Abstract
Objective:
Advancing our initial, cross-sectional study, which showed that adult Latinas’ mother–daughter attachment relates to their substance use, the current, longitudinal study tests whether mother and daughter attachment scores at baseline predict their substance use over time.
Method:
We analyzed data from a convenience sample of 133 Latina adult mothers (mean age = 52 years, SD = 10) and 133 Latina adult daughters (mean age = 27, SD = 9) at baseline and at 5-year and 6-year follow-ups after baseline (attrition rate = 16%). Multilevel longitudinal modeling was used to examine the effect of mother–daughter attachment at baseline on their substance use over time.
Results:
Each unit of increase in the attachment score at baseline is associated with a 0.28 drink decrease in monthly alcohol use (p < .05) and a lower likelihood of being a heavy alcohol or other drug user [exp(β) = 0.97, p < .01] compared with average attachment score at baseline (M = 91.52, SD = 18.00). Time and older age at baseline are associated with decreased substance use. Being born outside the United States is associated with decreased risk of heavy alcohol or other drug use. Being a mother is associated with increased substance use.
Conclusions:
The findings of this longitudinal study on adult Latinas indicate that mother–daughter attachment has long-lasting effects on substance use trajectories among adult Latinas. Future research should focus on (a) investigating social and cultural factors mediating this relationship and (b) greater substance use among Latina mothers compared with daughters.
Over the past two decades, significant knowledge has been gained regarding the familial factors that influence substance use behaviors (heavy alcohol use, use of cannabis, and nonmedical use of prescription drugs) of U.S.- and foreign-born Latinos (Bacio et al., 2013; Hilarski, 2005; Sokol-Katz et al., 1997; Wagner et al., 2010). These research efforts suggest that familial factors such as cohesion, attachment, and structure affect substance use behaviors of Latinos. Two of the first major studies to document the importance of familial factors on the substance use behaviors of Latinos were Vega et al. (1993) and Brook et al. (1992). Vega et al. determined that familial protective factors significantly influenced delinquent and deviant behaviors in a cohort of young Cuban male adolescents. Similarly, studying a sample of 637 Puerto Rican male and female adolescents, Brook et al. reported that more parent–child attachment is associated with adolescents’ internalization of parents’ conventional attitudes and behaviors—which in turn reduces adolescents’ drug use behaviors.
These findings have been replicated over the past decades by other researchers exploring the substance use behaviors of immigrant and U.S.-born Latino adolescents (Bacio et al., 2013; Cavendish et al., 2012; Warner et al., 2008). For example, in a study conducted in 2005, Sale et al. found that family factors were strongly linked to alcohol use among Hispanic females ages 9–18 years (Sale et al., 2005). Results from these studies show that improving the connection between parents and adolescents leads to a delay or reduction in child alcohol use. Moreover, in a systematic review of the literature, parental bonding (i.e., receipt of parental praise) was found to be associated with lower nonmedical use of prescription medication among adolescents including Latinos (Young et al., 2012). In a more recent study, Wagner et al. (2010) found that parental monitoring appeared to be particularly important in predicting substance use in a sample of Latino adolescents.
Although the parent–child relationship has been studied extensively among Latino adolescents, research on how familial factors influence the substance use behaviors of adult Latina women is rare. Most studies examining mother–daughter attachment (Golder et al., 2005; Vungkhanching et al., 2004) only included a small percentage of Latinas in their samples—Latinas comprise 5% of the sample in the Golder et al. (2005) study. However, alcohol and other drug use problems have become more prevalent among Latinas in the United States. For example, although foreign-born Latinas are less likely than women from other racial/ethnic groups in the United States to misuse alcohol and other drugs, drug use among U.S.-born Latina women is comparatively higher, approaching levels found in non-Whites and non-Hispanic Blacks (Castillo-Mancilla et al., 2012; Gilbert & Collins, 1997; Loue, 1998). Examining the association between family relationships and substance use among Latinas is particularly important (Alegría et al., 1998; Galanti, 2003) because family is a central institution in Latino culture (Canino et al., 1980), and Latinas often rely more on family than friends (Galanti, 2003).
Recently, we conducted an initial, cross-sectional community-based study that documented the association between mother–daughter attachment and substance use behaviors among 158 U.S.- and foreign-born adult Latina mother and daughter dyads (De La Rosa et al., 2010). In that study, we found that higher levels of mother–daughter attachment may serve as a protective factor that decreases substance use among daughters. Moreover, dyads in which mothers and daughters are both substance users showed lower attachment scores than dyads in which only the mother or daughter is a substance user or both mother and daughter are not substance users (De La Rosa et al., 2010).
Although these studies have advanced our understanding of the link between attachment and the substance use behaviors of adolescent and adult Latinas, no longitudinal studies exist that have explored the influence of mother–daughter attachment on changes in the heavy alcohol and illegal drug use (i.e., illicit drug use and nonmedical use of prescription drugs) behaviors of U.S.- and foreign-born adult Latina women residing in the United States. Thus, our article addresses this significant gap in the scientific literature by reporting findings from a 6-year longitudinal study that documented whether attachment scores at baseline predict monthly alcohol use over time among U.S.- and foreign-born adult Latina women residing in the United States.
This longitudinal study was guided in part by the Bogenschneider (1996) ecological risk/protective model, which underlines the central role of familial factors in influencing parent–child relationships. For example, ecological theory indicates that close parental monitoring (e.g., knowing a child’s whereabouts) can moderate the influences of parental work schedule (i.e., “latchkey kids”) on antisocial behaviors among children and adolescents (Bronfenbrenner, 1986). In essence, Bogenschneider’s (1996) ecological risk/protective model suggests that family relations represent the primary context for human development over the life span (Szapocznik & Coatsworth, 1999). Parents and other family members have the longest history with an individual and play major roles in shaping patterns of that individual’s development (Perrino et al., 2000). These influences extend well beyond childhood and adolescence, such that family influences continue to be important in adulthood (Castillo-Mancilla et al., 2012; Fergusson et al., 2007; Overbeek et al., 2007). The importance of family in the Latino culture heightens the influence family members have on their behaviors over the entire life span (Umaña-Taylor et al., 2009).
Our present study focuses on how attachment affects alcohol use over time rather than the bidirectional relationship because we aim to address the knowledge gap identified in our previous study (De La Rosa et al., 2010), which used cross-sectional data to show the correlation between attachment and substance use among Latinas. We hypothesize that stronger attachment between mother and daughter is associated with less alcohol use for both mothers and daughters. The social development model explains the relationship between attachment and substance use. This model indicates that bonding to family is associated with the increased likelihood of adopting conventional values and, therefore, reduces the risk of substance use (Brook et al., 1990; Farrington & Hawkins, 1991; Hawkins & Weis, 1985). In addition, empirical studies (Golder et al., 2005; Kassel et al., 2007) have reported that psychological stress and self-esteem mediate the relationship between poor attachment and substance use. More explicitly, poor attachment is associated with psychological distress and low self-esteem that, in turn, can limit one’s capacity for internal self-regulation and result in external behavioral problems, such as substance use.
Method
Procedures
We purposely attempted to recruit both substance-using and nonusing participants in our sample to ensure adequate range of variability in alcohol/other drug use practices. Our previous publication (De La Rosa et al., 2010) details our recruitment procedures at Wave 1 (316 individuals; 158 mother–daughter dyads); an overview of these procedures is presented here. Substance-using and nonusing Latinas were simultaneously recruited through announcements at community health fairs, health clinics, radio announcements on local Spanish-language stations, and advertisements on local television channels. Further outreach was achieved via announcements posted at local drug court programs and community-based substance use support groups such as Narcotics Anonymous (NA) and Alcoholics Anonymous (AA) meetings as well as through advertising in a local alternative newspaper and on an FM radio station. We applied five eligibility criteria in sample recruitment: (a) consenting to be interviewed for at least 1–2 hours; (b) being 18 years of age or older; (c) self-identifying as Latina; (d) living in Miami–Dade County, Florida; and (e) being willing to provide two telephone numbers to researchers for correspondence during participation in the study.
