Abstract
Background
While colonoscopy with polypectomy can prevent up to 80% of colorectal cancers, a significant adenoma miss rate still exists, particularly in the right colon. Previous studies addressing right colon retroflexion have revealed discordant evidence regarding the benefit of this maneuver on adenoma detection with concomitant concerns about safety and rates of maneuver success. In this meta-analysis, we sought to determine the effect of right colon retroflexion on improving adenoma detection compared with conventional colonoscopy without retroflexion, as well as determine the rates of retroflexion maneuver success and adverse events.
Methods
Multiple databases including MEDLINE, Embase, and Web of Science were searched for studies on right colon retroflexion and its impact on adenoma detection compared with conventional colonoscopy. Pooled analyses of adenoma detection and retroflexion success were based on mixed-effects and random-effects models with heterogeneity analyses.
Results
Eight studies met the inclusion criteria (N = 3660). The primary analysis comparing colonoscopy with right-sided retroflexion vs. conventional colonoscopy to determine the per-adenoma miss rate in the right colon was 16.9% [95% CI, 12.5-22.5%]. The overall rate of successful retroflexion was 91.9% [95% CI, 86-95%] and rate of adverse events was 0.03%.
Conclusions
Colonoscopy with right-sided retroflexion significantly increases the detection of adenomas in the right colon compared with conventional colonoscopy with a high rate of maneuver success and small risk of adverse events. Thus, reexamination of the right colon in retroflexed view should be strongly considered in future standard of care colonoscopy guidelines for quality improvement in colon cancer prevention.
Introduction
Colonoscopy is currently considered the gold standard test in screening for colorectal cancer.1 Detection and removal of precancerous polyps such as adenomas has been shown to reduce mortality from colorectal cancer.2, 3 Additionally, adenoma detection rate (ADR) has been shown to be inversely associated with the risk of interval colorectal cancer and mortality and thus is increasingly targeted as a core quality indicator in colonoscopy.4-6 However, colonoscopy remains imperfect and evidence indicates that the overall miss rate for adenomatous polyps approximates 20%.7 Failure to detect such adenomas is one of the proposed mechanisms in the development of interval colorectal cancers that occur in the screened population.8 Additionally, recent studies have demonstrated that colonoscopy is less effective in preventing right-sided compared with left-sided colon cancer.9-11 Possible explanations for this discrepancy include differences in tumor biology and polyp morphology with right-sided lesions having faster growth rates and flatter polyp profiles making them harder to identify endoscopically.12 As a result, research has focused on advancing colonoscopy technology to improve visualization and adenoma detection with wide-angle colonoscopy, third eye retroscope, full spectrum endoscopy, and cap-fitted colonoscopy.13-16
Retroflexion of the colonoscope is a technique that has been suggested to improve visualization in the right colon, and refers to making a U-turn with the bending section of the colonoscope so that the viewing lens is looking backward.17 In theory, this technique could allow for improved visibility of the backs of the haustral folds and the inner curvature of the hepatic flexure leading to increase detection of adenomas that were missed during conventional forward view withdrawal.
Over the last decade, multiple studies have examined the utility, maneuver success, and adverse event rates of retroflexion in the right colon.18-29 However, controversy remains over whether or not right colon retroflexion leads to significantly improved adenoma detection in the context of concerns about procedural safety and retroflexion maneuver success. Therefore, right colon retroflexion has not yet become a standard of care quality indicator for colonoscopy. Previous work evaluating the benefit of right colon retroflexion upon adenoma detection compared with conventional colonoscopy has been discordant showing per-adenoma miss rates as low as 4.7% 18 and as high as 33.3%.28 Therefore we conducted a systematic review and meta-analysis to determine the effect of retroflexion in the right colon during colonoscopy on adenoma detection compared with conventional colonoscopy (primary aim) as well as to determine the rate of retroflexion maneuver success and the rate of adverse events (secondary aims).
Methods
The PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) statement and guidelines were consulted during the stages of design, analysis, and reporting of this meta-analysis.30 The search strategy, study inclusion and exclusion criteria, primary and secondary outcomes, and analyses were defined on an a priori basis and are described in this section. Institutional review board approval was not required for this study as per meta-analysis guidelines whereby no individual patient data is analyzed.
