Abstract
Objective:
Converging lines of research suggest that adolescents’ smoking behaviors are strongly influenced by the characteristics of their social network and the social processes their network facilitates. The primary goal of this study was to conduct a detailed comparison of the social networks of adolescent smokers and nonsmokers to determine what aspects relate the most to smoking status. A secondary goal was to conduct within-group analyses to examine relationships between key measures of behavior-specific social support and (a) smoking susceptibility among nonsmokers, and (b) readiness to quit smoking among smokers.
Method:
A matched sample of 190 adolescent smokers and nonsmokers (Mage = 16.8 years; 51% female) completed a questionnaire in which they nominated and reported on up to 10 important people in their lives. This measure allowed us to examine adolescents’ overall networks (both peers and family) and to investigate numerous aspects, including general network characteristics (e.g., size of network, average contact with network members), social support (e.g., importance of people in the network), and the pervasiveness of smoking in the network (e.g., percentage of smoking peers).
Results:
The pervasiveness of smoking in adolescents’ social network was the strongest distinguisher of smokers versus nonsmokers. In addition, behavior-specific social support was strongly associated with susceptibility to initiate smoking among nonsmokers and readiness to quit among smokers.
Conclusions:
This research offers insight into potential targets for prevention and early intervention by demonstrating how social networks can both promote and attenuate risk for smoking.
Despite declines in cigarette use over the last 15 years, reductions in adolescent smoking have recently stalled (U.S. Department of Health and Human Services [USDHHS], 2012). Approximately 16% of 8th graders and 40% of 12th graders report having smoked a cigarette in their lifetime (Johnston et al., 2013). Early cigarette smoking is related to an array of negative health outcomes in the short term (Gilliland et al., 2006; Gold et al., 1996) and life-threatening diseases in the long term (Fagerström, 2002; Huxley, 2012). Furthermore, with nearly 90% of smoking initiation occurring during adolescence (USDHHS, 2012), reducing the prevalence of adolescent smoking is crucial for long-term eradication of smoking in the general population. To this end, one important line of research seeks to understand key factors related to the onset and maintenance of adolescent cigarette use (Centers for Disease Control and Prevention, 2011; Lantz et al., 2000; Tyas & Pederson, 1998). Findings from such work point to the strong influence of an adolescent’s social network.
The social context of adolescent smoking
Social networks refer to “the web of social relationships that surround individuals” (Heaney & Israel, 2008, p. 190). Important general network characteristics include its size, the extent to which members are connected, and the frequency of contact among members (Berkman et al., 2000). Substance-specific network characteristics include the percentage of substance users and the amount and type of interactions with substance users (Valente et al., 2004; Zywiak et al., 2002). According to comprehensive models of tobacco use (e.g., Moolchan et al., 2007), as well social psychology perspectives on health (Heaney & Israel, 2008), understanding these types of social network characteristics is crucial for understanding and predicting health behavior. Indeed, current conceptualizations posit that social networks give rise to various social functions; more specifically, they provide the social structure for various interpersonal processes, including the conveying of social support and social norms (Wills & Ainette, 2012).
Social support
Social support refers to information from others that one is loved, valued, cared for, and part of a network of communication and obligation (Cobb, 1976; Cohen & Wills, 1985). A large literature links greater social support with more positive health outcomes at all stages of the life course (Uchino, 2006). During adolescence, supportive relationships often serve as protective factors against risk behaviors—including smoking (Fagan et al., 2001; Wills & Cleary, 1996).
Further investigations into social support’s protective influence have distinguished general social support from behavior-specific social support (Longabaugh et al., 1993; Wilson et al., 1986). General, or global, social support refers to the overall strength and extent of social support. Some adolescent studies have found that greater general social support predicts a lower likelihood of smoking (Johns et al., 2013; So-kum Tang et al., 2011). Yet other adolescent studies have found null or opposite effects (Lakon et al., 2010; Lifrak et al., 1997). These mixed findings point to the need for greater precision and conceptual clarity to identify when specific types of social support are, or are not, protective.
In contrast to general social support, behavior-specific social support refers to support that is directly tied to a certain function (Beattie & Longabaugh, 1999; Groh et al, 2008). For example, there are differences between romantic partners who enable substance use and those who encourage cessation (Falkin & Strauss, 2003). Likewise, differential effects occur based on the extent to which network members support (vs. oppose) drinking and the extent to which they support (vs. oppose) alcohol treatment (Nargiso et al., 2014). Within the context of early cigarette use, research indicates that, compared with adolescent regular smokers, adolescent never-smokers perceived greater objections to their smoking from their social network (Fagan et al, 2001). Likewise, among adult current smokers, greater abstinence-specific social support appears to be beneficial during the early stages of quitting (Lawhon et al., 2009).
Despite these findings highlighting the protective function of social support (both general and behavior-specific) in adolescent smoking, some argue that its role in health is not particularly substantial when compared with other, more strongly predictive factors (e.g., negative interpersonal relations; Heaney & Israel, 2008). Thus, when examining adolescent smoking, it is important to test multivariable models that simultaneously test the contribution of multiple factors. Many of the preceding studies were also constrained by design limitations. For example, smokers and nonsmokers tend to vary on demographic factors, including age, gender, socioeconomic status, and race/ethnicity (Grogan et al., 2009; Hiscock et al., 2012; Trinidad et al., 2004), which present confounds to any observed differences. Overall, more work needs to examine how young smokers and nonsmokers differ on general social support. Furthermore, based on the research described above examining substance use and behavior-specific support, work needs to test whether adolescents’ smoking- and cessation-specific social support influence the likelihood of behavior change (i.e., smoking initiation among nonsmokers and cessation among smokers).
Peer and family smoking
Beyond providing social support, network members can influence adolescents by conveying injunctive and descriptive norms about smoking behavior (Elek et al., 2006; Ennett et al., 2008). As laid out formally in social learning theory (Bandura, 1977) and tested empirically in models of parental influence (Andrews et al., 1993; Otten et al., 2008; Stanton et al., 2014), this influence appears to occur explicitly, through verbal communication, as well as implicitly, via modeling. Accordingly, having parents or other family members who smoke is a risk factor for adolescent smoking initiation (Farkas et al., 2000; Fawzy et al., 1983), especially at early ages (before age 13; Gilman et al., 2009). The influence of family then tends to decline as youth age, such that the influence of peers becomes increasingly important during adolescence (Olds & Thombs, 2001). Thus, numerous studies have demonstrated how friends’ and classmates’ behaviors influence adolescent smoking (e.g., Ennett et al., 2006; Hall & Valente, 2007).
