Abstract
Background
More than half of the global population currently lives in cities, with an increasing trend for further urbanization. Living in cities is associated with increased population density, traffic noise and pollution, but also with better access to health care and other commodities.
Methods
This review is based on a selective literature search, providing an overview of the risk factors for mental illness in urban centers.
Results
Studies have shown that the risk for serious mental illness is generally higher in cities compared to rural areas. Epidemiological studies have associated growing up and living in cities with a considerably higher risk for schizophrenia. However, correlation is not causation and living in poverty can both contribute to and result from impairments associated with poor mental health. Social isolation and discrimination as well as poverty in the neighborhood contribute to the mental health burden while little is known about specific interactions between such factors and the built environment.
Conclusion
Further insights on the interaction between spatial heterogeneity of neighborhood resources and socio-ecological factors is warranted and requires interdisciplinary research.
Urbanization is one of the main health-relevant changes humanity is facing in our time, and will be facing in the coming decades (1). Today more than 50 percent of the global population is living in cities; by 2050, this rate will increase to nearly 70 percent with more than 50 percent of the urban population living in cities of over 500 000 inhabitants (2). With growing urbanization, more and more people are exposed to risk factors originating from the urban social (e.g. poverty) or physical environment (e.g. traffic noise), contributing to increased stress, which in turn is negatively associated with mental health. By contrast, cities provide better access to health care, employment, and education. The balance between those factors that are deleterious and those that are protective for mental health calls for a better understanding of the interaction between city living and mental health.
Methods
We performed a selective literature review that synthesizes the current evidence for urban population mental health. We mainly included meta-analyses and quantitative studies presenting evidence from rural-urban or inner-urban differences in mental disorders. Qualitative studies were excluded as well as studies in which mental health was used to predict other outcomes. Results are interpreted based on the theories by Stokols (3), Galea et al. (4), and Gruebner et al. (5) with particular consideration of socio-ecological environments and their associations with mental health.
Results
Rural-urban differences in mental health
The risk for some major mental illnesses (e.g. anxiety, psychotic, mood, or addictive disorders) is generally higher in cities (e.g. 6). Studies on anxiety disorders (including posttraumatic stress disorder, distress, anger, and paranoia) found higher rates in urban versus rural areas in several Latin American and Asian countries (7– 10). The same was true for psychotic disorders (e.g. schizophrenia) in China (11) and in large urban areas in Germany (12, 13). In a Danish study, the risk for schizophrenia was more than twofold for individuals who had spent their first 15 years in a major city versus those who had grown up in rural areas (14) (see the Table for a selective summary). Epidemiological studies further confirmed that the risk for schizophrenia was higher in people who grew up in cities (versus rural areas), thereby exhibiting a dose-response relationship: The more time spent in an urban environment as a child, the higher the risk for schizophrenia as an adult (15– 23).
Likewise, mood disorders were observed more frequently among residents of large cities in Germany (12). In contrast, rural residents in China were more likely to have depressive disorders (8, 24). This was also true in a study on common perinatal mental disorders (depression and substance use) in women in Vietnam (25). Addictive disorders (for instance excessive use of massive multiplayer online role-playing games [MMORPG]) was mainly found among young adult university graduates living alone in urban France (26). In contrast, rural residents were more likely to have alcohol dependence than were urban residents, as shown in a study in China (8).
Inner-urban differences and mental health
Urban social environments:
Social risk factors for mental health in cities include
concentrations of low socio-economic status (SES) (e.g. education levels, income),
low social capital (e.g. social support, efficacy),
or social segregation (e.g. perceived minority status, ethnic group membership) (27– 34).
SES is by far the most studied risk factor and has been consistent in its association with mental health. For example, living in poor or deprived neighborhoods is associated with greater risk of poor mental health (e.g. depression, schizophrenia) versus living in richer neighborhoods (27, 29, 33, 35– 40, e1– e4). The association between familial liability and mental illness was stronger in more deprived neighborhoods, with neighborhood variables mediating urbanicity effects in Turkey (38). In another study, adverse conditions associated with very poor neighborhoods in slums were associated with mental health disorders in India (39). Persons within disadvantaged areas may have more difficulties building and sustaining supportive social relationships and may have increasing susceptibility to mental illness. Evidence also exists for socially disorganized neighborhoods in which people feel insecure and frequently experience violence (e1, e2), contributing to increased trauma exposure with related consequences for mental health (40, e3, e4).
However, it is important to keep in mind that correlation is not causation. Selective migration may lead to worse population health in those neighborhoods that movers leave behind and to better health at the destination, as movers often have better health status (e5, e6).
