Abstract
Introduction
We described associations between the type of disaster experience and change in instrumental activities of daily living among older adult survivors before-after a terrible disaster.
Methods
The study took advantage of a “natural experiment” afforded by the Japan Gerontological Evaluation Study (JAGES), a nationwide cohort study established in 2010, seven months prior to the earthquake and tsunami. A follow-up survey was conducted in 2013. This study was conducted in Iwanuma, which was directly struck by tsunami. Our sample comprised community-dwelling aged survivors in Iwanuma who responded to questions about personal circumstances and functional status both before and after the disaster(N=3,547). Personal experiences of earthquake and tsunami damage was used as an exposure variable. The outcome was changes in self-reported 13-item instrumental activities of daily living (IADL), which was assessed both before and after the disaster.
Results
Among the participants, 931 reported losing family member(s) to the disaster, while a further 549 reported losing friend(s). More than half of the participants reported any damage to their houses while approximately 1 in 8 lost their car(s). The multivariable OLS regression revealed that complete house loss and disruption of internal medicine were associated with significantly worse IADL: -0.67 points (95%CI: -0.99, -0.34) for entirely destroyed homes; -0.40 points (95% CI: -0.71, -0.092) for disruption of internal medicine. By contrast, loss of family/friends/pets/cars and disruption to the other medical service were not associated with decline in IADL.
Conclusion
Complete house loss and disruption of access to internal medicine after a disaster were associated with significant adverse impact on decline in physical and cognitive functions 2.5 years after the disaster, while loss of family/friends was not.
Keywords: Independent Living, Natural Disaster, Natural Experiment, Japan
Introduction
In contrast to the wealth of evidence on the lingering mental health effects (e.g. PTSD) of exposure to natural disaster (Davidson & McFarlane, 2006), much less is understood about the residual physical health effects of disaster, particularly in the elderly. On the March 11, 2011 earthquake/tsunami that stuck northeastern Japan, roughly one-quarter of residents in the affected zones were over the age of 65 years. Given this demographic profile, we sought to document the lingering impacts of the disaster on functional declines among the elderly.
In fact, ecological studies reported increased disability prevalence among older people in the affected areas during one year and 3 years after the disaster. (Tomata et al., 2014; Tomata et al., 2015) The maintenance of functional independence with aging is influenced by a set of well characterized factors, including: a) physical activity vs. inactivity, b) social engagement vs. isolation, c) active vs. passive coping, and d) health services utilization vs. unmet medical needs.(Berkman, 2003) We hypothesized that older survivors are particularly vulnerable to the impacts of the earthquake/tsunami because many of them were relocated to temporary housing following the destruction of their property. In turn, the residential relocation disrupted their access to health services as well as their patterns of social interaction with their neighbors.
To our knowledge, no previous studies have examined what factors affect physical functioning declines among older survivors, while considering information about their mobility status pre-dating the disaster. In the absence of pre-disaster information, it can be difficult to causally attribute differences in functional capacity to the impacts of disaster experience. For example, even if we find a higher prevalence of functional limitations among people who experienced destruction of their property (compared to those who escaped such damage), we cannot exclude the possibility that these differences preceded the disaster. Hence we need studies with information pre-dating the event to clarify the causal relationship between disaster exposure and health impacts.
In the present study we took advantage of a unique “natural experiment”(Craig et al., 2012), afforded by the ongoing Japan Gerontological Evaluation Study (JAGES), a nationwide cohort of older community-dwelling adults which was established in 2010 – seven months prior to the March 11 event -- to examine prospectively the determinants of healthy aging.(Fujiwara et al., 2014; Kondo, 2010) By chance, one of the field sites of the cohort was located in Iwanuma city, Miyagi Prefecture, roughly 80 km the west of the epicenter of the 2011 Earthquake and Tsunami. This unique design allowed us to conduct a follow-up study of survivors three years after the disaster.
Methods
Data Sources and Participants
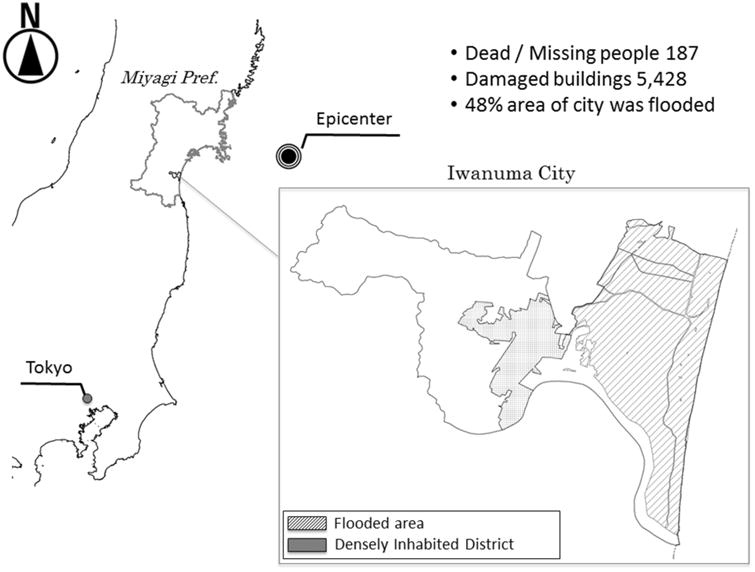
We utilized two surveys waves of the JAGES cohort conducted in 2010 (baseline) and in 2013 (in the aftermath of the East Japan Earthquake). The study profile has been previously described in detail. (Hikichi et al., 2016; Tsuboya et al., 2016) The East Japan Earthquake and Tsunami struck on March 11th, 2011. Iwanuma city, the field site for the present study, is a coastal municipality in Miyagi prefecture in Japan, located approximately 80 km west of the epicenter of the 3.11 earthquake. A total of 187 people lost their lives or were reported missing in Iwanuma, while 48% of the land mass was inundated by the tsunami. (see Figure 1) (Ishigaki et al., 2013)
Figure 1.
