Abstract
Objective: We evaluated the evidence supporting the use of virtual reality among patients in acute inpatient medical settings.
Method: We conducted a systematic review of randomized controlled trials conducted that examined virtual reality applications in inpatient medical settings between 2005 and 2015. We used PsycINFO, PubMed, and Medline databases to identify studies using the keywords virtual reality, VR therapy, treatment, and inpatient.
Results: We identified 2,024 citations, among which 11 met criteria for inclusion. Studies addressed three general areas: pain management, eating disorders, and cognitive and motor rehabilitation. Studies were small and heterogeneous and utilized different designs and measures. Virtual reality was generally well tolerated by patients, and a majority of studies demonstrated clinical efficacy. Studies varied in quality, as measured by an evaluation metric developed by Reisch, Tyson, and Mize (average quality score=0.87; range=0.78–0.96).
Conclusion: Virtual reality is a promising intervention with several potential applications in the inpatient medical setting. Studies to date demonstrate some efficacy, but there is a need for larger, well-controlled studies to show clinical and cost-effectiveness.
Keywords: virtual reality, treatment efficacy, inpatients, pain management, eating disorders, rehabilitation
INTRODUCTION
Overview. Since the 1990s, virtual reality (VR) has had promising applications in science and medicine, including intervention delivery.1–4 Use of VR interventions has been studied in a wide range of medical conditions, including anxiety, phobias, obesity, chronic pain, and eating disorders.1,5–10 In recent years, VR technology has become increasingly affordable, immersive, flexible, and portable, enabling its use in a broad range of environments, including the inpatient medical setting.1,7,11 The capacity of VR to modulate subjective experience makes it a compelling intervention in inpatient medical settings, where VR may offer respite from the confining nature of medical wards, or where it may augment or replace analgesics in pain management. To date, no systematic review has been conducted on the use of VR in the inpatient medical setting. Herein, we review controlled studies evaluating the utility and efficacy of VR-based treatments for patients admitted to hospitals or rehabilitation centers.
VR and its use in healthcare. VR refers to the interactions between an individual and a computer-generated environment stimulating multiple sensory modalities, including visual, auditory, or haptic experiences.9 The user’s perception of reality is facilitated by the use of head-mounted displays (HMDs, in goggles or headsets), wall projectors, and/or gloves fitted with sensors or touch-sensitive motors. Sensors may allow researchers to monitor and record a patient’s level of interactivity (known as “immersion” or “presence”) in a way that is reliable, safe, and replicable.3
VR’s immersive, entertaining effects are useful for redirecting the patient’s attention away from painful treatment experiences and reducing anxiety, discomfort, or unpleasantness.12 VR has been utilized in many studies to distract (often pediatric) patients during wound redressing in burn care, and in exposure therapy for phobias or posttraumatic stress disorder (PTSD) as a substitute for imagination of a feared environment.7 VR has been used to treat eating disorders and obesity, allowing patients to improve body image perceptions and promote healthier eating habits by inhabiting realistic avatars in stress-inducing virtual situations, such as food shopping.7 VR is also used for patient motor rehabilitation, aiding patients to reacquire specific skills and improve body movement in virtual environments that are less dull or discouraging than standard gym exercises.7
METHODS
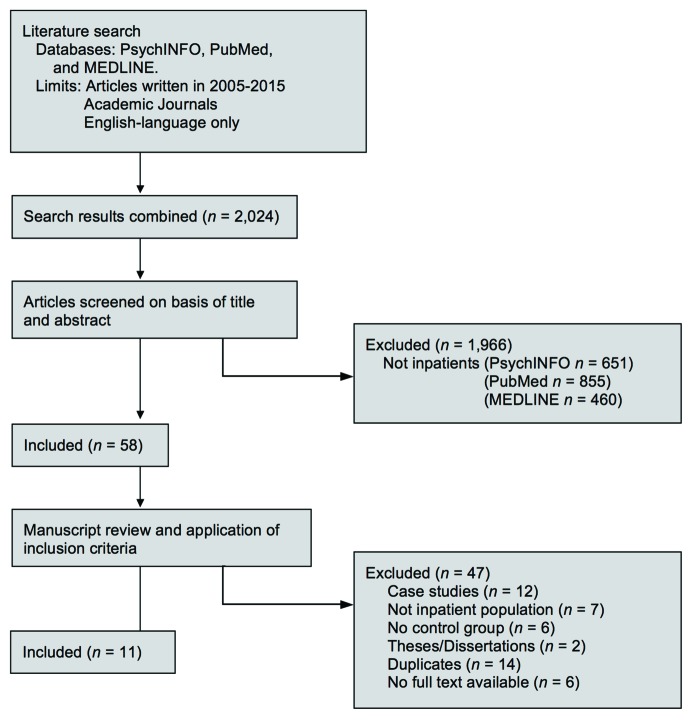
Literature search strategy. We reviewed all controlled trials of VR in inpatient medical settings published over the last 10 years. We used PsycINFO, PubMed, and Medline electronic databases to identify studies from 2005 to 2015, based on the following keywords: virtual reality, VR therapy, treatment, and inpatient. We also reviewed reference lists of previous reviews and meta-analyses to identify titles not captured in our initial search. We excluded trials with no control or comparison group, case studies, outpatient studies, theses or dissertations, and articles not published in the English language. As displayed in Figure 1, our initial search yielded 2,024 citations of journal articles written in English over the last decade. We discarded 1,966 citations not involving inpatient populations and reviewed the remaining 58 studies in more detail. We excluded 42 of these studies because they did not meet all inclusion criteria, were duplicates, or because the full text was not available. We grouped the final 11 eligible studies based on their application of VR to three broad medical conditions: pain distraction, eating disorders/obesity, and cognitive/motor rehabilitation. These studies are described in Table 1.
