Abstract
Purpose
Children’s health is influenced by the context in which they live. We provide a descriptive essay on the status of children in rural America to highlight features of the rural environment that may affect health.
Description
We compiled information concerning components of the rural environment that may contribute to health outcomes. Areas addressed include the economic characteristics, provider availability, uniquely rural health risks, health services use, and health outcomes among rural children.
Assessment
Nearly 12 million children live in the rural US. Rural counties are economically disadvantaged, leading to higher rates of poverty among rural versus urban children. Rural and urban children are approximately equally likely to be insured, but Medicaid insures a higher proportion of children in rural areas. While generally similar in health, rural children are more likely to be overweight or obese than urban children. Rural parents are less likely to report that their children received preventive medical or oral health visits than urban parents. Rural children are more likely to die than their urban peers, largely due to unintentional injury.
Conclusion
Improving rural children’s health will require both increased public health surveillance and research that creates solutions appropriate for rural environments, where health care professionals may be in short supply. Most importantly, solutions must be multi-sectoral, engaging education, economic development, and other community perspectives as well as health care.
Keywords: children’s health, epidemiology, health disparities, rural, social determinants of health
Children’s health and life prospects are entwined with the context in which they develop. The descriptive essay presented below explores the rural context in America and notes some of the implications of this context for children’s health. Our perspective emerges from multiple theoretical stances, including Andersen’s behavioral model1,2 and Stokols’ social ecological approach,3 which posit that health outcomes are influenced by contextual as well as individual characteristics. Contextual factors include local demographic, economic, social, and belief structures, as well as local implementation of health policy; the availability, organization and quality of local institutions and infrastructure; and finally, environmental factors. In the sections that follow, we discuss definitions of rurality, how the rural economy affects the status of children, children’s health, risk factors in the rural environment, and health services use among rural children.i
Context: Rural Defined
“Rural” has multiple definitions, set to meet varying policy and research needs.4 Lack of uniformity hampers efforts to summarize research on rural children. When citing prior research, this essay specifies the unit at which “rural” is measured, when provided by the authors of the work cited. Whenever possible, we base our presentation on national or nationally representative data. Given the variations in rural environments across the US, however, research relevant to risks faced by rural children is often highly geographically specific.
Rurality is most often measured at the county level, since county boundaries, unlike Census tracts, ZIP Code Tabulation Areas (ZCTAs) or other small area measures, coincide with a unit of government and are relatively unchanging over time. The largest dichotomous measure is the metropolitan/nonmetropolitan definition of the Office of Management and Budget, which categorizes counties as metropolitan or urban if they contain a population cluster with more than 50,000 persons, and nonmetropolitan or rural if they do not. The term “micropolitan” is sometimes used for rural counties that contain a town with between 10,000 and 50,000 residents. Because a single urban area of more than 50,000 residents within a county leads to a metropolitan classification for all residents, county-based definitions undercount rural populations in states where counties encompass large geographic areas. For example, the Grand Canyon and most of California’s Central Valley both fall in metropolitan counties.5 Unless noted otherwise, we use the terms “large” rural and “small” rural to refer to population size and not to geographic size. Thus, large rural counties contain at least one cluster of 10,000–50,000 residents, whereas small rural counties have only clusters with fewer than 10,000 people.
Based on the nonmetropolitan county definition, rural America contained 11.8 million children ages 0 – 17 years in 2010, principally non-Hispanic white (hereafter, white 71.8%), Hispanic (11.9%), non-Hispanic black (hereafter, black 9.4%), Asian (0.9%) and “other” (6.1%).6 Reflecting changing American demographics, the absolute number of both white and black rural children declined between 2000 and 2010, while other populations increased.6
Economic Characteristics of Rural America
Rural counties are economically diverse. While nearly all farming and mining counties are nonmetropolitan (91.6% and 88.3%, respectively), these categories make up only 25.1% of all rural counties (Table 1).7 Among counties with a specialized economic base, manufacturing is the leading type for both urban and rural counties. Rural counties are over-represented in the adverse sociodemographic indicators tracked by the Economic Research Service of the US Department of Agriculture. The majority of persistent child poverty counties (82%), low employment counties (86.1%), and low education counties (80.2%) are rural.
Table 1.
County Typologies, as Defined by the US Department of Agriculture,7 by Rurality
| Rural Counties | Urban Counties | Total | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Total, all US | 1,976 | 100.0 | 1,166 | 100.0 | 3,142 | 100.0% |
| Counties, by economic type (2010 – 2012) | ||||||
| Farming-dependent (≥25% income or ≥ 16% employment) |
391 | 19.8 | 53 | 4.5 | 440 | 14.2 |
| Mining-dependent (≥13% income or ≥ 8% employment) |
183 | 9.3 | 36 | 3.1 | 128 | 7.0 |
| Manufacturing-dependent (≥23% income or ≥ 16% employment) |
351 | 17.8 | 155 | 13.3 | 905 | 16.2 |
| Federal-State Government- dependent (≥14% income or ≥ 9% employment) |
238 | 12.0 | 167 | 14.3 | 381 | 13.0 |
| Recreation (multiple criteria)a |
228 | 11.5 | 104 | 8.9 | 340 | 10.6 |
| Non-specialized (all other) | 585 | 29.6 | 651 | 55.8 | 948 | 39.6 |
|
Counties, by policy type (2008 – 2012) (not mutually exclusive) | ||||||
| Low education (≥20% of residents age 25–64 less than high school education) |
367 | 18.6 | 100 | 8.6 | 467 | 14.9 |
| Low employment (<65% of person 21–64 employed) |
720 | 36.4 | 186 | 16.0 | 906 | 28.8 |
| Persistent poverty (≥20% residents in poverty, 1980 – 2007–11) |
301 | 15.2 | 52 | 4.5 | 353 | 11.2 |
| Persistent child poverty (≥20% of children living in poverty, 1980 – 2007–11) |
558 | 28.2 | 150 | 12.9 | 708 | 22.5 |
Recreation: weighted index combining income, employment and seasonal housing.