Literature search
A comprehensive literature search was performed in August 2015 using the PubMed/Medline, Embase, Web of Science, Cochrane databases and Google Scholar. Main search terms included both MeSH and non-MeSH terms related to the colonoscopic technique of retroflexion linked with multiple anatomical descriptors as well as colonic polyps or adenomas. The search strategy, shown in Supplementary Table 1, was engineered by two authors (J.C. and D.G.) with the assistance of a Harvard University medical librarian. Abstracts from major conferences (Digestive Disease Week (DDW) and American College of Gastroenterology (ACG) national meetings were also searched. References from the retrieved sources were manually reviewed for any additional articles. We communicated with corresponding authors of any studies that required clarification of the data.
After elimination of duplicate references, we reviewed the title and abstract of the remaining articles. Articles were removed if they did not meet the pre-specified inclusion criteria: human patients >18 years of age, pertained to colonic retroflexion, and were of a cohort, case-control, or randomized controlled trial (RCT) study design. Exclusion criteria included studies with pediatric patients, studies where histology was unavailable, outcomes of interest not fully assessed, review articles, and preliminary data captured elsewhere. All of the studies were available in English. We then performed a full article review of the remaining studies.
Data extraction
Data of interest was extracted by two independent reviewers (J.C. and D.G.). Any disagreements were evaluated and settled by consensus or a third party (L.G.). The primary outcome measure was based on the success of the retroflexion technique in identifying missed adenomas in the right colon. In all included studies, we determined the number of right-sided adenomas detected during standard colonoscopy and the number of ‘missed’ adenomas that were detected in retroflexion following the conventional forward-viewing withdrawal. Two RCT studies compared the number of polyps detected by retroflexion technique versus a second forward view and thus only the retroflexed cohort of these studies were included 19, 25. All other observational studies, however, only looked at a single forward view which is the conventional standard followed by retroflexion. Therefore, in order to eliminate this important study design heterogeneity, only data from the single arm of the RCTs which pertained to retroflexion was included in this analysis.
Outcome measures
The primary outcome measure was defined in two ways. First, we wanted to determine a more precise estimate for the right-sided adenoma miss rate. This proportion required knowledge of the total number of adenomas detected in the right colon on standard view and the total number of additional adenomas detected during retroflexion. Thus, we calculated as the primary metameter of per-adenoma miss rate of the right colon as the number of additional adenomas in right colon detected by retroflexed view divided by the total adenomas in right colon detected with conventional plus retroflexed view. This miss rate definition is the standard terminology used in many colonoscopy quality-measure studies.23 Second, we determined the per-colonoscopy adenoma miss rate of the right colon by determining the number of additional adenomas in right colon detected by retroflexed view divided by the number of total colonoscopies performed in each study.
Our secondary outcomes evaluated the success rate of the retroflexion technique as well as adverse event rates.
Study quality
The QUADAS-2 and Newcastle-Ottawa Scale are two validated measures for assessing the quality of observational studies, however, they were not directly applicable to our intervention given the pre-post comparisons within the studies. Therefore, we modified the scoring system using the framework provided from a previous gastroenterology meta-analysis which also evaluated adenoma detection (Supplemental Figure 1).31 Out of a possible 8 points, high quality studies were defined as attaining a score of 7 or higher. Low quality studies scored less than 7. If the quality indicator was not well defined, then no points were given for that indicator (Supplemental Table 2).
Statistical analysis
The primary outcome measure was the right colon per-adenoma miss rate which has been validated in previous studies evaluating colonoscopy retroflexion.23 Each study had a standard error inversely proportional to the square root of the sample size. The second primary outcome measure was the per-colonoscopy adenoma miss rate in the right colon. Pooling of each study's estimate yielded the summary statistics. Heterogeneity was determined using the I2 statistic. Where significant inter-study heterogeneity existed (P<0.05 for no heterogeneity), the analysis was performed using the random effects model. A priori sensitivity analysis was performed by stratifying the studies into both high and low quality. In addition, a pre-specified meta-regression controlling for the total adenoma rate in each study was applied to the per-colonoscopy adenoma miss rate in the right colon. This was done to evaluate whether the prevalence of adenomas (affected by population biology, indication for colonoscopy and/or ability of an endoscopist to detect adenomas during standard forward withdrawal) was correlated with the rate of adenomas during retroflexion.