FIGURE 1.
Flowchart of search strategy and study selection process
TABLE 1.
Studies using virtual reality (VR) as a tool for improving medical conditions
| APPLICATION | FIRST AUTHOR (YEAR) | EQUIPMENT | PARTICIPANTS | STUDY DESIGN | OUTCOME/EFFECTIVENESS (PRIMARY RESULT) | SECONDARY OBSERVATIONS | AVERAGE QUALITY SCORE |
|---|---|---|---|---|---|---|---|
| Pain distraction | Schmitt et al15 (2011) | Head-mounted disolays (HMD) (Kaiser-Electro Optics) | n=54; hospitalized pediatric burn inpatients aged 6–19 years; not randomized. | Within-subject: both VR and non-VR in each session. Each patient was his own control. 30–40 min/ session; 1–5 days. | VR as effective analgesic treatment in conjunction with physical therapy: 27–44% decrease (p<0.05) in pain ratings during first session of VR condition, was maintained in subsequent sessions. | Improved affect, “fun,” decreased time thinking about pain. 16% reported mild nausea. | 0.96 |
| Pain distraction | Kipping et al18 (2012) | Low-cost, off-the-shelf HMD: eMagin Z800 3DVisor | n=41; adolescents (aged 11–17 years) in hospital/burn centers | Randomized, controlled trial (RCT) with parallel group design: VR group and standard distraction group (SDG); watched TV, listened to music, etc | No significant differences in self-reported pain in VR vs. SDG; however, nursing staff reported observing a statistically significant reduction in pain scores when helping patients with dress removal | No side effects observed; no differences b/t conditions in reporting nausea | 0.94 |
| Pain distraction | Morris et al19 (2010) | Low-cost, off-the-shelf, HMD: eMagin Z800 3DVisor. Walt Disney’s Chicken Little PC game software | n=11; adult burn patients undergoing physiotherapy | Within-subject, random assignment to VR (20min session) and non-VR. | Marginally insignificant (p=0.06) difference between VR and non-VR conditions in terms of pain reduction; no significant decrease (p=0.58) in anxiety | Low-cost VR therapy may be promising for developing countries with stringent budgets. | 0.89 |
| Pain distraction | Hoffman et al20 (2008) | Fiberoptic water-friendly VR HMD system (SnowWorld) | n=11; aged 9–40 years (M=27) hospitalized inpatients at a burn center | Controlled, within-subject, order randomized; single wound care session: 3-min w/no distraction; 3-min with VR; used subjective pain ratings scales (GRS) from 0–10. | Significant reduction in pain reported in VR sessions; those reporting highest pain (>7.6) in non-VR had 41% reduction in pain in VR condition | Patients reporting strongest “immersion” in VR environment reported greatest analgesic effect and had greatest drop in pain ratings (from 7.2–3.7) | 0.85 |
| Pain distraction | Patterson et al21 (2010) | HMD showing a virtual valley with a lake; hpnosis delivered by the experimenter to induce relaxation (e.g., “your body feels very good… you will only have positive experiences”) | n=21 patients (M=31.8 years old) at a trauma center; injuries included motor vehicle accidents, gunshot wounds, bone fractures, and joint dislocations | All received analgesic care (opioids and benzodiazepines); 1 experimental condition: VR w/hypnotic distraction (VRH; 40min); and 2 controls: VR without hypnosis, and standard care alone. | 0–10 GRS ratings for pain intensity and unpleasantness decreased | Not Applicable | 0.78 |
| Pain distraction | Li et al25 (2011) | PlayMotion system w/out HMD; video projectors capture body movements and transforms walls into play spaces | n=122; children (8–16 years old) with cancer at a pediatric oncology ward in Hong Kong; not randomized | Pre-/post-test between subjects design; 30-min therapeutic play interventions 5 days a week | Fewer depressive symptoms in experimental group after 1 week; no significant differences in anxiety levels. | Not Applicable | 0.83 |
| Pain pistraction | Carrougher et al17 (2009) | HMD (Nvis Nvisor) SnowWorld software | n=39 adult patients with burn injuries at a burn center | Within-subjects crossover; 2-day study (randomize): standard medication given on both days (OxyContin or Methadone); VR day: 10-min treatment; self-reported pain scores and range of motion (ROM) assessed before and after each session | Reductions in VR condition of 27% for worst pain, 37% for time spent thinking about pain, 31% for pain unpleasantness; no statistically significant improvements in ROM | 2 patients withdrew; 97% reported none to mild nausea after using VR equipment | 0.91 |
