Abstract
Propofol (2,6-diisopropylphenol) is the most commonly used intravenous agent for induction of anesthesia. It is also used for maintenance of anesthesia and sedation in both Intensive Care Units and outpatient procedural settings. Its success in the clinical setting has been a result of its rapid onset, short duration of action, and minimal side effects despite disadvantages associated with its oil emulsion formulation. Early attempts to alter the standard emulsion or to develop new formulations with cyclodextrins and micelles to resolve issues with pain upon injection, the need for antimicrobial agents, and possible hyperlipidemia have mostly failed. With these challenges in the foreground, attention has now shifted to the use of more prodrugs and exogenous alternatives, the success of which is yet to be determined. These new agents must offer significant clinical advantages over the well-entrenched, generic propofol oil emulsion to justify higher costs and to be well received in the increasingly cost-conscious healthcare marketplace.
Key words: Alphaxalone, AZD-3043, cyclodextrin, emulsion, fospropofol, HX0507, HX0969w, induction, micelle, PF0713, propofol, prodrug
Introduction
Propofol (2,6-diisopropylphenol) is the most commonly used intravenous (IV) agent for induction of anesthesia. It is also used for maintenance of anesthesia and sedation in both Intensive Care Units (ICUs) and outpatient procedural settings. Approved propofol formulations in the United States include Diprivan injectable emulsion 1% (Fresenius Kabi USA, Lake Zurich, IL, USA), propofol injectable emulsion 1% (Pfizer, Inc.,/Hospira, Inc., New York, NY, USA), and propofol injectable emulsion 1% (Sagent Pharmaceuticals, Schaumburg, IL, USA). The popularity of propofol results from its rapid onset, short duration of action, and minimal side effects. However, it is water insoluble and difficult to formulate in a stable aqueous delivery vehicle. Disadvantages include emulsion instability,[1] hyperlipidemia,[2,3] pain upon injection,[4] microbial contamination,[5] and propofol infusion syndrome.[6,7] In this article, we provide an update on the many alternatives have been developed to potentially resolve the aforementioned issues.
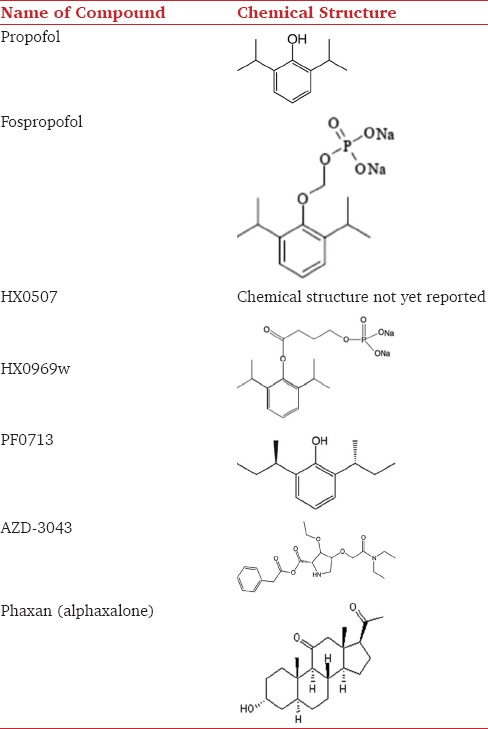
The empirical formula of propofol is C12H18O, with two isopropyl groups positioned on each side of a hydroxyl group in the ortho position on a phenol ring [Table 1]. The molecule is highly lipophilic, and miscibility can only be achieved in lipophilic substances or organic solvents. The current standard emulsion formulation for all three products on the market (standard propofol emulsion) includes soybean oil (10%), egg yolk lecithin (1.2%), and glycerol (2.25%).[8]
Table 1.
