Abstract
Objectives:
Boswellic acid (BA), a compound isolated from the gum-resin of Boswellia carterii, is a pentacyclic terpenoid that is active against many inflammatory diseases, including cancer, arthritis, chronic colitis, ulcerative colitis, Crohn's disease, and memory impairment, but the mechanism is poorly understood. This study investigated the effects of boswellic acid on spatial learning and memory impairment induced by trimethyltin (TMT) in Wistar rats.
Methods:
Forty male Wistar rats were randomly divided into 5 groups: Normal group, TMT-administrated rats (8.0 mg/kg, Intraperitoneally, i.p.) and TMT + BA (40, 80 and 160 mg/kg, i.p.)-administrated rats. BA was used daily for 21 days. To evaluate the cognitive improving of BA, we performed the Morris water maze test. Moreover, to investigate the neuroprotective effect of BA, we determined the acetylcholinesterase (AchE) activity, the malondialdehyde (MDA) level as a marker of lipid peroxidation, and the glutathione (GSH) content in the cerebral cortex.
Results:
Treatment with TMT impaired learning and memory, and treatment with BA at a dose of 160 mg/kg produced a significant improvement in learning and memory abilities in the water maze tasks. Consistent with behavioral data, the activity of AChE was significantly increased in the TMT-injected rats compared to the control group (P < 0.01) whereas all groups treated with BA presented a more significant inhibitory effect against AChE than the TMT-injected animals. In addition, TMT reduced the GSH content and increased the MDA level in the cerebral cortex as compared to the control group) P < 0.01). On the other hand, treatment with BA at 160 mg/kg slightly increased the GSH content and reduced the MDA level in comparison to the TMT-administered group (P < 0.01).
Conclusion:
The above results suggest that the effect of BA in improving the cognitive function may be mediated through its antioxidant activity.
Keywords: acetylcholinesterase, antioxidant, boswellic acid, lipid peroxidation, trimethyltin
1. Introduction
Trimethyltin (TMT), a short-chain trialkyltin, is used as a stabilizing agent for certain plastics and is a neurotoxin that induces neuronal damage in both humans and experimental animals [1-3]. TMT causes a selective degeneration of pyramidal neurons in the hippocampus and the cortical areas connected to the hippocampus [4, 5]. The precise mechanisms underlying TMT-induced neurotoxicity are not clear [6]. Proposals have been made that TMT produces excess generation of cellular oxidative species, which leads to apoptotic cell death. Therefore, oxidative stress and apoptosis resulting in cognitive dysfunction may be a hallmark feature of neurodegeneration [7]. In this case, drugs, including herbal-based drugs, that can inhibit TMT-induced oxidative damage may represent a new generation of therapeutics for neurological diseases [8].
Herbal medicines have been shown to have memory-enhancing effects in different models. Administration of saffron extract and crocin improved spatial cognitive abilities following chronic cerebral hypoperfusion in rats in part through their antioxidant activities [9]. Additionally, treatment with Rosmarinus officinalis aerial parts essential oil was found, through performance on the Morris water maze task, to enhance both the memory function in the intact memory and the scopolamine-induced learning deficits in rats [10].
Frankincense is a member of the family Burseraceae and the genus Boswellia [11]. Lipophilic extracts of the gum resin of Boswellia species have been used in herbal medicine since ancient times for various indications in folk medicine to treat inflammatory and infectious diseases [12]. Boswellia species contain a broad variety of different components. Among these constituents, a rich unique group of pentacyclic triterpenes, termed boswellic acids (BAs), accounts for the active substances in the extract [13]. Some of the chemical compounds present in frankincense are acid resin (56%), gum, which is similar to gum arabic (30% - 36%), 3-acetyl-beta- boswellic acid (Boswellia sacra), alpha-boswellic acid (Boswellia sacra), 4-O-methyl-glucuronic acid (Boswellia sacra), incensole acetate and phellandrene. Olibanum gum resin, as a medicinal plant, is traditionally used in India to treat various diseases, including inflammatory ailments, arthritis, cardiac disorders and pain [7, 14]. Several studies have shown that BAs are the major constituents in olibanum gum resin and that they have anti-inflammatory, anti-cancerous and anti-ulcerous activities [8-11]. Moreover, in in vivo and in vitro studies, BAs have been found to inhibit the synthesis of pro-inflammatory enzymes and 5-lipoxygenase such as leukotrine B4 (LTB4), which cause inflammatory reactions, bronchoconstriction, and increased vascular permeability [12, 13, 15]. Also, the administration of ethyl acetate (0.1 mg/ kg) and N-butanol (0.1 mg/kg) fractions obtained from gum resin of Boswellia carterii (B. carterii) has been reported to improve memory function in intact rats and in animals with hyoscine-induced memory impairment [15].
