Abstract
Objective
Mental stress-induced myocardial ischemia (MSIMI) is a common phenomenon in patients with coronary artery disease (CAD), but contemporary studies of its prognostic significance and its underlying pathophysiology are limited.
Methods
We prospectively enrolled patients with confirmed CAD in the Mental Stress Ischemia Prognosis Study (MIPS) between 2011 and 2014. All patients underwent mental stress testing using a standardized public speaking task and ischemia was detected by 99mTc sestamibi myocardial perfusion imaging. Patients also underwent conventional stress testing for myocardial ischemia (CSMI) using exercise or pharmacological stress testing. Furthermore, digital microvascular flow, endothelial function, arterial stiffness and blood sample collections were performed before, during and after mental stress. Two-year adverse clinical outcomes are being assessed.
Results
Six-hundred and ninety-five patients completed baseline enrollment in the MIPS. Their mean (SD) age was 62.9 (9.1) years, 72% were men, 30% were African American, and 32% had a history myocardial infarction. The prevalence of MSIMI and CSIMI are 16.1% and 34.7%, respectively. A total of 151 (22.9%) patients had only CSIMI, 28 (4.2%) had only MSIMI and 78 (11.8%) had both MSIMI and CISIMI. Patients with ischemia had a lower ejection fraction and higher prevalence of previous coronary artery bypass grafting compared to those without inducible ischemia (p<0.050). The prevalence of obstructive CAD was not statistically different between patients with and without MSIMI (p=0.426); in contrast, it was higher in patients with CSIMI (p<0.001).
Conclusion
The MIPS data will provide useful information to assess the prognostic significance and underlying mechanisms of MSIMI.
Keywords: Mental stress, myocardial ischemia, coronary artery disease, prognosis
Introduction
The idea that psychological stress can precipitate myocardial ischemia was first described by Deanfield and Selwyn in 1984 when they demonstrated the presence of mental stress-induced reversible perfusion abnormalities using nuclear imaging.1 It is now well established that emotional stress, anger, depressed mood and other psychological states can trigger acute myocardial infarction and sudden cardiac death in susceptible individuals.2–9 Mental stress-induced myocardial ischemia (MSIMI) has been shown to occur in a substantial proportion of patients with stable coronary artery disease (CAD) and evidence of exercise-induced ischemia (18% to 67% or more).10 Limited study data suggest that MSIMI is associated with a doubling of the risk for subsequent death or adverse cardiovascular events,11 and promising treatments are being tested.10 Therefore, mental stress testing represents a useful technique for assessing individual patients susceptibility to the effects of psychological stress and emotion on cardiac function. However, MSIMI has not gained broad awareness and is not yet being assessed clinically. Only five previous studies have assessed and published the impact of MSIMI on the incidence of adverse cardiovascular events.12–16 These studies were generally small (the largest study enrolled <200 patients) and they included largely white male patients, were performed in cohorts enrolled decades ago, and none used myocardial perfusion imaging (the current gold standard for ischemia detection).17 A larger investigation to study a diverse contemporary population was therefore needed to assess the prognosis of MSIMI and investigate its underlying mechanisms.
The specific aims of the Mental Stress Ischemia Prognosis Study (MIPS) are to study the impact of MSIMI on long-term cardiovascular outcomes in a contemporary cohort of patients with CAD and to identify potential vascular, neurobiological and genetic determinants of this phenomenon.
Methods
Study Sample and Patient Enrollment
MIPS is a prospective study of stable CAD patients enrolled between June 2011 and August 2014 from Emory University affiliated hospitals and clinics, including Emory University Hospital, Grady Memorial Hospital, Emory Midtown Hospital and the Atlanta VA Medical Center. Patients were enrolled if they were 30 to 79 years of age and had documented CAD defined as any of the following: an abnormal coronary angiogram demonstrating evidence of atherosclerosis with at least luminal irregularities, previous percutaneous or surgical coronary revascularization, a history of myocardial infarction (MI), or a positive nuclear stress test. Patients were excluded if they had an acute coronary syndrome or decompensated heart failure in the prior week, severe psychiatric conditions other than major depression, pregnancy (women of childbearing age were screened by pregnancy test), uncontrolled high blood pressure (≥180/110 mmHg), or with contraindications for regadenoson administration. Beta-adrenergic antagonists were held for 24 hours and calcium channel blockers and nitrates for at least 12 hours prior to the stress test. Patients for whom withholding medications was considered unsafe were excluded. The diagnosis of heart failure was made using the following criteria: a) self-reported history of heart failure that was confirmed by chart review; b) medical chart review for previous diagnosis of heart failure (all patients were seen by a cardiologist at Emory affiliated hospitals before enrollment); c) ICD codes and adjudication by research personnel. Coronary angiographic data were collected by chart review with a median time between the angiogram and enrollment of 2.1 (1.0 – 4.4) years. The Emory University Institutional Review Board approved the research protocol, and all participants provided written informed consent.
Study Protocol
Baseline studies were performed during two visits within a week (Figure 1). At the initial visit (Visit 1), patients were consented and underwent a medical history and psychosocial/psychiatric assessments, blood draw, baseline vascular function testing and a resting SPECT study. This was followed by a stress SPECT study after either a conventional (exercise or chemical) stress test or a mental stress test. During Visit 2, they had the other stress test performed. The sequence of the two stressors was randomly assigned.
Figure 1.