Research also indicated a reciprocal effect, that is, people who had poor health or who experienced difficult life events (e.g. relationship breakdown, job loss) were more likely to move to more deprived areas versus others (e7, e8), e.g., due to low, affordable rents. For example, increased schizophrenia risk was reported for living in an urban environment five years after disease onset (14). However, this effect did not fully explain increased schizophrenia rates in inner cities, because numerically, effects of urbanization early in life were somewhat larger, suggesting at least two mechanisms: First, growing up in cities has an effect on illness risk, and second, higher amounts of people with health problems move to urban areas (17).
Living in socially deprived neighborhoods itself may have a heritable component (ranging from a 65% elevated variance in a sibling study to 41% in a twin study) (e9). The authors assume that genetic susceptibility for schizophrenia predicts subsequent residence in individuals with schizophrenia. They found that effects of population density on schizophrenia risk disappeared when known familial risk factors were accounted for, and assumed that in relatives of schizophrenia subjects, familial or specifically genetic risk factors are associated with cognitive functions, which causally contribute to living in poverty (e9). However, such familial and even genetic risk factors may be independent of cognitive style and rather include visible minority status.
Indeed, schizophrenia risk is substantially increased in migrants, not only in the first generation exposed to transitional stressors, but also in subsequent generations (e10). Moreover, psychosis rates are particularly high when patients belong to a visible minority (e.g., people from West Africa and the Caribbean in London, Moroccans in Den Haag) (34) and when the ethnic density in the neighborhood is low. These findings suggest that social exclusion and discrimination play an important role in the development of schizophrenia (e11).
In turn, neighborhoods characterized by higher social support and collective efficacy may buffer perceived stress through support networks promoting mental health (e12, e13). In addition, neighborhood social support networks may also contribute to social norms and practices that have been found to be protective for substance use disorders or suicide attempts (30– 32).
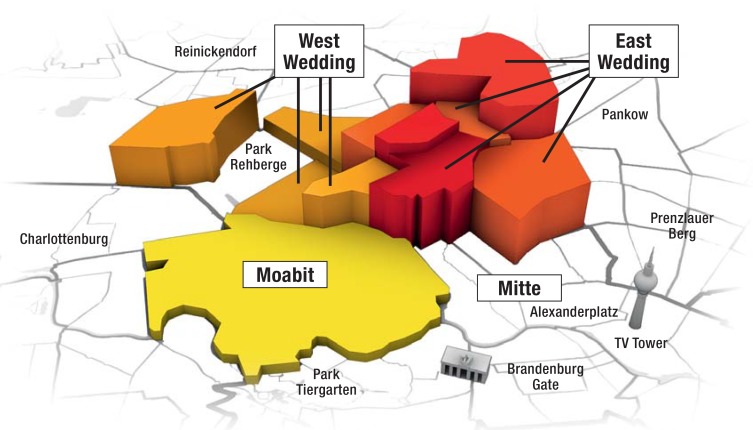
Living in neighborhoods characterized by residential ethnic segregation is associated with greater risk of depression and anxiety, versus living in less segregated neighborhoods (29, e3, e14). Our research group investigated the differential contribution of poverty and minority status at the community level on individual-level mental health, controlled by individual-level differences in SES and migration in an inner city population in Berlin, Germany (27) (Figure).
Figure.
Mental distress (mean GHQ-28 scores) as a function of local poverty levels (beyond individual SES), as defined by the percentage of residents receiving public welfare, in 11 local neighborhoods in the inner city borough of Berlin (Mitte).
The percentage of residents receiving public welfare is depicted in yellow (low) to red (high) color-coding (range: 18% to 45%), and mean levels of mental distress (Mean GHQ-28 scores = 18.53, standard deviation = 4.79, range 10.7 to 26.3) are shown as column heights in each local neighborhood.
GHQ, General Health Questionnaire; SES, socio-economic status
We found that individual-level mental distress in migrants was associated with community-level poverty, independent of individual-level SES, in that, roughly, a 10% increase in the percentage of residents receiving public welfare in the neighborhood corresponded to an increase of 8 points on the GHQ-28 (General Health Questionnaire).
We noted that the effect of poverty was more pronounced in migrants versus native citizens, in that a 10% increase in the proportion of residents with a migration background accounted for an additional 5 points on the GHQ-28. Our observations suggest that the high level of mental distress in migrants was largely driven by community-level SES, beyond the effects of individual resources, emphasizing the need for targeted interventions (27).
There is also cumulative evidence that urban residents belonging to a minority group including those with a migration background carry an increased risk for depression and psychosis (e15– e18). Remarkably, social support among minorities appears to be an important protective factor, while having visible minority status as a resident in neighborhoods with low numbers of ethnic minorities (“lower ethnic density”) was associated with increased rates of e.g. schizophrenia (34). Such effects may well be due to increased discrimination in segregated neighborhoods and are supported by neurobiological studies emphasizing the role of social isolation stress in the development of mental disorders (e11, e19).