Several studies have demonstrated that excessive production of reactive oxygen species (ROS), which occurs in TMT-induced neurotoxicity, leads to oxidative damage in the brain; therefore, pursuing antioxidant therapies to reduce that damage could be supportive [16-19]. The present study was designed to evaluate the possible neuroprotective or ameliorative effects of BA on TMT-induced learning and memory deficits and oxidative stress. For this purpose, rats were tested in the Morris water maze for spatial learning and memory. Furthermore, acetylcholinesterase (AchE) activity, glutathione (GSH) content and malondialdehyde (MDA) level in the cerebral cortex were measured. Because of the important role of the cerebral cortex in memory function and easy separation of total brain, this part of brain has often been used for biochemical analysis.
2. Materials and Methods
TMT chloride, MDA tetrabutylammonium, reduced GSH and DTNB [5,5’-dithiobis-(2-nitrobenzoic acid)] were obtained from Sigma-Aldrich, and BA was purchased from Shanghai Research Institute of the Chemical Industry Testing Center. Male Wistar rats weighting 230 - 260 g were purchased from the animal facilities of the Pharmaceutical Research Center, Bu-Ali Research Institute, Mashhad University of Medical Sciences. All animal experiments were approved and were carried out in accordance with the Ethical Committee Acts of Mashhad University of Medical Sciences. The animals were housed in standard cages under hygienic conditions and were provided standard animal feed and water ad libitum throughout the treatment period. For acclimatization, the rats were kept in the animal houses for one week prior to the beginning of the study.
Forty rats were randomly divided into five groups (n = 8 per group): the control group and four TMT-treated groups. The rats with TMT-induced lesions were treated with saline [(TMT-lesioned + saline group, 1.6 mL/kg) which means rats received saline instead of BA], BA at 40 mg/kg (B40 group), BA at 80 mg/kg (B80 group), or BA at 160 mg/kg (B160 group). The rats were injected intraperitoneally (i.p.) with TMT (8.0 mg/kg body weight) dissolved in 0.9% saline [20]. BA (40, 80 and 160 mg/kg) was administered i.p. daily for 21 days. From the 13th day, the water maze test was performed for 7 days.
The Morris water maze task [21] was used to determine spatial memory impairment induced by TMT administration. The apparatus was a circular pool of 136 cm in diameter and 60 cm in depth. The pool was filled with water to a depth of 25 cm, and the water temperature remained between 20 - 22°C. The surface of the water was divided into four equal quadrants. Several visual cues were placed on the walls of the experiment room. The experiment consisted of five days of training. On the training days, the rats were subjected to 4 sessions (on days 1 - 5) with 10-seconds intervals for each of 2 trials to find a hidden, transparent platform submerged 1 cm below the water’s surface. In every trial, the rat was placed in the water facing the wall of the pool in one of the four possible starting locations. Everyday, the order of the starting points was randomly chosen using software. The rat was allowed to search for the platform for 60 seconds and was gently guided if it could not reach it. Rats were allowed to remain on the platform for 15 seconds to learn extra maze cues. Two days after the last training day, each rat was subjected to a probe trial, in which the platform was removed from the pool, and the animals were tested in a 60-second spatial probe trial. The time spent in the quadrant where the platform had been located during the training days was measured, and the amount of time spent in that quadrant was calculated. This parameter was taken as an indicator of spatial memory.
At the end of the experiment, the rats were sacrificed for biochemical studies, and the cerebral cortex was dissected. The samples were snap-frozen in liquid nitrogen and stored at - 80°C until use. The evaluation of lipid peroxidation was done by determining the (MDA) level, as a marker of lipid peroxidation, in the cerebral cortex. MDA reacts with thiobarbituric acid (TBA) as a TBA reactive substance (TBARS) to produce a pink-colored complex, which has a maximum absorbance at 532 nm. In this method, 3 mL of phosphoric acid (1%) and 1 mL of TBA (0.6%) were added to brain tissue homogenate (10%) in KCl, after which the mixtures were heated for 45 minutes in boiling water. After the mixture had been cooled, 4 mL of n-butanol was added and vortex-mixed for 1 minutes, followed by centrifugation at 3,000 g for 10 minutes. Then, the organic layers were separated and transferred to a fresh tube, and the absorbance was recorded at 532 nm. A calibration curve was plotted using MDA tetrabutylammonium. MDA levels were expressed as nmoL/g tissue [22].
The GSH level in rat brain tissue was measured based on the method of Ellman [14]. In this method, DTNB is reduced by -SH groups to form 2-nitro-5-mercaptobenzoic acid. The nitromercaptobenzoic acid anion released has an intense yellow color and can be used to determine the presence of -SH groups. The absorbance of this yellow component was measured at 412 nm and compared with the standard curve to determine the GSH concentration. The levels of reduced GSH were reported as nmoL/g tissue.
The AChE assay was performed according to the colorimetric method of Ellman [14] by using acetylthiocholine iodide as a substrate .The reaction of the thiol compound with DTNB forms a complex with absorbance at 405 nm. For this test, 20 μL of sample serum and 100 μL of 5% (w/v) acetylthiocholine iodide solution were added to 3 mL of Elman reagent (0.02% DTNB in 0.1-M sodium dihydrogen phosphate buffer solution, pH = 7.4). The absorbances of different samples were recorded at 0.5 minutes intervals for 2 minutes. The cholinesterase activity was calculated as follows: cholinesterase (mU/ mL, at 25°C) = change in absorbance in 30 s × 23400 [23].