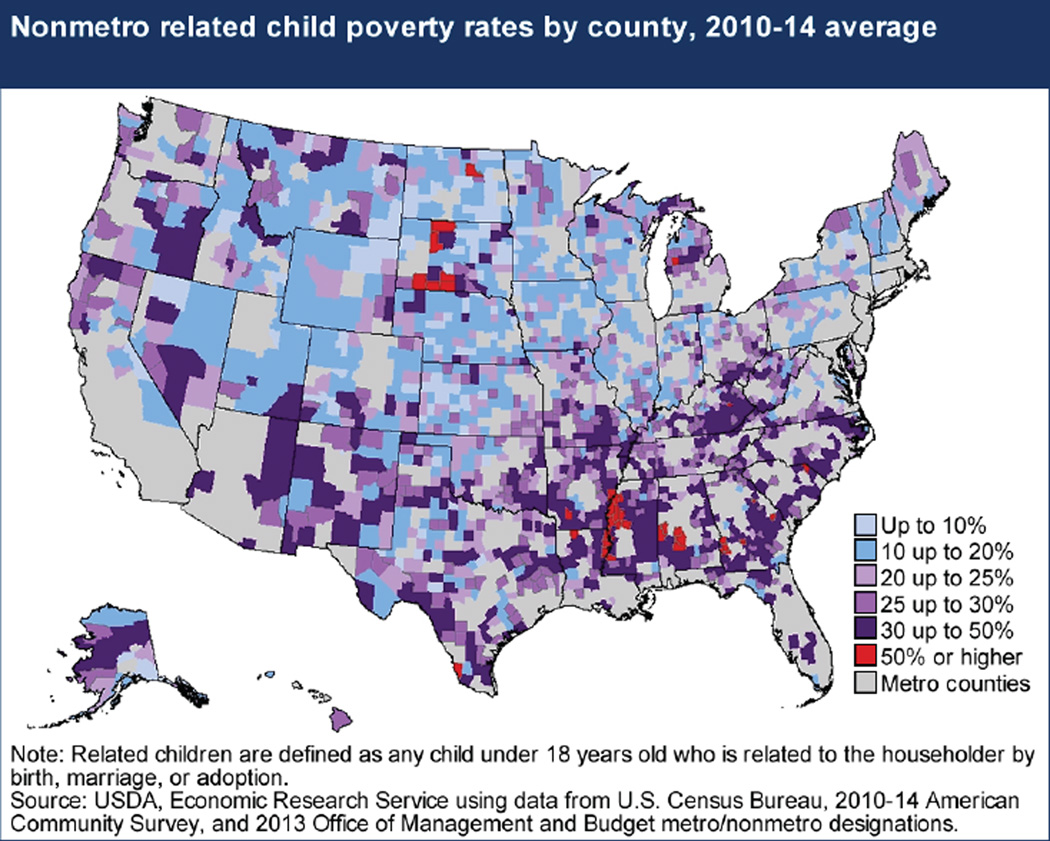
Poverty is particularly acute among rural children. Of the 100 US counties with the highest childhood poverty rates, 95 are rural counties, and 66 are counties in which white residents are in the minority.7 Measured at the county level, 25.2% of rural and 21.1% of urban children lived below the Federal Poverty Level (FPL) in 2014.8 More than half of rural African American children (51.1%) live in poverty, versus 37.2% of similar urban children; comparable values for non-Hispanic white children were 19.5% and 11.4%, respectively.8 The 2011–2012 National Survey of Children’s Health found that 41.8% of children in urban ZCTAs were low income, at or below 199% of the FPL, versus 54.0% of children in both large rural ZCTAs (areas in and around towns of 10,000 – 50,000 persons) and smaller rural ZCTAs.9 An estimated 29% of rural children are served by 1 of the 4 federal child nutrition programs (school lunch, school breakfast, Women Infants and Children and the Child and Adult Day Care Food Program).10 Persistent child poverty counties, in which the rates of children in poverty have exceeded 20% for the past 30 years, are concentrated in central Appalachia, the Deep South, the US-Mexican border, the Southwest, the Central Valley of California, and the American Indian reservations of the Northern Plains (Figure 1).
Figure 1.