Publication bias was assessed by visual inspection of a funnel plot. No statistical test of funnel plot asymmetry was used because of the low power to detect a difference between chance and true asymmetry when < 10 studies are included in a meta-analysis.32 Comprehensive Meta-Analysis Version 3.0 software (Englewood, NJ, USA) was used for all statistical analysis and image production.
Results
Search results
The initial search strategy yielded 85 studies from PubMed and 118 studies from Embase. A review of the other databases revealed only a small number of duplicate entries. Out of 138 non-duplicate articles, 119 were removed because they did not meet the pre-specified inclusion criteria. Of the remaining 19 studies, 11 were excluded for the following reasons: contained preliminary data found elsewhere (2), were clinical reviews (3), did not quantify the outcomes of interest (3), or did not contain histologic confirmation of adenomas (3). At the end of study selection, 8 studies remained that contained information meeting the PICO (population, intervention, comparison, outcome) framework (Figure 1). The funnel plot appeared symmetric (Figure 2) without gross acknowledgement of missing studies. As stated in the methods, we did not perform a statistical analysis for asymmetry given that we had less than 10 studies in the final analysis.
Figure 1. Flow diagram of study selection for systematic review and meta-analysis.
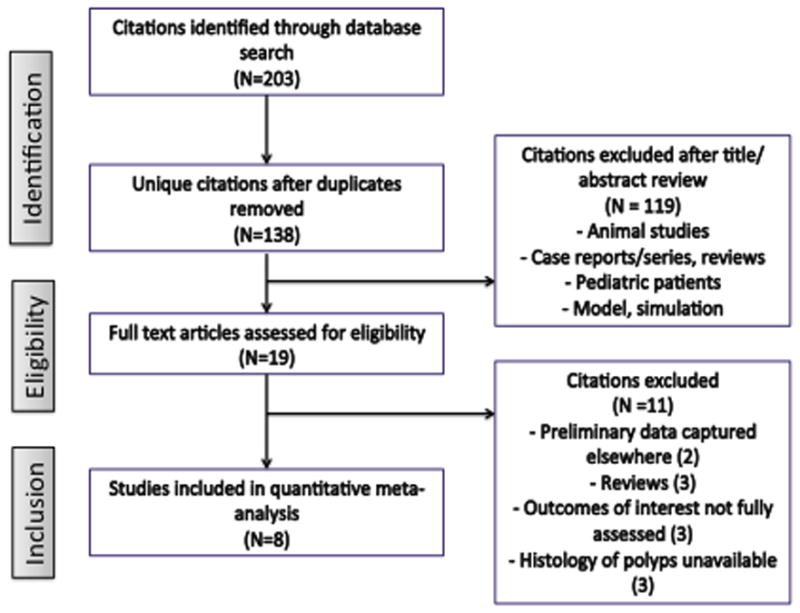
Figure 2. Funnel plot of studies included in the meta-analysis demonstrating no publication bias.
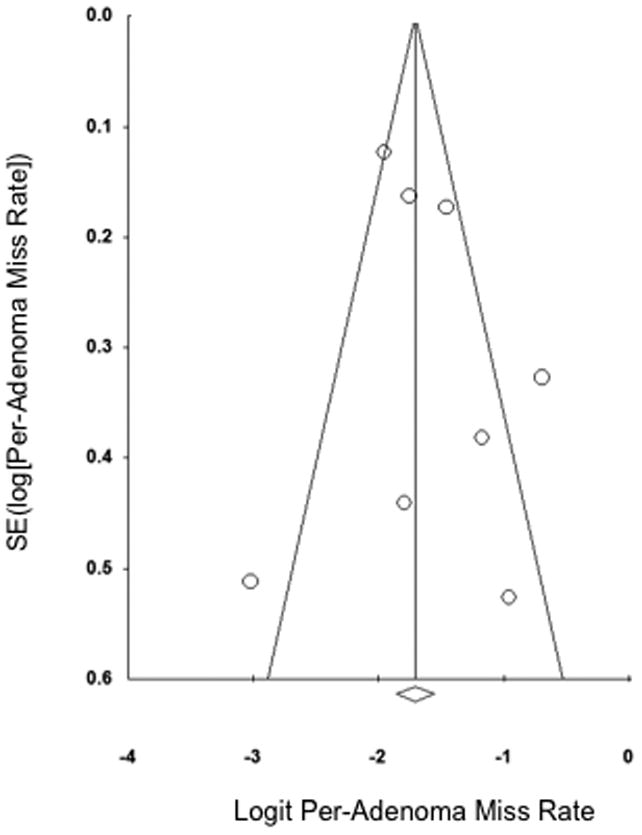
Table 1 shows an analysis of our included studies. Most studies were prospective and performed in the United States. Four studies only included subjects undergoing screening or surveillance colonoscopies.18, 22, 23, 25 The total number of colonoscopies performed in the 8 studies was 3,660. Retroflexion was attempted in each procedure and the success rate ranged from 77-100%. There was only one serious adverse event (perforation) reported out of all procedures. The determination of study quality is shown in Supplemental Table 2.
