Abstract
Objectives:
Neutrophils represent the front line of human defense against infections. Immediately after stimulation, neutrophilic enzymes are activated and produce toxic mediators such as pro-inflammatory cytokines, nitric oxide (NO) and myeloperoxidase (MPO). These mediators can be toxic not only to infectious agents but also to host tissues. Because flavonoids exhibit antioxidant and anti-inflammatory effects, they are subjects of interest for pharmacological modulation of inflammation. In the present study, the effects of rutin on stimulus-induced NO and tumor necrosis factor (TNF)-α productions and MPO activity in human neutrophils were investigated.
Methods:
Human peripheral blood neutrophils were isolated using Ficoll-Hypaque density gradient centrifugation coupled with dextran T500 sedimentation. The cell preparations containing > 98% granulocytes were determined by morphological examination through Giemsa staining. Neutrophils were cultured in complete Roswell Park Memorial Institute (RPMI) medium, pre-incubated with or without rutin (25 μM) for 45 minutes, and stimulated with phorbol 12-myristate 13-acetate (PMA). Then, the TNF-α, NO and MPO productions were analyzed using enzyme-linked immunosorbent assay (ELISA), Griess Reagent, and MPO assay kits, respectively. Also, the viability of human neutrophils was assessed using tetrazolium salt 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT), and neutrophils were treated with various concentrations of rutin (1 - 100 μM), after which MTT was appended and incubated at 37ºC for 4 hour.
Results:
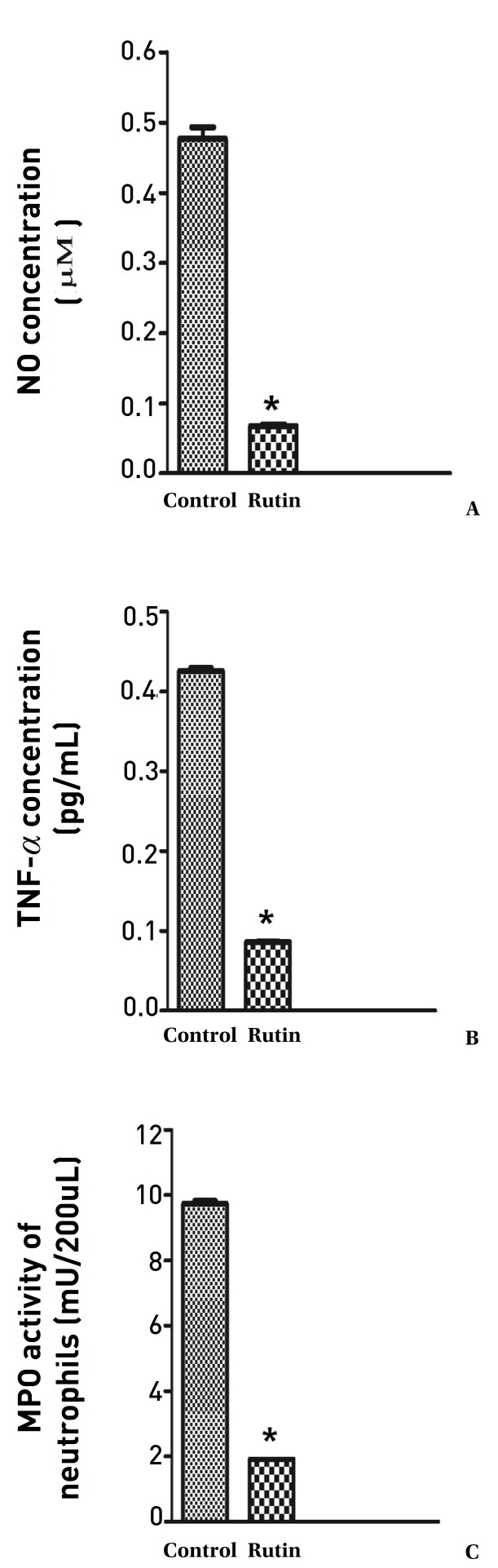
Rutin at concentrations up to 100 μM did not affect neutrophil viability during the 4-hour incubation period. Rutin significantly decreased the NO and TNF-α productions in human peripheral blood neutrophils compared to PMA-control cells (P < 0.001). Also, MPO activity was significantly reduced by rutin (P < 0.001).
Conclusion:
In this in vitro study, rutin had an anti-inflammatory effect due to its inhibiting NO and TNF-α productions, as well as MPO activity, in activated human neutrophils. Treatment with rutin may be considered as a therapeutic strategy for neutrophil-mediated inflammatory/ autoimmune diseases.