Persistent Child Poverty Counties (from Farrigan8)
Rural and urban children are approximately equally likely to be insured, but from different sources: Medicaid insures a higher proportion of children in rural versus urban areas (urban ZCTAs, 34.9%, large rural ZCTAs 44.3%, small rural ZCTAs 46.8%).9 Overall, between 5.6% and 6.1% of rural children lack any insurance coverage, but this proportion markedly increases for vulnerable subgroups, reaching 22.0% uninsured among children in Hispanic households in large rural ZCTAs. Parents from rural counties are less likely than urban parents to report that their child’s insurance covers dental care.11
Provider availability is lower in rural counties, both in areas specifically designated as health professional shortage areas (HPSAs) and in general. Only 15.1% of the nation’s 2,054 rural counties are not whole or part-county HPSAs, versus 22.8% of urban counties.12 In urban non-HPSA counties, there is an average of 976 patients per physician; in urban HPSA counties, this increases to 1,590 patients for each physician. In rural, non-HSPA counties, the ratio is 1,286 persons per physician, increasing to 1,845 in rural HPSAs.13 Directly relevant to rural children, 56.6% of rural counties lack even a single pediatrician.12
Compared to urban counties, rural counties have fewer generalist dentists (22 per 100,000 persons in rural versus 30 per 100,000 in urban counties).13, 14 Suggestive of greater future disparities, 42% of rural dentists were age 56 or older, versus 38% of urban dentists.14 Ancillary health care providers, such as physical, occupational or speech therapists, mental health and substance use counselors, and medical social workers, are also in short supply in rural areas.15,16
Health Status Among Rural Children
It is difficult to build a comprehensive picture of rural child health and development from previous research. While prevalence patterns for various health conditions and associated outcomes have been described for rural children in the aggregate, information stratified by child age, gender, ethnicity, or geographic location is frequently difficult to locate or unavailable. Conversely, detailed studies of morbidity, mortality, access to and utilization of services, and treatment or service costs tend to be limited in scope. Our presentation focuses on national assessments of children’s health status, for the broadest possible picture.
Children living in rural and urban counties had similar parentally reported health status in 201017 and 2011,18 although rural children were more likely to have missed one or more days of school in the preceding year. Only a small proportion of parents responding to the 2011–2012 National Survey of Children’s Health rated their child’s overall health as less than “excellent” or “very good,” with insignificant differences across residence: 15.8% in urban ZCTAs, 15.3% in large rural ZCTAs, 15.7% in small rural ZCTAs (urban and large rural significantly different).9 The proportion of parents describing their child’s oral health as less than “excellent” or “very good” also did not differ significantly with residence, estimated at 28.2% in urban ZCTAs, 28.9% in large rural ZCTAs, and 30.2% in small rural ZCTAs.9 Despite parental perceptions of good oral health status, children in rural areas, especially children of seasonal or migrant farmworkers, experience disproportionately high rates of dental caries and other oral problems as well as low rates of utilization of dental services.19–21 The overall rate of disability, defined as vision, hearing, cognitive, ambulatory, self-care, or independent living difficulty, is higher among rural (6.3%) than among urban children (5.0%).22
Rural children are more likely to be classified as overweight (BMI greater than the 85th percentile) or obese (BMI > 95th percentile) than are urban children, even after controlling for reported dietary patterns and exercise.23–26 More than a third of rural children aged 10–17 (35.5% large rural, 38.2% small rural ZCTAs), versus 30.5% of urban children, were obese in 2011–2012.9 Food availability may play a part in geographic disparities, as rural communities are less likely to have access to grocery stores.27
Studies using the Strengths and Difficulties Questionnaire28 found no parentally reported differences between rural and urban children in the prevalence of behavioral health issues.29, 30 Similarly, analysis using the National Survey of American Families failed to find differential prevalence of mental health problems.31 On the other hand, a survey using the 2005–2006 National Survey of Children with Special Health Care needs found a slightly higher prevalence of mental health problems among rural versus urban children (5.8% and 5.3%, respectively).32
Evidence on rural disparities in behavioral health risks, such as being in a fight, experiencing dating violence, or engaging in drug use, is mixed. One study found no difference between rural and urban children in violence-related behavior, although rural teens were more likely to report tobacco use than their urban peers.33 An analysis using the 2002 through 2004 National Survey of Drug Use found rural adolescents more likely to report alcohol and cocaine use than their urban peers, with no differences across other drug types.34 Related to higher alcohol use, rural adolescents were also more likely to report binge drinking, heavy drinking and driving under the influence.33 Rural girls (ages 15–19) are more likely to report having had sex in the past 3 months (2006–2010 data).35 Birth rates per 1,000 for this age group are higher for rural teens (42.0 in micropolitan counties and 45.3/1,000 in other rural counties) than for teens in metropolitan counties (range 24.2 in fringe counties through 37.1 in small metropolitan areas).35
Of the 2.9 million rural children estimated to have behavioral problems through the Strengths and Difficulties Questionnaire, 68% lived in counties that were mental health HPSAs.29 Addressing potential sources of resilience and stress, rural children have slightly different family patterns than urban children. While 64.1% of children in urban counties lived with 2 biological parents, this decreased to 62.4% in large rural counties, 61.0% in mid-sized rural counties, and 61.8% in small rural counties.29
All cause mortality rates, adjusted for local socioeconomic deprivation, are higher among rural than among urban children, across both males and females and all major racial/ethnic categories.36 Rural residence is associated with reduced risk of death due to homicide, but increased risk of death from unintentional injury or suicide.37, 38 Further, disparities in suicide rates between urban and rural youth have increased steadily since the mid 1990s.38 Research has linked mortality rates to socioeconomic deprivation, which is disproportionately present in rural communities.
Risk Factors
The home environment for rural children presents a mixed picture. Housing quality, as ascertained through the American Housing Survey (AHS), was more likely to be classified as moderately or severely inadequate for rural than for urban children (Table 2). Rural households were also more likely to have lacked running water at least once during the preceding 3 months or to heat with a kerosene space heater. Rural children were also more likely to live in a household where one or more residents smoke cigarettes inside the home. Rural and urban households with children did not differ in 2 inexpensive childhood safety measures, use of electrical outlet covers and safe storage of chemicals and pesticides, but rural households were more likely to lack a working carbon monoxide detector. Absence of carbon monoxide detectors is problematic among rural residents, who experience disproportionately high hospital utilization39 and death40 rates due to carbon monoxide poisoning, often associated with kerosene heating. Research among rural parents has found that poverty was associated with failure to install safety devices, such as smoke detectors.41
Table 2.
