Abstract
Objective
Lesbian, gay, bisexual, and transgender (LGBT) older adult caregivers may encounter obstacles in obtaining health and aging services due to discrimination in service and legal systems. The caregiving relationships in LGBT communities also differ from the general population in that friends are providing a large portion of informal care. This article examines how the relational context of caregiving relates to caregiving demands and resources, which in turn, influence perceived stress and depressive symptomatology among older LGBT caregivers.
Method
Using data from the National Health, Aging, and Sexuality Study: Caring and Aging with Pride, this study examines 451 participants who are providing caregiving to partners and friends. Structural equation modeling was applied to estimate the associations among the caregiver–care recipient relationship and caregiving demands, resources, perceived stress, and depressive symptomatology.
Results
On average, as compared with those caring for partners, those who provided care to friends reported experiencing lower levels of caregiving demands and lower levels of social support. The lower caregiving demands correlated positively with both lower perceived stress and less severe depressive symptomatology; however, the lower levels of social support were related to higher perceived stress and higher depressive symptomatology.
Conclusions
Caregiving provided by friends, which has long been under recognized, plays an important role in the LGBT community. Because lower levels of caregiving demands are offset by less social support, LGBT friend-caregivers experience similar levels of perceived stress and depressive symptomatology to those providing care to spouses and partners. Policy and service reforms are needed to better acknowledge the continuum of informal caregiving relationships.
Keywords: caregiving, LGBT, aging, mental health
In the more than four decades since the Stonewall riots, increasing numbers of sexual and gender minorities have disclosed their identities, built communities, and live openly within their families of choice. The first generation of openly lesbian, gay, bisexual, and transgender (LGBT) community members is now part of the “graying” population of the United States. By 2030, the number of self-identified older LGBT adults is expected to more than double (Fredriksen-Goldsen, Kim, Barkan, Muraco, & Hoy-Ellis, 2013; Fredriksen-Goldsen, Kim, Muraco, & Mincer, 2009). As in the general population, concerns about older adult care and caregiving are taking on greater importance in LGBT communities, given increases in both life expectancy and chronic health conditions (Arias, 2012; Murphy, Xu, & Kochanek, 2013).
Caregiving, informal care provided by those who are unpaid, plays a critical role in addressing the long-term care needs of older adults in the United States. Estimates have suggested that 43.5 million people in the United States are providing informal, unpaid care to people who are 50 years and older (Ginzler, 2010). The support and care provided by informal caregivers has contributed significantly to the well-being of older adults who need assistance with the activities of daily living, including those with chronic and other health conditions (Arno, Levine, & Memmott, 1999; Van Houtven & Norton, 2004; Wolff & Agree, 2004).
In LGBT communities, informal caregiving is also crucial to the well-being of older adults. Given the potential for cumulative disadvantages throughout their lifetime, older LGBT adults are more likely to have chronic health conditions than heterosexual peers (Baumle, 2014; Fredriksen-Goldsen et al., 2011). For example, Fredriksen-Goldsen and colleagues found that the total number of lifetime discrimination and victimization experiences (e.g., loss of jobs as a result of discrimination, exposure to physical violence) were associated with poor physical and mental health outcomes (Fredriksen-Goldsen, Kim, Shiu, Goldsen, & Emlet, 2015) as well as greater likelihoods of disabilities and depression in a national sample of older LGBT adults (Fredriksen-Goldsen, Kim, et al., 2013).
Caregiving provided by a partner is the most common type of caregiving across all types of caregiving for both older heterosexuals and older LGBT adults. However, when compared with their heterosexual peers, older LGBT adults have fewer traditional supports outside of their partners, such as children, to help them (Fredriksen-Goldsen, Kim, et al., 2013). Thus, older LGBT individuals rely more heavily on their close peers to provide informal care. In one sample of older LGBT adults, more than half (54%) were receiving care from their partner and about a quarter (24%) were receiving care from a friend (Fredriksen-Goldsen et al., 2011).
Indeed, friends play an increasingly important role in delivering informal care-giving for older adults across communities due to several critical social changes in contemporary U.S. society. As suggested by Himes and Reidy (2000), greater residential mobility and the increasing numbers of single-parent households and stepfamilies can limit the capacities of modern families to provide informal care-giving to older family members. Yet, despite the large body of work on caregiving, friend caregiving remains an underresearched area, with the majority of existing studies on caregiving focusing on care provided by either partners or biological family members. Thus, current knowledge about friends as caregivers is limited, with little information available on friends’ experiences of caregiving burden, social support, and mental health sequelae.
When compared with heterosexual older adults, older LGBT adults are more likely to report that they provide care to other LGBT friends in need. One study showed that in contrast to 6% of heterosexual older adults who provided care to a friend, 21% of older LGBT adults have provided caregiving to friends (MetLife Mature Market Institute & American Society on Aging [MetLife], 2010). The commonplace nature of friend-care in LGBT communities might have its historical roots in the HIV epidemic. In the 1980s and early 1990s, LGBT communities were disproportionately affected by the HIV/AIDS epidemic as many gay and bisexual men, as well as transgender women, became infected with HIV. However, discrimination related to HIV and sexuality severely limited the options for sources of caregiving. To cope with this growing health crisis, LGBT communities across the nation mobilized to provide care to those living with HIV, who often did not have sufficient support from biological families (Muraco & Fredriksen-Goldsen, 2011; Turner & Catania, 1997). As a consequence, a cultural norm of mutual care emerged within LGBT communities as a way to cultivate solidarity (Aronson, 1998), with gay men and lesbians not only providing care to their friends but also providing more hours of care per week on average as compared with heterosexual men and women (MetLife, 2010).
Informal caregiving brings benefits both to those receiving care and to those providing care. Research has shown that caregiving can promote the personal growth of the caregiver as well as strengthen the caregiver’s relationships with loved ones (Beach, Schulz, Yee, & Jackson, 2000; Cohen, Colantonio, & Vernich, 2002; Kramer, 1997). In addition to instrumental care (e.g., transportation, grocery shopping, laundry), LGBT caregivers provide social and emotional support to their friends and partners (Cantor, Brennan, & Shippy, 2004; Muraco & Fredriksen-Goldsen, 2011). In turn, providing assistance to friends and partners provides many LGBT caregivers with positive gains such as an elevated sense of self-esteem and self-efficacy (Kia, 2012; Muraco & Fredriksen-Goldsen, 2011).