Keywords: human neutrophils, myeloperoxidase, nitric oxide, rutin, tumor necrosis factor-α
1. Introduction
A neutrophil is a type of phagocyte that sweeps up pathogens into the phagosome and fuses them with granules containing toxic compounds, such as reactive oxygen species (ROS) produced by oxidant enzymes such as myeloperoxidase (MPO), to annihilate those pathogens [1]. Activated neutrophils begin to produce reactive nitrogen and oxygen species (RNOS) such as hydrogen peroxide (H2O2), which is a substrate for MPO to produce a potent oxidant compound [2], and nitric oxide (NO), which is produced by inducible NO synthase (iNOs) and forms reactive species or is transformed into another substrate for MPO [3]. Major compounds that are receiving attention nowadays because of their anti-inflammatory and antioxidant activities are the flavonoids [4].
One of the important flavonoids is rutin (3,3´,4´,5,7-pentahydroxy flavone-3-rutinoside), which is a glycone of quercetin (also known as quercetin-3-rutinoside) and is found in various fruits and vegetables, such as apple peels, potatoes, tomatoes, carrots, oranges, grapefruits, lemons, etc. [5, 6]. Rutin (also called vitamin P) has been shown to have excellent therapeutic effects, such as anti-inflammatory [7], antioxidant [8], anti-allergic [9], neuroprotective [10, 11], and antiplatelet [12] activities. Rutin has been reported to have protective effects against acute lung injury via inhibition of neutrophil infiltration and iNOS gene expression [13]. In rats, pretreatment with rutin can decrease oxidative stress, the systemic level of increased tumor necrosis factor (TNF)-α in renal inflammation, and apoptosis induced by cisplatin in rats [14]. The aim of this study was to investigate the anti-inflammatory effects of rutin against phorbol 12-myristate 13-acetate (PMA)-induced neutrophil stimulation by evaluating its potential modulatory role in tissue necrosis factor-α and NO production and in MPO activity.
2. Materials and Methods
The protocol used in this study was approved by the local ethics committee of Qazvin University of Medical Sciences (28.20.8991). Neutrophils were isolated from freshly heparinized (5 U/mL) venous blood from healthy volunteers by using Ficoll-Hypaque solution and Dextran T500. In this method, 5 mL of blood was layered onto 5 mL of Ficoll solution and centrifuged at 400 g for 30 minutes (min) at room temperature (RT) [15]. After centrifugation, the layer containing erythrocytes and neutrophils was harvested using a sterile Pasteur pipette. Then, Dextran sedimentation was carried out with a 3% dextran solution. A suspension of erythrocytes and neutrophils was mixed with 3% dextran for 30 min at RT in a dark room. After sedimentation, the neutrophil-rich supernatant in the upper layer was collected and centrifuged for 5 min at 200 g at RT. Red blood cell (RBC) lysis was performed to gain pure neutrophils. After dextran sedimentation, the remaining RBCs were lysed using the hypotonic lysis method. A neutrophil/ RBC pellet was suspended in 20 mL of cold 0.2% NaCl for 30 s; then, isotonicity was restored by adding 20 mL of icecold 1.6% NaCl. The hypotonic lysis step is based on the high sensitivity of RBC to hypotonicity in comparison with neutrophils. However, the 30-s limit must be carefully monitored because a more prolonged period of hypotonicity will result in neutrophil damage. After centrifugation, the supernatant was discarded, and a white pellet consisting of neutrophils was obtained and re-suspended immediately in RPMI 1640 complete medium supplemented with 10% fetal calf serum (FCS). After lysis, the morphological examinations and the trypan-blue exclusion tests were performed to determine the cell count and the purity of the neutrophils. The viability of the cells was more than 98%, as assessed by using the trypan- blue exclusion test. The cell preparations contained more than 98% neutrophils, as determined by using morphological examinations based on Giemsa staining.
Cell viability and cytotoxicity assays are used for drug screening and cytotoxicity tests of chemicals. In this study, the viability of human neutrophils was assessed using tetrazolium salt 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) (Sigma, USA). Mitochondrial dehydrogenase enzymes reduce MTT to an insoluble, colored formazan product. Neutrophils were treated with various concentrations of rutin (1 - 100 μM) (Sigma), which was dissolved in dimethylsulfoxide (DMSO), for 2 h, after which MTT (5 mg/ mL) was appended, and the sample was incubated at 37ºC for 4 h. Then, 0.04-N HCl in isopropanol was used to stop the reaction. Neutrophils were harvested, and the blue crystals of formazan were dissolved in DMSO for 10 min. The absorbency was measured at a reference wavelength of 630 nm and a test wavelength of 570 nm by using a spectrophotometer. Cell viability was determined by comparing the absorbency of the treated and the untreated cells.