| Eating disorders/obesity | Cesa et al26 (2013) | NeuroVR 2 software; HMD showing virtual environments +2 body image comparisons. | n=90 women with binge eating disorder (BED) at rehab center | Random assignment: (n=31 CBT+VR, n=30 CBT, n=29 usual care inpatient regimen [IP]); 15 weekly group sessions over 5 weeks | Body image concerns (BIAQ) improvement and weight loss aid in CBT+VR only; overall improvements in body satisfaction (BSS and CDRS) in all 3 conditions | 34.6% of patients dropped out after 1-year follow-up; increased weight gain in all 3 after 1 year | 0.85 |
| Eating disorders/obesity | Manzoni et al27 (2009) | HMD: VE called Green Valley showed mountain landscape with relaxing lake scenes; participants asked to walk around, observe nature, then sit down on a bench and relax. Imaginative condition: psychologists asked participants to imagine similar environments. | n=60; adult female inpatients at a weight reduction facility in Italy | 12 relaxation training sessions (4 per week) over 3 weeks either with VR, traditional imagination treatments, or standard hospital care (control) | At 3-month follow-up: VR condition—reduced emotional eating; both relaxation training conditions (VR and Imaginative) helped reduce emotional eating (WELSQ; EOQ), anxiety (STAI), depressive symptoms (BDI); improvements in self-efficacy (WELSQ) | Not applicable | 0.87 |
| Cognitive and motor rehabilitation | Larson et al23 (2011) | VRROOM: a 3-D system through which patients view virtual objects super-imposed onto real world | n=18; patients with traumatic brain injury (TBI) aged 19–73 years receiving acute inpatient rehabilitation; not randomized | Within-subjects design; 2-day treatment (with 12 four-minute trials) | Improvements in memory impairments and attention; treatment with haptic cues helped improve performance vs. when cues were not present | 3 participants dropped out due to fatigue and eye pain | 0.85 |
Evaluation of study quality. To evaluate the strength of scientific evidence reported in these studies, we utilized a measure developed by Reisch, Tyson, and Mize, chosen among several measures reviewed and approved by the Agency for Healthcare Research and Quality (AHRQ).13,14 We selected the Reisch measure because it can be used for both observational studies and randomized, controlled trials (RCTs) and thoroughly assesses many important domains, including the following: study purpose, experimental design, sample size determination, description and suitability of subjects, randomization and stratification, usage of control/comparison group, treatment procedures, blinding, attrition, subject and treatment evaluation metrics, data analysis and presentation, and treatment recommendations. The measure aggregates data on 34 attributes within these 12 domains to produce a quality ratio (0–1), and can be adjusted to exclude attributes that do not apply to a given study. For example, blinding to the usage of VR is impossible by design, so this domain was not included in our evaluation of study quality.
Two raters (study authors JR and MR) scored each VR trial, utilizing a subset of applicable questions that totaled 27 points. After each rater completed a review of one of the VR trials, the raters conferred and discussed differences in scoring. Then, each rater reviewed the complete set of articles presented herein.15 We assessed inter-rater reliability by computing Cohen’s Kappa statistic.16 Because of the apparent heterogeneity of studies and inconsistency of reported results, we opted not to conduct a meta-analysis.
RESULTS
Overview. We identified 11 controlled studies of medical inpatients for the current review, but only eight studies randomized patients to VR conditions, or randomized the order of delivery of VR or standard interventions using crossover designs. We observed that studies were heterogeneous with regard to targeted disease state, VR equipment and intervention materials, and outcomes assessed. Thus, we categorized results within each application of VR to medical inpatients.