Chemical structure of propofol and its derivatives
The anesthetic properties of propofol were initially reported in 1973, followed by the first clinical trials in 1977 using a 1% preparation formulated in Cremophor EL.[9,10] However, this formulation was associated with a high incidence of anaphylaxis and was subsequently withdrawn from the market. Propofol in a lipid emulsion was subsequently evaluated in clinical trials and launched in the late 1980s.[11] However, the new emulsion was associated with clusters of postoperative infections, prompting ethylenediaminetetraacetic acid (EDTA) or metabisulfite to be added to the formulation for retardation of bacterial growth in the late 1990s.[12]
Propofol causes rapid and reliable loss of consciousness. The dose of propofol required to induce general anesthesia in adults is normally between 1.5 and 2.5 mg/kg.[13] Propofol anesthesia can be maintained either with a continuous intravenous infusion (approximately 6–12 mg/kg/h) or with intermittent bolus administrations (20–50 mg). The pharmacokinetics of propofol follows a three-compartment linear model, including the plasma, rapidly, and slowly equilibrating tissues. Initially, there is rapid equilibration of propofol levels between plasma and highly perfused tissue of the brain, accounting for the rapid onset of anesthesia. Subsequent redistribution from the brain into other slowly equilibrating tissues terminates the anesthetic effects of propofol. Propofol is mainly eliminated by hepatic conjugation to inactive glucuronide metabolites, which are excreted by the kidney.[14]
The exact mechanism of action of propofol remains unclear, but it is noted to have many pharmacological effects. Propofol directly activates γ-aminobutyric acid (GABA) receptors, which specifically interact with the β subunits, resulting in endocytosis at the GABA receptor by decreasing association with adaptin complexes AP2.[15] Propofol also inhibits glutamate receptors,[16] and reduces extracellular glutamate levels by either inhibiting sodium channel-dependent glutamate release or enhancing glutamate uptake.[17] In addition, propofol reduces cerebral blood flow, cerebral metabolic rate, and intracranial pressure.[18] It causes a global metabolic and vascular depression in the human brain, especially with a significant reduction in activity in the thalamocortical network and the frontoparietal network.[19]
Methods
The search sequence, “propofol AND (derivative OR alternative)” was performed in the Back66 file of the Medline Database via PubMed on December 1, 2015, resulting in 697 articles. The initial search was purposefully made very broad to ensure that no relevant articles were missed. No language or publication date restrictions were applied. All titles and abstracts of these studies were reviewed for relevance. In this process, 37 studies were selected based on the following criteria: (1) includes study of propofol alternative or derivative, and (2) conducts original research. Full texts of these studies were reviewed, and their references were searched for any other relevant articles. Ultimately, the results from these studies were included in this review article.
Emulsion Modifications
To overcome the disadvantages of propofol emulsions such as pain on injection and infection risk, different modifications to the emulsion formulation have been attempted with minimal success [Table 2]. The first approach was to decrease the oil content of the emulsion. Ampofol (Amphastar Pharmaceuticals, Inc., Rancho Cucamonga, CA, USA) was a 1% propofol emulsion containing 5% soybean oil and 0.6% lecithin.[45] While Ampofol provided identical anesthetic properties, had less triglyceride per dose, and was less supportive of microbial growth, it was associated with higher incidence of pain on injection.[20,21] The clinical trials for this agent were discontinued in the late 2000s.
Table 2.
Comparison of the properties of propofol derivatives
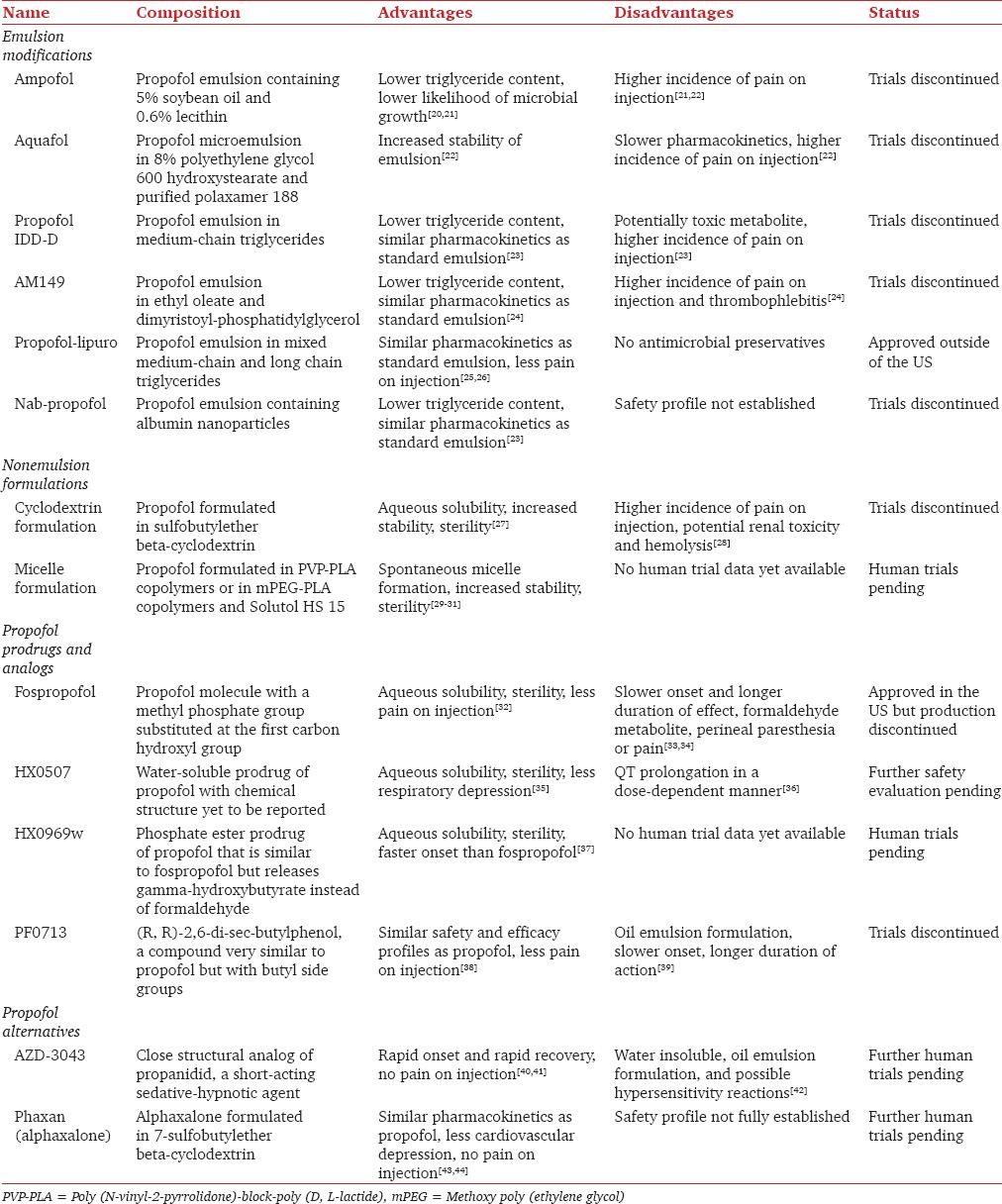