Given the consistency with which research finds family/peer smoking to be a risk factor, we would expect the overall pervasiveness of smoking to be an extremely strong factor distinguishing smokers and nonsmokers. A major limitation to previous studies, however, is that the majority used the school or the classroom as the level of analysis. Thus, they omitted the influence of parents, other family, and peers outside of school. Further work needs to examine these additional network members to understand how adolescent smokers differ from nonsmokers in terms of the overall pervasiveness of smoking in their social networks. Moreover, it would be useful to determine the extent to which the social network factors distinguishing smokers from nonsmokers forecast change in behavior (i.e., initiation and cessation).
Current study
The purpose of the present study was to conduct a detailed comparison of the social networks of adolescent smokers and nonsmokers to determine what aspects relate the most to smoking status. We used a measure of social networks that allowed us to examine adolescents’ overall networks (both peers and family) and to investigate numerous aspects, including general network characteristics (e.g., size of network), social support (e.g., importance of people in the network), and the pervasiveness of smoking in the network (e.g., percentage of smoking peers). Our sample’s adolescent smokers and nonsmokers were closely matched on demographics to reduce the likelihood of confounds. The main hypothesis was that, above all other network factors, pervasiveness of smoking in an adolescent’s social network would be the strongest distinguisher of smokers versus nonsmokers. A secondary goal was to conduct within-group analyses to test relationships between key measures of behavior-specific social support and (a) smoking susceptibility among nonsmokers, and (b) readiness to quit smoking among smokers.
Method
Participants
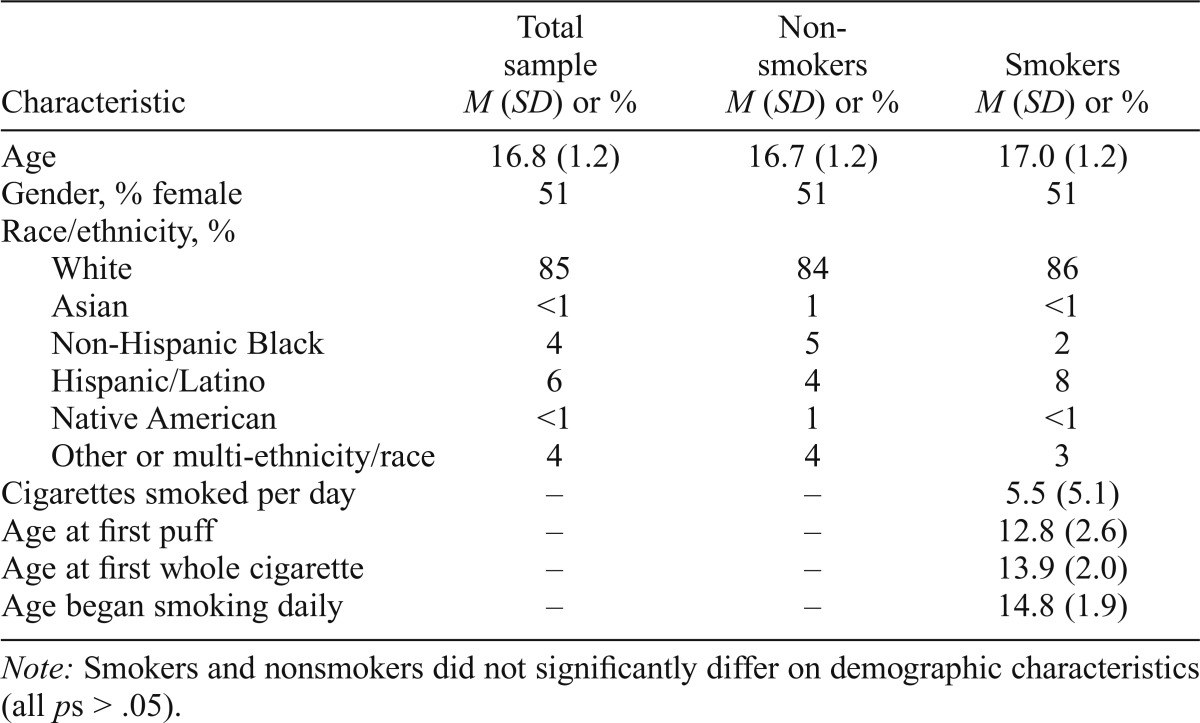
The current study was part of a broader investigation comparing adolescent smokers with nonsmokers on a variety of psychosocial and environmental characteristics. All procedures were approved by Brown University’s Institutional Review Board. Enrolled were 263 high school students, recruited from Rhode Island and Massachusetts communities. The group included a matched sample of 190 adolescent smokers (n = 95) and nonsmokers (n = 95). There were, in addition, several unmatched adolescents, but data from these individuals were not included in present article. See Table 1 for a more detailed description of participants.
Table 1.
Participant characteristics (means or percentages) for whole sample and by smoking status (total sample N = 190)
| Characteristic | Total sample M (SD) or % | Non smokers M (SD) or % | Smokers M (SD) or % |
| Age | 16.8 (1.2) | 16.7 (1.2) | 17.0 (1.2) |
| Gender, % female | 51 | 51 | 51 |
| Race/ethnicity, % | |||
| White | 85 | 84 | 86 |
| Asian | <1 | 1 | <1 |
| Non-Hispanic Black | 4 | 5 | 2 |
| Hispanic/Latino | 6 | 4 | 8 |
| Native American | <1 | 1 | <1 |
| Other or multi-ethnicity/race | 4 | 4 | 3 |
| Cigarettes smoked per day | – | – | 5.5 (5.1) |
| Age at first puff | – | – | 12.8 (2.6) |
| Age at first whole cigarette | – | – | 13.9 (2.0) |
| Age began smoking daily | – | – | 14.8 (1.9) |
Note: Smokers and nonsmokers did not significantly differ on demographic characteristics (all ps > .05).