Housing Characteristics and Parental Home Safety Practices in Homes With at Least One Child, American Housing Survey,69 2011
| Rural | Urban | P val | |||
|---|---|---|---|---|---|
| % | SE | % | SE | ||
| Housing quality | |||||
| Household was without running water for 6 hours or more at least once in past 3 months |
5.2 | 0.5 | 4.1 | 0.2 | .0001 |
| Reported use of kerosene space heater during winter months |
2.8 | 0.3 | 1.2 | 0.1 | < .0001 |
| No working carbon monoxide detector inside the home |
57.7 | 1.1 | 52.0 | 0.4 | < .0001 |
| Home safety practices | |||||
| A member of the household smokes inside the house |
15.3 | 0.7 | 8.7 | 0.2 | < .0010 |
| Some or all chemicals, pesticides, cleaning supplies and medicines are not stored out of the reach of young children |
18.7 | 1.1 | 19.5 | 0.5 | .7689 |
| Some or all outlets lack child tamper-resistant outlet covers |
67.7 | 1.5 | 66.9 | 0.6 | .9643 |
Source: American Housing Survey; Authors’ analysis
More positively, parental assessments suggest higher perceptions of neighborhood safety in rural areas. This was particularly true among low income families, with 77.9% of parents below the FPL in large rural areas, and 83.6% of similar parents in small rural areas, reporting that their children are always or usually safe, versus only 72.9% of poor urban parents.9 Rural parents were less likely to report violent disagreements than parents in urban counties (odds ratio 0.86; 95% confidence interval: 0.77–0.95), even after adjustment for other family characteristics.42
Uniquely Rural Injury Risk Factors
Rural children experience greater injury risk, with increasing remoteness being associated with higher risk, greater injury severity, higher treatment costs, and poorer outcomes which can include prolonged morbidity, lasting disability or death.43 Approximately 12.9% of the 2-year deficit in life expectancy between rural and urban residents is attributable to deaths under age 25.44 More troubling, the rural/urban mortality ratio among children age 1–14 has been increasing, from 1.20 in 1990–1992 to 1.41 in 2005–2009; the pattern is similar among persons aged 15–24 years.45
Rural children experience a higher risk for motor vehicle crash injury; studies regarding bicycle and pedestrian risk were less consistent.43 Rural areas frequently lack access to public transportation. Rural families travel further for services, exposing rural children to high risk for injury from motor vehicle crashes.46, 47 Firearm fatalities were similar across rural and urban children, but with different etiologies: rural children are more likely to die from suicide or unintentional injury, while urban children are more likely to experience homicide.47
Rural adolescents in small rural area ZCTAs are more likely to work outside the home than those in urban areas.9 Although farming is no longer the dominant economic activity across rural areas, it remains a large and well-studied source of youth injuries. More than 26,000 non-fatal injuries were estimated to have occurred annually among children living, working at or visiting farms during 2000–2006, with approximately 14% resulting in hospitalization and an average of 84 fatal accidents per year.48 Among all injuries, 29.3% or an estimated 7,795 injuries per year, occurred while the youth was working.48 While most working injuries involved youth aged 15–19, work injuries occurred among children as young as 5–9 years of age.48
Within children living on farms, injury was more likely when the child performed agricultural work, carried out chores recommended for older children, and worked close to a full-time work week.49 Rural youth may drive tractors that lack rollover protective structures or work with power take off shafts (exposed rotating devices linked to additional equipment), and they experience exposure to dust and noise.50, 51 Children do not have to be engaged in agricultural work to be exposed, as children who play near or during farm operations can also be injured, with the rate of such injuries being highest among children younger than 5 years.52 Within minority farm children, American Indian children were more likely than others to be injured, with an estimated injury rate of 7.86 per 1000, compared to 5.15/1000 among black children and 5.5 among Hispanic youth.53
Pesticide exposure, with uncertain long-term effects,54 is more common among children in agricultural families, and particularly among children of farm workers.55 While farm workers recognize the importance of protecting their children’s health and most avoid holding young children while wearing work clothes, many do not employ other practices to reduce contamination, such as washing hands after work or removing shoes/boots on entering the home.56 Fears of pesticide or chemical contamination frequently lead farm working families, especially Hispanics, to purchase and use bottled water for domestic purposes rather than consume cheaper water from wells or town municipal supplies.57, 58
Health Services Use Among Rural Children
While rural and urban children have similar health status, health care use differs. Rural parents are less likely than urban parents to report that their child had a preventive health care visit or a preventive dental care visit.9 Lower use of preventive care may translate into higher use of inappropriate services, such as emergency department visits for conditions that could be managed in primary care settings, including dental caries and complex chronic diseases. For example, among children with asthma, residence in a rural areas was associated with increased emergency department visits (adjusted rate ratio compared to urban, 1.25, CI: 1.19–1.33, P < .001).59
The prevalence of behavioral health problems among rural children has been found to be similar29–31 or to be only slightly higher32 than among their urban peers. However, research has found lower utilization of behavioral health services among rural children. An analysis of children with attention deficit hyperactivity disorder found that the odds of a visit to a mental health professional were 2.17 higher among urban than rural youth.60 Among youth with psychiatric diagnoses visiting hospital emergency departments, rural residence and lack of health insurance were both associated with hospitalization after controlling for clinical need, suggesting the lack of effective outpatient treatment.61
Looking Forward and Recommendations
Rural children live in an environment characterized by economic deprivation and adverse long-term trends. These trends include demographic changes in the rural population, anticipated declines in provider availability, and the poor prospects for those rural settings in greatest need, the “persistent poverty” counties. Countering these adverse trends, increasing financial access to care through the Affordable Care Act and innovative approaches to maximize the effectiveness of health care providers already in place may bolster outcomes for young rural residents.
