Abstract
Background
A chalazion is a common eyelid disease that causes eye morbidity due to inflammation and cosmetic disfigurement. Corneal topographic changes are important factors in corneal refractive surgery, intraocular lens power calculations for cataract surgery, and visual acuity assessments. However, the effects of chalazia on corneal astigmatism have not been thoroughly investigated. The changes in corneal astigmatism according to chalazion size and location is necessary for better outcome of ocular surgery. The aim of this study is to evaluate changes in corneal astigmatism according to chalazion size and location.
Methods
In this cross-sectional study, a total of 44 eyes from 33 patients were included in the chalazion group and 70 eyes from 46 patients comprised the control group. Chalazia were classified according to location and size. An autokeratorefractometer (KR8100, Topcon; Japan) and a Galilei™ dual-Scheimpflug analyzer (Ziemer Group; Port, Switzerland) were utilized to evaluate corneal changes.
Result
Oblique astigmatism was greater in the chalazion group compared with the control group (p < 0.05). Astigmatism by simulated keratometry (simK), steep K by simK, total root mean square, second order aberration, oblique astigmatism, and vertical astigmatism were significantly greater in the upper eyelid group (p < 0.05). Astigmatism by simK, second order aberration, oblique astigmatism, and vertical astigmatism were significantly greater in the large-sized chalazion group (p < 0.05). Corneal wavefront aberration was the greatest in the upper eyelid chalazion group, whole area group, and large-sized chalazion group (p < 0.05).
Conclusions
Large-sized chalazia in the whole upper eyelid should be treated in the early phase because they induced the greatest change in corneal topography. Chalazion should be treated before corneal topography is performed preoperatively and before the diagnosis of corneal diseases.
Electronic supplementary material
The online version of this article (doi:10.1186/s12886-017-0426-2) contains supplementary material, which is available to authorized users.
Keywords: Chalazia, Astigmatism, Wavefront, Corneal topography
Background
A chalazion is a meibomian gland lipogranuloma which accompanies swelling on the eyelid and eyelid tenderness [1]. It is a common eyelid disease that causes eye morbidity due to inflammation and cosmetic disfigurement [2]. A variety of factors are believed to be associated with the development of chalazia including meibomian gland dysfunction, chronic blepharitis, seborrheic dermatitis, gastritis, and smoking [1]. Chalazia treatment includes medical treatments, such as warm compression and topical antibiotic eye drops or ointment, and surgical incision and curettage, with or without triamcinolone intralesional injection [3].
Corneal topographic changes are important factors in corneal refractive surgery, intraocular lens power calculations for cataract surgery, and visual acuity assessments [4–6]. In addition, amblyopia may develop in children with corneal astigmatism [7]. It has been reported that the pressure of an upper lid chalazion induces hyperopia and astigmatism.7 Chalazia can increase higher-order aberrations (HOAs), as measured by the Hartmann–Shack aberrometer; these can affect the preoperative evaluation and refractive surgery outcomes, especially wavefront-guided approaches [8]. In addition, decreased vision due to a chalazion of the upper eyelid has been documented in a patient following laser-assisted in situ keratomileusis (LASIK) [9]. Furthermore, corneal aberration has been reported to contribute to the visual function [10, 11]. The changes in corneal astigmatism according to chalazion size and location is necessary for better outcome of ocular surgery.
However, the effects of chalazia on corneal astigmatism have not been thoroughly investigated. In this study, we investigated changes in corneal astigmatism according to chalazion size and location.
Methods
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Hallym University Medical Center. Medical charts of a total of 114 eyes from 64 patients were reviewed retrospectively in this study between July 2013 and April 2015 at the Hallym University Gangnam Sacred Heart Hospital, Seoul, South Korea. Forty four eyes from 33 patients exhibiting an eyelid chalazion were assigned to the chalazion group. The control group comprised 22 contralateral normal eyes of chalazion patients and 48 eyes from 24 patients without a chalazion, randomly selected and matched for age and sex. Patient medical history including diabetes mellitus and hypertension was obtained and a physical examination of eye and eyelid was performed prior to study procedures. Patients in the control group did not have a history of ophthalmic surgery including eyelid surgery and were not using topical or systemic medications on examination.
Chalazia were classified according to their site (upper, lower, or both eyelid groups) and location (nasal, middle, temporal, or whole area of eyelid). They also were classified into groups according to their size; small (≤1/5 of eyelid), medium (2/5–3/5), or large (>4/5).
An autokeratorefractometer (ARK; KR8100, Topcon; Japan) was utilized to measure keratometric values (K) including mean K, flat and steep K, astigmatism, and axis. Central corneal thickness (CCT), corneal topographic data, and wavefront aberration data were obtained using a Galilei™ dual-Scheimpflug analyzer (Ziemer Group; Port, Switzerland). Simulated K (simK) were obtained from the central 3-mm zone of the corneas including flat and steep K, mean K, astigmatism (difference between steep and flat Ks), and the axis of the steep meridian.
Corneal wavefront aberrations were analyzed, including total root mean square (RMS, in microns) of the total high order aberration, second order aberration, oblique astigmatism (Z−2 2), defocus (Z0 2), vertical astigmatism (Z2 2), third order aberration, vertical trefoil (Z−3 3), vertical coma (Z−1 3), horizontal coma (Z1 3), oblique trefoil (Z3 3), fourth order aberration, oblique quadrefoil (Z−4 4), secondary oblique astigmatism (Z−2 4), primary spherical aberration (Z0 4), vertical secondary astigmatism (Z2 4), and vertical quadrefoil (Z4 4).
Statistical analysis
All statistical analyses were performed using SPSS v.18.0 (IBM Corp., NY, USA). An independent t-test was used to compare the outcomes between the chalazion and control groups. Analysis of variance, followed by Tukey post hot test, was performed to determine differences between subgroups.