Data are expressed as means ± standard deviation. Statistical differences were evaluated by using the one-way analysis of variance (ANOVA), followed by the Tukey post-hoc test. Additionally, for the Morris water maze test, statistical analyses were performed using the two-way ANOVA, followed by the Bonferroni test. A P-value < 0.05 was considered as significant.
3. Results
3.1. Effects of BA on spatial memory impairment induced by TMT
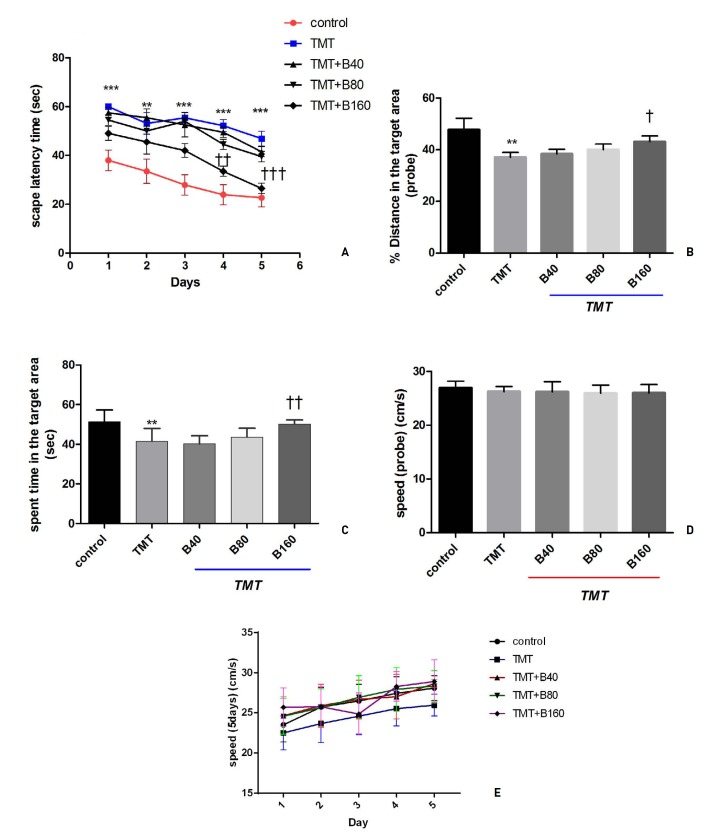
To evaluate spatial memory impairment induced by TMT administration, we used the Morris water maze task. Animals were treated with different doses of BA (40, 80 and 160 mg/ kg) after treatment with TMT at 8 mg/kg. As shown in (Fig. 1)A, the escape latency time (ELT), the time spent to find the platform during five days was measured. Administration of TMT at 8 mg/kg significantly increased the ELT in five days compared with the control group, and the administration of BA at 160 mg/kg to the TMT-treated rats significantly decreased the ELT on days 4 and 5 (P < 0.01 and P < 0.001). The results for the swimming paths indicated that rats in the TMT-treated group and the BA treatment groups often searched for the platform in a wrong way. Thus, the rats took a longer time to locate the platform and had fewer excursions into the target region, thereby making the ELT longer. A statistically significant decrease in the mean ELT was found in B160 group compared with TMT-group lesioned + saline group.
Fig. 1. Effects of BA on spatial working memory following treatment with TMT as determined using the MWM test: (A) escape latency time, (B) % distance in the target area, (C) time spent in the target area, (D) speed on the probe day, (E) speeds on the 5 days of the test. Animals were treated with different doses of BA (40, 80 and 160 mg/ kg) after treatment with TMT at 8 mg/kg. Data are expressed as the means ± SD (n = 8). **P < 0.01 and ***P < 0.001 compared with the control group; †P < 0.05, ††P < 0.01 and †††P < 0.001 compared with the TMT group.
BA, boswellic acid; TMT, trimethyltin; SD, standard deviation; B, boswellic acid.
Fig. 1B shows % distance in the target area (probe). Administration of TMT at 8 mg/kg significantly decreased the distance compared with the control group (P < 0.01), and the administration of BA at 160 mg/kg significantly increased the distance as compared with the TMT-lesioned + saline group (P < 0.05). During the test trial, the percentage of distance traveled in quadrant 1 (Q1) in the control group was higher than it was in the TMT-treated groups. Moreover, the percentage of distance traveled in Q1 for the B160 group was increased significantly.
Fig. 1C shows the spent time in the target area (probe) (s). Administration of TMT at 8 mg/kg decreased the time the rats spent in the target area compared with the control group (P < 0.01), and the treatment of rats with BA at 160 mg/kg significantly increased that time compared with the TMT-lesioned + saline group (P < 0.01). In the final test trials, the swimming time spent in Q1 (the target quadrant) was used to estimate retention. In this case, the TMT-lesioned + saline group spent more time swimming in the target quadrant compared with the control group. Moreover, the rats in the B160 group spent more time swimming in the target quadrant than (Fig. 1)D and (Fig. 1)E show the rats in the TMT-lesioned + saline group. Finally, (Fig. 1)D and (Fig. 1)E shows the measured swimming speeds of the test (cm/s) on the probe day and during the 5 days of the test respectively. Results showed the swimming speeds did not differ among the groups.