NO production was determined by measuring the nitrite content in the supernatant of the neutrophil culture [16]. The spectrophotometric analysis of the total nitrite content was performed by using Griess reagent (1% sulfanilic acid, 0.1% N-1-naphthyl-ethylenediamine dihydrochloride). Neutrophils (5 × 105/well) in RPMI 1640 medium were treated with and without 25-μM rutin for 45 min and then stimulated with phorbol 12-myristate 13-acetate (PMA) (10–7 M) for 4 h. Then, 100 μL of Griess reagent was added to 100 μL of the supernatant of the cell culture. After a 15-min incubation at RT, the absorbance was measured at 550 nm by using a spectrophotometer. The nitrite concentration was determined using sodium nitrite as a standard (0 - 60 μM).
Cytokine TNF-α production in the supernatant of the cell culture was determined by using enzyme-linked immunosorbent assay (ELISA) kits according to the manufacturer’s instructions (eBioscience, USA). Neutrophils (1 × 106/mL) were cultured with and without 25-μM rutin, after which 10–7- M PMA was added for 6 h. Finally, the cells were centrifuged (1,000 g, 4ºC, 10 min), and the supernatant was collected and used for the cytokine assessments.
The activity of the MPO enzyme was measured using MPO assay kits according to the manufacturer’s instructions (Abcam, UK). Neutrophils (2 × 106 cells/well) were exposed for 45 min at 37ºC with and without 25-μM rutin, after which 10–7-M PMA was added for 2 h. In Abcam’s MPO Activity Assay Kit, the HClO produced from H2O2 and Cl is reacted with taurine to generate taurine chloramine, which subsequently reacts with the TNB2-probe to eliminate color (λ = 412 nm). The kit provides a rapid, simple, sensitive, and reliable test suitable for high throughput activity assays of MPO. This kit can be used to detect MPO in amounts as low as 0.05 mU per well.
Data were statistically analyzed using GraphPad PrismTM (version 5.0; GraphPad Software). Results are expressed as means ± standard errors of the mean (SEMs). Statistical comparisons between groups were done using the student’s t-test. In all cases, P values lower than 0.05 were considered as statistically significant.
3. Results
Rutin was assessed for its cytotoxicity on neutrophils before the determination of its effects on neutrophil functions. Rutin at concentrations up to 100 μM did not affect neutrophil viability during the 4-h incubation period. Rutin significantly decreased the production of NO compared to that in the PMA-control cells (P < 0.001) (Fig. 1). Neutrophils treated with PMA alone exhibited significantly increased cytokine production. The production of the pro-inflammatory cytokine TNF-α by human neutrophils treated with rutin was signifi- cantly decreased compared with that in the PMA-control cells (P < 0.001) Fig. 1). MPO activity in the neutrophils was evaluated after the cells had been treated with rutin. As compared with the MPO activity in the PMA-control stimulated cells, that in the rutin-treated cells was significantly reduced (P < 0.001) (Fig. 1).
Fig. 1. Anti-inflammatory effects of rutin (25 μM) against PMA-induced neutrophil stimulation through evaluation of the potential modulatory role of rutin on (A) NO and (B) TNF-α productions and (C) MPO activity. Data are expressed as means SEMs (n = 10) with 3 repeated experiments; t-test: *P < 0.001, compared to control.
PMA, phorbol 12-myristate 13-acetate; NO, nitric oxide; TNF, tumor necrosis factor; MPO, myeloperoxidase; SEMs, standard errors of the mean.
4. Discussion
Overactivation of neutrophils is associated with excess degranulation, which was obviously seen in this study, as administration of PMA to isolated human peripheral blood neutrophils significantly increased NO and TNF-α productions and MPO activity. Our results showed that pre-incubation of neutrophils with rutin significantly reduced the productions/ activity of these factors. Rutin can effectively inhibit lipopolysaccharide (LPS)-induced iNOs gene expression and subsequent NO production in macrophages [17]. We obtained a similar result in our study as rutin significantly reduced NO from neutrophils in vitro. The mechanism underlying this result in neutrophils may be similar to that in the mentioned studies on macrophages.