Results
A total 114 eyes from 64 patients were included in this study: 44 eyes in the chalazion group and 70 eyes in the control group (Table 1). Mean patient age was 40.0 ± 13.9 years in the chalazion group and 43.4 ± 14.0 years in the control group. The chalazion group was divided into the following subgroups: 1) according to site of the chalazion, the upper eyelid (n = 22), lower eyelid (n = 16), and both eyelids (n = 6), 2) according to the location of the chalazion, the nasal eyelid (n = 10), middle eyelid (n = 25), temporal eyelid (n = 4), and whole eyelid (n = 3), and 3) according to the size of the chalazion, small (n = 14), medium (n = 17), and large (n = 11) (Additional file 1).
Table 1.
Demographic data of subjects
| N | |
|---|---|
| Control | 70 |
| Chalazion group | 44 |
| Site | |
| Upper eyelid | 22 |
| Lower eyelid | 16 |
| Both eyelid | 6 |
| Location | |
| Nasal | 10 |
| Middle | 25 |
| Temporal | 4 |
| Whole | 3 |
| Size | |
| Small | 14 |
| Medium | 17 |
| Large | 11 |
Corneal topographic data for the chalazion and control groups are presented in Fig. 1 and Table 2. There was no difference in CCT different between the two groups. Astigmatism measured by ARK was not significantly different between the chalazion and control groups (p = 0.074; independent t-test). Oblique astigmatism (Z−2 2) was greater in the chalazion group compared with the control group (p = 0.013; independent t-test). Other topographic data were similar between the chalazion and control groups.
Fig. 1.
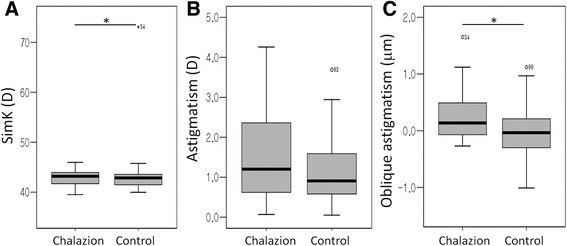
Corneal topographic data for the chalazion and control groups. Simulated K (simK; (a) and astigmatism by simK (b) is similar between the two groups. Oblique astigmatism (Z−2 2; c) is greater in the chalazion group compared with the control group (p = 0.013; independent t-test)
Table 2.
Corneal topographic data between chalazion and control group
| Total | Chalazion group | Control group | p-value | |
|---|---|---|---|---|
| N (eyes) | 114 | 44 | 70 | |
| Gender (M:F) | 52:62 | 19:25 | 33:37 | |
| Age (year) | 41.59 ± 14.08 | 39.57 ± 13.83 | 42.86 ± 14.18 | 0.226 |
| CCT (μm) | 547.25 ± 39.90 | 546.91 ± 43.64 | 547.46 ± 37.69 | 0.943 |
| Average keratometry by ARK (D) | 42.96 ± 1.86 | 42.84 ± 2.08 | 43.03 ± 1.72 | 0.603 |
| Astigmatism by ARK (D) | -0.85 ± 0.99 | −0.94 ± 1.44 | −0.79 ± 0.58 | 0.546 |
| Axis by ARK (°) | 104.23 ± 63.36 | 108.63 ± 60.74 | 101.48 ± 65.26 | 0.579 |
| SimK (D) | 42.76 ± 3.49 | 42.43 ± 2.28 | 42.96 ± 4.08 | 0.434 |
| Astigmatism by simK (D) | 1.31 ± 0.96 | 1.53 ± 1.16 | 1.17 ± 0.78 | 0.074 |
| Axis by simK (°) | 84.74 ± 35.24 | 85.16 ± 28.23 | 84.47 ± 39.20 | 0.914 |
| Mean K of posterior surface (D) | −6.28 ± 0.27 | −6.25 ± 0.24 | −6.29 ± 0.28 | 0.514 |
| Astigmatism of posterior surface (D) | −0.44 ± 0.29 | −0.46 ± 0.26 | −0.43 ± 0.32 | 0.691 |
| Total RMS (μm) | 1.81 ± 0.80 | 1.97 ± 1.05 | 1.71 ± 0.59 | 0.127 |
| 2nd order aberration (μm) | 1.55 ± 0.70 | 1.68 ± 0.87 | 1.48 ± 0.55 | 0.184 |
| Oblique astigmatism (Z−2 2; μm) | 0.04 ± 0.49 | 0.18 ± 0.52 | −0.05 ± 0.45 | 0.013* |
| Defocus (Z0 2; μm) | −0.85 ± 0.50 | −0.83 ± 0.53 | −0.87 ± 0.49 | 0.693 |
| Vertical astigmatism (Z2 2; μm) | −0.74 ± 1.06 | −0.98 ± 1.16 | −0.59 ± 0.98 | 0.057 |
| 3rd order aberration (μm) | 0.67 ± 0.42 | 0.71 ± 0.53 | 0.64 ± 0.34 | 0.398 |
| Vertical trefoil (Z−3 3; μm) | −0.18 ± 0.40 | −0.24 ± 0.44 | −0.14 ± 0.37 | 0.216 |
| Vertical Coma (Z−1 3; μm) | 0.34 ± 3.01 | 0.13 ± 0.37 | 0.48 ± 3.84 | 0.555 |