Sampling and recruitment
Recruitment occurred via (a) newspaper advertisements and (b) posted flyers and informational tables set up in school cafeterias. Youth interested in participating completed a brief screening survey to determine eligibility and provide information for the matching procedure (described below). To be eligible, individuals had to be English speakers, age 14–19, and currently attending high school. Nonsmokers were defined as those who reported never smoking a whole cigarette, not smoking at all (even a puff) in the past year, and not using other forms of tobacco or nicotine in the past 30 days. Smokers were defined as those who reported both (a) smoking cigarettes in the past 14 days and (b) not using other forms of tobacco or nicotine on more than 4 days in the past 30 days.
Matching procedure
Nonsmoker participants were recruited to match enrolled smoker participants on gender, grade (within 1 year), a proxy of socioeconomic status (eligible for free or reduced-price lunch vs. full-pay lunch), racial/ethnic minority status (non-Hispanic White vs. other), and school type (private parochial, private nonparochial, Rhode Island public school, Massachusetts public school). Rhode Island public school students were further matched on school performance (based on statewide testing scores of high performing, moderately performing, or needs improvement); Massachusetts public school students were matched within specific schools.
Study procedure
Participation involved two 90-minute afterschool sessions. In addition to completing paper-and-pencil questionnaires, students provided breath and saliva samples to test for biomarkers of smoking. Sessions took place at school, community locations such as libraries, and Brown University research offices. Participants received $25 for completing each of the two sessions. Written informed consent was obtained from parents of minors and from participants 18 and older; participants 17 and under gave assent before research participation.
Measures
For brevity, only the assessments analyzed for the current study are described below. All of these assessments occurred at the first session.
Demographics.
A demographics questionnaire assessed age, gender, grade, race, and ethnicity.
Smoking behavior.
Smoking versus nonsmoking status was established based on participants’ responses to the screener. Self-reports were confirmed during the study session with breath and saliva samples that tested for biomarkers of smoking (carbon monoxide and cotinine, respectively). During this time, smokers also responded to a Timeline Followback for smoking (Harris et al, 2009; Lewis-Esquerre et al., 2005) to assess the average number of cigarettes smoked per day for the prior 14 days and the Smoking History and Patterns Questionnaire (Colby et al., 2005) to assess age at onset for first puff, first whole cigarette, and daily smoking.
Important People.
We selected a smoking version of the Important People (IP) measure (Longabaugh et al., 1993; Stanton et al., 2009; Zywiak et al., 2002) to assess general and smoking-specific aspects of adolescent social networks. The IP (Longabaugh & Zywiak, 1998) is a structured interview assessing important people in the respondent’s life; it also prompts more specific recall and has no restrictions on type of network members considered. The IP was used originally to evaluate the social networks of adults undergoing alcohol treatment, but has since been adapted to assess other populations and health-risk behaviors. It yields a number of indices that have been shown to predict alcohol and smoking intervention outcomes (Zywiak et al., 2002, and Stanton et al., 2009, respectively).
The smoking-IP instructed participants to list up to 10 people (e.g., family, friends) who had been important to them in last 6 months (“important” was defined as having “a significant impact on your life, regardless of whether or not you like them”). For each network member identified, the participant completed 11 items (if a nonsmoker) or 12 items (if a smoker; the extra item for smokers is described below for smoking-specific social support), including their relationship to the network member, the frequency of contact with him or her, the smoking status of the network member, and the degree of general and smoking-specific support. Data from the IP were scored as follows:
General network characteristics comprised three variables. Size of network was measured as the number of network members listed by the participant. Percentage of peers was calculated by first obtaining a total count of members coded as romantic partners, present or former friends, roommates, or coworkers; this count was then divided by the total number of network members identified by the adolescent. Average contact measured the average frequency of contact with network members (ranging from 7 = 7 days a week to 1 = once in the past 6 months).
General social support comprised four variables. Average general support measured the average supportiveness of network members (“To what extent is this person generally supportive of you, by being sensitive to your personal needs, helping you to think about things, solve problems, and by giving you the moral support you need?” from 1 = not at all to 7 = extremely). Frequency of support was calculated as the product of Frequency of Contact and Supportiveness; products were calculated for each network member and then aggregated to obtain an average score for the network. Average importance measured the level of importance of network members (from 1 = not at all to 6 = extremely). Quality of relations was calculated as the product of Frequency of Contact and Importance; products were calculated for each network member and then aggregated to obtain an average score for the network.
Pervasiveness of smoking comprised four variables. For the percentage of smokers, a total count was first generated for all members, coded as a daily or occasional smoker; this count was then divided by the size of the adolescents’ network. Likewise, variables for the percentage of peers smoking and percentage of family smoking were made by creating a count of peers (or family members) who were daily or occasional smokers and dividing it by the total number of peers (or family members) in the network. For adolescents who did not report any peers (n = 14) or any family members (n = 8) in their networks, data for the percentage of peers (or family) smoking was coded as missing (cases were not imputed because the data were missing not at random). Smoking involvement was calculated as the product of Frequency of Contact and Smoking Status; products were calculated for each network member and then aggregated to obtain an average score for the network.
Smoking-specific social support was differentially measured according to participants’ smoking status. For nonsmokers, support for smoking measured the average expected support for smoking among the network members (“How would this person react if you were to smoke?” from 1 = would strongly oppose it to 6 = would strongly support it). For smokers, the variable measured average current support (“How has this person reacted to your smoking?”). In addition, for smokers, support for quitting measured the average expected support for smoking cessation (“How would this person feel about you quitting smoking?” from 1 = would strongly oppose it to 6 = would strongly support it).
Susceptibility to smoking.
For nonsmokers, susceptibility to smoke was assessed with the four-item Susceptibility to Smoking Scale (Pierce et al., 1995). Prospective work indicates that the items are significant predictors of smoking initiation (Pierce et al., 1996). Items were aggregated to create a single scale (α = .89). Unlike the binary and other categorical factors sometimes created with these measures, our continuous variable allowed for a broad range of responses.
Readiness to quit smoking.
For smokers, three items assessed readiness to quit smoking: The Contemplation Ladder (Abrams & Biener, 1992; Biener & Abrams, 1991), a stage of change algorithm (Colby et al., 1998; DiClemente et al., 1991; Prochaska et al., 1994), and a single, Likert-type item: “How much would you like to quit smoking?” These three items were standardized and then aggregated to create a single scale (α = .84).