3.2. Biochemical findings
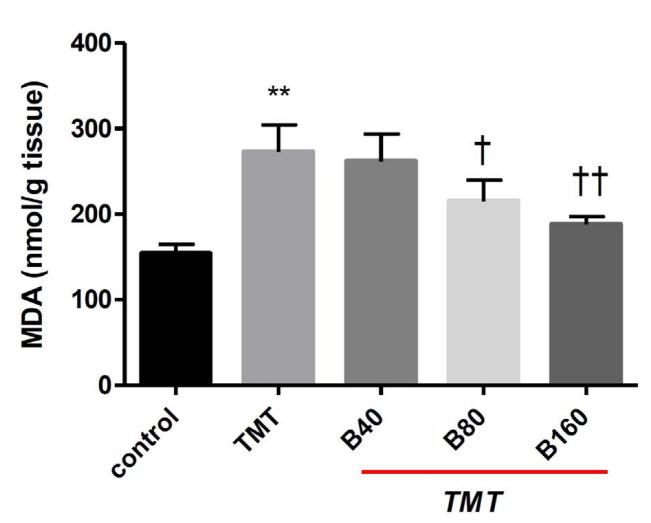
As Fig. 2 shows, exposure to TMT increased the level of MDA in the cortex of brain tissue compared with the control group (P < 0.01). Remarkably, in the B80 (P < 0.05) and the B160 (P < 0.01) groups, the levels of MDA in brain tissue were significantly decreased in comparison with that in the TMT-lesioned + saline group. However, the MDA levels in the rats in the B40 groups were not significantly different from those in the TMT-lesioned + saline group.
Fig. 2. Effect of BA on lipid peroxidation in the cerebral cortex following treatment with TMT. Animals were treated with different doses of BA (40, 80 and 160 mg/kg) after treatment with TMT at 8 mg/ kg. Data are expressed as the means ± SD (n = 8). **P < 0.01 compared with the control group; †P < 0.05 and ††P < 0.01 compared with the TMT-lesioned + saline group.
BA, boswellic acid; TMT, trimethyltin; SD, standard deviation.
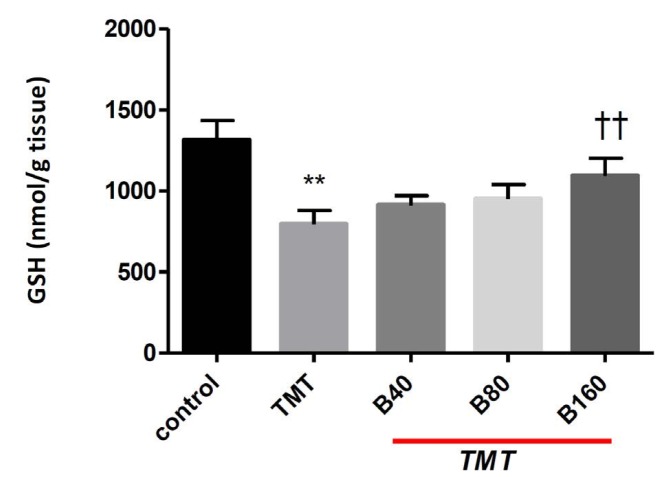
As Fig. 3 shows, a significant decrease in the level of GSH was observed in TMT-lesioned + saline group compared with the control group (P < 0.01). Furthermore, the GSH levels for the rats in the B40 and B80 groups were not significantly different from the GSH levels in the TMT-lesioned + saline group. However, the rats in the B160 group showed significantly increased GSH levels compared with the GSH levels in the rats in the TMT-lesioned + saline group (P < 0.01).
Fig. 3. Effect of BA on GSH content in the cerebral cortex following treatment with TMT. Animals were treated with different doses of BA (40, 80 and 160 mg/ kg) after treatment with TMT at 8 mg/kg). Data are expressed as the means ± SD (n = 8). **P < 0.01 compared with the control group; ††P < 0.01 compared with the TMT-lesioned + saline group.
BA, boswellic acid; GSH, glutathione; TMT, trimethyltin; SD, standard deviation.
