Abstract
The objective of the present research was to examine the association between lifetime cannabis use disorder (CUD), current suicidal ideation, and lifetime history of suicide attempts in a large and diverse sample of Iraq/Afghanistan-era veterans (N = 3,233) using a battery of well-validated instruments. As expected, CUD was associated with both current suicidal ideation (OR = 1.683, p = 0.008) and lifetime suicide attempts (OR = 2.306, p < 0.0001), even after accounting for the effects of sex, posttraumatic stress disorder, depression, alcohol use disorder, non-cannabis drug use disorder, history of childhood sexual abuse, and combat exposure. Thus, the findings from the present study suggest that CUD may be a unique predictor of suicide attempts among Iraq/Afghanistan-era veterans; however, a significant limitation of the present study was its cross-sectional design. Prospective research aimed at understanding the complex relationship between CUD, mental health problems, and suicidal behavior among veterans is clearly needed at the present time.
Keywords: suicide, suicide attempts, suicidal ideation, cannabis, marijuana, substance abuse, depression, posttraumatic stress disorder
Introduction
It is estimated that between 125 and 227 million people use cannabis worldwide, making it the most widely used illicit drug in the world (United Nations, 2014; Hoch et al., 2015). Indeed, nearly 20 million Americans report that they have used cannabis in the past month (i.e., 7.5% of Americans 12 years or older; SAMHSA, 2014). Moreover, heavy cannabis use (i.e., cannabis use on 20 or more days during the past month) increased by nearly 60% in the U.S. from 2007 to 2013 (SAMHSA, 2014). Such findings are important because cannabis use has been associated with a wide range of health problems (e.g., Goldman et al., 2010; Joshi et al., 2014). To date, however, there has been only limited attention paid to the relationship between cannabis use and suicidal behavior.
A recent review and meta-analysis (Borges et al., 2016) on cannabis use and suicidal behavior (i.e., suicidal ideation and attempts) identified five studies examining the association between suicidal ideation and heavy cannabis use and six studies examining the association between suicide attempts and heavy cannabis use. Meta-analysis indicated that heavy cannabis use was likely to be associated with both suicidal ideation (OR = 2.53, 95% CI: 1.00 – 6.39) and suicide attempts (OR = 3.20, 95% CI: 1.72 – 5.94); however, the authors of this review noted the limited number of studies examined as well as several key issues to be addressed in future research, such as inclusion of more diverse samples, inclusion of patients with and without comorbid mental disorders, and use of clinical interviews to diagnose cannabis use disorders (CUD). Borges et al. (2016) also noted the importance of accounting for the effects of key risk factors (e.g., depression, other drug use problems, and alcohol misuse) that are likely to be associated with both cannabis use and suicidal behavior in statistical analyses.
Cannabis Use and Suicidal Behavior in Veterans
Death by suicide and suicidal behavior are major concerns among veterans at the present time [Bullman and Kang, 1994; DeBeer et al., 2014; Kang and Bullman, 2008; Kaplan, Huguet, McFarland, & Newsom, 2007; Kimbrel et al., 2014, 2015, 2016a, 2016b; U.S. Department of Veterans Affairs (VA), 2016]. Indeed, the most recent statistics available from the Department of Veterans Affairs (2016) suggest that approximately 20 veterans die by suicide each day in the United States. Considerable evidence suggests that veterans with mental health disorders, such as PTSD and depression, are at particularly high risk for suicidal behavior and death by suicide (Bullman and Kang, 1994; DeBeer et al., 2014; Kang and Bullman, 2008; Kaplan et al., 2007; Kimbrel et al., 2014, 2016a; VA, 2016); however, there has been only limited research on the association between CUD and suicidal behavior among veterans to date. In fact, we are aware of only one other study that has examined the association between CUD and suicide attempts in veterans. Specifically, Kimbrel and colleagues (in press) recently reported that CUD was significantly associated with suicide attempts (OR=3.10, p=0.045) in a sample of 292 Iraq/Afghanistan-era veterans after adjusting for a wide range of covariates, including PTSD, depression, alcohol use disorder, and non-cannabis drug use disorder. This finding is highly consistent with prior research among civilians (e.g., Borges et al., 2016) and suggests that CUD may also increase veterans’ risk for self-injurious behavior; however, this finding has not yet been replicated in an independent sample of veterans.