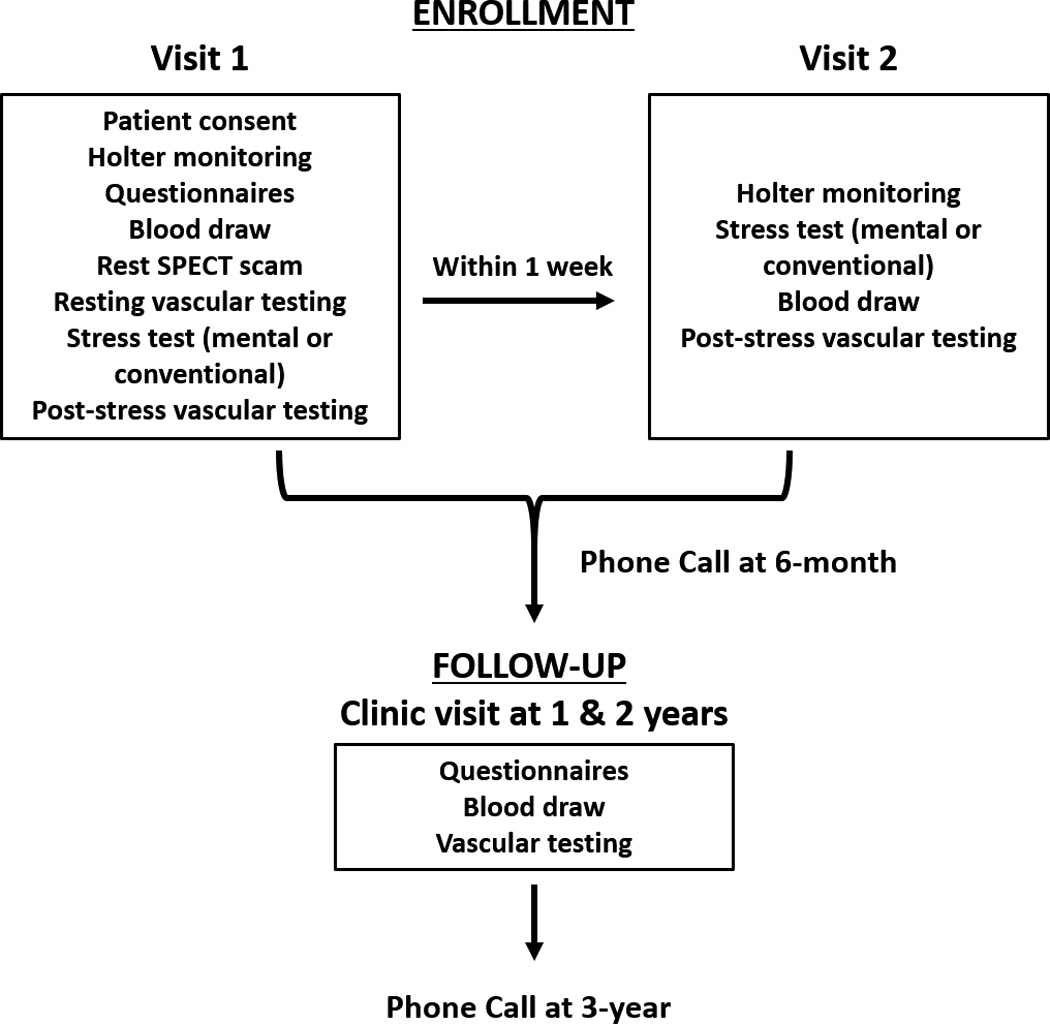
Study visits and follow up.
SPECT Imaging Protocol
For resting myocardial blood flow assessment, patients were injected with a low dose 99m Tc-sestamibi (10–14 mCi based on weight). Thirty to 45 minutes after injection, resting SPECT images were acquired.
Conventional (Exercise or Pharmacological) Stress Test
Patients underwent treadmill exercise testing using the standard Bruce protocol. The ECG, blood pressure and heart rate were continuously monitored. Once the subject attained 85% of their target heart rate, they were injected with a regular dose of 99mTc-sestamibi (30–40 mCi based on weight) intravenously. Patients who were unable to exercise18 underwent pharmacological stress testing with regadenoson (Astellas, Northbrook, IL). Forty to 60 minutes after isotope injection, stress SPECT imaging was performed. A physician was present during the study and the electrocardiogram and vital signs were continuously monitored.
Mental Stress Testing
After a 30-minute rest period in a quiet room, mental stress testing was performed by trained staff. Patients were required to listen to a scripted message that provided instructions for the mental stress task. They were asked to imagine a stressful situation, using a scenario in which a close relative had been mistreated in a nursing home. They then were asked to prepare a statement for 2 minutes and then present it over a 3-minute period in front of a video camera and an audience wearing white coats. Patients were told that their speech would be evaluated for content and duration. Blood pressure and heart rate were recorded at 5-minute intervals during the resting phase and at 1-minute intervals during the mental stress period using an automatic oscillometric device. At 60 seconds into the mental stress task, a regular dose of 99mTc-sestamibi (30–40 mCi based on weight) was injected intravenously and images were acquired 40 minutes to 1 hour later.
SPECT Image Interpretation
Myocardial perfusion images were interpreted by two experienced readers blinded to the stressor (mental or conventional) and without prior knowledge of the medical history or angiographic data. Discrepancies in interpretation of SPECT images were resolved by consensus. Rest and stress images were visually compared for the number and severity of perfusion defects using a 17-segment model.19 Each segment was scored from 0 to 4, with 0 being normal uptake, 1 possibly normal perfusion, 2 definitely abnormal perfusion, 3 severe perfusion defect and 4 no uptake. A sum rest score was calculated by adding up the perfusion scores across the 17 myocardial segments. Ischemia was defined as a new myocardial perfusion defect with a score of ≥2 in any segment, or worsening of a pre-existing impairment of at least 2 points in a single segment, or worsening of at least 1 point in 2 or more contiguous segments.19 We also assessed ischemia using The Emory Cardiac Tool Box (Emory University, Atlanta, GA) software, which is a quantitative, operator independent assessment of myocardial perfusion as previously described.20
Long-Term Follow-Up
Patients are being followed periodically by phone calls and clinic visits for a mean follow up period of 2 years (Figure 1). At 1 year and at 2 years, patients have a clinic visit where medical history, psychosocial and vascular assessments that were collected at baseline are repeated. At 6-month and 3-year intervals, patients are contacted by phone to assess health status, evaluate selected psychosocial factors, and study outcomes. If patients state that they have been hospitalized or have had a procedure since the last visit, their physicians are contacted and discharge summaries obtained.
Primary End-Points
The primary end points are: 1) death or nonfatal MI and 2) a composite of death, nonfatal MI, hospitalization for unstable angina, and coronary revascularization.