Urban physical environments: Similar patterns can be found for the urban physical environment that compared to rural areas may contain
higher rates of pollution (e.g., air, water),
noise pollution (e.g., traffic)
specific urban designs (e.g. tall buildings that may be perceived as oppressive),
or more physical threats (e.g., accidents, violence),
thereby likely increasing stress levels with negative effects on mental health (5, e20– e25). Research indicates that urban air, water, and noise pollution can have substantial effects on the mental health of urban populations. For example, living close to major streets or airports increases exposure to traffic noise and pollution and is associated with higher levels of stress and aggression (e20, e26– e28).
Adjusted by SES, age, and type of residential area, one study in Germany found that those who were highly annoyed by road traffic, had a 1.8-fold (women) and 2.5-fold (men) increased risk for impaired mental health (e29). Urban light exposure may further influence the circadian rhythm and change sleeping patterns with known consequences for mental well-being (e30).
Urban design exhibits associations with population mental health (4, e22, e23, e31– e41). For example, greater access to green space and better walkability was associated with less depression and enhanced physical activity that may promote health (e32– e34). Furthermore, the recreational aspects of well-maintained urban green and blue spaces are apparently associated with the mental well-being of urban populations (e33, e42, e43). Urban green and blue features additionally have the capability to buffer urban heat island effects and to reduce heat stress (e44). Moreover, urban street canopy can reduce the “oppressive” effects of tall buildings (e22, e23).
In addition, urban density (as opposed to sprawl) has been associated with better mental health as it comprises better access to resources (e.g. parks, playgrounds, health-, and social care) (e45).
In contrast, less green space may indicate more traffic noise and worse access to neighborhood resources, which may lead to low housing rents attracting low SES groups. Work in the field of environmental justice may offer more insights into these relationships and may help further promote mental health in urban areas.
Future challenges
Urban neighborhoods play a particular role in shaping urban population health due to their unique socio-ecological environments constituting both risk and health promoting factors (6, 12, 36, e46). Six key challenges and opportunities for future research directions need to be addressed:
First: there remains much we need to know about the functional relationships between city living or upbringing and mental health problems in urban populations (19– 22, 37, e47– e49). Research would benefit from more longitudinal studies facilitating the analysis of causal relationships between the duration of exposure to inner-urban socio-ecological factors and mental health.
Second: we do not know much about the associations of neighborhood resources (e.g. green spaces) with different dimensions of mental health. Although studies have looked into different mental health outcomes, they have not been systematically assessed within the same contexts, that is, whether e.g. green spaces are associated with similar effects across mental health dimensions.
Third: we also do not know much about socio-demographic differences in the relationship between access to neighborhood resources and mental health (19). Socio-demographic groups may not have similar access to these resources and may be disproportionately distributed benefiting e.g. more affluent populations, which is increasingly recognized as an environmental justice issue (e50). Including these issues in the context of urban mental health may help for more sustainable distributions of balanced resources.
Fourth: our understanding of moderators (e.g. social or ethnic segregation) to help explain differences between groups in mental health is also limited (27, 28, 30). In this context, breaking up social and ethnic segregation and discrimination appears to be warranted to improve living conditions and reduce social isolation. Furthermore, both heterogeneous and homogeneous neighborhoods (e.g. low SES) may have negative associations with individual level mental health such that respective effects can only be assessed in multilevel-adjusted research studies. In addition, we do not know whether the risk of mental health problems is reduced in people if they think they have the option to move away.
We also do not know much about the spatial heterogeneity in the association of neighborhood resources with mental health across urban neighborhoods. High unemployment rates in one neighborhood may have an effect also on adjacent neighborhoods (30). For example, high unemployment rates are associated with higher substance abuse (e51) and may affect drug use in neighboring parks or facilities, even though unemployment (or substance use) rates are low there.
Fifth: our knowledge on synergies between interventions is limited, so that we do not know much about the mental health effects of policies that were not specifically designed for improving mental health of urban populations (e.g. introducing street trees, reduced-traffic areas). Systematic evaluations of interventions that have worked in other settings and their effects on urban mental health are still scarce in the literature, especially in developing cities of resource poor countries (e52, e53).
Sixth: interdisciplinary research between architecture, city planning, epidemiology, geography, neurosciences, and sociology are crucial to better understand to which extent urban socio-ecological environments affect population mental health. Such an approach may also identify populations who lack the “urban advantage” and who are at risk for psychopathology.
Conclusions
A series of studies exhibit interaction between urbanicity, the socio-ecological environment, and mental health (19, 27). Research would benefit from more longitudinal studies focusing on both rural-urban and inner-urban causes and distributions of mental health.
