Abstract
Purpose
To describe imaging the external eye with crossed polarizers to enhance clinically important features in digital photographs of the eyelids.
Methods
External photographs with and without crossed polarizing filters were taken of patients with blepharitis and controls with no clinical eye pathology.
Results
Photographing eyelid skin through crossed polarizers decreased reflections on the skin surface and improved visualization of eyelid telangiectasias and blood vessels in patients with a broad range of skin pigmentation and ethnicities.
Conclusions
The use of crossed polarizers in imaging the external eye reduces reflections and glare from the eyelid skin and margins, thereby allowing for a more detailed evaluation of underlying structures and analysis of images. These findings suggest that including crossed polarizers in clinical photography has informative applications for assessing eyelid disease.
Keywords: conjunctiva, cornea, eyelids, imaging, cross-polarizers
INTRODUCTION
The use of polarized light for diagnostic imaging has been studied in dermatology1, pathology2, and ophthalmology3, 4, where it can reveal the reflectance, polarizing, depolarizing, and/or birefringence properties of tissues under study. In dermatology, polarization methods have been applied to a variety of conditions including pigmented and non-pigmented skin lesions5, skin malignancies6, photoaging7, and acne.8, 9 Photography using a polarizing filter parallel to the polarization of the light source (parallel polarizers) enhances superficial structures of the skin, while using a filter at cross-polarization to the light source (crossed polarizers) improves visualization of subsurface tissue structures.1 By reducing specular reflections from superficial epidermal tissue and skin surface lipids, imaging with crossed polarizers specifically enhances the assessment of blood vessels and chromophores in skin10, 11, thus improving assessments of pigmented lesions and vascular lesions10, 11, and reducing the impact of epidermal melanin.12
In ophthalmology, polarization manipulations have been applied to image various parts of the human eye, including the conjunctiva13, cornea13, 14, lens15, sclera13, and retinal nerve fiber layer.16 Because approximately 90% of the cornea is composed of parallel sheets of collagen fibers, the cornea behaves as a uniaxial birefringent or anisometropic medium.17 When imaged using crossed polarizers, a characteristic interference pattern develops, known as an “isogyre”, which was first described in 1941 by Cogan.18 The mechanism for the appearance of the corneal isogyre is due to a combination of the optical properties created by the curvature of the cornea and distribution of collagen fibrils.19 Briefly, light that is parallel or perpendicular to the corneal surface is not altered, whereas light that is oblique to the surface of the cornea is rotated and retarded, thereby appearing as a dark cross shape.19 Birefringence of the cornea is influenced by intraocular pressure(IOP) and corneal birefringence was once explored as a non-invasive measure of IOP but found to have limited utility.20
While the lens similarly produces an isogyre interference pattern17, its birefrigence is much weaker than that of the cornea.15 Scanning laser polarimetry utilizes the birefringence of the retinal nerve fiber layer to estimate its thickness.21 Polarization sensitive ocular coherence tomography (PS-OCT) can measure tissue birefringence and has been studied for several applications, including measuring scleral elasticity and retinal nerve fiber layer damage.22
In the present study, we used crossed polarizers to image the eyelids. We hypothesized that photography through cross-polarizers would reduce specular reflectance and glare and thus improve visualization of sub-epidermal structures and the vasculature of the eyelids.
MATERIALS AND METHODS
This study was approved by the University of Pennsylvania Institutional Review Board and complied with the Health Insurance Portability and Accountability Act. Informed consent was obtained from all subjects prior to participation, and the patients were photographed using the protocol described below (a modification of the Eyelid Photography Protocol previously published by our group).23 The use of polarized filters with an external camera is not registered as a device with the United States Food and Drug Administration for the diagnosis of external eye disease, and its use here should be considered investigational.
A Canon EOS Rebel T2i camera and external flash (Canon 600 EX-RT) were attached to a custom-made frame that screwed onto a monopod (Manofrotto 608B monopod with ball joint attachment) for stability. This arrangement enabled the external electronic flash to be aligned at a 45 degree angle downward towards the subject’s eye. The external flash was set to ETTL (exposure through the lens) mode, with 1/60s shutter speed. A Canon 100mm f/2.8L macro lens, attached to the camera, was set to manual focus at 0.34 meters and F22 aperture. The camera was connected via a USB cable to a laptop computer with Canon EOS Utility Software that permitted real-time viewing and management of the images.