We conducted the baseline interview between 2005 and 2007 (Wave 1). We identified 57% (n = 150) of the sample as heavy alcohol users or illicit drug users at Wave 1 and subsequently conducted two follow-ups. Five years after Wave 1, the first follow-up (Wave 2) was conducted; the second follow-up (Wave 3) was conducted 1 year after Wave 2. At Wave 2, we located 278 individuals from 139 dyads (i.e., 88% of our original sample), who then completed the assessment. At Wave 3, we located 266 individuals from 133 dyads (i.e., 84% of our original sample), who then completed the assessment. The main causes of attrition, in order of prevalence, included death, hospitalization, or refusals.
We tested for patterns of missing data in our sample. We compared the individuals available at all three waves (n = 266) and the individuals who were not available for all three waves (n = 50) by age, generation (i.e., mother or daughter), education level, history of alcohol use treatment, birth country (United States vs. outside the United States), and attachment score at baseline. We found no significant difference for any of these variables between the individuals who were available at all three waves and the individuals who were not available for all three waves. Therefore, our final sample—comprising individuals who were available at all three waves—is representative of our original sample.
All consenting study participants completed a face-to-face interview that was conducted at locations convenient for participants. Interviews were conducted in the participants’ chosen language, either Spanish or English, by eight bilingual trained and supervised female assessors. The study was approved by, and conducted in compliance with, the institutional review board at a large southeastern university.
Measures
Demographic variables.
Sociodemographic covariates assessed at Wave 1 for all participants included age, education, nativity, and history of alcohol use treatment. Education level at baseline included the following response options: 1 (less than high school), 2 (high school diploma or equivalent), 3 (post–high school training), 4 (bachelor’s degree), and 5 (graduate/professional studies). Nativity was assessed with the question, “Where were you born?” and then recoded into U.S. born versus foreign born. History of alcohol use treatment was assessed with the question, “How many times (only include periods of 30 days or more) have you been treated for alcohol abuse? Include detoxification, halfway houses, in/outpatient counseling, and AA or NA (if three or more meetings within 1-month period). (Include treatment in person).” It was then recoded into a dichotomous variable.
Attachment assessment.
Attachment was measured at Wave 1 using an adapted 25-item version of the Inventory of Parent and Peer Attachment (IPPA) developed by Armsden and Greenberg (1987). In a review by Reese et al. (2002), the IPPA was deemed one of five superior measures of adult attachment found in the literature. The IPPA was developed to assess individuals’ perceptions of positive and negative affective and cognitive dimensions of relationships with parents and peers along three hypothesized dimensions of secure attachment (i.e., trust, communication, and alienation). Using a 5-point Likert scale ranging from “almost never or never true” to “almost always or always true,” dyad members were interviewed separately and asked to indicate their level of agreement with each item. Sample items include, “I trust my daughter/mother” (trust scale) and “I can count on my daughter/mother when I need to get something off my chest” (communication scale). A confirmatory factor analysis of the scale at baseline revealed that a factor solution provided an adequate fit to the data, χ2(268) = 587.52, p < .0001; comparative fit index = .91; root mean square error of approximation = .06. Therefore, we used a total attachment scale score in our analyses (Cronbach’s α coefficients for the total scale score were .93 for the total sample, .93 for the daughter sample, and .92 for the mother sample at baseline). Additional information on the scale and its use in this sample can be found in previous publications (De La Rosa et al., 2010).
Monthly alcohol use assessment.
Alcohol consumption items from the Health and Daily Living Form (HDLF; Billings et al., 1983) were used to assess participants’ monthly alcohol use during the 12 months before assessment. We chose the past 12 months as a timeframe because the National Institute on Alcohol Abuse and Alcoholism (2014) suggests that this timeframe accounts for issues of recall and issues pertaining to individuals who drink infrequently. Following previous studies using the HDLF (Brennan et al., 2010; Moos et al., 2004), monthly alcohol use was calculated by multiplying participants’ monthly frequency of consumption for each beverage type (wine, beer, and distilled spirits) on an 8-point Likert scale ranging from 1 (never uses) to 8 (uses every day) by the quantity (number of drinks) consumed. We summed all three frequency-by-quantity products to obtain monthly alcohol use.
Heavy alcohol or other drug use assessment.
Alcohol consumption items from the HDLF were used to assess participants’ heavy use of alcohol, and drug use items from the Drug Use Frequency measure (O’Farrell et al., 2003) were used to assess participants’ heavy use of illicit drugs. As in the monthly alcohol use measure above, we chose the past 12 months as a timeframe for this assessment. Heavy alcohol use was defined as meeting at least one of the following four criteria: (a) four to five glasses of wine or more in one occasion at least once a month, (b) three to four cans/bottles of beer or more in one occasion at least once a month, (c) three to four drinks or more in one occasion with 4 oz. of alcohol in each drink at least once a month, and/or (d) five to seven drinks or more in one occasion with 2 oz. of alcohol in each drink at least once a month.
Heavy drug use was defined as meeting at least one of the following five criteria: (a) marijuana use at least 3 days per week, (b) cocaine use at least 2 days per week, (c) heroin use at least once per week, (d) Ecstasy (3,4-methylenedioxy-methamphetamine [MDMA]) use at least three times per month, and/or (e) nonmedical use of prescription drugs (use of a medication without prescription, or medication taken in greater amounts than prescribed or used for a longer period than prescribed; adapted from Turner et al., 2001). Past research indicates that Drug Use Frequency scores correlate closely with collateral reports of drug use frequency and with self-reports in other drug and alcohol use measures, indicating evidence of convergent validity (O’Farrell et al., 2003). We combined heavy alcohol use and heavy drug use into a single variable to indicate heavy alcohol or other drug use. If a person met the criteria of heavy use of alcohol and/ or illicit drugs, the person was assigned the value “1” for this variable. If a person met neither criterion, the person was assigned the value “0” for this variable.
Data analytic plan.
Descriptive statistics were used to outline the characteristics of the sample. Bivariate statistics were used to explore the relationships between participants’ demographics, attachment score at baseline, and monthly alcohol use at each wave. We used the chi-square test, t test, and analysis of variance to examine the statistical significance of the relationships. Multilevel longitudinal modeling was used to examine the effect of attachment score at baseline on monthly alcohol use and heavy use of alcohol/ illicit drugs over time. Multilevel longitudinal modeling has the advantage of accounting for varying spacing of waves (Singer & Willett, 2003). In our data collection, the time between Waves 1 and 2 was 5 years, and the time between Waves 2 and 3 was 1 year.
More explicitly, in our multilevel longitudinal modeling, we used PROC MIXED in SAS Version 9.3 (SAS Institute Inc., Cary, NC) to model monthly alcohol use. The PROC MIXED procedure offers great flexibility, allowing us to combine individual longitudinal modeling with modeling the effects of higher level structures (Singer, 1998). Our data involve tracking longitudinal monthly alcohol use data of individuals nested within mother–daughter dyads. Thus, we ran four models in the multilevel longitudinal modeling. First, we fit the unconditional means two-level model with time point as Level 1 and individual as Level 2. Second, we fit the unconditional means three-level model with time point as Level 1, individual as Level 2, and dyad as Level 3. Third, we added time to the model. Fourth, we added age, generation (i.e., mother or daughter), education level, history of alcohol use treatment, birth country (United States vs. outside the United States), and attachment score at baseline. The attachment score at baseline used in our analysis is the grand mean-centered attachment score, which was computed by centering each individual’s attachment score on the mean of attachment score. We used model fit statistics for model comparison.