Current standard propofol emulsions consist of oil droplets between 0.15 and 0.5 µm.[46] Microemulsions with droplets smaller than 0.1 µm that are more stable have been developed. Aquafol (Daewon Pharmaceuticals, Seoul, Korea) is a 1% propofol microemulsion in 8% polyethylene glycol 600 hydroxystearate and purified poloxamer 188. In initial clinical trials, time to loss of consciousness and time to recovery of consciousness were both prolonged for Aquafol. In addition, it was associated with more severe and frequent injection pain.[22] Trials for this agent were discontinued. In 2015, a new formulation that is manufactured and stored as a microemulsion and diluted to a macroemulsion at the point of use has been developed.[47] This new approach could potentially achieve greater stability and longer shelf life without the increase in injection pain with microemulsions.
Another modification was to increase the proportion of medium-chain triglycerides (MCTs) in the emulsion. MCTs are more polar than long-chain triglycerides (LCTs) and are more rapidly metabolized, but they can release potentially toxic metabolites such as acetoacetate or octanoate.[48] These new formulations included IDD-D propofol (SkyePharma Inc., New York, NY, USA), AM149 (AMRAD Pharmaceuticals, Victoria, Australia), and Propofol-Lipuro (B. Braun, Meslungen, Germany). IDD-D propofol 2% had similar pharmacokinetics as the standard propofol emulsion. Although octanoate concentration returned to normal by 90 minutes after the termination of the infusion of IDD-D propofol, its safety was yet to be determined.[23] IDD-D propofol was shown to cause greater pain on injection and had a prolonged induction time.[23] Further development of this agent was stopped after Phase II clinical trials in 2006. AM149 contained ethyl oleate and dimyristoyl phosphatidylglycerol as emulsifiers, but it was associated with higher incidence of pain on injection and thrombophlebitis. Clinical trials for this agent were also discontinued in 1999.[24] Propofol-Lipuro® is another mixed MCT–LCT propofol formulation. The emulsion did not affect the pharmacokinetics or pharmacodynamics of propofol, caused less pain upon injection, and increased speed of triglyceride elimination.[25,26] This agent has been available outside of the United States since 1999. It is not available in the US because of the lack of EDTA in the solvent.
Emulsion modification by adding albumin to form nanoparticles of propofol has also been attempted. Nab-Propofol (American BioScience, Inc., Santa Monica, CA, USA) utilized ProtoSphere technology to form propofol particles in the range of 50–200 nm. It contained reduced oil content and showed similar anesthetic activity as the standard propofol emulsion without risk of hyperlipidemia.[49] No further studies on this formulation were published after the merger of American BioScience, Inc., and APP Pharmaceuticals, a maker of the standard propofol emulsion, in 2006.
Nonemulsion Formulations
Nonemulsion formulations of propofol have also been developed [Table 2]. One alternative to oil emulsions is the use of cyclodextrins. Cyclodextrins are capable of forming inclusion complexes with drugs having lipophilic properties while maintaining aqueous solubility.[27] Pharmacodynamic studies of propofol cyclodextrin formulations showed reduced induction times and longer duration of action in rats compared with the standard propofol emulsion.[50] The first-in-human propofol cyclodextrin formulation study used a sulfobutylether beta-cyclodextrin formulation called Captisol (Ligand Pharmaceuticals, La Jolla, CA, USA), showing no difference in the onset and duration of anesthesia but increased incidence of pain upon injection with the cyclodextrin formulation.[51] Other concerns with cyclodextrin formulations include potential renal toxicity, hemolysis, and potential binding of co-administered lipophilic drugs such as rocuronium.[28] Further investigations are necessary to determine the safety and suitability of this new formulation, but it is unclear whether more clinical trials on this new formulation are being pursued.