Photographs were taken in examination rooms with fluorescent overhead lighting of approximately 320 lux. Photos of the eyelids were taken with the patient looking straight ahead, up, or down with gentle traction of the lids to allow full visualization of the eyelid margins. For each photo, the camera was positioned so the lens focused on the region of interest on the eyelid, with the camera re-positioned for each image.
For the polarized photographs, a circular polarizing filter (Heliopan ES 67mm SH PMC high transmission circular polarizer) was attached over the lens of the camera and an orthogonally oriented piece of TECHSPEC linear polarizing laminated film (Edmund Optics, Barrington, NJ, custom-cut to fit a filter holder) was placed over the external flash (Figure 1).
Figure 1.
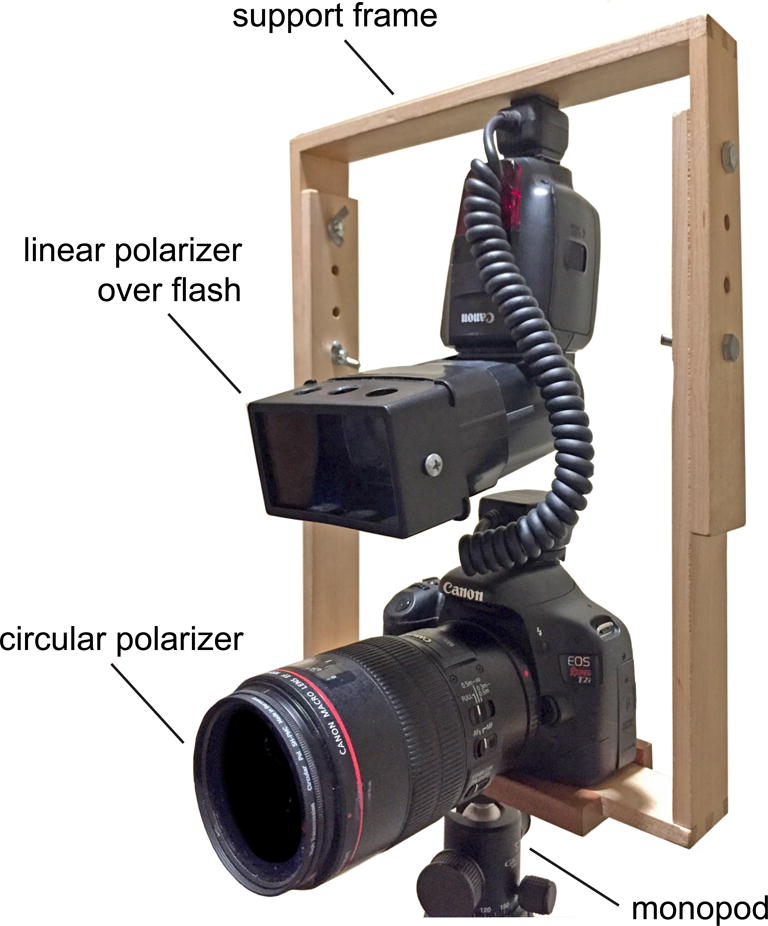
Camera set-up. The wooden frame was custom-made to hold the flash above the body of the camera, so that the flash could be angled down at an appropriate 45 degree angle. A linear polarizer was inserted over the flash and a circular polarizer over the camera lens for polarized images, and were removed for non-polarized images.
RESULTS
Polarized and non-polarized photos were taken of patients with blepharitis and controls with no clinical eyelid pathology. The novel observations here relate to improved visualization of eyelid blood vessels and telangiectasias. These observations are summarized in Table 1.
Table 1.
Summary of effects of crossed polarized imaging on eyelids and anterior segment
| Effect of crossed polarizers on image | |
|---|---|
| Eyelids | Enhanced visualization of blood vessels and telangiectasias of eyelid. Decreased reflections from skin surface. |
| Conjunctiva | Decreased reflections from conjunctival surface. |
| Cornea | Appearance of corneal isogyre. Decreased reflections from corneal surface. |
Eyelids
Eyelid photographs with crossed polarizers decreased reflections from the skin surface and revealed blood vessels and telangiectasias that were either poorly visualized or not visualized in the non-polarized photographs (Figure 2). Crossed polarizers improved the visualization of eyelid telangiectasias and vasculature for patients with a broad range of skin pigmentation and ethnicities.