Nevertheless, informal caregivers often provide care at the cost of their own mental and physical well-being given the likelihood of experiencing high caregiving demands and role conflicts, which in turn, can lead to elevated levels of stress and depression (Pinquart & Sörensen, 2003, 2007; Rush, Williamson, Stephen, & Schulz, 2011). Moreover, LGBT caregivers might face declining health related to their own aging, challenges of maintaining paid employment while providing care, and increased need for social support (Cantor et al., 2004; Grossman, D’Augelli, & Hershberger, 2000). Fredriksen-Goldsen and colleagues (2011) also found that as compared with LGBT noncaregivers, LGBT caregivers were more likely to report poor physical and mental health. Moreover, when compared with their heterosexual counterparts, LGBT caregivers were found to be less likely to use formal services and received less support from family members, thus decreasing these caregiver’s resources and abilities to manage the demands, burden, and stresses related to their caregiving responsibilities (Cantor et al., 2004; Croghan, Moone, & Olson, 2014; Fredriksen-Goldsen, 2007). Although the informal care provided by friends is comparable to the tasks performed by partners (Muraco & Fredriksen-Goldsen, 2011), the challenges of caregiving—especially when dealing with medical and other service systems—can be compounded when the friend-caregiver does not have the care recipient’s power of attorney or other next-of-kin privileges (Muraco & Fredriksen-Goldsen, 2011). In addition, the current support services for informal caregivers have been largely designed for heterosexual partners or other biological family members, leaving older LGBT adults who provide care to friends or partners as a potentially underserved group (Brotman et al., 2007; Fredriksen-Goldsen, 2007).
Despite the vast literature on the informal care of older adults in general, research on caregiving in the LGBT community is still in the early stages of development. In addition, the majority of the existing empirical studies on LGBT care-giving have used qualitative research methods to explore caregiving experiences among LGBT caregivers (Washington et al., 2015). As a result, limited quantitatively verified information is available about LGBT caregiving, including the demands these caregivers face, the supports and resources available to them, and the potential psychological sequelae of their caregiving experiences. Further, although the research on caregiving in general has predominantly focused on care-giving within biological family and marital relationships, little attention has been given to friend care (for notable exceptions, see Barker, 2002; Himes & Reidy, 2000). This study sought to address these gaps by investigating the ways in which the context of differing caregiving relationships (friend vs. partner caregiving) are associated with the caregiving demands, resources, and mental health sequelae among older LGBT adults.
Conceptual Framework
This study used the conceptual perspective developed by Romeis (1989) regarding caregiving demands, resources, and stress. According to Romeis, informal care-givers experience caregiving demands within the context of resources they can mobilize to manage those demands. In large part, caregiving demands depend on the care recipients’ needs and level of functioning. Caregiving encompasses a wide range of tasks requiring various time and efforts, with personal care cited as the most demanding type of care (Fredriksen & Scharlach, 2001). Additionally, when one caregiver is providing more types of care, the caregiver is likely to spend more hours per week providing care, experience increased financial strains related to the provision of care, and feel the burden of increased caregiving demands. Resources to manage caregiving demands are the various supports caregivers can access or mobilize, such as social support. When the perceived support is greater than demands, caregivers can manage caregiving tasks; however, when demands exceed the resources available, caregivers might suffer from increasing levels of role strain and stress. Further, the interaction between caregiving demands and resources is a dynamic and potentially cumulative process. The balance of demands and resources can change over time as a function of the care recipients’ changing health conditions and the sustainability of resources. In other words, duration of care can influence the demands as well as the stress levels experienced by informal caregivers.
Stress is predictive of mental health outcomes among caregivers as evidenced by several studies (Pinquart & Sörensen, 2003; Schwarz & Dunphy, 2003; Sherwood, Given, Given, & von Eye, 2005). In the multistep stress-proliferation model (Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995), caregiving demands are conceptualized as objective stressors: Higher caregiving demands mixed with fewer resources lead to higher levels of perceived stress, which in turn, contributes to poor outcomes among caregivers, including elevated risk of poor mental health and greater levels of depressive symptomatology. However, only limited research has investigated specific factors linked to caregiving burden (Shippy, 2007) and depressive symptomatology among older LGBT adult caregivers (Fredriksen-Goldsen et al., 2009).
Finally, Fredriksen-Goldsen and Scharlach (2001) incorporated contextual factors in a model to predict both demands and resources for caregivers. An important element among the contextual factors is the relationship between the caregiver and the care recipient because this relationship not only defines the boundaries of interpersonal interactions but also determines which types of care can be provided (Lapierre & Keating, 2013). For example, as compared with care-givers caring for partners, people providing care to friends might be less likely to provide personal care that involves intimate interaction or contact between care-giver and care recipient. At the same time, friend-care might lack recognition, be less visible, and might not be understood to be “real” caregiving. The lack of recognition of friend-caregivers might contribute to these caregivers receiving less social support from their personal networks as well as health and human service providers.
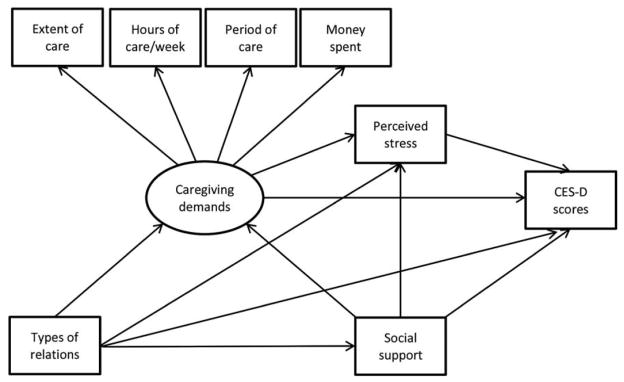
To address these gaps in our understanding of caregiving in this potentially vulnerable community, we examined the ways in which perceived stress and depressive symptomatology among LGBT caregivers can be predicted by caregiving demands, resources, and the relationship between the caregiver and care recipient. Our hypothetical model is presented in Figure 1. In the model, we hypothesized that (a) perceived stress would mediate the relationship between caregiving demands and depressive symptomatology; (b) social resources would be negatively associated with caregiving demands, perceived stress, and depressive symptomatology; and (c) the relationships between care recipients and caregivers would be associated with caregiving demands, social resources, perceived stress, and depressive symptomatology.
Figure 1.
Hypothetical caregiving model. Note. CES-D = Center for Epidemiologic Studies–Depression Scale.