Micelle formulations of propofol have also been attempted. Potential advantages of micelles include enhanced stability, spontaneous micelle formation, and possible sterilization. However, early studies of poloxamers for propofol delivery were largely unsuccessful. In 2008, a polymeric micelle formulation was developed using poly(N-vinyl-2-pyrrolidone)-block-poly (D, L-lactide) (PVP-PLA) copolymers to dissolve propofol and form a solid lyophilizate, Propofol-PM (Paladin Labs, Inc., Montreal, Canada).[29] The addition of an aqueous medium reconstitutes the compound to a clear solution instantaneously. Initial animal experiments show similar kinetics as the standard propofol emulsion in whole blood, and there was no statistically significant difference in the timing of recovery endpoints compared to the standard propofol emulsion.[29] The greatest advantage was that the PVP-PLA formulation did not support microbial growth.[30] In 2011, another micelle formulation was developed using methoxy poly(ethylene glycol)-b-poly(D, L-lactide) diblock copolymers and Solutol HS15.[31] Initial studies showed similar kinetics and anesthetic effects as standard propofol emulsion. In addition, the free propofol content was 74% lower than that in standard emulsions, potentially reducing pain on injection.[31] Human trial data for either micelle formulation are not yet available.
Propofol Prodrugs and Analogs
Another approach to solving the propofol formulation problem has been the development of propofol prodrugs that are water-soluble and can be converted to propofol in vivo [Table 2]. Many propofol esters have been developed, such as propofol hemisuccinate, propofol hemiglutarate, propofol hemiadipate, monopropofol phosphate, and dipropofol phosphate.[46] However, only fospropofol disodium has been approved by the US Food and Drug Administration for monitored anesthesia care in adults under the brand name Lusedra (Eisai Co, Ltd., Tokyo, Japan), previously known as Aquavan. Fospropofol is a 2,6-diisopropyl phenol molecule with a methyl phosphate group substituted at the first carbon hydroxyl group on the propofol molecule [Table 1].[52] To be activated, alkaline phosphatases must cleave the molecule into the active propofol molecule, phosphate, and formaldehyde. Clinical studies did not note toxic elevations in serum formaldehyde levels.[32] Fospropofol has a slower onset and a longer duration of effect than propofol because of the enzymatic conversion process. Phase II and III clinical trials showed faster recovery and greater patient satisfaction after sedation for fospropofol compared to midazolam.[33] Safety and efficacy for monitored anesthesia care sedation using fospropofol have also been shown in bronchoscopies, short-term induction, and maintenance of sedation in mechanically ventilated ICU patients, and total IV anesthesia for coronary artery bypass surgery.[28] Finally, fospropofol causes less pain on injection than propofol but is associated with a greater incidence of perineal paresthesia or pain.[34] In 2010, six studies characterizing the pharmacokinetics of fospropofol were retracted because of possible errors in propofol assays. Production of the drug was discontinued in the early 2010s before the completion of clinical trials on its use for induction of general anesthesia.
HX0507 is another water-soluble prodrug of propofol that was found to have anesthetic effects similar to those of propofol. In beagle dogs, HX0507 was found to cause similar dose-dependent hypotension and less dose-dependent respiratory depression than propofol.[35] However, in the first-in-human study in 2009, HX0507 caused QT interval prolongation in a dose-dependent linear manner.[36] Further safety evaluations of this agent are necessary.
Furthermore, in early development is a compound called HX0969w, a water-soluble phosphate ester prodrug of propofol that is similar to fospropofol but releases gamma-hydroxybutyrate instead of formaldehyde [Table 1].[53] In initial animal pharmacodynamics comparison studies, HX0969w had similar sedative-hypnotic effects but a longer onset time and shorter duration than fospropofol.[54] Two more recent modifications to the HX0969w molecule in 2014 showed greater water solubility and faster onset of anesthesia compared to the original HX0969w compound and fospropofol in rats.[37] Further optimization of HX0969w and evaluations of its safety and efficacy in humans are required.
PF0713 (Signature Therapeutics, Palo Alto, CA, USA), with a molecular formula (R, R)-2,6-di-sec-butylphenol, is a compound very similar to propofol but with butyl side groups [Table 1]. PF0713 is a potent GABAA receptor agonist and behaves similarly to propofol in the hippocampal brain slice assay.[55] This compound was originally synthesized in 1980 as a follow-up to propofol in attempt to improve the properties of propofol. Initial studies in mice indicated that it was similar in hypnotic potency to propofol, but had a slower onset of action and longer duration of hypnotic action.[39] Phase I trials showed similar safety and efficacy profiles as propofol but caused less pain on injection.[38] It is also minimally soluble in water and has to be formulated in an oil emulsion. Further development of this drug has been discontinued.