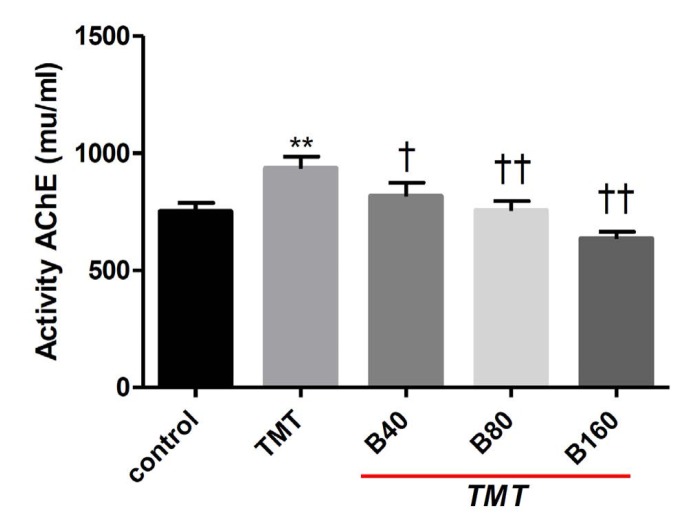
The activity of AChE was significantly increased in the rats in the TMT-lesioned + saline group compared to the control group (P < 0.01) (Fig. 4) whereas all groups treated with BA at any of the three doses used in this study exhibited a significant inhibitory effect against AChE. Thus, treatments with any of the three different doses of BA (40, 80 and 160 mg/kg) used in this research led to significant reductions in AChE activity compared to that in the TMT-lesioned + saline group.
Fig. 4. Effect of BA on AChE activity in serum samples following treatment with TMT. Animals were treated with different doses of BA (40, 80 and 160 mg/ kg) after they had been treatment with TMT at 8 mg/kg. Data are expressed as the means ± SD (n = 8). **P < 0.01 compared with the control group; †P < 0.05 and ††P < 0.01 compared with the TMT-treated + saline group.
BA, boswellic acid; AChE, acetylcholinesterase; TMT, trimethyltin; SD, standard deviation.
4. Discussion
Treatment with TMT induced learning and memory impairment in Wistar rats, and treatment with BA at a dose of 160 mg/kg markedly improved learning and memory abilities on the water maze tasks. Additionally, the activity of AChE was significantly elevated following exposure to TMT whereas all groups treated with BA presented a significant inhibitory effect against AChE. Administration of TMT reduced GSH content and increased the level of MDA in the cerebral cortex while treatment with BA at 160 mg/kg increased the GSH content and decreased the TMT-induced lipid peroxidation in rat brain tissue.
The pathogenesis of TMT neurotoxicity is a complex event; it contains multiple processes such as glutamate excitotoxicity and impairment of neurotransmission with oxidative stress [24, 25]. A suggestion has been made that TMT causes neuronal oxidative stress and increases the free radical production, which is a potential contributor in apoptotic cell death [26]. Several studies have shown that lipid peroxidation and oxidative stress are increased in TMT-induced neurotoxicity [7, 27]. Moreover, free radial scavengers have an important role in protection against TMT-induced neurotoxicity in experimental animals.
The possibility of BA being an antioxidant and memory enhancer makes this agent an ideal choice as a neuroprotective agent. For manifestation of oxidative damage, MDA, the end product of lipid peroxidation generated in tissues by free radical injury, is considered to be a sensitive biomarker. In the present experiment, MDA was significantly higher in animals treated only with TMT. Many researchers have found lipid peroxidation changes in brain tissue after treatment with TMT [7, 27]. As mentioned in the results, lipid peroxidation returned to near control levels in the B80 and the B160 groups. On the other hand, a major antioxidant, which protects cells against oxidative stress, is GSH [28]. Exposure to TMT induces oxidative stress, which decreases the GSH levels and reflects the degree of oxidative insult. In this study, GSH was measured in all groups, and a significant depletion of GSH was observed in the rats treated only with TMT. A decrease in GSH levels is an important factor in TMT-induced neurotoxicity. Several reports have indicated that GSH depletion is a critical factor in the induction of oxidative stress [5, 6, 29, 30]. GSH depletion accelerates signaling processes, leading to neuronal death and central excitabilities. Therefore, depletion of endogenous GSH invariably sensitizes an animal to TMT-induced neuronal damage [6]. In the present study, rats treated with 160 mg/kg of BA showed increased GSH levels, which is evidence for a compromised antioxidant defense. An elevated level of GSH may be part of a protective mechanism to reduce neuronal damage.
Previous studies have reported that BA has an efficient antioxidant activity [16, 17, 19]. Hartmann et al evaluate the antioxidant effect of an extract of the plant Boswellia serrata (B. serrata), which consists of BA, in an experimental model of acute ulcerative colitis induced by administration of acetic acid in rats [17]. They suggested that B. serrata acted by inhibiting lipid peroxidation. Assimopoulou et al reported that B. serrata resin could additionally be used as a natural antioxidant in cosmetics and pharmaceutical preparations [16]. In the research of Sabina et al treatment with BA normalized the levels of lipid peroxidation and antioxidant status in mice with inflammation induced by using monosodium-urate crystals. They suggested that the effect of BA was similar to that of other pentacyclic triterpenes, such as ursolic acid and lutein [19]. Moreover, several researchers have reported the efficacy of agents with antioxidant activity in reducing TMT-induced neurotoxicity. Kuar et al suggested that a prophylactic treatment with Ginkgo biloba extract protected against TMT-induced neurodegeneration because of its antioxidant effects [7]. The findings of Qu et al showed that the anti-apoptotic effect of lycopene against TMT-induced neurotoxicity was due to its potential antioxidant activity [31]. In the investigations of Shin et al, ascorbate treatment significantly attenuated the early oxidative stress induced by TMT, leading to a persistent deficiency in GSH status [5]. Choi et al reported that quercetin, with its high antioxidant activity, could possess a wide range of beneficial activities for treating neurodegenerative disorders, notably Alzheimer's disease (AD) [32].