Method
To test the model, we conducted a secondary data analysis with a sample drawn from the National Health, Aging and Sexuality Study: Caring and Aging with Pride (CAP; see http://caringandaging.org/). The CAP study used cross-sectional study design. Through collaborations with 11 community sites across the United States, the CAP study surveyed 2,560 LGBT adults who were 50 years old and older in 2010. Additional information regarding the CAP study design has been published elsewhere (see Fredriksen-Goldsen et al., 2013). The sample of older LGBT caregivers used in this study (N = 451) was a subset of the larger CAP sample, and selected based on participant reports of providing care to spouses, partners, or friends.
Measures
The variables selected for modeling included caregiving demands, relationship type, social resources, perceived stress, depressive symptomatology, and demographic characteristics.
Caregiving demands
Caregiving demands are conceptualized as overall hardships in conjunction with caregiving activities (Pearlin, Aneshensel, & LeBlanc, 1997; Pearlin, Mullan, Semple, & Skaff, 1990) and are a latent variable measured by four indicators: extent of care, hours of care per week, duration of care, and money spent on care. Extent of care is a composite score summarizing four distinct types of care LGBT caregivers provide to care recipients, including instrumental care, financial assistance, health care management (i.e., coordination of care), and personal care (i.e., bathing, grooming, toileting), with personal care weighted by a factor of two (Fredriksen-Goldsen & Scharlach, 2001). The indicator extent of care ranged from 0 to 5, with higher values representing more types of care provided by the caregiver. The indicator hours of care per week was measured by the question, “Overall, approximately how many hours do you spend helping this person in a typical week?” Duration of care was measured by a single item, in terms of months, “How long have you been providing care to this person?” Both caregiving demands and extent of care were continuous variables and had highly skewed distributions with several outliers; therefore, both variables were divided into six groups based on the relative percentiles. Money spent on care was measured by one item, “Overall, approximately how much money do you spend helping this person in a typical month?” with five potential response categories: none, less than $100, $100 to $249, $250 to $499, and $500 or more. To construct the caregiving demands latent variable, we used the reflective indicator measurement model instead of the causal indicator model (Bollen & Bauldry, 2011). We chose this approach because in our conceptualization, caregiving demands can be measured by the four indicators rather than caused by the four indicators. Moreover, the causal indicator model requires an additional strong assumption of error-free measurement in the observed formative indicators (Edwards & Bagozzi, 2000), which might be less realistic in our study given the nature of the measurements.
Relationship between caregivers and care recipients
The relationship between LGBT caregivers and care recipients was measured by the question, “How is the person [you assist] related to you?” For this analysis, participants who selected either partner/spouse or friend were included and placed into 1 of 2 categories as spousal caregivers or friend caregivers.
Social resources
Social resources were measured by four questions that asked participants to rate the extent to which four different types of support were available to them. The four types of support included tangible support, emotional-informational support, positive social interaction support, and affectionate support (e.g., “Someone to turn to for suggestions about how to deal with a personal problem?”). Response options ranged from never (coded 1) to always (coded 4). A composite score was created that averaged across the four questions, with higher scores representing greater support (Cronbach’s alpha = 0.85).
Perceived stress
The perceived stress of LGBT caregivers was assessed using the short version of the Perceived Stress Scale (PSS-4; Cohen, Kamarck, & Mermelstein, 1983). The scale contains four items that ask participants to rate how they felt in the past month. For example, one item asked, “How often have you felt that you were unable to control the important things in your life?” Responses options ranged from never (coded 0) to very often (coded 4). A composite score was computed by averaging the four items. Higher scores indicated greater perceived stress (Cronbach’s alpha = 0.78).
Depressive symptomatology
Depressive symptomatology was measured by the 10-item version of the Center for Epidemiological Studies Depression Scale (CES-D; Andresen, Malmgren, Carter, & Patrick, 1994). The CES-D is widely used in mental health research, and asks participants to rate how often in the past week they felt or behaved in certain ways (e.g., “I felt depressed” and “my sleep was restless.”) A score was calculated by summing the 10 items, with higher scores representing greater severity of depressive symptomatology (Cronbach’s alpha = 0.87).
Demographic characteristics
Demographic characteristics included age group (50 to 64 years, 65 to 79 years, 80 years and older), sex assigned at birth (female vs. male), sexual orientation (lesbian and gay vs. bisexual), gender identity (transgender identified vs. non-transgender identified), race/ethnicity (non-Hispanic White vs. other racial and ethnic groups), geographic location (urban vs. rural), education (high school and below vs. some college and above), employment (employed vs. not employed), poverty (living under federal poverty level [FPL] vs. at or above 200% of the FPL), and living arrangement (currently living with the care recipient vs. not living with the care recipient).
Analysis
First, we conducted bivariate analyses for comparisons between two groups: care-givers who provided care to a partner and caregivers who provided care to a friend. The bivariate analyses allowed us to obtain a general picture of the similarities and differences between these two groups on the selected study variables. For categorical variables, chi-square or Fisher’s exact tests were used depending on the distributions of the variables between the two groups. For continuous variables, we used bootstrap techniques to compute standard errors to avoid explicit assumptions of variables’ distributions. Next, we applied structural equation modeling (SEM) techniques to simultaneously estimate the relationships among variables. The SEM analyses included the following steps:
We standardized all continuous variables so that their means centered on 0 with standard deviations of 1.
A measurement model was built to create a latent variable, caregiving demands, with four observable variables: the extent of care, hours of care per week, duration of care, and money spent on care. This step examined the relationships between the latent variable and observed variables while taking into account potential measurement errors. Both unstandardized and standardized estimations were reported.
The hypothetical structural model was fitted to estimate the relationships among the latent variable, relationship types, social support, perceived stress, and depressive symptomology (CES-D scores). We used several model fit indices to evaluate the extent to which the hypothetical model could reconstruct the covariance structure in the data, as recommended by Kenny (2014), including the chi-square test; Akaike information criterion (AIC); Bayesian information criterion (BIC); root mean square errors of approximation (RMSEA); comparative fit index (CFI); and the Tucker-Lewis index (TLI). Given that less than 10% of the sample had e missing values, we used full maximum likelihood estimation. In addition, to avoid an explicit assumption of normal residuals, we used accelerated bootstrap methods to calculate the standard errors.
We ran an additional model that incorporated a set of selected background factors to adjust for the estimations.
Last, we applied a linear combination of model estimates and Wald test to examine the direct, indirect, and total effects among unstandardized estimations. All statistical analyses were carried out in a commercial statistical package Stata 13.