Rutin has been found to be able to attenuate the LPS-induced increased serum systemic TNF-α level in D-galactosamine- sensitized mice. However, it was ineffective in reducing serum TNF-α in the presence of a high dose of LPS. Rutin has also been reported to be able to prevent the transcription of more than 20 genes responsible for pro-inflammatory factors such as TNF-α in macrophages [18]. Similar results in decreasing the serum level of TNF-α have been attained due to the effect of rutin on systemic pro-inflammatory cytokines [19], LPS-induced TNF-α production, and TNF-α-mediated vascular barrier disruption [20]. Our finding was in agreement with the results in those studies as rutin remarkably decreased TNF-α production in the neutrophils. As a coincident result with our finding of reduced MPO activity due to rutin treatment, rutin has been reported to bind with a hydrophobic region at the distal heme pocket of the MPO, thus reducing MPO activity, as well as the production of MPO-dependent ROS [21]. Reductions in the MPO activity and the levels of pro-inflammatory cytokines such as TNF-α have also been shown by evaluating the effects of rutin in the treatment of LPS-induced acute lung injury [22]. On the other hand, some studies have demonstrated various effects of rutin on these factors (NO, TNF-α, and MPO). In the mouse pleurisy model, rutin only reduced the production of TNF-α [23]. In another study on rats, rutin was found to significantly attenuate esophageal MPO activity and neutrophil accumulation [24].
5. Conclusion
Our study showed that neutrophils treated with PMA alone exhibited significant increases in NO and TNF-α production and MPO activity whereas neutrophils treated with rutin exhibited significant decreases in NO and TNF-α production and MPO activity. However, the precise cellular mechanisms leading to these effects of rutin on neutrophils are unknown, so more studies are required if those mechanisms are to be identified.
Acknowledgments
The authors are thankful to the Vice Chancellor of Research, Qazvin University of Medical Sciences, for financial support (Grant No. 28.20.8682).
Footnotes
Conflict of interest The authors declare that there are no conflicts of interest.
ORCID Marjan Nassiri-Asl. http://orcid.org/0000-0003-3701-0758.
References
- 1.Faurschou M, Borregaard N. Neutrophil granules and secretory vesicles in inflammation. Microbes Infect. 2003;5(14):1317–1327. doi: 10.1016/j.micinf.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Powers SK, Jackson MJ. Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production. Physiol Rev. 2008;88(4):1243–1276. doi: 10.1152/physrev.00031.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deby-Dupont G, Deby C, Lamy M. Neutrophil myeloperoxidase revisited: it’s role in health and disease. Intensivmed Notfallmed. 1999;36(6):500–513. [Google Scholar]
- 4.Heim KE, Tagliaferro AR, Bobilya DJ. Flavonoid antioxidants: chemistry, metabolism and structure-activity relationships. J Nutr Biochem. 2002;13(10):572–584. doi: 10.1016/s0955-2863(02)00208-5. [DOI] [PubMed] [Google Scholar]
- 5.Fabjan N, Rode J, Kosir IJ, Wang Z, Zhang Z, Kreft I. Tartary buckwheat (Fagopyrum tataricum Gaertn) as a source of dietary rutin and quercitrin. J Agric Food Chem. 2003;51(22):6452–6455. doi: 10.1021/jf034543e. [DOI] [PubMed] [Google Scholar]
- 6.Wang M, Tadmor Y, Wu QL, Chin CK, Garrison SA, Simon JE. Quantification of protodioscin and rutin in asparagus shoots by LC⁄MS and HPLC methods. J Agric Food Chem. 2003;51(21):6132–6136. doi: 10.1021/jf0344587. [DOI] [PubMed] [Google Scholar]
- 7.Yoo H, Ku SK, Baek YD, Bae JS. Anti-inflammatory effects of rutin on HMGB1-induced inflammatory responses in vitro and in vivo. Inflamm Res. 2014;63(3):197–206. doi: 10.1007/s00011-013-0689-x. [DOI] [PubMed] [Google Scholar]
- 8.Nassiri-Asl M, Naserpour Farivar, T, Abbasi E, Sadeghnia HR, Sheikhi M, Lotfizadeh M et al. Effects of rutin on oxidative stress in mice with kainic acid-induced seizure. J Integr Med. 2013;11(5):337–342. doi: 10.3736/jintegrmed2013042. [DOI] [PubMed] [Google Scholar]