Study quality. Studies varied in terms of quality (average quality score=0.87; standard deviation [SD]=0.06; range=0.78–0.96).13 The raters were in strong agreement on most study quality domains assessed (Cohen’s κ=0.84). No studies defined the magnitude of the outcome to be evaluated (e.g., a 20% drop in pain GRS scores) or explicitly discussed cost-effectiveness, although four studies did consider VR device cost.15,17–19 Five of the 11 studies used small samples (i.e., n<30), as expected in a novel technology efficacy trial.19–23 Notably, the lowest rated study (Patterson et al21) and the highest rated study (Schmitt et al15) were authored by members of the same study team.15,21 Lower quality studies utilized smaller samples, did not randomize participants, and did not consider all factors associated with treatment (e.g., cost, adherence, side effects). Higher quality studies conformed to the expected structure of an RCT, justified and utilized larger samples, and considered patient side effects. We observed no temporal patterns in study quality, and found no associations between targeted disease state and quality score.
Pain distraction. As shown in Table 1, VR is used for pain management in inpatient populations more commonly than for other applications. Most researchers utilized the SnowWorld VR system (University of Washington HITLab and Harborview Burn Center, Seattle Washington)—the first VR software created for pain control during burn wound redressing—consisting of an HMD through which patients view and interact with snow-themed characters and throw virtual snowballs at approaching snowmen via a computer mouse or keyboard.20,24 In a first-of-its-kind study of burn victims using SnowWorld, Hoffman et al20 observed a 41-percent reduction in pain in the VR condition versus a control group, as well a strong negative correlation between self-reported “immersion” in the VR environment and pain ratings. Schmitt et al15 observed significant reductions in cognitive pain (time spent thinking about pain, reduced 44%), affective pain (emotional unpleasantness, reduced 32%), and sensory pain (reduced 27%), as well as highly positive feelings toward the VR intervention (which many labelled as “fun”). Carrougher et al17 also observed reductions in pain unpleasantness (31%), time spent thinking about pain (31%), and worst pain experienced (27%) in VR conditions, but did not observe statistically significant improvements in range of motion (ROM) physical therapy, which consists of assisted exercises designed to help patients gain movement in affected body segments (e.g. hand, wrist, elbow, shoulder, knee, or ankle).
A study by Patterson et al21 assessed the analgesic efficacy of virtual reality hypnosis (VRH), a new procedure in which the hypnotist verbally expresses suggestions that focus the patient’s attention away from pain. Based on scores obtained both immediately after the interventions and eight hours later, VRH patients reported less unpleasantness and less pain intensity than both control groups (VR without hypnosis, or standard analgesic treatment alone).
Two studies of burn patients utilizing low-cost, easily accessible and affordable VR HMD systems (Z800 3DVisor, eMagin, New York, New York) and off-the-shelf software computer games did not report significant differences in self-reported pain measures or anxiety (see Table 2 for detailed descriptions of scales used). Morris et al19 compared adult burn patient exposure to VR (video games plus analgesics) to a control condition (analgesics alone) and found a marginally significant difference in pain reduction between conditions (p=0.06), but no significant decreases in self-reported anxiety. In the Kipping et al study,18 patients did not report decreases in pain during burn wound redressing, but nursing staff observed significant reductions.
TABLE 2.
Summary of measures used in various studies in the present review
| SOURCE | SCALE/MEASURE | DESCRIPTION |
|---|---|---|
| Kipping et al18 (2012) | Faces, Legs, Activity, Cry, Consolability Scale (FLACC) Visual Analogue Scale (VAS) |
Self-reported pain measure and caregiver observation. Nursing staff reported scores on a scale of 0–2 for 5 measurement categories: faces, legs, activity, cry, and consolability (e.g., face: no particular expression [0], occasional frown [1], frequent quivering chin [2]. A total score out of 10 is then created) 10cm horizontal line measuring pain (0=no pain; 10=pain as bad as could be), presence (0=not at all, 10=totally went into game world), and nausea (0=no sick tummy; 10=as bad as could be) |
| Morris et al19 (2010) | Numeric Pain Rating Scale (NPRS) Burn Specific Pain Anxiety Scale (BSPAS) |
Self-reported pain scale ranging from none (0), mild (1–3), moderate (4–6), and severe (7–10) 9-item self-report scale highly correlated with the State-Trait Anxiety Inventory (STAI-S, r = 0.58, p < 0.005) |
| Li et al25 (2011) | Chinese Version of the State Anxiety for Children (CSAS-C) Center for Epidemiologic Studies Depression Scale (CES-D) |
10-items scored ranging from 1–3 with a maximum total score of 10–30; higher scores represent higher anxiety 20-item test with short statements regarding cognitive, behavioral, and emotional aspects of depression; responses are measured on a 4-point Likert scale (0=not at all, 1=a little, 2=some, 3=a lot) |
| Cesa et al26 (2013) | Body Image Avoidance Questionnaire (BIAQ) | 19-item self-reported scale measuring the likelihood of a patient to situations and habits provoking negative body image |
| Manzoni et al27 (2009) | Weight Efficacy Life-Style Questionnaire (WELSQ) Emotional Overeating Questionnaire (EOQ) State-Trait Anxiety Inventory (STAI) Beck Depression Inventory (BDI) |