Results
The sample included 451 participants, of whom 52% were providing care to a partner, and 44% were providing care to a friend. Table 1 summarizes the demographic backgrounds and the caregiving demands and resources, stress and depressive symptomology of the sample, as well as the results of comparisons between partner caregivers and friend caregivers. Overall, about 40% of the participants were between 50 and 64 years old, about half of the participants were between 65 and 79 years old, and the other 10% were 80 years or older. The majority of the sample was male (37% female); 8% of the sample self-identified as transgender. The vast majority of participants (93%) identified as a lesbian or gay male and White, with only 15% of the sample identifying as a person of color. Slightly more than 92% of the participants had some college education, and approximately 60% were unemployed. More than a third of the sample (34%) had incomes below 200% of the FPL. About half of the sample resided with the care recipient.
Table 1.
Characteristics of the Sample and Results of Bivariate Analysis
| Demographic factors | All (N = 451)
|
Spouse/partner caregiver (n = 233)
|
Friend caregiver (n = 218)
|
p
|
|---|---|---|---|---|
| % | % | % | ||
| Age (in years) | 0.983 | |||
|
| ||||
| 50–64 | 39.47 | 39.06 | 39.91 | |
|
| ||||
| 65–79 | 48.56 | 48.93 | 48.17 | |
|
| ||||
| 80+ | 11.97 | 12.02 | 11.93 | |
|
| ||||
| Sex | 0.123 | |||
|
| ||||
| Female | 37.11 | 33.49 | 40.52 | |
|
| ||||
| Sexual orientation | 0.884 | |||
|
| ||||
| Lesbian & Gay | 92.81 | 92.63 | 92.99 | |
|
| ||||
| Transgendera | 0.001 | |||
|
| ||||
| Yes | 8.46 | 12.88 | 3.7 | |
|
| ||||
| Race | 0.147 | |||
|
| ||||
| White | 85.01 | 87.39 | 82.49 | |
|
| ||||
| Residencya | 0.020 | |||
|
| ||||
| Urban | 96.38 | 94.30 | 98.60 | |
|
| ||||
| Education | 0.802 | |||
|
| ||||
| Some college | 92.81 | 93.1 | 92.49 | |
|
| ||||
| Unemployed | 0.367 | |||
|
| ||||
| Yes | 61.74 | 59.74 | 63.89 | |
|
| ||||
| Poverty | 0.015 | |||
|
| ||||
| Yes | 34.04 | 28.64 | 39.90 | |
|
| ||||
| Living arrangement | < 0.001 | |||
|
| ||||
| Live together | 48.21 | 87.34 | 6.91 | |
|
| ||||
| Caregiving factors | M (SD) | M (SD) | M (SD) | p |
|
| ||||
| Extent of care | 1.59 (1.26) | 1.90 (1.42) | 1.26 (0.96) | < 0.001 |
|
| ||||
| Hours of care/week | 14.37 (26.62) | 21.25 (32.97) | 7.52 (15.54) | < 0.001 |
|
| ||||
| Duration (months) | 99.71 (127.32) | 132.34 (149.22) | 65.17 (86.88) | < 0.001 |
|
| ||||
| Financial support | 2.24 (1.35) | 2.54 (1.60) | 1.93 (0.95) | < 0.001 |
|
| ||||
| Social resources | 3.20 (0.72) | 3.31 (0.69) | 3.07 (0.74) | < 0.001 |
|
| ||||
| Stress | ||||
|
| ||||
| Perceived stress | 1.36 (0.83) | 1.35 (0.83) | 1.37 (0.83) | 0.716 |
|
| ||||
| Mental health | ||||
|
| ||||
| CES-D scores | 7.71 (6.45) | 7.48 (6.21) | 7.95 (6.72) | 0.488 |
Note.
Fisher exact tests were used in these analyses.
CES-D = Center for Epidemiological Studies-Depression Scale (Andresen, Malmgren, Carter, & Patrick, 1994).
In terms of differences between partner caregivers and friend caregivers, only a handful of background characteristics were associated with relationship type. Compared with partner-caregivers who identified as transgender (12.9%), fewer friend-caregivers identified as transgender (3.7%), and friend-caregivers had a lower rate of residing with care recipients than partner-caregivers (6.91% vs. 87.34%, respectively). In addition, the comparison of partner-caregiver and friend-caregiver groups showed friend caregivers had greater proportions residing in urban settings (98.6% vs. 94.3%) and living below 200% of the poverty level (39.9% vs. 28.6%). Friend-caregivers did not differ from partner-caregivers on characteristics of age, sex assigned at birth, sexual orientation, race, education level, or employment status.
Caregiving Demands, Resources, Stress, and Depressive Symptomology
As shown in Table 1, on average, LGBT caregivers who assisted friends indicated providing fewer types of care, providing fewer hours of care, providing shorter duration of care, and spending less money on care than LGBT caregivers caring for partners. As a group, friend-caregivers also experienced lower levels of social support as compared with those assisting a partner. The two groups did not differ in levels of perceived stress or depressive symptomatology.
When testing the measurement model as a first step, we found that the correlation between extent of care and hours of care per week (unstandardized coefficient = .27, p < 0.001) had to be added to the measurement model to ensure a good fit with the data (χ2(1) = 2.33, p = 0.13; RMSEA = 0.054, 90% CI of RMSEA: 0.000–0.149, p = 0.326; CFI = 0.993; TLI = 0.958). Adding the additional correlation between extent of care and number of hours of care per week was reasonable given that a greater extent of care would likely require more time to be spent on caregiving. All the standardized loadings of measurement items on the latent variable caregiving burden were larger than 0.3.