By extending health insurance coverage more broadly across rural children and adults, the Affordable Care Act may serve to make medical, dental, rehabilitative, mental or behavioral health practice economically feasible in more rural communities. However, even with more families fully covered by health insurance, some rural counties may not be able to attract new providers. Counties that lack broad economic resources or natural amenities such as lakes or mountains are less likely to grow through in-migration.62 The problems of maintaining an adequate infrastructure for children and of retaining health care providers may be particularly acute among the nation’s “persistent child poverty” rural counties. Despite federal efforts to spur economic development, these regions have not made meaningful economic progress in decades.
What can be done to address problems experienced by rural children? First, improved surveillance is needed. Problems cannot be defined nor effective policy solutions documented without adequate information. At present, very little information about the health and behavior of rural children is provided in a form that allows assessment of rural/urban differences. For example, the CDC-published reports summarizing findings from the Youth Risk Behavior Surveillance survey, the most comprehensive assessment of youth behavior available, do not separately address rural children and their needs.63 Within the constraints needed for data privacy, research and information dissemination need to switch from a solely individualistic perspective to include a contextual focus. Increasing attention must be given to the social determinants of health at the community level, including residence, when reporting on childhood outcomes. The role of the environment in promoting healthy behaviors (exercise, purchase of nutritious food) and in facilitating or impairing access to care deserves recognition.
Second, information is needed about approaches that improve health in all stages of childhood—newborns, toddlers, school age and adolescents—in rural areas. Research suggests that the traditional approaches to service provision, which assume provider availability, may fail in rural locales. Public health may serve a different role in under-resourced rural communities, one in which the assurance function is more prominent. A longitudinal study of the transfer of Early Periodic Screening Diagnosis and Treatment services from the public health agency to private medical providers in a southern state found that urban counties were more likely to be successful in this transition, while rural children fell behind.64 In rural settings, non-traditional providers and cross-disciplinary approaches may be key. School health clinics, for example, may be more important in rural than urban settings;65 successful program elements should be identified and disseminated. Cross-disciplinary approaches to services may also have greater effects for rural children. An evaluation of Wisconsin Medicaid claims found that a policy change allowing fluoride varnish, a dental caries preventative, to be applied by medical practitioners was associated with a greater increase in claims in rural than in urban counties.66
Emerging technologies, from mobile vans through telehealth and other electronic mechanisms, also offer promise of improving access to care for rural children. At present, however, availability of telemedicine remains low. As of 2013, only about a third of rural hospitals (34.0%) had any telemedicine applications in place; of those, only 2.5% focused on pediatric or obstetric populations.67 Even successful projects are hampered by a lack of consistent funding models,68 suggesting that telemedicine has not yet been integrated into routine care. Given the long horizon for technological solutions, communities will need to continue to focus on innovative ways for recruiting clinicians to serve rural children.
Finally, while surveillance and research are needed, action is needed even more urgently. Childhood is brief. Communities of practice that do not typically engage one another, such as education and economic development and public health and the health care sector, need to develop modes of working cooperatively to improve the determinants of health and health outcomes. A collaborative, “no silos” commitment to rural children is essential.
Acknowledgments
Disclosures: This manuscript was reviewed in draft by 2 anonymous NICHD staffers. NICHD provided no funding for manuscript development and had no input into the conclusions of the authors.
Funding: The rural health research conducted by the first author (Probst) is funded in part by grant no. U1CRH03711 from the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration, U.S. Department of Health and Human Services. The National Institute of Dental and Craniofacial Research (NIDCR), through grant U54DE019285 to the Center to Address Disparities in Children’s Oral Health (known as CANDO) at the University of California San Francisco, partly supported Barker’s (second author’s) participation in the 2011 conference. Neither FORHP nor NIDCR had any input into the creation of this manuscript or interpretation of its results.
The authors would like to thank Ashley Robertson, JD, PhD for her contributions to the analysis of the American Housing Survey data pertaining to rural families.
Footnotes
Some materials in this paper were presented at a conference convened by the National Institute of Child Health and Human Development (NICHD), “Health Outcomes among Children and Families Living in Rural Communities,” held December 1–2, 2011.
Any differences noted between rural and urban children were statistically significant in the source document from which the information was drawn; other observations are characterized as “similar.”