We used PROC GLIMMIX in SAS Version 9.3 to model heavy alcohol or other drug use. Compared with PROC MIXED, the PROC GLIMMIX procedure is able to model a dependent variable with a nonnormal distribution. Heavy alcohol or other drug use is a dichotomous variable with a binomial distribution. As with monthly alcohol use, we ran four models to model the binary variable heavy alcohol or other drug use. To detect multicollinearity, we used the Variance Inflation Factor (VIF). A VIF value greater than 10 is regarded as severe multicollinearity (O’Brien, 2007). We computed VIFs in PROC REG in SAS 9.3. VIFs for all our independent variables are less than four. Therefore, there is no multicollinearity between the independent variables.
Results
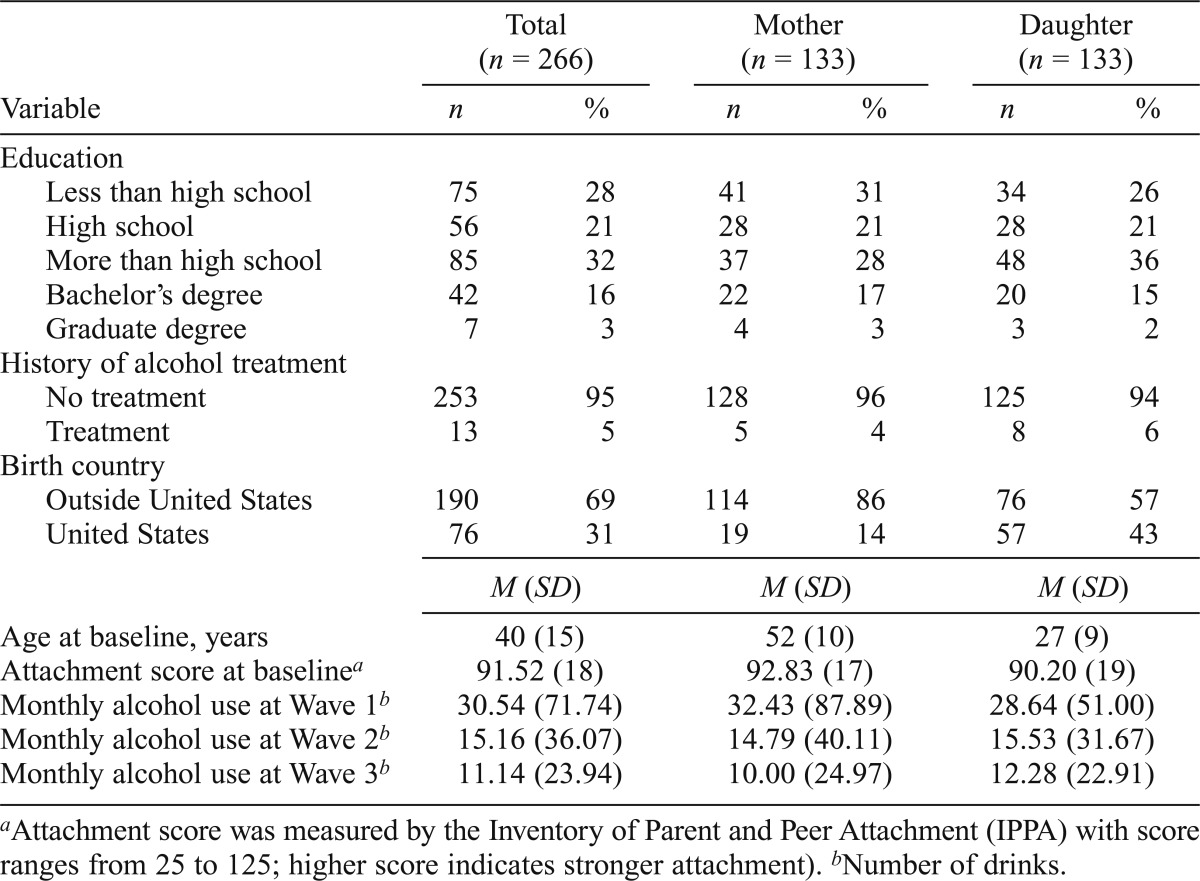
We report descriptive findings for our sample in Table 1. In the sample, 69% of participants were born outside the United States, 28% had less than a high school education, 21% had high school or equivalent education, 32% had trade training post high school, 16% had bachelor’s degrees, 3% had graduate degrees, and 5% received alcohol use treatment before the baseline interview. The average age at the baseline interview was 40 years old (SD = 15). The average attachment score at baseline was 91.52 (SD = 18). As shown in Table 1, our descriptive analysis suggests that monthly alcohol use decreased over the 6-year window. We present descriptive analyses for the mother subsample and daughter subsample separately.
Table 1.
Descriptive analysis of the whole sample and mother and daughter subsamples
| Total (n = 266) |
Mother (n = 133) |
Daughter (n = 133) |
||||
| Variable | n | % | n | % | n | % |
| Education | ||||||
| Less than high school | 75 | 28 | 41 | 31 | 34 | 26 |
| High school | 56 | 21 | 28 | 21 | 28 | 21 |
| More than high school | 85 | 32 | 37 | 28 | 48 | 36 |
| Bachelor’s degree | 42 | 16 | 22 | 17 | 20 | 15 |
| Graduate degree | 7 | 3 | 4 | 3 | 3 | 2 |
| History of alcohol treatment | ||||||
| No treatment | 253 | 95 | 128 | 96 | 125 | 94 |
| Treatment | 13 | 5 | 5 | 4 | 8 | 6 |
| Birth country | ||||||
| Outside United States | 190 | 69 | 114 | 86 | 76 | 57 |
| United States | 76 | 31 | 19 | 14 | 57 | 43 |
| M (SD) | M (SD) | M (SD) | ||||
| Age at baseline, years | 40 (15) | 52 (10) | 27 (9) | |||
| Attachment score at baselinea | 91.52 (18) | 92.83 (17) | 90.20 (19) | |||
| Monthly alcohol use at Wave 1b | 30.54 (71.74) | 32.43 (87.89) | 28.64 (51.00) | |||
| Monthly alcohol use at Wave 2b | 15.16 (36.07) | 14.79 (40.11) | 15.53 (31.67) | |||
| Monthly alcohol use at Wave 3b | 11.14 (23.94) | 10.00 (24.97) | 12.28 (22.91) | |||
Attachment score was measured by the Inventory of Parent and Peer Attachment (IPPA) with score ranges from 25 to 125; higher score indicates stronger attachment).
Number of drinks.