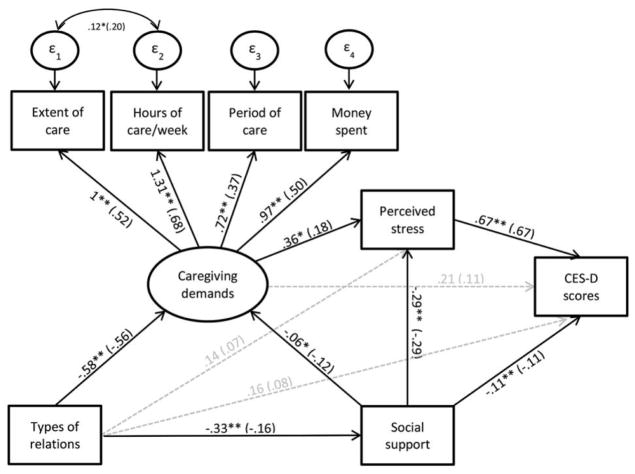
The model fitting results are presented in Figure 2. Overall, the hypothetical model we proposed fit the data well. Three associations were nonsignificant at 0.05 levels: the association between caregiver-recipient relationship and perceived stress, the association between caregiver-recipient relationship and depressive symptomatology, and the association between caregiving demands and depressive symptomatology. The p value for the chi-square test was higher than 0.05, suggesting that the model did not significantly deviate from the data. All other fit indices, including RMSEA, CFI, and TLI, showed that the model fit relatively well to the data. The RMSEA was smaller than 0.05 (RMSEA = 0.020, 90% CI of RMSEA [0.000, 0.054], p = 0.920), and both CFI and TLI were greater than 0.90 (CFI = 0.996; TLI = 0.992). We further fit an additional model (not shown) that incorporated the four demographic factors significantly related to the relational type between caregivers and recipients in Table 1. However this additional model did not fit as well as the hypothetical model based on the model fit indices (χ2(37) = 65.86, p = 0.002, RMSEA = 0.042, 90% CI of RMSEA [0.025, 0.058], p = 0.792; CFI = 0.960; TLI = 0.939). The estimations in this later model did not substantively differ from the estimations in the original model and the conclusions remained unaltered.
Figure 2.
Results of the model fitting. Note. CES-D = Center for Epidemiologic Studies–Depression Scale. Unstandardized coefficients were reported with corresponding statistical testing results; standardized coefficients are reported in parenthesis; * represented p < 0.05; ** represented p < 0.01; insignificant unstandardized coefficients at 0.05 levels are presented with gray broken arrows.
As expected, in the model shown in Figure 2, caregiving demands were positively related to perceived stress. For every one unit increase in caregiving demands, the level of perceived stress increased 0.357 standard units (SE = 0.167, p = 0.033). However, caregiving demands were not directly related to CES-D scores (unstandardized coefficient = 0.206, SE = 0.135, p = 0.126). In contrast, perceived stress had a highly significant positive association with CES-D scores such that when there was one standard unit increase in perceived stress, there was a 0.674 standard unit increase in CES-D scores (SE = 0.042, p < 0.001). The indirect effect from care demand to CES-D scores through perceived stress was also significant, such that when there was one standard unit increase in caregiving demands, CES-D scores also increased 0.240 standard units (SE = 0.112, p = 0.033). This finding suggests that the relationship between caregiving demands and CES-D scores were mediated by perceived stress. As hypothesized, the levels of caregiving demands depended on the types of relationship between caregivers and care recipients. As compared with partner-caregivers, friend-caregivers had lower levels of caregiving demands by 0.581 units (SE = 0.084, p < 0.001). At the same time, friend-caregivers had lower levels of social support by an average 0.326 standard units (SE = 0.094, p < 0.001). In turn, social support not only had direct effects on decreasing depressive symptomatology (a standard unit increase in social support was related to 0.112 standard unit decrease in CES-D scores, SE = 0.040, p = 0.004) and levels of perceived stress (a standard unit increase in social support was related to 0.293 standard unit decrease in perceived stress, SE = 0.052, p < 0.001) but also had an indirect effect on decreasing levels of perceived stress and reducing CES-D scores by alleviating caregiving demands. The combined indirect effect of social support on CES-D scores through caregiving demands and perceived stress equaled −0.226 (SE = 0.038, p < 0.001).
Compared with participants who provided spousal or partner care, older LGBT adults who provided care to a friend had lower levels of perceived stress and CES-D scores, which might be attributed to lower caregiving demands. However, friend-caregivers also had less social support than did partner-caregivers. Overall, there were differing indirect effects by relationship type on levels of perceived stress and depressive symptomatology, which seemed to cancel each other out, such that the total effect of types of relationships on the levels of perceived stress equaled 0.041 (SE = 0.094, p = 0.667) and for CES-D = 0.112 (SE = 0.097, p = 0.252).
Discussion
The current study sheds light on the ways in which informal caregivers might experience varying levels of caregiving demands, depending on the nature of their relationships with the care recipients, and enjoy different extent of social support, but share similar mental health sequelae among older LGBT adults. This study provides additional information about friend caregiving, a form of caregiving that has largely remained invisible in both research literature and policy, yet might have implications beyond the current sample. In this analysis, we found that those who provided care to friends experienced fewer caregiving demands, but also perceived less social support compared with those who provided care to partners; as a result, the two groups of caregivers had similar levels of perceived stress and depressive symptomatology. We also found that caregiving demands were positively related to perceived stress and indirectly related to higher depressive symptomatology, regardless of the caregiver and care recipient relationship type. Finally, social support was found to be negatively associated with caregiving demands, perceived stress, and depressive symptomatology.
Generally, we would expect lower levels of caregiving demands to coincide with lower subjective stress and depressive symptomatology as documented by existing literature (Pinquart & Sörensen, 2003). However, as compared with partner caregivers, LGBT older caregivers assisting friends experienced lower levels of social support, which generally plays an important role in offsetting the negative impacts of caregiving demands on perceived stress levels and depressive symptomology. These findings are partially supported by other studies. For example, caregivers for partners generally experience greater caregiving demands when compared with caregivers for “others,” which included friends (van Groenou, de Boer, & Iedema, 2013). However, another study found that caregivers for friends had similar levels of health as those who provided care for partners (Himes & Reidy, 2000). In fact, LGBT friend-caregivers may suffer a double disadvantage. As a friend providing informal care, these caregivers might not have access to other types of traditional supports that have been developed for biological or spousal caregivers. In addition, LGBT caregivers might have less access to support services (Brotman et al., 2007) because of service providers’ lack of sensitivity to LGBT issues, or these caregivers might be reluctant to use services based on their past negative experiences (Moore, 2002; Fredriksen-Goldsen, 2007; Price, 2010). Therefore, LGBT caregivers remain largely invisible, their caregiving work is unrecognized by others, and they have less access to services and policies designed to support informal caregiving.
As expected, among the LGBT caregivers, caregiving demands were positively related to perceived stress, which in turn, was related to CES-D scores. Moreover, the relationship between objective stressors (caregiving demands) and depressive symptomatology was mediated through perceived stress. This is consistent with literature that has found higher caregiving demands were related to greater subjective caregiving burden and stress (Shippy, 2007), which was subsequently associated with poor mental health outcomes, including depressive symptomatology. In their meta-analysis, Pinquart and Sörensen (2003) summarized 228 studies and concluded that higher levels of subjective caregiving burden and subsequent higher depressive symptomatology were significantly related to a greater number of care-giving tasks, more hours of caregiving activities per week, and longer durations of care.