References
- 1.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 2.Andersen RM. National health surveys and the behavioral model of health services use. Medical Care. 2008;46(7):647–653. doi: 10.1097/MLR.0b013e31817a835d. [DOI] [PubMed] [Google Scholar]
- 3.Stokols D. Translating social ecological theory into guidelines for community health promotion. American Journal of Health Promotion. 1996;10(4):282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 4.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. American Journal of Public Health. 2005;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Enders A. Presented at the Health Outcomes Among Children & Families Living in Rural Communities Conference. Bethesda, MD: Eunice Kennedy Shriver National Institute of Child Health and Human Development; 2011. Dec, Inclusion of Families of Children with Disabilities in Health Services Research. [Google Scholar]
- 6.Murdock S. Population growth and diversification in rural and urban America: implications for health, education, the labor force and economic development. Presented at the National Rural Health Association Annual Conference; December 2011; Orlando FL. [Google Scholar]
- 7.Parker T. Updated ERS County Economic Types Show a Changing Rural Landscape. [Accessed March 31, 2016];Economic Research Service, US Department of Agriculture. 2015 Available at: http://www.ers.usda.gov/amber-waves/2015-december/updated-ers-county-economic-types-show-a-changing-rural-landscape.aspx/
- 8.Farrigan T. Child poverty. [Accessed March 31, 2016];Economic Research Service, US Department of Agriculture. 2015 Available at: http://ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/child-poverty.aspx.
- 9.U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. The Health and Well-Being of Children in Rural Areas: A Portrait of the Nation, 2011–2012. Rockville, MD: U.S. Department of Health and Human Services; 2015. [Google Scholar]
- 10.Wauchope B, Shattuck A. Federal Child Nutrition Programs are Important to Rural Households, Issue Brief No. 11. Durham, NH: Carsey Institute, University of New Hampshire; 2010. [Google Scholar]
- 11.Liu J, Probst JC, Martin AB, Wang JY, Moore CG, Salinas CF. Disparities in dental insurance coverage and dental care among US children. Pediatrics. 2007;119(Suppl 1):S12–S21. doi: 10.1542/peds.2006-2089D. [DOI] [PubMed] [Google Scholar]
- 12.US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions. Rockville (MD): Authors’ analysis. Data source: Area Resource File (ARF). [Internet]. 2011–2012. [Google Scholar]
- 13.Doescher MP, Keppel GA, Skillman SM, Rosenblatt RA. The Crisis in Rural Dentistry. Seattle, Washington: WWAMI Rural Health Research Center; 2009. [Accessed March 31, 2016]. Available from: http://depts.washington.edu/uwrhrc/uploads/Rural_Dentists_PB_2009.pdf/ [Google Scholar]
- 14.Mertz E, Mouradian W. Addressing Children’s Oral Health in the New Millennium: Trends in the Dental Workforce. Academic Pediatrics: Special issue on Children’s Oral Health. 2009;9(6):433–439. doi: 10.1016/j.acap.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roots RK, Li LC. Recruitment and retention of occupational therapists and physiotherapists in rural regions: a meta-synthesis. BMC Health Services Research. 2013;13:59. doi: 10.1186/1472-6963-13-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniels ZM, Vanleit BJ, Skipper BJ, Sanders ML, Rhyne RL. Factors in recruiting and retaining health professionals for rural practice. Journal of Rural Health. 2007;23(1):62–71. doi: 10.1111/j.1748-0361.2006.00069.x. [DOI] [PubMed] [Google Scholar]
- 17.Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2010. Washington (DC): National Center for Health Statistics (US); 2011. Series No:10. Report No: 250. [PubMed] [Google Scholar]
- 18.Bloom B, Cohen RA, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey 2011. Washington (DC): National Center for Health Statistics; 2012. Series No:10. Report No:254. [PubMed] [Google Scholar]
- 19.Barnes GP, Parker WA, Lyon TC, Jr, Drum MA, Coleman GC. Ethnicity, location, age, and fluoridation factors in baby bottle tooth decay and caries prevalence of Head Start children. Public Health Reports. 1992;107(2):155–159. [PMC free article] [PubMed] [Google Scholar]
- 20.Quandt SA, Clark HM, Rao P, Arcury TA. Oral health of children and adults in Latino migrant and seasonal farmworker families. Journal of Immigrant and Minority Health. 2007;9(3):229–235. doi: 10.1007/s10903-006-9033-7. [DOI] [PubMed] [Google Scholar]
- 21.Vargas CM, Ronzi CR, Hayes KL. Oral health status of children and adolescents by rural residence, United States. Journal of Rural Health. 2003;19(3):260–268. doi: 10.1111/j.1748-0361.2003.tb00572.x. [DOI] [PubMed] [Google Scholar]
- 22.Brault MW. School-Age children with disability in U.S. Metropolitan Statistical Areas: 2010. [Accessed March 30, 2016];American Community Survey Brief. [Internet] 2011 Available at http://www.census.gov/prod/2011pubs/acsbr10-12.pdf.