Other Outcome Measures
i) Vascular function assessment
All patients underwent peripheral vascular function assessments including digital blood flow, endothelial function and arterial stiffness measurements. Microvascular blood flow was continuously measured using pulsatile arterial tonometry throughout the mental stress test.18, 21–24 As previously described, endothelium-dependent function was assessed using brachial artery flow-mediated vasodilation (Acuson Aspen ultrasound system), the reactive hyperemia index using pulsatile arterial tonometry (Itamar Inc.), and arterial stiffness using the SphygmoCor device (Atcor Medical, Australia), before and 30 minutes after mental stress testing.25–29
ii) Blood testing
Blood samples were obtained for biomarkers, genomic testing, catecholamine levels, oxidative and inflammatory markers and circulating progenitor cells. On the day of the mental stress study, samples were collected at rest, 5 min, 45 min and 90 min after completion of the mental stress test. On the day of the conventional stress test, samples were drawn 45 minutes after the test. Blood samples are being collected at 1- and 2-year visits. Catecholamines were measured at rest and 5 min post mental stress test in heparinized plasma using a commercial high-sensitivity EIA Kit (2-CAT ELISA, Labor Diagnostika Nord as supplied by Rocky Mountain Scientific, Centennial, CO).
iii) Psychological assessments
At baseline and at each follow-up visit, patients underwent a comprehensive psychological assessment including the Cook-Medley Hostility Scale,30 the State-Trait Anger expression scale,31, 32 the Beck Depression Inventory,33–35 the State-Trait Anxiety Inventory,36, 37 the Multidimensional Scale Of Perceived Social Support,38, 39 the Life Experiences Survey,40, 41 the Perceived Stress Scale,42 the Early Trauma Inventory,43 the Post-Traumatic Stress Disorder checklist (civilian version)44, 45 and the Wechsler Memory Scale.46 In addition, we administered the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders for the assessment of psychiatric diagnoses (SCID).47 Before and after mental stress testing, patients completed the Subjective Units of Distress Scale,48 an analog scale of subjective distress.
Data Management
Data are being entered and managed using Clinical DataFax Systems Incorporated client-server data management software (iDataFax, Ontario, Canada). The validity and quality of data are checked through regular data queries for out-of-range values and missing values. Omissions and errors are conveyed to the study staff for corrections on an ongoing basis.
Statistical analysis
For this manuscript, we used Student’s t-tests and chi square tests to examine the differences between groups. We used mixed linear models to test the change in hemodynamic parameters and catecholamines during mental stress. All statistical analysis was conducted using SPSS (v 23.0, IBM Corp., Armonk, NY, USA).
Results
Between June 2011 and August 2014 we enrolled 695 patients in the MIPS. Mean age was 62.9±9.1 years (range of 34 to 79 years), 72% male and 30% African American. As expected, CAD risk factors were prevalent (Table 1); approximately a third (38%) had a previous myocardial infarction, 34.7% had previous coronary artery bypass procedure and 53.4% previous percutaneous intervention. About 14% of our population had a current diagnosis of heart failure. Mean ejection fraction (EF) was lower in patients with heart failure in comparison to patients without history of heart failure (SPECT assessed resting EF of 71±11 vs. 55±19%, and echocardiogram assessed EF of 55±9 vs 39±16%, p<0.001 for both). In a subgroup of patients with available coronary angiogram data (n=575), the median time between coronary angiography and enrollment was 2.1 (1.0 – 4.4) years. Most patients had a history of obstructive CAD by angiography (83.8% with at least one coronary artery with ≥70% stenosis).
Table 1.
Baseline characteristics
| MSIMI | CSIMI | |||||
|---|---|---|---|---|---|---|
| Negative | Positive | P value | Negative | Positive | P value | |
| Number | 554 | 106 | 431 | 229 | ||
| Age, years, mean ± SD | 63 ± 9 | 63 ± 9 | 0.665 | 63 ± 9 | 63 ± 9 | 0.565 |
| Men, % | 72 | 76 | 0.352 | 71 | 76 | 0.236 |
| African American, % | 29 | 36 | 0.175 | 29 | 32 | 0.521 |
|
Body mass index, kg/m2, mean ± SD |
30 ± 5 | 30 ± 5 | 0.187 | 30 ± 5 | 30 ± 5 | 0.599 |
| Current/former Smoking, % | 58 | 63 | 0.325 | 58 | 60 | 0.726 |
| Systemic Hypertension. % | 75 | 78 | 0.505 | 75 | 77 | 0.631 |
| Hyperlipidemia, % | 81 | 82 | 0.837 | 80 | 84 | 0.233 |
| Diabetes Mellitus, % | 31 | 39 | 0.133 | 30 | 37 | 0.060 |
| Myocardial infarction, % | 36 | 42 | 0.202 | 37 | 36 | 0.778 |
|
Coronary artery bypass grafting, % |
31 | 52 | <0.001 | 27 | 49 | <0.001 |
|
Percutaneous transluminal coronary angioplasty, % |
55 | 50 | 0.339 | 53 | 57 | 0.342 |
| Congestive heart failure, % | 14 | 15 | 0.784 | 13 | 17 | 0.208 |
| SPECT LVEF,%, mean ± SD | 69 ± 14 | 65 ± 14 | 0.010 | 70 ± 13 | 66 ± 14 | <0.001 |
|
Echocardiogram LVEF, %, mean ± SD |
53 ± 12 | 52 ± 11 | 0.538 | 53 ± 12 | 52 ± 11 | 0.584 |
|
At least 1 coronary vessel with 50% stenosis*, % |
90 | 93 | 0.335 | 89 | 94 | 0.037 |
|
At least 1 coronary vessel with 70% stenosis*, % |
83 | 87 | 0.426 | 80 | 92 | <0.001 |
| Aspirin, % | 87 | 86 | 0.832 | 86 | 87 | 0.849 |
| Clopidogrel, % | 34 | 39 | 0.317 | 32 | 38 | 0.145 |
| ACEi, % | 44 | 53 | 0.092 | 44 | 48 | 0.361 |
| ARBs, % | 17 | 14 | 0.525 | 16 | 16 | 0.821 |
| Beta blocker, % | 74 | 75 | 0.745 | 74 | 75 | 0.734 |
| Statins, % | 85 | 86 | 0.857 | 84 | 87 | 0.411 |
| Antidepressant, % | 23 | 19 | 0.334 | 23 | 21 | 0.409 |
MSIMI: Mental stress induced myocardial ischemia. CSIMI: conventional stress induced myocardial ischemia. SPECT: Single-photon emission computed tomography. LVEF: left ventricular ejection fraction. ACEi: Angiotensin converting enzyme inhibitor. ARB: Angiotensin receptor blocker.