Data analysis
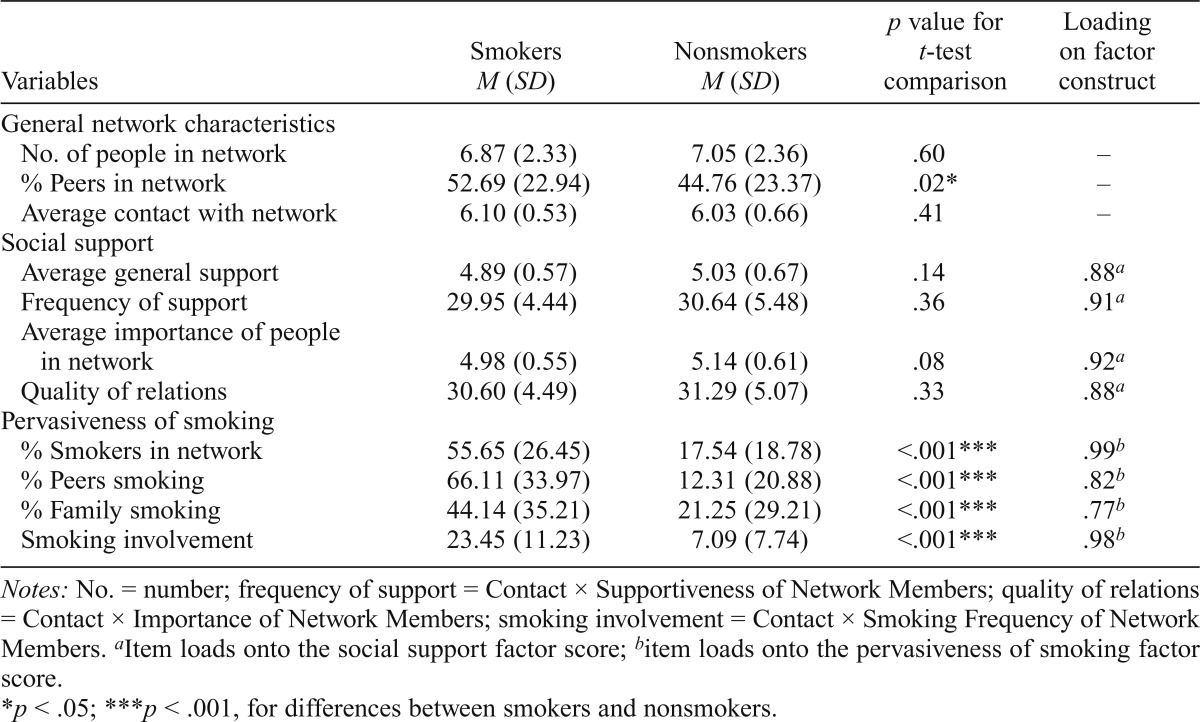
Descriptive statistics were first conducted on the overall sample and by smoking status. We then conducted a series of bivariate analyses to compare smokers and nonsmokers on key social network variables. Next, we used multivariable regressions to simultaneously test the effects of multiple factors. To avoid issues of overfitting and multicollinearity, we condensed highly correlated items by creating factor scores using exploratory factor analysis with varimax rotation. Ultimately, we created regression factor scores for two higher-level constructs: general social support and the pervasiveness of smoking (all factor loadings were .78 or higher). The remaining IP variables were not highly intercorrelated and were kept as single items (Table 2 provides details on the items included within each category).
Table 2.
Social network variables among adolescent smokers (n = 95) and nonsmokers (n = 95), by mean and paired sample t-test comparisons
| Variables | Smokers M (SD) | Nonsmokers M (SD) | p value for t-test comparison | Loading on factor construct |
| General network characteristics | ||||
| No. of people in network | 6.87 (2.33) | 7.05 (2.36) | .60 | – |
| % Peers in network | 52.69 (22.94) | 44.76 (23.37) | .02* | – |
| Average contact with network | 6.10 (0.53) | 6.03 (0.66) | .41 | – |
| Social support | ||||
| Average general support | 4.89 (0.57) | 5.03 (0.67) | .14 | .88a |
| Frequency of support | 29.95 (4.44) | 30.64 (5.48) | .36 | .91a |
| Average importance of people in network | 4.98 (0.55) | 5.14 (0.61) | .08 | .92a |
| Quality of relations | 30.60 (4.49) | 31.29 (5.07) | .33 | .88a |
| Pervasiveness of smoking | ||||
| % Smokers in network | 55.65 (26.45) | 17.54 (18.78) | <.001*** | .99b |
| % Peers smoking | 66.11 (33.97) | 12.31 (20.88) | <.001*** | .82b |
| % Family smoking | 44.14 (35.21) | 21.25 (29.21) | <.001*** | .77b |
| Smoking involvement | 23.45 (11.23) | 7.09 (7.74) | <.001*** | .98b |
Notes: No. = number; frequency of support = Contact × Supportiveness of Network Members; quality of relations = Contact × Importance of Network Members; smoking involvement = Contact × Smoking Frequency of Network Members.
Item loads onto the social support factor score;
item loads onto the pervasiveness of smoking factor score.
p < .05;
p < .001, for differences between smokers and nonsmokers.
Finally, within-group comparisons tested the predictive effects of baseline measures on (a) smoking susceptibility among the nonsmokers and (b) readiness to quit among the smokers. For all regressions, general network characteristics were entered in Step 1; smoking pervasiveness and all social support variables were entered in Step 2. Outliers with residual statistics greater than 3 were removed from the specific regressions (such instances are noted in the results).
Results
Descriptive statistics
Average age was 16.8 years (SD = 1.2); 51% of the adolescents were female, and 85% were White (see Table 1 for further demographic and smoking characteristics). Smokers and nonsmokers did not differ on demographic characteristics. For the overall sample, adolescents reported on an average of seven important people (SD = 2.3), and 49% of their social networks were coded as peers. Overall, adolescents rated their social support network as highly supportive (on the 6-point scale, M = 5.0, SD = 0.63). Social support variables were highly intercorrelated (e.g., for average general support with average importance, r = .76, p < .001); likewise, smoking pervasiveness variables were correlated (e.g., for percentage of peer smokers and percentage of family smokers, r = .31, p < .001). Among nonsmokers, Msusceptibility was 1.3 (SD = 0.5); among smokers, Mreadiness to quit was -0.02 (SD = 0.9). The number of cigarettes smokers used each day was uncorrelated with their readiness to quit (p > .25).