Figure 2.
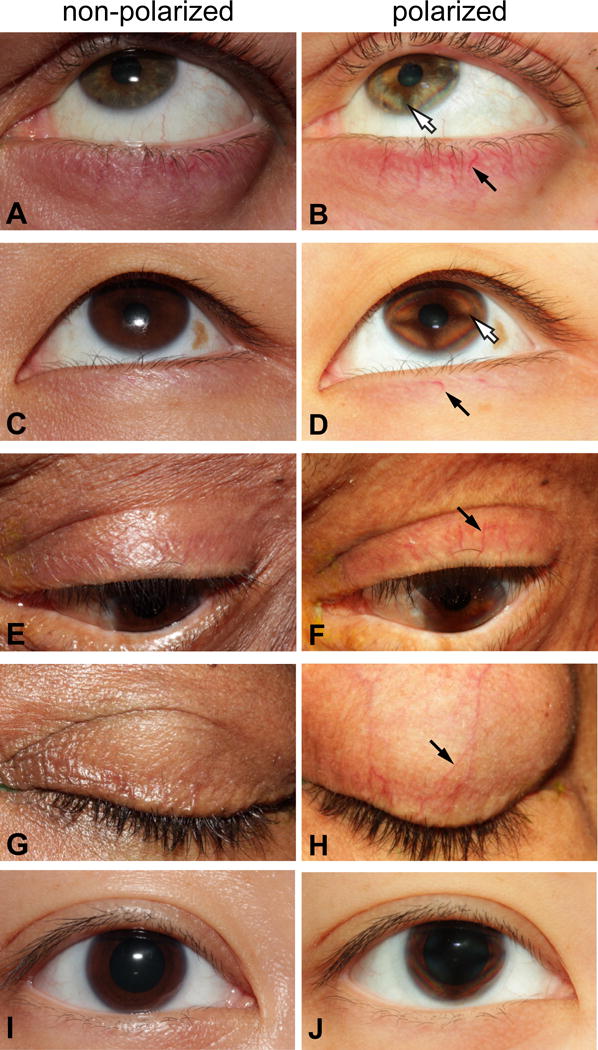
Non-polarized and cross-polarized eyelid photographs. Conventional, non-polarized images of the eyelids of patients with blepharitis (panels A, C, E, and G) and the corresponding images of the same eyes through crossed-polarizers (panels B, D, F, and H). The method is illustrated in patients with blepharitis of different races (A, B: Caucasian; C, D: South Asian; E, F: lightly pigmented African-American; G, H: more heavily pigmented African-American). The control subject (I and J) is Asian. Black arrows indicate a representative blood vessel in each patient that is made more visible with cross-polarizers. One patient (E,F) has a loose eyelash visible on the upper eyelid (not highlighted). White arrows in B, D indicate the typical isogyre when the cornea is visualized through crossed-polarizers. No adjustments were made to any of the images other than the insertion of arrows and labeling.
Cornea and conjunctiva
Use of crossed polarizers revealed the typical isogyre in the cornea (Figures 2B, 2D). As previously described13, 14, photographs through crossed polarizers decreased reflections from the corneal and conjunctival surfaces (Figure 2).
DISCUSSION
The use of crossed polarizers in imaging the external eye reduces reflections and glare from the eyelid skin and margins, as well as from conjunctival and corneal surfaces.13 Polarized digital images using commercially available photography equipment can be easily acquired in many clinical settings. The isogyre in cornea can confirm the correct orthogonal orientation of the two polarizing filters13, when the cornea is fully visible in the image.
For the eyelids, photography through crossed polarizers improves visualization of telangiectasias beneath the skin and lid margins that were not readily visible in non-polarized images. Importantly, this method improves vascular visualization in subjects with both lightly and heavily pigmented skin, suggesting potentially useful applications.
