Summary
Background
Code status (CS) of a patient (part of their end-of-life wishes) can be critical information in healthcare delivery, which can change over time, especially at transitions of care. Although electronic health record (EHR) tools exist for medication reconciliation across transitions of care, much less attention is given to CS, and standard EHR tools have not been implemented for CS reconciliation (CSR). Lack of CSR creates significant potential patient safety and quality of life issues.
Objective
To study the tools, workflow, and impact of clinical decision support (CDS) for CSR.
Methods
We established rules for CS implementation in our EHR. At admission, a CS is required as part of a patient’s admission order set. Using standard CDS tools in our EHR, we built an interruptive alert for CSR at discharge if a patient did not have the same inpatient (current) CS at discharge as that prior to admission CS.
Results
Of 80,587 admissions over a four year period (2 years prior to and post CSR implementation), CS discordance was seen in 3.5% of encounters which had full code status prior to admission, but Do Not Resuscitate (DNR) CS at discharge. In addition, 1.4% of the encounters had a different variant of the DNR CS at discharge when compared with CS prior to admission. On pre-post CSR implementation analysis, DNR CS per 1000 admissions per month increased significantly among patients discharged and in patients being admitted (mean ± SD: 85.36 ± 13.69 to 399.85 ± 182.86, p<0.001; and 1.99 ± 1.37 vs 16.70 ± 4.51, p<0.001, respectively).
Conclusion
EHR enabled CSR is effective and represents a significant informatics opportunity to help honor patients’ end-of-life wishes. CSR represents one example of non-medication reconciliation at transitions of care that should be considered in all EHRs to improve care quality and patient safety.
Keywords: Code status, advance directive, meaningful use, reconciliation, medication, DNR
Background and Significance
Advanced cardiac life support (ACLS), including cardiopulmonary resuscitation (CPR) and other measures, is part of the standard of care for patients who experience cardiac and/or respiratory arrest during hospitalizations. One of the primary tenets of patient-centered care is incorporating the desires of patients and their families for end-of-life care and resuscitation needs into care plans. These advanced directives for ACLS are commonly referred to as a patient’s code status. The code status communicates to the medical team if ACLS measures should be administered during cardiopulmonary arrest [1]. Documentation of code status is a key quality measure to improve end-of-life experience desired by the patient [2]. The Department of Health and Human Services’ Meaningful Use program identifies honoring a patient’s end-of-life wishes as one of its major objectives in improving patient care quality and safety, and has had recording the presence of advance directives for patients 65 and older as a core objective beginning in Stage 1 of Meaningful Use [3]. Documenting code status in electronic records helps to create a ready reference for care providers and facilitates smoother transition of patient care. However, code status is frequently documented incompletely and inconsistently in the patient’s electronic health records (EHR) [4, 5]. Unless a code status order to the contrary is documented in the patient’s EHR, the patient is assumed to have a full code status and ACLS measures are initiated on every patient in the hospital who undergoes cardiopulmonary arrest, even if death is expected. Thus, discussing patients’ preferred code status and documenting it accurately is important, so that patient‘s desired end-of-life resuscitation wishes may be clearly documented in the EHR and honored fully [6].
As modern healthcare systems have advanced, inadequate communication systems and processes continue to be a significant barrier to effectively honoring patient’s ACLS wishes for cardio-pulmonary arrest [7]. Since code status may change during an inpatient admission or hospitalization, code status reconciliation (CSR) at discharge is especially important to maintain patients’ end-of-life resuscitation wishes across transitions of care. In addition, in Ohio and in our healthcare system, multiple Do Not Resuscitate (DNR) variants exist which can create confusion for caregivers. EHR clinical decision support (CDS) tools can help with information reconciliation across transitions of care, which typically have been limited to medication reconciliation.