Social network differences
Univariate regressions.
Univariate conditional logistic regression analyses indicated that several social network variables differed significantly between adolescent smokers and nonsmokers (Table 2). In terms of general network characteristics, smokers reported a higher percentage of peers (regardless of their smoking status) compared with nonsmokers. However, smokers and nonsmokers did not differ in terms of network size or average contact with their network members (ps > .4). Likewise, there were no significant differences on the general social support variables, although nonsmokers rated members of their social networks as marginally more important than did smokers (p = .08). Follow-up analyses distinguishing peers from family indicated that smokers and nonsmokers did not differ on their ratings of peer importance (p > .61), but family network members’ importance was significantly higher among nonsmokers (p = .014).
For pervasiveness of smoking, smokers’ social networks were composed of a higher percentage of smokers overall (55.65% vs. 17.54%, p < .001); this difference remained significant when only network members who were daily smokers were considered. When examined by relationship status, smokers also reported higher percentages of peers who smoke and family members who smoke in their networks (ps < .001). Furthermore, smokers, compared with nonsmokers, reported greater smoking involvement (p < .001).
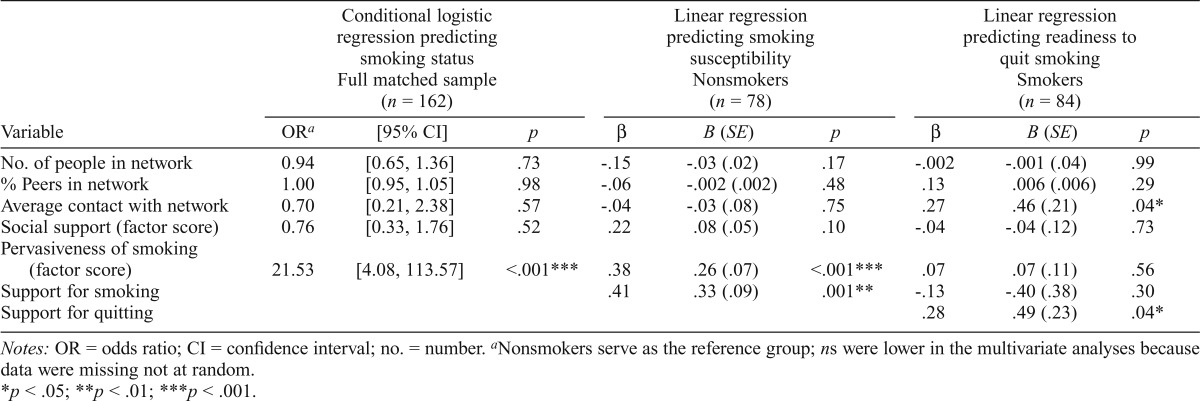
Multivariable analyses.
The multivariable logistic regression first entered general network characteristics (size, percentage of peers, and average contact); Step 2 entered the higher-level constructs (the social support factor score and the pervasiveness of smoking factor score). At this second and final step, the only statistically significant predictor of smoking status was pervasiveness of smoking factor (p < .001; Table 3). Thus, after taking other key social network characteristics into account, adolescents whose social networks were more saturated with smokers were more likely to be smokers themselves.
Table 3.
Regression outcomes predicting adolescent smoking status, smoking susceptibility, and readiness to quit smoking
| Conditional logistic regression predicting smoking status Full matched sample (n = 162) |
Linear regression predicting smoking susceptibility Nonsmokers (n = 78) |
Linear regression predicting readiness to quit smoking Smokers (n = 84) |
|||||||
| Variable | ORa | [95% CI] | p | β | B (SE) | p | β | B (SE) | p |
| No. of people in network | 0.94 | [0.65, 1.36] | .73 | -.15 | -.03 (.02) | .17 | -.002 | -.001 (.04) | .99 |
| % Peers in network | 1.00 | [0.95, 1.05] | .98 | -.06 | -.002 (.002) | .48 | .13 | .006 (.006) | .29 |
| Average contact with network | 0.70 | [0.21, 2.38] | .57 | -.04 | -.03 (.08) | .75 | .27 | .46 (.21) | .04* |
| Social support (factor score) | 0.76 | [0.33, 1.76] | .52 | .22 | .08 (.05) | .10 | -.04 | -.04 (.12) | .73 |
| Pervasiveness of smoking (factor score) | 21.53 | [4.08, 113.57] | <.001*** | .38 | .26 (.07) | <.001*** | .07 | .07 (.11) | .56 |
| Support for smoking | .41 | .33 (.09) | .001** | -.13 | -.40 (.38) | .30 | |||
| Support for quitting | .28 | .49 (.23) | .04* | ||||||
Notes: OR = odds ratio; CI = confidence interval; no. = number.
Nonsmokers serve as the reference group; ns were lower in the multivariate analyses because data were missing not at random.
p < .05;
p < .01;
p < .001.
Forecasting behavior change
Susceptibility in nonsmokers.
Similar to the preceding analysis, a hierarchical linear regression predicting smoking susceptibility among the nonsmokers entered the three general network characteristics at Step 1 and the two factor scores (social support and pervasiveness of smoking) at Step 2. In addition, Step 2 entered the measure of support for smoking (three cases with residual statistics > 3 were excluded). At this second and final step, greater pervasiveness of smoking predicted greater susceptibility (p < .001; Table 3). In addition, greater support for smoking predicted greater susceptibility (p = .001). All other predictors in the model were nonsignificant. Thus, after taking other key social network characteristics into account, nonsmoking adolescents whose social networks had a greater pervasiveness of smoking and reflected greater support for smoking indicated greater susceptibility to smoking initiation.
Readiness to quit in smokers.
In a hierarchical linear regression predicting smokers’ readiness to quit, Step 1 entered the three general network characteristics; Step 2 then entered the social support and pervasiveness of smoking factor scores, support for smoking, and support for quitting. Results indicated that average contact was a significant predictor, such that greater contact with network members was associated with greater readiness to quit (p = .04; Table 3). Support for quitting was also significant, such that a more positive expected reaction to quitting was associated with greater readiness to quit (p = .04). No other variables were significant predictors.
