Abstract
Objective:
Anxiety sensitivity appears to be relevant in understanding the nature of emotional symptoms and disorders associated with smoking. Negative-reinforcement smoking expectancies and motives are implicated as core regulatory processes that may explain, in part, the anxiety sensitivity–smoking interrelations; however, these pathways have received little empirical attention.
Method:
Participants (N = 471) were adult treatment-seeking daily smokers assessed for a smoking-cessation trial who provided baseline data; 157 participants provided within-treatment (pre-cessation) data. Anxiety sensitivity was examined as a cross-sectional predictor of several baseline smoking processes (nicotine dependence, perceived barriers to cessation, severity of prior withdrawal-related quit problems) and pre-cessation processes including nicotine withdrawal and smoking urges (assessed during 3 weeks before the quit day). Baseline negative-reinforcement smoking expectancies and motives were tested as simultaneous mediators via parallel multiple mediator models.
Results:
Higher levels of anxiety sensitivity were related to higher levels of nicotine dependence, greater perceived barriers to smoking cessation, more severe withdrawal-related problems during prior quit attempts, and greater average withdrawal before the quit day; effects were indirectly explained by the combination of both mediators. Higher levels of anxiety sensitivity were not directly related to pre-cessation smoking urges but were indirectly related through the independent and combined effects of the mediators.
Conclusions:
These empirical findings bolster theoretical models of anxiety sensitivity and smoking and identify targets for nicotine dependence etiology research and cessation interventions.
Emotional disorders and cigarette smoking frequently co-occur and are dynamically interrelated (Goodwin et al., 2012; Leventhal et al., 2012; Piper et al., 2011; Zvolensky et al., 2005). One psychological vulnerability factor that appears to be a robust predictor of both smoking and emotional disorders is anxiety sensitivity. Anxiety sensitivity is an individual difference factor related to psychological sensitivity to aversive internal states of anxiety and an amplifier of negative mood states (Reiss et al., 1986). Empirically, anxiety sensitivity is distinguishable from anxiety symptoms and general negative affect (Rapee & Medoro, 1994) and increases the risk of future development of anxiety symptoms, panic attacks, and certain anxiety and mood disorders (Schmidt et al., 1999).
Anxiety sensitivity also is related to certain aspects of smoking behavior (Leventhal & Zvolensky, in press). Smokers with higher levels of anxiety sensitivity perceive quitting as more difficult (Johnson et al., 2013) and report more intense nicotine withdrawal during early phases of quitting (Johnson et al., 2012). Higher levels of anxiety sensitivity are also related to greater odds of cessation failure (Assayag et al., 2012). Other research suggests that negative affect and smoking urges worsen before the quit date and increase the risk of lapse and relapse in some cases (Strong et al., 2009). This finding suggests that affect-relevant pre–quit-smoking processes could prevent smokers from making a quit attempt in the first place. However, it is unknown how anxiety sensitivity may affect the subjective experience of these processes. In addition, anxiety disorder status is associated with difficulties initiating smoking abstinence among treatment-seeking smokers (Piper et al., 2011), which suggests that anxiety sensitivity, an underlying mechanism of anxiety and negative-affective symptoms generally, may be related to these aspects of smoking.
The anxiety sensitivity–smoking comorbidity is theoretically based on negative-reinforcement models of substance use (Baker et al., 2004; Zvolensky & Schmidt, 2003). Specifically, holding stronger beliefs about the anticipated negative affect–reduction properties of smoking (outcome expectancies; Brandon & Baker, 1991) and negative affect–reduction reasons for smoking (motives; McCarthy et al., 2010) are two central processes thought to underlie the anxiety sensitivity–smoking relationships. Indeed, higher levels of anxiety sensitivity are associated with negative affect–reduction smoking motives and expectancies (Battista et al., 2008; Johnson et al., 2013; Leyro et al., 2008).
These subjective expectations and motives may be linked to actual smoking effects, as high anxiety-sensitive smokers also report greater smoking-induced reductions in subjective anxiety after stressful laboratory situations (Evatt & Kassel, 2010; Perkins et al., 2010). Nevertheless, expectations and subjective motives may be particularly salient factors for high anxiety-sensitive smokers. The cognitive tendency to “forecast” and form inaccurate conclusions related to somatic–affective symptoms may be simultaneously related to both anxiety sensitivity and smoking behavior. Although some existing work has examined anxiety sensitivity, negative-affect–reduction expectancies, and motives in terms of various aspects of smoking cessation (Gonzalez et al., 2008), no studies have empirically examined the role of the affect-regulatory processes (which are posited as mediator variables).
The present study examined the independent and combined effects of two potential mediators (affect-regulatory expectancies and motives) in the relation of anxiety sensitivity to various smoking variables. Among a sample of treatment-seeking smokers, baseline smoking characteristics (nicotine dependence, perceived barriers to smoking cessation, and severity of problematic symptoms during prior quit attempts) and smoking processes related to the present quit attempt (average nicotine withdrawal and smoking urges during 3 weeks before quitting) were examined as relevant criterion processes. It was hypothesized that higher levels of anxiety sensitivity would be related to higher levels of nicotine dependence, greater perceived barriers to quitting, and more severe problems during prior quit attempts. Anxiety sensitivity was also expected to be predictive of higher average levels of self-reported nicotine withdrawal and smoking urges during the 3 weeks before the quit day. These relations were expected to be mediated by both the independent and the combined indirect effects of negative affect–reduction smoking expectancies and motives, which would be evident after adjusting for variables known to co-occur with anxiety sensitivity and smoking (Johnson et al., 2013).
Method
Participants
Adult treatment-seeking daily smokers (N = 471; Mage = 36.5 years, SD = 13.54; 48.4% female) were recruited to participate in a large, randomized controlled trial examining the efficacy of two smoking-cessation interventions. Inclusion criteria for the parental study included daily cigarette use (average of eight or more cigarettes per day for at least 1 year), age between 18 and 65 years, and reported motivation to quit smoking of at least 5 on a 10-point scale. Exclusion criteria included inability to give informed consent, current use of smoking-cessation treatment, past-month suicidality, and history of psychotic-spectrum disorders.