In our analysis, social support was directly and negatively associated with objective stressors, perceived stress, and depressive symptomology. The total effect of social support on depressive symptomology across the three pathways was highly significant (including social support → depressive symptomology; social support → perceived stress → depressive symptomatology; and social support → caregiving demands → perceived stress → depressive symptomatology), suggesting that social support received by the LGBT caregivers had a significant relationship to their mental health through both direct and indirect pathways. These results mirror findings from other studies that have reported that social support can provide critical buffers for informal caregivers to offset negative influences associated with heavy caregiving demands (Hash, 2002). For example, through instrumental support, caregivers can share their caregiving duties with others (Vrabec, 1997); and, with emotional support, caregivers can better cope with their perceived stress and emotional reactions to stress levels (Shippy, 2007).
Limitations
The study findings need to be interpreted in the context of the study limitations. First, this study used a cross-sectional, observation study design that prevents any causal inference. All the relationships estimated in the SEM model were correlational in nature. Second, because caregivers often struggle to precisely quantify the hours of caregiving they provide per week, the measurement used in the current study might suffer from self-report biases, although the latent variable approach applied in the current study might help to mitigate the potential scope of this problem. Third, the sample of older LGBT caregivers was a nonprobability, community-based sample. Although community samples of LGBT populations can often have greater variability than probability samples, the study results from nonprobability samples have limited generalizability. Finally, despite the fact that most demographic factors were not significantly related to the study outcomes, other variables that were not included in the model might further influence model estimations. Future studies that incorporate longitudinal study designs will allow the assessments of caregiving demands and resources over time by relationship type. Future studies should also consider the analysis of additional factors with greater measurement quality that might further improve model estimations.
Applications to Social Work Practice
This is one of the first quantitative studies to investigate the association between the nature of caregiving relationships and the mechanisms through which care-giving demands and resources contribute to the stress and mental health among older adult LGBT caregivers. An important finding in this study is that the older adult LGBT caregivers providing friend caregiving experienced similar levels of perceived stress and depressive symptomology to their counterparts providing care to their partners and who experienced higher levels of caregiving demands. As more nations pass marriage equality laws, it is likely that LGBT partner-caregivers will be recognized by policies and social service agencies aiming at assisting informal family caregivers. However, because friend caregivers are such an important source of caregiving in LGBT communities, it is imperative that these caregivers are also recognized and provided with much-needed support and assistance.
It is critical that formal policies and health and human services agencies expand service programs in ways that are responsive to the needs of LGBT care-givers, including those providing care to friends. As argued by Himes and Reidy (2000), given the critical social and demographic changes that have eroded the capacities of modern families to provide informal caregiving to older family members, friends will likely play an increasingly significant role in care provision to older adults. For example, greater residential mobility and the increasing numbers of single-parent households and stepfamilies will likely result in the need for a range of informal caregivers, including caregiving friends (Himes & Reidy, 2000). Such needs are further exacerbated within LGBT communities because older LGBT adults are less likely to have children or other biological or legal family members to care for them as they age (Fokkema & Kuyper, 2009; Fredriksen-Goldsen, 2007; MetLife, 2010). With the growing number of older LGBT adults, friend-care must be recognized as both a real and potential source of support in these communities. Indeed, in a community sample of LGBT midlife and older adults from Minnesota, the single, older LGBT adults identified friends as the primary source of help and assistance in the hierarchy of help-seeking resources (Croghan et al., 2014). The development of promising new ways to cultivate support for these largely invisible caregivers is critical as they provide much-needed care. Even though this study focused on older adult LGBT caregivers, the findings also have implications for lifelong single and childless heterosexuals; specifically, people who do not have normative support structures will likely turn elsewhere to find caregiving (Muraco, 2012). In the coming decades, with family demographics shifting away from heterosexual marriage toward cohabitation and the declining U.S. birth rates (Cherlin, 2010), issues of informal caregiving by friends, neighbors, and others are likely to be increasingly relevant.
To encourage greater use of services among LGBT caregivers, whether caring for a partner or a friend, it will be important for social work practitioners to target specific outreach efforts to LGBT caregivers and to promote awareness of care-giving in the LGBT community as well as among service providers. Psychoeducation aimed at teaching skills for effective caregiving and stress management should be available and provided, as needed, to LGBT caregivers. Social workers in the United States can assist older LGBT adults and their caregivers in navigating complex service systems to obtain the resources available to them, such as support services through the National Family Caregiver Support Act. Finally, social workers can advocate for greater inclusion of LGBT friend-caregivers into national policies originally designed for caregivers related by blood or marriage, as well as implementation of training programs designed to promote culturally competent practices among health and aging service providers (Fredriksen-Goldsen, Hoy-Ellis, Goldsen, Emlet, & Hooyman, 2014; Valenti & Katz, 2014).
Biographies
Chengshi Shiu is a research associate in the School of Social Work, University of Washington.
Anna Muraco is an associate professor and the acting department chair of the Department of Sociology, Loyola Marymount University, Los Angeles.
Karen I. Fredriksen-Goldsen is a professor and the director of the Hartford Center of Excellence at the School of Social Work, University of Washington.
Contributor Information
Chengshi Shiu, University of Washington.
Anna Muraco, Loyola Marymount University.
Karen Fredriksen-Goldsen, University of Washington.