| Horizontal coma (Z1 3; μm) | −0.04 ± 0.31 | −0.04 ± 0.29 | −0.04 ± 0.33 | 0.961 |
| Oblique trefoil (Z3 3; μm) | −0.02 ± 0.44 | −0.06 ± 0.55 | −0.01 ± 0.35 | 0.378 |
| 4th order aberration (μm) | 0.40 ± 0.30 | 0.40 ± 0.30 | 0.40 ± 0.30 | 0.921 |
| Oblique quadrefoil (Z−4 4; μm) | 0.01 ± 0.09 | 0.02 ± 0.10 | 0.00 ± 0.07 | 0.293 |
| Oblique secondary astigmatism (Z−2 4; μm) | 0.01 ± 0.13 | −0.01 ± 0.14 | 0.01 ± 0.11 | 0.333 |
| Primary spherical (Z0 4; μm) | 0.17 ± 0.30 | 0.17 ± 0.32 | 0.16 ± 0.30 | 0.922 |
| Vetical secondary astigmatism (Z2 4; μm) | 0.07 ± 0.18 | 0.05 ± 0.19 | 0.08 ± 0.18 | 0.447 |
| Vertical quadrefoil (Z4 4; μm) | −0.11 ± 0.23 | −0.11 ± 0.22 | −0.12 ± 0.24 | 0.888 |
SimK simulated keratometry, ARK autorefractokeratometry, RMS root mean square, D diopter; *Statistically significant by independent t-test
The CCT was not significantly different between the chalazion site subgroups (Fig. 2, Table 3). However, astigmatism by simK, steep K by simK, total RMS, second order aberration, Z−2 2, and Z2 2 were significantly different between these subgroups (p = 0.001, 0.022, 0.002, <0.001, 0.009, and 0.001, respectively; ANOVA). Astigmatism by simK was greater in the upper eyelid group compared with the control and lower eyelid groups (p = 0.001 and 0.004, respectively; Tukey post hoc test). Steep K by simK significantly differed between upper and lower lids (p = 0.011; Tukey post hoc test). Total RMS was greater in the upper eyelid group compared with the control and lower eyelid groups (p = 0.004 and 0.003, respectively; Tukey post hoc test). Second order aberration was greater in the upper eyelid group compared with the control, lower eyelid, and whole eyelid groups (p = 0.001, <0.001, and 0.019, respectively; Tukey post hoc test). The Z−2 2 was greater in the upper eyelid group compared with the control (p = 0.06, Tukey post hoc test). The Z2 2 was greater in the upper eyelid group compared with the control and lower eyelid group, and lower in the upper eyelid group compared with whole eyelid group (p = 0.002, 0.008 and, 0.028, respectively; Tukey post hoc test).
Fig. 2.
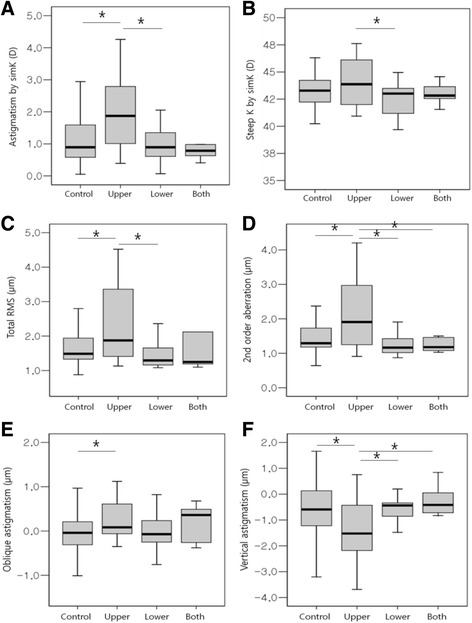
Corneal topographic data according to the site of chalazion. Chalazia are classified into control, upper, lower, or both eyelid group. Astigmatism by simulated keratometry (simK; (a), steep keratometry (K) by simK (b), total root mean square (RMS; c), second order aberration (d), oblique astigmatism (Z−2 2; e), and vertical astigmatism (Z2 2; f) are significantly different between the subgroups (p = 0.001, 0.022, 0.002, < 0.001, 0.009, and 0.001, respectively; one-way analysis of variance)
Table 3.
Corneal topographic data according to site of chalazion
| Control | Upper eyelid | Lower eyelid | Both eyelids | p-value | |
|---|---|---|---|---|---|
| n | 70 | 22 | 16 | 6 | |
| Gender (M:F) | 33:37 | 10:12 | 3:13 | 6:0 | |
| Age (year) | 42.86 ± 14.18 | 41.27 ± 12.41 | 38.63 ± 16.74 | 35.83 ± 11.16 | 0.519 |
| CCT (μm) | 547.46 ± 37.69 | 5583.27 ± 42.50 | 528.25 ± 45.57 | 555.00 ± 28.33 | 0.136 |
| Average keratometry by ARK (D) | 43.03 ± 1.72 | 43.38 ± 1.69 | 42.18 ± 2.58 | 42.82 ± 1.44 | 0.269 |
| Astigmatism by ARK (D) | -0.79 ± 0.58 | −1.12 ± 1.93 | −0.88 ± 0.85 | −0.50 ± 0.45 | 0.490 |
| Axis by ARK (°) | 101.48 ± 65.26 | 118.16 ± 67.99 | 102.50 ± 53.94 | 92.00 ± 57.73 | 0.750 |
| SimK (D) | 42.96 ± 4.08 | 43.11 ± 1.69 | 41.51 ± 2.99 | 42.42 ± 1.21 | 0.470 |