Study Objective and Hypothesis
The objective of the present study was to attempt to replicate Kimbrel and colleagues’ (in press) recent finding that lifetime CUD is associated with increased risk for suicidal behavior in a large and diverse sample of Iraq/Afghanistan-era veterans. Consistent with the findings of Borges et al. (2016) and Kimbrel et al. (in press), we hypothesized that CUD would be significantly associated with both current suicidal ideation and lifetime history of suicide attempts in this sample of Iraq/Afghanistan-era veterans, even after accounting for established predictors of suicidal behavior among veterans, including sex, PTSD, depression, alcohol use disorder, non-cannabis drug use disorder, history of childhood sexual abuse, and combat exposure (Ashrafioun et al., 2016; Kimbrel et al., 2014, 2015, 2016a, 2016b, in press; Maguen et al., 2015).
Materials and Methods
Participants and Procedures
Participants included 3,233 Iraq/Afghanistan-era veterans who took part in a cross-sectional, multi-site study conducted by the Department of Veterans Affairs’ (VA) VISN 6 Mid-Atlantic Mental Illness, Research, Education and Clinic Center (MIRECC). Procedures for this study have been fully described elsewhere (Ashley-Koch et al., 2015; Calhoun et al., 2008; Guerra et al., 2011; Kimbrel et al., 2014). To be eligible for the study, participants had to have served in the United States military after September 11, 2001. Recruitment for this study began in 2005 and is ongoing. Most (78.7%; n = 2,544), but not all, participants reported deployments to one or more warzones. The most common warzone participants had been deployed to was Iraq (59.3%; n = 1918). On average, participants had been deployed 1.5 (SD = 1.3) times during their military service. The vast majority of participants (~90%) were enrolled at one of the four VA Medical Centers. The study protocol was approved by the local institutional review boards at each participating site. All participants provided written informed consent prior to enrollment. Study procedures primarily involved completion of a clinical interview and a battery of self-report questionnaires. Sample characteristics are provided in Table 1.
Table 1.
Participant Characteristics
| % | N | ||
|---|---|---|---|
| Gender | |||
| Male | 79.7% | 2,577 | |
| Female | 20.3% | 655 | |
| Race | |||
| White | 48.7% | 1575 | |
| Black | 48.3% | 1560 | |
| American Indian | 2.1% | 68 | |
| Asian | 1.3% | 43 | |
| Pacific Islander | 0.5% | 17 | |
| Ethnicity | |||
| Non-Hispanic | 93.1% | 3011 | |
| Hispanic | 5.2% | 168 | |
| Deployment History | |||
| Iraq | 59.3% | 1918 | |
| Kuwait | 29.1% | 942 | |
| Afghanistan | 17.3% | 559 | |
| Diagnostic History | |||
| Lifetime Depression | 37.6% | 1215 | |
| Lifetime Alcohol Use Disorder | 36.6% | 1182 | |
| Lifetime Posttraumatic Stress Disorder | 36.4% | 1176 | |
| Lifetime Cannabis Use Disorder | 9.9% | 320 | |
| Lifetime Non-Cannabis Drug Use Disorder | 5.8% | 186 | |
| Suicidal Behavior | |||
| Current Suicidal Ideation (BSS ≥ 3) | 9.9% | 320 | |
| Lifetime Suicide Attempt | 9.0% | 292 |
Measures
The Structured Clinical Interview for DSM-IV Disorders (SCID; First et al., 1994) was used to diagnose lifetime psychiatric disorders based on DSM-IV criteria. The present analyses focused on lifetime psychiatric diagnoses because of our interest in lifetime history of suicide attempts. All study interviewers received extensive training as well as on-going supervision from experienced clinicians. Reliability was excellent (Fleiss’ kappa = 0.95) among study interviewers when scoring a series of seven SCID-based training videos. Substance dependence and abuse diagnoses were combined into a single substance use disorder variable for each substance. Thus, participants who met criteria for either cannabis dependence or cannabis abuse were coded as “1,” whereas participants who had never met criteria for either disorder were categorized as “0.” Alcohol and non-cannabis drug use disorders were coded similarly. History of childhood sexual abuse was assessed with the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000). Combat exposure was assessed with the Combat Exposure Scale (CES; Keane et al., 1989). Current suicidal ideation and lifetime history of suicide attempts were assessed with the Beck Scale for Suicide Ideation (BSS; Beck & Steer, 1991), which has demonstrated reliability and validity in previous research (Brown et al., 2000), including studies of suicidal behavior in Iraq/Afghanistan-era veterans (DeBeer et al., 2014; Guerra et al., 2011; Kimbrel et al., 2014). Scores of 3 or higher on the BSS have been prospectively associated with increased risk for death by suicide (Brown et al., 2000). Therefore, scores of 3 or more on the BSS were operationalized as a clinically significant level of current suicidal ideation and were scored as “1”, whereas scores of 0-2 were scored as “0”, reflecting an absence of clinically significant ideation at the time of the assessment. Suicide attempts were also dichotomized such that a lifetime history of 1 or more suicide attempts was coded as “1”, whereas no lifetime history of suicide attempts was coded as “0”.