References
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. New York, NY: Academic Press; 1995. [Google Scholar]
- Arias E. United States life tables, 2008 (National Vital Statistics Reports) 2012 Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_03.pdf. [PubMed]
- Aronson J. Lesbians giving and receiving care: Stretching conceptualizations of caring and community. Women’s Studies International Forum. 1998;21:505–519. http://dx.doi.org/10.1016/S0277-5395(98)00065-X. [Google Scholar]
- Arno PS, Levine C, Memmott MM. The economic value of informal caregiving. Health Affairs. 1999;18:182–188. doi: 10.1377/hlthaff.18.2.182. http://dx.doi.org/10.1377/hlthaff.18.2.182. [DOI] [PubMed] [Google Scholar]
- Barker JC. Neighbors, friends, and other non-kin caregivers of community-living dependent elders. Journal of Gerontology: Social Sciences. 2002;57:158–167. doi: 10.1093/geronb/57.3.s158. http://dx.doi.org/10.1093/geronb/57.3.S158. [DOI] [PubMed] [Google Scholar]
- Baumle AK. Same-sex cohabiting elders versus different-sex cohabiting and married elders: Effects of relationship status and sex of partner on economic and health outcomes. Social Science Research. 2014;43:60–73. doi: 10.1016/j.ssresearch.2013.09.003. http://dx.doi.org/10.1016/j.ssresearch.2013.09.003. [DOI] [PubMed] [Google Scholar]
- Beach SR, Schulz R, Yee JL, Jackson S. Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the caregiver health effects study. Psychology and Aging. 2000;15:259–271. doi: 10.1037//0882-7974.15.2.259. http://dx.doi.org/10.1037/0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Bauldry S. Three Cs in measurement models: Causal indicators, composite indicators, and covariates. Psychological Methods. 2011;16:265–284. doi: 10.1037/a0024448. http://dx.doi.org/10.1037/a0024448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotman S, Ryan B, Collins S, Chamberland L, Cormier R, Julien D, … Richard B. Coming out to care: Caregivers of gay and lesbian seniors in Canada. Gerontologist. 2007;47:490–503. doi: 10.1093/geront/47.4.490. http://dx.doi.org/10.1093/geront/47.4.490. [DOI] [PubMed] [Google Scholar]
- Cantor M, Brennan M, Shippy RA. Caregiving among older lesbian, gay, bisexual, and transgender New Yorkers. New York, NY: National Gay and Lesbian Task Force Policy Institute; 2004. Retrieved from http://www.thetaskforce.org/static_html/downloads/reports/reports/CaregivingAmongOlderLGBT.pdf. [Google Scholar]
- Cherlin AJ. Demographic trends in the United States: A review of research in the 2000s. Journal of Marriage and Family. 2010;72:403–419. doi: 10.1111/j.1741-3737.2010.00710.x. http://dx.doi.org/10.1111/j.1741-3737.2010.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen CA, Colantonio A, Vernich L. Positive aspects of caregiving: Rounding out the caregiver experience. International Journal of Geriatric Psychiatry. 2002;17:184–188. doi: 10.1002/gps.561. http://dx.doi.org/10.1002/gps.561. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. http://dx.doi.org/10.2307/2136404. [PubMed] [Google Scholar]
- Croghan CF, Moone RP, Olson AM. Friends, family, and caregiving among midlife and older lesbian, gay, bisexual, and transgender adults. Journal of Homosexuality. 2014;61:79–102. doi: 10.1080/00918369.2013.835238. http://dx.doi.org/10.1080/00918369.2013.835238. [DOI] [PubMed] [Google Scholar]
- Edwards JR, Bagozzi RP. On the nature and direction of relationships between constructs and measures. Psychological Methods. 2000;5(2):155–174. doi: 10.1037/1082-989x.5.2.155. http://dx.doi.org/10.1037/1082-989X.5.2.155. [DOI] [PubMed] [Google Scholar]
- Fokkema T, Kuyper L. The relation between social embeddedness and loneliness among older lesbian, gay, and bisexual adults in the Netherlands. Archives of Sexual Behavior. 2009;38:264–275. doi: 10.1007/s10508-007-9252-6. http://dx.doi.org/10.1007/s10508-007-9252-6. [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Emlet CA, Kim HJ, Muraco A, Erosheva EA, Goldsen J, Hoy-Ellis CP. The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. Gerontologist. 2013;53:664–675. doi: 10.1093/geront/gns123. http://dx.doi.org/10.1093/geront/gns123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K, Hoy-Ellis C, Goldsen J, Emlet C, Hooyman N. Creating a vision for the future: Key competencies and strategies for culturally competent practice with lesbian, gay, bisexual, and transgender (LGBT) older adults in the health and human services. Journal of Gerontological Social Work. 2014;57:80–107. doi: 10.1080/01634372.2014.890690. http://dx.doi.org/10.1080/01634372.2014.890690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: Results from a population-based study. American Journal of Public Health. 2013;103:1802–1809. doi: 10.2105/AJPH.2012.301110. http://dx.doi.org/10.2105/AJPH.2012.301110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen K, Kim H-J, Emlet C, Muraco A, Erosheva E, Hoy-Ellis C, … Petry H. The Aging and Health Report: Disparities and resilience among lesbian, gay, bisexual, and transgender older adults. Institute for Multigenerational Health; 2011. Retrieved from http://caringandaging.org/wordpress/wp-content/uploads/2011/05/Full-Report-FINAL-11-16-11.pdf. [Google Scholar]
- Fredriksen-Goldsen K, Kim HJ, Muraco A, Mincer S. Chronically ill midlife and older lesbians, gay men, and bisexuals and their informal caregivers: The impact of the social context. Sexuality Research and Social Policy. 2009;6:52–64. doi: 10.1525/srsp.2009.6.4.52. http://dx.doi.org/10.1525/srsp.2009.6.4.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Shiu C, Goldsen J, Emlet CA. Successful aging among LGBT older adults: Physical and mental health-related quality of life by age group. Gerontologist. 2015;55:154–168. doi: 10.1093/geront/gnu081. http://dx.doi.org/10.1093/geront/gnu081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Scharlach A. Families and work: New directions in the twenty-first century. New York, NY: Oxford University Press; 2001. [Google Scholar]
- Fredriksen-Goldsen KI, editor. Caregiving with pride. Binghamton, NY: Haworth Press; 2007. [Google Scholar]
- Ginzler E. The cost of caregiving. 2010 Retrieved from the AARP website: http://www.aarp.org/relationships/caregiving/info-01-2010/ginzler_impact_of_caregiving.1.html.
- Grossman AH, D’Augelli AR, Hershberger SL. Social support networks of lesbian, gay, and bisexual adults 60 years of age and older. Journals of Gerontology Series B. 2000;55:P171–P179. doi: 10.1093/geronb/55.3.p171. http://dx.doi.org/10.1093/geronb/55.3.P171. [DOI] [PubMed] [Google Scholar]
- Hash K. Preliminary study of caregiving and post-caregiving experiences of older gay men and lesbians. Journal of Gay & Lesbian Social Services. 2002;13:87–94. http://dx.doi.org/10.1300/J041v13n04_10. [Google Scholar]
- Himes CL, Reidy EB. The role of friends in caregiving. Research on Aging. 2000;22:315–336. http://dx.doi.org/10.1177/0164027500224001. [Google Scholar]
- Kenny DA. Measuring model fit. 2014 Retrieved from http://davidakenny.net/cm/fit.htm.