Table 1. Characteristics of studies included in the meta-analysis.
| Author, year |
Location | Study design | Study population | Total Procedures |
Age (mean) | Male N (%) |
Successful retroflexion N (%) |
Right-sided adenomas detected (conventional) |
Additional right-sided adenomas detected (retroflexion) |
Complications N (%) |
Qualitya |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aadam, 2013 | USA | Prospective | Screening/surveillance | 134 | Not given | Not given | 126 (94) | 82 | 4 | 0 (0) | High |
| Baumann, 2009 | Switzerland | Prospective | Any colonoscopy | 200 | 58 | 94 (47) | 178 (89) | 13 | 5 | 0 (0) | Low |
| Chandran, 2015 | Australia | Prospective | Any colonoscopy | 1351 | 60 | 685 (51) | 1295 (96) | 531 | 75 | 0 (0) | High |
| Gaddam, 2012 | USA | Retrospective | Screening/surveillance | 172 | 59 | 80 (47) | 148 (86) | 36 | 6 | 1 (0.6) | High |
| Harrison, 2004 | USA | Prospective (RCT) | Any colonoscopy | 50 | 58 | 24 (48) | 50 (100) | 29 | 9 | 0 (0) | Low |
| Hewett, 2011 | USA | Prospective | Screening/surveillance | 1000 | 59 | 484 (48) | 944 (94) | 254 | 44 | 0 (0) | High |
| Kushnir, 2015 | USA | Prospective (RCT) | Screening/surveillance | 450 | 60 | 183 (41) | 421 (94) | 176 | 41 | 0 (0) | High |
| Vargas, 2015 | Spain | Prospective | Any colonoscopy | 303 | Not given | Not given | 232 (77) | 28 | 14 | 0 (0) | High |
Adapted from Newcastle–Ottawa scale and QUADAS2 as described in Methods and Supplementary Figure 1. Supplementary Table 2 shows the scores for the eight components of this quality assessment.
Primary aim: the effect of right colon retroflexion on adenoma detection compared with conventional colonoscopy
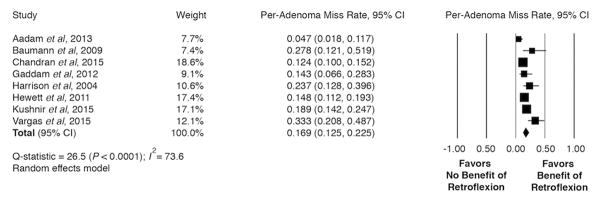
Figure 3 shows the Forest plot for the right colon per-adenoma miss rate. The minimum-maximum adenoma miss rate of the 8 individual studies ranged from 4.7% to 33.3%. The measure of heterogeneity was large; I2 = 74%, therefore, we modeled this data using random effects. The pooled per-adenoma miss rate from the 8 studies equaled 16.9% [95% CI, 12.5-22.5%]. Pre-specified analysis stratified by quality of studies (high/low) revealed results similar to the primary analysis with a per-adenoma miss rate of 17.8%. In addition, quality of study did not fully account for the heterogeneity seen between the studies based on I2 statistic.
Figure 3. Comparison of right colon per-adenoma miss rates for studies evaluating right colon retroflexion compared with conventional colonoscopy.
CI, confidence interval.