Participants self-identified their race as White (85.9%), African American (8.3%), Hispanic (2.5%), Asian (1.1%), or other (2.5%). Participants were generally well educated (74.0% completed at least part of college) and primarily indicated being either never married (44.2%) or married/ cohabitating (33.1%). The smoking rate in the past week was 16.7 (SD = 9.92) cigarettes per day with moderate levels of nicotine dependence (Fagerström Test for Nicotine Dependence [FTND]; Heatherton et al., 1991: M = 5.1, SD = 2.30). The average number of prior quit attempts was 3.4 (SD = 2.48). Nearly one third of the sample (29.5%) reported a tobacco-related illness, and 51.2% met criteria for a lifetime history of an emotional disorder. Past-month alcohol and cannabis use was 80.7% and 56.1%, respectively.
Of the baseline sample, 209 (44.4%) participants were determined eligible for the treatment phase of the study, and of that subset, 157 (75.1%) provide pre-cessation (within treatment) data. There were no statistically significant differences in any of the pretreatment variables among treatment-eligible participants who did and did not initiate treatment.
Measures
Covariates.
The Structured Clinical Interview for DSM-IV Axis I Disorders, Non-Patient Version (SCID-I/ NP; First et al., 2007) is an assessment of lifetime Axis I psychopathology. A dichotomous variable was created to reflect those who met criteria for any history of a depressive or anxiety disorder (1 = emotional disorder); all other participants were coded as the reference group (0 = no emotional disorder). The Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 1992) is a 10-item self-report measure developed to identify individuals with alcohol problems. The AUDIT total score was used as a covariate; internal consistency was α = .84. The Marijuana Smoking History Questionnaire (MSHQ; Bonn-Miller & Zvolensky, 2009) is a 40-item measure that assesses cannabis use history and patterns of use. One item was used as a covariate in the current study: “Please rate your marijuana use in the past 30 days”; dichotomously coded (0 = no use, 1 = past-30-day use). A medical history checklist was used to index tobacco-related medical problems (heart problems, hypertension, respiratory disease, and asthma). Items endorsed were totaled (observed range: 0–3), with higher scores reflecting greater tobacco-related disease.
Predictor variable.
The Anxiety Sensitivity Index–3 (ASI-3; Taylor et al., 2007) is an 18-item measure in which respondents indicate the extent to which they are concerned about possible negative consequences of anxiety-related symptoms (e.g., “It scares me when my heart beats rapidly”). Responses are rated on a 5-point Likert scale ranging from 0 (very little) to 4 (very much) and summed to create a total score. ASI-3 has strong and improved psychometric properties (Reiss et al., 1986; Taylor et al., 2007); internal consistency was α = .93.
Mediator variables.
The Smoking Consequences Questionnaire (SCQ; Brandon & Baker, 1991) is a 50-item self-report measure that assesses smoking expectancies on a 10-point scale for likelihood of occurrence (0 = completely unlikely to 9 = completely likely). The entire measure and its factors have demonstrated sound psychometric properties. The Negative Reinforcement/Negative Affect Reduction subscale (SCQ-NR) was used as a mediator variable (M1); internal consistency was α = .93.
The Reasons for Smoking (RFS; Ikard et al., 1969) is a 23-item self-report measure that assesses motivations for smoking. Participants rate their tendency to smoke in circumstances listed, rated on a 5-point Likert scale (1 = never to 5 = always). The psychometric properties of this scale are well established. The Negative Affect Reduction subscale (RFS-NA) was used as a mediator variable (M2); internal consistency was α = .89.
Criterion variables.
The FTND (Heatherton et al., 1991) is a six-item scale that assesses gradations in tobacco dependence. Scores range from 0 to 10, with higher scores reflecting high levels of physiological dependence on nicotine. The FTND has adequate reliability and is associated with key smoking variables; internal consistency was α = .64.
The Barriers to Cessation Scale (BCS; Macnee & Talsma, 1995) is a 19-item self-report assessment of barriers associated with quitting smoking. Respondents indicate, on a 4-point Likert scale (0 = not a barrier or not applicable to 3 = large barrier), the degree to which they identify with each barrier (e.g., “Weight gain,” “Friends encouraging you to smoke,” “Fear of failing to quit”). Scores are summed and a total score is derived. The BCS has strong psychometric properties (Macnee & Talsma, 1995); internal consistency was α = .89 in the sample.
The Smoking History Questionnaire (SHQ; Brown et al., 2002) is a self-report questionnaire used to assess smoking history, pattern, and retrospective quit history. In the present study, the SHQ was used to describe the sample on smoking history and patterns of use and then to create a mean composite score of withdrawal-related problem symptoms experienced during past quit attempts (e.g., nausea, irritability, and anxiety).
The Minnesota Nicotine Withdrawal Scale (MNWS; Hughes & Hatsukami, 1986) is an eight-item measure of nicotine withdrawal symptoms experienced in the past week, which are rated on a 4-point Likert-type scale, ranging from 0 = not present to 3 = severe (e.g., depression, insomnia, irritability/frustration, anxiety, difficulty concentrating, urges/ cravings, restlessness, and increased appetite). The MNWS was administered during the 3 weeks before the quit day, and scores were averaged to compute a mean composite of pre-cessation withdrawal severity; Cronbach’s α range was .85–.87 in the sample across the three time points.
The Questionnaire of Smoking Urges (QSU; Tiffany & Drobes, 1991) is a 32-item self-report measure of smoking urges and cravings in which respondents rate the extent to which they agree or disagree with each item (e.g., “I will smoke as soon as I get a chance”) based on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree). A total sum score of smoking urges is computed. The QSU was administered during the 3 weeks before the quit day, and scores were averaged to compute a mean composite of pre-cessation smoking urges; Cronbach’s α range was .61–.74 in the sample across the three time points.
Procedure
Community-recruited daily smokers (responding to flyers, newspaper ads, and radio announcements) were recruited for a dual-site smoking-cessation trial. The study protocol was approved by the institutional review board at both sites. Individuals were scheduled for a baseline assessment during which study inclusion and exclusion criteria were evaluated. After providing written, informed consent, participants were interviewed using the SCID-I/NP and completed a computerized battery of self-report questionnaires, including measures of nicotine dependence, barriers to smoking cessation, and quit history. Eligible participants were randomly assigned to one of two smoking-cessation treatment programs and scheduled for treatment initiation approximately 1–2 weeks after the baseline assessment.