Coronary angiogram data was available for only 575 patients with a median time between angiogram and enrollment of 2.1 (1.0–4.4) years.
More than one quarter of patients met criteria for diagnosis of major depression (26.4%) with the SCID and 6.5% for post-traumatic stress disorder (Table 2).
Table 2.
Baseline Psychological Characteristics
| Lifetime history of major depression, % | 26.4 |
| Lifetime history of post-traumatic stress disorder, % |
6.5 |
| Beck depression inventory score | 8.4 ± 8.4 |
| Post-traumatic stress disorder score | 26.7 ± 11.1 |
| Multidimensional scale of perceived social support |
67.2 ± 14.8 |
| Cook-Medley hostility scale | 16 ± 8 |
| Early trauma inventory self-report | 6.5 ± 4.8 |
Hemodynamic and catecholamine response to mental stress
Significant increases in systolic blood pressure, diastolic blood pressure and heart rate were observed during the mental stress test (p<0.001 for interaction with time for all, Figure 2). Mean percent increases from rest to stress were 20±12%, 17±11% and 18±15% for systolic blood pressure, diastolic blood pressure and heart rate, respectively.
Figure 2.
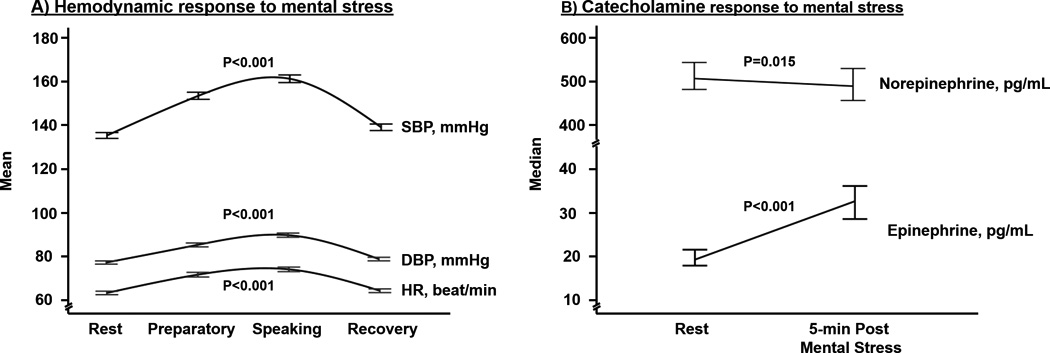
A) Hemodynamic and B) catecholamine response to mental stress. SBP: Systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate. Error bars represent 95%CI.
Overall, 501 patients had catecholamine levels measured at baseline and 5 minutes after the mental stress test. Significant increases in epinephrine levels were observed with a median (interquartile) change of 77 (13 – 160) %, (Figure 2). In contrast, norepinephrine levels decreased slightly after mental stress with a median (interquartile) change of −0.02 (−0.17 – 0.16) %.
MSIMI and CSIMI
Few patients had missing or poor quality SPECT scans. Of the 695 patients enrolled, 680 patients completed scans at rest and after mental stress, 666 patients completed scans at rest and after conventional stress testing, and 660 patients had all scans completed with good imaging quality. For conventional stress testing, most patients underwent a treadmill stress test (68.3%), while the remaining patients had pharmacological stress testing.
Among 660 patients with data during both stress tests, the incidence of MSIMI and CSIMI was 16.1% (n=106) and 34.7% (n=229), respectively. Table 1 shows the basic demographics, CAD risk factors and medication history in the 660 patients who have available data for all scans. There were no statistical differences between patients with and without ischemia during either stress test, except for a slightly lower ejection fraction and higher prevalence of previous coronary artery bypass grafting in those with ischemia. The prevalence of obstructive CAD was not different between patients with and without MSIMI; in contrast, it was higher in patients with CSIMI (Table 1).
A total of 151 (22.9%) patients had only CSIMI, 28 (4.2%) had only MSIMI and 78 (11.8%) had both MSIMI and CISIMI. The incidence of MSIMI was higher in those who developed CSIMI (34.1%) compared to those without CSIMI (6.5%).
Discussion
The MIPS will provide important information about the pathophysiology of MSIMI and its impact on long-term outcomes in patients with CAD. The large sample size and ethnic diversity of our cohort, as well as the comprehensive vascular, genetic, molecular and psychosocial assessments are unique features and major strengths of the study that will likely generate useful study data regarding MSIMI.