Discussion
This study examined the social networks of a matched sample of adolescent smokers and nonsmokers to identify the factors most strongly related to smoking status. Our analyses indicated that smokers and nonsmokers tended not to differ on general network characteristics or general social support (with the exception that smokers had a higher percentage of peers in their networks). However, the groups did differ on the pervasiveness of smoking in their networks: smokers had higher percentages of both peers and family members who smoke, as well as greater smoking involvement (an index reflecting frequency of contact with smokers in the network). Results from the multivariable analyses were consistent: after accounting for other key social network characteristics, adolescents whose social networks had a greater pervasiveness of smoking were more likely to be smokers themselves.
A second line of within-group, multivariable analyses examined (a) predictors of smoking susceptibility among the nonsmokers and (b) predictors of readiness to quit among the smokers. Although we were not predicting future behavior, we were forecasting change by using validated susceptibility and readiness measures known to be predictive of behavior. Our results indicated that, for the nonsmoking adolescents, greater pervasiveness of smoking and greater social support for smoking were associated with greater susceptibility to smoking initiation. Such findings suggest that social network members can increase risk by conveying (explicitly and/or implicitly) support for the adolescent smoking. For the smoking adolescents, greater contact with network members and greater social support for quitting were associated with greater readiness to quit. These findings likewise support the notion that behavior-specific social support is a key predictor of behavior change (Beattie & Longabaugh, 1999; Groh et al., 2008). That is, while general social support did not appear to have a protective main effect in this population, behavior-specific support (i.e., support for smoking and support for quitting) may play a role in initiation and cessation.
This research offers insight into potential targets for prevention and early intervention by demonstrating how social networks can both promote and attenuate smoking risk. In particular, the results indicate that although smoking pervasiveness increases risk, smoking-specific support is also involved as a protective factor. Such results argue against the fatalistic notion that family and peer smoking unfailingly increase an adolescent’s smoking risk. Moreover, targeting smoking- and cessation-specific support (e.g., promoting the communication of anti-smoking or pro-cessation messages, helping adolescents to elicit support from their networks) may enhance the effectiveness of prevention/intervention programs.
The value and novelty of our study is not wholly in the findings but also the methods: Our matched design allowed us to minimize alternative, demographic-based explanations for study findings. Also, our use of a smoking-IP was advantageous for two reasons. First, this measure was inclusive to assessing peers outside of the classroom, thereby acknowledging the breadth of the peer context of adolescent smoking. Second, the smoking-IP allowed parents and other family members to be included within the social network. This feature is often lacking in studies, and its value was bolstered by our finding that only 49% of participants’ social networks were coded as peers.
Limitations and future directions
Although the purpose of the smoking-IP was to measure adolescents’ overall social networks, it is important to note that network members were nominated for inclusion by the adolescent participants. Thus, it is likely that some influential network members were unreported, and thereby left out of the analyses. The IP does not assess the extent to which participants are socially integrated (central) versus isolated (peripheral) in their social networks’ structure. Likewise, the IP limits participants to nominating a maximum of 10 network members, and adolescent networks are undoubtedly larger than that (Falci & McNeely, 2009). The measure was also limited to assessing cigarette use and did not assess use of other tobacco products, such as e-cigarettes. This study is also limited by its primarily White sample and by its cross-sectional nature, which prevents us from assessing the sequential, causal order of events. For example, although we can logically assume that family smoking preceded adolescent smoking, it is more difficult to determine the extent to which socialization versus selection played a role in the relation between peer smoking and adolescent smoking. Future studies are needed to examine these relations prospectively.
Future research may benefit from expanding on the constructs examined in the present study. For example, a measure of contact with network members may be more informative if, in the expanding social context of online media, it distinguished between virtual and offline contact. The measures of support for smoking and support for quitting may be tapping into the construct of subjective norms (Fishbein & Ajzen, 1975). To rule against this alternative explanation, further research will need to ask more specific questions and clarify the conveying of social support (e.g., providing emotional support for smoking/quitting to a particular individual) from the conveying of social norms (e.g., voicing approval for smoking/quitting generally).
Conclusions
This study adds nuance to the wealth of research emphasizing the risk for adolescents of having a social network saturated with smokers. Using a smoking-IP questionnaire and a matched-samples design, we found that the pervasiveness of smoking in adolescents’ social networks was the strongest distinguisher of smokers versus nonsmokers. Furthermore, two types of behavior-specific social support appeared to be protective: smoking-specific support was associated with susceptibility to initiate smoking among non-smokers, and cessation-specific support was associated with readiness to quit among smokers. These findings may help advance the research and efficacy of smoking prevention and early intervention programs by demonstrating how social networks provide the framework for both risk and protective influences.
Footnotes
This research was supported by National Institute on Drug Abuse Grants 1R01 DA16737 and T32 DA016184 and National Cancer Institute Grants K07CA091831 and P30CA051008.
References
- Abrams D. B., Biener L. Motivational characteristics of smokers at the workplace: A public health challenge. Preventive Medicine. 1992;21:679–687. doi: 10.1016/0091-7435(92)90075-s. [DOI] [PubMed] [Google Scholar]
- Andrews J. A., Hops H., Ary D., Tildesley E., Harris J. Parental influence on early adolescent substance use: Specific and nonspecific effects. Journal of Early Adolescence. 1993;13:285–310. [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- Beattie M. C., Longabaugh R. General and alcohol-specific social support following treatment. Addictive Behaviors. 1999;24:593–606. doi: 10.1016/s0306-4603(98)00120-8. [DOI] [PubMed] [Google Scholar]
- Berkman L. F., Glass T., Brissette I., Seeman T. E. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Biener L., Abrams D. B. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Tobacco use: Targeting the nation s leading killer at a glance 2011. 2011 Retrieved from http://www.cdc.gov/chronicdisease/resources/publications/aag/osh.htm.