Data Analysis Plan
Chi-square tests were used to examine bivariate associations between CUD and suicidal behavior (i.e., current suicidal ideation and lifetime suicide attempts). Logistic regression was used to assess the relationship between lifetime history of CUD and suicidal behavior. Both adjusted and unadjusted models were conducted. Sex (male=0; female=1), lifetime PTSD (not present = 0; present = 1), lifetime depression (not present = 0; present = 1), lifetime alcohol use disorder (not present = 0; present = 1), lifetime non-cannabis drug use disorder (not present = 0; present = 1), history of childhood sexual abuse (not present = 0; present = 1), and combat exposure (continuous) were included in the adjusted models based on prior research demonstrating significant associations between these variables and suicidal behavior in veterans (e.g., Ashrafioun et al., 2016; Kimbrel et al., 2014, 2015, 2016a, 2016b; Maguen et al., 2015).
Results
CUD was significantly associated with both current suicidal ideation [χ2(1)=14.695, p <0.001] and lifetime history of suicide attempts [χ2(1)=45.053, p <0.001] at the bivariate level (Figure 1). Unadjusted logistic regression models revealed that veterans with a lifetime history of CUD had 1.921 times the odds (95% CI: 1.369–2.696) of endorsing current suicidal ideation and 2.831 times the odds (95% CI: 2.065–3.881) of having made a suicide attempt compared to veterans with no lifetime history of CUD. After adjusting for sex, PTSD, depression, alcohol use disorder, non-cannabis drug use disorder, history of childhood sexual abuse, and combat exposure (Table 1), CUD continued to be significantly associated with current suicidal ideation (OR = 1.683, 95% CI: 1.149–2.464, p = 0.008) and lifetime suicide attempts (OR = 2.306, 95% CI: 1.591–3.343, p < 0.0001).
Figure 1.