In this large and diverse sample, we found an overall incidence of MSIMI of 16.1% by means of SPECT myocardial perfusion imaging. MSIMI was more common among patients who had ischemia during conventional stress testing. There were only few correlates of either MSIMI or CSIMI. Patients with either MSIMI or CSIMI had a lower ejection fraction and higher prevalence of previous coronary artery bypass grafting compared to those without inducible ischemia. The prevalence of obstructive CAD was not statistically different between patients with and without MSIMI; in contrast, it was higher in patients with CSIMI. Previous studies have reported an incidence of MSIMI between 18% and 67%, measured with a variety of methods.13, 15, 16 Although the incidence of MSIMI is lower in our study, these studies are not comparable because of differences in the methodologies for ischemia assessment, mental stress protocols, the definition of ischemia, and characteristics of the study population. For example, only few previous studies have used SPECT myocardial perfusion imaging to assess MSIMI.49–53 In addition, most previous investigations studied MSIMI only in patients with a documented positive exercise stress test, a subgroup that is at higher risk of MSIMI as also shown in our study. Although investigators have employed different mental stress protocols, the hemodynamic responses achieved in our study were comparable to previously reported changes in heart rate and blood pressure, suggesting that the mental stress challenge was adequate.54–59 However, the epinephrine response was lower than previously reported, likely because we measured epinephrine levels 5 minutes after the mental stress rather than during the peak mental stress period.54 Interestingly, we observed a slight decrease in norepinephrine levels 5 minutes after the mental stress.54
It is still unclear why some patients develop ischemia during mental stress while others do not. MSIMI is known to be a distinct phenomenon from ischemia induced by a conventional stress test. It is typically painless, occurs at lower levels of oxygen demand than ischemia due to physical exertion, and it is not related to CAD severity.60 Consistent with previous investigations, we show that some patients develop ischemia with mental stress but not with exercise or pharmacological stress.51, 61 Thus, other factors besides increases in heart rate and blood pressure due to stress lie behind the MSIMI phenomenon. A promising area of investigation is endothelial and microvascular dysfunction. MSIMI is associated with peripheral vasoconstriction,54, 62–66 which can be measured as a change in digital arterial pulse volume using digital tonometry.18, 67, 68 Since changes in peripheral vascular tone may reflect changes in coronary vascular resistance, peripheral microvascular vasomotor response to mental stress may serve as a surrogate for similar changes in the coronary vasculature.69
Although MSIMI has been studied before, there are several important gaps in our knowledge. Most studies have included small, selected samples of CAD patients enrolled decades ago, mostly with a history of exercise-induced myocardial ischemia, a group that represents a minority of CAD patients in the current era of aggressive therapeutic interventions.12, 13, 15, 16, 70 In contrast, our study is the first to assess prevalence and outcomes of MSIMI in a large and contemporary sample of patients with stable and broadly defined CAD (we only excluded patients who had an acute coronary syndrome within a week prior to enrollment).
Women and minority patients were severely underrepresented in previous studies. A strength of our study is the very good representation of women and African Americans, which makes our study population more representative of stable CAD patients in today’s clinical practice. Importantly, many previous studies used the presence of wall motion abnormality or an arbitrary drop in EF (between 5–8%) during mental stress as criteria for MSIMI.11, 71 Since mental stress is associated with a significant increase in peripheral vascular resistance, a change in left ventricular function may reflect an increase in afterload rather than true myocardial ischemia.11 An advantage of our protocol is the use of SPECT myocardial perfusion imaging with ischemia definition based on the American Society of Nuclear Cardiology guidelines.19 A specific advantage of SPECT imaging for MSIMI assessment is that the radioisotope, injected at peak stress, is trapped in the myocytes and thus provides a snapshot of perfusion at the time of stress, even though scanning occurs later.
Additional strengths of our study include the use of conventional stress testing as a control condition, the comprehensive assessment of vascular changes during mental stress to examine vascular dynamics, the collection of blood samples at different time points for the assessment of immune/inflammatory responses and genomic profiling. Finally, the prospective follow-up for a mean of 2 years with independent adjudication of cardiovascular endpoints will provide data on the long term consequences of MSIMI.
Conclusion
Exposure to psychological stress is pervasive during life, yet its effects in subjects with CAD are poorly understood. The MIPS is the largest prospective study of MSIMI that has been designed to promote a better understanding of this phenomenon, and to help provide robust data on the prognostic significance of MSIMI in individuals with CAD. The study will identify psychosocial and genetic susceptibilities and novel causal mechanisms underlying the effects of acute psychological stress in patients with CAD, and will provide an impetus for the development of effective interventions in this area of critical public health importance.
Acknowledgments
We would like to thank Naser Abdulhadi, Ayman Alkhoder, Malik Obideen, Tene T. Lewis, and Oleksiy Levantsevych for their significant contributions to the MIPS study including patient enrollment and data collection.
Sources of Funding: Dr. Vaccarino and Dr. Quyyumi report research support from NIH. Ernest V. Garcia receives royalties from the sale of the Emory Cardiac Toolbox, used for some analyses in this study. This work was supported by the NIH (P01 HL101398, P20HL113451-01, P01HL086773-06A1, R56HL126558-01, R01 HL109413, R01HL109413-02S1, UL1TR000454, KL2TR000455, K24HL077506, and K24 MH076955). The sponsors of this study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Abbreviations
- MSIMI
Mental stress induced myocardial ischemia
- CSIMI
Conventional stress induced myocardial ischemia
- CAD
Coronary artery disease
- SPECT
Single photon emission computed tomography
- MI
Myocardial infarction
Footnotes
Conflicts of Interest: None of the other authors report conflict of interest relevant to this article.