More in-depth knowledge about different dimensions of mental health disorders across diverse socio-demographic groups might shed light on the distributions of these disorders and guide us in better developing health promoting urban designs. Knowledge on moderators from the socio-ecological environment, on the spatial heterogeneity of neighborhood resources, and their associations with mental health within and across neighborhoods will help to elucidate the mechanisms linking urban environments to mental health.
Table. Studies on the effect of urban exposure on mental health*1.
| Reference | Exposure factor | Outcome | Effect size |
95% CI [Lower level; upper level] |
| Peen et al. (2010) (6) |
Urban vs. rural | Any disorder*2 | 1.38 (OR) | [1.17; 1.64] |
| Urban vs. rural | Mood disorder*2 | 1.39 (OR) | [1.23; 1.58] | |
| Urban vs. rural | Anxiety disorder*2 | 1.21 (OR) | [1.02; 1.42] | |
| Urban vs. rural | Substance use disorder*2 | 1.31 (OR) | [0.97; 1.78] | |
| Vassos et al. (2012) (15) |
Continuous urbanicity index | Schizophrenia | 2.38 (OR) | [2.01; 2.81] |
| Pedersen & Mortensen (2001) (14) |
Per 15 years lived in capital city vs. rural area | Schizophrenia*3 | 2.75 (RR) | [2.31; 3.28] |
| Per 15 years lived in capital suburb vs. rural area | Schizophrenia*3 | 1.69 (RR) | [1.43; 1.99] | |
| Per 15 years lived in provincial city vs. rural area | Schizophrenia*3 | 1.71 (RR) | [1.41; 2.06] | |
| Per 15 years lived in provincial town vs. rural area | Schizophrenia*3 | 1.32 (RR) | [1.13; 1.54] | |
| Mortensen et al. (1999) (23) |
Place of birth: Capital vs. rural area | Schizophrenia*3 | 2.40 (RR) | [2.13; 2.70] |
| Place of birth: Capital suburb vs. rural area | Schizophrenia*3 | 1.62 (RR) | [1.37; 1.90] | |
| Place of birth: Provincial city vs. rural area | Schizophrenia*3 | 1.57 (RR) | [1.36; 1.81] | |
| Place of birth: Provincial town vs. rural area | Schizophrenia*3 | 1.24 (RR) | [1.10; 1.41] | |
| Cantor-Graae & Selten (2005) (e10) |
First generation migrants vs. natives | Schizophrenia | 2.7 (RR) | [2.3; 3.2] |
| Second generation migrants vs. natives | Schizophrenia | 4.5 (RR) | [1.5; 13.1] | |
| First and second generation migrants vs. natives | Schizophrenia | 2.9 (RR) | [2.5; 3.49] | |
| Veling et al. (2008) (34) |
Immigrant vs. Dutch in urban area of low ethnic density | Psychotic disorder*3 | 2.36 (IRR) | [1.89; 2.95] |
*1Selective summary results of studies using meta analyses (6, 15 ###,e10) or large population sizes (>1.75 million) (14, 23);
Provincial cities had more than 100 000 inhabitants and provincial towns more than 10 000 inhabitants (14, 23).
We also included one study that looked at psychotic disorders among immigrants in The Hague, Netherlands (34), to cover inner urban differences in mental health.
*2 Unadjusted; *3 adjusted;
CI, confidence interval; IRR=Incidence rate ratio; OR= Odds ratio; RR=Risk ratio
Acknowledgments
We would like to thank Mr. Werner of the Audiovisual Center at the University of Potsdam for his support in creating the Figure.
This study was funded by the German Research Foundation (DFG, GR 4302/1–1, GR 4302/2–1 to OG).
Footnotes
Conflict of interest statement
Prof. Rapp has received consultancy fees from Eli Lilly. He has received reimbursement of travel and accommodation expenses from Servier Germany. He has received lecture fees from Merz, GlaxoSmithKline and Johnson & Johnson, as well as study support (third-party funds) from Willmar Schwabe.
PD Dr. Adli has received author’s royalties from Random House. He has received lecture and consultancy fees from Deutsche Bank, ViiV, Gilead Sciences, MSD, Servier, aristo, Janssen-Cilag, Merz, mytomorrows and Lundbeck. He has received study support (third-party funds) from Servier and aristo, as well as reimbursement of travel and accommodation expenses from Lundbeck and Servier.
The other authors declare that no conflict of interest exists.