20-item questionnaire measuring self-efficacy across 5 situational factors: negative emotions, availability, social pressure, physical discomfort, and positive activities 6-items; each begins with “on how many days out of the past 28 days have you eaten an unusually large amount of food of…” followed by 6 emotions; participants must indicate which one describes their reasoning most accurately (e.g., anxiety: worry, jittery, nervous); other emotions include sadness, loneliness, tiredness, anger, and happiness 40-item test on a 4-point Likert scale; 20 items measure state anxiety (current feelings) and 20 items measure trait anxiety (more stable over time and situations 21-item test ranging from 1–20 (normal) to over 40 (extreme depression); items inquire about feelings of sadness, thoughts about the future, self-image |
| Larson et al23 (2011) | Virtual Reality and Robotic Optical Operations Machine (VRROOM) | A 3-D system that allows patients to view virtual objects super-imposed onto the real world |
| Yin et al22 (2014) | Fugl-Meyer Assessment (FMA) | 33 items that measure upper extremity motor impairement on a 3-point rating scale; performance-based index that assesses balance, sensation, and motor functioning |
One study utilized wall projections and motion detection instead of HMDs to examine the effectiveness of therapeutic play for reducing depressive symptoms in pediatric oncology patients.25 After a week of treatment, children in the experimental group reported significantly fewer depressive symptoms than those in the control group, but they did not report significant differences in state anxiety.
Eating disorders (EDs) and obesity. Two recent studies investigating the efficacy of VR treatment in populations with EDs are presented in Table 1. Cesa et al26 assessed the brief and long-term efficacy of VR plus cognitive-behavioral therapy in a group of 90 female patients with obesity at an inpatient rehabilitation clinic. In the VR treatment arm, participants wore HMDs and navigated through 14 different virtual environments. Patients were exposed to tempting situations (e.g., buying unhealthy food at the supermarket) to improve self-control and motivation, as well as situations that challenged negative body image (e.g., swimming pool). Although improvements in body satisfaction were reported in all study conditions, only patients in the VR condition reported improved body image perceptions at five-week follow-up. After one year, VR patients were significantly better (44.4%) at improving or maintaining weight loss than patients in control conditions (10.4%).
Manzoni et al27 demonstrated that both VR and imagination-based relaxation training conditions helped reduce emotional eating, anxiety, depressive symptoms, and self-efficacy (see Table 2 for scales used). However, at a three-month follow-up, the VR condition—wherein patients wandered in an idyllic mountain landscape—demonstrated greater efficacy in reducing emotional eating than control conditions.
Cognitive and motor rehabilitation. In a study by Larson et al,23 patients of all ages with traumatic brain injuries (TBI) completed 12 four-minute-long cancellation exercises using a system called Virtual Reality and Robotic Optical Operations Machine (VRROOM [developed by Patton et al38]; See Table 2) over a period of two days.23 The authors observed improvements in memory and attention across trials as measured by target acquisition times. Distractions involving both visual and haptic stimuli were especially effective. Also, in a study by Yin et al,22 stroke patients utilized the Sixense VR system (Sixense, Los Gatos, California), a rehabilitation gaming software consisting of an avatar on a screen that is synchronized with the patient’s movements.22 In a virtual environment, users are instructed to pick fruit from a shelf and release it into a basket as many times as possible within a two-minute time frame. The authors observed improved sensorimotor function for both VR and non-VR (conventional physical therapy) conditions, as measured by the Fugl-Meyer Assessment (FMA; see Table 2), though no significant differences were found between conditions.
Patient satisfaction and side effects. Patient satisfaction and side effects are displayed in the “Secondary Observations” column in Table 1. Participants often rated VR sessions as more fun, more immersive, more useful, and more enjoyable than non-VR conditions.15,20,22 Despite previous findings that HMDs or peripheral devices often restrict movement, no such results were found in the present review.28
A majority of studies did not report VR side effects, such as motion sickness or fatigue, as factors negatively influencing patient satisfaction or the efficacy of VR treatments. When asked, patients in the study by Kipping et al17 did not report experiencing nausea, and 97 percent of patients in the sutdy by Carrougher et al18 reported no to mild nausea after using HMDs. Yin et al22 found no significant side effects, and deemed VR technology feasible and safe for participants. However, in the Larson et al23 study of 18 patients with TBI, three participants dropped out due to fatigue and eye pain caused by the VRROOM system (Table 2).
DISCUSSION
In contrast to previous reviews of case reports and observational evidence, the present review focused on controlled studies that describe applications of VR technology in the treatment and rehabilitation of medical inpatients.29,30 Data from 11 eligible studies provide insight into three current medical applications of VR technology: pain distraction, eating disorders, and cognitive/motor rehabilitation.