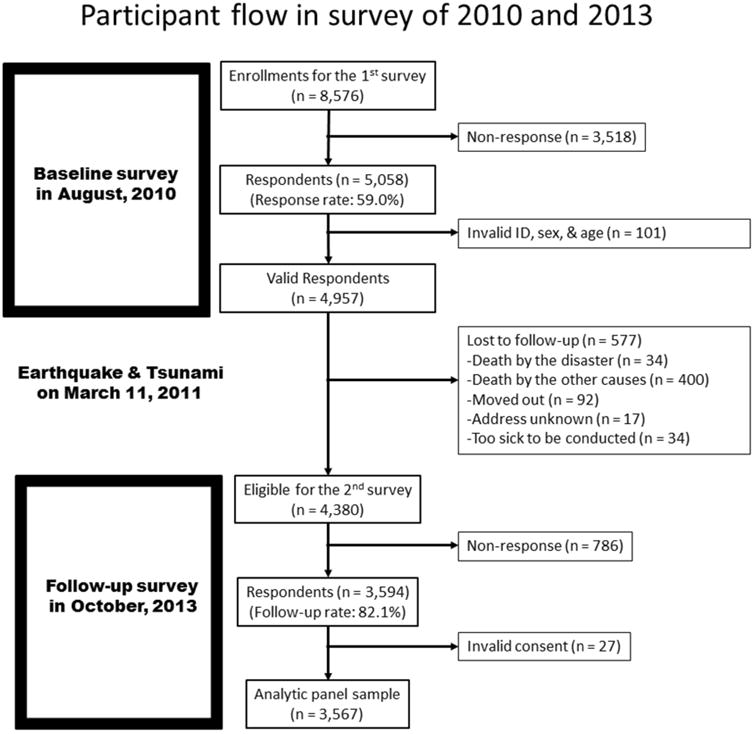
The baseline survey was completed in August 2010, seven months prior to the earthquake. A census was conducted on every resident of Iwanuma aged 65 years or older (n= 8,576), inviting them to participate in the JAGES cohort study. The mailed survey inquired about their health status, health behaviors, as well as a 13-item inventory of their Instrumental activities of daily living (IADL). The response rate to the initial invitation was 59.0% (5,058/8,576), which is somewhat higher than the average among comparable community surveys of this type. (Santos-Eggimann et al., 2009; Sinclair et al., 2012; WD, 2013) Out of the 5,058 respondents, we excluded 101 due to missing sex or age, resulting in 4,957 valid responses to the baseline survey. Out of the 4,957 baseline respondents, a further 577 individuals were excluded at the follow-up survey because of the following reasons: death by the disaster (n = 34), death by other causes (n = 400), moved out (n = 92), address unknown (n = 17), too sick to be conducted (n = 34).
Approximately 2.5 years after the earthquake and tsunami, we mailed a follow-up survey to all eligible survivors between Oct 2013 and Jan 2014. The follow-up survey inquired about personal experiences of the disaster, such as property damage/loss as well as the loss of loved ones. Trained survey teams then visited all the households to collect the completed surveys. Informed consent was obtained at the time of survey collection. The response rate to the 2013 follow-up survey was 82.1% (3,594/4,380) among the eligible participants. From the 3,594 respondents, we excluded 27 due to invalid consent form, resulting in 3,567 participants at the follow-up survey. We also excluded 20 participants who were missing 7 or more items on the 13-item IADL questionnaire, resulting in a final analytic sample of 3,547. A detailed flow chart of the participant selection is presented in Figure 2 (participants flow).
Figure 2.
Dependent Variable: Instrumental Activities of Daily Living (IADL)
Instrumental activities of daily living (IADL) consist of physical and cognitive activities that people perform in daily life such as cooking, driving, using the telephone or computer, shopping, keeping track of finances, managing their medication and so on. In the present study, IADL was measured by a 13-item self-reported battery, which has been validated in a previous study. (Koyano et al., 1991) Respondents check ‘yes’(1) or ‘no’(0) to each item. The total score is the sum total of 13-items, with higher score indicating higher ability to perform these instrumental activities of daily living. Among the eligible 3,547 participants, we imputed the overall score for 367 (10.3%) respondents who were missing up to six items on the IADL score, based upon the average of the available items. The dependent variable in our analysis was the difference in IADL score between baseline (2010) and follow-up (2013), i.e. subtracting the IADL score (2010) from IADL score (2013). For example, if the value of the change score is negative, the functional status of that individual deteriorated between 2010 and 2013. Averages and standards deviation of IADL scores are also shown in Table 1.
Table 1. Characteristics in 2010 and Instrumental Activities of Daily Living (IADL) Scores among the Study Participants (N=3,547).