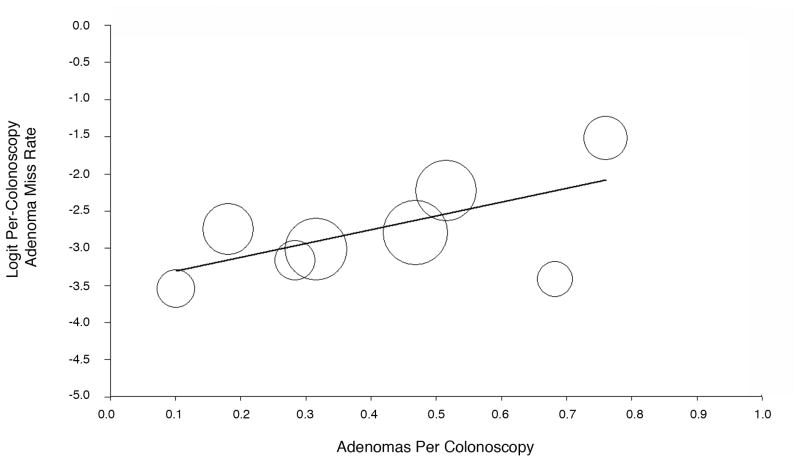
Figure 4 shows the Forest plot for the per-colonoscopy adenoma miss rate in the right colon. This value ranged in the studies from 2.8% to 18.0%. Again, the measure of heterogeneity was large, I2 = 77%, therefore a random effects model was used to get a pooled statistic. The pooled per-colonoscopy adenoma miss rate in the right colon was 6.2% [95% CI, 5.4-7.1%]. Again, stratified sensitivity analysis based on the quality did not change the magnitude of the effect. Pre-hoc, we hypothesized that the number of adenomas detected in the forward view in each study would have a direct relationship with the number of adenomas detected in the retroflexed view. Therefore, we performed a meta-regression of our analysis controlling for this variable. The positive slope of the regression showed that an incremental increase in the prevalence of adenomas detected by conventional colonoscopy was associated with an increase in the per-colonoscopy adenoma miss rate as more adenomas are detected in retroflexed view (P-value = 0.0002) (Figure 5).
Figure 4. Comparison of right colon per-colonoscopy miss rates for studies evaluating right colon retroflexion compared with conventional colonoscopy.
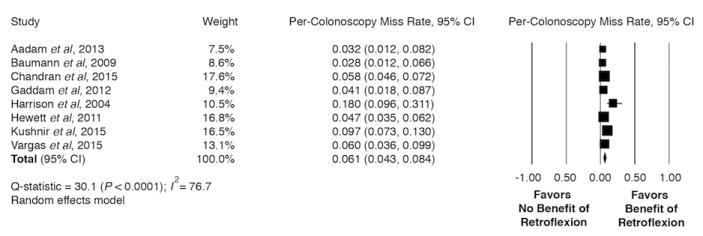
CI, confidence interval.
Figure 5. Meta-regression for the per-colonoscopy adenoma miss rate in the right colon with the prevalence of adenomas detected per colonoscopy.
Secondary aims: retroflexion success and safety
Our secondary aim was to determine a more exact point estimate for the success of the right colon retroflexion maneuver as well as adverse event rate. The retroflexion success rate in the 8 studies ranged from 77-100%. The random effects pooled retroflexion success rate was 91.9% [95% CI, 86-95%]. There was only 1 serious adverse event of perforation reported out of 3,660 retroflexion maneuvers, yielding a retroflexion adverse event rate of 0.03%.
Discussion
In this systematic review and meta-analysis, we found that reexamination of the right colon in retroflexed view detects approximately 17% of right-sided adenomas that would have been missed with conventional colonoscopy and can be successfully performed in 92% of patients with few reported adverse events. This is the first meta-analysis on this important topic and elucidates the value-added of right colon retroflexion in screening and surveillance colonoscopy after evaluation of 3,660 patients.