Pain distraction. VR is particularly useful as a pain distraction that supplements or replaces traditional pharmacotherapies. According to Wiederhold,7 pain perception is dependent on a patient’s capacity to attend to a certain stimulus. Thus, pain management may be achieved by blocking sensory information via opioid analgesics or by creating a distraction from pain by immersing a patient in a virtual environment.11,31 Previous studies have demonstrated that opioid analgesics may lead to undesirable consequences, such as nausea, increased length of hospitalizations, and inadequate pain alleviation.32 VR presents a useful alternative with minimal side effects, although nausea may be reported from either treatment.
Five of seven studies demonstrated that VR is an efficacious non-pharmacologic adjunct to standard opioid analgesic treatments to reduce pain, distress, and anxiety in adult and pediatric patients undergoing unpleasant medical procedures. Highlighting the psychological components of pain, VR distraction treatments reduce self-reported unpleasantness, time spent thinking about pain, and levels of worst pain experienced.15,17 These patient-reported observations are corroborated by neuroimaging studies that have highlighted five brain regions showing reduced activity during VR interventions—thalamus, insula, primary and secondary somatosensory cortices, and the anterior cingulate cortex.17 Overall, both physiological and psychological measures suggest that VR is a helpful clinical tool in pain distraction.
EDs and obesity. VR is used in eating disorders to improve patient body image experiences, increase self-efficacy, and practice healthy decision-making.7 Participants may navigate a virtual supermarket to make healthy food choices or they may be encouraged to adopt less harmful perceptions of body image through repeated exposure to images of diverse body types.1 In conjunction with other psychological therapies (e.g., graded exposure or cognitive-behavioral therapy), patients develop skills that carry over into the real world.
VR therapies are useful not only for replicating a desired environment, but also for altering reality (e.g., an avatar that no longer resembles the patient).9 This strategy is consistent with Bem’s (1972) self-perception theory,39 which postulates that “individuals develop attitudes by observing their own behavior and concluding what attitudes must have caused them.” Observing an avatar’s appearance as different from the actual self may shape and change the patients’ own attitudes—a phenomenon known as the Proteus effect.40 This strategy has been especially successful in the treatment of body dysmorphic disorder, binge eating, and anorexia.7 As reviewed herein, use of virtual environments, plus low-calorie diets and exercise, led to significant improvements in body image concerns, weight loss, and body satisfaction while also reducing anxiety and emotional eating.26 Additional longitudinal studies must be conducted in order to assess the long-term efficacy of VR interventions in preventing weight gain.
Cognitive and motor rehabilitation. VR also presents a novel rehabilitation approach for patients with strokes, Parkinson’s disease, and brain injuries.7 VR training allows for high ecological validity in a safe and controlled environment, provides immediate visual and tactile feedback about the individual’s specific performance, and may boost motivation.33–35 Experimenter-manipulated environments allow for individualized training to enhance specific skills and neuroplasticity through repeated practice, as well as a means of helping patients overcome underutilization of limbs.28 The intervention studies reviewed herein consisted of repeated safe practice of particular skills with the help of superimposed virtual limbs that train individuals in tasks specific to their medical condition. Inconsistent results suggest that further testing of VR in motor and cognitive rehabilitation is required.22,23
Limitations. We only included 11 controlled trials in medical inpatient populations, and did not consider other successful case studies or efficacious outpatient interventions. Because of the heterogeneity of this small number of studies, we could not conduct a formal meta-analysis. Additional studies will need to be conducted to assess the efficacy of VR fully.
Future research. Whereas early studies of VR utilized costly platforms precluding widespread use, more recent versions are available at price points that greatly improve affordability and accessibility.36 In the present review, two studies using low-cost off-the-shelf HMD visors did not report significant pain reductions.18,19 Future research should further examine whether the quality of HMD technology is associated with improved efficacy.
Future studies of VR in medical inpatients should utilize larger samples assessed over time to investigate long-term effects.37 Although most VR studies are found within hospital settings, some clinicians predict VR will be used as home-based rehabilitation in the future. According to Sandlund, McDonough and Häger-Ross, interactive computer play and VR are especially helpful for physicallydisabled children who are often treated at home.29
In the hospital setting, VR could be used by patients suffering from chronic pain syndromes (e.g., chronic pancreatitis, back pain, and/or refractory migraines) or used to reduce pain and anxiety in the emergency department (e.g., for reduction of dislocated joints, suturing of lacerations, cardioversion for arrhythmias, or casting of fractures). VR could also be used as a distraction for patients undergoing magnetic resonance imaging or computed tomography scanning, during interventional procedures or hemodialysis, or as part of chemotherapy infusion protocols.