- Cobb S. Presidential Address–1976. Social support as a moderator of life stress. Psychosomatic Medicine. 1976;38:300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Cohen S., Wills T. A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Colby S. M., Monti P. M., Barnett N. P., Rohsenow D. J., Weissman K., Spirito A., Lewander W. J. Brief motivational interviewing in a hospital setting for adolescent smoking: A preliminary study. Journal of Consulting and Clinical Psychology. 1998;66:574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- Colby S. M., Monti P. M., O’Leary Tevyaw T., Barnett N. P., Spirito A., Rohsenow D. J., Lewander W. Brief motivational intervention for adolescent smokers in medical settings. Addictive Behaviors. 2005;30:865–874. doi: 10.1016/j.addbeh.2004.10.001. [DOI] [PubMed] [Google Scholar]
- DiClemente C. C., Prochaska J. O., Fairhurst S. K., Velicer W. F., Velasquez M. M., Rossi J. S. The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology. 1991;59:295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- Elek E., Miller-Day M., Hecht M. L. Influences of personal, injunctive, and descriptive norms on early adolescent substance use. Journal of Drug Issues. 2006;36:147–172. [Google Scholar]
- Ennett S. T., Bauman K. E., Hussong A., Faris R., Foshee V. A., Cai L., DuRant R. H. The peer context of adolescent substance use: Findings from social network analysis. Journal of Research on Adolescence. 2006;16:159–186. [Google Scholar]
- Ennett S. T., Faris R., Hipp J., Foshee V. A., Bauman K. E., Hussong A., Cai L. Peer smoking, other peer attributes, and adolescent cigarette smoking: A social network analysis. Prevention Science. 2008;9:88–98. doi: 10.1007/s11121-008-0087-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan P., Eisenberg M., Stoddard A. M., Frazier L., Sorensen G. Social influences, social norms, social support, and smoking behavior among adolescent workers. American Journal of Health Promotion. 2001;15:414–421. doi: 10.4278/0890-1171-15.6.414. [DOI] [PubMed] [Google Scholar]
- Falci C., McNeely C. Too many friends: Social integration, network cohesion and adolescent depressive symptoms. Social Forces. 2009;87:2031–2061. [Google Scholar]
- Falkin G. P., Strauss S. M. Social supporters and drug use enablers: A dilemma for women in recovery. Addictive Behaviors. 2003;28:141–155. doi: 10.1016/s0306-4603(01)00219-2. [DOI] [PubMed] [Google Scholar]
- Farkas A. J., Gilpin E. A., White M. M., Pierce J. P. Association between household and workplace smoking restrictions and adolescent smoking. Journal of the American Medical Association. 2000;284:717–722. doi: 10.1001/jama.284.6.717. [DOI] [PubMed] [Google Scholar]
- Fawzy F. I., Coombs R. H., Gerber B. Generational continuity in the use of substances: The impact of parental substance use on adolescent substance use. Addictive Behaviors. 1983;8:109–114. doi: 10.1016/0306-4603(83)90003-5. [DOI] [PubMed] [Google Scholar]
- Fagerström K. The epidemiology of smoking: Health consequences and benefits of cessation. Drugs, 62, Supplement. 2002;2:1–9. doi: 10.2165/00003495-200262002-00001. [DOI] [PubMed] [Google Scholar]
- Fishbein M., Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Gilliland F. D., Islam T., Berhane K., Gauderman W. J., McConnell R., Avol E., Peters J. M. Regular smoking and asthma incidence in adolescents. American Journal of Respiratory and Critical Care Medicine. 2006;174:1094–1100. doi: 10.1164/rccm.200605-722OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman S. E., Rende R., Boergers J., Abrams D. B., Buka S. L., Clark M. A., Niaura R. S. Parental smoking and adolescent smoking initiation: An intergenerational perspective on tobacco control. Pediatrics. 2009;123:e274–e281. doi: 10.1542/peds.2008-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold D. R., Wang X., Wypij D., Speizer F. E., Ware J. H., Dockery D. W. Effects of cigarette smoking on lung function in adolescent boys and girls. The New England Journal of Medicine. 1996;335:931–937. doi: 10.1056/NEJM199609263351304. [DOI] [PubMed] [Google Scholar]
- Grogan S., Conner M., Fry G., Gough B., Higgins A. Gender differences in smoking: A longitudinal study of beliefs predicting smoking in 11–15 year olds. Psychology & Health. 2009;24:301–316. doi: 10.1080/08870440701746586. [DOI] [PubMed] [Google Scholar]
- Groh D. R., Jason L. A., Keys C. B. Social network variables in Alcoholics Anonymous: A literature review. Clinical Psychology Review. 2008;28:430–450. doi: 10.1016/j.cpr.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall J. A., Valente T. W. Adolescent smoking networks: The effects of influence and selection on future smoking. Addictive Behaviors. 2007;32:3054–3059. doi: 10.1016/j.addbeh.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K. J., Golbeck A. L., Cronk N. J., Catley D., Conway K., Williams K. B. Timeline follow-back versus global self-reports of tobacco smoking: A comparison of findings with nondaily smokers. Psychology of Addictive Behaviors. 2009;23:368–372. doi: 10.1037/a0015270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney C. A., Israel B. A. Social networks and social support. In: Glanz K., Rimer B. K., Viswanath K., editors. Health behavior and health education: Theory, research, and practice (4th ed., pp. 189–210) San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- Hiscock R., Bauld L., Amos A., Fidler J. A., Munafò M. Socioeconomic status and smoking: A review. Annals of the New York Academy of Sciences. 2012;1248:107–123. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- Huxley R. R., Yatsuya H., Lutsey P. L., Woodward M., Alonso A., Folsom A. R. Impact of age at smoking initiation, dosage, and time since quitting on cardiovascular disease in African Americans and Whites: The atherosclerosis risk in communities study. American Journal of Epidemiology. 2012;175:816–826. doi: 10.1093/aje/kwr391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns M. M., Pingel E. S., Youatt E. J., Soler J. H., McClelland S. I., Bauermeister J. A. LGBT community, social network characteristics, and smoking behaviors in young sexual minority women. American Journal of Community Psychology. 2013;52:141–154. doi: 10.1007/s10464-013-9584-4. [DOI] [PubMed] [Google Scholar]
- Johnston L. D., O’Malley P. M., Bachman J. G., Schulenberg J. E. Monitoring the Future national results on drug use: 2012 Overview, Key Findings on Adolescent Drug use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2013. [Google Scholar]