Treatment consisted of either a standard smoking-cessation program (Fiore et al., 2008) or anxiety-focused smoking-cessation treatment (Zvolensky et al., 2008). Treatment consisted of four 60-minute weekly sessions conducted by a trained doctoral-level graduate student. Nicotine replacement therapy (NRT), which was initiated at Session 4 (quit day), was used in both treatments. After each treatment session (Sessions 1–4), self-report assessments were completed, including assessment of smoking urges and nicotine withdrawal. Only self-reported nicotine withdrawal and urge assessments from treatment Sessions 1–3 were used in the current analyses (pre-cessation processes).
Data analytic strategy
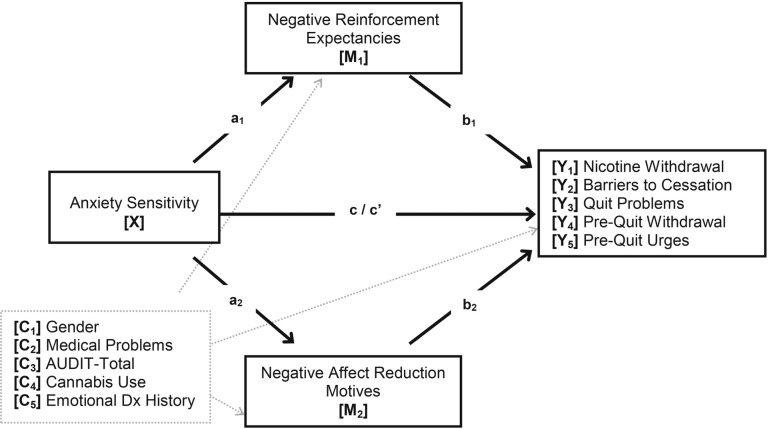
First, correlations among study variables were examined. Next, five models were conducted to examine the impact of the mediators (expectancies, SCQ-NR; M1 and motives, RFS-NA; M2) in relation to anxiety sensitivity (ASI-3; X) and the five criterion outcomes: nicotine dependence (FTND; Y1), barriers to smoking cessation (BCS-Total; Y2), severity of prior quit problems (Quit Problems; Y3), pre-cessation withdrawal symptoms (MNWS; Y4), and pre-cessation smoking urges (QSU; Y5). See Figure 1 for a visual of the conceptual model.
Figure 1.
Conceptual model of parallel multiple mediator analyses. AUDIT = Alcohol Use Disorders Identification Test; Dx = diagnosis; a1 and a2 = specific direct effects of X on M1 and M2; b1 and b2 = specific direct effects of M1 and M2 on Y; c = total effect of X on Y, independent of M1 and M2; c′ = direct effect of X on Y, controlling for M1 and M2; a1 × b1 and a2 × b2 can be computed to determine the relative indirect effects of M1 and M2; (a1 × b1) × (a2 × b2) is computed to determine the combined indirect effect of both mediators.
Gender, tobacco-related medical problems, problematic alcohol use (AUDIT), cannabis use status (MSHQ), and history of emotional disorders (per SCID-I/NP) were included as covariates in all models. The analyses were conducted using PROCESS, a conditional modeling program that uses an ordinary least squares–based analytical framework to test for both direct and indirect effects. All relative and total indirect effects were subjected to follow-up bootstrap analyses with 10,000 samples. A 95-percentile confidence interval (CI) estimate was derived for significance testing (Hayes, 2009, 2013; Preacher & Hayes, 2004, 2008).
Results
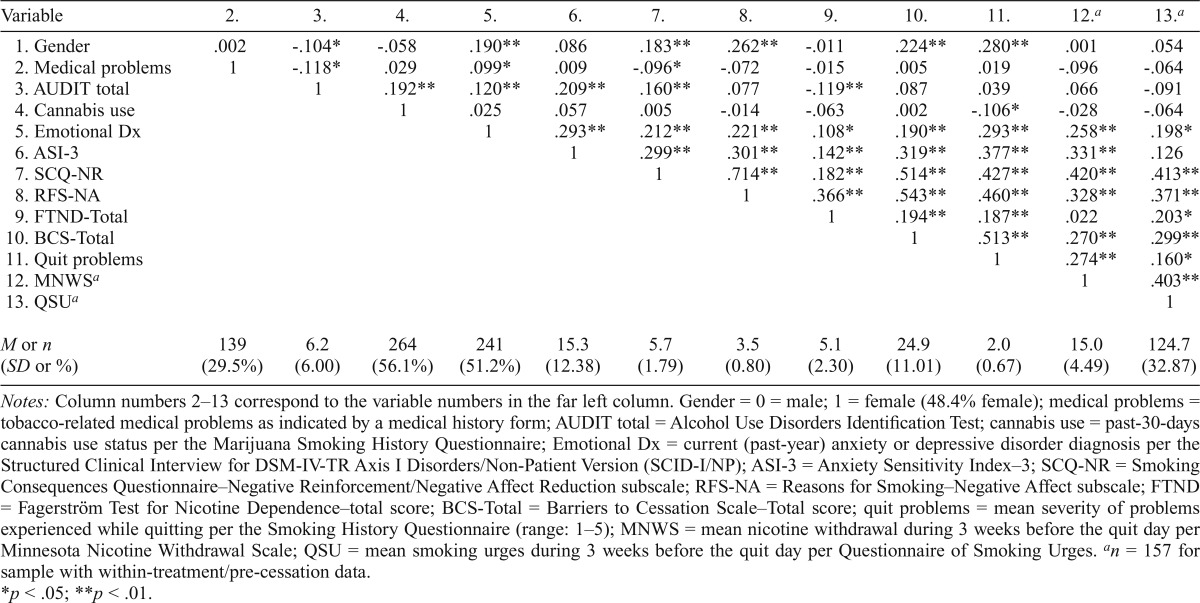
Baseline levels of anxiety sensitivity were in the moderate range (M = 15.3, SD = 12.38). Anxiety sensitivity was positively associated with negative affect–reduction expectancies and smoking motives, baseline smoking characteristics (nicotine dependence, perceived barriers to smoking cessation, and severity of prior withdrawal-related quit problems), and pre-cessation nicotine withdrawal but not with smoking urges (Table 1). Of note, negative-reinforcement smoking expectancies and motives were highly interrelated. In addition, female gender was significantly positively associated with expectancies and motives as well as greater perceived barriers to quitting smoking and more severe withdrawal-related problems during previous quit attempts.
Table 1.