For example, polarized photography could be useful for diagnosis and research in eyelid diseases such as blepharitis and meibomian gland dysfunction (MGD). While the enhancement of vessels in rosacea of the skin1 and other disorders6 has been described in the dermatology literature, we are not aware of prior reports describing the utility of cross-polarizing filters for imaging the eyelids. Blepharitis and MGD are under-diagnosed in ophthalmology, particularly in patients with heavily pigmented skin24; and patients often present with non-specific signs or symptoms.25 Earlier clinical diagnosis of blepharitis and MGD, along with improved research end-points, could result from the application of cross-polarization imaging.
While reduction of corneal and conjunctival surface reflections from photography with crossed polarizers has been described previously13, this imaging technique has not been extensively applied to investigating conjunctival or corneal disease. Besides potential use in diagnosing eyelid pathology, removing reflections could improve the accuracy of objective assessment algorithms now being developed to quantify redness or other biomarkers from digital conjunctival and corneal photographs.
Acknowledgments
We would like to thank Dominique Caggiano and Trenton Rivera for their assistance in obtaining the photograph used for Figure 1.
Funding:
This work was supported by National Eye Institute grants K12 EY015398 (VYB) and core grant P30 EY001583, the Paul and Evanina Bell Mackall Foundation Trust (RAS), and an unrestricted grant from Research to Prevent Blindness (VYB, MMG, RAS).
Footnotes
Conflict of Interest Statement:
The Eyelid Photography Protocol is copyright-protected by the University of Pennsylvania. Use of the protocol in investigational studies sponsored in whole or part by for-profit entities or for commercial purposes by any entities is prohibited without the express written consent of the University of Pennsylvania. The authors retain intellectual rights to the photography protocol for the possibility of future licensing (VYB, DHB, MMG, WCN, MGM, RAS).
Disclosures not relevant to submitted work: Dr. Massaro-Giordano owns stock in Physician Recommended Nutriceuticals. Dr. Stone received an honorarium from Santen, Inc., in 2016 for a seminar and travel expenses; and is co-inventor on 3 patents licensed to EyeIC but does not receive any royalties.
References
- 1.Anderson RR. Polarized light examination and photography of the skin. Arch Dermatol. 1991;127:1000–5. [PubMed] [Google Scholar]
- 2.Yaroslavsky AN, Neel V, Anderson RR. Demarcation of nonmelanoma skin cancer margins in thick excisions using multispectral polarized light imaging. J Invest Dermatol. 2003;121:259–66. doi: 10.1046/j.1523-1747.2003.12372.x. [DOI] [PubMed] [Google Scholar]
- 3.Gotzinger E, Pircher M, Dejaco-Ruhswurm I, et al. Imaging of birefringent properties of keratoconus corneas by polarization-sensitive optical coherence tomography. Invest Ophthalmol Vis Sci. 2007;48:3551–8. doi: 10.1167/iovs.06-0727. [DOI] [PubMed] [Google Scholar]
- 4.Weinreb RN, Bowd C, Zangwill LM. Glaucoma detection using scanning laser polarimetry with variable corneal polarization compensation. Arch Ophthalmol. 2003;121:218–24. doi: 10.1001/archopht.121.2.218. [DOI] [PubMed] [Google Scholar]
- 5.Benvenuto-Andrade C, Dusza SW, Agero AL, et al. Differences between polarized light dermoscopy and immersion contact dermoscopy for the evaluation of skin lesions. Arch Dermatol. 2007;143:329–38. doi: 10.1001/archderm.143.3.329. [DOI] [PubMed] [Google Scholar]
- 6.Jacques SL, Ramella-Roman JC, Lee K. Imaging skin pathology with polarized light. J Biomed Opt. 2002;7:329–40. doi: 10.1117/1.1484498. [DOI] [PubMed] [Google Scholar]