References
- 1.Adli M, Berger M, Brakemeier EL, et al. Neurourbanism—a joint methodological approach between urban planning and neurosciences. Die Psychiatrie. 2016;13:70–78. [Google Scholar]
- 2.United Nations, Department of Economic and Social Affairs, Population Division. United Nations. New York: 2015. World urbanization prospects. The 2014 revision; 1p pp. [Google Scholar]
- 3.Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol. 1992;47:6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 4.Galea S, Freudenberg N, Vlahov D. Cities and population health. Soc Sci Med. 2005;60:1017–1033. doi: 10.1016/j.socscimed.2004.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gruebner O, Staffeld R, Khan M, Burkart K, Krämer A, Hostert P. International Human Dimensions Programme (IHDP) Bonn: 2011. Urban health in megacities: extending the framework for developing countries Bonn. [Google Scholar]
- 6.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 7.Prina AM, Ferri CP, Guerra M, Brayne C, Prince M. Prevalence of anxiety and its correlates among older adults in Latin America, India and China: cross-cultural study. Br J Psychiatry. 2011;199:485–491. doi: 10.1192/bjp.bp.110.083915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phillips MR, Zhang J, Shi Q, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet. 2009;373:2041–2053. doi: 10.1016/S0140-6736(09)60660-7. [DOI] [PubMed] [Google Scholar]
- 9.Silove D, Ivancic L, Rees S, Bateman-Steel C, Steel Z. Clustering of symptoms of mental disorder in the medium-term following conflict: an epidemiological study in Timor-Leste. Psychiatry Research. 2014;219:341–346. doi: 10.1016/j.psychres.2014.05.043. [DOI] [PubMed] [Google Scholar]
- 10.Sharifi V, Amin-Esmaeili M, Hajebi A, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey 2011. Arch Iran Med. 2015;18:76–84. [PubMed] [Google Scholar]
- 11.Long J, Huang G, Liang W, et al. The prevalence of schizophrenia in mainland China: evidence from epidemiological surveys. Acta Psychiatr Scand. 2014;130:244–256. doi: 10.1111/acps.12296. [DOI] [PubMed] [Google Scholar]
- 12.Jacobi F, Höfler M, Siegert J, et al. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: the Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH) Int J Methods Psychiatr Res. 2014;23:304–319. doi: 10.1002/mpr.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frick U, Frick H, Langguth B, Landgrebe M, Hubner-Liebermann B, Hajak G. The revolving door phenomenon revisited: time to readmission in 17“145 [corrected] patients with 37”697 hospitalisations at a German psychiatric hospital. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0075612. e75612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pedersen CB, Mortensen PB. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry. 2001;58:1039–1046. doi: 10.1001/archpsyc.58.11.1039. [DOI] [PubMed] [Google Scholar]
- 15.Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. 2012;38:1118–1123. doi: 10.1093/schbul/sbs096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Os J, Kenis G, Rutten BPF. The environment and schizophrenia. Nature. 2010;468:203–212. doi: 10.1038/nature09563. [DOI] [PubMed] [Google Scholar]
- 17.March D, Hatch SL, Morgan C, et al. Psychosis and place. Epidemiol Rev. 2008;30:84–100. doi: 10.1093/epirev/mxn006. [DOI] [PubMed] [Google Scholar]
- 18.Haddad L, Schäfer A, Streit F, et al. Brain structure correlates of urban upbringing, an environmental risk factor for schizophrenia. Schizophr Bull. 2015;41:115–122. doi: 10.1093/schbul/sbu072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heinz A, Deserno L, Reininghaus U. Urbanicity, social adversity and psychosis. World Psychiatry. 2013;12:187–197. doi: 10.1002/wps.20056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lederbogen F, Kirsch P, Haddad L, et al. City living and urban upbringing affect neural social stress processing in humans. Nature. 2011;474:498–501. doi: 10.1038/nature10190. [DOI] [PubMed] [Google Scholar]
- 21.Abbott A. City living marks the brain. Nature. 2011;474 doi: 10.1038/474429a. [DOI] [PubMed] [Google Scholar]
- 22.Galea S, Uddin M, Koenen K. The urban environment and mental disorders: Epigenetic links. Epigenetics. 2011;6:400–404. doi: 10.4161/epi.6.4.14944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340:603–608. doi: 10.1056/NEJM199902253400803. [DOI] [PubMed] [Google Scholar]
- 24.Li N, Pang L, Chen G, Song X, Zhang J, Zheng X. Risk factors for depression in older adults in Beijing. Can J Psychiatry. 2011;56:466–473. doi: 10.1177/070674371105600804. [DOI] [PubMed] [Google Scholar]