| n | (%) | IADL in 2010 | IADL in 2013 | Change in IADL | ||||
|---|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | |||
| Sex | ||||||||
| Men | 1,543 | 43.5 | 11.6 | 2.0 | 11.0 | 2.7 | -0.6 | 2.1 |
| Women | 2,004 | 56.5 | 11.5 | 2.5 | 10.8 | 3.3 | -0.7 | 2.1 |
| in total | 3,547 | 100.0 | 11.6 | 2.3 | 10.9 | 3.0 | -0.7 | 2.1 |
| Age (years old) | ||||||||
| Average (standard deviation) | 73.6 | (6.3) | ||||||
| Marital status | ||||||||
| Married | 2,453 | 69.2 | 11.8 | 2.0 | 11.3 | 2.7 | -0.5 | 2.0 |
| Windowed | 828 | 23.3 | 11.1 | 2.8 | 10.0 | 3.6 | -1.0 | 2.3 |
| Divorced | 85 | 2.4 | 11.5 | 2.3 | 11.3 | 2.5 | -0.2 | 1.6 |
| Never married | 42 | 1.2 | 10.9 | 2.5 | 10.3 | 3.0 | -0.6 | 1.8 |
| Others | 21 | 0.6 | 10.6 | 3.3 | 10.1 | 3.5 | -0.5 | 1.8 |
| Education (years) | ||||||||
| <6 | 47 | 1.3 | 8.3 | 4.4 | 6.2 | 5.0 | -2.1 | 3.0 |
| 6-9 | 1,173 | 33.1 | 11.1 | 2.6 | 10.3 | 3.3 | -0.8 | 2.4 |
| 10-12 | 1,483 | 41.8 | 11.9 | 1.9 | 11.4 | 2.5 | -0.5 | 1.8 |
| 13 or more | 711 | 20.0 | 12.0 | 1.9 | 11.5 | 2.6 | -0.5 | 1.9 |
| Others | 30 | 0.8 | 10.7 | 3.3 | 9.8 | 3.8 | -0.9 | 2.5 |
| Equivalized household income (JPY, Japanese yen)a | ||||||||
| < 2million | 1,414 | 39.9 | 11.4 | 2.5 | 10.8 | 3.0 | -0.6 | 2.0 |
| 2-4 million | 1,202 | 33.9 | 11.9 | 2.0 | 11.4 | 2.7 | -0.5 | 1.8 |
| > 4million | 285 | 8.0 | 11.7 | 2.2 | 11.0 | 3.2 | -0.7 | 2.1 |
| Self-rated health | ||||||||
| Excellent | 422 | 11.9 | 12.2 | 1.6 | 11.8 | 2.2 | -0.4 | 1.6 |
| Good | 2,407 | 67.9 | 11.9 | 1.9 | 11.3 | 2.7 | -0.6 | 2.0 |
| Fair | 536 | 15.1 | 10.3 | 3.0 | 9.3 | 3.6 | -1.0 | 2.7 |
| Poor | 119 | 3.4 | 8.3 | 3.9 | 6.9 | 4.0 | -1.4 | 3.1 |
| Body mass index (kg/m2) | ||||||||
| <18.5 | 152 | 4.3 | 11.0 | 2.9 | 9.9 | 3.9 | -1.1 | 2.8 |
| 18.5-24.9 | 2,219 | 62.6 | 11.7 | 2.1 | 11.1 | 2.8 | -0.6 | 2.0 |
| ≥25 | 948 | 26.7 | 11.6 | 2.3 | 10.9 | 2.8 | -0.7 | 1.9 |
| Smoking habit | ||||||||
| Never smoker | 1,996 | 56.3 | 11.6 | 2.4 | 11.0 | 3.1 | -0.7 | 2.1 |
| Former smoker (quit 4 year or more ago) | 763 | 21.5 | 11.6 | 2.1 | 11.0 | 2.7 | -0.6 | 2.1 |
| Former smoker (quit in 4 years) | 137 | 3.9 | 11.3 | 2.4 | 10.8 | 3.2 | -0.6 | 2.1 |
| Current smoker | 365 | 10.3 | 11.6 | 1.9 | 10.9 | 2.6 | -0.7 | 2.1 |
| Drinking habit | ||||||||
| Drinker | 1,277 | 36.0 | 11.9 | 1.7 | 11.5 | 2.2 | -0.4 | 1.8 |
| Former drinker | 119 | 3.4 | 11.0 | 2.7 | 9.9 | 3.5 | -1.0 | 2.5 |
| Rarely drink | 2,081 | 58.7 | 11.4 | 2.6 | 10.6 | 3.4 | -0.8 | 2.2 |
| Having any chronic diseases or conditions | ||||||||
| Present | 2,743 | 77.3 | 11.4 | 2.4 | 10.7 | 3.2 | -0.7 | 2.2 |
| No | 735 | 20.7 | 12.0 | 1.7 | 11.6 | 2.4 | -0.4 | 1.9 |
| Frequency of informal socializing with neighbors | ||||||||
| Almost everyday | 417 | 11.8 | 12.1 | 1.4 | 11.4 | 2.6 | -0.7 | 2.0 |
| Twice or three times a week | 841 | 23.7 | 12.1 | 1.8 | 11.4 | 2.6 | -0.6 | 1.9 |
| Once a week | 608 | 17.1 | 11.9 | 1.8 | 11.3 | 2.7 | -0.6 | 2.1 |
| Once or twice a month | 719 | 20.3 | 11.9 | 1.9 | 11.3 | 2.6 | -0.6 | 2.0 |
| Several times a year | 566 | 16.0 | 11.3 | 2.2 | 10.7 | 2.8 | -0.6 | 2.1 |
| Rarely | 247 | 7.0 | 8.4 | 3.8 | 7.8 | 4.1 | -0.6 | 2.5 |
Note. Instrumental Activities of Daily Living (IADL). SD: standard deviation.
JPY=Japanese Yen, 120 JPY is approximately equal to 1 USD (US dollar) in April 2016.
Independent Variable: Disaster experiences
On the follow-up survey we inquired about the following experiences of the earthquake and tsunami: 1) loss of family/friends, 2) loss of pets, 3) loss of property (housing and cars), 4) loss of employment, and 5) disruption in access to medical care.
1) Loss of family or friends
Loss of family or friends due to the disaster was assessed by the following question. “Did you lose a close relative or friend in the earthquake?” Potential responses ranged from “1. Close relative, 2. Close friend, 3. No”.
2) Loss of pets
Loss of family or friends due to the disaster was assessed by the following question. “Did you lose a dog, cat, or other pet in the earthquake?” Potential responses ranged from “1. Dog, 2. Cat, 3. Other pet, 4. No, 5. I did not have a pet”. Previous studies reported that owing dogs is positively associated with habitual exercising, which would affect IADL. (Christian et al., 2013; Levine et al., 2013)
3) Loss of property (housing and cars)
Damage/loss of property due to the disaster was assessed by the following question. “How badly was your residence damaged in the earthquake?” Potential responses ranged from “1. Completely destroyed, 2. Mostly destroyed, 3. Half destroyed, 4. Partially destroyed, 5. No damage”. The five response categories are based on official designations determined by the local government for the purposes of compensation. Loss of cars due to the disaster was assessed by the following question. “Did you lose your car in the earthquake?” Potential responses ranged from “1. Yes, 2. No, 3. I did not have car(s) when the disaster happened” In the analysis, we dichotomized the answers: Yes, or the others. In the area, people in general need cars to go to grocery stores.