- 7.Muccini JA, Kollias N, Phillips SB, et al. Polarized light photography in the evaluation of photoaging. J Am Acad Dermatol. 1995;33:765–9. doi: 10.1016/0190-9622(95)91813-2. [DOI] [PubMed] [Google Scholar]
- 8.Rizova E, Kligman A. New photographic techniques for clinical evaluation of acne. J Eur Acad Dermatol Venereol. 2001;15(Suppl 3):13–8. doi: 10.1046/j.1468-3083.15.s.3.1.x. [DOI] [PubMed] [Google Scholar]
- 9.Phillips SB, Kollias N, Gillies R, et al. Polarized light photography enhances visualization of inflammatory lesions of acne vulgaris. J Am Acad Dermatol. 1997;37:948–52. doi: 10.1016/s0190-9622(97)70070-7. [DOI] [PubMed] [Google Scholar]
- 10.Jung B, Choi B, Durkin AJ, et al. Characterization of port wine stain skin erythema and melanin content using cross-polarized diffuse reflectance imaging. Lasers Surg Med. 2004;34:174–81. doi: 10.1002/lsm.10242. [DOI] [PubMed] [Google Scholar]
- 11.Kang H, Jung B, Nelson JS. Polarization color imaging system for on-line quantitative evaluation of facial skin lesions. Dermatol Surg. 2007;33:1350–6. doi: 10.1111/j.1524-4725.2007.33288.x. [DOI] [PubMed] [Google Scholar]
- 12.Jung B, Kim CS, Choi B, et al. Use of erythema index imaging for systematic analysis of port wine stain skin response to laser therapy. Lasers Surg Med. 2005;37:186–91. doi: 10.1002/lsm.20218. [DOI] [PubMed] [Google Scholar]
- 13.Fariza E, O’Day T, Jalkh AE, Medina A. Use of cross-polarized light in anterior segment photography. Arch Ophthalmol. 1989;107:608–10. doi: 10.1001/archopht.1989.01070010622044. [DOI] [PubMed] [Google Scholar]
- 14.Stanworth A, Naylor EJ. The polarization optics of the isolated cornea. Br J Ophthalmol. 1950;34:201–11. doi: 10.1136/bjo.34.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bueno JM, Campbell MC. Polarization properties of the in vitro old human crystalline lens. Ophthalmic Physiol Opt. 2003;23:109–18. doi: 10.1046/j.1475-1313.2003.00095.x. [DOI] [PubMed] [Google Scholar]
- 16.Weinreb RN, Shakiba S, Zangwill L. Scanning laser polarimetry to measure the nerve fiber layer of normal and glaucomatous eyes. Am J Ophthalmol. 1995;119:627–36. doi: 10.1016/s0002-9394(14)70221-1. [DOI] [PubMed] [Google Scholar]
- 17.Pierscionek BK. Explanation of isogyre formation by the eye lens. Ophthalmic Physiol Opt. 1993;13:91–4. doi: 10.1111/j.1475-1313.1993.tb00431.x. [DOI] [PubMed] [Google Scholar]
- 18.Cogan D. Some ocular phenomena produced with polarized light. Arch Ophthalmol. 1941;25:391–400. [Google Scholar]
- 19.Cope WT, Wolbarsht ML, Yamanashi BS. The corneal polarization cross. J Opt Soc Am. 1978;68:1139–41. doi: 10.1364/josa.68.001139. [DOI] [PubMed] [Google Scholar]
- 20.Stanworth A. Polarized light studies of the cornea II: the effect of intra-ocular pressure. J Exp Biol. 1953;30:164–9. [Google Scholar]
- 21.Greenfield DS, Knighton RW, Huang XR. Effect of corneal polarization axis on assessment of retinal nerve fiber layer thickness by scanning laser polarimetry. Am J Ophthalmol. 2000;129:715–22. doi: 10.1016/s0002-9394(00)00353-6. [DOI] [PubMed] [Google Scholar]
- 22.Pircher M, Hitzenberger CK, Schmidt-Erfurth U. Polarization sensitive optical coherence tomography in the human eye. Prog Retin Eye Res. 2011;30:431–51. doi: 10.1016/j.preteyeres.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bunya VY, Brainard DH, Daniel E, et al. Assessment of signs of anterior blepharitis using standardized color photographs. Cornea. 2013;32:1475–82. doi: 10.1097/ICO.0b013e3182a02e0e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Browning DJ, Rosenwasser G, Lugo M. Ocular rosacea in blacks. Am J Ophthalmol. 1986;101:441–4. doi: 10.1016/0002-9394(86)90644-6. [DOI] [PubMed] [Google Scholar]
- 25.Nichols KK, Foulks GN, Bron AJ, et al. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011;52:1922–9. doi: 10.1167/iovs.10-6997a. [DOI] [PMC free article] [PubMed] [Google Scholar]