Descriptive statistics and correlations for study variables
| Variable | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12.a | 13.a |
| 1. Gender | .002 | -.104* | -.058 | .190** | .086 | .183** | .262** | -.011 | .224** | .280** | .001 | .054 |
| 2. Medical problems | 1 | -.118* | .029 | .099* | .009 | -.096* | -.072 | -.015 | .005 | .019 | -.096 | -.064 |
| 3. AUDIT total | 1 | .192** | .120** | .209** | .160** | .077 | -.119** | .087 | .039 | .066 | -.091 | |
| 4. Cannabis use | 1 | .025 | .057 | .005 | -.014 | -.063 | .002 | -.106* | -.028 | -.064 | ||
| 5. Emotional Dx | 1 | .293** | .212** | .221** | .108* | .190** | .293** | .258** | .198* | |||
| 6. ASI-3 | 1 | .299** | .301** | .142** | .319** | .377** | .331** | .126 | ||||
| 7. SCQ-NR | 1 | .714** | .182** | .514** | .427** | .420** | .413** | |||||
| 8. RFS-NA | 1 | .366** | .543** | .460** | .328** | .371** | ||||||
| 9. FTND-Total | 1 | .194** | .187** | .022 | .203* | |||||||
| 10. BCS-Total | 1 | .513** | .270** | .299** | ||||||||
| 11. Quit problems | 1 | .274** | .160* | |||||||||
| 12. MNWSa | 1 | .403** | ||||||||||
| 13. QSUa | 1 | |||||||||||
| M or n (SD or %) | 139 (29.5%) | 6.2 (6.00) | 264 (56.1%) | 241 (51.2%) | 15.3 (12.38) | 5.7 (1.79) | 3.5 (0.80) | 5.1 (2.30) | 24.9 (11.01) | 2.0 (0.67) | 15.0 (4.49) | 124.7 (32.87) |
Notes: Column numbers 2–13 correspond to the variable numbers in the far left column. Gender = 0 = male; 1 = female (48.4% female); medical problems = tobacco-related medical problems as indicated by a medical history form; AUDIT total = Alcohol Use Disorders Identification Test; cannabis use = past-30-days cannabis use status per the Marijuana Smoking History Questionnaire; Emotional Dx = current (past-year) anxiety or depressive disorder diagnosis per the Structured Clinical Interview for DSM-IV-TR Axis I Disorders/Non-Patient Version (SCID-I/NP); ASI-3 = Anxiety Sensitivity Index–3; SCQ-NR = Smoking Consequences Questionnaire–Negative Reinforcement/Negative Affect Reduction subscale; RFS-NA = Reasons for Smoking–Negative Affect subscale; FTND = Fagerström Test for Nicotine Dependence–total score; BCS-Total = Barriers to Cessation Scale–Total score; quit problems = mean severity of problems experienced while quitting per the Smoking History Questionnaire (range: 1–5); MNWS = mean nicotine withdrawal during 3 weeks before the quit day per Minnesota Nicotine Withdrawal Scale; QSU = mean smoking urges during 3 weeks before the quit day per Questionnaire of Smoking Urges.
n = 157 for sample with within-treatment/pre-cessation data.
p<.05;
p<.01.
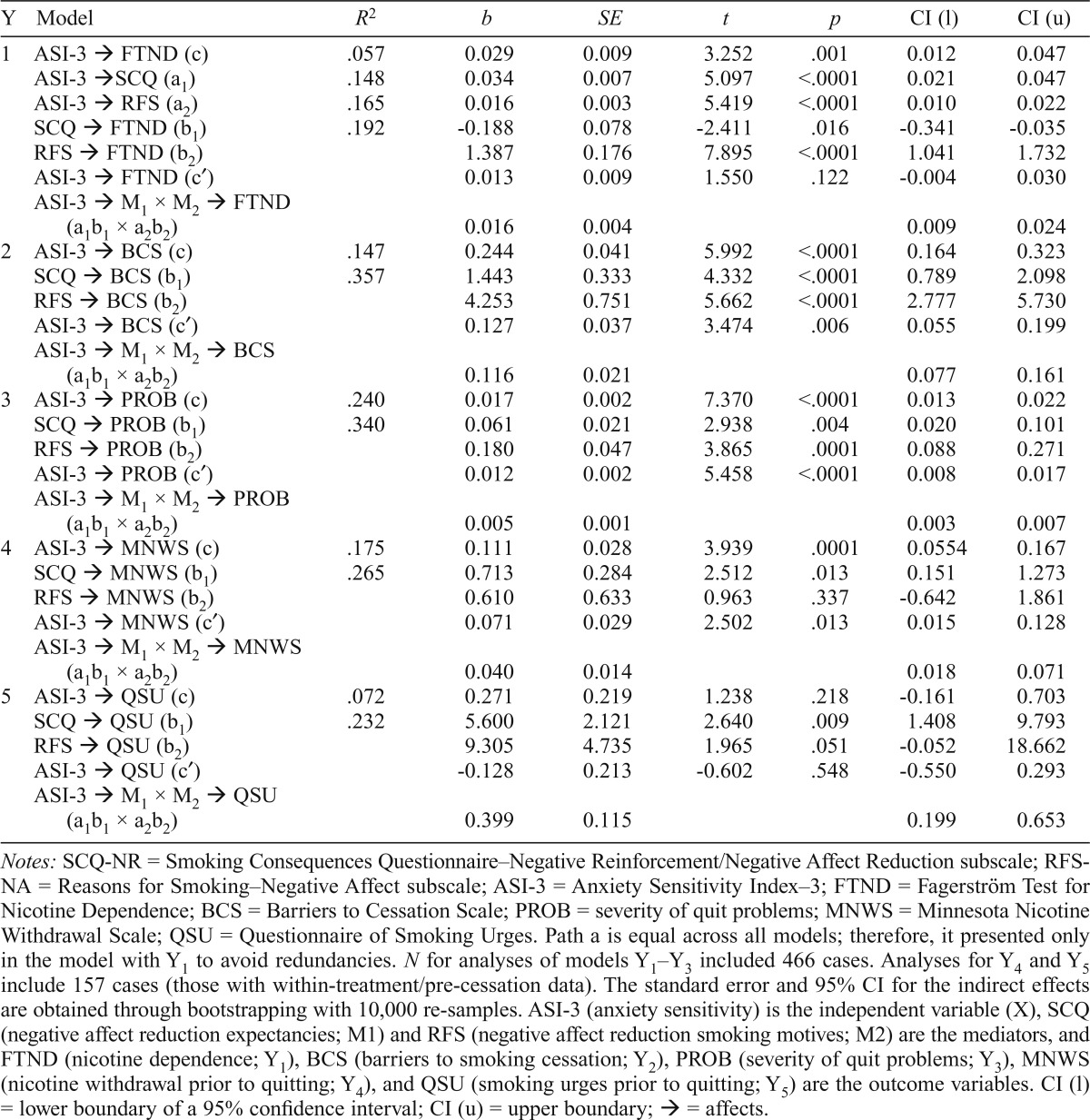
Results for regression pathways and estimates of the indirect effects tested for mediation are presented in Table 2. Results indicated that the total effects model for nicotine dependence (Y1) was significant, F(6, 464) = 4.687, p = .0001, with higher levels of anxiety sensitivity predicting higher levels of nicotine dependence. To test for mediation, the combined indirect effects of expectancies and motives were estimated. Bootstrapping estimate revealed that the indirect effects of expectancies and motives were significant (b = .016, 95% CI [.009, .024]), such that the association between anxiety sensitivity and nicotine dependence occurred indirectly through holding stronger expectancies about the negative-reinforcement properties of smoking and smoking for negative affect–reduction reasons. The independent indirect effect of negative-reinforcement motives was also significant (b = .022, 95% CI [.014, .032]). After we controlled for the mediators, the effect of anxiety sensitivity on nicotine dependence was nonsignificant.