Colonoscopy has been shown to be the diagnostic and therapeutic test-of-choice for the prevention of colon cancer. However, many studies have shown significant adenoma miss rates exist even in the most skilled endoscopists' hands and thus colonoscopy has less success preventing right-sided colon cancers.10 While some evidence suggests that the biology of right-sided polyps to cancer sequence may be different than proximal lesions12, others believe that there is a higher miss rate of right sided lesions because of the folds in the cecum and ascending colon that are difficult to see behind without a retroflexed view.20 While some theorize that right colon retroflexion is merely a surrogate for increased withdrawal time and that it isn't the retroflexion maneuver per se which detects more polyps, there is evidence which supports that withdrawal time beyond a minimum accepted threshold of 7 minutes does not in fact improve polyp detection.33
While the present meta-analysis implicates a per-adenoma miss rate of 17% in the right colon by not performing right colon retroflexion, it cannot definitively claim that reexamination of the right colon in retroflexed view is superior to a second forward-view withdrawal because there were insufficient numbers of studies to evaluate this additional important question. However a single recent RCT of 850 patients showed that a second examination of the right colon in either retroflexed or forward view yielded similarly increased adenoma detection rates.25 Therefore, while it remains uncertain whether the optimal strategy for improving detection of right-sided adenomas is reexamination of the right colon in retroflexed view or a second forward view, the aforementioned evidence strongly indicates that performing at least one of these two techniques should be strongly considered in future standard of care colonoscopy quality guidelines given the formidable challenge of right-sided colon cancer prevention and significant adenoma miss rates associated with the absence of right colon reexamination. Additional future studies comparing reexamination of the right colon in retroflexed view with second forward view may be needed to better elucidate which of these two strategies should be universally recommended.
This study has several strengths. Firstly, the present study is the first meta-analysis addressing this important controversial question with a very extensive search of multiple databases. Furthermore, this meta-analysis analyzes a large number of patients (N = 3660) with precise measures of clinically relevant outcomes with respect to adenoma miss rates, retroflexion success rates and adverse event occurrence. Finally, sensitivity analysis stratifying by study quality was done and this did not change the magnitude of our primary outcome regarding per-adenoma miss rate.
However, as with any study, limitations are present and include the following. Firstly, the statistical heterogeneity among studies was relatively high which is likely accounted for by the range in adenoma miss rates among the studies. Stratified analyses for study quality did not change these heterogeneity results however. This may be accounted for by the endoscopist's ADR as well as population prevalence of adenomas. Interestingly, meta-regression (Figure 5) showed that an incremental increase in adenomas detected in conventional colonoscopy was associated with an increase in additional adenomas detected in retroflexed view. This may reflect the fact that patients or populations with higher prevalence of adenomas are more likely to benefit from right colon retroflexion. Additionally, this could reflect the fact that endoscopists with higher ADR in general, will concomitantly find more adenomas in the retroflexed view than those endoscopists with lower ADR. Interestingly while the pooled per-adenoma miss rate from the 8 studies was 16.9% [12.5-22.5, P value < 0.0005], the range spanned from 4.7%18 to 33.3%28 whereby in this latter study over 30% of the ascending colon polyps were detected only by colonoscope withdrawal in retroflexion.
While generalizability of adenoma detection, retroflexion success and adverse event rates may be affected by the fact that colonoscopies in many of these studies were performed by highly skilled endoscopists at major academic medical centers, a recent large RCT found that the overall right colon retroflexion success rate was 94% involving ten endoscopists with varying levels of experience.25 Furthermore, it is not clear what the learning curve is for the maneuver or how much additional time per procedure this maneuver requires once proficiency is obtained, which aside from retroflexion adverse event rate may be clinically relevant concerns. Notably, not all procedures in this study were done for screening and surveillance, therefore it is possible that the adenomas detected may underestimate the numbers detected in purely a screening or surveillance colonoscopy cohort.
While there were insufficient data to globally assess the impact of right colon retroflexion on surveillance intervals, one large study in this meta-analysis did address this question.20 Chandran et al found that 2.4% of patients (33/1351) had additional polyps identified on right colon retroflexion that shortened their recommended surveillance interval compared with conventional colonoscopy. Furthermore, of these, 60.6% (20/33) went from no adenomas identified on conventional colonoscopy to an additional 1 to 2 adenomas identified with reexamination of the right colon in retroflexed view shortening the recommended follow-up colonoscopy to 5 years as opposed to 10 years based on most guidelines. Again, given the critical challenge of interval right-sided colon cancers, these data are compelling and further supports reexamination of the right colon in retroflexed view given the maneuver's favorable safety profile. Finally, there are no current studies which directly address the effect of right colon retroflexion on colon cancer development, however, evidence increasingly indicates that adenoma detection is a valuable surrogate marker to this end.4, 5, 8
In summary, our systematic review and meta-analysis demonstrates that colonoscopy with right-sided retroflexion significantly increases the detection of adenomas in the ascending colon compared with conventional colonoscopy with a high rate of maneuver success and small risk of adverse events. Thus, while it remains uncertain whether the optimal strategy for improving detection of right-sided adenomas is reexamination of the right colon in retroflexed view or a second forward view, our study indicates that right colon retroflexion is a safe and highly effective technique which improves adenoma detection and should be strongly considered in future standard of care colonoscopy guidelines given the important challenge of right-sided colon cancer prevention.