Propofol Alternatives
Other compounds with similar clinical pharmacology profiles as propofol are also currently under investigation [Table 2]. AZD-3043 (AstraZeneca US, Wilmington, DE, USA) is a close structural analog of propanidid [Table 1], a short-acting sedative-hypnotic agent that was introduced into clinical practice in the 1960s. It was withdrawn in 1984 because of a high incidence of anaphylactic reactions, believed to be caused by its solvent, Cremophor EL. AZD-3043 contains an additional methylene group compared to propanidid and is formulated in an oil emulsion similar to propofol. Animal studies have shown that AZD-3043 produces rapid-onset hypnosis and rapid recovery upon infusion termination, even after prolonged continuous infusion.[56] A recent first-in-human study published in 2015 showed high systemic clearance and low volume of distribution, consistent with the rapid onset and offset profile.[40,41] In addition, none of the subjects reported pain on injection in contrast to propofol.[40] However, three patients experienced episodes of erythema, chest discomfort, and dyspnea after drug administration. Another cause for concern is sporadic episodes of involuntary movements and increased muscle tone in patients on an infusion of the drug.[42] More clinical studies will follow to better assess this agent.
Phaxan (Drawbridge Pharmaceuticals, Melbourne, Australia) is another fast onset, short duration anesthetic agent with a fast cognitive recovery that completed Phase I clinical trials in 2015. It is an alphaxalone formulated in 7-sulfobutylether beta-cyclodextrin [Table 1], making it water-soluble.[43] Alphaxalone was used as a short-acting IV anesthetic used between 1972 and 1984, but it was withdrawn from the market because its solvent, Cremophor EL, was associated with hypersensitivity. Animal studies indicated that Phaxan had a greater therapeutic index than propofol.[43] In the first-in-human trials of Phaxan, its anesthetic effects measured by time to induce hypnosis and patient recovery were similar to those of propofol.[44] Notably, Phaxan caused less cardiovascular depression than propofol and was not associated with pain on injection. No hypersensitivity reactions were noted. Further clinical trials on this new agent are underway.
Conclusion
Propofol has been a transformative anesthetic agent since its introduction 40 years ago. Its success in the clinical setting has been a result of its rapid onset, short duration of action, and minimal side effects despite disadvantages associated with its oil emulsion formulation. Early attempts to alter the standard emulsion or to develop new formulations to resolve issues with pain upon injection, the need for antimicrobial agents, and possible hyperlipidemia have mostly failed. With these challenges in the foreground, attention has now shifted to the use of more exogenous substances and novel compounds, the success of which is yet to be determined. These new agents must offer significant advantages over the well-entrenched, generic, standard propofol emulsion to justify higher costs and to be well received in the increasingly cost-conscious healthcare marketplace.
Financial support and sponsorship
Internal Department funding from Brigham and Women's Hospital/Harvard Medical School.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Park JW, Park ES, Chi SC, Kil HY, Lee KH. The effect of lidocaine on the globule size distribution of propofol emulsions. Anesth Analg. 2003;97:769–71. doi: 10.1213/01.ANE.0000074797.70349.CA. [DOI] [PubMed] [Google Scholar]
- 2.Wolf A, Weir P, Segar P, Stone J, Shield J. Impaired fatty acid oxidation in propofol infusion syndrome. Lancet. 2001;357:606–7. doi: 10.1016/S0140-6736(00)04064-2. [DOI] [PubMed] [Google Scholar]
- 3.McKeage K, Perry CM. Propofol: A review of its use in intensive care sedation of adults. CNS Drugs. 2003;17:235–72. doi: 10.2165/00023210-200317040-00003. [DOI] [PubMed] [Google Scholar]
- 4.Tan CH, Onsiong MK. Pain on injection of propofol. Anaesthesia. 1998;53:468–76. doi: 10.1046/j.1365-2044.1998.00405.x. [DOI] [PubMed] [Google Scholar]
- 5.Bennett SN, McNeil MM, Bland LA, Arduino MJ, Villarino ME, Perrotta DM, et al. Postoperative infections traced to contamination of an intravenous anesthetic, propofol. N Engl J Med. 1995;333:147–54. doi: 10.1056/NEJM199507203330303. [DOI] [PubMed] [Google Scholar]