Objectives
In our healthcare system, with the same EHR throughout all inpatient, emergency room, surgical/procedural and outpatient sites, all inpatients receive a code status order by computerized physician order entry at admission. Inpatient code status orders, like all active inpatient orders, are automatically discontinued two hours after discharge. Like medications, code status orders placed during a prior admission or in an outpatient encounter are invalidated upon admission. However, prior to this work, no structured process or technology tools forced CSR between current and prior code status at the time of admission or discharge. As a result, for a patient coming to the hospital there was no valid code status in the patient’s chart to guide the physician on the resuscitation needs of the patient, especially in an emergent situation. This led to at least one patient in which full resuscitation was performed, even though the prior code status was DNR. The objective of this work was to study the tools, workflow, and impact of CDS for CSR at discharge.
Materials and Methods
The MetroHealth System is an integrated public/safety-net healthcare delivery system with the Epic EHR (Verona WI) since 1999. Our EHR is well deployed (Healthcare Informatics Management and Systems Society Electronic Medical Record Adoption Model Stage 7 ambulatory and hospital [2014]) throughout all ambulatory, emergency departments, surgical/procedural, and inpatient areas [8]. To address CSR, we took the same basic methods and tools of medication reconciliation and applied them to CSR, using the five rights of CDS [9].
Ohio‘s DNR or non-full code status law recognizes two orders: (1) DNR Comfort Care (DNRCC), which is activated immediately upon signing, and (2) DNR Comfort Care – Arrest (DNRCC-A), which is activated at the moment of cardiac or respiratory arrest. The standard DNRCC-A order specifically excludes intubation; however a significant minority of patients (especially those with chronic respiratory diagnoses) desire intubation in case of respiratory arrest. Accordingly, in our healthcare system we have subdivided the DNRCC-Arrest code status order into DNRCC-Arrest-Intubate (DNRCC-A-I) and DNRCC-Arrest-Do Not Intubate (DNRCC-A-DNI). Thus in our healthcare system, four different code statuses exists – Full Code, DNRCC, DNRCC-A-I and DNRCC-A-DNI.
We established rules for code status implementation in our EHR. At admission a code status order is required as part of patients’ admission order set. We implemented CSR at discharge such that if the patient has the same inpatient (current) code status at discharge as the prior to admission code status, the inpatient code status is automatically continued as the patient’s outpatient code status. If any discrepancy exists between an inpatient (current) code status at discharge and the prior to admission code status at the time the patient’s discharge order is signed, we used standard CDS tools in our EHR to create an interruptive alert (► Figure 1), forcing CSR to be addressed by the care provider. The interruptive alert shows the providers the discrepancy between the current code status and the prior to admission code status and forces the provider to pick one of the four possible code statuses to be the outpatient code status after discharge. The provider cannot make the CSR alert go away and there is no way to by-pass this alert at discharge without selecting a code status to be the outpatient code status after discharge. This is similar to the approach we use to force the discharging provider to address medication reconciliation at the time of discharge. As part of this effort, we also reconfigured the patient’s code status to be more prominently displayed in all EHR headers. Finally, we enabled clicking on the code status in the patient’s header to show current and prior code status details.
Fig. 1.

Interruptive Code Status Reconciliation Alert at Signing of Discharge Order it Prior to Admission and Inpatient (Current) Code Status is Discordant. © 2017 Epic Systems Corporation. Used with permission.
CSR was implemented on 2/1/2014. For this analysis, we divided our study period into 48 one-month time intervals (24 months before and 24 months after our intervention). We utilized de-identified EHR meta-data to evaluate: 1) the number of code status orders placed during a single inpatient admission, 2) the active code status (if any) at the moment of admission for every admission during each one-month interval, and 3) whether or not each outpatient code status in our system was active at any time during each one-month interval. Data were analyzed in Microsoft Excel. Calculated differences between number of code statuses per 1000 admissions per month (to ensure findings were not confounded by changes in the number of admitted/discharged patients over time) prior to and post CSR implementation were evaluated using the Mann-Whitney U test.