CONCLUSION
Overall, a majority of studies from the past decade found VR to be efficacious, easy to use, safe, and contributing to high patient satisfaction. Studies varied in terms of quality, but we observed no relationship between study quality and key findings. In most cases, patients considered the VR experience to be fun, immersive, and enjoyable, and few patients were lost to attrition due to side effects.
The use of VR in medical fields is relatively novel but also promising.37 It is highly interactive, flexible, tailored to the individual, and applicable to people varying in age, sex, and medical disorders. As technology improves and costs are reduced, VR will undoubtedly shape the future of healthcare.
Footnotes
FUNDING:No funding was received for the preparation of this article.
FINANCIAL DISCLOSURES:The authors have no conflicts of interest relevant to the content of this article.
REFERENCES
- 1.Ferrer-Garcia M, Gutiérrez-Maldonado J, Riva G. Virtual reality based treatments in eating disorders and obesity: a review. J Contemp Psychother. 2013;43:207–221. [Google Scholar]
- 2.Medling B. Virtual reality utilization in health care: it’s virtually done. Biomed Instrum Technol. 2005;39:16–18. [PubMed] [Google Scholar]
- 3.Riener R, Harders M. Virtual Reality in Medicine. London: Springer; 2012. pp. 1–2. [Google Scholar]
- 4.Riva G, Gaggioli A, Villani D, et al. NeuroVR: an open source virtual reality platform for clinical psychology and behavioral neurosciences. Stud Health Technol Inform. 2007;125:394–399. [PubMed] [Google Scholar]
- 5.McCann RA, Armstrong CM, Skopp NA, et al. Virtual reality exposure therapy for the treatment of anxiety disorders: an evaluation of research quality. J Anxiety Disord. 2014;28:625–631. doi: 10.1016/j.janxdis.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Rothbaum BO, Hodges L, Smith S, et al. A controlled study of virtual reality exposure therapy for the fear of flying. J Consult Clin Psych. 2000;68:1020–1026. doi: 10.1037//0022-006x.68.6.1020. [DOI] [PubMed] [Google Scholar]
- 7.Wiederhold BK. VRMC: The Virtual Reality Medical Center [website] The potential for virtual reality to improve health care. 2006. [Accessed May 3, 2016]. http://www.iactor.eu/downloads/WP%20The%20Potential%20for%20VR%20to%20Improve%20Healthcare.pdf
- 8.Mühlberger A, Wiedemann G, Pauli P. Efficacy of a one-session virtual reality exposure treatment for fear of flying. Psychother Res. 2003;13:323–336. doi: 10.1093/ptr/kpg030. [DOI] [PubMed] [Google Scholar]
- 9.Cornick JE, Blascovich J. Are virtual environments the new frontier in obesity management? Soc Personal Psychol Compass. 2014;8:650–658. [Google Scholar]
- 10.Llobera J, González-Franco M, Perez-Marcos D, et al. Virtual reality for assessment of patients suffering chronic pain: a case study. Exper Brain Res. 2013;225:105–117. doi: 10.1007/s00221-012-3352-9. [DOI] [PubMed] [Google Scholar]
- 11.Parsons TD, Rizzo AA, Rogers S, York P. Virtual reality in paediatric rehabilitation: a review. Dev Neurorehabil. 2009;12:224–238. doi: 10.1080/17518420902991719. [DOI] [PubMed] [Google Scholar]
- 12.Wiederhold MD, Wiederhold BK. Virtual reality and interactive simulation for pain distraction. Pain Med. 2007;8:182–188. [Google Scholar]
- 13.Reisch JS, Tyson JE, Mize SG. Aid to the evaluation of therapeutic studies. Pediatrics. 1989;84:815–827. [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research And Quality, U.S. Department of Health and Human Services [website] Systems to Rate the Strength of Scientific Evidence. Apr, 2002. [Accessed May 3, 2016]. http://www.thecre.com/pdf/ahrq-system-strength.pdf
- 15.Schmitt YS, Hoffman HG, Blough DK, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns. 2011;37:61–68. doi: 10.1016/j.burns.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 17.Carrougher GJ, Hoffman HG, Nakamura D, et al. The effect of virtual reality on pain and range of motion in adults with burn injuries. J Burn Care Res. 2009;30:785–791. doi: 10.1097/BCR.0b013e3181b485d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kipping B, Rodger S, Miller K, Kimble RM. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns. 2012;38:650–657. doi: 10.1016/j.burns.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Morris LD, Louw QA, Crous LC. Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country. Burns. 2010;36:659–664. doi: 10.1016/j.burns.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Hoffman HG, Patterson DR, Seibel E, et al. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008;24:299–304. doi: 10.1097/AJP.0b013e318164d2cc. [DOI] [PubMed] [Google Scholar]