- Lakon C. M., Hipp J. R., Timberlake D. S. The social context of adolescent smoking: A systems perspective. American Journal of Public Health. 2010;100:1218–1228. doi: 10.2105/AJPH.2009.167973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantz P. M., Jacobson P. D., Warner K. E., Wasserman J., Pollack H. A., Berson J., Ahlstrom A. Investing in youth tobacco control: A review of smoking prevention and control strategies. Tobacco Control. 2000;9:47–63. doi: 10.1136/tc.9.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawhon D., Humfleet G. L., Hall S. M., Reus V. I., Muñoz R. F. Longitudinal analysis of abstinence-specific social support and smoking cessation. Health Psychology. 2009;28:465–472. doi: 10.1037/a0015206. [DOI] [PubMed] [Google Scholar]
- Lewis-Esquerre J. M., Colby S. M., Tevyaw T. O. L., Eaton C. A., Kahler C. W., Monti P. M. Validation of the timeline follow-back in the assessment of adolescent smoking. Drug and Alcohol Dependence. 2005;79:33–43. doi: 10.1016/j.drugalcdep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Lifrak P. D., McKay J. R., Rostain A., Alterman A. I., O’Brien C. P. Relationship of perceived competencies, perceived social support, and gender to substance use in young adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:933–940. doi: 10.1097/00004583-199707000-00015. [DOI] [PubMed] [Google Scholar]
- Longabaugh R., Beattie M., Noel N., Stout R., Malloy P. The effect of social investment on treatment outcome. Journal of Studies on Alcohol. 1993;54:465–478. doi: 10.15288/jsa.1993.54.465. [DOI] [PubMed] [Google Scholar]
- Longabaugh R., Zywiak W. Brown University, Providence RI (available on request from the first author); 1998. Important People instrument. Center for Alcohol & Addiction Studies. [Google Scholar]
- Moolchan E. T., Fagan P., Fernander A. F., Velicer W. F., Hayward M. D., King G., Clayton R. R. Addressing tobacco-related health disparities. Addiction, 102, Supplement 2. 2007:30–42. doi: 10.1111/j.1360-0443.2007.01953.x. [DOI] [PubMed] [Google Scholar]
- Nargiso J. E., Kuo C. C., Zlotnick C., Johnson J. E. Social support network characteristics of incarcerated women with co-occurring major depressive and substance use disorders. Journal of Psychoactive Drugs. 2014;46:93–105. doi: 10.1080/02791072.2014.890766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds R. S., Thombs D. L. The relationship of adolescent perceptions of peer norms and parent involvement to cigarette and alcohol use. Journal of School Health. 2001;71:223–228. doi: 10.1111/j.1746-1561.2001.tb01322.x. [DOI] [PubMed] [Google Scholar]
- Otten R., Engels R. C. M. E., van den Eijnden R. J. J. M. General parenting, anti-smoking socialization and smoking onset. Health Education Research. 2008;23:859–869. doi: 10.1093/her/cym073. [DOI] [PubMed] [Google Scholar]
- Pierce J. P., Choi W. S., Gilpin E. A., Farkas A. J., Merritt R. K. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychology. 1996;15:355–361. doi: 10.1037//0278-6133.15.5.355. [DOI] [PubMed] [Google Scholar]
- Pierce J. P., Farkas A. J., Evans N., Gilpin E. An improved surveillance measure for adolescent smoking? Tobacco Control, 4, Supplement 1. 1995:S47–S56. [Google Scholar]
- Prochaska J. O., Velicer W. F., Rossi J. S., Goldstein M. G., Marcus B. H., Rakowski W., Rossi S. R. Stages of change and decisional balance for 12 problem behaviors. Health Psychology. 1994;13:39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- So-kum Tang C., Wong W. C. W., Leung P. M. S., Chen W. Q., Lee A., Ling D. C. Health compromising behaviors among Chinese adolescents: Role of physical abuse, school experience, and social support. Journal of Health Psychology. 2011;16:457–466. doi: 10.1177/1359105310384297. [DOI] [PubMed] [Google Scholar]
- Stanton C. A., Highland K. B., Tercyak K. P., Luta G., Niaura R. S. Authoritative parenting and cigarette smoking among multiethnic preadolescents: The mediating role of anti-tobacco parenting strategies. Journal ofPediatric Psychology. 2014;39:109–119. doi: 10.1093/jpepsy/jst087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton C. A., Lloyd-Richardson E. E., Papandonatos G. D., de Dios M. A., Niaura R. Mediators of the relationship between nicotine replacement therapy and smoking abstinence among people living with HIV/AIDS. AIDS education and prevention: Official publication of the International Society for AIDS Education, 21, Supplement 3. 2009:65. doi: 10.1521/aeap.2009.21.3_supp.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinidad D. R., Gilpin E. A., Lee L., Pierce J. P. Do the majority of Asian-American and African-American smokers start as adults? American Journal of Preventive Medicine. 2004;26:156–158. doi: 10.1016/j.amepre.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Tyas S. L., Pederson L. L. Psychosocial factors related to adolescent smoking: A critical review of the literature. Tobacco Control. 1998;7:409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino B. N. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the Surgeon General. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- Valente T. W., Gallaher P., Mouttapa M. Using social networks to understand and prevent substance use: A transdisciplinary perspective. Substance Use & Misuse. 2004;39:1685–1712. doi: 10.1081/ja-200033210. [DOI] [PubMed] [Google Scholar]
- Wills T. A., Ainette M. G. Social networks and social support. In: Baum A., Revenson T., Singer J., editors. Handbook of health psychology (2nd ed., pp. 465–492) New York, NY: Psychology Press; 2012. [Google Scholar]
- Wills T. A., Cleary S. D. How are social support effects mediated? A test with parental support and adolescent substance use. Journal of Personality and Social Psychology. 1996;71:937–952. doi: 10.1037//0022-3514.71.5.937. [DOI] [PubMed] [Google Scholar]
- Wilson W., Ary D. V., Biglan A., Glasgow R. E., Toobert D. J., Campbell D. R. Psychosocial predictors of self-care behaviors (compliance) and glycemic control in non-insulin-dependent diabetes mellitus. Diabetes Care. 1986;9:614–622. doi: 10.2337/diacare.9.6.614. [DOI] [PubMed] [Google Scholar]
- Zywiak W. H., Longabaugh R., Wirtz P. W. Decomposing the relationships between pretreatment social network characteristics and alcohol treatment outcome. Journal of Studies on Alcohol. 2002;63:114–121. [PubMed] [Google Scholar]