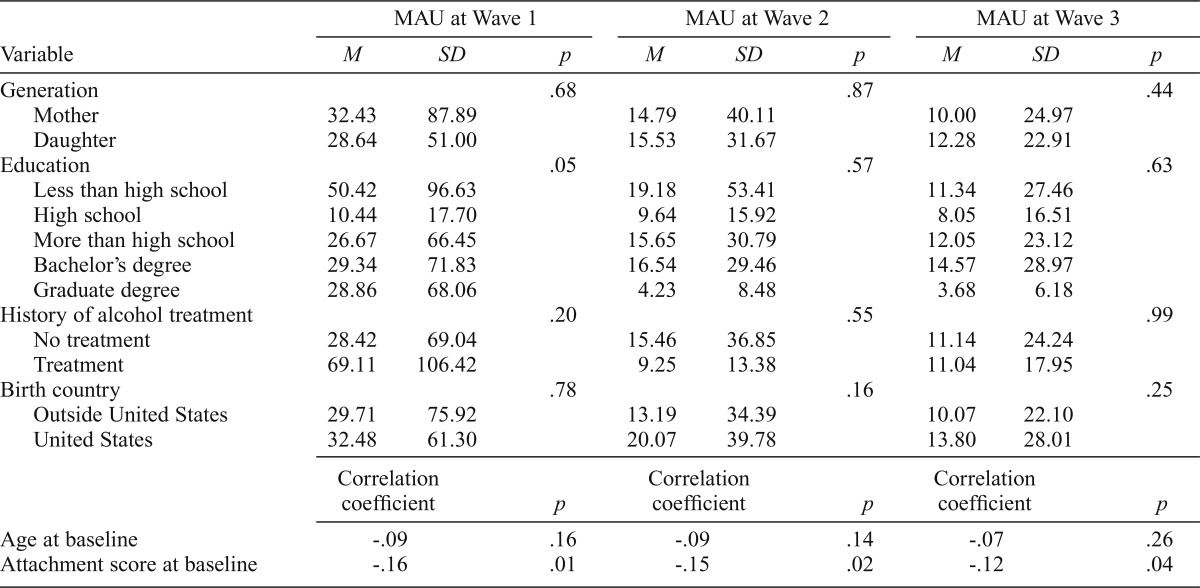
The results of bivariate analyses are shown in Table 2. We examined the relationship between demographics, history of alcohol use treatment, attachment score at baseline, and monthly alcohol use at each wave. The results show that attachment score at baseline is consistently negatively associated with monthly alcohol use at each wave. As for other variables, education level is also significantly associated with monthly alcohol use at Wave 1.
Table 2.
Descriptive analysis on the relationship between covariates and monthly alcohol use (MAU) over time
| MAU at Wave 1 |
MAU at Wave 2 |
MAU at Wave 3 |
|||||||
| Variable | M | SD | p | M | SD | p | M | SD | p |
| Generation | .68 | .87 | .44 | ||||||
| Mother | 32.43 | 87.89 | 14.79 | 40.11 | 10.00 | 24.97 | |||
| Daughter | 28.64 | 51.00 | 15.53 | 31.67 | 12.28 | 22.91 | |||
| Education | .05 | .57 | .63 | ||||||
| Less than high school | 50.42 | 96.63 | 19.18 | 53.41 | 11.34 | 27.46 | |||
| High school | 10.44 | 17.70 | 9.64 | 15.92 | 8.05 | 16.51 | |||
| More than high school | 26.67 | 66.45 | 15.65 | 30.79 | 12.05 | 23.12 | |||
| Bachelor’s degree | 29.34 | 71.83 | 16.54 | 29.46 | 14.57 | 28.97 | |||
| Graduate degree | 28.86 | 68.06 | 4.23 | 8.48 | 3.68 | 6.18 | |||
| History of alcohol treatment | .20 | .55 | .99 | ||||||
| No treatment | 28.42 | 69.04 | 15.46 | 36.85 | 11.14 | 24.24 | |||
| Treatment | 69.11 | 106.42 | 9.25 | 13.38 | 11.04 | 17.95 | |||
| Birth country | .78 | .16 | .25 | ||||||
| Outside United States | 29.71 | 75.92 | 13.19 | 34.39 | 10.07 | 22.10 | |||
| United States | 32.48 | 61.30 | 20.07 | 39.78 | 13.80 | 28.01 | |||
| Correlation coefficient | p | Correlation coefficient | p | Correlation coefficient | p | ||||
| Age at baseline | -.09 | .16 | -.09 | .14 | -.07 | .26 | |||
| Attachment score at baseline | -.16 | .01 | -.15 | .02 | -.12 | .04 | |||
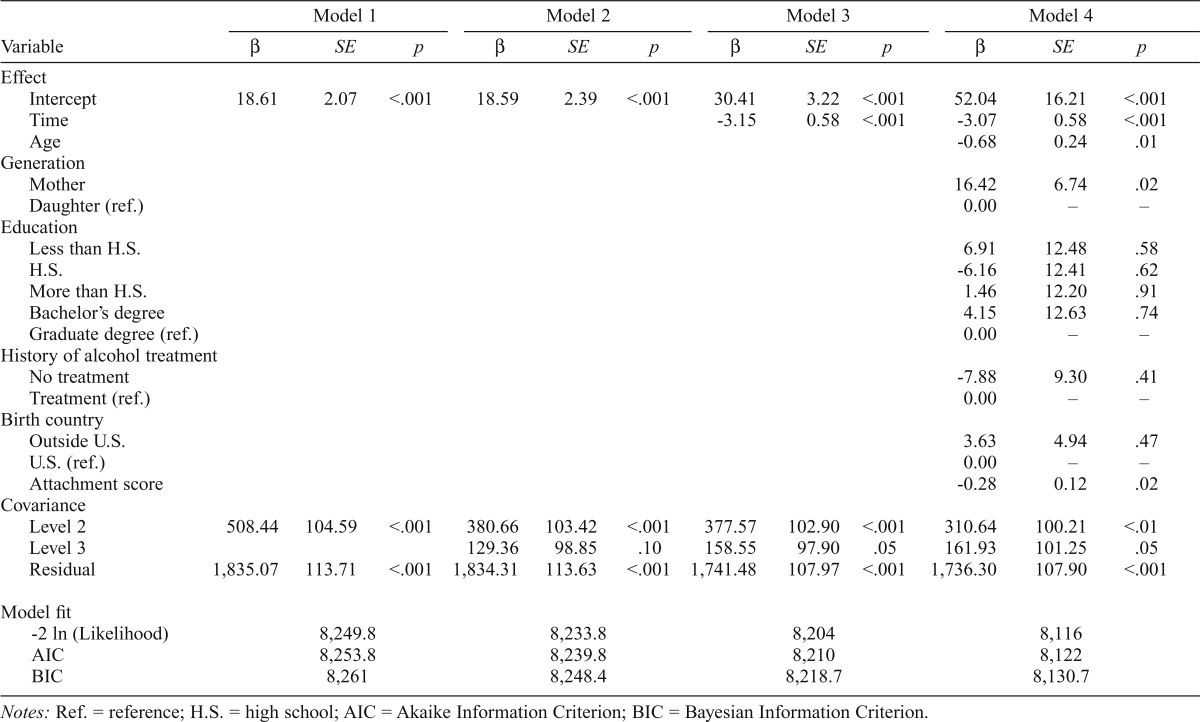
We report results of all multilevel longitudinal models of monthly alcohol use in Table 3. In Model 1, we fit the unconditional means model to the data and started from the two-level model with time point as Level 1 and individual as Level 2. We found significant variance between monthly alcohol use at various time points (likelihood ratio [LR] = 33.89, df = 1, p < .001).
Table 3.
