD for the outpatient cases compared with the most common standard (3–4 d) LOS cohort.11 Similarly, Aynardi and colleagues12 compared the outcomes and cost-effectiveness of outpatient versus inpatient total hip arthroplasty (THA) on a selected patient population in a case–control study. Similar to our outcomes, they found a significantly decreased cost for the outpatient cohort compared with the inpatient cases ($24 529 v. $31 327, p < 0.001), with no differences in complications or estimated blood loss between the groups.12 The trend in these studies is that patients in the outpatient group have a lower comorbidity profile. Conversely, our matched cohorts did not show any significant difference in age, BMI or comorbidity index. Furthermore the median LOS was closer to 3 days in keeping with younger, healthier patients. Our study also found no increased rates for readmission for the outpatient group, and they did not have an increased likelihood of complications — a fact likely attributed to the standardized patient pathway that included preoperative education, home nursing visits and modern occlusive dressings.
The financial benefits associated with outpatient TKA can have an immense impact on the operating budgets of public hospitals. Health care spending in Canada has continued to grow since the inception of the Canada Health Act. Currently, Canada spends approximately 11% of its gross domestic product (GDP) on health care, a number that is expanding by approximately 2% per year.13 In Ontario, approximately 42% of tax dollars are allocated to health care, a number that is expected to rise if spending is not curtailed.14 Classically, hospitals were funded on a global budget, a provider-centric model based on nonmedical factors, including previous budgets, rates of inflation, capital investment decisions and lobbying. The Ontario government now has a new objective, evidence and health-based allocation model.15 Quality-based procedures (QBP),3 such as TKA, are reimbursed a specific dollar figure based on the 40th percentile of the provincial average cost of the procedure, with hospital-specific multipliers for patient medical complexity. From a cost perspective, an outpatient TKA program can create the opportunity for value in patient care, where value can be defined as providing an equivalent level of care at a reduced cost.16 The cost per case in this study came well under the QBP price paid by the provincial Ministry of Health, and helped to subsidize higher-cost revision cases. In fact, the cost per case may be further reduced now given the recently improved costing methods implemented in Ontario, as the year-to-year differences and the wide range of costs in this study would likely be eliminated. The concerns that some of the costs of outpatient surgery will be borne by the patient are also unfounded. For example, physiotherapy costs in the first 2 weeks are borne by the public health care system in the form of home care, regardless of whether the patient is an inpatient or outpatient. Furthermore, the advent of novel occlusive dressings that can be left on has already reduced the need for the nursing visits as a routine in our current practice,17 resulting in more savings.
Limitations
The strengths of this study rely upon detailed hospital costing methodologies, which accurately portray the direct, indirect and total costs attributed to the care of both cohorts of patients. Furthermore, the groups were closely matched on patient demographics known to influence the cost of health care. The limitations of this pilot study lie in its small sample size, as it may have been underpowered to identify any added complication risks. Patient selection may also be perceived as a weakness as our patients were generally healthier and moderately younger than the average TKA patient. This is, however, becoming more relevant as North American trends forecast continued growth in the percentage of patients younger than 65 years expected to receive TKA, which is now well over 50% and represents a major contributor to the absolute annual increases seen in both countries.18 The 30% savings estimate approaches previously reported inpatient cost estimates for primary TKA, where 28% of total costs were allocated to the room and board and ward costs.2,19 As such, the costs incurred are likely representative of savings that other hospitals could realize given that the median LOS of 3 days in the inpatient cohort would be expected for similar patients in other settings.
Conclusion
Outpatient TKA is a safe and cost-effective alternative to inpatient TKA in selected individuals. Savings were achieved largely from costs associated with the inpatient stay, including ward, pharmacy and meal costs. Future studies will be required to confirm the safety of this protocol in unselected patients, and efforts to enhance the safety of the pathway could make this a more mainstream alternative beyond the increasingly younger and healthier cohort of patients undergoing TKA.
Acknowledgements
The authors thank Ginette Bisson from the finance department of The Ottawa Hospital, who helped retrieve and clarify the case costing data for the 2 groups of patients, and Johanna Dobransky for her assistance in manuscript preparation for submission
Footnotes
Presented at the American Orthopedic Association/ Canadian Orthopaedic Association Combined Meeting 2014
Funding: The study received funding from The Ottawa Hospital Academic Medical Organization Innovation Fund. The views expressed in the submitted article are those of the authors and are not an official position of the institution or funder.
Competing interests: None declared.
Contributors: A. Huang and G. Dervin designed the study. A Huang acquired the data, which all authors analyzed. All authors wrote and reviewed the manuscript and approved the final version for publication.
References
- 1.Lavernia CJ, Guzman JF, Gachupin-Garcia A. Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop Relat Res. 1997;345:134–9. [PubMed] [Google Scholar]
- 2.Cram P, Lu X, Kates SL, et al. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ontario HQ. Quality-based procedures: clinical handbook for primary hip and knee replacement [Internet] Toronto (ON): Health Quality Ontario; 2013. pp. 1–95. [Google Scholar]
- 4.Berger RA, Sanders S, Gerlinger T, et al. Outpatient total knee arthroplasty with a minimally invasive technique. J Arthroplasty. 2005;20:33–8. doi: 10.1016/j.arth.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Berger RA, Kusuma SK, Sanders SA, et al. The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res. 2009;467:1443–9. doi: 10.1007/s11999-009-0736-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 7.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 8.Ontario MHLTC. Ontario Case Costing Guide Version. 2014;9:1–144. [Google Scholar]
- 9.Dervin GF, Madden SM, Crawford-Newton BA, et al. Outpatient unicompartment knee arthroplasty with indwelling femoral nerve catheter. J Arthroplasty. 2012;27:1159–1165.e1. doi: 10.1016/j.arth.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Munk S, Dalsgaard J, Bjerggaard K, et al. Early recovery after fast-track Oxford unicompartmental knee arthroplasty. 35 patients with minimal invasive surgery. Acta Orthop. 2012;83:41–5. doi: 10.3109/17453674.2012.657578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lovald ST, Ong KL, Malkani AL, et al. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. 2014 Mar;29:510–5. doi: 10.1016/j.arth.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 12.Aynardi M, Post Z, Ong A, et al. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J. 2014;10:252–5. doi: 10.1007/s11420-014-9401-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canadian Institute for Health Information. National health expenditure trends, 1975 to 2014. Ottawa (ON): CIHI; 2014. [accessed 2017 Jan. 11]. Available: www.cihi.ca/en/nhex_2014_report_en.pdf. [Google Scholar]
- 14.Ontario MHLTC. Ontario’s Action Plan. Health Care (Don Mills) 2012:1–16. [Google Scholar]
- 15.Canadian Health Services Research Foundation. Hospital payment mechanisms: an overview and options for Canada. Ottawa (ON): the Foundation; 2011. pp. 1–26. [Google Scholar]
- 16.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–81. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 17.Hopper GP, Deakin AH, Crane EO, et al. Enhancing patient recovery following lower limb arthroplasty with a modern wound dressing: a prospective comparative audit. J Wound Care. 2012;21:32–2. doi: 10.12968/jowc.2012.21.4.200. [DOI] [PubMed] [Google Scholar]
- 18.Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–12. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maradit Kremers H, Visscher SL, Moriarty JP, et al. Determinants of direct medical costs in primary and revision total knee arthroplasty. Clin Orthop Relat Res. 2012;471:206–14. doi: 10.1007/s11999-012-2508-z. [DOI] [PMC free article] [PubMed] [Google Scholar]