Table 2.
Regression results for the mediation of the effect of anxiety sensitivity on smoking variables by SCQ-NR and RFS-NA
| Y | Model | R2 | b | SE | t | p | CI (l) | CI (u) |
| 1 | ASI-3 → FTND (c) | .057 | 0.029 | 0.009 | 3.252 | .001 | 0.012 | 0.047 |
| ASI-3 →SCQ (a1) | .148 | 0.034 | 0.007 | 5.097 | <.0001 | 0.021 | 0.047 | |
| ASI-3 → RFS (a2) | .165 | 0.016 | 0.003 | 5.419 | <.0001 | 0.010 | 0.022 | |
| SCQ → FTND (b1) | .192 | -0.188 | 0.078 | -2.411 | .016 | -0.341 | -0.035 | |
| RFS → FTND (b2) | 1.387 | 0.176 | 7.895 | <.0001 | 1.041 | 1.732 | ||
| ASI-3 → FTND (c′) | 0.013 | 0.009 | 1.550 | .122 | -0.004 | 0.030 | ||
| ASI-3 → M1 × M2 → FTND (a1b1 × a2b2) | 0.016 | 0.004 | 0.009 | 0.024 | ||||
| 2 | ASI-3 → BCS (c) | .147 | 0.244 | 0.041 | 5.992 | <.0001 | 0.164 | 0.323 |
| SCQ → BCS (b1) | .357 | 1.443 | 0.333 | 4.332 | <.0001 | 0.789 | 2.098 | |
| RFS → BCS (b2) | 4.253 | 0.751 | 5.662 | <.0001 | 2.777 | 5.730 | ||
| ASI-3 → BCS (c′) | 0.127 | 0.037 | 3.474 | .006 | 0.055 | 0.199 | ||
| ASI-3 → M1 × M2 → BCS (a1b1 × a2b2) | 0.116 | 0.021 | 0.077 | 0.161 | ||||
| 3 | ASI-3 → PROB (c) | .240 | 0.017 | 0.002 | 7.370 | <.0001 | 0.013 | 0.022 |
| SCQ → PROB (b1) | .340 | 0.061 | 0.021 | 2.938 | .004 | 0.020 | 0.101 | |
| RFS → PROB (b2) | 0.180 | 0.047 | 3.865 | .0001 | 0.088 | 0.271 | ||
| ASI-3 → PROB (c′) | 0.012 | 0.002 | 5.458 | <.0001 | 0.008 | 0.017 | ||
| ASI-3 → M1 × M2 → PROB (a1b1 × a2b2) | 0.005 | 0.001 | 0.003 | 0.007 | ||||
| 4 | ASI-3 → MNWS (c) | .175 | 0.111 | 0.028 | 3.939 | .0001 | 0.0554 | 0.167 |
| SCQ → MNWS (b1) | .265 | 0.713 | 0.284 | 2.512 | .013 | 0.151 | 1.273 | |
| RFS → MNWS (b2) | 0.610 | 0.633 | 0.963 | .337 | -0.642 | 1.861 | ||
| ASI-3 → MNWS (c′) | 0.071 | 0.029 | 2.502 | .013 | 0.015 | 0.128 | ||
| ASI-3 → M1 × M2 → MNWS (a1b1 × a2b2) | 0.040 | 0.014 | 0.018 | 0.071 | ||||
| 5 | ASI-3 → QSU (c) | .072 | 0.271 | 0.219 | 1.238 | .218 | -0.161 | 0.703 |
| SCQ → QSU (b1) | .232 | 5.600 | 2.121 | 2.640 | .009 | 1.408 | 9.793 | |
| RFS → QSU (b2) | 9.305 | 4.735 | 1.965 | .051 | -0.052 | 18.662 | ||
| ASI-3 → QSU (c′) | -0.128 | 0.213 | -0.602 | .548 | -0.550 | 0.293 | ||
| ASI-3 → M1 × M2 → QSU (a1b1 × a2b2) | 0.399 | 0.115 | 0.199 | 0.653 |
Notes: SCQ-NR = Smoking Consequences Questionnaire–Negative Reinforcement/Negative Affect Reduction subscale; RFS-NA = Reasons for Smoking–Negative Affect subscale; ASI-3 = Anxiety Sensitivity Index–3; FTND = Fagerström Test for Nicotine Dependence; BCS = Barriers to Cessation Scale; PROB = severity of quit problems; MNWS = Minnesota Nicotine Withdrawal Scale; QSU = Questionnaire of Smoking Urges. Path a is equal across all models; therefore, it presented only in the model with Y1 to avoid redundancies. N for analyses of models Y1–Y3 included 466 cases. Analyses for Y4 and Y5 include 157 cases (those with within-treatment/pre-cessation data). The standard error and 95% CI for the indirect effects are obtained through bootstrapping with 10,000 re-samples. ASI-3 (anxiety sensitivity) is the independent variable (X), SCQ (negative affect reduction expectancies; M1) and RFS (negative affect reduction smoking motives; M2) are the mediators, and FTND (nicotine dependence; Y1), BCS (barriers to smoking cessation; Y2), PROB (severity of quit problems; Y3), MNWS (nicotine withdrawal prior to quitting; Y4), and QSU (smoking urges prior to quitting; Y5) are the outcome variables. CI (l) = lower boundary of a 95% confidence interval; CI (u) = upper boundary; → = affects.