Multilevel longitudinal modeling of longitudinal data on monthly alcohol use over time
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||||||
| Variable | β | SE | p | β | SE | p | β | SE | p | β | SE | p |
| Effect | ||||||||||||
| Intercept | 18.61 | 2.07 | <.001 | 18.59 | 2.39 | <.001 | 30.41 | 3.22 | <.001 | 52.04 | 16.21 | <.001 |
| Time | -3.15 | 0.58 | <.001 | -3.07 | 0.58 | <.001 | ||||||
| Age | -0.68 | 0.24 | .01 | |||||||||
| Generation | ||||||||||||
| Mother | 16.42 | 6.74 | .02 | |||||||||
| Daughter (ref.) | 0.00 | – | – | |||||||||
| Education | ||||||||||||
| Less than H.S. | 6.91 | 12.48 | .58 | |||||||||
| H.S. | -6.16 | 12.41 | .62 | |||||||||
| More than H.S. | 1.46 | 12.20 | .91 | |||||||||
| Bachelor’s degree | 4.15 | 12.63 | .74 | |||||||||
| Graduate degree (ref.) | 0.00 | – | – | |||||||||
| History of alcohol treatment | ||||||||||||
| No treatment | -7.88 | 9.30 | .41 | |||||||||
| Treatment (ref.) | 0.00 | – | – | |||||||||
| Birth country | ||||||||||||
| Outside U.S. | 3.63 | 4.94 | .47 | |||||||||
| U.S. (ref.) | 0.00 | – | – | |||||||||
| Attachment score | -0.28 | 0.12 | .02 | |||||||||
| Covariance | ||||||||||||
| Level 2 | 508.44 | 104.59 | <.001 | 380.66 | 103.42 | <.001 | 377.57 | 102.90 | <.001 | 310.64 | 100.21 | <.01 |
| Level 3 | 129.36 | 98.85 | .10 | 158.55 | 97.90 | .05 | 161.93 | 101.25 | .05 | |||
| Residual | 1,835.07 | 113.71 | <.001 | 1,834.31 | 113.63 | <.001 | 1,741.48 | 107.97 | <.001 | 1,736.30 | 107.90 | <.001 |
| Model fit | ||||||||||||
| -2 ln (Likelihood) | 8,249.8 | 8,233.8 | 8,204 | 8,116 | ||||||||
| AIC | 8,253.8 | 8,239.8 | 8,210 | 8,122 | ||||||||
| BIC | 8,261 | 8,248.4 | 8,218.7 | 8,130.7 | ||||||||
Notes: Ref. = reference; H.S. = high school; AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion.
In Model 2, we fit the three-level unconditional means model with time point as Level 1, individual as Level 2, and dyad as Level 3. We conducted a likelihood ratio test to compare the model fits between the two-level and three-level models. The model fit for the three-level model (LR = 49.97, df = 2, p < .001) is significantly better than the two-level model (LR = 16.08, df = 1, p < .001). The intraclass correlation coefficients (Snijders & Bosker, 1999) indicate that correlation among monthly alcohol use for different time points within the same individual is .22, and correlation among monthly alcohol use for different time points for different individuals within the same dyad is .06.
In Model 3, we added time to test our hypothesis that individuals would report changes in monthly alcohol use over time. As hypothesized, time was a significant predictor of change in monthly alcohol use (β = -3.15, p < .001). The negative coefficient indicates that, overall, monthly alcohol use decreased over time.
In Model 4, we added age, generation, education level, history of alcohol use treatment, birth country, and attachment score at baseline. We chose this model as the final model because this was the best model in terms of goodness of fit (i.e., it had the smallest -2 Ln [likelihood], Akaike Information Criterion, and Bayesian Information Criterion among the models).
Time remains significant (β = -3.07, p < .001), which indicated that each passing year is associated with a 3.07 drink decrease in monthly alcohol use. Regarding the effect of age at baseline, each additional year of age is associated with a 0.68 drink decrease in monthly alcohol use (β = -0.68, p < .05). Being a mother is associated with a 16.42 drink increase in monthly alcohol use compared with being a daughter. Each unit of increase in the attachment score at baseline is associated with a 0.28 drink decrease in monthly alcohol use (β = -0.28, p < .05) compared with average attachment score (M = 91.52). In other words, individuals with attachment score 1 SD (SD = 18) higher than the average attachment score are associated with a 5.04 drink decrease in monthly alcohol use. Regarding the effect size of attachment on monthly alcohol use, we compared the r correlation to the benchmarks of small, medium, and large effects (r = .1, .3, and .5, respectively) (Cohen, 1988). Converting the t value to the r correlation value (Nakagawa & Cuthill, 2007), we found that the r value for attachment is .09, which is close to .1, the benchmark of small effect (Cohen, 1988).
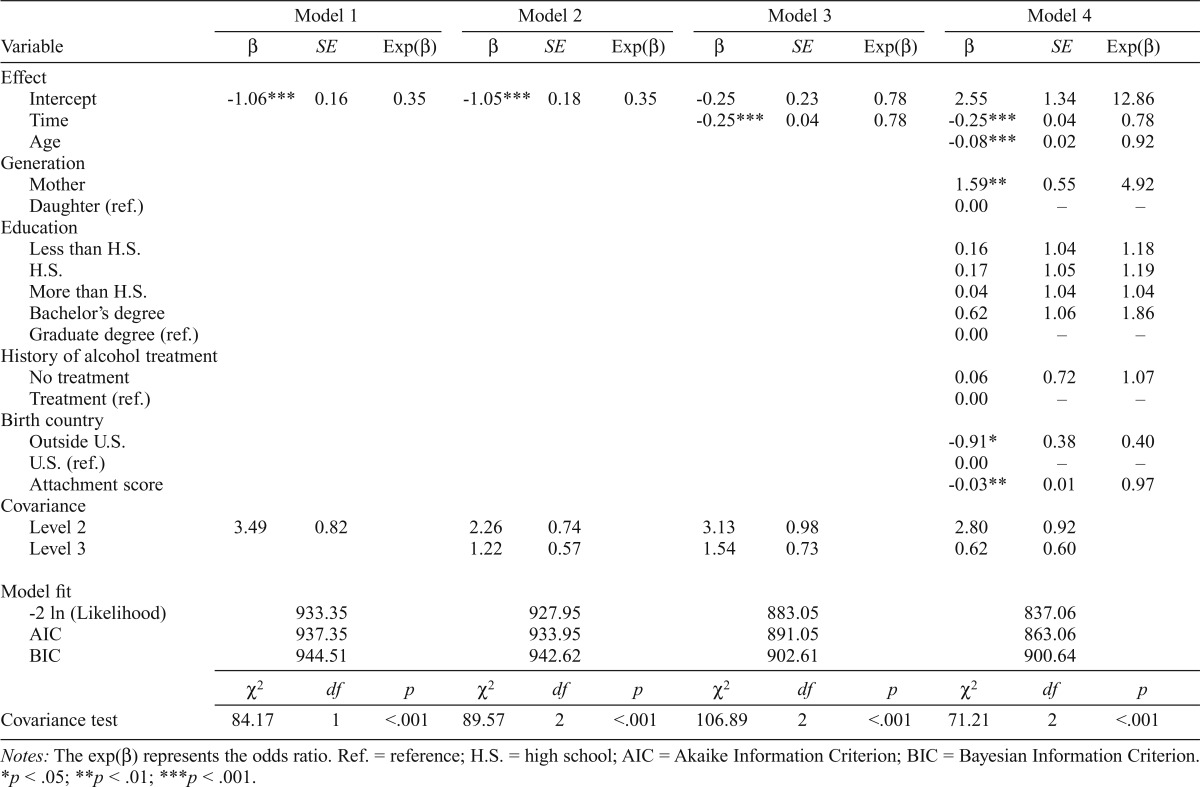
We report results of all multilevel longitudinal models of modeling heavy alcohol or other drug use in Table 4. As with monthly alcohol use, we ran four models for heavy alcohol or other drug use. Model 1 is the unconditional means two-level model with time point as Level 1 and individual as Level 2. Model 2 is the unconditional means three-level model with time point as Level 1, individual as Level 2, and dyad as Level 3. In Model 3, we added time. In Model 4, we added age, generation, education level, history of alcohol use treatment, birth country, and attachment score at baseline.
Table 4.