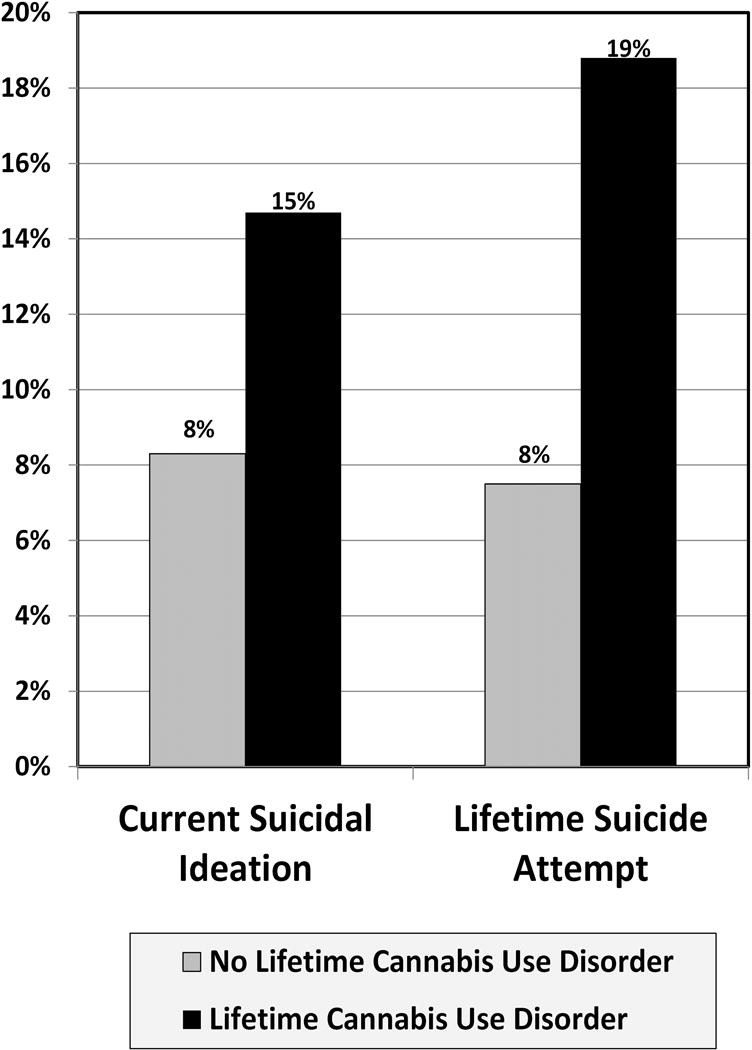
Bivariate Association between Lifetime Cannabis Use Disorder and Current Suicidal Ideation and Lifetime History of Suicide Attempts.
Discussion
According to Bonn-Miller and colleagues (2012), rates of CUD diagnoses have increased by more than 50% among veterans receiving care from the Veterans Affairs (VA) Health Care System between 2002 and 2009. Such findings are critically important, as the present research provided further evidence that CUD may be a unique predictor of suicide attempts among veterans. Importantly, the present research begins to address some of the limitations in the extant literature by examining a large and diverse group of veterans with a relatively high rate of current suicidal ideation (9.9%) and lifetime history of suicide attempts (9.0%). An additional strength of the present study was the use of diagnostic interviews to assess CUD as well as relevant comorbid disorders that might also influence veterans’ risk for suicidal behavior, including PTSD, depression, alcohol use disorder, and non-cannabis drug use disorders.
As noted by Borges and colleagues (2016), few studies have evaluated the relationship between cannabis abuse/dependence and suicide attempts (e.g., Bovasso, 2001; Beautrais et al., 1999). Moreover, there has been only one previous study of CUD and suicide attempts among veterans (Kimbrel et al., in press), despite the fact that veterans are known to be at elevated risk for suicidal behavior (e.g., U.S. Department of Veterans Affairs, 2016). Consistent with prior research (e.g., Borges et al., 2016; Kimbrel et al., in press), the findings from the present study suggest that CUD may be a unique predictor of suicide attempts among veterans, even after a wide array of relevant covariates are considered.
Clinical Implications
The present findings have a number of implications for clinicians who work with veterans, as cannabis use is strongly associated with mental health problems within this population (Boden et al., 2013; Cheung et al., 2010; Hall et al., 2004). For example, Boden and colleagues (2013) found that psychiatric symptoms (e.g., PTSD, depression, anxiety, insomnia) were the most common reason that veterans provided for using cannabis. Moreover, medicinal use of cannabis has been legalized in many U.S. states, with multiple states listing PTSD as an approved condition. Paradoxically, the present findings suggest the possibility that chronic cannabis use could actually increase risk for suicidal behavior among veterans with mental health problems, a group known to already be at elevated risk (e.g., Bullman and Kang, 1994; Kimbrel et al., 2014, 2016a; U.S. Department of Veterans Affairs, 2016). Unfortunately, due to the cross-sectional nature of the present findings, we are only able to speculate on this important issue at the present time. Thus, further research is needed to determine if CUD prospectively predicts suicide attempts among veterans above and beyond the risks associated with other types of psychiatric disorders. One particularly interesting approach to collecting this type of data would involve collecting data on suicidal behavior before, during, and after CUD treatment to determine if successfully quitting cannabis leads to clinically meaningful reductions in suicidal ideation and suicide attempts during long-term follow-ups. Additional research aimed at increasing understanding of the potential mechanisms through which CUD might increase veterans’ risk for suicidal behavior is also needed at the present time.