- 6.Kam PC, Cardone D. Propofol infusion syndrome. Anaesthesia. 2007;62:690–701. doi: 10.1111/j.1365-2044.2007.05055.x. [DOI] [PubMed] [Google Scholar]
- 7.Diaz JH, Brabhakar A, Urman RD, Kaye AD. Propofol infusion syndrome: a retrospective analysis at a level 1 trauma center. Crit Care Res Pract 2014. 2014:346968. doi: 10.1155/2014/346968. PMID: 25580289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu GH, Jarstrand C, Nordenström J. Phagocyte-induced lipid peroxidation of different intravenous fat emulsions and counteractive effect of Vitamin E. Nutrition. 1999;15:359–64. doi: 10.1016/s0899-9007(99)00052-0. [DOI] [PubMed] [Google Scholar]
- 9.James R, Glen JB. Synthesis, biological evaluation, and preliminary structure-activity considerations of a series of alkylphenols as intravenous anesthetic agents. J Med Chem. 1980;23:1350–7. doi: 10.1021/jm00186a013. [DOI] [PubMed] [Google Scholar]
- 10.Kay B, Rolly G. I.C.I 35868 – The effect of a change of formulation on the incidence of pain after intravenous injection. Acta Anaesthesiol Belg. 1977;28:317–22. [PubMed] [Google Scholar]
- 11.Cummings GC, Dixon J, Kay NH, Windsor JP, Major E, Morgan M, et al. Dose requirements of ICI 35,868 (propofol, ‘Diprivan’) in a new formulation for induction of anaesthesia. Anaesthesia. 1984;39:1168–71. doi: 10.1111/j.1365-2044.1984.tb06425.x. [DOI] [PubMed] [Google Scholar]
- 12.Kotani Y, Shimazawa M, Yoshimura S, Iwama T, Hara H. The experimental and clinical pharmacology of propofol, an anesthetic agent with neuroprotective properties. CNS Neurosci Ther. 2008;14:95–106. doi: 10.1111/j.1527-3458.2008.00043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bryson HM, Fulton BR, Faulds D. Propofol. An update of its use in anaesthesia and conscious sedation. Drugs. 1995;50:513–59. doi: 10.2165/00003495-199550030-00008. [DOI] [PubMed] [Google Scholar]
- 14.Raoof AA, van Obbergh LJ, de Ville de Goyet J, Verbeeck RK. Extrahepatic glucuronidation of propofol in man: Possible contribution of gut wall and kidney. Eur J Clin Pharmacol. 1996;50:91–6. doi: 10.1007/s002280050074. [DOI] [PubMed] [Google Scholar]
- 15.Ito Y, Izumi H, Sato M, Karita K, Iwatsuki N. Suppression of parasympathetic reflex vasodilatation in the lower lip of the cat by isoflurane, propofol, ketamine and pentobarbital: Implications for mechanisms underlying the production of anaesthesia. Br J Anaesth. 1998;81:563–8. doi: 10.1093/bja/81.4.563. [DOI] [PubMed] [Google Scholar]
- 16.Zhan RZ, Qi S, Wu C, Fujihara H, Taga K, Shimoji K. Intravenous anesthetics differentially reduce neurotransmission damage caused by oxygen-glucose deprivation in rat hippocampal slices in correlation with N-methyl-D-aspartate receptor inhibition. Crit Care Med. 2001;29:808–13. doi: 10.1097/00003246-200104000-00026. [DOI] [PubMed] [Google Scholar]
- 17.Sitar SM, Hanifi-Moghaddam P, Gelb A, Cechetto DF, Siushansian R, Wilson JX. Propofol prevents peroxide-induced inhibition of glutamate transport in cultured astrocytes. Anesthesiology. 1999;90:1446–53. doi: 10.1097/00000542-199905000-00030. [DOI] [PubMed] [Google Scholar]
- 18.Murphy PG, Myers DS, Davies MJ, Webster NR, Jones JG. The antioxidant potential of propofol (2,6-diisopropylphenol) Br J Anaesth. 1992;68:613–8. doi: 10.1093/bja/68.6.613. [DOI] [PubMed] [Google Scholar]
- 19.Song XX, Yu BW. Anesthetic effects of propofol in the healthy human brain: Functional imaging evidence. J Anesth. 2015;29:279–88. doi: 10.1007/s00540-014-1889-4. [DOI] [PubMed] [Google Scholar]
- 20.Song D, Hamza MA, White PF, Byerly SI, Jones SB, Macaluso AD. Comparison of a lower-lipid propofol emulsion with the standard emulsion for sedation during monitored anesthesia care. Anesthesiology. 2004;100:1072–5. doi: 10.1097/00000542-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Doenicke AW, Roizen MF, Rau J, Kellermann W, Babl J. Reducing pain during propofol injection: The role of the solvent. Anesth Analg. 1996;82:472–4. doi: 10.1097/00000539-199603000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Jung JA, Choi BM, Cho SH, Choe SM, Ghim JL, Lee HM, et al. Effectiveness, safety, and pharmacokinetic and pharmacodynamic characteristics of microemulsion propofol in patients undergoing elective surgery under total intravenous anaesthesia. Br J Anaesth. 2010;104:563–76. doi: 10.1093/bja/aeq040. [DOI] [PubMed] [Google Scholar]