Multilevel longitudinal modeling of longitudinal data on heavy alcohol or drug use over time
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||||||
| Variable | β | SE | Exp(β) | β | SE | Exp(β) | β | SE | Exp(β) | β | SE | Exp(β) |
| Effect | ||||||||||||
| Intercept | -1.06*** | 0.16 | 0.35 | -1.05*** | 0.18 | 0.35 | -0.25 | 0.23 | 0.78 | 2.55 | 1.34 | 12.86 |
| Time | -0.25*** | 0.04 | 0.78 | -0.25*** | 0.04 | 0.78 | ||||||
| Age | -0.08*** | 0.02 | 0.92 | |||||||||
| Generation | ||||||||||||
| Mother | 1.59** | 0.55 | 4.92 | |||||||||
| Daughter (ref.) | 0.00 | – | – | |||||||||
| Education | ||||||||||||
| Less than H.S. | 0.16 | 1.04 | 1.18 | |||||||||
| H.S. | 0.17 | 1.05 | 1.19 | |||||||||
| More than H.S. | 0.04 | 1.04 | 1.04 | |||||||||
| Bachelor’s degree | 0.62 | 1.06 | 1.86 | |||||||||
| Graduate degree (ref.) | 0.00 | – | – | |||||||||
| History of alcohol treatment | ||||||||||||
| No treatment | 0.06 | 0.72 | 1.07 | |||||||||
| Treatment (ref.) | 0.00 | – | – | |||||||||
| Birth country | ||||||||||||
| Outside U.S. | -0.91* | 0.38 | 0.40 | |||||||||
| U.S. (ref.) | 0.00 | – | – | |||||||||
| Attachment score | -0.03** | 0.01 | 0.97 | |||||||||
| Covariance | ||||||||||||
| Level 2 | 3.49 | 0.82 | 2.26 | 0.74 | 3.13 | 0.98 | 2.80 | 0.92 | ||||
| Level 3 | 1.22 | 0.57 | 1.54 | 0.73 | 0.62 | 0.60 | ||||||
| Model fit | ||||||||||||
| -2 ln (Likelihood) | 933.35 | 927.95 | 883.05 | 837.06 | ||||||||
| AIC | 937.35 | 933.95 | 891.05 | 863.06 | ||||||||
| BIC | 944.51 | 942.62 | 902.61 | 900.64 | ||||||||
| χ2 | df | p | χ2 | df | p | χ2 | df | p | χ2 | df | p | |
| Covariance test | 84.17 | 1 | <.001 | 89.57 | 2 | <.001 | 106.89 | 2 | <.001 | 71.21 | 2 | <.001 |
Notes: The exp(β) represents the odds ratio. Ref. = reference; H.S. = high school; AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion.
p < .05;
p < .01;
p < .001.
We chose Model 4 as the final model because this was the best model in terms of goodness of fit. The test of covariance parameters results in a chi-square statistic of 71.21 (p < .001), which indicates that the model with random intercept fits the data significantly better than the model without random intercept. The intraclass correlation coefficients values indicate that correlation among heavy use of alcohol or illicit drugs for different time points within the same individual is .51, and correlation for different time points for different individuals within the same dyad is .09.
The results from modeling the dichotomous dependent variable heavy alcohol or other drug use are displayed in Table 4. Time remains significant [exp(β) = 0.78, p < .001], which indicates that the odds of being a heavy user of alcohol or illicit drugs at 1 year later are 0.78 times the odds in the previous year. Regarding the effect of age at baseline, the odds of being a heavy user for individuals who are 1 year older are 0.92 times that of individuals who are 1 year younger [exp(β) = 0.92, p < .001]. The odds of being a heavy user for mothers are 4.92 times that of daughters [exp(β) = 4.92, p < .01]. The odds of being a heavy user for individuals born outside the United States are 0.40 times that of individuals born in the United States [exp(β) = 0.40, p < .05]. Each unit of increase in the attachment score at baseline is associated with a lower likelihood of being a heavy alcohol or other drug user [exp(β) = 0.97, p < .01] compared with the average attachment score (M = 91.52). Regarding the effect size of attachment on heavy alcohol or other drug use, the r value for attachment is .13, which is slightly greater than .1, the benchmark of small effect (Cohen, 1988).
Discussion
This is the first longitudinal study of adult Latina mother and daughter alcohol use; our efforts yielded several substantive results. First, attachment at baseline was significantly associated with decreased substance use over time for both mothers and daughters. Second, substance use among adult Latinas decreased over time. Third, older age at baseline interview is associated with decreased substance use over time.
Fourth, being a mother in the relationship is associated with increased substance use over time. Fifth, being born outside the United States is associated with lower risk of heavy alcohol or other drug use over time.
Our previous cross-sectional study using baseline data documented that levels of mother–daughter attachment were significantly lower among dyads in which both members were heavy alcohol or other drug users than among dyads in which only one member used these substances or neither member used them (De La Rosa et al., 2010). The current study uses longitudinal data and shows that attachment at baseline is significantly associated with decreased substance use over time for our sample of mother–daughter dyads. Although the effect of parent–child attachment on the onset and persistence of substance use has been widely explored in child populations (Bahr et al., 1998; Brook et al., 1992; Thornberry et al., 2006), few studies have examined the effects of parent–child attachment on adults. Our findings are consistent with previous studies that included non-Latinas as the majority in their samples (Golder et al., 2005; Vungkhanching et al., 2004). Conceptually, this life span perspective of attachment and its effects follow John Bowlby’s pioneering work on attachment theory, in which he asserts that “attachment behaviour is held to characterize human beings from the cradle to the grave” (Bowlby, 1979, p. 129).
Four mechanisms might explain our finding on the relationship between attachment and substance use. First, better attachment can enhance mutual monitoring, as suggested by ecological theory (Bogenschneider, 1996). Mothers and daughters with better attachment to each other are more likely to be aware of each other’s substance overuse and intervene, which therefore reduces substance use. Second, better attachment increases the likelihood of adopting conventional Latino values (Brook et al., 1990; Farrington & Hawkins, 1991; Hawkins & Weis, 1985). One of these conventional Latino values is fulfilling traditional gender roles, and according to these roles Latina women are expected to refrain from heavy alcohol and other drug use (Rienzi et al., 1996; Torres Stone & Meyler, 2007; Villarreal, 2007). Women are also expected to bear and raise children (Calzada et al., 2010; Durand, 2011), which may have led our study participants—most of whom are immigrant Latinas—to value attachment, resulting in long-lasting effects on their substance use behaviors. Third, better attachment can reduce stress and, therefore, can reduce the risk of substance use (Golder et al., 2005; Kassel et al., 2007). Fourth, better attachment can provide alternative sources of reinforcement and, therefore, can reduce the risk of substance use (Commons, 1991).
Despite the small effect sizes of attachment on monthly alcohol use and heavy alcohol or other drug use over time, we believe that improving mother–daughter attachment should be a component of intervention strategies aiming to reduce substance use among adult Latina women. Practitioners can design interventions that directly target substance use but also improve family attachment, which can further reduce substance use. For example, practitioners can invite both mothers and daughters to attend the same treatment sessions and encourage communication between them.
Our findings—namely that (a) substance use among adult Latinas decreased over time and (b) older age at baseline is associated with decreased substance use—support the following findings from previous research: alcohol use and misuse tend to increase at adolescence, peak at early adulthood, and then decline during the third decade of life (Chen & Kandel, 1995; Johnstone et al., 1996). Additionally, our findings indicate that being a mother in the relationship is associated with increased substance use over time. One explanation might be the cohort effect that substance use in the daughter’s generation is lower than in the mother’s generation. However, there is a lack of demographic trend data to support this speculation. We also found that being born outside the United States is associated with a lower risk of heavy alcohol or other drug use over time compared with those born in the United States, which is consistent with findings from previous research (Gfroerer & Tan, 2003).