Analyses for the model of barriers to smoking cessation (Y2) revealed a significant total effect, F(6, 464) = 13.336, p < .0001, with higher levels of anxiety sensitivity predicting greater perceived barriers to smoking cessation. After we controlled for the mediators, the effect of anxiety sensitivity on perceived barriers remained significant. The combined indirect effect of negative-reinforcement expectancies and motives was significant (b = .116, 95% CI [.077, .161]), such that the association between anxiety sensitivity and barriers to smoking cessation occurred indirectly through stronger negative-reinforcement smoking expectancies and negative affect–reduction smoking motives. The indirect effect of each independent mediator was also significant: expectancies (b = .049, 95% CI [.024, .084]) and motives (b = .068, 95% CI [.036, .110]).
Results of the total effects model for prior quit problems (Y3) were significant, F(6, 464) = 24.360, p < .0001, with higher levels of anxiety sensitivity predictive of greater severity of prior quit problems. This effect remained significant after we controlled for both mediators. The combined indirect effect of negative-reinforcement expectancies and motives was significant (b = .005, 95% CI [.003, .007]).
Each independent indirect effect of expectancies (b = .007, 95% CI [.001, .020]) and motives (b = .007, 95% CI [.001, .020]) was also significant.
Results indicated that the total effects model for pre-cessation nicotine withdrawal severity (Y4) was significant, F(6, 150) = 5.295, p < .0001, with higher levels of anxiety sensitivity predicting higher levels of pre-cessation nicotine withdrawal. After the mediators were controlled for, the direct effect of anxiety sensitivity on pre-cessation nicotine withdrawal remained significant; however, in the test of mediation, results revealed a significant combined indirect effect of SCQ-NR and RFS-NA (b = .040, 95% CI [.018, .071]), with anxiety sensitivity predicting more severe nicotine withdrawal at treatment initiation through the combination of negative-reinforcement smoking expectances and negative affect–reduction smoking motives. In addition, the independent indirect effect of negative-reinforcement expectancies was significant (b = .028, 95% CI [.008, .057]).
In the model of smoking urges (Y5), the total effects model was nonsignificant, F(6, 150) = 1.936, p = .079; anxiety sensitivity did not predict pre-cessation smoking urges. However, the combined indirect effect of negative-reinforcement expectancies and motives (b = .399, 95% CI [.199, .653]) was significant, such that higher levels of anxiety sensitivity were predictive of greater pre-cessation smoking urges through the greater negative-reinforcement smoking expectances and motives. Each independent indirect effect of expectancies (b = .220, 95% CI [.079, .428]) and motives (b = .179, 95% CI [.016, .414]) was also significant.
Post hoc specificity analyses
As a method of further strengthening the interpretation of the cross-sectional indirect effects, alternative models of the direct effects were tested by reversing the two proposed mediators with the predictor. Analyses were conducted using MEDIATE (Hayes & Preacher, 2014), a modeling program that allows for testing of the direct, indirect, and total effects of independent variables (Xi) on an outcome variable (Y) through a proposed mediator variable (M) or set of mediator variables (Mi); inferences for indirect effects were based on a 95-percentile bootstrap CI.
Results of the alternative mediational models were nonsignificant when expectancies and motives were entered as (X1,2) and when anxiety sensitivity was the mediator (M1) for nicotine dependence (b = 0.007, 95% CI [-0.001, 0.002]), prior withdrawal-related quit problems (b = 0.001, 95% CI [0.000, .001]), and pre-cessation smoking urges (b = -.016, 95% CI [-.093, .039]) but was significant for barriers to smoking cessation (b = .007, 95% CI [.002, .015]) and nicotine withdrawal (b = .009, 95% CI [.002, .023]). Thus, holding strong affect-regulatory expectancies and motives appears to give rise to anxiety sensitivity, which in turn may give rise to perceived barriers to quitting and subjective nicotine withdrawal before the quit day.
Discussion
Cross-sectional findings indicated that among treatment-seeking smokers, higher levels of anxiety sensitivity were directly related to nicotine dependence, greater perceived barriers to smoking cessation, and more severe withdrawal-related problems during prior quit attempts. Consistent with negative-reinforcement theories of smoking (McCarthy et al., 2010), the effects of anxiety sensitivity on these smoking processes were explained, at least in part, by the combined effects of negative affect–reduction smoking expectancies and motives. All effects were observed beyond the effects of gender, problematic alcohol use, past-month cannabis use, tobacco-related medical problems, and history of emotional disorders. Thus, among high anxiety-sensitive smokers, holding strong beliefs about the negative-reinforcement properties of smoking (e.g., “Cigarettes help me reduce or handle tension”) in addition to smoking for these reasons (e.g., “When I feel ‘blue’, I smoke cigarettes” or “When I want to take my mind off cares and worries, I smoke cigarettes”) appear to be particularly relevant in explaining the greater dependence on cigarettes and perceived/actual quit difficulties. This finding uniquely contributes empirical data to support conceptual and theoretical models of anxiety sensitivity and smoking.
Anxiety sensitivity was also examined in relation to average levels of nicotine withdrawal and smoking urges during the 3 weeks before the quit day. Partially consistent with the hypotheses, higher levels of anxiety sensitivity were directly related to more severe pre-quit withdrawal symptoms but not smoking urges. However, the combined effect of negative-affect–reduction smoking expectancies and motives indirectly influenced the effect of anxiety sensitivity on pre-cessation nicotine withdrawal and smoking urges. Thus, high anxiety-sensitive smokers may report greater levels of pre-cessation nicotine withdrawal and smoking urges (even without making smoking changes) when in the context of affect regulation-oriented expectancies and motives for smoking.