4) Loss of employment
Loss of employment due to the disaster was assessed by the following question. “Did your job conditions change after the earthquake?” Potential responses ranged from “1. I lost my job, but it was later reinstated, 2. I lost my job, and do not currently work, 3. I did not work prior to the earthquake, 4. I work in the same job as I did prior to the earthquake, 5. I started a new job”. In the analysis, we dichotomized the answers: we regarded “1 and 2” as those who lost their job due to the disaster.
5) Disruption in access to medical care
Disruption in access to medical care was assessed by the following question. For which types of services did you experience interruption of care? Check all that apply.” Potential responses ranged from “1. Dentistry, 2. Internal medicine, 3. Orthopedics, 4. Ophthalmology, 5. Psychiatry, 6. Other”.
Covariates
The surveys also gathered information on socio-demographic characteristics (sex, age, marital status, years of education, income), self-rated health, body mass index (BMI), smoking and drinking habits, history of diseases, as well as frequency of informal socializing with neighbors. Descriptive information about respondents is summarized in Table 1 and Table 2. These demographic characteristics and IADL score in 2010 were adjusted in the multivariable model in Table 3.
Table 2. Disaster Damage and Instrumental Activities of Daily Living (IADL) Scores among the Study Participants (N=3,547).
| n | (%) | IADL in 2010 | IADL in 2013 | Change in IADL | ||||
|---|---|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | |||
| Loss of family and friends | ||||||||
| No loss | 2,223 | 62.7 | 11.5 | 2.4 | 10.7 | 3.1 | -0.7 | 2.2 |
| Loss of family members | 775 | 21.8 | 11.6 | 2.2 | 11.0 | 3.0 | -0.6 | 2.1 |
| Loss of friends | 393 | 11.1 | 11.9 | 2.0 | 11.4 | 2.5 | -0.4 | 1.7 |
| Both | 156 | 4.4 | 11.7 | 2.7 | 11.3 | 3.0 | -0.4 | 2.1 |
| Loss of pet(s) | ||||||||
| Had no pets | 2,513 | 70.8 | 11.6 | 2.2 | 11.0 | 2.9 | -0.6 | 2.1 |
| No pet loss | 742 | 20.9 | 11.5 | 2.5 | 10.9 | 3.2 | -0.6 | 2.1 |
| Lost dog(s) | 73 | 2.1 | 11.7 | 1.8 | 10.7 | 3.0 | -1.0 | 2.5 |
| Lost cat(s) | 52 | 1.5 | 11.2 | 2.6 | 9.9 | 3.6 | -1.3 | 3.0 |
| Lost other pets | 18 | 0.5 | 10.9 | 3.3 | 10.3 | 3.9 | -0.5 | 1.3 |
| Lost dog(s) & cat(s) | 9 | 0.3 | 9.7 | 4.3 | 8.8 | 4.9 | -1.0 | 2.9 |
| Lost cat(s) & other pets | 2 | 0.1 | 4.5 | 2.1 | 4.5 | 3.5 | 0.0 | 1.4 |
| Lost dog(s) & other pets | 1 | 0.0 | 1.0 | . | 0.0 | . | -1.0 | . |
| House damage | ||||||||
| Entirely destroyed | 157 | 4.4 | 11.0 | 2.9 | 9.8 | 3.7 | -1.24 | 2.8 |
| Largely destroyed | 131 | 3.7 | 11.4 | 2.7 | 10.5 | 3.5 | -0.91 | 2.4 |
| Half destroyed | 256 | 7.2 | 11.3 | 2.5 | 10.7 | 3.1 | -0.61 | 2.1 |
| Partly destroyed | 1,488 | 42.0 | 11.7 | 2.2 | 11.1 | 2.9 | -0.62 | 2.0 |
| No damage | 1,417 | 39.9 | 11.6 | 2.3 | 11.0 | 2.9 | -0.58 | 2.0 |
| Car damage | ||||||||
| Lost cars | 452 | 12.7 | 11.5 | 2.5 | 10.7 | 3.3 | -0.78 | 2.4 |
| Did not have cars at that time | 409 | 11.5 | 11.2 | 2.5 | 10.3 | 3.2 | -0.85 | 2.1 |
| No damage of cars | 2,595 | 73.2 | 11.6 | 2.2 | 11.0 | 2.9 | -0.59 | 2.0 |
| Job change | ||||||||
| Lost jobs, but have restarted the same job | 54 | 1.5 | 12.0 | 1.8 | 12.0 | 1.5 | 0.08 | 1.2 |
| Have lost jobs | 141 | 4.0 | 11.4 | 2.2 | 10.7 | 2.8 | -0.62 | 1.8 |
| Have not been working | 2,216 | 62.5 | 11.4 | 2.4 | 10.7 | 3.2 | -0.76 | 2.2 |
| Have been working | 660 | 18.6 | 12.1 | 1.6 | 11.9 | 1.8 | -0.16 | 1.4 |
| Have started a new job after the disaster | 28 | 0.8 | 12.2 | 1.2 | 11.9 | 1.4 | -0.28 | 1.4 |
| Disruption to medical service | ||||||||
| Dentistry | 74 | 2.1 | 11.7 | 1.9 | 11.2 | 2.3 | -0.45 | 1.5 |
| Internal medicine | 161 | 4.5 | 11.2 | 2.6 | 10.0 | 3.5 | -1.23 | 2.7 |
| Orthopedics | 89 | 2.5 | 10.6 | 2.7 | 9.7 | 3.4 | -0.96 | 2.5 |
| Ophthalmology | 75 | 2.1 | 11.0 | 2.7 | 10.0 | 3.3 | -0.91 | 2.7 |
| Psychiatry | 19 | 0.5 | 9.2 | 3.9 | 7.6 | 5.0 | -1.64 | 3.8 |
| Either | 327 | 9.2 | 11.0 | 2.7 | 10.1 | 3.5 | -0.88 | 2.4 |
Note. Instrumental Activities of Daily Living (IADL). SD: standard deviation.