Our findings should be interpreted in light of the following limitations. First, the study of a nonnormative behavior such as heavy alcohol use is commonly prone to social desirability and reporting bias. In this regard, additional efforts were made to increase the quality of the data collection process by training interviewers to detect any inconsistencies in participants’ responses and to help respondents overcome literacy barriers. Second, the assessment of attachment was based on multiple assessments and used a scale that, although validated, does not necessarily capture the complexity of this construct. Empirical work on attachment has revealed the difficulty of defining attachment as a trait, a social construct, or a combination of both, and the difficulty surrounding its measurement as a graded or categorical entity (Bartholomew & Shaver, 1998; Feeney et al., 1994; Griffin & Bartholomew, 1994). Third, we used a small, nonrandomly selected sample of Latinas in Miami–Dade County; therefore, the findings might not be generalizable to the entire U.S. Latina population. Fourth, we did not include other forms of psychopathology and marital status because of the lack of data on these variables. Future research should consider other forms of psychopathology and marital status when studying determinants of alcohol use among Latina women. Fifth, we did not test the mediation effect of traditional Latino cultural values. Future research should test these mediation effects to explore how attachment influences individual alcohol use.
Despite these limitations, this first longitudinal study on adult Latina mother and daughter alcohol use provides insights into the role that mother–daughter attachment plays in the alcohol and other drug use trajectories of adult Latinas. Recognizing the positive impact of mother–daughter attachment in the process of reducing alcohol and other drug use is essential to the development of future family-based drug use prevention interventions targeting adult Latinas. Future research is needed on attachment taxonomy and on psychometrically sound attachment scales that address adult Latino cultural values within the framework of a developmental approach across the life span.
Acknowledgments
The authors acknowledge and thank Arnaldo Gonzalez for his editorial assistance, Weize Wang for data cleaning and preparation, and all the study participants and research staff for their collaborative efforts and invaluable contributions.
Footnotes
This research was supported by National Institute on Minority Health and Health Disparities Award #P20MD002288, National Institute on Drug Abuse Award #R24DA014260, and National Institute of Nursing Research Award #5R01NR012150-04. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Minority Health and Health Disparities, the National Institute on Drug Abuse, or the National Institute of Nursing Research.
References
- Alegría M., Vera M., Negrón G., Burgos M., Albizu C., Canino G. Methodological and conceptual issues in understanding female Hispanic drug users. In: Wetherington L., Roman A. B., editors. Drug addiction research and the health of women. Rockville, MD: National Institute on Drug Abuse; 1998. pp. 529–551. [Google Scholar]
- Armsden G. C., Greenberg M. T. The Inventory of Parent and Peer Attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence. 1987;16:427–454. doi: 10.1007/BF02202939. [DOI] [PubMed] [Google Scholar]
- Bacio G. A., Mays V. M., Lau A. S. Drinking initiation and problematic drinking among Latino adolescents: Explanations of the immigrant paradox. Psychology of Addictive Behaviors. 2013;27:14–22. doi: 10.1037/a0029996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahr S. J., Maughan S. L., Marcos A. C., Li B. Family, religiosity, and the risk of adolescent drug use. Journal of Marriage and Family. 1998;60:979–992. [Google Scholar]
- Bartholomew K., Shaver P. R. Methods of assessing adult attachment: Do they converge? In: Simpson J. A., Rholes W. S., editors. Attachment theory and close relationships. New York, NY: Guilford; 1998. pp. 25–45. [Google Scholar]
- Billings A. G., Cronkite R. C., Moos R. H. Social-environmental factors in unipolar depression: Comparisons of depressed patients and nondepressed controls. Journal of Abnormal Psychology. 1983;92:119–133. doi: 10.1037//0021-843x.92.2.119. [DOI] [PubMed] [Google Scholar]
- Bogenschneider K. An ecological risk/protective theory for building prevention programs, policies, and community capacity to support youth. Family Relations. 1996;45:127–138. [Google Scholar]
- Bowlby J. The making and breaking of affectional bonds. London, England: Tavistock; 1979. [Google Scholar]
- Brennan P. L., Schutte K. K., Moos R. H. Patterns and predictors of late-life drinking trajectories: A 10-year longitudinal study. Psychology of Addictive Behaviors. 2010;24:254–264. doi: 10.1037/a0018592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. [Google Scholar]
- Brook J. S., Brook D. W., Gordon A. S., Whiteman M., Cohen P. The psychosocial etiology of adolescent drug use: A family interactional approach. Genetic, Social, and General Psychology Monographs. 1990;116:111–267. [PubMed] [Google Scholar]
- Brook J. S., Whiteman M., Balka E. B., Hamburg B. A. African-American and Puerto Rican drug use: Personality, familial, and other environmental risk factors. Genetic, Social, and General Psychology Monographs. 1992;118:417–438. [PubMed] [Google Scholar]
- Calzada E. J., Fernandez Y., Cortes D. E. Incorporating the cultural value of respeto into a framework of Latino parenting. Cultural Diversity & Ethnic Minority Psychology. 2010;16:77–86. doi: 10.1037/a0016071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino I. A., Earley B. F., Rogler L. H. The Puerto Rican child in New York City: Stress and mental health (No. 4) New York, NY: Hispanic Research Center, Fordham University; 1980. [Google Scholar]
- Castillo-Mancilla J., Allshouse A., Collins C., Hastings-Tolsma M., Campbell T. B., Mawhinney S. Differences in sexual risk behavior and HIV/AIDS risk factors among foreign-born and US-born Hispanic women. Journal of Immigrant and Minority Health. 2012;14:89–99. doi: 10.1007/s10903-011-9529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavendish W., Nielsen A. L., Montague M. Parent attachment, school commitment, and problem behavior trajectories of diverse adolescents. Journal of Adolescence. 2012;35:1629–1639. doi: 10.1016/j.adolescence.2012.08.001. [DOI] [PubMed] [Google Scholar]
- Chen K., Kandel D. B. The natural history of drug use from adolescence to the mid-thirties in a general population sample. American Journal of Public Health. 1995;85:41–47. doi: 10.2105/ajph.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Commons M. L. A comparison and synthesis of Kohlberg’s cognitive-developmental and Gewirtz’s learning-developmental attachment theories. In: Gewirtz J. L., Kurtines W. M., editors. Intersections with attachment. Hillsdale, NJ: Lawrence Erlbaum Associates; 1991. pp. 257–291. [Google Scholar]
- De La Rosa M., Dillon F. R., Ganapati N. E., Rojas P., Pinto E., Prado G. Mother-daughter attachment and drug abuse among Latinas in the United States. Journal of Drug Issues. 2010;40:379–404. [Google Scholar]
- Durand T. M. Latina mothers’ cultural beliefs about their children, parental roles, and education: Implications for effective and empowering home-school partnerships. Urban Review. 2011;43:255–278. [Google Scholar]
- Farrington D. P., Hawkins J. D. Predicting participation, early onset and later persistence in officially recorded offending. Criminal Behaviour and Mental Health. 1991;1:1–33. [Google Scholar]
- Feeney J. A., Noller P., Hanrahan M. Assessing adult attachment: Developments in the conceptualization of security and insecurity. In: Sperling M. B., Berman W. H., editors. Attachment in adults: Theory, assessment and treatment. New York, NY: Guilford Press; 1994. pp. 128–152. [Google Scholar]