In particular, anxiety sensitivity may directly increase negative-reinforcement expectancies and motives, which in turn predict increase in pre-cessation smoking urges, but anxiety sensitivity alone does not appear to directly relate to higher levels of urges during the week preceding quit day. Notably, mediation is possible without a significant total effect when there are other mediators not accounted for in the model (Hayes, 2009). Thus, a more comprehensive model of anxiety sensitivity and cessation-related processes may be warranted. Further research should examine the nature of these relations using experimental methodological designs (Zvolensky et al., 2014).
It appears that having either negative-reinforcement–based expectancies or motives accounts for the effect of anxiety sensitivity and some smoking processes (perceived or actual quit barriers, pre-cessation smoking urges). Further, even without strong beliefs about the negative-affect–reduction properties of cigarettes, smoking motives for these purposes explain anxiety sensitivity–smoking relations, specifically with nicotine dependence. The opposite is true for pre-cessation nicotine withdrawal, with negative-reinforcement smoking expectancies without such motives for smoking being associated with pre-cessation withdrawal severity. These findings, in conjunction with the primary meditational results, further confirm the importance of evaluating and clinically addressing both beliefs about the effects of smoking and actual reasons for smoking when preparing high anxiety-sensitive smokers for quitting.
Interestingly, the directionality of the mediational effects was not consistently supported via post hoc analyses. Specifically, affect-regulatory expectancies and motives were associated with perceived barriers to smoking cessation and pre-cessation nicotine withdrawal through the effect of higher levels of anxiety sensitivity, although this was not found for other smoking processes—nicotine dependence, prior withdrawal-related quit problems, or pre-cessation smoking urges. Although anxiety sensitivity is conceptualized as a risk factor for the maintenance of certain smoking processes via affect-regulatory processes, the data suggest reciprocal relations may be present for certain smoking processes. That is, holding expectancies about and being motivated to smoke for affect-regulatory properties of smoking appear to be related to perceptions about quitting and pre-cessation withdrawal, which may be explained by higher levels of anxiety sensitivity. Importantly, anxiety sensitivity and expectancies/motives were assessed cross-sectionally, which naturally limits the comprehensive understanding of these associations. Further work is needed to explore the patterning among anxiety sensitivity, affect-regulatory processes, and smoking characteristics over time.
The findings have several clinical implications. First, in the context of smoking-cessation treatment, it is increasingly evident that it is important to assess one’s interpretation of somatic distress (i.e., anxiety sensitivity) rather than just anxiety/depressive symptoms and disorders per se. Second, for high anxiety-sensitive smokers, it is important to assess beliefs about the effects smoking will produce. Psycho-educational information about the nature of negative affect, smoking, and their cyclical nature is important, and describing how catastrophically interpreting somatic sensations can further potentiate and maintain emotional distress and smoking is key. The educational focus should be that smoking does not effectively ameliorate anxiety-related problems but actually can increase anxiety symptoms and problems in the long run, presumably encouraging further reliance on smoking.
Of note, the observed direct effects in this study were moderate in size, and indirect associations were relatively small; thus the extent of the clinical relevance of such statistical effects should be understood in the context of their relative magnitude. Also, although the current study was focused on the process of smoking maintenance, it would perhaps be useful to examine how changes in anxiety sensitivity and affect-regulatory processes (expectancies/motives) affect actual smoking behavior (puff topography), cessation processes (withdrawal, urges while quitting), and abstinence outcomes. Such investigation would aid in the further elucidation of how these processes may change over the course of a cessation attempt of smoking-cessation treatment (i.e., beyond cross-sectional analyses presented here).
There are a number of study limitations. First, the sample consisted of a community-recruited, relatively homogenous group of treatment-seeking smokers with moderate nicotine dependence. In addition, the sample did not include smokers reporting active suicidal ideation or psychotic-spectrum symptoms, which may limit generalizability of the findings to certain psychiatric populations. Second, self-report measures were used as the primary assessment methodology; thus, future studies could use more comprehensive multi-method protocols. Third, although changes in smoking were not expected before cessation given that the quit date was not set until later stages of the treatment, systematic information was not available on the rate or recency of smoking immediately before the treatment appointment. Last, future research could examine the role of anxiety sensitivity over time or through experimental research designs to better isolate patterning of effects with smoking expectancies and motives in terms of actual use and how these processes may change over the course of treatment and during quitting.
Together, the current findings further uniquely document the nature of the anxiety sensitivity and pre-cessation processes as a function of negative-reinforcement–based smoking expectancies and motives. This work aids in the further conceptual understanding of anxiety sensitivity, documents how this cognitive-affective vulnerability relates to pre-quit smoking processes, and informs the assessment and treatment of emotionally vulnerable smokers.