- 25.Fisher J, Tran T, La BT, Kriitmaa K, Rosenthal D, Tran T. Common perinatal mental disorders in northern Viet Nam: community prevalence and health care use. Bull World Health Organ. 2010;88:737–745. doi: 10.2471/BLT.09.067066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Achab S, Nicolier M, Mauny F, et al. Massively multiplayer online role-playing games: comparing characteristics of addict vs non-addict online recruited gamers in a French adult population. BMC Psychiatry. 2011;11 doi: 10.1186/1471-244X-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rapp MA, Kluge U, Penka S, et al. When local poverty is more important than your income: Mental health in minorities in inner cities. World Psychiatry. 2015;14:249–250. doi: 10.1002/wps.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Honold J, Wippert PM, van der Meer E. Urban health resources: physical and social constitutes of neighborhood social capital. Procedia Soc Behav Sci. 2014;131:491–496. [Google Scholar]
- 29.Meyer OL, Castro-Schilo L, Aguilar-Gaxiola S. Determinants of mental health and self-rated health: a model of socioeconomic status, neighborhood safety, and physical activity. Am J Public Health. 2014;104:1734–1741. doi: 10.2105/AJPH.2014.302003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fone D, White J, Farewell D, et al. Effect of neighbourhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychol Med. 2014;44:2449–2460. doi: 10.1017/S0033291713003255. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization, Calouste Gulbenkian Foundation. World Health Organization. Geneva: 2014. Social determinants of mental health. [Google Scholar]
- 32.Maimon D, Browning CR, Brooks-Gunn J. Collective efficacy, family attachment, and urban adolescent suicide attempts. J Health Soc Behav. 2010;51:307–324. doi: 10.1177/0022146510377878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Ann Epidemiol. 2007;17:171–179. doi: 10.1016/j.annepidem.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Veling W, Susser E, van Os J, Mackenbach JP, Selten JP, Hoek HW. Ethnic density of neighborhoods and incidence of psychotic disorders among immigrants. Am J Psychiatry. 2008;165:66–73. doi: 10.1176/appi.ajp.2007.07030423. [DOI] [PubMed] [Google Scholar]
- 35.Beard JR, Cerdá M, Blaney S, Ahern J, Vlahov D, Galea S. Neighborhood characteristics and change in depressive symptoms among older residents of New York City. Am J Public Health. 2009;99:1308–1314. doi: 10.2105/AJPH.2007.125104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62:940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 37.Faris REL, Dunham HW. Mental disorders in urban areas: an ecological study of schizophrenia and other psychoses. Univ Chicago Press; 1939 [Google Scholar]
- 38.Binbay T, Drukker M, Alptekin K, et al. Evidence that the wider social environment moderates the association between familial liability and psychosis spectrum outcome. Psychol Med. 2012;42:2499–2510. doi: 10.1017/S0033291712000700. [DOI] [PubMed] [Google Scholar]
- 39.Subbaraman R, Nolan L, Shitole T, et al. The psychological toll of slum living in Mumbai, India: a mixed methods study. Soc Sci Med. 2014;119:155–169. doi: 10.1016/j.socscimed.2014.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L, Sherbourne CD. The importance of social context: Neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Soc Sci Med. 2007;65:1867–1881. doi: 10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: social processes and new directions in Research on JSTOR. Annu Rev Sociol. 2002;28:443–478. [Google Scholar]
- E2.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- E3.Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37 [PubMed] [Google Scholar]
- E4.Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: a study of youths in urban America. J Urban Health. 2004;81:530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.Norman P, Boyle P, Rees P. Selective migration, health and deprivation: a longitudinal analysis. Soc Sci Med. 2005;60:2755–2771. doi: 10.1016/j.socscimed.2004.11.008. [DOI] [PubMed] [Google Scholar]
- E6.Ullmann SH, Goldman N, Massey DS. Healthier before they migrate, less healthy when they return? The health of returned migrants in Mexico. Soc Sci Med. 2011;73:421–428. doi: 10.1016/j.socscimed.2011.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Tunstall H, Shortt NK, Pearce JR, Mitchell RJ. Difficult life events, selective migration and spatial inequalities in mental health in the UK. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0126567. e0126567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.Arcaya MC, Subramanian SV, Rhodes JE, Waters MC. Role of health in predicting moves to poor neighborhoods among Hurricane Katrina survivors. Proc Natl Acad Sci USA [Internet] 2014;111:16246–16253. doi: 10.1073/pnas.1416950111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E9.Sariaslan A, Fazel S, D‘Onofrio BM, et al. Schizophrenia and subsequent neighborhood deprivation: revisiting the social drift hypothesis using population, twin and molecular genetic data. Transl Psychiat. 2016;6 doi: 10.1038/tp.2016.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E10.Cantor-Graae E, Selten JP. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162:12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- E11.Heinz A. Dopaminergic dysfunction in alcoholism and schizophrenia—psychopathological and behavioral correlates. Eur Psychiat. 2002;17:9–16. doi: 10.1016/s0924-9338(02)00628-4. [DOI] [PubMed] [Google Scholar]