- Fergusson D. M., Boden J. M., Horwood L. J. Exposure to single parenthood in childhood and later mental health, educational, economic, and criminal behavior outcomes. Archives of General Psychiatry. 2007;64:1089–1095. doi: 10.1001/archpsyc.64.9.1089. [DOI] [PubMed] [Google Scholar]
- Galanti G. A. The Hispanic family and male-female relationships: An overview. Journal of Transcultural Nursing. 2003;14:180–185. doi: 10.1177/1043659603014003004. [DOI] [PubMed] [Google Scholar]
- Gfroerer J. C., Tan L. L. Substance use among foreign-born youths in the United States: Does the length of residence matter? American Journal of Public Health. 2003;93:1892–1895. doi: 10.2105/ajph.93.11.1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert M. J., Collins R. L. Ethnic variation in women’s and men’s drinking. In: Wilsnack R. W., Wilsnack S. C., editors. Gender and alcohol. New Brunswick, NJ: Rutgers Center of Alcohol Studies; 1997. pp. 357–378. [Google Scholar]
- Golder S., Gillmore M. R., Spieker S., Morrison D. Substance use, related problem behaviors and adult attachment in a sample of high risk older adolescent women. Journal of Child and Family Studies. 2005;14:181–193. [Google Scholar]
- Griffin D. W., Bartholomew K. Models of the self and other: Fundamental dimensions underlying measures of adult attachment. Journal of Personality and Social Psychology. 1994;67:430–445. [Google Scholar]
- Hawkins J. D., Weis J. G. The social development model: An integrated approach to delinquency prevention. Journal of Primary Prevention. 1985;6:73–97. doi: 10.1007/BF01325432. [DOI] [PubMed] [Google Scholar]
- Hilarski C. Primary caregiver and child attachment: An important assessment issue for substance use in African American and Hispanic youth. Journal of Evidence-Based Social Work. 2005;2:175–189. [Google Scholar]
- Johnstone B. M., Leino E. V., Ager C. R., Ferrer H., Fillmore K. M. Determinants of life-course variation in the frequency of alcohol consumption: Meta-analysis of studies from the collaborative alcohol-related longitudinal project. Journal of Studies on Alcohol. 1996;57:494–506. doi: 10.15288/jsa.1996.57.494. [DOI] [PubMed] [Google Scholar]
- Kassel J. D., Wardle M., Roberts J. E. Adult attachment security and college student substance use. Addictive Behaviors. 2007;32:1164–1176. doi: 10.1016/j.addbeh.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Loue S. Handbook of immigrant health. New York, NY: Plenum Press; 1998. [Google Scholar]
- Moos R. H., Brennan P. L., Schutte K. K., Moos B. S. High-risk alcohol consumption and late-life alcohol use problems. American Journal of Public Health. 2004;94:1985–1991. doi: 10.2105/ajph.94.11.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa S., Cuthill I. C. Effect size, confidence interval and statistical significance: A practical guide for biologists. Biological Reviews of the Cambridge Philosophical Society. 2007;82:591–605. doi: 10.1111/j.1469-185X.2007.00027.x. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Recommended alcohol questions. 2014. Retrieved from http://www.niaaa.nih.gov/research/guidelines-and-resources/recommended-alcohol-questions. [Google Scholar]
- O’Brien R. M. A caution regarding rules of thumb for variance inflation factors. Quality & Quantity. 2007;41:673–690. [Google Scholar]
- O’Farrell T. J., Fals-Stewart W., Murphy M. Concurrent validity of a brief self-report drug use frequency measure. Addictive Behaviors. 2003;28:327–337. doi: 10.1016/s0306-4603(01)00226-x. [DOI] [PubMed] [Google Scholar]
- Overbeek G., Stattin H., Vermulst A., Ha T., Engels R. C. M. E. Parent-child relationships, partner relationships, and emotional adjustment: A birth-to-maturity prospective study. Developmental Psychology. 2007;43:429–437. doi: 10.1037/0012-1649.43.2.429. [DOI] [PubMed] [Google Scholar]
- Perrino T., González-Soldevilla A., Pantin H., Szapocznik J. The role of families in adolescent HIV prevention: A review. Clinical Child and Family Psychology Review. 2000;3:81–96. doi: 10.1023/a:1009571518900. [DOI] [PubMed] [Google Scholar]
- Reese R. J., Kieffer K. M., Briggs B. K. A reliability generalization study of select measures of adult attachment style. Educational and Psychological Measurement. 2002;62:619–646. [Google Scholar]
- Rienzi B. M., McMillin J. D., Dickson C. L., Crauthers D., McNeill K. F., Pesina M. D., Mann E. Gender differences regarding peer influence and attitude toward substance abuse. Journal of Drug Education. 1996;26:339–347. doi: 10.2190/52C7-5P6B-FPH2-K5AH. [DOI] [PubMed] [Google Scholar]
- Sale E., Sambrano S., Springer J. F., Peña C., Pan W., Kasim R. Family protection and prevention of alcohol use among Hispanic youth at high risk. American Journal of Community Psychology. 2005;36:195–205. doi: 10.1007/s10464-005-8614-2. [DOI] [PubMed] [Google Scholar]
- Singer J. D. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;23:323–355. [Google Scholar]
- Singer J. D., Willett J. B. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Snijders T., Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Sokol-Katz J., Dunham R., Zimmerman R. Family structure versus parental attachment in controlling adolescent deviant behavior: A social control model. Adolescence. 1997;32:199–215. [PubMed] [Google Scholar]
- Szapocznik J., Coatsworth J. D. An ecodevelopmental framework for organizing risk and protection for drug abuse: A developmental model of risk and protection. In: Glantz M., Hartel C. R., editors. Drug abuse: Origins and interventions. Washington, DC: American Psychological Association; 1999. pp. 331–366. [Google Scholar]
- Thornberry T. P., Krohn M. D., Freeman-Gallant A. Intergenerational roots of early onset substance use. Journal of Drug Issues. 2006;36:1–28. [Google Scholar]
- Torres Stone R. A., Meyler D. Identifying potential risk and protective factors among non-metropolitan Latino youth: Cultural implications for substance use research. Journal of Immigrant and Minority Health. 2007;9:95–107. doi: 10.1007/s10903-006-9019-5. [DOI] [PubMed] [Google Scholar]
- Turner B. J., Fleishman J. A., Wenger N., London A. S., Burnam M. A., Shapiro M. F., Bozzette S. A. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. Journal of General Internal Medicine. 2001;16:625–633. doi: 10.1046/j.1525-1497.2001.016009625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umaña-Taylor A. J., Alfaro E. C., Bámaca M. Y., Guimond A. B. The central role of familial ethnic socialization in Latino adolescents’ cultural orientation. Journal of Marriage and Family. 2009;71:46–60. [Google Scholar]
- Vega W. A., Gil A. G., Warheit G. J., Zimmerman R. S., Apospori E. Acculturation and delinquent behavior among Cuban American adolescents: Toward an empirical model. American Journal of Community Psychology. 1993;21:113–125. doi: 10.1007/BF00938210. [DOI] [PubMed] [Google Scholar]
- Villarreal M. I. Women and health disparities: Implications for treating Hispanic women in rural and urban communities. Alcoholism Treatment Quarterly. 2007;25:91–110. [Google Scholar]
- Vungkhanching M., Sher K. J., Jackson K. M., Parra G. R. Relation of attachment style to family history of alcoholism and alcohol use disorders in early adulthood. Drug and Alcohol Dependence. 2004;75:47–53. doi: 10.1016/j.drugalcdep.2004.01.013. [DOI] [PubMed] [Google Scholar]
- Wagner K. D., Ritt-Olson A., Chou C.-P., Pokhrel P., Duan L., Baez-conde-Garbanati L., Unger J. B. Associations between family structure, family functioning, and substance use among Hispanic/Latino adolescents. Psychology of Addictive Behaviors. 2010;24:98–108. doi: 10.1037/a0018497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner T. D., Krebs C. P., Fishbein D. H. Perceiving the risk of substance use: The roles of nativity, acculturation, and family support among Hispanic children. Journal of Drug Issues. 2008;38:119–147. [Google Scholar]
- Young A. M., Glover N., Havens J. R. Nonmedical use of prescription medications among adolescents in the United States: A systematic review. Journal of Adolescent Health. 2012;51:6–17. doi: 10.1016/j.jadohealth.2012.01.011. [DOI] [PubMed] [Google Scholar]