Footnotes
This research was supported by National Institute of Mental Health Grant R01-MH076629-01A1 (awarded to Michael J. Zvolensky and Norman B. Schmidt). Samantha G. Farris is supported by a pre-doctoral National Research Service Award from the National Institute on Drug Abuse (F31-DA035564). Adam M. Leventhal’s effort was supported, in part, by National Institute on Drug Abuse Grant K08-DA025041. The content presented does not necessarily represent the official views of the National Institutes of Health, and the funding sources had no role other than financial support. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Assayag Y., Bernstein A., Zvolensky M. J., Steeves D., Stewart S. S. Nature and role of change in anxiety sensitivity during NRT-aided cognitive-behavioral smoking cessation treatment. Cognitive Behaviour Therapy. 2012;41:51–62. doi: 10.1080/16506073.2011.632437. [DOI] [PubMed] [Google Scholar]
- Babor T. F., de la Fuente J. R., Saunders J., Grant M. AUDIT The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care (English revision, WHO document No. WHO/ PSA/92.4) Geneva, Switzerland: World Health Organization; 1992. Retrieved from http://whqlibdoc.who.int/hq/1 992/WHO_PSA_92.4.pdf. [Google Scholar]
- Baker T. B., Piper M. E., McCarthy D. E., Majeskie M. R., Fiore M. C. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Battista S. R., Stewart S. H., Fulton H. G., Steeves D., Darredeau C., Gavric D. A further investigation of the relations of anxiety sensitivity to smoking motives. Addictive Behaviors. 2008;33:1402–1408. doi: 10.1016/j.addbeh.2008.06.016. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Zvolensky M. J. An evaluation of the nature of marijuana use and its motives among young adult active users. American Journal on Addictions. 2009;18:409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- Brandon T. H., Baker T. B. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:484–491. [Google Scholar]
- Brown R. A., Lejuez C. W., Kahler C. W., Strong D. R. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111:180–185. [PubMed] [Google Scholar]
- Evatt D. P., Kassel J. D. Smoking, arousal, and affect: The role of anxiety sensitivity. Journal of Anxiety Disorders. 2010;24:114–123. doi: 10.1016/j.janxdis.2009.09.006. [DOI] [PubMed] [Google Scholar]
- Fiore M. C., Jaen C. R., Baker T. B., Bailey W. C., Benowitz N., Curry S. J. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- First M. B., Spitzer R. L., Gibbon M., Williams J. B. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition (SCIDI/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2007. [Google Scholar]
- Gonzalez A., Zvolensky M. J., Vujanovic A. A., Leyro T. M., Marshall E. C. An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: Relation to smoking motives and barriers to quitting. Journal of Psychiatric Research. 2008;43:138–147. doi: 10.1016/j.jpsychires.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin R. D., Zvolensky M. J., Keyes K. M., Hasin D. S. Mental disorders and cigarette use among adults in the United States. American Journal on Addictions. 2012;21:416–423. doi: 10.1111/j.1521-0391.2012.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. F. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. [Google Scholar]
- Hayes A. F. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- Hayes A. F., Preacher K. J. Statistical mediation analysis with a multicategorical independent variable. British Journal of Mathematical and Statistical Psychology. 2014;67:451–470. doi: 10.1111/bmsp.12028. [DOI] [PubMed] [Google Scholar]
- Heatherton T. F., Kozlowski L. T., Frecker R. C., Fagerström K. O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hughes J. R., Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Ikard F. F., Green D. E., Horn D. A scale to differentiate between types of smoking as related to the management of affect. International Journal of the Addictions. 1969;4:649–659. [Google Scholar]
- Johnson K. A., Farris S. G., Schmidt N. B., Smits J. A., Zvolensky M. J. Panic attack history and anxiety sensitivity in relation to cognitive-based smoking processes among treatment-seeking daily smokers. Nicotine & Tobacco Research. 2013;15:1–10. doi: 10.1093/ntr/ntr332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K. A., Stewart S., Rosenfield D., Steeves D., Zvolensky M. J. Prospective evaluation of the effects of anxiety sensitivity and state anxiety in predicting acute nicotine withdrawal symptoms during smoking cessation. Nicotine & Tobacco Research. 2012;26:289–297. doi: 10.1037/a0024133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal A. M., Japuntich S. J., Piper M. E., Jorenby D. E., Schlam T. R., Baker T. B. Isolating the role of psychological dysfunction in smoking cessation: Relations of personality and psychopathology to attaining cessation milestones. Nicotine & Tobacco Research. 2012;26:838–849. doi: 10.1037/a0028449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal A. M., Zvolensky M. J. Anxiety, depression, and cigarette smoking: A transdiagnostic vulnerability framework to understanding emotion–smoking comorbidity. Psychological Bulletin. in press doi: 10.1037/bul0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro T. M., Zvolensky M. J., Vujanovic A. A., Bernstein A. Anxiety sensitivity and smoking motives and outcome expectancies among adult daily smokers: Replication and extension. Nicotine & Tobacco Research. 2008;10:985–994. doi: 10.1080/14622200802097555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macnee C. L., Talsma A. Development and testing of the barriers to cessation scale. Nursing Research. 1995;44:214–219. [PubMed] [Google Scholar]
- McCarthy D. E., Curtin J. J., Piper M. E., Baker T. B. Negative reinforcement: Possible clinical implications of an integrative model. In: Kassel J. D., editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 15–42. [Google Scholar]
- Perkins K. A., Karelitz J. L., Giedgowd G. E., Conklin C. A., Sayette M. A. Differences in negative mood-induced smoking reinforcement due to distress tolerance, anxiety sensitivity, and depression history. Psychopharmacology. 2010;210:25–34. doi: 10.1007/s00213-010-1811-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper M. E., Cook J. W., Schlam T. R., Jorenby D. E., Baker T. B. Anxiety diagnoses in smokers seeking cessation treatment: Relations with tobacco dependence, withdrawal, outcome and response to treatment. Addiction. 2011;106:418–427. doi: 10.1111/j.1360-0443.2010.03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rapee R. M., Medoro L. Fear of physical sensations and trait anxiety as mediators of the response to hyperventilation in nonclinical subjects. Journal of Abnormal Psychology. 1994;103:693–699. doi: 10.1037//0021-843x.103.4.693. [DOI] [PubMed] [Google Scholar]
- Reiss S., Peterson R. A., Gursky D. M., McNally R. J. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Schmidt N. B., Lerew D. R., Jackson R. J. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Strong D. R., Kahler C. W., Leventhal A. M., Abrantes A. M., Lloyd-Richardson E., Niaura R., Brown R. A. Impact of bupropion and cognitive-behavioral treatment for depression on positive affect, negative affect, and urges to smoke during cessation treatment. Nicotine & Tobacco Research. 2009;11:1142–1153. doi: 10.1093/ntr/ntp111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Zvolensky M. J., Cox B. J., Deacon B., Heimberg R. G., Ledley D. R., Cardenas S. J. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Tiffany S. T., Drobes D. J. The development and initial validation of a questionnaire on smoking urges. British Journal of Addiction. 1991;86:1467–1476. doi: 10.1111/j.1360-0443.1991.tb01732.x. [DOI] [PubMed] [Google Scholar]
- Zvolensky M. J., Farris S. G., Guillot C. R., Leventhal A. M. Anxiety sensitivity as an amplifier of subjective and behavioral tobacco abstinence effects. Drug and Alcohol Dependence. 2014;142:224–230. doi: 10.1016/j.drugalcdep.2014.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky M. J., Feldner M. T., Leen-Feldner E. W., McLeish A. C. Smoking and panic attacks, panic disorder, and agoraphobia: A review of the empirical literature. Clinical Psychology Review. 2005;25:761–789. doi: 10.1016/j.cpr.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky M. J., Schmidt N. B. Panic disorder and smoking. Clinical Psychology: Science and Practice. 2003;10:29–51. [Google Scholar]
- Zvolensky M. J., Yartz A. R., Gregor K., Gonzalez A., Bernstein A. Interoceptive exposure-based cessation intervention for smokers high in anxiety sensitivity: A case series. Journal of Cognitive Psychotherapy. 2008;22:346–365. [Google Scholar]