References
- 1.Deanfield J, Kensett M, Wilson R, Shea M, Horlock P, De Landsheere C, Selwyn A. Silent myocardial ischemia due to mental stress. The Lancet. 1984;324:1001–1005. doi: 10.1016/s0140-6736(84)91106-1. [DOI] [PubMed] [Google Scholar]
- 2.Strike PC, Magid K, Whitehead DL, Brydon L, Bhattacharyya MR, Steptoe A. Pathophysiological processes underlying emotional triggering of acute cardiac events. Proc Natl Acad Sci U S A. 2006;103:4322–4327. doi: 10.1073/pnas.0507097103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steptoe A, Strike PC, Perkins-Porras L, McEwan JR, Whitehead DL. Acute depressed mood as a trigger of acute coronary syndromes. Biological Psychiatry. 2006;60:837–842. doi: 10.1016/j.biopsych.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 4.Strike PC, Steptoe A. Behavioral and emotional triggers of acute coronary syndromes: a systematic review and critique. Psychosomatic Medicine. 2005;67:179–186. doi: 10.1097/01.psy.0000155663.93160.d2. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharyya MR, Steptoe A. Emotional triggers of acute coronary syndromes: strength of evidence, biological processes, and clinical implications. Prog Cardiovasc Dis. 2007;49:353–365. doi: 10.1016/j.pcad.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health. 2013;34:337–354. doi: 10.1146/annurev-publhealth-031912-114452. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y, Zhao Z, Gao X, Li L, Liu G, Chen W, Xing L, Yu B, Lin P. Type D Personality and Coronary Plaque Vulnerability in Patients With Coronary Artery Disease: An Optical Coherence Tomography Study. Psychosomatic Medicine. 2016;78:583–592. doi: 10.1097/PSY.0000000000000307. [DOI] [PubMed] [Google Scholar]
- 8.Doyle F, McGee H, Conroy R, Conradi HJ, Meijer A, Steeds R, Sato H, Stewart DE, Parakh K, Carney R, Freedland K, Anselmino M, Pelletier R, Bos EH, de Jonge P. Systematic Review and Individual Patient Data Meta-Analysis of Sex Differences in Depression and Prognosis in Persons With Myocardial Infarction: A MINDMAPS Study. Psychosomatic Medicine. 2015;77:419–428. doi: 10.1097/PSY.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 9.Shively CA, Register TC, Appt SE, Clarkson TB. Effects of long-term sertraline treatment and depression on coronary artery atherosclerosis in premenopausal female primates. Psychosomatic Medicine. 2015;77:267–278. doi: 10.1097/PSY.0000000000000163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burg MM, Vashist A, Soufer R. Mental stress ischemia: present status and future goals. Journal of Nuclear Cardiology. 2005;12:523–529. doi: 10.1016/j.nuclcard.2005.06.085. [DOI] [PubMed] [Google Scholar]
- 11.Wei J, Rooks C, Ramadan R, Shah AJ, Bremner JD, Quyyumi AA, Kutner M, Vaccarino V. Meta-analysis of mental stress-induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease. Am J Cardiol. 2014;114:187–192. doi: 10.1016/j.amjcard.2014.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain D, Burg M, Soufer R, Zaret BL. Prognostic Implications of Mental Stress-Induced Silent Loft Ventricular Dysfunction in Patients With Stable Angina Pectoris. The American Journal of Cardiology. 1995;76:31–35. doi: 10.1016/s0002-9149(99)80796-6. [DOI] [PubMed] [Google Scholar]
- 13.Jiang W, Babyak M, Krantz DS, Waugh RA, Coleman RE, Hanson MM, Frid DJ, McNulty S, Morris JJ, O'Connor CM, Blumenthal JA. Mental stress--induced myocardial ischemia and cardiac events. JAMA. 1996;275:1651–1656. doi: 10.1001/jama.275.21.1651. [DOI] [PubMed] [Google Scholar]
- 14.Krantz DS, Santiago HT, Kop WJ, Merz CNB, Rozanski A, Gottdiener JS. Prognostic value of mental stress testing in coronary artery disease∗. The American Journal of Cardiology. 1999;84:1292–1297. doi: 10.1016/s0002-9149(99)00560-3. [DOI] [PubMed] [Google Scholar]
- 15.Sheps DS, McMahon RP, Becker L, Carney RM, Freedland KE, Cohen JD, Sheffield D, Goldberg AD, Ketterer MW, Pepine CJ, Raczynski JM, Light K, Krantz DS, Stone PH, Knatterud GL, Kaufmann PG. Mental Stress–Induced Ischemia and All-Cause Mortality in Patients With Coronary Artery Disease: Results From the Psychophysiological Investigations of Myocardial Ischemia Study. Circulation. 2002;105:1780–1784. doi: 10.1161/01.cir.0000014491.90666.06. [DOI] [PubMed] [Google Scholar]
- 16.Babyak MA, Blumenthal JA, Hinderliter A, Hoffman B, Waugh RA, Coleman RE, Sherwood A. Prognosis After Change in Left Ventricular Ejection Fraction During Mental Stress Testing in Patients With Stable Coronary Artery Disease. The American Journal of Cardiology. 2010;105:25–28. doi: 10.1016/j.amjcard.2009.08.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krantz DS, Burg MM. Current perspective on mental stress-induced myocardial ischemia. Psychosomatic medicine. 2014;76:168–170. doi: 10.1097/PSY.0000000000000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramadan R, Sheps D, Esteves F, Maziar Zafari A, Douglas Bremner J, Vaccarino V, Quyyumi AA. Myocardial Ischemia During Mental Stress: Role of Coronary Artery Disease Burden and Vasomotion. Journal of the American Heart Association. 2013;2 doi: 10.1161/JAHA.113.000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, Ficaro EP, Freeman MR, Hendel RC, Jain D, Leonard SM, Nichols KJ, Polk DM, Soman P American Society of Nuclear C. Single photon-emission computed tomography. J Nucl Cardiol. 2010;17:941–973. doi: 10.1007/s12350-010-9246-y. [DOI] [PubMed] [Google Scholar]
- 20.Garcia EV, Faber TL, Cooke CD, Folks RD, Chen J, Santana C. The increasing role of quantification in clinical nuclear cardiology: the Emory approach. J Nucl Cardiol. 2007;14:420–432. doi: 10.1016/j.nuclcard.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 21.Burton A. The range and variability of the blood flow in the human fingers and the vasomotor regulation of body temperature. Amer J Physiology. 1939;127:437–453. [Google Scholar]
- 22.Wilkins R, Doupe J, Newman HW. The rate of blood flow in normal fingers. Clinical Science. 1938;3:403–411. [Google Scholar]