| Astigmatism by simK (D) | 1.17 ± 0.78 | 2.01 ± 1.27 | 0.98 ± 0.59 | 1.23 ± 1.26 | 0.001* |
| Axis by simK (°) | 84.47 ± 39.20 | 83.05 ± 25.31 | 88.31 ± 27.04 | 84.50 ± 43.78 | 0.470 |
| Mean K of posterior surface (D) | −6.29 ± 0.28 | −6.29 ± 0.29 | −6.24 ± 0.15 | −6.16 ± 0.25 | 0.653 |
| Astigmatism of posterior surface (D) | −0.43 ± 0.32 | −0.53 ± 0.32 | −0.36 ± 0.13 | −0.42 ± 0.16 | 0.336 |
| Total RMS (μm) | 1.71 ± 0.59 | 2.35 ± 1.13 | 1.46 ± 0.39 | 1.96 ± 1.47 | 0.002* |
| 2nd order aberration (μm) | 1.48 ± 0.55 | 2.11 ± 1.04 | 1.23 ± 0.31 | 1.24 ± 0.20 | <0.001* |
| Oblique astigmatism (Z−2 2; μm) | −0.05 ± 0.45 | 0.33 ± 0.57 | −0.03 ± 0.40 | 0.21 ± 0.43 | 0.009* |
| Defocus (Z0 2; μm) | −0.87 ± 0.49 | −0.79 ± 0.72 | −0.82 ± 0.25 | −0.99 ± 0.10 | 0.820 |
| Vertical astigmatism (Z2 2; μm) | −0.59 ± 0.98 | −1.55 ± 1.28 | −0.48 ± 0.69 | −0.25 ± 0.62 | 0.001* |
| 3rd order aberration (μm) | 0.64 ± 0.34 | 0.85 ± 0.68 | 0.55 ± 0.17 | 0.62 ± 0.43 | 0.129 |
| Vertical trefoil (Z−3 3; μm) | −0.14 ± 0.37 | −0.28 ± 0.54 | −0.16 ± 0.21 | −0.31 ± 0.50 | 0.470 |
| Vertical Coma (Z−1 3; μm) | 0.48 ± 3.84 | 0.23 ± 0.41 | −0.02 ± 0.31 | 0.18 ± 0.30 | 0.939 |
| Horizontal coma (Z1 3; μm) | −0.04 ± 0.33 | −0.025 ± 0.29 | −0.13 ± 0.31 | 0.13 ± 0.15 | 0.398 |
| Oblique trefoil (Z3 3; μm) | −0.01 ± 0.35 | −0.16 ± 0.72 | −0.01 ± 0.28 | 0.14 ± 0.30 | 0.332 |
| 4th order aberration (μm) | 0.40 ± 0.30 | 0.44 ± 0.21 | 0.39 ± 0.40 | 0.30 ± 0.27 | 0.802 |
| Oblique quadrefoil (Z−4 4; μm) | 0.00 ± 0.07 | 0.03 ± 0.14 | 0.02 ± 0.05 | −0.02 ± 0.03 | 0.422 |
| Oblique secondary astigmatism (Z−2 4; μm) | 0.01 ± 0.11 | −0.02 ± 0.16 | −0.00 ± 0.11 | 0.03 ± 0.15 | 0.618 |
| Primary spherical (Z0 4; μm) | 0.16 ± 0.30 | 0.10 ± 0.23 | 0.29 ± 0.43 | 0.11 ± 0.09 | 0.243 |
| Vetical secondary astigmatism (Z2 4; μm) | 0.08 ± 0.18 | 0.10 ± 0.21 | −0.01 ± 0.16 | 0.02 ± 0.06 | 0.230 |
| Vertical quadrefoil (Z4 4; μm) | −0.12 ± 0.24 | −0.13 ± 0.25 | −0.07 ± 0.11 | −0.15 ± 0.33 | 0.876 |
SimK simulated keratometry, ARK autorefractokeratometry, RMS root mean square, D diopter; Results were presented as mean ± standard deviation
*Statistically significant by ANOVA
Corneal topographic changes according to chalazion location are presented in Fig. 3 and Table 4. The CCT was also not significantly different between chalazion location subgroups. Astigmatism by ARK, Z−2 2, Z0 2, and Z−2 4 were significantly different between groups (p = 0.046, 0.033, 0.003, and 0.015, respectively; ANOVA). Astigmatism by ARK was significantly different between the control and temporal area groups or between middle and temporal area group (p = 0.019 and 0.025; Tukey post hoc test). The Z0 2 was greater in the whole area group compared with the control, nasal, middle, and temporal area groups (p = 0.002, 0.021, 0.001, and 0.004, respectively; Tukey post hoc test). There was a significant difference in Z−2 4 between temporal and whole area groups (p = 0.018; Tukey post hoc test).
Fig. 3.
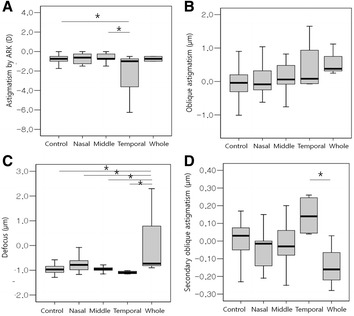
Corneal topographic changes according to the chalazion location. Chalazia are classified into control, nasal, middle, temporal, or whole area group. Astigmatism by auto-refractokeratometer (a), oblique astigmatism (Z−2 2; b), defocus (Z0 2; c), and secondary oblique astigmatism (Z−2 4; d) are significantly different between groups (p = 0.046, 0.033, 0.003, and 0.015, respectively, one-way analysis of variance)
Table 4.