Supplementary Material
Supplemental Table 1: Article search terms by database
Supplemental Table 2: Quality assessment score of studies included in the meta-analysis
Supplemental Figure 1: Study quality assessment tool
Acknowledgments
Funding Declaration: Dr. Cohen received funding for this research from an NIH T32 grant. Drs. Grunwald, Grossberg and Sawhney have no funding sources to declare relevant to this research.
Footnotes
Conflicts of Interest: Drs. Cohen, Grunwald, Grossberg and Sawhney have no conflicts of interest to declare relevant to this research.
References
- 1.Rex DK, Johnson DA, Anderson JC, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected] Am J Gastroenterol. 2009;104(3):739–50. doi: 10.1038/ajg.2009.104. [DOI] [PubMed] [Google Scholar]
- 2.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329(27):1977–81. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 3.Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366(8):687–96. doi: 10.1056/NEJMoa1100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. The New England journal of medicine. 2014;370(14):1298–306. doi: 10.1056/NEJMoa1309086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meester RG, Doubeni CA, Lansdorp-Vogelaar I, et al. Variation in Adenoma Detection Rate and the Lifetime Benefits and Cost of Colorectal Cancer Screening: A Microsimulation Model. JAMA : the journal of the American Medical Association. 2015;313(23):2349–58. doi: 10.1001/jama.2015.6251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. The American journal of gastroenterology. 2015;110(1):72–90. doi: 10.1038/ajg.2014.385. [DOI] [PubMed] [Google Scholar]
- 7.van Rijn JC, Reitsma JB, Stoker J, et al. Polyp miss rate determined by tandem colonoscopy: a systematic review. The American journal of gastroenterology. 2006;101(2):343–50. doi: 10.1111/j.1572-0241.2006.00390.x. [DOI] [PubMed] [Google Scholar]
- 8.Pohl H, Robertson DJ. Colorectal cancers detected after colonoscopy frequently result from missed lesions. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2010;8(10):858–64. doi: 10.1016/j.cgh.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 9.Baxter NN, Goldwasser MA, Paszat LF, et al. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150(1):1–8. doi: 10.7326/0003-4819-150-1-200901060-00306. [DOI] [PubMed] [Google Scholar]
- 10.Singh H, Nugent Z, Demers AA, et al. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010;139(4):1128–37. doi: 10.1053/j.gastro.2010.06.052. [DOI] [PubMed] [Google Scholar]
- 11.Brenner H, Hoffmeister M, Arndt V, et al. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010;102(2):89–95. doi: 10.1093/jnci/djp436. [DOI] [PubMed] [Google Scholar]
- 12.Azzoni C, Bottarelli L, Campanini N, et al. Distinct molecular patterns based on proximal and distal sporadic colorectal cancer: arguments for different mechanisms in the tumorigenesis. Int J Colorectal Dis. 2007;22(2):115–26. doi: 10.1007/s00384-006-0093-x. [DOI] [PubMed] [Google Scholar]
- 13.Matsushita M, Hajiro K, Okazaki K, et al. Efficacy of total colonoscopy with a transparent cap in comparison with colonoscopy without the cap. Endoscopy. 1998;30(5):444–7. doi: 10.1055/s-2007-1001305. [DOI] [PubMed] [Google Scholar]
- 14.Rex DK, Chadalawada V, Helper DJ. Wide angle colonoscopy with a prototype instrument: impact on miss rates and efficiency as determined by back-to-back colonoscopies. Am J Gastroenterol. 2003;98(9):2000–5. doi: 10.1111/j.1572-0241.2003.07662.x. [DOI] [PubMed] [Google Scholar]
- 15.Dik VK, Moons LM, Siersema PD. Endoscopic innovations to increase the adenoma detection rate during colonoscopy. World J Gastroenterol. 2014;20(9):2200–11. doi: 10.3748/wjg.v20.i9.2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gralnek IM, Segol O, Suissa A, et al. A prospective cohort study evaluating a novel colonoscopy platform featuring full-spectrum endoscopy. Endoscopy. 2013;45(9):697–702. doi: 10.1055/s-0033-1344395. [DOI] [PubMed] [Google Scholar]