Study Limitations
Although the present sample was relatively large (N = 3,233), even larger sample sizes are optimal for research on behaviors as rare as suicide attempts. In addition, because the sample was a convenience sample of Iraq/Afghanistan veterans that was not randomly selected from the larger population, the present findings may not generalize to the larger population of Iraq/Afghanistan-era veterans or to veterans from other eras. Finally, the most significant limitations of the present research were use of a cross-sectional design and failure to assess the specific dates of participants’ lifetime suicide attempts. As a result of these study limitations, we were unable to determine if the onset of CUD temporally preceded veterans’ suicide attempts.
Conclusions
In sum, the findings from the present study suggest that CUD may be uniquely associated with suicide attempts in veterans, even after a wide array of relevant covariates are considered. This finding is highly significant given the high rate of suicidal behavior observed among veterans with mental health disorders as well as the increasing rate of CUD observed among veterans in recent years. Additional research aimed at understanding the complex relationship between CUD, other mental health problems, and suicidal behavior is needed at the present time.
Supplementary Material
Table 2.
Summary of the Adjusted Logistic Regression Models Predicting Suicidal Behavior
| Variable | Current Suicidal Ideation (n = 320) | |
|---|---|---|
| Odds Ratio | 95% Confidence Intervals | |
| Sex | 0.88 | 0.60 – 1.26 |
| Lifetime PTSD | 2.08*** | 1.50 – 2.89 |
| Lifetime Depression | 2.80*** | 2.06 – 3.80 |
| Lifetime Alcohol Use Disorder | 1.30 | 0.98 – 1.73 |
| Lifetime Non-Cannabis Drug Use Disorder | 0.95 | 0.59 – 1.53 |
| Lifetime History of Childhood Sexual Abuse | 1.94*** | 1.35 – 2.78 |
| Lifetime History of Combat Exposure | 1.03*** | 1.02 – 1.04 |
| Lifetime History of Cannabis Use Disorder | 1.68** | 1.15 – 2.46 |
|
| ||
| Variable | Lifetime Suicide Attempt (n = 292) | |
| Odds Ratio | 95% Confidence Intervals | |
|
| ||
| Sex | 2.15*** | 1.53 – 3.02 |
| Lifetime PTSD | 2.60*** | 1.87 – 3.61 |
| Lifetime Depression | 2.48*** | 1.82 – 3.38 |
| Lifetime Alcohol Use Disorder | 1.45* | 1.07 – 1.97 |
| Lifetime Non-Cannabis Drug Use Disorder | 2.28*** | 1.50 – 3.48 |
| Lifetime History of Childhood Sexual Abuse | 2.64*** | 1.90 – 3.67 |
| Lifetime History of Combat Exposure | 1.00 | 0.99 – 1.01 |
| Lifetime History of Cannabis Use Disorder | 2.31*** | 1.59 – 3.34 |
Note: PTSD = posttraumatic stress disorder. Sex coded as 0 = male, 1 = female.
p < 0.05;
p < 0.01;
p < 0.001.
Acknowledgments
Role of the Funding Source
This project was supported in part by the Department of Veterans Affairs’ (VA) Mid-Atlantic Mental Illness Research, Education and Clinical Center (MIRECC) of the VA Office of Mental Health Services, the VA VISN 6 Mid-Atlantic Healthcare Network, and the Research and Development and Mental Health Services of the Durham VA Medical Center. Drs. Kimbrel and Dedert were supported by Career Development Awards #IK2CX000525 and #IK2CX000718, respectively, from the Clinical Science Research and Development (CSR&D) Service of the VA Office of Research and Development (ORD). Drs. Van Voorhees and Naylor were supported by Career Development Awards #5IK2RX001298 and #1lK2RX000908, respectively, from the Rehabilitation Research and Development (RR&D) of the VA Office of Research and Development (ORD). Dr. Beckham was supported by a Research Career Scientist Award (#11S-RCS-009) from CSR&D. VA CSR&D and RR&D played no role in study design, data collection, data analysis, manuscript preparation, or the decision to submit this article for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government.