- 21.Patterson DR, Jensen MP, Wiechman SA, Sharar SR. Virtual reality hypnosis for pain associated with recovery from physical trauma. Int J Clin Exp Hypn. 2010;58:288–300. doi: 10.1080/00207141003760595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yin CW, Sien NY, Ying LA, et al. Virtual reality for upper extremity rehabilitation in early stroke: a pilot randomized controlled trial. Clin Rehabil. 2014;28:1107–1114. doi: 10.1177/0269215514532851. [DOI] [PubMed] [Google Scholar]
- 23.Larson EB, Ramaiya M, Zollman FS, et al. Tolerance of a virtual reality intervention for attention remediation in persons with severe TBI. Brain Injury. 2011;25:274–281. doi: 10.3109/02699052.2010.551648. [DOI] [PubMed] [Google Scholar]
- 24.Hoffman HG, Chambers GT, Meyer WJ, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annal Behav Med. 2011;41:183–191. doi: 10.1007/s12160-010-9248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li WC, Chung JK, Ho EY. The effectiveness of therapeutic play, using virtual reality computer games, in promoting the psychological well-being of children hospitalised with cancer. J Clin Nurs. 2011;20:2135–2143. doi: 10.1111/j.1365-2702.2011.03733.x. [DOI] [PubMed] [Google Scholar]
- 26.Cesa GL, Manzoni GM, Bacchetta M, et al. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: randomized controlled study with one-year follow-up. J Med Internet Res. 2013;15:139–151. doi: 10.2196/jmir.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manzoni GM, Pagnini F, Gorini A, et al. Can relaxation training reduce emotional eating in women with obesity? an exploratory study with 3 months of follow-up. J Am Diet Assoc. 2009;109:1427–1432. doi: 10.1016/j.jada.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 28.You SH, Jang SH, Kim Y, et al. Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev Med Child Neurol. 2005;47:628–635. [PubMed] [Google Scholar]
- 29.Sandlund M, McDonough S, Häger-Ross C. Interactive computer play in rehabilitation of children with sensorimotor disorders: a systematic review. Dev Med Child Neurol. 2009;51:173–179. doi: 10.1111/j.1469-8749.2008.03184.x. [DOI] [PubMed] [Google Scholar]
- 30.Snider L, Majnemer A, Darsaklis V. Virtual reality as a therapeutic modality for children with cerebral palsy. Dev Neurorehabil. 2010;13:120–128. doi: 10.3109/17518420903357753. [DOI] [PubMed] [Google Scholar]
- 31.Gershon J, Zimand E, Pickering M, Rothbaum BO, Hodges L. A pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatry. 2004;43:1243–1249. doi: 10.1097/01.chi.0000135621.23145.05. [DOI] [PubMed] [Google Scholar]
- 32.Teeley AM, Soltani M, Wiechman SA, et al. Virtual reality hypnosis pain control in the treatment of multiple fractures: a case series. Am J Clin Hypn. 2012;54:184–194. doi: 10.1080/00029157.2011.619593. [DOI] [PubMed] [Google Scholar]
- 33.Subramanian SK, Lourenço CB, Chilingaryan G, et al. Arm motor recovery using a virtual reality intervention in chronic stroke: randomized control trial. Neurorehabil Neural Repair. 2013;27:13–23. doi: 10.1177/1545968312449695. [DOI] [PubMed] [Google Scholar]
- 34.Brunner I, Skouen JS, Hofstad H, et al. Virtual reality training for upper extremity in subacute stroke (VIRTUES): study protocol for a randomized controlled multicenter trial. BMC Neurol. 2014;14:186. doi: 10.1186/s12883-014-0186-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crosbie JH, Lennon S, McGoldrick MC, et al. Virtual reality in the rehabilitation of the arm after hemiplegic stroke: a randomized controlled pilot study. Clin Rehabil. 2012;26:798–806. doi: 10.1177/0269215511434575. [DOI] [PubMed] [Google Scholar]
- 36.Nilsson S, Finnström B, Kokinsky E, Enskär K. The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur J Oncol Nurs. 2009;13:102–109. doi: 10.1016/j.ejon.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 37.Turner WA, Casey LM. Outcomes associated with virtual reality in psychological interventions: where are we now? Clin Psychol Rev. 2014;34:634–644. doi: 10.1016/j.cpr.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 38.Patton J, Dawe G, Scharver C, et al. Robotics and virtual reality: a perfect marriage for motor control research and rehabilitation. Asst Technol. 2006;18:181–195. doi: 10.1080/10400435.2006.10131917. [DOI] [PubMed] [Google Scholar]
- 39.Bem DJ. Self-perception theory. Adv Exp Soc Psychol. 1972;6:1–62. [Google Scholar]
- 40.Yee N, Bailenson J. The Proteus effect: the effect of transformed self-representation on behavior. Hum Commun Res. 2007;33:271–290. [Google Scholar]