- 9.Morimoto Y, Yasuhara T, Sugimoto A, Inoue A, Hide I, Akiyama M et al. Anti-allergic substances contained in the pollen of Cryptomeria japonica possess diverse effects on the degranulation of RBL-2H3 cells. J Pharmacol Sci. 2003;92(3):291–295. doi: 10.1254/jphs.92.291. [DOI] [PubMed] [Google Scholar]
- 10.Moghbelinejad S, Nassiri-Asl M, Farivar TN, Abbasi E, Sheikhi M, Taghiloo M et al. Rutin activates the MAPK pathway and BDNF gene expression on beta-amyloid induced neurotoxicity in rats. Toxicol Lett. 2014;224(1):108–113. doi: 10.1016/j.toxlet.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 11.Motamedshariaty VS, Amel Farzad, S, Nassiri-Asl M, Hosseinzadeh H. Effects of rutin on acrylamide-induced neurotoxicity. Daru. 2014;22(1):27. doi: 10.1186/2008-2231-22-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim DS, Ji HD, Rhee MH, Sung YY, Yang WK, Kim SH et al. Antiplatelet activity of Morus alba leaves extract, mediated via inhibiting granule secretion and blocking the phosphorylation of extracellular-signal-regulated kinase and Akt. . Evid Based Complement Alternat Med. 2014;2014 doi: 10.1155/2014/639548.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang YC, Horng CT, Chen ST, Lee SS, Yang ML, Lee CY et al. Rutin improves endotoxin-induced acute lung injury via inhibition of iNOS and VCAM-1 expression. Environ Toxicol. 2016;31(2):185–191. doi: 10.1002/tox.22033. [DOI] [PubMed] [Google Scholar]
- 14.Arjumand W, Seth A, Sultana S. Rutin attenuates cisplatin induced renal inflammation and apoptosis by reducing NFκB, TNF-α and caspase-3 expression in wistar rats. Food Chem Toxicol. 2011;49(9):2013–2021. doi: 10.1016/j.fct.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 15.Maqbool M, Vidyadaran S, George E, Ramasamy R. Optimisation of laboratory procedures for isolating human peripheral blood derived neutrophils. Med J Malaysia. 2011;66(4):296–299. [PubMed] [Google Scholar]
- 16.Ding AH, Nathan CF, Stuehr DJ. Release of reactive nitrogen intermediates and reactive oxygen intermediates from mouse peritoneal macrophages. comparison of activating cytokines and evidence for independent production. J Immunol. 1988;141(7):2407–2412. [PubMed] [Google Scholar]
- 17.Chen JW, Zhu ZQ, Hu TX, Zhu DY. Structure-activity relationship of natural flavonoids in hydroxyl radical-scavenging effects. Acta Pharmacol Sin. 2002;23(7):667–672. [PubMed] [Google Scholar]
- 18.Kauss T, Moynet D, Rambert J, Al-Kharrat A, Brajot S, Thiolat D et al. Rutoside decreases human macrophage derived inflammatory mediators and improves clinical signs in adjuvant induced arthritis. . Arthritis Res Ther. 2008;10(1) doi: 10.1186/ar2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lago JH, Toledo-Arruda AC, Mernak M, Barrosa KH, Martins MA, Tibério IF et al. Structure-activity association of flavonoids in lung diseases. Molecules. 2014;19(3):3570–3595. doi: 10.3390/molecules19033570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee W, Ku SK, Bae JS. Barrier protective effects of rutin in LPS-induced inflammation in vitro and in vivo. Food Chem Toxicol. 2012;50(9):3048–3055. doi: 10.1016/j.fct.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 21.Shiba Y, Kinoshita T, Chuman H, Taketani Y, Takeda E, Kato Y et al. Flavonoids as substrates and inhibitors of myeloperoxidase: molecular actions of aglycone and metabolites. Chem Res Toxicol. 2008;21(8):1600–1609. doi: 10.1021/tx8000835. [DOI] [PubMed] [Google Scholar]
- 22.Yeh CH, Yang JJ, Yang ML, Li YC, Kuan YH. Rutin decreases lipopolysaccharide-induced acute lung injury via inhibition of oxidative stress and the MAPK-NF-κB pathway. Free Radic Biol Med. 2014;69:249–257. doi: 10.1016/j.freeradbiomed.2014.01.028. [DOI] [PubMed] [Google Scholar]
- 23.Arruda-Silva F, Nascimento MV, Luz AB, Venzke D, Queiroz GS, Fröde TS et al. Polygala molluginifolia A. St.-Hil. and Moq. prevent inflammation in the mouse pleurisy model by inhibiting NF-κB activation. Int Immunopharmacol. 2014;19(2):334–341. doi: 10.1016/j.intimp.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 24.Shin YK, Sohn UD, Choi MS, Kum C, Sim SS, Lee MY. Effects of rutin and harmaline on rat reflux oesophagitis. Auton Autacoid Pharmacol. 2002;22(1):47–55. doi: 10.1046/j.1474-8673.2002.00241.x. [DOI] [PubMed] [Google Scholar]