- 17.Rex DK, Vemulapalli KC. Retroflexion in colonoscopy: why? Where? When? How? What value? Gastroenterology. 2013;144(5):882–3. doi: 10.1053/j.gastro.2013.01.077. [DOI] [PubMed] [Google Scholar]
- 18.Aadam AA, Saeian K, Massey BT, et al. Proximal colon retroflexion with adult versus pediatric colonoscopes. Gastrointestinal Endoscopy. 2013;77(5):AB426–AB7. [Google Scholar]
- 19.Harrison M, Singh N, Rex DK. Impact of proximal colon retroflexion on adenoma miss rates. The American journal of gastroenterology. 2004;99(3):519–22. doi: 10.1111/j.1572-0241.2004.04070.x. [DOI] [PubMed] [Google Scholar]
- 20.Chandran S, Parker F, Vaughan R, et al. Right-sided adenoma detection with retroflexion versus forward-view colonoscopy. Gastrointestinal endoscopy. 2015;81(3):608–13. doi: 10.1016/j.gie.2014.08.039. [DOI] [PubMed] [Google Scholar]
- 21.Baumann UA. Does retroflexion improve adenoma miss rates on the right side of the colon when using a pediatric variable-stiffness colonoscope during routine colonoscopy? Endoscopy. 2009;41(7):654. doi: 10.1055/s-0029-1214876. Epub 2009/07/10. [DOI] [PubMed] [Google Scholar]
- 22.Gaddam S, Hollander TG, Edmundowicz SA, et al. Extending right colon retroflexion to the splenic flexure. Gastroenterology. 2012;142(5):S227. [Google Scholar]
- 23.Hewett DG, Rex DK. Miss rate of right-sided colon examination during colonoscopy defined by retroflexion: an observational study. Gastrointest Endosc. 2011;74(2):246–52. doi: 10.1016/j.gie.2011.04.005. Epub 2011/06/18. [DOI] [PubMed] [Google Scholar]
- 24.Kim HU, Boo SJ, Na SY, et al. [Additional polyp detection rate using colonoscopic retroflexion in right colon] Korean J Gastroenterol. 2015;65(2):90–8. doi: 10.4166/kjg.2015.65.2.90. Epub 2015/02/27. [DOI] [PubMed] [Google Scholar]
- 25.Kushnir VM, Oh YS, Hollander T, et al. Impact of retroflexion vs. second forward view examination of the right colon on adenoma detection: a comparison study. The American journal of gastroenterology. 2015;110(3):415–22. doi: 10.1038/ajg.2015.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robles-Medranda C, Alcívar MS, Vargas M, et al. Colonoscope for the evaluation of colon mucosa in forward and retroviewing: A safety and feasibility pilot study. Gastrointestinal Endoscopy. 2015;81(5):AB156–AB7. [Google Scholar]
- 27.Thoufeeq M, Khiyar Y. Retroflexion in the proximal colon: A single centre study. Endoscopy. 2012;44(4):442. [Google Scholar]
- 28.Vargas AL, Alburquerque M, Figa M, et al. Ascending colon exploration by retroviewing: technical feasibility and diagnosis performance. Gastrointestinal Endoscopy. 2015;81(5):AB293. [Google Scholar]
- 29.Zago RR, Cavalcante DB, Teixeira CV, et al. Feasibility and safety of proximal retroflexion maneuver performed by an endoscopy fellow using colonoscopes from two different manufacturers. Gastrointestinal Endoscopy. 2012;75(4):AB299–AB300. [Google Scholar]
- 30.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Clark BT, Rustagi T, Laine L. What level of bowel prep quality requires early repeat colonoscopy: systematic review and meta-analysis of the impact of preparation quality on adenoma detection rate. Am J Gastroenterol. 2014;109(11):1714–23. doi: 10.1038/ajg.2014.232. quiz 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Higgins JPTGS. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration. 2011 [Google Scholar]
- 33.Sawhney MS, Cury MS, Neeman N, et al. Effect of institution-wide policy of colonoscopy withdrawal time > or = 7 minutes on polyp detection. Gastroenterology. 2008;135(6):1892–8. doi: 10.1053/j.gastro.2008.08.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: Article search terms by database
Supplemental Table 2: Quality assessment score of studies included in the meta-analysis
Supplemental Figure 1: Study quality assessment tool