JPY=Japanese Yen, 120 JPY is approximately equal to 1 USD (US dollar) in April 2016.
Table 3. Multivariable Adjusted Association of Each Disaster Damage with Change in Instrumental Activities of Daily Living (IADL) Scores among the Survivors from the Disaster in Japan (N=3,547).
| Characteristics | Coefficient | SE | 95%CI | p-value | |
|---|---|---|---|---|---|
| Age (continuous) | -0.11 | 0.006 | -0.12, -0.10 | <.0001 | |
| Loss of family and friends | |||||
| No loss | reference | ||||
| Loss of family members | 0.07 | 0.08 | -0.09 0.23 | 0.39 | |
| Loss of friends | 0.10 | 0.11 | -0.11 0.31 | 0.37 | |
| Both | 0.19 | 0.16 | -0.13 0.51 | 0.24 | |
| Loss of pet(s) | |||||
| Had no pets | 0.09 | 0.08 | -0.07 0.25 | 0.27 | |
| No pet loss | reference | ||||
| Lost dog(s) | -0.17 | 0.24 | -0.64 0.30 | 0.49 | |
| Lost cat(s) | -0.42 | 0.28 | -0.97 0.13 | 0.13 | |
| Lost other pets | -0.34 | 0.47 | -1.25 0.58 | 0.47 | |
| House damage | |||||
| Entirely destroyed | -0.67 | 0.17 | -0.99 -0.34 | <.0001 | |
| Largely destroyed | -0.26 | 0.18 | -0.61 0.09 | 0.15 | |
| Half destroyed | -0.11 | 0.13 | -0.37 0.15 | 0.40 | |
| Partly destroyed | -0.05 | 0.07 | -0.19 0.09 | 0.48 | |
| No damage | reference | ||||
| Car damage | |||||
| Lost cars | -0.18 | 0.10 | -0.37 0.02 | 0.08 | |
| Did not have cars at that time | 0.12 | 0.11 | -0.09 0.34 | 0.25 | |
| No damage of cars | reference | ||||
| Job loss | |||||
| Lost jobs, but have restarted the same job | 0.23 | 0.28 | -0.31 0.77 | 0.40 | |
| Have lost jobs | -0.36 | 0.18 | -0.72 -0.01 | 0.045 | |
| Have not been working | -0.28 | 0.09 | -0.46 -0.11 | 0.0016 | |
| Have been working | reference | ||||
| Have started a new job after the disaster | -0.29 | 0.38 | -1.03 0.45 | 0.44 | |
| Disruption of access to medical service | |||||
| Dentistry | 0.22 | 0.23 | -0.23, 0.67 | 0.35 | |
| Internal Medicine | -0.40 | 0.16 | -0.71, -0.092 | 0.011 | |
| Orthopedics | 0.027 | 0.21 | -0.39, 0.44 | 0.90 | |
| Ophthalmology | -0.10 | 0.23 | -0.55, 0.35 | 0.65 | |
| Psychiatry | -0.71 | 0.45 | -1.60, 0.18 | 0.12 | |
| Either | -0.13 | 0.11 | -0.36, 0.090 | 0.24 |
Note. Instrumental Activities of Daily Living (IADL). SE: standard error.
Age, sex, marital status, educational attainment, income, self-rated health, BMI, smoking status, drinking status, history of diseases, frequency of informal socializing with neighbors and IADL score in 2010 were adjusted in the multivariable analysis.
Other types of disaster damage were not simultaneously included in the same model.
Statistical Analysis
We used OLS regression to examine the association between experiences of the disaster and change in IADL scores. Change in IADL score was modeled as a continuous variable. The multivariate adjusted results were expressed as non-standardized coefficients with 95% confidence intervals (CI) in Table 3. Many respondents suffered from more than one type of disaster experience. We therefore mutually controlled for different categories of disaster experience in Table 3. The significant adverse experiences in the disaster (housing damage, job loss, interruption of medical care) were adjusted in the same model (Supplementary Table 1). In Table 4, we have repeated the analyses after dividing the IADL into 3 categories (1: instrumental IADL, 2: intellectual IADL, 3: social IADL) and treating the three sub-scales as separate outcomes. All analyses were performed with SAS version 9.4 statistical software (SAS Institute Inc, Cary, North Carolina). We defined significance as a 2-sided P value <.05.
Table 4.
Association between disaster damages and change in sub Instrumental Activities of Daily Living. Several disaster damage (loss of family/friends, house/car, job, medical utility) were adjusted in the same model.