Results
During the four year analysis period, 80,587 admissions occurred. Two years prior to CSR implementation on 2/1/2014, 48,810 admissions occurred; while 31,777 admissions occurred post CSR implementation. For the 80,587 admissions, 91.31% (92,211) of the code status orders placed during the four year study period were for Full Code, 2.27% (2296) for DNRCC, 1.78% (1800) for DNRCC-A-I, and 4.63% (4679) for DNRCC-A-DNI. Code status orders placed or changed during a single inpatient hospital admission for the same patient ranged from 1–10 times (► Table 1). Code status discordance was seen in 3.5% of encounters. These encounters had full code status prior to admission, but DNR code status at discharge. In addition, 1.4% of the encounters had a different variant of the DNR code status at discharge when compared with the DNR code status prior to admission.
Table 1.
Number of code status orders placed for a patient during a single inpatient hospital admission over the 4 year study period. (n=80,587)
| Total no of Code Status Orders Placed | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Frequency | 65518 | 11535 | 2391 | 716 | 279 | 98 | 29 | 15 | 5 | 1 |
| Percent | 81.3 | 14.3 | 3.0 | 0.9 | 0.3 | 0.1 | <0.1 | <0.1 | <0.1 | <0.1 |
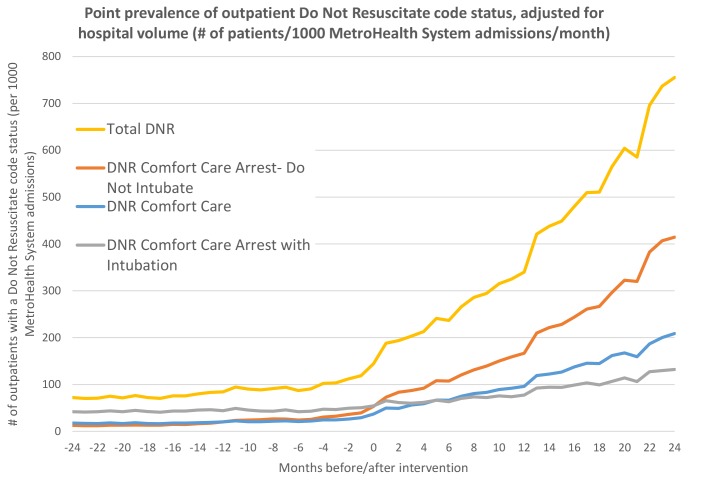
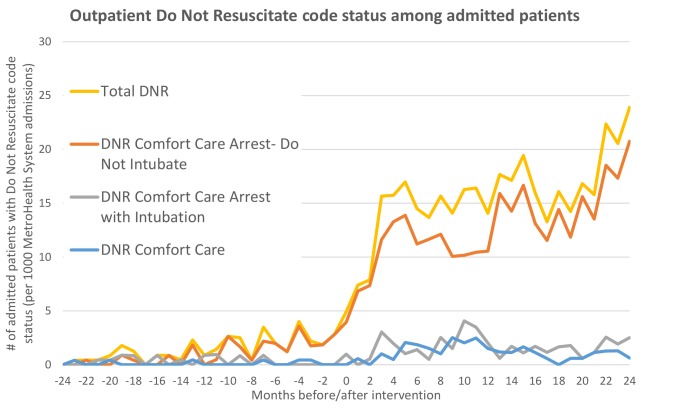
We compared active outpatient code status among patients discharged, after excluding patients that were admitted. Post CSR implementation, the number of active DNR code statuses per 1000 admissions per month increased from 85.36 ± 13.69 to 399.85 ± 182.86, p<0.001 (mean ± SD). This increase was seen in all the three variants of DNR code status (► Figure 2). We also analyzed the outpatient code status of patients being admitted. We found a significant increase in the number of active DNR code statuses per 1000 admissions per month post CSR implementation (1.99 ± 1.37 vs 16.70 ± 4.51, p<0.001; (mean ± SD)). This was due to an increase in all the three variants of DNR code status (► Figure 3). Thus, the significant increase in the number of valid DNR code status among discharged patients because of CSR at discharge was mirrored by a significant increase in the number of DNR code status in patients being admitted.