Corneal topographic changes according to chalazion location
| Control | Nasal | Middle | Temporal | Whole | p-value | |
|---|---|---|---|---|---|---|
| n | 70 | 10 | 25 | 4 | 3 | |
| Gender (M:F) | 33:37 | 5:5 | 9:16 | 2:2 | 2:1 | |
| Age (year) | 42.86 ± 14.18 | 42.20 ± 16.29 | 38.12 ± 13.66 | 43.75 ± 14.48 | 45.67 ± 4.51 | 0.679 |
| CCT (μm) | 547.46 ± 37.69 | 550.50 ± 19.60 | 542.16 ± 50.65 | 542.25 ± 32.40 | 552.33 ± 14.05 | 0.952 |
| Average keratometry by ARK (D) | 43.03 ± 1.72 | 42.44 ± 1.71 | 42.83 ± 2.35 | 44.79 ± 1.51 | 42.51 ± 0.88 | 0.411 |
| Astigmatism by ARK (D) | -0.79 ± 0.58 | −0.93 ± 1.01 | −0.79 ± 58.50 | −2.58 ± 3.19 | −0.75 ± 0.35 | 0.046* |
| Axis by ARK (°) | 101.48 ± 65.26 | 108.89 ± 61.53 | 115.00 ± 58.50 | 126.67 ± 70.77 | 105.00 ± 49.50 | 0.851 |
| SimK (D) | 42.96 ± 4.08 | 41.96 ± 1.91 | 42.33 ± 2.59 | 43.47 ± 1.62 | 43.86 ± 2.15 | 0.823 |
| Astigmatism by simK (D) | 1.17 ± 0.78 | 1.16 ± 1.14 | 1.54 ± 1.13 | 1.61 ± 1.79 | 2.30 ± 0.56 | 0.143 |
| Axis by simK (°) | 84.47 ± 39.20 | 80.00 ± 33.72 | 82.92 ± 27.77 | 103.00 ± 29.06 | 92.00 ± 22.54 | 0.843 |
| Mean K of posterior surface (D) | −6.29 ± 0.28 | −6.19 ± 0.20 | −6.24 ± 0.24 | −6.40 ± 0.34 | −6.42 ± 0.37 | 0.543 |
| Astigmatism of posterior surface (D) | −0.43 ± 0.32 | −0.43 ± 0.13 | −0.45 ± 0.32 | −0.46 ± 0.19 | −0.58 ± 0.13 | 0.942 |
| Total RMS (μm) | 1.71 ± 0.59 | 1.64 ± 0.76 | 2.03 ± 1.14 | 2.09 ± 1.48 | 2.37 ± 1.05 | 0.243 |
| 2nd order aberration (μm) | 1.48 ± 0.55 | 1.35 ± 0.78 | 1.69 ± 0.82 | 1.90 ± 1.53 | 2.14 ± 0.93 | 0.219 |
| Oblique astigmatism (Z−2 2; μm) | −0.05 ± 0.45 | 0.06 ± 0.48 | 0.17 ± 0.49 | 0.44 ± 0.82 | 0.58 ± 0.47 | 0.033* |
| Defocus (Z0 2; μm) | −0.87 ± 0.49 | −0.75 ± 0.34 | −0.94 ± 0.15 | −1.09 ± 0.06 | 0.22 ± 1.80 | 0.003* |
| Vertical astigmatism (Z2 2; μm) | −0.59 ± 0.98 | −0.56 ± 1.11 | −1.00 ± 1.19 | −1.18 ± 1.68 | −1.51 ± 0.54 | 0.269 |
| 3rd order aberration (μm) | 0.64 ± 0.34 | 0.65 ± 0.36 | 0.75 ± 0.66 | 0.67 ± 0.19 | 0.71 ± 0.30 | 0.877 |
| Vertical trefoil (Z−3 3; μm) | −0.14 ± 0.37 | −0.27 ± 0.40 | −0.31 ± 0.47 | −0.01 ± 0.24 | 0.11 ± 0.51 | 0.212 |
| Vertical Coma (Z−1 3; μm) | 0.48 ± 3.84 | 0.18 ± 0.24 | 0.16 ± 0.41 | −0.12 ± 0.39 | 0.10 ± 0.46 | 0.986 |
| Horizontal coma (Z1 3; μm) | −0.04 ± 0.33 | −0.07 ± 0.26 | −0.05 ± 0.28 | 0.15 ± 0.47 | 0.00 ± 0.24 | 0.820 |
| Oblique trefoil (Z3 3; μm) | −0.01 ± 0.35 | −0.12 ± 0.42 | −0.13 ± 0.64 | 0.29 ± 0.19 | 0.10 ± 0.24 | 0.349 |
| 4th order aberration (μm) | 0.40 ± 0.30 | 0.43 ± 0.20 | 0.38 ± 0.34 | 0.36 ± 0.07 | 0.56 ± 0.50 | 0.885 |
| Oblique quadrefoil (Z−4 4; μm) | 0.00 ± 0.07 | 0.03 ± 0.14 | 0.03 ± 0.10 | 0.01 ± 0.01 | −0.05 ± 0.06 | 0.380 |
| Oblique secondary astigmatism (Z−2 4; μm) | 0.01 ± 0.11 | −0.03 ± 0.12 | −0.02 ± 0.12 | 0.15 ± 0.12 | −0.14 ± 0.16 | 0.015* |
| Primary spherical (Z0 4; μm) | 0.16 ± 0.30 | −0.03 ± 0.12 | −0.02 ± 0.12 | 0.20 ± 0.14 | −0.11 ± 0.50 | 0.590 |
| Vetical secondary astigmatism (Z2 4; μm) | 0.08 ± 0.18 | 0.17 ± 0.26 | 0.20 ± 0.34 | −0.03 ± 0.15 | 0.12 ± 0.41 | 0.754 |
| Vertical quadrefoil (Z4 4; μm) | −0.12 ± 0.24 | 0.03 ± 0.25 | 0.05 ± 0.12 | 0.01 ± 0.20 | −0.18 ± 0.39 | 0.710 |
SimK simulated keratometry, ARK autorefractokeratometry, RMS root mean square, D diopter; Results were presented as mean ± standard deviation.; *Statistically significant by ANOVA
Corneal topographic changes according to chalazion size are presented in Fig. 4 and Table 5. The CCT was not significantly different between chalazion size subgroups. Astigmatism by simK, second order aberration, Z−2 2, and Z2 2 were greater in the large-sized chalazion group (p = 0.037, 0.036, 0.006, and 0.002, respectively; ANOVA). Astigmatism by simK and second order aberration was greater in the large-sized chalazion group compared with the control (p = 0.049 for both; Tukey post hoc test). There was a significantly greater Z−2 2 in the large-sized chalazion group compared with the control (p = 0.003; Tukey post hoc test). Z2 2 was greater in the large-sized chalazion group compared with the control and small-sized chalazion groups (p = 0.015 and 0.004, respectively; Tukey post hoc test).