- 23.Schnall RP, Shlitner A, Sheffy J, Kedar R, Lavie P. Periodic, profound peripheral vasoconstriction--a new marker of obstructive sleep apnea. Sleep. 1999;22:939–946. [PubMed] [Google Scholar]
- 24.Lavie P, Schnall RP, Sheffy J, Shlitner A. Peripheral vasoconstriction during REM sleep detected by a new plethysmographic method. Nat Med. 2000;6:606. doi: 10.1038/76135. [DOI] [PubMed] [Google Scholar]
- 25.Bonetti PO, Barsness GW, Keelan PC, Schnell TI, Pumper GM, Kuvin JT, Schnall RP, Holmes DR, Higano ST, Lerman A. Enhanced external counterpulsation improves endothelial function in patients with symptomatic coronary artery disease. J Am Coll Cardiol. 2003;41:1761–1768. doi: 10.1016/s0735-1097(03)00329-2. [DOI] [PubMed] [Google Scholar]
- 26.Verma S, Buchanan MR, Anderson TJ. Endothelial Function Testing as a Biomarker of Vascular Disease. Circulation. 2003;108:2054–2059. doi: 10.1161/01.CIR.0000089191.72957.ED. [DOI] [PubMed] [Google Scholar]
- 27.Gerhard MD, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, Selwyn AP, Anderson TJ, Uehata A, Meredith IT. Close Relation of Endothelial Function in the Human Coronary and Peripheral Circulations. Journal of the American College of Cardiology. 1995;26:1235–1241. doi: 10.1016/0735-1097(95)00327-4. [DOI] [PubMed] [Google Scholar]
- 28.Cohn JN, Quyyumi AA, Hollenberg NK, Jamerson KA. Surrogate markers for cardiovascular disease: functional markers. Circulation. 2004;109:IV31–IV46. doi: 10.1161/01.CIR.0000133442.99186.39. [DOI] [PubMed] [Google Scholar]
- 29.Pauca AL, O'Rourke MF, Kon ND. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension. 2001;38:932–937. doi: 10.1161/hy1001.096106. [DOI] [PubMed] [Google Scholar]
- 30.Cook WW, Medley DM. Proposed hostility and pharisaic-virtue scales for the MMPI. J of Applied Psychology. 1954;38:414–418. [Google Scholar]
- 31.Speilberger C. Manual for the State-Trait Anger Expression Scale (STAXI) Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- 32.Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB., Jr The Cook-Medley hostility scale: item content and ability to predict survival. Psychosomatic medicine. 1989;51:46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Beck AT, Steer RA, Brown GK. BDI-II. Beck Depression Inventory: Second Edition. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 34.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 35.Carney RM, Rich MW, Tevelde A, Saini J, Clark K, Jaffe AS. Major depressive disorder in coronary artery disease. American Journal of Cardiology. 1987;60:1273–1275. doi: 10.1016/0002-9149(87)90607-2. [DOI] [PubMed] [Google Scholar]
- 36.Spielberger C, Gorsuch R. STAI Manual for the State-Trait Anxiety Inventory. Palo Alto, California: Consulting Psychologists Press Inc; 1970. [Google Scholar]
- 37.Jeter CR, Bush JP, Porter JH. Situational anxiety and blood pressure lability in the physician's office. Clin Exp Hypertens A. 1988;10:169–185. doi: 10.3109/10641968809046806. [DOI] [PubMed] [Google Scholar]
- 38.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 39.Canty-Mitchell J, Zimet GD. Psychometric properties of the Multidimensional Scale of Perceived Social Support in urban adolescents. Am J Community Psychol. 2000;28:391–400. doi: 10.1023/A:1005109522457. [DOI] [PubMed] [Google Scholar]
- 40.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. J Consult Clin Psychol. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- 41.Pretorius TB. Measuring life events in a sample of South African students: comparison of the Life Experiences Survey and the Schedule of Recent Experiences. Psychol Rep. 1998;83:771–780. doi: 10.2466/pr0.1998.83.3.771. [DOI] [PubMed] [Google Scholar]
- 42.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 43.Bremner JD, Bolus R, Mayer EA. Psychometric properties of the Early Trauma Inventory-Self Report. J Nerv Ment Dis. 2007;195:211–218. doi: 10.1097/01.nmd.0000243824.84651.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behavioral Research & Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 45.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology. 2008;76:272–281. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- 46.Sullivan K. Estimates of interrater reliability for the Logical Memory subtest of the Wechsler Memory Scale-Revised. J Clin Exp Neuropsychol. 1996;18:707–712. doi: 10.1080/01688639608408293. [DOI] [PubMed] [Google Scholar]
- 47.First MB, Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSMIV-Patient Edition (SCID-P) Washington, D.C.: American Psychiatric Press; 1995. [Google Scholar]
- 48.Wolpe J. The practice of behavior therapy. New York: New York Pergamon Press; 1969. [Google Scholar]
- 49.Burg MM, Meadows J, Shimbo D, Davidson KW, Schwartz JE, Soufer R. Confluence of depression and acute psychological stress among patients with stable coronary heart disease: effects on myocardial perfusion. J Am Heart Assoc. 2014;3 doi: 10.1161/JAHA.114.000898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arrighi JA, Burg M, Cohen IS, Soufer R. Simultaneous assessment of myocardial perfusion and function during mental stress in patients with chronic coronary artery disease. Journal of Nuclear Cardiology. 2003;10:267–274. doi: 10.1016/s1071-3581(02)43235-7. [DOI] [PubMed] [Google Scholar]