- 23.Liu JH, Jones SJ, Sun H, Probst JC, Merchant AT, Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: an urban and rural comparison. Childhood Obesity. 2012;8(5):440–448. doi: 10.1089/chi.2012.0090. [DOI] [PubMed] [Google Scholar]
- 24.Lutfiyya MN, Lipsky MS. Is rural residency a risk factor for overweight and obesity for U.S. children? Obesity. 2007;15(9):2348–2356. doi: 10.1038/oby.2007.278. [DOI] [PubMed] [Google Scholar]
- 25.Davis AM, Bennett KJ, Befort C, Nollen N. Obesity and related health behaviors among urban and rural children in the United States: Data from the National Health and Nutrition Examination Survey 2003–2004 and 2005–2006. Journal of Pediatric Psychology. 2011;36(6):669–676. doi: 10.1093/jpepsy/jsq117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kenney MK, Wang J, Iannotti R. Residency and racial/ethnic differences in weight status and lifestyle behaviors among US youth. Journal of Rural Health. 2014;30(1):89–100. doi: 10.1111/jrh.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 28.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Moore CG, Mink M, Probst JC, Tompkins M, Johnson A, Hughley S. Mental Health Risk Factors, Unmet Needs, and Provider Availability for Rural Children. [Internet]. 2005. [Accessed February 15, 2016];2005 Available from http://rhr.sph.sc.edu. [Google Scholar]
- 30.Cuffe SP, Moore CG, McKeown RE. Prevalence and correlates of ADHD symptoms in the National Health Interview Survey. Journal of Attention Disorders. 2005;9(2):392–401. doi: 10.1177/1087054705280413. [DOI] [PubMed] [Google Scholar]
- 31.Howell E, McFeeters J. Children's mental health care: differences by race/ethnicity in urban/rural areas. Journal of Health Care for the Poor and Underserved. 2008;19(1):237–247. doi: 10.1353/hpu.2008.0008. [DOI] [PubMed] [Google Scholar]
- 32.Lenardson JD, Ziller EC, Lambert D, Race MM, Yousefian A. Access to Mental Health Services and Family Impact of Rural Children with Mental Health Problems. Maine Rural Health Research Center Working Paper #45; University of Southern Maine; 2010; Portland, ME. [Google Scholar]
- 33.Johnson AO, Mink MD, Harun N, Moore CG, Martin AB, Bennett KJ. Violence and drug use in rural teens: national prevalence estimates from the 2003 Youth Risk Behavior Survey. Journal of School Health. 2008;78(10):554–561. doi: 10.1111/j.1746-1561.2008.00343.x. [DOI] [PubMed] [Google Scholar]
- 34.Lambert D, Gale JA, Hartley D. Substance abuse by youth and young adults in rural AmericA. Journal of Rural Health. 2008;24(3):221–228. doi: 10.1111/j.1748-0361.2008.00162.x. [DOI] [PubMed] [Google Scholar]
- 35.Ng AS, Kaye K. Sex in the (Non) City :Teen Childbearing in Rural America. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy; 2015. [Google Scholar]
- 36.Singh GK, Azuine RE, Siahpush M, Kogan MD. All-cause and cause-specific mortality among US youth: socioeconomic and rural-urban disparities and international patterns. Journal of Urban Health. 2013;90(3):388–405. doi: 10.1007/s11524-012-9744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nance ML, Carr BG, Kallan MJ, Branas CC, Wieb DJ. Variation in pediatric and adolescent firearm mortality rates in rural and urban US counties. Pediatrics. 2010;125(6):1112–1118. doi: 10.1542/peds.2009-3219. [DOI] [PubMed] [Google Scholar]
- 38.Fontanella CA, Hiance-Steelesmith DL, Phillips GS, Bridge JA, Lester N, Sweeney HA, Campo JV. Widening rural-urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatrics. 2015;169(5):466–473. doi: 10.1001/jamapediatrics.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. American Journal of Emergency Medicine. 2012;30(5):657–664. doi: 10.1016/j.ajem.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 39.Hnatov MV. Non-Fire Carbon Monoxide Deaths Associated with the Use of Consumer Products 2009 Annual Estimates. Bethesda (MD): US Consumer Product Safety Commission; 2012. [Google Scholar]
- 40.Zolotor AJ, Burchinal M, Skinner D, Rosenthal M. Maternal psychological adjustment and knowledge of infant development as predictors of home safety practices in rural low-income communities. Pediatrics. 2008;121(6):e1668–e1675. doi: 10.1542/peds.2007-1255. [DOI] [PubMed] [Google Scholar]
- 41.Moore CG, Probst JC, Tompkins M, Cuffe S, Martin AB. The Prevalence of Violent Disagreements in US Families: Effects of Residence, Race-Ethnicity and Parental Stress. Pediatrics. 2007;119(Suppl 1):S68–S76. doi: 10.1542/peds.2006-2089K. [DOI] [PubMed] [Google Scholar]
- 42.Kim K, Ozegovic D, Voaklander DC. Differences in incidence of injury between rural and urban children in Canada and the USA: a systematic review. Injury Prevention. 2012;18(4):264–271. doi: 10.1136/injuryprev-2011-040306. [DOI] [PubMed] [Google Scholar]
- 43.Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S, 1969–2009. American Journal of Preventive Medicine. 2014;46(2):e19–e29. doi: 10.1016/j.amepre.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 44.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. Journal of Urban Health. 2014;91(2):272–292. doi: 10.1007/s11524-013-9847-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Children: 2014 data (Traffic Safety Facts. Report No. DOT HS 812 271) Washington, DC: National Highway Traffic Safety Administration; 2016. National Center for Statistics and Analysis. [Google Scholar]
- 46.National Highway Traffic Safety Administration. Traffic Crashes Take Their Toll On America’s Rural Roads. [Internet]. Publication No. DOT HS 810 658. [Accessed January 27, 2016];2006 Available at www.nhtsAdoTgov.