The VA Mid-Atlantic Mental Illness Research, Education, and Clinical Center Workgroup includes John A. Fairbank, Kimberly T. Green, Robin A. Hurley, Angela C. Kirby, Jason D. Kilts, Christine E. Marx, Gregory McCarthy, Scott D. McDonald, Marinell Miller-Mumford, Scott D. Moore, Rajendra A. Morey, Treven C. Pickett, Jared Rowland, Jennifer J. Runnals, Cindy Swinkels, Steven T. Szabo, Katherine H. Taber, Larry A. Tupler, Richard D. Weiner, and Ruth Yoash-Gantz.
References
- Ashley-Koch AE, Garrett ME, Gibson J, Liu Y, Dennis MF, Kimbrel NA, VA Mid-Atlantic MIRECC Workgroup. Beckham JC, Hauser MA. Genome-wide association study of posttraumatic stress disorder in a cohort of Iraq-Afghanistan-era veterans. Journal of Affective Disorders. 2015;184:225–234. doi: 10.1016/j.jad.2015.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashrafioun L, Pigeon WR, Conner KR, Leong SH, Oslin DW. Prevalence and correlates of suicidal ideation and suicide attempts among veterans in primary care referred for a mental health evaluation. J Affect Disord. 2016;189:344–350. doi: 10.1016/j.jad.2015.09.014. [DOI] [PubMed] [Google Scholar]
- Beautrais AL, Joyce PR, Mulder RT. Cannabis abuse and serious suicide attempts. Addiction. 1999;94(8):1155–1164. doi: 10.1046/j.1360-0443.1999.94811555.x. [DOI] [PubMed] [Google Scholar]
- Boden MT, Babson KA, Vujanovic AA, Short NA, Bonn-Miller MO. Posttraumatic stress disorder and cannabis use characteristics among military veterans with cannabis dependence. Am J Addict. 2013;22:277–284. doi: 10.1111/j.1521-0391.2012.12018.x. [DOI] [PubMed] [Google Scholar]
- Bovasso GB. Cannabis abuse as a risk factor for depressive symptoms. Am J Psychiatry. 2001;158:2033–2037. doi: 10.1176/appi.ajp.158.12.2033. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Harris AH, Trafton JA. Prevalence of cannabis use disorder diagnoses among veterans in 2002–2008 and 2009. Psychol Serv. 2012;9:404–416. doi: 10.1037/a0027622. [DOI] [PubMed] [Google Scholar]
- Borges G, Bagge CL, Orozco R. A literature review and meta-analyses of cannabis use and suicidality. J Affect Disord. 2016;195:63–74. doi: 10.1016/j.jad.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J Consult Clin Psychol. 2000;68(3):371–377. [PubMed] [Google Scholar]
- Bullman TA, Kang HK. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. J Nerv Ment Dis. 1994;182:604–610. doi: 10.1097/00005053-199411000-00002. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, McDonald SD, Guerra VS, Eggleston AM, Beckham JC, Straits-Troster K, Mid-Atlantic OEF/OIF Registry Workgroup Clinical utility of the Primary Care – PTSD Screen among U.S. veterans who served since September 11, 2001. Psychiatry Research. 2008;178(2):330–335. doi: 10.1016/j.psychres.2009.11.009. [DOI] [PubMed] [Google Scholar]
- Cheung JT, Mann RE, Ialomiteanu A, Stoduto G, Chan V, Ala-Leppilampi K, Rehm J. Anxiety and mood disorders and cannabis use. Am J Drug Alcohol Abuse. 2010;36:118–122. doi: 10.3109/00952991003713784. [DOI] [PubMed] [Google Scholar]
- DeBeer BB, Kimbrel NA, Meyer EC, Gulliver SB, Morissette SB. Combined posttraumatic stress (PTSD) and depressive symptoms interact with social support to predict suicidal ideation in Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) veterans. Psychiatry Res. 2014;216:357–362. doi: 10.1016/j.psychres.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structural Clinical Interview for Axis I DSM-IV Disorders. 2nd. Biometrics Research Department; New York, NY: 1994. [Google Scholar]