Fig. 4.
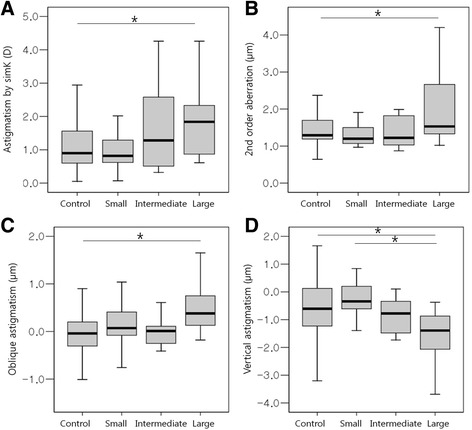
Corneal topographic changes according to chalazia size. Chalazia are classified into control, small-, medium- or large-sized groups. Astigmatism by simulated keratometry (simK; a), second order aberration (b), oblique astigmatism (Z-2 2; c), and vertical astigmatism (Z2 2; d) are significantly greater in the large-sized chalazion group (p = 0.037, 0.036, 0.006, and 0.002, respectively; one-way analysis of variance)
Table 5.
Corneal topographic changes according to chalazion size
| Control | Small | Medium | Large | p-value | |
|---|---|---|---|---|---|
| n | 70 | 14 | 17 | 11 | |
| Gender (M:F) | 33:37 | 5:9 | 6:11 | 7:4 | |
| Age (year) | 42.86 ± 14.18 | 43.64 ± 19.08 | 38.47 ± 10.72 | 38.36 ± 10.00 | 0.543 |
| CCT (μm) | 547.46 ± 37.69 | 539.29 ± 27.84 | 555.29 ± 34.43 | 535.91 ± 60.86 | 0.526 |
| Average keratometry by ARK (D) | 43.03 ± 1.72 | 43.66 ± 1.01 | 42.71 ± 2.11 | 42.09 ± 2.96 | 0.224 |
| Astigmatism by ARK (D) | -0.79 ± 0.58 | −0.85 ± 0.88 | −0.89 ± 1.67 | −1.20 ± 1.82 | 0.688 |
| Axis by ARK (°) | 101.48 ± 65.26 | 108.33 ± 50.24 | 113.75 ± 66.37 | 121.00 ± 55.42 | 0.714 |
| SimK (D) | 42.96 ± 4.08 | 43.07 ± 1.11 | 42.23 ± 2.30 | 42.05 ± 3.41 | 0.767 |
| Astigmatism by simK (D) | 1.17 ± 0.78 | 1.05 ± 0.67 | 1.69 ± 1.43 | 1.82 ± 1.13 | 0.037* |
| Axis by simK (°) | 84.47 ± 39.20 | 89.93 ± 39.47 | 80.76 ± 26.52 | 84.45 ± 13.91 | 0.917 |
| Mean K of posterior surface (D) | −6.29 ± 0.28 | −6.23 ± 0.19 | −6.25 ± 0.27 | −6.30 ± 0.29 | 0.858 |
| Astigmatism of posterior surface (D) | −0.43 ± 0.32 | −0.34 ± 0.12 | −0.54 ± 0.36 | −0.48 ± 0.14 | 0.322 |
| Total RMS (μm) | 1.71 ± 0.59 | 1.77 ± 0.96 | 1.90 ± 1.05 | 2.33 ± 1.24 | 0.113 |
| 2nd order aberration (μm) | 1.48 ± 0.55 | 1.34 ± 0.37 | 1.68 ± 1.04 | 2.06 ± 1.00 | 0.036* |
| Oblique astigmatism (Z−2 2; μm) | −0.05 ± 0.45 | 0.09 ± 0.48 | 0.09 ± 0.50 | 0.49 ± 0.55 | 0.006* |
| Defocus (Z0 2; μm) | −0.87 ± 0.49 | −0.89 ± 0.31 | −0.94 ± 0.15 | −0.56 ± 0.96 | 0.222 |
| Vertical astigmatism (Z2 2; μm) | −0.59 ± 0.98 | −0.20 ± 0.87 | −1.15 ± 1.21 | −1.60 ± 1.01 | 0.002* |
| 3rd order aberration (μm) | 0.64 ± 0.34 | 0.63 ± 0.30 | 0.64 ± 0.44 | 0.94 ± 0.84 | 0.169 |
| Vertical trefoil (Z−3 3; μm) | −0.14 ± 0.37 | −0.24 ± 0.34 | −0.23 ± 0.43 | −0.26 ± 0.60 | 0.691 |
| Vertical Coma (Z−1 3; μm) | 0.48 ± 3.84 | 0.01 ± 0.37 | 0.18 ± 0.42 | 0.22 ± 0.30 | 0.947 |
| Horizontal coma (Z1 3; μm) | −0.04 ± 0.33 | −0.11 ± 0.32 | 0.03 ± 0.24 | −0.01 ± 0.33 | 0.632 |
| Oblique trefoil (Z3 3; μm) | −0.01 ± 0.35 | −0.04 ± 0.28 | −0.02 ± 0.35 | −0.19 ± 0.98 | 0.619 |
| 4th order aberration (μm) | 0.40 ± 0.30 | 0.29 ± 0.18 | 0.38 ± 0.21 | 0.58 ± 0.45 | 0.094 |
| Oblique quadrefoil (Z−4 4; μm) | 0.00 ± 0.07 | 0.04 ± 0.12 | −0.00 ± 0.05 | 0.05 ± 0.14 | 0.296 |
| Oblique secondary astigmatism (Z−2 4; μm) | 0.01 ± 0.11 | 0.01 ± 0.13 | −0.02 ± 0.11 | −0.06 ± 0.17 | 0.264 |
| Primary spherical (Z0 4; μm) | 0.16 ± 0.30 | 0.10 ± 0.09 | 0.20 ± 0.26 | 0.22 ± 0.54 | 0.739 |
| Vetical secondary astigmatism (Z2 4; μm) | 0.08 ± 0.18 | 0.05 ± 0.16 | 0.03 ± 0.19 | 0.06 ± 0.22 | 0.840 |
| Vertical quadrefoil (Z4 4; μm) | −0.12 ± 0.24 | −0.09 ± 0.18 | −0.09 ± 0.21 | −0.15 ± 0.31 | 0.903 |
SimK simulated keratometry, ARK autorefractokeratometry, RMS root mean square, D diopter; Results were presented as mean ± standard deviation.; *Statistically significant by ANOVA
Discussion
A chalazion is a common eyelid disease, affecting individuals of all ages, caused by plugged meibomian glands and chronic lipogranulomatous inflammation [12]. Chalazia have been reported to increase corneal astigmatism and HOAs [7, 8, 13, 14]. In this study, we evaluated the effects of chalazia on the cornea according to chalazia site, location, and size using corneal topography and wavefront analysis. This study systematically revealed the mechanical effects of chalazia on corneal astigmatism. In this study, a large-sized chalazion in the whole upper eyelid induced changes in the corneal topographical and wavefront assessments. The mechanisms behind the effects of chalazia on corneal astigmatism can be