| Characteristics | 1) 5 items for instrumental IADL, N=3409 | 2) 4 items for intellectual IADL, N=3381 | 3) 4 items for social IADL, N=3365 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Coefficient | 95%CI | p-value | Coefficient | 95%CI | p-value | Coefficient | 95%CI | p-value | |
| Loss of family and friends | |||||||||
| No loss | reference | reference | reference | ||||||
| Loss of family members | 0.03 | -0.04 0.11 | 0.40 | 0.02 | -0.04 0.08 | 0.50 | 0.06 | -0.02 0.13 | 0.13 |
| Loss of friends | 0.01 | -0.09 0.11 | 0.89 | 0.03 | -0.05 0.10 | 0.51 | 0.13 | 0.03 0.22 | 0.011 |
| Both | 0.08 | -0.07 0.23 | 0.28 | 0.09 | -0.02 0.20 | 0.12 | 0.15 | 0.00 0.30 | 0.046 |
| House damage | |||||||||
| Entirely destroyed | -0.36 | -0.54 -0.18 | 0.0001 | -0.19 | -0.33 -0.06 | 0.006 | -0.11 | -0.29 0.06 | 0.21 |
| Largely destroyed | -0.13 | -0.30 0.05 | 0.15 | -0.08 | -0.22 0.05 | 0.22 | -0.03 | -0.21 0.14 | 0.72 |
| Half destroyed | -0.06 | -0.20 0.07 | 0.35 | -0.07 | -0.17 0.03 | 0.17 | 0.02 | -0.11 0.15 | 0.74 |
| Partly destroyed | -0.03 | -0.10 0.03 | 0.33 | -0.02 | -0.07 0.03 | 0.39 | 0.00 | -0.07 0.06 | 0.92 |
| No damage | reference | reference | reference | ||||||
| Car damage | |||||||||
| Lost cars | -0.05 | -0.16 0.07 | 0.41 | -0.01 | -0.09 0.08 | 0.86 | 0.03 | -0.08 0.14 | 0.64 |
| Did not have cars at that time | 0.09 | -0.01 0.19 | 0.08 | 0.06 | -0.02 0.14 | 0.12 | 0.05 | -0.05 0.15 | 0.33 |
| No damage of cars | reference | reference | reference | ||||||
| Job loss | |||||||||
| Lost jobs, but have restarted the same job | 0.22 | -0.03 0.48 | 0.08 | 0.10 | -0.09 0.29 | 0.31 | -0.01 | -0.26 0.24 | 0.96 |
| Have lost jobs | -0.01 | -0.18 0.16 | 0.94 | 0.01 | -0.12 0.14 | 0.86 | -0.23 | -0.40 -0.06 | 0.007 |
| Have not been working | -0.05 | -0.14 0.03 | 0.20 | -0.07 | -0.13 -0.01 | 0.03 | -0.16 | -0.24 -0.08 | 0.0001 |
| Have been working | reference | reference | reference | ||||||
| Have started a new job after the disaster | -0.01 | -0.35 0.34 | 0.97 | -0.08 | -0.35 0.18 | 0.54 | -0.12 | -0.47 0.22 | 0.49 |
| Disruption to medical service | |||||||||
| Internal medicine | -0.21 | -0.36 -0.06 | 0.006 | -0.07 | -0.18 0.04 | 0.22 | -0.08 | -0.22 0.07 | 0.29 |
Note. Instrumental Activities of Daily Living (IADL). SE: standard error.
Age, sex, marital status, educational attainment, income, self-rated health, BMI, smoking status, drinking status, history of diseases, frequency of informal socializing with neighbors and IADL score in 2010 were adjusted in the multivariable analysis.
Results
Among the participants, 931(26.2%) reported losing family member(s), and 549(15.5%) losing friend(s). More than half of the participants reported some extent of housing damage, while approximately 1 in 8 (12.7%) lost their car(s). Compared with the human and property loss, the number of those who lost their job(s) was relatively small: 186 (5.1%). One hundred sixty one (4.5%) participants reported disruption in access to internal medicine. Mean (SD) of IADL scores were 11.6 (2.3) at baseline (2010, pre-disaster) and 10.9 (3.0) at follow-up (2013).
Table 2 shows the average (unadjusted) change in IADL score between waves. The changes by the disaster damages were -1.24 points for ”entirely destroyed” of housing ; -0.62 points for ”have lost jobs”; -1.23 points for disruption of access to internal medicine.
Table 3 shows the multivariate adjusted associations between each type of disaster damage and change in IADL score. In these models, house loss was significantly associated with worsening IADL scores: -0.67 (95%CI: -0.99, -0.34, p<.0001) for total housing loss in comparison to those whose houses were not affected at all. Losing jobs due to the disaster was also significantly associated with worsening IADL scores: -0.36 (95%CI: -0.72, -0.01, p=0.045) in comparison to those who had been working before and after the disaster. Besides, disruption of access to internal medicine after the disaster was also significantly associated with worsening IADL: -0.40 points (95%CI: -0.71, -0.092, p=0.011) in comparison to those who did not experience the disruption. The size of these coefficients can be compared to the average impact of a year of age in this sample (-0.11); effect of complete house loss on IADL (-0.67) was comparable to that from ageing by 6 years. By contrast, the other kinds of damage/loss were not associated with IADL: loss of family members or friends, loss of dogs/cats/other pets, loss of cars, or disruption of access to medical service other than internal medicine were not significantly associated with worsening IADL.
Table 4 shows that housing damage was associated with decline in instrumental & intellectual IADL, but not decline in social IADL. Disruption in access to internal medicine was associated with decline in instrumental IADL. On the other hand, loss of family or friends was associated with increased (not decreased) social IADL.
Discussions
To our knowledge, this is the first study to utilize pre-disaster information to examine the impact of disaster exposure on functional status in a community-dwelling sample of older adults. We found that loss of housing and disruption in access to internal medicine predicts worsening of functional status among elderly survivors up to three years after the disaster. Specifically, housing damage was associated with decline in instrumental & intellectual IADL. Unexpectedly, we found that experiencing the loss of loved ones were not associated with change in functional status.
To our knowledge, no studies have examined the long-term impact of disaster damage on physical and cognitive function. Our present study is consistent previous reports about the adverse mental health impacts of property damage and job loss; but no previous reports were found on functional status. The present study is consistent with the ecological data (Tomata et al.,2015) reporting increased disability prevalence in the affected areas, and provides a possible mechanism for explaining the increase. The present finding also agrees with the report that cognitive ability among survivors in the affected areas declined more than people in non-affected areas. (Ishiki et al., 2016)
Our study was unique in that we followed the participants for about 2.5 years. Most studies on survivors after natural disasters have been conducted up to one year or so following the experience of disaster. One notable exception was the study by Arnberg et al. following the 2,204 Indian Ocean tsunami. (Arnberg et al., 2015) They reported that exposure of tsunami was associated with an increased risk of severe psychopathology among victims up to 5 years after the disaster independently of previous psychiatric morbidity. (Arnberg et al., 2015) However, we are not aware of studies that have focused on functional limitations among elderly survivors.
To our surprise, loss of family/friends was not associated with decline of IADL. In general, the loss of a loved one is associated with an increased risk of excess mortality in the short term – as in the “widowhood” effect. (Moon et al., 2011) Because our follow-up survey only included individuals who were alive at both waves, it is possible that we missed individuals who died as a result of a grief reaction in the immediate aftermath of the disaster.