- E12.Ahern J, Galea S. Collective efficacy and major depression in urban neighborhoods. Am J Epidemiol. 2011;173:1453–1462. doi: 10.1093/aje/kwr030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E13.Bertotti M, Watts P, Netuveli G, et al. Types of social capital and mental disorder in deprived urban areas: a multilevel study of 40 disadvantaged London neighbourhoods. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0080127. e80127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E14.French D. Residential segregation and health in Northern Ireland. Health & Place. 2009;15:873–881. doi: 10.1016/j.healthplace.2009.02.012. [DOI] [PubMed] [Google Scholar]
- E15.Aichberger MC, Schouler-Ocak M, Mundt A, et al. Depression in middle-aged and older first generation migrants in Europe: results from the Survey of Health, Ageing and Retirement in Europe (SHARE) Eur Psychiatry. 2010;25:468–475. doi: 10.1016/j.eurpsy.2009.11.009. [DOI] [PubMed] [Google Scholar]
- E16.Potochnick SR, Perreira KM. Depression and anxiety among first-generation immigrant Latino youth: key correlates and implications for future research. J Nerv Ment Dis. 2010;198:470–477. doi: 10.1097/NMD.0b013e3181e4ce24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E17.Morgan C, Charalambides M, Hutchinson G, Murray RM. Migration, ethnicity, and psychosis: toward a sociodevelopmental model. Schizophr Bull. 2010;36:655–664. doi: 10.1093/schbul/sbq051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E18.Bresnahan M, Begg MD, Brown A, et al. Race and risk of schizophrenia in a US birth cohort: another example of health disparity? Int J Epidemiol. 2007;36:751–758. doi: 10.1093/ije/dym041. [DOI] [PubMed] [Google Scholar]
- E19.Heinz AJ, Beck A, Meyer-Lindenberg A, Sterzer P, Heinz A. Cognitive and neurobiological mechanisms of alcohol-related aggression. Nat Rev Neurosci. 2011;12:400–413. doi: 10.1038/nrn3042. [DOI] [PubMed] [Google Scholar]
- E20.Rocha K, Pérez K, Rodríguez-Sanz M, Obiols JE, Borrell C. Perception of environmental problems and common mental disorders (CMD) Soc Psychiatry Psychiatr Epidemiol. 2012;47:1675–1684. doi: 10.1007/s00127-012-0474-0. [DOI] [PubMed] [Google Scholar]
- E21.Honold J, Beyer R, Lakes T, van der Meer E. Multiple environmental burdens and neighborhood-related health of city residents. J Environ Psychol. 2012;32:305–317. [Google Scholar]
- E22.Asgarzadeh M, Lusk A, Koga T, Hirate K. Measuring oppressiveness of streetscapes. Landsc Urban Plan. 2012;107:1–11. [Google Scholar]
- E23.Asgarzadeh M, Koga T, Yoshizawa N, Munakata J, Hirate K. Investigating green urbanism. Building Oppressiveness. 2010;9:555–562. [Google Scholar]
- E24.Guite HF, Clark C, Ackrill G. The impact of the physical and urban environment on mental well-being. Public Health. 2006;120:1117–1126. doi: 10.1016/j.puhe.2006.10.005. [DOI] [PubMed] [Google Scholar]
- E25.Sampson RJ, Raudenbush SW. Seeing disorder: Neighborhood stigma and the social construction of “broken windows” ?Soc Psychol Q. 2004;67:319–342. [Google Scholar]
- E26.Seidler A, Wagner M, Schubert M, et al. Myocardial infarction risk due to aircraft, road, and rail traffic noise: results of a case-control study based on secondary data. Dtsch Arztebl Int. 2016;113:407–414. doi: 10.3238/arztebl.2016.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E27.Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: multi-airport retrospective study. BMJ. 2013;347:f5561–f5561. doi: 10.1136/bmj.f5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E28.Dzhambov A, Dimitrova D. Neighborhood noise pollution as a determinant of displaced aggression: a pilot study. Noise Health. 2014;16:95–101. doi: 10.4103/1463-1741.132090. [DOI] [PubMed] [Google Scholar]
- E29.Hammersen F, Niemann H, Hoebel J. Environmental noise annoyance and mental health in adults: findings from the Cross-Sectional German Health Update (GEDA) Study 2012. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13100954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E30.Cho Y, Ryu SH, Lee BR, Kim KH, Lee E, Choi J. Effects of artificial light at night on human health: A literature review of observational and experimental studies applied to exposure assessment. Chronobiol Int. 2015;32:1294–1310. doi: 10.3109/07420528.2015.1073158. [DOI] [PubMed] [Google Scholar]