suggested as follow. Firstly, with regards to the biomechanical properties of the cornea, it has been reported that its tensile strength is 3.81 ± 0.40 MPa and its stress-strain is α = 42.81 ± 11.67 and β = 2.97 ± 0.21 [15]. Compressive pressure of chalazia in excessive of these levels can induce the corneal astigmatism. In contrast, cornea under reduced strain by corneal refractive surgery (such as LASIK) may be more affected by lower pressure [9]. Secondly, lamellar orientation in human corneas has been shown to be related to mechanical properties [16, 17]. The mechanical effects increase in the meridian direction as they become closer to the center of the cornea [17]. Variations in the regional elastic performance of the human cornea have been reported; the pressure-induced meridional strains were smallest at the corneal paracenter and periphery, with the largest recorded at the limbus [18]. The circumferential strains varied less between regions with the para-centre straining to the greatest extent. In the meridional direction, Young’s modulus of elasticity was greatest at the central and para-central corneal regions, while the greatest circumferential elastic modulus was found at the limbus [17, 18]. Some authors have suggested the notion of circumferentially orientated reinforcing structures in human limbal tissue [18]. The para-central region of the human cornea was found to be stiffer in the meridional direction compared with the circumferential direction, suggesting a meridionally-orientated reinforcement of the para-central parts of the human cornea [18]. Furthermore, the human corneal stroma exhibit a preferred collagen orientation in the inferior-superior and nasal-temporal directions. However, at the limbus, the preferred orientation is tangential to the cornea [19]. Therefore, it is difficult for the pressure on the sclera to have an effect on the cornea in the meridian direction. Chalazia in the middle eyelid can more easily induce corneal astigmatism in the meridian direction because it is located superior to the cornea and close to the center of the cornea. The mass effect of a chalazion could increase with size. Chalazia generally affected Z−2, an aberration of off-axis rays. Furthermore, HOAs influence sensitivity to contrast to varying degrees at different orientations [20].
These findings may have implications in pediatric patients at risk of amblyopia [13]. In addition, transient chalazion-induced astigmatism can disturb the visual acuity, mislead intraocular lens calculation before cataract surgery, and result in serious error during refractive surgery. Therefore, in these cases, chalazia should be treated in the early phase. Long-term chalazia may induce the remodeling of corneal stroma through the secretion of inflammatory mediators including matrix metalloproteinases. Chalazia excision can decrease corneal astigmatism and irregularity; this is more prominent in single, firm, and central upper eyelid lesions [14]. Treatment modality includes incision and curettage, intralesional triamcinolone injection, and intralesional botulinum injection.
Conclusions
Large-sized chalazia in the whole upper eyelid should be treated in the early phase because they induced the greatest change in corneal topography. Chalazion should be treated before corneal topography is performed preoperatively and before the diagnosis of corneal diseases.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Research Foundation (NRF) grant (NRF-2015R1D1A1A09058505) funded by the Korea government and by Hallym University Research Fund 2016 (HURF-2016-12).
Availability of data and material
If needed, data will be shared upon request.
Authors’ contributions
Literature screening and selection was performed by KWJ and YJS. JYH and YJS participated in the design of the study. KWJ and YJS drafted the manuscript. KWJ and YJS carried out the statistical analysis. YJS and JYH interpreted the data. JYH prepare and review of the manuscript. All authors have given final approval of the version to be published. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work.