- 47.Zaloshnja E, Miller TR, Lawrence B. Incidence and cost of injury among youth in agricultural settings, United States, 2001–2006. Pediatrics. 2012;129(4):728–734. doi: 10.1542/peds.2011-2512. [DOI] [PubMed] [Google Scholar]
- 48.Larson-Bright M, Gerberich SG, Alexander BH, Gurney JG, Masten AS, Church TR, et al. Work practices and childhood agricultural injury. Injury Prevention. 2007;13(6):409–415. doi: 10.1136/ip.2006.014233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reed DB, Browning SR, Westneat SC, Kidd PS. Personal protective equipment use and safety behaviors among farm adolescents: gender differences and predictors of work practices. Journal of Rural Health. 2006;22(4):314–320. doi: 10.1111/j.1748-0361.2006.00052.x. [DOI] [PubMed] [Google Scholar]
- 50.Humann M, Sanderson W, Flamme G, Kelly KM, Moore G, Stromquist A, et al. Noise exposures of rural adolescents. Journal of Rural Health. 2011;27(1):72–80. doi: 10.1111/j.1748-0361.2010.00306.x. [DOI] [PubMed] [Google Scholar]
- 51.Williams QL, Jr, Alexander BH, Gerberich SG, Nachreiner NM, Church TR, Ryan A. Bystander injury evaluation of children from Midwestern agricultural operations. Journal of Safety Research. 2010;41(1):31–37. doi: 10.1016/j.jsr.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 52.Helitzer DL, Gilmore K, Benally J. Children's safety on American Indian farms: information and recommendations. Journal of Agromedicine. 2012;17(2):251–258. doi: 10.1080/1059924X.2012.658011. [DOI] [PubMed] [Google Scholar]
- 53.Jurewicz J, Hanke W, Johansson C, Lundqvist C, Ceccatelli S, van den Hazel P, et al. Adverse health effects of children’s exposure to pesticides: what do we really know and what can be done about it. Acta Paediatrica. 2006;95(453):71–80. doi: 10.1080/08035320600886489. [DOI] [PubMed] [Google Scholar]
- 54.Dilworth-Bart JE, Moore CF. Mercy mercy me: social injustice and the prevention of environmental pollutant exposures among ethnic minority and poor children. Child Development. 2006;77(2):247–265. doi: 10.1111/j.1467-8624.2006.00868.x. [DOI] [PubMed] [Google Scholar]
- 55.Strong LL, Thompson B, Koepsell TD, Meischke H. Factors associated with pesticide safety practices in farmworkers. American Journal of Industrial Medicine. 2008;51(1):69–81. doi: 10.1002/ajim.20519. [DOI] [PubMed] [Google Scholar]
- 56.Scherzer T, Barker JC, Pollick H, Weintraub JA. Water consumption beliefs and practices in a rural Latino community: Implications for fluoridation. Journal of Public Health Dentistry. 2010;70:337–343. doi: 10.1111/j.1752-7325.2010.00193.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Van Derslice J. Drinking water infrastructure and environmental disparities: Evidence and methodological considerations. American Journal of Public Health. 2011;101:51, S109–S114. doi: 10.2105/AJPH.2011.300189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Diedhiou A, Probst JC, Hardin JW, Martin AB, Xirasagar S. Relationship between presence of a reported medical home and emergency department use among children with asthma. Medical Care Research and Review. 2010;67(4):450–475. doi: 10.1177/1077558710367735. [DOI] [PubMed] [Google Scholar]
- 60.Cuffe SP, Moore CG, McKeown RE. ADHD and health services utilization in the National Health Interview Survey. Journal of Attention Disorders. 2009;12(4):330–340. doi: 10.1177/1087054708323248. [DOI] [PubMed] [Google Scholar]
- 61.Huffman LC, Wang NE, Saynina O, Wren FJ, Wise PH, Horwitz SM. Predictors of hospitalization after an emergency department visit for California youths with psychiatric disorders. Psychiatric Services. 2012;63(9):896–905. doi: 10.1176/appi.ps.201000482. [DOI] [PubMed] [Google Scholar]
- 62.Cromartie J. Shifting Geography of Population Change. [Accessed June 29, 2016];2016 Available at http://www.ers.usdAgov/topics/rural-economy-population/population-migration/shifting-geography-of-population-change.aspx.
- 63.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, et al. Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance - United States, 2011. Morbidity and Mortality Weekly Report. 2012;61(4):1–162. [PubMed] [Google Scholar]
- 64.Hale NL, Smith M, Hardi J, Brock-Martin A. Rural Populations and Early Periodic Screening, Diagnosis, and Treatment Services: Challenges and Opportunities for Local Public Health Departments. American Journal of Public Health. 2015;105(Suppl 2):S330–S336. doi: 10.2105/AJPH.2014.302449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Reports. 2008;123(6):739–750. doi: 10.1177/003335490812300610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Okunseri C, Szabo A, Garcia RI, Jackson S, Pajewski NM. Provision of fluoride varnish treatment by medical and dental care providers: variation by race/ethnicity and levels of urban influence. Journal of Public Health Dentistry. 2010;70(3):211–219. doi: 10.1111/j.1752-7325.2010.00168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lower CL, Bronstein JM, Benton TL, Fletcher DA. Distributing medical expertise:the evolution and impact of telemedicine in Arkansas. Health Affairs (Millwood) 2014;33(2):235–243. doi: 10.1377/hlthaff.2013.1001. Erratum in:Health Affairs (Millwood). 2015;34(1):189. [DOI] [PubMed] [Google Scholar]
- 68.Ward MM, Ullrich F, Mueller K. Extent of telehealth use in rural and urban hospitals. Rural Policy Brief. 2014;(2014 4):1–4. [PubMed] [Google Scholar]
- 69.American Housing Survey. [Internet]. U.S. Department of Commerce:United States Census Bureau. [] [Accessed April 10, 2013];2011 Available from: http://www.census.gov/housing/ahs/