Fig. 2.
Number of outpatients with Do Not Resuscitate code status per 1000 admissions per month among all outpatient patients, during Pre and Post Discharge Code Status Reconciliation implementation (0 months on y-axis is date of code status reconciliation implementation).
Fig. 3.
Number of outpatients with Do Not Resuscitate code status per 1000 admissions per month among patients being admitted to the hospital, during Pre and Post Discharge Code Status Reconciliation implementation (0 months on y-axis is date of code status reconciliation implementation).
Discussion
Implementing standard EHR CDS building blocks and applying them to CSR can have a significant impact on CSR. For the first time in medical literature, to the best of our knowledge, we have implemented and reported on the results of CSR in an EHR. As seen in our study, a patient’s code status can change multiple times during the same admission, and even if only ordered once, can be different from the patient’s prior-to-admission code status. Studies show that code status orders for critically ill patients are frequently miscommunicated between attending physicians, house staff and nurses [10], with more than 70% of caregivers recalling situations when confusion around a code status order led to problems in patient care [11], leading to important quality and patient safety issues. Thus, with multiple code status changes during a single admission, the code status of a patient in the EHR when discharged should be thoughtfully considered, especially when the discharge code status differs from the code status prior to admission.
As expected, we saw a significant (>4-fold) increase in number of patients discharged with a valid DNR code status post CSR implementation. This increase in discharge DNR code status post CSR implementation eventually manifests itself in a significant (>8-fold) increase in patients being admitted to the hospital with a valid DNR code status, thereby potentially avoiding unwanted ACLS measures. Because non-full code or DNR code status make up less than 8.7% of all code statuses, and because a patients’ “default” code status is full code, CSR should make much more of an impact on non-full code status patients.
Documenting code status is important in preventing undesired resuscitation and improving patient safety outcomes. It provides a more predictable environment for patients, families, and providers. ACLS measures can have negative consequences such as physical distress, loss of dignity and family suffering with complicated bereavement, in patients who do not want resuscitation [12]. Expensive resources such as emergency medical technician personnel and equipment, emergency room visits, intensive care unit stays, and acute hospitalizations may be used more prudently in patients who have a known code status [1, 13]. Without clear and proper documentation, end-of-life decisions and the dignity of the patient may be compromised because of a simple, easily avoided miscommunication. Thus having a known code status in the patient’s EHR, specifically during emergency situations, can lead to avoidance of ineffective clinical interventions that may compromise patient safety and increase suffering and/or cause harm. The optimal timing to discuss end-of-life care and resuscitation preferences are well in advance of the patient’s cardiopulmonary arrest, with the decisions clearly documented in the EHR. Decisions regarding intubation are often made urgently in high stress environments such as emergency rooms or hospital setting, which limits the opportunity for patients and their families to consider their options for care thoroughly [14, 15]. Thus, it is important that the decisions regarding code status made during outpatient visits or a prior hospitalization are reflected in the EHR for future healthcare system encounters.
This study has limitations. This study only documented a significant increase in valid code status in the EHR, but it does not necessarily mean improved adherence to a patient’s end-of-life resuscitation wishes. However, presumably documenting a patient’s resuscitation wishes more accurately should lead to better adherence to a patient’s end-of-life resuscitation wishes. Further studies are needed to evaluate whether having a valid code status in the EHR translates to delivery of appropriate ACLS measures to improve the end-of-life resuscitation wishes of the patients. Also, we did not implement or evaluate CDS tools to force CSR at admission to the healthcare system. Implementing CDS for CSR at admission could also have a positive impact on adherence to a patient’s end-of-life resuscitation wishes. However, we expect this impact to be minimal because our standard admission process necessitates updating a patient’s code status in the EHR by computerized physician order entry, and any discrepancies between prior to admission code status and prior inpatient code status would already be reconciled at discharge through the CSR process implemented.