Competing interests
The Authors declare that they had no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Hallym University Medical Center. Informed consent was obtained from all subjects.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ANOVA
Analysis of variance
- ARK
Autokeratorefractometer
- CCT
Central corneal thickness
- D
Diopter
- HOA
High order aberration
- K
Keratometry
- RMS
Root mean square
Additional file
Dataset_1. The data for chalazion and corneal topography. Data were obtained from the review of medical charts of a total of 114 eyes from 64 patients between July 2013 and April 2015. Data included the size and location of chalazia and corneal topographic measurements in the chalazion group and control. (XLS 79 kb)
Contributor Information
Ki Won Jin, Email: kangajis15@gmail.com.
Young Joo Shin, Phone: 82-2-829-5193, Email: schinn@hanmail.net, Email: schinn7@naver.com.
Joon Young Hyon, Email: jyhyon@snu.ac.kr.
References
- 1.Nemet AY, Vinker S, Kaiserman I. Associated morbidity of chalazia. Cornea. 2011;30:1376–1381. doi: 10.1097/ICO.0b013e31821de36f. [DOI] [PubMed] [Google Scholar]
- 2.Ben Simon GJ, Huang L, Nakra T, Schwarcz RM, McCann JD, Goldberg RA. Intralesional Triamcinolone Acetonide Injection for Primary and Recurrent Chalazia: Is It Really Effective? Ophthalmology. 2005;112:913–917. doi: 10.1016/j.ophtha.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 3.Goawalla A, Lee V. A prospective randomized treatment study comparing three treatment options for chalazia: triamcinolone acetonide injections, incision and curettage and treatment with hot compresses. Clin Experiment Ophthalmol. 2007;35:706–712. doi: 10.1111/j.1442-9071.2007.01617.x. [DOI] [PubMed] [Google Scholar]
- 4.Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85:472–485. doi: 10.1111/j.1755-3768.2007.00879.x. [DOI] [PubMed] [Google Scholar]
- 5.Holland S, Lin DT, Tan JC. Topography-guided laser refractive surgery. Curr Opin Ophthalmol. 2013;24:302–309. doi: 10.1097/ICU.0b013e3283622a59. [DOI] [PubMed] [Google Scholar]
- 6.Myrowitz EH, Chuck RS. A comparison of wavefront-optimized and wavefront-guided ablations. Curr Opin Ophthalmol. 2009;20:247–250. doi: 10.1097/ICU.0b013e32832a2336. [DOI] [PubMed] [Google Scholar]
- 7.Santa Cruz CS, Culotta T, Cohen EJ, Rapuano CJ. Chalazion-induced hyperopia as a cause of decreased vision. Ophthalmic Surg Lasers. 1997;28:683–684. [PubMed] [Google Scholar]
- 8.Sabermoghaddam AA, Zarei-Ghanavati S, Abrishami M. Effects of chalazion excision on ocular aberrations. Cornea. 2013;32:757–760. doi: 10.1097/ICO.0b013e318268d6b3. [DOI] [PubMed] [Google Scholar]
- 9.Cosar CB, Rapuano CJ, Cohen EJ, Laibson PR. Chalazion as a cause of decreased vision after LASIK. Cornea. 2001;20:890–892. doi: 10.1097/00003226-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Packer M, Fine IH, Hoffman RS. Wavefront technology in cataract surgery. Curr Opin Ophthalmol. 2004;15:56–60. doi: 10.1097/00055735-200402000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Tang CY, Charman WN. Effects of monochromatic and chromatic oblique aberrations on visual performance during spectacle lens wear. Ophthalmic Physiol Opt. 1992;12:340–349. doi: 10.1111/j.1475-1313.1992.tb00407.x. [DOI] [PubMed] [Google Scholar]
- 12.Perry HD, Serniuk RA. Conservative treatment of chalazia. Ophthalmology. 1980;87:218–221. doi: 10.1016/S0161-6420(80)35250-0. [DOI] [PubMed] [Google Scholar]
- 13.Bagheri A, Hasani HR, Karimian F, Abrishami M, Yazdani S. Effect of chalazion excision on refractive error and corneal topography. Eur J Ophthalmol. 2009;19:521–526. doi: 10.1177/112067210901900401. [DOI] [PubMed] [Google Scholar]
- 14.Park YM, Lee JS. The effects of chalazion excision on corneal surface aberrations. Cont Lens Anterior Eye. 2014;37:342–345. doi: 10.1016/j.clae.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Zeng Y, Yang J, Huang K, Lee Z, Lee X. A comparison of biomechanical properties between human and porcine cornea. J Biomech. 2001;34:533–537. doi: 10.1016/S0021-9290(00)00219-0. [DOI] [PubMed] [Google Scholar]
- 16.Boote C, Dennis S, Huang Y, Quantock AJ, Meek KM. Lamellar orientation in human cornea in relation to mechanical properties. J Struct Biol. 2005;149:1–6. doi: 10.1016/j.jsb.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 17.Shin TJ, Vito RP, Johnson LW, McCarey BE. The distribution of strain in the human cornea. J Biomech. 1997;30:497–503. doi: 10.1016/S0021-9290(97)84433-8. [DOI] [PubMed] [Google Scholar]
- 18.Hjortdal JO. Regional elastic performance of the human cornea. J Biomech. 1996;29:931–942. doi: 10.1016/0021-9290(95)00152-2. [DOI] [PubMed] [Google Scholar]
- 19.Meek, K.M., Newton, R.H. Organization of collagen fibrils in the corneal stroma in relation to mechanical properties and surgical practice. J Refract Surg 1999;15:695-9. [DOI] [PubMed]
- 20.Murray IJ, Elliott SL, Pallikaris A, Werner JS, Choi S, Tahir HJ. The oblique effect has an optical component: Orientation-specific contrast thresholds after correction of high-orderaberrations. J Vis. 2010;10:10. doi: 10.1167/10.11.10. [DOI] [PMC free article] [PubMed] [Google Scholar]