- 23.Ward DS, Norton JR, Guivarc'h PH, Litman RS, Bailey PL. Pharmacodynamics and pharmacokinetics of propofol in a medium-chain triglyceride emulsion. Anesthesiology. 2002;97:1401–8. doi: 10.1097/00000542-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Paul M, Dueck M, Kampe S, Fruendt H, Kasper SM. Pharmacological characteristics and side effects of a new galenic formulation of propofol without soyabean oil. Anaesthesia. 2003;58:1056–62. doi: 10.1046/j.1365-2044.2003.03345.x. [DOI] [PubMed] [Google Scholar]
- 25.Larsen R, Beerhalter U, Erdkönig R, Larsen B. Injection pain from propofol-MCT-LCT in children. A comparison with propofol-LCT. Anaesthesist. 2001;50:676–8. doi: 10.1007/s001010100213. [DOI] [PubMed] [Google Scholar]
- 26.Doenicke AW, Roizen MF, Rau J, O'Connor M, Kugler J, Klotz U, et al. Pharmacokinetics and pharmacodynamics of propofol in a new solvent. Anesth Analg. 1997;85:1399–403. doi: 10.1097/00000539-199712000-00040. [DOI] [PubMed] [Google Scholar]
- 27.Irie T, Uekama K. Pharmaceutical applications of cyclodextrins. III. Toxicological issues and safety evaluation. J Pharm Sci. 1997;86:147–62. doi: 10.1021/js960213f. [DOI] [PubMed] [Google Scholar]
- 28.Melton MS, Nielsen KC, Tucker M, Klein SM, Gan TJ. New medications and techniques in ambulatory anesthesia. Anesthesiol Clin. 2014;32:463–85. doi: 10.1016/j.anclin.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Ravenelle F, Vachon P, Rigby-Jones AE, Sneyd JR, Le Garrec D, Gori S, et al. Anaesthetic effects of propofol polymeric micelle: A novel water soluble propofol formulation. Br J Anaesth. 2008;101:186–93. doi: 10.1093/bja/aen147. [DOI] [PubMed] [Google Scholar]
- 30.Ravenelle F, Gori S, Le Garrec D, Lessard D, Luo L, Palusova D, et al. Novel lipid and preservative-free propofol formulation: Properties and pharmacodynamics. Pharm Res. 2008;25:313–9. doi: 10.1007/s11095-007-9471-5. [DOI] [PubMed] [Google Scholar]
- 31.Li X, Zhang Y, Fan Y, Zhou Y, Wang X, Fan C, et al. Preparation and evaluation of novel mixed micelles as nanocarriers for intravenous delivery of propofol. Nanoscale Res Lett. 2011;6:275. doi: 10.1186/1556-276X-6-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fechner J, Schwilden H, Schüttler J. Modern Anesthetics. Springer Berlin Heidelberg; 2008. Pharmacokinetics and pharmacodynamics of GPI 15715 or fospropofol (Aquavan injection) – A water-soluble propofol prodrug; pp. 253–266. [DOI] [PubMed] [Google Scholar]
- 33.Cohen LB, Cattau E, Goetsch A, Shah A, Weber JR, Rex DK, et al. A randomized, double-blind, phase 3 study of fospropofol disodium for sedation during colonoscopy. J Clin Gastroenterol. 2009;44:1. doi: 10.1097/MCG.0b013e3181c2987e. [DOI] [PubMed] [Google Scholar]
- 34.Struys MM, Vanluchene AL, Gibiansky E, Gibiansky L, Vornov J, Mortier EP, et al. AQUAVAN injection, a water-soluble prodrug of propofol, as a bolus injection: A phase I dose-escalation comparison with DIPRIVAN (part 2): Pharmacodynamics and safety. Anesthesiology. 2005;103:730–43. doi: 10.1097/00000542-200510000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Lei L, Liu J. Respiratory and cardiovascular safety of HX0507 in beagle dogs. Anesthesiology. 2007;107:A1102. [Google Scholar]
- 36.Xue X, Zhu T, Zhang W, Kang Y, Liu J. Effect of HX0507, a water-soluble propofol pro-drug, on subarachnoid hemorrhage-induced cerebral vasospasm in rabbits. Neural Regen Res. 2009;4:890–5. [Google Scholar]
- 37.Lang BC, Yang J, Wang Y, Luo Y, Kang Y, Liu J, et al. An improved design of water-soluble propofol prodrugs characterized by rapid onset of action. Anesth Analg. 2014;118:745–54. doi: 10.1213/ANE.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 38.Siegel LC, Konstantatos A. PF0713 produced rapid induction of general anesthesia without injection pain in a phase 1 study. Anesthesiology. 2009;111:A869. [Google Scholar]
- 39.Siegel LC, Pelc LR, Shaff K. Dose response of PF0713, a novel investigational intravenous anesthetic agent. Anesthesiology. 2008;109:A869. [Google Scholar]
- 40.Norberg Å, Koch P, Kanes SJ, Björnsson MA, Barassin S, Ahlén K, et al. A bolus and bolus followed by infusion study of AZD3043, an investigational intravenous drug for sedation and anesthesia: Safety and pharmacodynamics in healthy male and female volunteers. Anesth Analg. 2015;121:894–903. doi: 10.1213/ANE.0000000000000804. [DOI] [PubMed] [Google Scholar]