- E31.Gascon M, Triguero-Mas M, Martínez D, et al. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int J Environ Res Public Health. 2015;12:4354–4379. doi: 10.3390/ijerph120404354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E32.Lee ACK, Maheswaran R. The health benefits of urban green spaces: a review of the evidence. J Public Health. 2011;33:212–222. doi: 10.1093/pubmed/fdq068. [DOI] [PubMed] [Google Scholar]
- E33.James P, Banay RF, Hart JE, Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep. 2015;2:131–142. doi: 10.1007/s40471-015-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E34.Cohen-Cline H, Turkheimer E, Duncan GE. Access to green space, physical activity and mental health: a twin study. J Epidemiol Community Health. 2015;69:523–529. doi: 10.1136/jech-2014-204667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E35.Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26:392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- E36.Völker S, Kistemann T. “I‘m always entirely happy when I’m here!” Urban blue enhancing human health and well-being in Cologne and Düsseldorf, Germany. Soc Sci Med. 2013;78:113–124. doi: 10.1016/j.socscimed.2012.09.047. [DOI] [PubMed] [Google Scholar]
- E37.van Dillen SME, de Vries S, Groenewegen PP, Spreeuwenberg P. Greenspace in urban neighbourhoods and residents‘ health: adding quality to quantity. J Epidemiol Community Health. 2012;66 doi: 10.1136/jech.2009.104695. [DOI] [PubMed] [Google Scholar]
- E38.Morrison DS, Thomson H, Petticrew M. Evaluation of the health effects of a neighbourhood traffic calming scheme. J Epidemiol Community Health. 2004;58:837–840. doi: 10.1136/jech.2003.017509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E39.Roswall N, Høgh V, Envold-Bidstrup P, et al. Residential exposure to traffic noise and health-related quality of life-a population-based study. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0120199. e0120199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E40.Woodward BM, Zadoroznyj M, Benoit C. Beyond birth: Women‘s concerns about post-birth care in an Australian urban community. Women Birth. 2016;29:153–159. doi: 10.1016/j.wombi.2015.09.006. [DOI] [PubMed] [Google Scholar]
- E41.Krabbendam L, van Os J. Schizophrenia and urbanicity: a major environmental influence—conditional on genetic risk. Schizophr Bull [Internet] 2005;31:795–799. doi: 10.1093/schbul/sbi060. [DOI] [PubMed] [Google Scholar]
- E42.Thomas F. The role of natural environments within women‘s everyday health and wellbeing in Copenhagen, Denmark. Health Place. 2015;35:187–195. doi: 10.1016/j.healthplace.2014.11.005. [DOI] [PubMed] [Google Scholar]
- E43.Völker S, Kistemann T. Developing the urban blue: Comparative health responses to blue and green urban open spaces in Germany. Health Place. 2015;35:196–205. doi: 10.1016/j.healthplace.2014.10.015. [DOI] [PubMed] [Google Scholar]
- E44.Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. 2008;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- E45.Melis G, Gelormino E, Marra G, Ferracin E, Costa G. The effects of the urban built environment on mental health: a cohort study in a large northern Italian city. Int J Environ Res Public Health. 2015;12:14898–14915. doi: 10.3390/ijerph121114898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E46.Peen J, Dekker J, Schoevers RA, Haveten M, de Graaf R, Beekman AT. Is the prevalence of psychiatric disorders associated with urbanization? Soc Psychiatry Psychiatr Epidemiol. 2007;42:984–989. doi: 10.1007/s00127-007-0256-2. [DOI] [PubMed] [Google Scholar]
- E47.Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG. Rural-urban differences in depression prevalence: implications for family medicine. Fam Med. 2006;38:653–660. [PubMed] [Google Scholar]
- E48.Lewis G, David A, Andréassson S, Allebeck P. Schizophrenia and city life. Lancet. 1992;340:137–140. doi: 10.1016/0140-6736(92)93213-7. [DOI] [PubMed] [Google Scholar]
- E49.Harpham T. Urbanization and mental health in developing countries: A research role for social scientists, public health professionals and social psychiatrists. Soc Sci Med. 1994;39:233–245. doi: 10.1016/0277-9536(94)90332-8. [DOI] [PubMed] [Google Scholar]
- E50.Wolch JR, Byrne J, Newell JP. Urban green space, public health, and environmental justice: The challenge of making cities “just green enough”. Landsc Urban Plan. 2014;125:234–234. [Google Scholar]
- E51.Henkel D. Unemployment and substance use: a review of the literature (1990-2010) Curr Drug Abuse Rev. 2011;4:4–27. doi: 10.2174/1874473711104010004. [DOI] [PubMed] [Google Scholar]
- E52.Cohen A, Eaton J, Radtke B, et al. Three models of community mental health services In low-income countries. Int J Ment Health Syst. 2011;5 doi: 10.1186/1752-4458-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E53.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]