Another possible mechanism underlying the beneficial effects of BA in our study is its AchE inhibitory effects. The cholinergic hypothesis was proposed for AD due to cholinergic changes in this disease [33]. Previous research has reported that AChE is significantly increased by TMT treatment. Additionally, neuronal damage in the cholinergic systems of animal models has been reported following exposure to TMT [34]. In our experiment, exposure to TMT led to increased AChE activity whereas BA treatment effectively reduced the activity of AchE in the serum samples. Therefore, another protective mechanism of BA in TMT-induced memory dysfunction may be mediated through inhibition of AChE activity. In another study, the ethyl acetate fraction from onion (Allium cepa L.) flesh and peel significantly reduced TMT-induced learning and memory impairment in mice due to AChE inhibition [33].
Obviously, TMT is a neurotoxin that induces neural damage, which leads to behavioral and learning deficits and disrupts memory [35, 36]. Many researchers have proven that TMT causes a degeneration of the pyramidal neurons in the rat hippocampus and the cortical areas (pyriform cortex, entorhinal cortex and subiculum) connected to the hippocampus, as well as neuronal loss in associated areas [2, 4, 37]. The best way to evaluate the deficits in hippocampal-dependent memory is to use the Morris water maze test. The present study showed impairment in spatial learning in the group treated only with TMT, which agrees with the results in previous reports on spatial learning impairments [35, 39]. Moreover, the results of the current study indicated that the spatial memory improved during the training days when the dose of BA in the treatment groups was increased. This finding is in agreement with the results reported by researcher that high antioxidant agents enhance the learning and memory abilities of rats [7, 32, 33].
5. Conclusion
In conclusion, BA effectively ameliorated TMT-induced neurotoxicity through AChE inhibition and antioxidant activity. Therefore, BA may be used as a potential natural resource for mitigating learning and memory dysfunction caused by aging and neurodegenerative diseases.
Footnotes
Conflict of interest The authors declare that there are no conflicts of interest.
References
- 1.Bouldin TW, Goines ND, Bagnell RC, Krigman MR. Pathogenesis of trimethyltin neuronal toxicity. ultrastructural and cytochemical observations. Am J Pathol. 1981;104(3):237–249. [PMC free article] [PubMed] [Google Scholar]
- 2.Dyer RS, Walsh TJ, Wonderlin WF, Bercegeay M. The trimethyltin syndrome in rats. Neurobehav Toxicol Teratol. 1982;4(2):127–133. [PubMed] [Google Scholar]
- 3.Fortemps E, Amand G, Bomboir A, Lauwerys R, Laterre EC. Trimethyltin poisoning. report of two cases. Int Arch Occup Environ Health. 1978;41(1):1–6. doi: 10.1007/BF00377794. [DOI] [PubMed] [Google Scholar]
- 4.Brown AW, Aldridge WN, Street BW, Verschoyle RD. The behavioral and neuropathologic sequelae of intoxication by trimethyltin compounds in the rat. Am J Pathol. 1979;97(1):59–82. [PMC free article] [PubMed] [Google Scholar]
- 5.Shin EJ, Suh SK, Lim YK, Jhoo WK, Hjelle OP, Ottersen OP et al. Ascorbate attenuates trimethyltin-induced oxidative burden and neuronal degeneration in the rat hippocampus by maintaining glutathione homeostasis. Neuroscience. 2005;133(3):715–727. doi: 10.1016/j.neuroscience.2005.02.030. [DOI] [PubMed] [Google Scholar]
- 6.Yoneyama M, Nishiyama N, Shuto M, Sugiyama C, Kawada K, Seko K et al. In vivo depletion of endogenous glutathione facilitates trimethyltin-induced neuronal damage in the dentate gyrus of mice by enhancing oxidative stress. Neurochem Int. 2008;52(4-5):761–769. doi: 10.1016/j.neuint.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Kaur S, Chhabra R, Nehru B. Ginkgo biloba extract attenuates hippocampal neuronal loss and cognitive dysfunction resulting from trimethyltin in mice. Phytomedicine. 2013;20(2):178–186. doi: 10.1016/j.phymed.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Stavric B. Role of chemopreventers in human diet. Clin Biochem. 1994;27(5):319–332. doi: 10.1016/0009-9120(94)00039-5. [DOI] [PubMed] [Google Scholar]