- Goldman M, Suh JJ, Lynch KG, Szucs R, Ross J, Hu X, O’Brien CP, Oslin DW. Identifying risk factors for marijuana use among veterans affairs patients. J Addict Med. 2010;4:47–51. doi: 10.1097/ADM.0b013e3181b18782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra VS, Calhoun PS, Mid-Atlantic Mental Illness Research, Education and Clinical Center Workgroup Examining the relation between posttraumatic stress disorder and suicidal ideation in an OEF/OIF veteran sample. Journal of Anxiety Disorders. 2011;25(1):12–18. doi: 10.1016/j.janxdis.2010.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Degenhardt L, Teesson M. Cannabis use and psychotic disorders: An update. Drug Alcohol Rev. 2004;23:433–443. doi: 10.1080/09595230412331324554. [DOI] [PubMed] [Google Scholar]
- Hoch E, Bonnet U, Thomasius R, Ganzer F, Havemann-Reinecke U, Preuss UW. Risks associated with the non-medicinal use of cannabis. Dtsch Arztebl Int 2015. 2015;112:271–8. doi: 10.3238/arztebl.2015.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi M, Joshi A, Bartter T. Marijuana and lung diseases. Curr Opin Pulm Med. 2014;20:173–179. doi: 10.1097/MCP.0000000000000026. [DOI] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Risk of suicide among US veterans after returning from the Iraq or Afghanistan war zones. JAMA. 2008;300:652–653. doi: 10.1001/jama.300.6.652. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, McFarland BH, Newsom JT. Suicide among male veterans: A prospective population-based study. J Epidemiol Commun H. 2007;61:619–624. doi: 10.1136/jech.2006.054346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical Evaluation of a Measure to Assess Combat Exposure. Psychol Assess. 1989;1(1):53–55. [Google Scholar]
- Kimbrel NA, Calhoun PS, Elbogen EB, Brancu M, MIRECC 6 Registry Workgroup. Beckham JC. The factor structure of psychiatric comorbidity among Iraq/Afghanistan veterans and its relationship to violence, incarceration, suicide attempts, and suicidality. Psychiatry Res. 2014;220:397–403. doi: 10.1016/j.psychres.2014.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, Morissette SB. Nonsuicidal self-injury and suicide attempts in Iraq/Afghanistan war veterans. Psychiatry Res. 2016b;243:232–237. doi: 10.1016/j.psychres.2016.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, Morissette SB. The impact of cannabis use disorder on suicidal and nonsuicidal self-injury in Iraq/Afghanistan-era veterans with and without mental health disorders. Suicide and Life-Threatening Behavior. doi: 10.1111/sltb.12345. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Gratz KL, Tull MT, Morissette SB, Meyer EC, DeBeer BB, Silvia PJ, Calhoun PC, Beckham JC. Non-suicidal self-injury as a predictor of active and passive suicidal ideation among Iraq/Afghanistan veterans. Psychiatry Res. 2015;227:360–362. doi: 10.1016/j.psychres.2015.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Meyer EC, DeBeer BB, Gulliver SB, Morissette SB. A 12-month prospective study of the effects of PTSD-depression comorbidity on suicidal behavior in Iraq/Afghanistan-era veterans. Psychiatry Res. 2016a;243:97–99. doi: 10.1016/j.psychres.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clin Psychol Psychother. 2011;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Maguen S, Madden E, Cohen BE, Bertenthal D, Neylan TC, Seal KH. Suicide risk in Iraq and Afghanistan veterans with mental health problems in VA care. J Psychiatr Res. 2015;68:120–124. doi: 10.1016/j.jpsychires.2015.06.013. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. (HHS Publication No. (SMA) 14-4887. NSDUH Series H-49). [Google Scholar]
- United Nations Office on Drugs and Crime: World Drug Report, 2014. (United Nations publication, Sales No. E.14.XI.7). [Google Scholar]
- U.S. Department of Veterans Affairs. 2016 VA Suicide Prevention Program Facts about Veteran Suicide. 2016 Jul; [Internet]. Retrieved from: https://www.va.gov/opa/publications/factsheets/Suicide_Prevention_FactSheet_New_VA_Stats_070616_1400.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