- 41.Björnsson MA, Norberg Å, Kalman S, Simonsson US. A recirculatory model for pharmacokinetics and the effects on bispectral index after intravenous infusion of the sedative and anesthetic AZD3043 in healthy volunteers. Anesth Analg. 2015;121:904–13. doi: 10.1213/ANE.0000000000000814. [DOI] [PubMed] [Google Scholar]
- 42.Kalman S, Koch P, Ahlén K, Kanes SJ, Barassin S, Björnsson MA, et al. First human study of the investigational sedative and anesthetic drug AZD3043: A dose-escalation trial to assess the safety, pharmacokinetics, and efficacy of a 30-minute infusion in healthy male volunteers. Anesth Analg. 2015;121:885–93. doi: 10.1213/ANE.0000000000000831. [DOI] [PubMed] [Google Scholar]
- 43.Goodchild CS, Serrao JM, Kolosov A, Boyd BJ. Alphaxalone reformulated: A water-soluble intravenous anesthetic preparation in sulfobutyl-ether-ß-cyclodextrin. Anesth Analg. 2015;120:1025–31. doi: 10.1213/ANE.0000000000000559. [DOI] [PubMed] [Google Scholar]
- 44.Monagle J, Siu L, Worrell J, Goodchild CS, Serrao JM. A phase 1c trial comparing the efficacy and safety of a new aqueous formulation of alphaxalone with propofol. Anesth Analg. 2015;121:914–24. doi: 10.1213/ANE.0000000000000856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Song D, Hamza M, White PF, Klein K, Recart A, Khodaparast O. The pharmacodynamic effects of a lower-lipid emulsion of propofol: A comparison with the standard propofol emulsion. Anesth Analg. 2004;98:687–91. doi: 10.1213/01.ane.0000103184.36451.d7. [DOI] [PubMed] [Google Scholar]
- 46.Baker MT, Naguib M. Propofol: The challenges of formulation. Anesthesiology. 2005;103:860–76. doi: 10.1097/00000542-200510000-00026. [DOI] [PubMed] [Google Scholar]
- 47.Damitz R, Chauhan A. “Micro to macro (M2M)” – A novel approach for intravenous delivery of propofol. Int J Pharm. 2015;494:218–26. doi: 10.1016/j.ijpharm.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 48.Traul KA, Driedger A, Ingle DL, Nakhasi D. Review of the toxicologic properties of medium-chain triglycerides. Food Chem Toxicol. 2000;38:79–98. doi: 10.1016/s0278-6915(99)00106-4. [DOI] [PubMed] [Google Scholar]
- 49.Naguib M, Baker MT, Gregerson M, Desai N. Potency of albumin-stabilized propofol formulations containing low and no oil. Anesthesiology. 2003;99:A507. [Google Scholar]
- 50.Trapani G, Latrofa A, Franco M, Lopedota A, Sanna E, Liso G. Inclusion complexation of propofol with 2-hydroxypropyl-beta-cyclodextrin. Physicochemical, nuclear magnetic resonance spectroscopic studies, and anesthetic properties in rat. trapani@ippo.uniba.it. J Pharm Sci. 1998;87:514–8. doi: 10.1021/js970178s. [DOI] [PubMed] [Google Scholar]
- 51.Wallentine CB, Shimode N, Egan TD, Pace NL. Propofol in a modified cyclodextrin formulation:First human study of dose-response with emphasis on injection pain. Anesth Analg. 2011;113:738–41. doi: 10.1213/ANE.0b013e31822b8648. [DOI] [PubMed] [Google Scholar]
- 52.Fechner J, Ihmsen H, Hatterscheid D, Jeleazcov C, Schiessl C, Vornov JJ, et al. Comparative pharmacokinetics and pharmacodynamics of the new propofol prodrug GPI 15715 and propofol emulsion. Anesthesiology. 2004;101:626–39. doi: 10.1097/00000542-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 53.Yang J, Yin W, Liu J, Wang Y, Zhou C, Kang Y, et al. Synthesis and characterization of novel quick-release propofol prodrug via lactonization. Bioorg Med Chem Lett. 2013;23:1813–6. doi: 10.1016/j.bmcl.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 54.Zhou Y, Yang J, Liu J, Wang Y, Zhang WS. Efficacy comparison of the novel water-soluble propofol prodrug HX0969w and fospropofol in mice and rats. Br J Anaesth. 2013;111:825–32. doi: 10.1093/bja/aet218. [DOI] [PubMed] [Google Scholar]
- 55.Sneyd JR, Rigby-Jones AE. New drugs and technologies, intravenous anaesthesia is on the move (again) Br J Anaesth. 2010;105:246–54. doi: 10.1093/bja/aeq190. [DOI] [PubMed] [Google Scholar]
- 56.Egan TD, Obara S, Jenkins TE, Jaw-Tsai SS, Amagasu S, Cook DR, et al. AZD-3043: A novel, metabolically labile sedative-hypnotic agent with rapid and predictable emergence from hypnosis. Anesthesiology. 2012;116:1267–77. doi: 10.1097/ALN.0b013e31825685a6. [DOI] [PMC free article] [PubMed] [Google Scholar]