Stage 1 of Meaningful Use requires that more than 50% of unique patients 65 years and older admitted to an eligible hospital or critical access hospital have an indication of advanced directive status recorded in their EHR. Stage 2 goes further, requiring the advanced directive to be included as structured data. Having advanced directives in structured format, and then having CSR at discharge, we are more likely to have an accurate code status in all care settings (inpatient, outpatient, ED, etc.) [3]. Medication reconciliation in EHRs significantly reduces medication errors and improves patient safety outcomes [16]. Similarly, we believe having a valid and accurate code status in the EHR should, over time, reduce communication errors, especially in emergent situation, by honoring patient’s end-of-life resuscitation wishes and avoiding unnecessary resuscitation attempts, thus improving patient safety and quality of care. The opportunity and relative effectiveness of CDS for CSR also points to the potential of CDS for other non-medication EHR data where reconciliation at transitions of care may improve patient safety and quality of care. One example is reconciliation of diet, activity, oxygen and other durable medical equipment requirement/settings; especially when the discharge information/instructions/orders in these areas differ from the prior to admission information/instructions/orders.
Conclusion
In summary, implementation of CSR, using standard EHR CDS building blocks, significantly improved the number of patients leaving the hospital with a valid DNR code status. This increase in DNR code status at discharge led to a significant increase in the number of patients with a valid DNR code status returning to the healthcare system for admission, thus potentially avoiding unnecessary resuscitation attempts, and improving patient safety and quality of care. Further studies on the impact of having a valid code status in the EHR post CSR implementation and its effect on the patient’s end-of-life care are needed. EHR enabled CSR is effective and represents a significant informatics opportunity to help honor patients’ end-of-life resuscitation wishes. EHR enabled information reconciliation for other non-medications should be investigated to improve patient safety and quality of care.
Abbreviations
- ACLS
Advanced Cardiac Life Support
- CSR
Code Status Reconciliation
- CPR
Cardio-Pulmonary Resuscitation
- CDS
Clinical Decision Support
- DNR
Do Not Resuscitate
- DNRCC
DNR Comfort Care
- DNRCC-A-I
DNR Comfort Care – Arrest – Intubate
- DNRCC-A-DNI
DNR Comfort Care – Arrest – Do Not Intubate
- EHR
Electronic Health Records
Multiple Choice Question
Documentation of which of the following is a key quality measure to improve end-of-life experience desired by the patient?
Dietary restrictions
Code status
Religious following
Exercise tolerance
Documentation of code status is a key quality measure to improve end-of-life experience desired by the patient. However, code status is frequently documented incompletely and inconsistently in the patient’s electronic health records (EHR). Unless a code status order to the contrary is documented in the patient’s EHR, the patient is assumed to have a full code status and resuscitation measures are initiated on every patient in the hospital who undergoes cardiopulmonary arrest, even if death is expected. Thus, discussing patients’ preferred code status and documenting it accurately is important, so that patient‘s desired end-of-life resuscitation wishes may be clearly documented in the EHR and honored fully.
Implementation of Code Status reconciliation (CSR) using standard EHR clinical decision support building blocks, significantly improves the number of patients leaving the hospital with a valid code status, thus potentially avoiding unnecessary resuscitation attempts, and improving patient safety and quality of care. EHR enabled CSR is effective and represents a significant informatics opportunity to help honor patients’ end-of-life resuscitation wishes.
Footnotes
Clinical Relevance Statement
To date, clinical and informatics information reconciliation efforts across transitions of care typically have focused solely on medications. Here we demonstrate the tools and value of code status reconciliation as an example of non-medication information that could be reconciled across transitions of care to improve patient safety and quality of care.
Conflict of Interest
None declared.