- 51.Akinboboye O, Krantz DS, Kop WJ, Schwartz SD, Levine J, Del Negro A, Karasik P, Berman DS, O'Callahan M, Ngai K, Gottdiener JS. Comparison of mental stress-induced myocardial ischemia in coronary artery disease patients with versus without left ventricular dysfunction. Am J Cardiol. 2005;95:322–326. doi: 10.1016/j.amjcard.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 52.Ramadan R, Quyyumi AA, Zafari AM, Binongo JN, Sheps DS. Myocardial ischemia and Angiotensin-converting enzyme inhibition: comparison of ischemia during mental and physical stress. Psychosomatic medicine. 2013;75:815–821. doi: 10.1097/PSY.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 53.Wawrzyniak AJ, Dilsizian V, Krantz DS, Harris KM, Smith MF, Shankovich A, Whittaker KS, Rodriguez GA, Gottdiener J, Li S, Kop W, Gottlieb SS. High Concordance Between Mental Stress-Induced and Adenosine-Induced Myocardial Ischemia Assessed Using SPECT in Heart Failure Patients: Hemodynamic and Biomarker Correlates. J Nucl Med. 2015;56:1527–1533. doi: 10.2967/jnumed.115.157990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goldberg AD, Becker LC, Bonsall R, Cohen JD, Ketterer MW, Kaufman PG, Krantz DS, Light KC, McMahon RP, Noreuil T, Pepine CJ, Raczynski J, Stone PH, Strother D, Taylor H, Sheps DS. Ischemic, hemodynamic, and neurohormonal responses to mental and exercise stress. Experience from the Psychophysiological Investigations of Myocardial Ischemia Study (PIMI) Circulation. 1996;94:2402–2409. doi: 10.1161/01.cir.94.10.2402. [DOI] [PubMed] [Google Scholar]
- 55.Stepanovic J, Ostojic M, Beleslin B, Vukovic O, Djordjevic-Dikic A, Giga V, Nedeljkovic I, Nedeljkovic M, Stojkovic S, Vukcevic V, Dobric M, Petrasinovic Z, Marinkovic J, Lecic-Tosevski D. Mental stress-induced ischemia in patients with coronary artery disease: echocardiographic characteristics and relation to exercise-induced ischemia. Psychosomatic Medicine. 2012;74:766–772. doi: 10.1097/PSY.0b013e3182689441. [DOI] [PubMed] [Google Scholar]
- 56.Holmes SD, Krantz DS, Kop WJ, Del Negro A, Karasik P, Gottdiener JS. Mental stress hemodynamic responses and myocardial ischemia: does left ventricular dysfunction alter these relationships? Psychosomatic medicine. 2007;69:495–500. doi: 10.1097/PSY.0b013e3180cabc73. [DOI] [PubMed] [Google Scholar]
- 57.Jain D, Shaker SM, Burg M, Wackers FJ, Soufer R, Zaret BL. Effects of mental stress on left ventricular and peripheral vascular performance in patients with coronary artery disease. J Am Coll Cardiol. 1998;31:1314–1322. doi: 10.1016/s0735-1097(98)00092-8. [DOI] [PubMed] [Google Scholar]
- 58.York KM, Hassan M, Li Q, Li H, Fillingim RB, Sheps DS. Coronary artery disease and depression: patients with more depressive symptoms have lower cardiovascular reactivity during laboratory-induced mental stress. Psychosomatic medicine. 2007;69:521–528. doi: 10.1097/PSY.0b013e3180cc2601. [DOI] [PubMed] [Google Scholar]
- 59.Jiang W, Samad Z, Boyle S, Becker RC, Williams R, Kuhn C, Ortel TL, Rogers J, Kuchibhatla M, O'Connor C, Velazquez EJ. Prevalence and clinical characteristics of mental stress-induced myocardial ischemia in patients with coronary heart disease. J Am Coll Cardiol. 2013;61:714–722. doi: 10.1016/j.jacc.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ramadan R, Sheps D, Esteves F, Zafari AM, Bremner JD, Vaccarino V, Quyyumi AA. Myocardial ischemia during mental stress: role of coronary artery disease burden and vasomotion. J Am Heart Assoc. 2013;2:e000321. doi: 10.1161/JAHA.113.000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ramachandruni S, Fillingim RB, McGorray SP, Schmalfuss CM, Cooper GR, Schofield RS, Sheps DS. Mental stress provokes ischemia in coronary artery disease subjects without exercise- or adenosine-induced ischemia. J Am Coll Cardiol. 2006;47:987–991. doi: 10.1016/j.jacc.2005.10.051. [DOI] [PubMed] [Google Scholar]
- 62.Schiffer F, Hartley LH, Schulman CL, Abelmann WH. Evidence for emotionally-induced coronary arterial spasm in patients with angina pectoris. Br Heart J. 1980;44:62–66. doi: 10.1136/hrt.44.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.L'Abbate A, Simonetti I, Carpeggiani C, Michelassi C. Coronary dynamics and mental arithmetic stress in humans. Circulation. 1991;83:II94–II99. [PubMed] [Google Scholar]
- 64.Miller PF, Light KC, Bragdon EE, Ballenger MN, Herbst MC, Maixner W, Hinderliter AL, Atkinson SS, Koch GG, Sheps DS. Beta-endorphin response to exercise and mental stress in patients with ischemic heart disease. J Psychosom Res. 1993;37:455–465. doi: 10.1016/0022-3999(93)90002-w. [DOI] [PubMed] [Google Scholar]
- 65.Cordero DL, Cagin NA, Natelson BH. Neurocardiology update: role of the nervous system in coronary vasomotion. Cardiovasc Res. 1995;29:319–328. [PubMed] [Google Scholar]
- 66.Yeung AC, Vekshtein VI, Krantz DS, Vita JA, Ryan TJ, Jr, Ganz P, Selwyn AP. The effect of atherosclerosis on the vasomotor response of coronary arteries to mental stress [see comments] N Engl J Med. 1991;325:1551–1556. doi: 10.1056/NEJM199111283252205. [DOI] [PubMed] [Google Scholar]
- 67.Burg MM, Graeber B, Vashist A, Collins D, Earley C, Liu J, Lampert R, Soufer R. Noninvasive detection of risk for emotion-provoked myocardial ischemia. Psychosomatic medicine. 2009;71:14–20. doi: 10.1097/PSY.0b013e318187c035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hassan M, York KM, Li H, Li Q, Lucey DG, Fillingim RB, Sheps DS. Usefulness of peripheral arterial tonometry in the detection of mental stress-induced myocardial ischemia. Clinical Cardiology. 2009;32:E1–E6. doi: 10.1002/clc.20515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anderson TJ, Uehata A, Gerhard MD, Meredith IT, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, Selwyn AP. Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol. 1995;26:1235–1241. doi: 10.1016/0735-1097(95)00327-4. [DOI] [PubMed] [Google Scholar]
- 70.Steg PG, Greenlaw N, Tendera M, Tardif JC, Ferrari R, Al-Zaibag M, Dorian P, Hu D, Shalnova S, Sokn FJ, Ford I, Fox KM. Prevalence of anginal symptoms and myocardial ischemia and their effect on clinical outcomes in outpatients with stable coronary artery disease: data from the International Observational CLARIFY Registry. JAMA Intern Med. 2014;174:1651–1659. doi: 10.1001/jamainternmed.2014.3773. [DOI] [PubMed] [Google Scholar]
- 71.Kim CK, Bartholomew BA, Mastin ST, Taasan VC, Carson KM, Sheps DS. Detection and reproducibility of mental stress-induced myocardial ischemia with Tc-99m sestamibi SPECT in normal and coronary artery disease populations. J Nucl Cardiol. 2003;10:56–62. doi: 10.1067/mnc.2003.26. [DOI] [PubMed] [Google Scholar]