A major strength of our study is the availability of information on physical and cognitive ability pre-dating the disaster. To our knowledge, only one previous study by Fergusson et al. has incorporated pre-disaster information. (Fergusson et al., 2014) In that study, the authors could take advantage of an ongoing birth cohort in Christchurch, New Zealand, which was struck by a major earthquake in the Canterbury Region in New Zealand's South Island. The outcome in that study was mental health, and as far as we know, there are no studies that focused on the impacts of disaster experience on physical and cognitive functioning.
The effect sizes for IADL decline following disruption in access to internal medicine and destruction of houses are both statistically and clinically meaningful. The magnitude of the changes in IADL scores was roughly equivalent to the impact of ageing by 4-6 years (Table 3). We also have reported that disruption of access to psychiatry after disasters was significantly associated with worsening of depressive symptoms. (Tsuboya et al., 2016) Disruption of access to medical service after disasters might worse not only mental function, but also physical and cognitive function for a few years among older survivors.
A possible mechanism for the association between disaster experience and decline of IADL is the disruptions in medical care access as well as social engagement caused by residential relocation. A mechanism between decline in IADL and the disruption of internal medicine care could be explained by, for example, an exacerbation of comorbid conditions due to interruptions in prescription medication (e.g. diabetes or cardiovascular disease). Aoki et al., reported that heart failure as well as stroke and pneumonia increased significantly during the months following the disaster. (Aoki et al., 2012) This implies that special medical services, such as mobile medical team including physicians and pharmacists with medical essential drugs, should be a priority in the aftermath of disasters, and may be effective in alleviating the burden of decline in physical and cognitive problems following disasters. The connection between housing loss and decline in IADL could be explained by, for example, deterioration in cognitive, physical or mental ability among the participants due to relocation after the disaster.
Limitations
There are a number of limitations in the current study. First, both experiences of disaster damage and IADL scores were based on self-reported information, and therefore, potentially subject to common method bias. (Podsakoff et al., 2003) In fact, we found attenuated coefficients when we repeated the main analysis with survivors with baseline GDS (geriatric depression scale) scores below 5. For example, the association “completely destroyed” housing and change in IADL score was attenuated from -0.67 (p<.001) in the full sample to -0.44 (p=.03) in the sub-sample who were not depressed at baseline (data not shown). On the other hand, the baseline reports of IADL functioning could not have been influenced by the exposure (disaster experience), since – by definition – our assessments were obtained seven months before the event. We cannot exclude the possibility that individuals whose IADL decreased between survey waves were also more likely to selectively recall personal experiences of damage. On the other hand, the respondents' report of damage to their property – although self-reported – was based upon official designations made by the local government assessors for the purposes of compensation. Therefore, these reports are not based on subjective judgement. Second, although the actual number of individuals lost to follow up in our sample is quite low (by international standards) (Santos-Eggimann et al., 2009; Sinclair et al., 2012; WD, 2013), a proportion of the baseline participants (577/4,957; 11.6 percent) were lost to follow-up, which might bias the concerned associations. Indeed, participants who were lost to follow-up were more likely to report lower IADL at baseline: average (SD) of IADL score at baseline was 7.52 (4.92) for those who were no followed, and 11.3 (2.62) for those who successfully followed. However, we also have confirmed similar results with multiple imputed dataset (N=5,048, Supplementary Table2), and therefore, we believe the effect of the selection bias would not be substantial. Third, we cannot differentiate whether the decline happened in the acute phase or in the chronic phase with the present data. Fourth, our results may not be generalizable to other regions, because of differences in the types and extent of housing damage, as well as local differences in the health status of affected populations. Lastly, the association between decline in IADL and disruption in access to internal medicine could be partly explained by reverse causation – i.e. survivors who experienced difficulty in accessing medical service after the disaster already had lower IADL function prior to the disaster. Indeed, the average pre-disaster IADL score among those who experienced “disruption to internal medicine” was slightly lower (average IADL=11.2, SD=2.6, N=161) than that among those who did not report disruption in access to care (average IADL=11.6, SD=2.3, N=3,386). Besides, the association might be overestimated because healthy persons who did not need to take medical service were included in reference group.
Conclusion
Loss of housing and disruption of access to internal medicine care were significantly associated with worsening IADL functioning approximately three years after the Great East Japan earthquake and tsunami. Older residents represent a vulnerable population in the context of disaster, and efforts to prevent functional decline in the aftermath of disaster should focus on the continuous provision medical services as well as the minimization of disruption to daily routines for displaced victims.
Supplementary Material
Supplementary Table 1. Association between disaster damages and change in Instrumental Activities of Daily Living. Significant disaster damage (house, job, medical utility) were adjusted in the same model.
Supplementary Table 2. Comparison of Complete Case Analyses(N=3,547) with Multiple Imputed Dataset(N=5,048) in the Multivariable Adjusted Association of Main Disaster Damage with Change in Instrumental Activities of Daily Living (IADL) Scores among the Survivors from the Disaster in Japan.
Highlights.
Few studies have examined physical and cognitive function after natural disasters.
House damage seemed to result in a more lasting adverse impact on physical health.
Accessing to internal medicine was associated physical and cognitive function.
Loss of loved ones was not associated with physical and cognitive functions.
Monitoring of survivors is needed even up to 3 years after natural disasters.
Acknowledgments
We appreciate the support and cooperation of the Iwanuma Mayor's office, and the staff of the Department of Health and Welfare of Iwanuma city government.
This work was supported by the NIH (R01 AG042463), as well as the Grant-in-Aid for Scientific Research2011-2016 (23243070), 2011-2014 (No. 22390400) and 2012-2015 (No. 24390469) from the Japanese Ministry of Education, Culture, Sports, Science and Technology (MEXT), Health Labour Sciences Research Grant 2012-2015 (H24-Choju-Wakate-009), and the Center for Well-being and Society, Nihon Fukushi University, MEXT-Supported Program for the Strategic Research Foundation at Private Universities, 2009-2013. The funding sources did not have a role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript: or the decision to submit the manuscript.