Protection of Human and Animal Subjects
Because this effort was initiated and evaluated for operational and quality improvement purposes and because only EHR metadata was used in the analysis (only dates and frequencies of code status/orders), Institutional Review Board approval was not sought or obtained for this project.
Authors Contribution
VGJ was responsible for writing the first draft, data collection, interpretation & analysis. PJG was responsible for designing the code status reconciliation, data collection, interpretation & analysis, and critical review of manuscript. DK was responsible for the study design, data analysis & interpretation, and critical review of manuscript.
References
- 1.Temel JS, Greer JA, Admane S, Solis J, Cashavelly BJ, Doherty S, Heist R, Pirl WF. Code status documentation in the outpatient electronic medical records of patients with metastatic cancer. J Gen Intern Med 2010; 25(2):150–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collier KS, Kimbrel JM, Protus BM. Medication appropriateness at end of life: a new tool for balancing medicine and communication for optimal outcomes-the BUILD model. Home Healthc Nurse 2013; 31(9):518–524. [DOI] [PubMed] [Google Scholar]
- 3.Bates D. Draft Recommendations Meaningful Use Stage 3 2013. [Accessed 10/18/16]; Available from: https://www.healthit.gov/FACAS/sites/faca/files/muwg_stage3_draft_rec_07_aug_13_.v3.pdf.
- 4.Weinerman AS, Dhalla IA, Kiss A, Etchells EE, Wu RC, Wong BM. Frequency and clinical relevance of inconsistent code status documentation. J Hosp Med 2015; 10(8):491–496. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia HL, Patel NR, Choma NN, Grande J, Giuse DA, Lehmann CU. Code status and resuscitation options in the electronic health record. Resuscitation 2015; 87: 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neubauer MA, Taniguchi CB, Hoverman JR. Improving incidence of code status documentation through process and discipline. J Oncol Pract 2015; 11(2): e263-e266. [DOI] [PubMed] [Google Scholar]
- 7.Schiebel N, Henrickson Parker S, Bessette RR, Cleveland EJ, Neeley JP, Warfield KT, Barth MM, Gaines KA, Naessens JM. Honouring patient‘s resuscitation wishes: a multiphased effort to improve identification and documentation. BMJ Qual Saf 2013; 22(1):85–92. [DOI] [PubMed] [Google Scholar]
- 8.EMRAM Stage Criteria. 2015. [Accessed 10/15/16]; Available from: http://www.himssanalytics.org/research/emram-stage-criteria
- 9.Campbell R. The five „rights“ of clinical decision support. J AHIMA 2013; 84(10): 42-47; quiz 48. [PubMed] [Google Scholar]
- 10.Heffner JE, Barbieri C. Compliance with do-not-resuscitate orders for hospitalized patients transported to radiology departments. Ann Intern Med 1998; 129(10):801–805. [DOI] [PubMed] [Google Scholar]
- 11.Sehgal NL, Wachter RM. Identification of inpatient DNR status: a safety hazard begging for standardization. J Hosp Med 2007; 2(6):366–371. [DOI] [PubMed] [Google Scholar]
- 12.Ardagh M. Futility has no utility in resuscitation medicine. J Med Ethics 2000; 26(5):396–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar P, Temel JS. End-of-life care discussions in patients with advanced cancer. J Clin Oncol 2013; 31(27):3315–3319. [DOI] [PubMed] [Google Scholar]
- 14.Kernerman P, Cook DJ, Griffith LE. Documenting life-support preferences in hospitalized patients. J Crit Care 1997; 12(4):155–160. [DOI] [PubMed] [Google Scholar]
- 15.Mack JW, Cronin A, Taback N, Huskamp HA, Keating NL, Malin JL, Earle CC, Weeks JC. End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med 2012; 156(3):204–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenwald JL, Halasyamani L, Greene J, LaCivita C, Stucky E, Benjamin B, Reid W, Griffin FA, Vaida AJ, Williams MV. Making inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. J Hosp Med 2010; 5(8):477–485. [DOI] [PubMed] [Google Scholar]