- Kia J. “I’m part of this family”: How five care-giving partners of gay men story their experiences. Journal of Gay & Lesbian Social Services. 2012;24:140–157. http://dx.doi.org/10.1080/10538720.2012.669369. [Google Scholar]
- Kramer BJ. Gain in the caregiving experience: Where are we? What next? Gerontologist. 1997;37:218–232. doi: 10.1093/geront/37.2.218. http://dx.doi.org/10.1093/geront/37.2.218. [DOI] [PubMed] [Google Scholar]
- Lapierre TA, Keating N. Characteristics and contributions of non-kin carers of older people: A closer look at friends and neighbours. Ageing and Society. 2013;33:1442–1468. http://dx.doi.org/10.1017/S0144686X12000736. [Google Scholar]
- MetLife Mature Market Institute & American Society on Aging. Still out, still aging: The MetLife study of lesbian, gay, bisexual, and transgender baby boomers. 2010 Retrieved from https://www.metlife.com/assets/cao/mmi/publications/studies/2010/mmi-still-out-still-aging.pdf.
- Moore WR. Lesbian and gay elders: Connecting care providers through a telephone support group. Journal of Gay & Lesbian Social Services. 2002;14:23–41. http://dx.doi.org/10.1300/J041v14n03_02. [Google Scholar]
- Muraco A. Odd couples: Friendship at the intersection of gender and sexual orientation. Durham, NC: Duke University Press; 2012. [Google Scholar]
- Muraco A, Fredriksen-Goldsen K. “That’s what friends do”: Informal caregiving for chronically ill midlife and older lesbian, gay, and bisexual adults. Journal of Social & Personal Relationships. 2011;28:1073–1092. doi: 10.1177/0265407511402419. http://dx.doi.org/10.1177/0265407511402419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy S, Xu J, Kochanek K. Deaths: Final data for 2010 (National Vital Statistics Reports) 2013 Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_04.pdf. [PubMed]
- Pearlin LI, Aneshensel CS, LeBlanc AJ. The forms and mechanisms of stress proliferation: The case of AIDS caregivers. Journal of Health and Social Behavior. 1997;38:223–236. http://dx.doi.org/10.2307/2955368. [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. http://dx.doi.org/10.2307/2955368. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. Journals of Gerontology Series B. 2003;58:P112–P128. doi: 10.1093/geronb/58.2.p112. http://dx.doi.org/10.1093/geronb/58.2.P112. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: A meta-analysis. Journals of Gerontology Series B. 2007;62:P126–P137. doi: 10.1093/geronb/62.2.p126. http://dx.doi.org/10.1093/geronb/62.2.P126. [DOI] [PubMed] [Google Scholar]
- Price E. Coming out to care: Gay and lesbian carers’ experiences of dementia services. Health and Social Care in the Community. 2010;18:160–168. doi: 10.1111/j.1365-2524.2009.00884.x. http://dx.doi.org/10.1111/j.1365-2524.2009.00884.x. [DOI] [PubMed] [Google Scholar]
- Romeis JC. Caregiver strain toward an enlarged perspective. Journal of Aging and Health. 1989;1:188–208. doi: 10.1177/089826438900100204. http://dx.doi.org/10.1177/089826438900100204. [DOI] [PubMed] [Google Scholar]
- Rush G, Williamson GM, Stephen L, Schulz R. Depression and quality of informal care: A longitudinal investigation of caregiving stressors. Psychology and Aging. 2011;26:584–591. doi: 10.1037/a0022263. http://dx.doi.org/10.1037/a0022263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz KA, Dunphy G. An examination of perceived stress in family caregivers of older adults with heart failure. Experimental Aging Research. 2003;29:221–235. doi: 10.1080/03610730303717. http://dx.doi.org/10.1080/03610730303717. [DOI] [PubMed] [Google Scholar]
- Sherwood PR, Given CW, Given BA, von Eye A. Caregiver burden and depressive symptoms analysis of common outcomes in caregivers of elderly patients. Journal of Aging and Health. 2005;17:125–147. doi: 10.1177/0898264304274179. http://dx.doi.org/10.1177/0898264304274179. [DOI] [PubMed] [Google Scholar]
- Shippy RA. We cannot go it alone. Journal of Gay & Lesbian Social Services. 2007;18(3–4):39–51. http://dx.doi.org/10.1300/J041v18n03_03. [Google Scholar]
- Turner HA, Catania JA. Informal caregiving to persons with AIDS in the United States: Caregiver burden among central cities residents eighteen to forty-nine years old. American Journal of Community Psychology. 1997;25(1):35–59. doi: 10.1023/a:1024693707990. http://dx.doi.org/10.1023/A:1024693707990. [DOI] [PubMed] [Google Scholar]
- Valenti K, Katz A. Needs and perceptions of LGBTQ caregivers: The challenges of services and support. Journal of Gay & Lesbian Social Services. 2014;26:70–90. http://dx.doi.org/10.1080/10538720.2013.865575. [Google Scholar]
- Van Groenou MIB, de Boer A, Iedema J. Positive and negative evaluation of caregiving among three different types of informal care relationships. European Journal of Ageing. 2013;10:301–311. doi: 10.1007/s10433-013-0276-6. http://dx.doi.org/10.1007/s10433-013-0276-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houtven CH, Norton EC. Informal care and health care use of older adults. Journal of Health Economics. 2004;23:1159–1180. doi: 10.1016/j.jhealeco.2004.04.008. http://dx.doi.org/10.1016/j.jhealeco.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Vrabec NJ. Literature review of social support and caregiver burden, 1980 to 1995. Image: The Journal of Nursing Scholarship. 1997;29:383–388. doi: 10.1111/j.1547-5069.1997.tb01062.x. http://dx.doi.org/10.1111/j.1547-5069.1997.tb01062.x. [DOI] [PubMed] [Google Scholar]
- Washington KT, McElroy J, Albright D, Oliver DP, Lewis A, Meadows S, Elliott S. Experiences of sexual and gender minorities caring for adults with non-AIDS-related chronic illnesses. Social Work Research. 2015;39:71–81. http://dx.doi.org/10.1093/swr/svu030. [Google Scholar]
- Wolff JL, Agree EM. Depression among recipients of informal care: The effects of reciprocity, respect, and adequacy of support. Journals of Gerontology Series B. 2004;59(3):S173–S180. doi: 10.1093/geronb/59.3.s173. http://dx.doi.org/10.1093/geronb/59.3.S173. [DOI] [PubMed] [Google Scholar]