- 9.Hosseinzadeh H, Sadeghnia HR, Ghaeni FA, Motamedshariaty VS, Mohajeri SA. Effects of saffron (Crocus sativus L.) and its active constituent, crocin, on recognition and spatial memory after chronic cerebral hypoperfusion in rats. Phytother Res. 2012;26(3):381–386. doi: 10.1002/ptr.3566. [DOI] [PubMed] [Google Scholar]
- 10.Hosseinzadeh H, Karimi G, Nobakht N. Effects of Rosmarinus officinalis L. aerial parts essential oil on intact memory and scopolamine-induced learning deficits in rats performing the morris water maze task. J Medicinal Plants. 2004;4(12):51–57. [Google Scholar]
- 11.Zhao W, Entschladen F, Liu H, Niggemann B, Fang Q, Zaenker KS et al. Boswellic acid acetate induces differentiation and apoptosis in highly metastatic melanoma and fibrosarcoma cells. Cancer Detect Prev. 2003;27(1):67–75. doi: 10.1016/s0361-090x(02)00170-8. [DOI] [PubMed] [Google Scholar]
- 12.Poeckel D, Werz O. Boswellic acids: biological actions and molecular targets. Curr Med Chem. 2006;13(28):3359–3369. doi: 10.2174/092986706779010333. [DOI] [PubMed] [Google Scholar]
- 13.Ammon H. Boswellic acids in chronic inflammatory diseases. Planta Med. 2006;72(12):1100–1116. doi: 10.1055/s-2006-947227. [DOI] [PubMed] [Google Scholar]
- 14.Forouzanfar F, Hosseinzadeh H, Ebrahimzadeh Bideskan, A, Sadeghnia HR. Aqueous and ethanolic extracts of Boswellia serrata protect against focal cerebral ischemia and reperfusion injury in rats. Phytother Res. 2016;30(12):1954–1967. doi: 10.1002/ptr.5701. [DOI] [PubMed] [Google Scholar]
- 15.Hosseinzadeh H, Ramezani M, Akhtar Y, Ziaei T. Effects Boswellia carterii gum resin fractions on intact memory and hyoscine-induced learning impairments in rats performing the morris water maze task. J Med Plants. 2010;2(34):95–101. [Google Scholar]
- 16.Assimopoulou AN, Zlatanos SN, Papageorgiou VP. Antioxidant activity of natural resins and bioactive triterpenes in oil substrates. Food Chem. 2005;92(4):721–727. [Google Scholar]
- 17.Hartmann RM, Morgan Martins, MI, Tieppo J, Fillmann HS, Marroni NP. Effect of Boswellia serrata on antioxidant status in an experimental model of colitis rats induced by acetic acid. Dig Dis Sci. 2012;57(8):2038–2044. doi: 10.1007/s10620-012-2134-3. [DOI] [PubMed] [Google Scholar]
- 18.Jaberian H, Piri K, Nazari J. Phytochemical composition and in vitro antimicrobial and antioxidant activities of some medicinal plants. Food Chem. 2013;136(1):237–244. doi: 10.1016/j.foodchem.2012.07.084. [DOI] [PubMed] [Google Scholar]
- 19.Sabina EP, Indu H, Rasool M. Efficacy of boswellic acid on lysosomal acid hydrolases, lipid peroxidation and anti- oxidant status in gouty arthritic mice. Asian Pac J Trop Biomed. 2012;2(2):128–133. doi: 10.1016/S2221-1691(11)60206-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shim HS, Park HJ, Ahn YH, Her S, Han JJ, Hahm DH et al. Krill-derived phosphatidylserine improves TMT-induced memory impairment in the rat. Biomol Ther. 2012;20(2):207–213. doi: 10.4062/biomolther.2012.20.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morris R. Developments of a water-maze procedure for studying spatial learning in the rat. J Neurosci Methods. 1984;11(1):47–60. doi: 10.1016/0165-0270(84)90007-4. [DOI] [PubMed] [Google Scholar]
- 22.Mihara M, Uchiyama M. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal Biochem. 1978;86(1):271–278. doi: 10.1016/0003-2697(78)90342-1. [DOI] [PubMed] [Google Scholar]
- 23.Razavi M, Hosseinzadeh H, Abnous K, Motamedshariaty VS, Imenshahidi M. Crocin restores hypotensive effect of subchronic administration of diazinon in rats. Iran J Basic Med Sci. 2013;16(1):64–72. [PMC free article] [PubMed] [Google Scholar]
- 24.Gasso S, Sanfeliu C, Sunol C, Rodriguez-Farre E, Cristofol RM. Trimethyltin and triethyltin differentially induce spontaneous noradrenaline release from rat hippocampal slices. Toxicol Appl Pharmacol. 2000;162(3):189–196. doi: 10.1006/taap.1999.8845. [DOI] [PubMed] [Google Scholar]
- 25.Jenkins SM, Barone S. The neurotoxicant trimethyltin induces apoptosis via caspase activation, p38 protein kinase, and oxidative stress in PC12 cells. Toxicol lett. 2004;147(1):63–72. doi: 10.1016/j.toxlet.2003.10.023. [DOI] [PubMed] [Google Scholar]