Dr. Tsuboya made the analysis plan, analyzed the data, and made a draft. Dr. Aida, Dr. Hikichi, Dr. Subramanian, Dr. Kondo, Dr. Osaka, and Dr. Kawachi conception and design, acquisition of data, analysis and interpretation of data. All authors revised the draft critically and approved the final manuscript. Dr. Tsuboya is a guarantor.
Footnotes
The aim of the present study is to investigate the prospective association of disaster damage and physical functional status after a terrible earthquake and the following tsunami in Japan.
No financial disclosures were reported by the authors of this paper
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aoki T, Fukumoto Y, Yasuda S, et al. The Great East Japan Earthquake Disaster and cardiovascular diseases. Eur Heart J. 2012;33:2796–2803. doi: 10.1093/eurheartj/ehs288. [DOI] [PubMed] [Google Scholar]
- Arnberg FK, Gudmundsdottir R, Butwicka A, et al. Psychiatric disorders and suicide attempts in Swedish survivors of the 2004 southeast Asia tsunami: a 5 year matched cohort study. Lancet Psychiatry. 2015;2:817–824. doi: 10.1016/S2215-0366(15)00124-8. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Kawachi I. Neighborhoods and Health. Oxford University Press; 2003. [Google Scholar]
- Christian HE, Westgarth C, Bauman A, et al. Dog ownership and physical activity: a review of the evidence. J Phys Act Health. 2013;10:750–759. doi: 10.1123/jpah.10.5.750. [DOI] [PubMed] [Google Scholar]
- Craig P, Cooper C, Gunnell D, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health. 2012;66:1182–1186. doi: 10.1136/jech-2011-200375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JR, McFarlane AC. The extent and impact of mental health problems after disaster. J Clin Psychiatry. 2006;67(2):9–14. [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Boden JM, et al. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry. 2014;71:1025–1031. doi: 10.1001/jamapsychiatry.2014.652. [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Kondo K, Shirai K, et al. Associations of childhood socioeconomic status and adulthood height with functional limitations among Japanese older people: results from the JAGES 2010 Project. J Gerontol A Biol Sci Med Sci. 2014;69:852–859. doi: 10.1093/gerona/glt189. [DOI] [PubMed] [Google Scholar]
- Hikichi H, Aida J, Tsuboya T, et al. Can Community Social Cohesion Prevent Posttraumatic Stress Disorder in the Aftermath of a Disaster? A Natural Experiment From the 2011 Tohoku Earthquake and Tsunami. Am J Epidemiol. 2016;183:902–910. doi: 10.1093/aje/kwv335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishigaki A, Higashi H, Sakamoto T, et al. The Great East-Japan Earthquake and devastating tsunami: an update and lessons from the past Great Earthquakes in Japan since 1923. Tohoku J Exp Med. 2013;229:287–299. doi: 10.1620/tjem.229.287. [DOI] [PubMed] [Google Scholar]
- Ishiki A, 1, Okinaga S, 1, Tomita N, et al. Changes in Cognitive Functions in the Elderly Living in Temporary Housing after the Great East Japan Earthquake. PLoS One. 2016 Jan 13;11(1):e0147025. doi: 10.1371/journal.pone.0147025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo K. Health Inequalities in Japan: An Empirical Study of Older People. Trans Pacific Press; 2010. [Google Scholar]
- Koyano W, Shibata H, Nakazato K, et al. Measurement of competence: reliability and validity of the TMIG Index of Competence. Arch Gerontol Geriatr. 1991;13:103–116. doi: 10.1016/0167-4943(91)90053-s. [DOI] [PubMed] [Google Scholar]
- Levine GN, Allen K, Braun LT, et al. Pet ownership and cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2013;127:2353–2363. doi: 10.1161/CIR.0b013e31829201e1. [DOI] [PubMed] [Google Scholar]
- Moon JR, Kondo N, Glymour MM, et al. Widowhood and mortality: a meta-analysis. PLoS One. 2011;6:e23465. doi: 10.1371/journal.pone.0023465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee JY, et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88:879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Santos-Eggimann B, Cuenoud P, Spagnoli J, et al. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. 2009;64:675–681. doi: 10.1093/gerona/glp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair M, O'Toole J, Malawaraarachchi M, et al. Comparison of response rates and cost-effectiveness for a community-based survey: postal, internet and telephone modes with generic or personalised recruitment approaches. BMC Med Res Methodol. 2012;12:132. doi: 10.1186/1471-2288-12-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomata Y, Kakizaki M, Suzuki Y, et al. Impact of the 2011 Great East Japan Earthquake and Tsunami on functional disability among older people: a longitudinal comparison of disability prevalence among Japanese municipalities. J Epidemiol Community Health. 2014 Jun;68(6):530–3. doi: 10.1136/jech-2013-203541. 2014. [DOI] [PubMed] [Google Scholar]
- Tomata Y, Suzuki Y, Kawado M, et al. Long-term impact of the 2011 Great East Japan Earthquake and tsunami on functional disability among older people: A 3-year longitudinal comparison of disability prevalence among Japanese municipalities. Soc Sci Med. 2015 Dec;147:296–9. doi: 10.1016/j.socscimed.2015.11.016. 2015. [DOI] [PubMed] [Google Scholar]
- Tsuboya T, Aida J, Hikichi H, et al. Predictors of depressive symptoms following the Great East Japan earthquake: A prospective study. Soc Sci Med. 2016;161:47–54. doi: 10.1016/j.socscimed.2016.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WD BJ. Explaining Rising Nonresponse Rates in Cross-Sectional Surveys. Ann Am Acad Polit Soc Sci. 2013:36–59. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Association between disaster damages and change in Instrumental Activities of Daily Living. Significant disaster damage (house, job, medical utility) were adjusted in the same model.
Supplementary Table 2. Comparison of Complete Case Analyses(N=3,547) with Multiple Imputed Dataset(N=5,048) in the Multivariable Adjusted Association of Main Disaster Damage with Change in Instrumental Activities of Daily Living (IADL) Scores among the Survivors from the Disaster in Japan.