- 26.Thompson TA, Lewis JM, Dejneka NS, Severs WB, Polavarapu R, Billingsley ML. Induction of apoptosis by organotin compounds in vitro: neuronal protection with antisense oligonucleotides directed against stannin. J Pharmacol Exp Ther. 1996;276(3):1201–1216. [PubMed] [Google Scholar]
- 27.Kim JK, Choi SJ, Bae H, Kim CR, Cho HY, Kim YJ et al. Effects of methoxsalen from Poncirus trifoliata on acetylcholinesterase and trimethyltin-induced learning and memory impairment. Biosci Biotechnol Biochem. 2011;75(10):1984–1989. doi: 10.1271/bbb.110386. [DOI] [PubMed] [Google Scholar]
- 28.Karpiak VC, Eyer CL. Differential gliotoxicity of organotins. Cell Biol Toxicol. 1999;15(4):261–268. doi: 10.1023/a:1007667830022. [DOI] [PubMed] [Google Scholar]
- 29.Cookson MR, Slamon ND, Pentreath VW. Glutathione modifies the toxicity of triethyltin and trimethyltin in C6 glioma cells. Arch Toxicol. 1998;72(4):197–202. doi: 10.1007/s002040050488. [DOI] [PubMed] [Google Scholar]
- 30.Gunasekar PG, Mickova V, Kotyzova D, Li L, Borowitz JL, Eybl V et al. Role of astrocytes in trimethyltin neurotoxicity. J Biochem Mol Toxicol. 2001;15(5):256–262. doi: 10.1002/jbt.10004. [DOI] [PubMed] [Google Scholar]
- 31.Qu M, Zhou Z, Chen C, Li M, Pei L, Chu F et al. Lycopene protects against trimethyltin-induced neurotoxicity in primary cultured rat hippocampal neurons by inhibiting the mitochondrial apoptotic pathway. Neurochem Int. 2011;59)8):1095–1103. doi: 10.1016/j.neuint.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Choi GN, Kim JH, Kwak JH, Jeong CH, Jeong HR, Lee U et al. Effect of quercetin on learning and memory performance in ICR mice under neurotoxic trimethyltin exposure. Food Chem. 2012;132(2):1019–1024. [Google Scholar]
- 33.Bohnen NI, Kaufer DI, Hendrickson R, Ivanco LS, Lopresti B, Davis JG et al. Cognitive correlates of alterations in acetylcholinesterase in Alzheimer's disease. Neurosci Lett. 2005;380(1-2):127–132. doi: 10.1016/j.neulet.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 34.Morita Y, Yanagida D, Shintani N, Ogita K, Nishiyama N, Tsuchida R et al. Lack of trimethyltin (TMT)-induced elevation of plasma corticosterone in PACAP-deficient mice. Ann N Y Acad Sci. 2006;1070(1):450–456. doi: 10.1196/annals.1317.060. [DOI] [PubMed] [Google Scholar]
- 35.Alessandri B, FitzGerald RE, Schaeppi U, Krinke GJ, Classen W. The use of an unbaited tunnel maze in neurotoxicology: I. trimethyltin-induced brain lesions. Neurotoxicology. 1993;15(2):349–357. [PubMed] [Google Scholar]
- 36.Swartzwelder H. Impaired maze performance in the rat caused by trimethyltin treatment: problem-solving deficits and perseveration. Neurobehavioral Toxicology & Teratology. 1982;4(2):169–176. [PubMed] [Google Scholar]
- 37.Balaban CD, O’Callaghan JP, Billingsle ML. Trimethyltin- induced neuronal damage in the rat brain: comparative studies using silver degeneration stains, immunocytochemistry and immunoassay for neuronotypic and gliotypic proteins. Neuroscience. 1988;26(1):337–361. doi: 10.1016/0306-4522(88)90150-9. [DOI] [PubMed] [Google Scholar]
- 38.Chang LW, Dyer RS. Trimethyltin induced pathology in sensory neurons. Neurobeh Toxicol Teratol. 1983;5(6):673–696. [PubMed] [Google Scholar]
- 39.Koczyk D. How does trimethyltin affect the brain: facts and hypotheses. Acta Neurobiol Exp. 1995;56(2):587–596. doi: 10.55782/ane-1996-1164. [DOI] [PubMed] [Google Scholar]
- 40.Earley B, Burke M, Leonard BE. Behavioural, biochemical and histological effects of trimethyltin (TMT) induced brain damage in the rat. Neurochem Int. 1992;21(3):351–366. doi: 10.1016/0197-0186(92)90186-u. [DOI] [PubMed] [Google Scholar]
- 41.Hagan JJ, Jansen JH, Broekkamp CL. Selective behavioural impairment after acute intoxication with trimethyltin (TMT) in rats. Neurotoxicology. 1987;9(1):53–74. [PubMed] [Google Scholar]
- 42.Walsh TJ, Miller DB, Dyer RS. Trimethyltin, a selective limbic system neurotoxicant, impairs radial-arm maze performance. Neurobeh Toxicol Teratol. 1982;4(2):177–183. [PubMed] [Google Scholar]
- 43.Woodruff ML, Baisden RH, Cannon RL, Kalbfleisch J, Freeman JN., 3rd Effects of trimethyltin on acquisition and reversal of a light-dark discrimination by rats. Physiol Behav. 1994;55(6):1055–1061. doi: 10.1016/0031-9384(94)90387-5. [DOI] [PubMed] [Google Scholar]